Abstract
Computerized tomography (CT) and magnetic resonance (MR) are complementary in the imaging of the labyrinth, the internal auditory canal and the brain in children with sensorineural hearing loss who are being evaluated for cochlear implantation. An accurate anatomical description of the inner ear is essential in the preoperative work up. Computerized tomography visualizes the bony structures, whereas MR can discern soft-tissue components including intra labyrinthine fluid, cerebrospinal fluid (CSF), nerves, and vessels within the IAC. This prospective study was conducted in the Department of Otorhinolaryngology, Head & Neck Surgery, Government Medical College, Srinagar. 40 children in the age group of 1–16 years with unidentified causes of bilateral SNHL were analysed radiologically over the period of 2 years from Dec 2011 to Jan 2014. Each patient underwent MRI and high resolution CT scanning of temporal bone in axial and coronal planes. Out of the 40 patients 22 were males (55 %) and 18 were females (45 %). 30 patients (72.5 %)in our study had normal radiological scans. Five patients (12.5 %) had B/L large vestibular aqueduct and two patients (5 %) had internal auditory canal stenosis with cochlear nerve hypoplasia on CT and MR imaging. Cochlear dysplasia was present in two patients (5 %) and semicircular canal dysplasia was present in one patient (2.5 %) as an isolated finding on HRCT. In addition isolated cochlear nerve hypoplasia was present in one patient (2.5 %). Hyperintense basal ganglia lesion suggestive of kernicterus was present in one patient (2.5 %) and hyperintense posterior parietal and occipital white matter lesions suggestive of congenital CMV infection was present in one patient (2.5 %) on MR imaging. Arachnoid cysts of middle cranial fossa was an incidental finding present in one patient. Radiological abnormalities of the inner ear are not uncommon. Computerized tomography and MRI are important modalities to analyze the inner ear in children with unexplained SNHL. MRI with an extremely small field of view should be used to study possible abnormalities of the vestibulocochlear nerves.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The prevalence of permanent, moderate to severe sensorineural HL is estimated to be between 1 and 2 per 1,000 live births [1, 2]. This disorder has a variety of causes and can be generally classified according to genetic and non-genetic etiologies. Cochleovestibular anomalies are common amongst pediatric cochlear implant candidates because they often correlate with sensorineural hearing loss. In evaluating children with unexplained SNHL, radiological studies such as high resolution CT and MR imaging have made it possible to identify a specific cause of auditory impairment. Approximately 20 % of patients with congenital hearing loss have a radiographically identifiable morphological abnormalities of inner ear [3]. In general, inner ear malformations can be associated with a wide range of hearing sensitivity [4]. As a general rule, however, the more severe is the deformity, the worse is the hearing [4]. It is generally accepted that first trimester inner ear malformations may be diagnose by HRCT. Inner ear malformations occurring beyond this time are thought to involve the membranous labyrinth only, thus not identifiable by HRCT [4].
Therefore, preoperative evaluation of cochleovestibular anatomy is an important component of the cochlear implant evaluation. The goals of the preoperative imaging evaluation are to determine whether there are cochleovestibular anomalies that preclude implantation, to evaluate for the evidence of luminal obstruction, to identify findings that may complicate the surgery or subsequent patient management, and to determine which ear may be the most appropriate to implant.
Materials and Methods
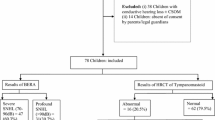
This prospective study was conducted in the Department of Otorhinolaryngology, Head & Neck Surgery, Government Medical College, Srinagar. 40 children in the age group of 1–16 years with unidentified causes of bilateral SNHL, after undergoing historical and audiological evaluation were analysed radiologically over a period of 2 years from Dec 2011 to Jan 2014. Each patient underwent MRI and high resolution CT scanning of temporal bone in axial and coronal planes. HRCT of the temporal bone was performed on a 128 slice volume in axial plane. The original isometric volume data was used to obtain coronal images. MRI was performed on 3 Tesla MRI (Siemens avanto). 3D CISS was obtained in axial and coronal planes.
