Abstract
Respiratory epithelial adenomatoid hamartoma (REAH) is an uncommon, benign glandular proliferation that arises from the surface epithelium of the nasal cavity and paranasal sinuses. Here we report a case, wherein a 62-year male from northern Kerala presented with bilateral nasal obstruction, loss of sense of smell, and bilateral nasal discharge. On examination, a polypoidal lesion was observed in the left nasal cavity, filling the entire left middle meatus. Diagnostic nasal endoscopy revealed a multilobulated polypoidal mass in the left nasal cavity extending posteriorly into the nasopharynx and causing partial occlusion of the (R) choana. Computerized tomography(CT) imaging was suggestive of a mass in (L) nasal cavity extending from the frontal sinus to the inferior turbinate and posteriorly extending into the nasopharynx. The patient underwent Endoscopic endonasal excision of the (L)nasal mass and intraoperatively the mass was seen to arise from the septum in the (L) nasal cavity posteriorly. Histopathological examination confirmed the diagnosis of REAH.
This case report emphasizes the significance of including REAH in the differential diagnosis of sinonasal masses as it simulates other inflammatory disorders. Appropriate diagnosis by biopsy prevents unnecessary aggressive surgery as this benign condition mimics malignant lesions. More research is needed to understand the etiopathogenesis and diagnostic usefulness of immunohistological staining in REAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bilateral sinonasal conditions are frequently encountered in otolaryngology practices. However, unilateral sinonasal masses are less common, and when discovered during clinical evaluations, these lesions require careful examination for potential malignancy until proven otherwise. Albrecht coined the term “hamartoma” for the first time in 1904 to refer to an abnormal growth with excessive tissue proliferation that is local to the affected area [1]. These tumors are uncommon in the head and neck region, particularly in the nose and paranasal sinuses [2].
Respiratory epithelial adenomatoid hamartomas (REAHs) are benign, glandular proliferations arising from the surface epithelium of the nasal cavity and paranasal sinuses. REAH is first reported by Wenig and Heffner in 1995 [3]. These lesions can manifest either in association with nasal polyps or as isolated growths, with the former being more common [4]. Since various sino-nasal masses and potentially cancerous pathologies, including nasal polyps or inverted papillomas, resembling clinically and radiologically similar to REAHs [2], it is essential to distinguish REAHs from these illnesses. Males, particularly those in their fifties and sixties, are more prone to developing REAH [5]. The underlying cause of REAH remains unclear. In order to differentiate REAHs from more aggressive diseases and prevent needless surgical treatments, obtaining a tissue biopsy is crucial. This case report details the diagnosis and treatment of a middle-aged male presenting with a unilateral nasal mass, finally diagnosed as REAH.
Case Report
A 62-year male from North Kerala presented with complaints of left-sided nasal blockage, bilateral nasal discharge, and loss of sense of smell for 01 year. The patient denied any past experience with allergies and other ENT complaints.
On anterior rhinoscopy, a deviated nasal septum was observed on the right side, with a spur touching the right inferior turbinate. There was a Polypoidal growth in the left middle meatus region. Diagnostic nasal endoscopy indicated the presence of a lobulated polypoid mass in the left nasal cavity. The anterior portion of the mass appeared pink, sensitive to touch, and bled on probing(Fig. 1a) while the posterior portion was greyish, soft, insensitive, and had not bled on probing. The mass was seen to extend posteriorly into the nasopharynx and behind the septum, partially obstructing the right choana(Fig. 1b). It was possible to pass a probe superior, lateral, and inferior to the mass during the examination but not medially.
CECT Nose & Paranasal Sinus revealed an expansion and obstruction of (L) nasal cavity due to a homogenous soft tissue lesion of size 70 mm x 25 mm x 60 mm. The mass lesion was found to extend superiorly from the frontal sinus to the inferior turbinate inferiorly(Fig. 2a), involving the frontal sinus, the frontal recess, agar nasi cells & anterior ethmoids along with the superior and middle turbinate. Anteriorly it is confined to (L) nasal cavity while posteriorly, it was found to extend beyond the posterior choana and protrude into the nasopharynx with partial obstruction of the right choana (Fig. 2b).