Results
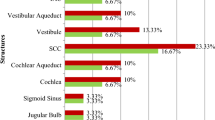
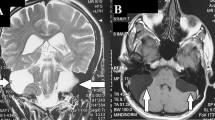
Out of the 40 patients 22 were males (55 %) and 18 were females (45 %). Moderate hearing loss was present in 3 (7.5 %), moderately severe hearing loss in 4 (10 %), severe hearing loss in 13 (32.5 %) and profound hearing loss in 20 (50 %) of the our patients. 29 patients (72.5 %) in our study had normal radiological scans. B/L large vestibular aqueduct (VA) (Fig. 1) was the most common finding being present in 5 patients (12.5 %). Two patients (5 %) had internal auditory canal stenosis (Fig. 2) with cochlear nerve hypoplasia on CT and MR imaging. B/L Duplication of the stenotic IAC (Fig. 3) was present in one these two patients. B/L Labrynthine aplasia (Michel’s anomaly) (Fig. 4) was present in one patient (2.5 %) and cochlear hypoplasia with a common cavity deformity (Mondini’s dysplasia)(Fig. 5) was present in one patient(2.5 %). Semicircular canal dysplasia (Fig. 6) was present in one patient (2.5 %) as an isolated finding on HRCT. In addition isolated cochlear nerve hypoplasia (Fig. 7) was present in one patient (2.5 %). MRI findings suggestive of kernicterus (Fig. 8) was present in one patient (2.5 %) and on enquiring the patient had history of hospital admission in neonatal period for jauidice. MRI findings of intrauterine CMV infection (Fig. 9) was present in one patient (2.5 %) whose mother had history multiple abortions and was positive for TORCH antibodies. Arachnoid cysts of middle cranial fossa (Fig. 10) was an incidental finding present in one patient with mild hearing loss (Fig. 11).
Discussion
Many children with congenital deafness will be found to have an associated cochlear malformation, typically a dilated vestibule, a wide VA, cochlear hypoplasia or a common cavity. Arrest of development during the 3rd week results in aplasia of the labyrinth, known as Michel’s anomaly. The cochlear duct has 1 and 1/2 turn by seventh week of gestation. Arrest in this development results in the classical Mondini dysplasia. The VA narrows from the fifth to the eighth week and it will be wide in ears with arrested development [4, 5]. Several reports have speculated on the cause of a sudden drop in hearing in patients with large VA;two of these possible causes are reflux of hyperosmolor fluid from the endolymphatic sac to the inner ear [6] and rupture of membranous labyrinth or perilymph fistula due to direct transmission of intracranial pressure to the inner ear through the enlarged VA [7]. Kernicterus (encephalopathy associated with severe unconjugated hyperbilirubinemia) may cause SNHL. The pattern of loss is usually mild to severe primarily affecting the higher frequencies. Mild hyperbilirubinemia less commonly produces hearing loss. However infants with hyperbilirubinemia should have hearing screening and follow up to detect delayed or progressive hearing loss [8]. Congenital internal auditory canal stenosis which implies absence or hypoplasia of the cochlear nerve is a relatively rare disorder [9]. This malformation comprises 12 % of congenital temporal bone anomalies [10, 11]. T A narrow IAC or IAC stenosis is defined as a canal of only 2 mm or less in diameter on HRCT [12–14]. The aetiology of congenital IAC stenosis is believed to be secondary to aplasia or hypoplasia of the vestibulocochlear nerve [13, 15]. There are two theories to explain the association of IAC stenosis with the absence of the cochleovestibular nerve. In the first theory, it is believed to be secondary to agenesis of the cochleo-vestibular nerve. This is due to the absence or failure of chemotactic factors directing nerve growth to their respective end organs or secondary to the absence of the end organs, the cochlea or vestibule [13, 16]. The other theory is that the bony defect is primary, inhibiting growth of the eighth nerve and resulting in impaired transmission of signal from an intact cochlea [15, 16]. To date, only seven cases of narrow IAC with duplication have been reported in the literature [17–23]. Narrow IAC with duplication associated with congenital sensorineural hearing loss and normal facial nerve function is extremely rare, and to the best of our knowledge, the patient in the present study may be 8th case reported for this malformation.
Radiographic imaging of the temporal bone is invaluable to the otological surgeon contemplating cochlear implantation [24]. Initial radiological evaluation of the cochlear implant candidate is typically performed with high resolution CT scanning. HRCT scanning technology has increased the ability to ascess the structures within the petrous pyramid [25]. An HRCT scan of the temporal bone reveals four major features: inner ear malformations, the patency of cochlear coils, the position of the juglar bulb (which if high enough may reach up to the level of the round window), and the presence of the retrocochlear and infracochlear air cells which may be mistaken for to round window niche [26].
Magnetic resonance techniques have been used to image the cochlea. The use of T2-weighted imaging offers the opportunity for diagnosis and preoperative assessment of the patients with congenital or acquired vestibulocochlear disease. This is of particular relevance in the planning of cochlear implantation in which detailed preoperative assessment of cochlear morphology is important. One previous report has examined the usefulness of MR imaging in measuring the transverse diameter of the cochlear nerve, which is known to correspond closely to the remaining number of spiral ganglion cells in the cochlea itself [27]. While this approach may reduce the instance of unsuccessful implantations in the ear with severe denervation, the success of implantation also depends on the presence of a patent cochlear fluid channel for electrode insertion. By using the T2-weighted sequences, the fluid of the cochlea, the semicircular canals, and the cerebellopontine angle can be visualized. The reason for obtaining MR imaging in a patient with inner ear anomaly are two fold: identification of nonosseous partitioning of the malformed cochlea an identification of the neural structures containe within the internal auditory canal.
Computerized tomography and MRI studies are only macroscopic evaluations of the cochleovestibular apparatus form does not necessarily imply function. Evidence of a stimulable auditory neural pathway, either by documentation of prior or residual hearing or by use of promontory stimulation testing, predict a more favorable outcome. A few cochleovestibular anomalies do preclude implantation. Complete labrynthine aplasia would be an absolute contraindication for implantation on the affected side. The failure to identify a cochlear nerve by high resolution MR imaging would also contraindicate implantation regardless of the presence of an implantable cavity.
It has been postulated that there is a period during gestation when the otic capsule has achieved normal morphology but has not attained its full size. Further more, it will not attain full size if subjected to an insult during this time. However, this is not likely to result in a hearing loss in and of itself: rather, hearing loss results from simultaneous damage to the membranous labyrinth, which is also developing at this time. The abnormal bone dimensions then serve as a marker to indicate an insult occurred in utero, as opposed to a perinatal or postnatal event [27]. Processes that affect only the neuroepithelium or sensory epithelium are not radiographically detectable, because the bony labyrinth is normal. Therefore the studies of patients with sensorineural hearing loss may be radiographically normal.
Identification of inner ear malformation has direct impact on management of these children, suggesting that all children should undergo radiological imaging as an integral component of evaluation of SNHL. The plan of surgical approach, choice of amplification aid and possible prosthetic use vary with the anomaly. On comparison of two modalities, MRI has been found to be superior in identifying early ossification of labyrinth and soft tissue anomalies in the inner ear the most important of which is presence or absence of cochlear nerve [28]. HRCT of temporal bones is superior at identifying the bony labyrinth, including enlarged VA and caliber of the cochlear nerve canal [29]. The radiographic scanning therefore acts as diagnostic as well as therapeutic indicator in these patients.