(a). Coronal section of CECT Nose and PNS: homogenous soft tissue lesion in (L) nasal cavity of size 70 mm x 25 mm x 60 mm extending superiorly from the frontal sinus to the inferior turbinate inferiorly
(b). Axial section of CECT Nose and PNS showing extention of (L) nasal mass, anteriorly it is confined to (L) nasal cavity while posteriorly, it was found to extend beyond the posterior choana into nasopharynx with a disease-free maxillary antrum
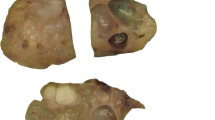
The patient underwent Endoscopic endonasal excision of the (L) nasal mass in toto under general anesthesia(Fig. 3a). Intraoperatively, the mass was found to arise from the posterior aspect of the nasal septum in the (L) nasal cavity. A papery-thin middle turbinate was observed, most likely due to pressure effects.
The post-operative hospital stay was uneventful. Histopathological examination of excised mass revealed glandular proliferation lined by respiratory epithelium found to arise from the surface respiratory epithelium, consistent with diagnosis of REHA. Individual was under follow up since one year with no signs of relapse.
Discussion
In 1995, Brit and Knight-Jones published the initial documented instance of a hamartoma in the upper aerodigestive tract [6]. In contrast to neoplasms, hamartomas demonstrate impeded growth and are usually self-limiting. Although hamartomas frequently develop in the intestine, kidney, and lung [4], their occurrence in the head and neck area, nose, and paranasal sinuses is infrequent [2].
REAHs are non-cancerous glandular growths that originate from the surface epithelium of the nasal cavity and paranasal sinuses. In a study by Hawley et al., REAH was associated with nasal polyps in 67% of cases in a series of 45 patients [4]. The cause of REAH is unclear, but its frequent connection with nasal polyps indicates an inflammatory source. However, some authors argue that inflammation occurs secondary to mass growth. Other etiological factors proposed include developmental congenital malformation or a benign neoplasm spectrum [7]. REAH predominantly affects males during their 5th and 6th decades [5].
Owing to the strong association with nasal polyps and inflammation, REAHs manifest symptoms similar to chronic inflammatory diseases. Around 70% of these lesions arise in the nasal cavity, primarily from the posterior septum, and subsequently from the ethmoid and frontal sinuses [6]. Typical symptoms comprise nasal obstruction, rhinorrhoea, facial pressure, pain, headache, and anosmia [8]. On nasal endoscopy, REAH appears as a pinkish, fleshy, distinct mass without specific features to distinguish it from other sinonasal lesions [1]. It is extremely difficult to distinguish REAH from other sinonasal masses in terms of clinical and radiological features [2]. However, subtle differences like polyp-like gross morphology, frequent origin from the septum, and indurated & firm consistency should raise suspicion. Inverted Schneiderian papillomas and adenocarcinomas are among the possible differential diagnoses for adenomatoid hamartomas [9].
Histopathological examination remains the gold standard for diagnosis. Prompt and accurate diagnosis avoids unnecessary aggressive surgery for a benign and curable condition. REAH presents distinctive histopathological characteristics, whether it appears alone or in conjunction with nasal polyps [5]. Glandular proliferation distended with mucous, and separated by stroma is a dominant histological feature. The surface epithelium invaginates into the submucosa in direct continuity with the glands. A thickened, hyalinised glandular basement membrane that envelopes the proliferating glands is another typical finding unique to REAH in contrast, nasal polyps. Inverted papillomas resemble the solitary form of RHEA. However, REAH lacks typical inverted growth of squamous epithelium as seen in Inverted papilloma.
It was previously believed that MIB-1 staining could help differentiate REAH from other sinonasal malignancies; However, multiple researchers have found it to be of little value in diagnosing REAH [10].