References
Brookhouser P (1996) SNHL in children. Pediatr Clin North Am 43:1195–1216
Mehl AL, Thomson V (1998) New born hearing screening the great omission. Pediatrics 101:e4
Jensen J (1969) Malformations of the inner ear in deaf children. Acta Radiol Suppl 286:1–97
Jackler RK, Luxford WM, House WF (1987) Congenital malformation of inner ear: a classification based on embryogenesis. Laryngoscope 97(3, part 2):2
Valvassori GE, Clemis JD (1978) The large vestibular aqueduct syndrome. Larnygoscope 88:723–728
Levenson MJ, Parisier SC, Jacobs M et al (1989) The large vestibular aqueduct syndrome in children. Arch Otolaryngol Head Neck Surg 115:54–58
Jackler RK, De La Cruz A (1989) The large vestibular aqueduct syndrome. Laryngoscope 99:1238–1243
Barr B, Wedenberg E (1965) Perceptive hearing loss in children with respect to genesis and use of hearing aid. Acta Otolaryngol Rhinol 59:462–474
Yuen HY, Ahuja AT, Wong KT, Yue V, Van Hasselt AC (2003) Computed Tomography of common congenital lesions of the temporal bone. Clin Radiol 58:687–693
Jackler RK, Luxford WM, House WF (1987) Congenital malformations of the inner ear: a classification based on embryogenesis. Laryngoscope 97:2–14
Winslow CP, Lepore ML (1997) Imaging quiz case 1. Bilateral agenesis of lateral semicircular canals with hypoplasia of the left internal auditory canal (IAC). Arch Otolaryngol Head Neck Surg 123:1236, 1238–1239
Cho YS, Na DG, Jung JY, Hong SH (2000) Narrow internal auditory canal syndrome: parasagittal reconstruction. J Laryngol Otol 114:392–394
Shelton C, Luxford WM, Tonokawa LL, Lo WWM, House WF (1989) The narrow internal auditory canal in children: a contraindication to cochlear implants. Otolaryngol Head Neck Surg 100:227–231
McClay JE, Tandy R, Grundfast K, Choi S, Vezina G, Zalzal G, Willner A (2002) Major and minor temporal bone abnormalities in children with and without congenital sensorineural hearing loss. Arch Otolaryngol Head Neck Surg 128(6):664–671
Yates JA, Patel PC, Millman B, Gibson WS (1997) Isolated congenital internal auditory canal atresia with normal facial nerve function. Int J Pediatr Otorhinolaryngol 41:1–8
Rothschild MA, Wackym PA, Silvers AR, Som PM (1999) Iso-lated primary unilateral stenosis of the internal auditory canal. Int J Pediatr Otorhinolaryngol 50:219–224
Ferreira T, Shayestehfar B, Lufkin R (2003) Narrow, duplicated internal auditory canal. Neuroradiology 45:308–310
Cho YS, Na DG, Jung JY, Hong SH (2000) Narrow internal auditory canal syndrome: parasaggital reconstruction. J Laryngol Otol 114:392–394
Casselman JW, Offeciers FE, Govaerts PJ, Kuhweide R, Geldof H, Somers T et al (1997) Aplasia and hypoplasia of the vestibulo- cochlear nerve: diagnosis with MR imaging. Radiology 202:773–781
Demir OI, Cakmakci H, Erdag TK, Men S (2005) Narrow duplicated internal auditory canal: radiological findings and review of the literature. Pediatr Radiol 35:1220–1223
Vilain J, Pigeolet Y, Casselman JW (1999) Narrow and vacant internal auditory canal. Acta Otorhinolaryngol Belg 53:67–71
Kesser BW, Raghavan P, Mukherjee S, Carfrae M, Essig G, Hashisaki GT (2010) Imaging case of the month: duplication of the internal auditory canal: radiographic imaging case of the month. Otol Neurotol 31:1352–1353
Baik HW, Yu H, Kim KS, Kim GH (2008) A narrow internal auditory canal with duplication in a patient with congenital sensorineural hearing loss. Korean J Radiol 9:22–25
Rosenberg RA, Cohen NL, Redde L (1987) Radiographic Imaging for the cochlear Implant. Ann Otol Rhinol Laryngol 96:300–304
Wiet RJ, Pyle GM, O’Connor CA et al (1990) Computed tomography: how accurate a predictor for cochlear implantation? Laryngoscope 100:687–692
Pheps PD, Annis JA, Robinson PJ (1990) Imaging for cochlear Implants. Br J Radiol 63:512–516
Pappas et al (1990) High-resolution CT: determination of the cause of pedriatic sensorineural hearing loss. Laryngoscope 100:564–569
Parry DA, Booth T, Roland PS (2005) Adavantages of magnetic resonance imaging over computed tomography in preoperative evaluation of pedriatic cochlear implant candidates. Otol Neurotol 26:976–982
Trimble K, Blaser S, Jmaes AL et al (2007) Computed tomography and/or magnetic resonance imaging before pedriatic cochlear implantation? Developing an investigative strategy. Otol Neurotol 28:317–324
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jallu, A.S., Jehangir, M., Ul Hamid, W. et al. Imaging Evaluation of Pediatric Sensorineural Hearing Loss in Potential Candidates for Cochlear Implantation. Indian J Otolaryngol Head Neck Surg 67, 341–346 (2015). https://doi.org/10.1007/s12070-015-0819-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-015-0819-6