Despite its slow growth and lack of malignant potential, orbital extension and intracranial involvement is rarely possible [11]. Endoscopic endonasal excision of REAH is usually curative. Recurrence is extremely rare [4]. Although it is rare, REAH should be considered as a potential differential diagnosis in clinical practice.
Conclusion
REAH is a rare and frequently misdiagnosed sinonasal lesion. Additional investigation into the etiology, pathogenesis of REAH, and the value of immunohistological staining is required. Otorhinolaryngologists should consider REAH as a potential differential diagnosis for sinonasal masses due to its clinical and radiological resemblance to other pathologies. Early recognition and definitive diagnosis through histopathology can prevent unnecessary aggressive surgical interventions for this benign and completely curable disease.
References
Nguyen et al published a review on Respiratory Epithelial Adenomatoid Hamartoma in the nasal cavity titled “Am J Rhinol Allergy” in 2014. https://doi.org/10.2500/ajra.2014.28.4085
Fitzhugh VA, Mirani N conducted a review on Respiratory Epithelial Adenomatoid Hamartoma, which was published in the journal Head Neck Pathology in 2008. https://doi.org/10.1007/s12105-008-0064-3
Wenig BM, Heffner CDK investigated 31 cases of respiratory epithelial adenomatoid hamartomas in sinonasal and nasopharyngeal regions. The study was published in 1995 in the Annals of Otology, Rhinology & Laryngology. https://doi.org/10.1177/000348949510400809
Hawley et al (2012) discussed the presentation and clinical significance of sinonasal respiratory epithelial adenomatoid hamartoma (REAH) in the International Forum of Allergy & Rhinology. https://doi.org/10.1002/alr.21083
Rom et al ‘s 2018 case report highlights the importance of considering respiratory epithelial adenomatoid hamartoma (REAH) as a differential diagnosis for sinonasal masses. The study can be found in Cureus. https://doi.org/10.7759/cureus.2495
Bradoo J Dhorje, and Agrawal discussed the challenges in diagnosing respiratory epithelial adenomatoid hamartoma in sinonasal lesions in their study published in BMJ Case Reports in 2019. https://doi.org/10.1136/bcr-2019-230082
Cathro C Jo, Mills, and Stelow conducted a study on low-grade sinonasal adenocarcinomas. The article, “Low-grade Sinonasal Adenocarcinomas,“ was published in The American Journal of Surgical Pathology in 2009 and can be found in volume 33, issue 3, pages 401–408. https://doi.org/10.1097/pas.0b013e3181874ee8
Wang MB, Bhuta S, Vira (2011) D investigated hamartomas with respiratory epithelial adenomas, as reported in Laryngoscope in The article can be found in volume 121, issue 12, pages 2706. https://doi.org/10.1002/lary.22399
Inaba H, Takahashi M, Hara M, Endo R, Tsukuda M (2002) Nasal cavity respiratory epithelial adenomatoid hamartoma. Acta Oto-Laryngol 122(4):398–400. https://doi.org/10.1080/00016480260000085
Wenig BM, Heffner CDK conducted a study on 31 cases of respiratory epithelial adenomatoid hamartomas in the nasal and sinonasal regions. Their research was published in Annals of Otology, Rhinology & Laryngology in 1995 and can be found in volume 104, issue 8, pages 639–645. https://doi.org/10.1177/000348949510400809
Athre and Ducic discusses frontal sinus hamartomas (2005) Am J Otolaryngol published article in. https://doi.org/10.1016/j.amjoto.2005.05.007
Funding
No funding was provided for the creation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
No conflicts of interest.
Consent to Publish
The patient provided informed/written consent for the publication of the case study.
Competing Interests
There are no material financial or non-financial interests to disclose by the authors.
No research involving human participants or animals was conducted.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sudheer kumar, M., Bishnoi, T., Sahu, P.K. et al. An Inflammatory Polyp-Like Benign Sinonasal Mass Lesion - Respiratory Epithelial Adenomatoid Hamartoma: A Case Report. Indian J Otolaryngol Head Neck Surg 75, 3999–4002 (2023). https://doi.org/10.1007/s12070-023-04012-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04012-9