Abstract
Pure red cell aplasia (PRCA) is a rare hematological complication associated with thymoma. Remission of PRCA occurs after thymectomy but can reappear after a latency period even without recurrence of thymoma. We report a case and we have reviewed the literature of thymoma associated with PRCA. Because of less number of reported cases, there have been no clinical trials investigating the immunosuppression regimen following thymectomy for thymoma associated with PRCA. After reviewing the literature, we came to a conclusion that thymectomy followed by immumosuppression with the cyclosporin-containing regimen is currently the most effective treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thymoma is a common anterior mediastinal tumor. Red cell aplasia is a rare disorder that results in a severe normochromic normocytic anemia and it occurs only in 5% of patients with thymoma [1]. The spectra of disease associated with thymoma are myasthenia gravis, agammaglobulinemia, malignancy, and various hematological disorders [2]. Thymoma may be very rarely associated with agranulocytosis [3]. The term “pure red cell aplasia” (PRCA) describes normocytic normochromic anemia associated with severe reticulocytopenia and marked reduction of erythroid precursors in the bone marrow. Thymoma-associated PRCA is a common form of secondary PRCA, found in 5–13% of such patients [4]. Hematological complications with thymoma occur far less frequently and include pure red cell aplasia, autoimmune hemolytic anemia, pernicious anemia, peripheral neutropenia, agranulocytosis, thrombocytopenia, and hypogammaglobulinemia. Remission of PRCA occurs after thymectomy but can reappear after a latency period even without recurrence of thymoma [5].
Case report
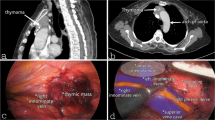
A 58-year-old male presented with symptoms of anemia expressed by pallor, dyspnea, fatigue, and palpitation during exercise which had progressively worsened during the last 2 months. On physical examination, he was moderately built and nourished with no lymphadenopathy or splenomegaly. The laboratory study revealed hemoglobin 5.4 g/dl, red blood cells (RBC) 1.72 mil/μl, mean corpuscular volume 92 μm3, mean corpuscular hemoglobin concentration 34 g/dl, reticulocytes 0.7%, leucocytes 7000 cells/cumm, and platelets 234,000 cells/uL. Bone marrow aspiration picture confirmed the diagnosis. The diagnosis of pure red cell aplasia was made and was started on oral cyclosporine. He responded well for the above treatment. He improved symptomatically and clinically. The computed tomography (CT) scan revealed a 7 × 6-cm well-defined, encapsulated heterogeneously enhancing mass in the anterior mediastinum (Fig. 1). The diagnosis of Thymoma associated with pure red cell aplasia was made and he was planned for thymectomy. He underwent thymectomy through a midline sternotomy. It was 7 × 5-cm mass with varying consistency removed in total from the anterior mediastinum. Adjacent structures like pericardium, phrenic nerve were not invaded by the tumor. Thymic mass, perithymic fat, and tissues were removed altogether. During the perioperative period, oral cyclosporine was continued. The histological examination showed a thymoma type AB. Focal capsular invasion was present with microscopic extension into mediastinal adipose tissue (Fig. 2). Mediastinal pleura was free of tumor. The extension of the tumor met the criteria of Masaoka stage I. Postoperative course was uneventful, and the patient was able to return to work after a month.
Review of literature
Among patients with thymoma, fewer than 10% will develop PRCA, whereas fewer than 5% of patients with PRCA have a thymoma. Other known associations with PRCA include medications such as erythropoietin, viral infections including parvovirus, immune disorders, ABO-incompatible hematopoietic stem cell or bone marrow transplantation, and other malignancies. Here we have reviewed the literature of thymoma associated with PRCA. Matras and Priesel were the first ones who described the association of PRCA with thymoma in 1928 [6].
Jacobs et al. reviewed the literature and found 26 cases of PRCA associated with thymoma including 2 cases reported by them. Sixteen of the 26 patients with thymoma and PRCA had thymectomies performed. Four patients (29%) obtained complete remission postoperatively. Two patients showed some improvement after thymectomy and complete cure after subsequent splenectomy and adrenocorticotropic hormone (ACTH). In these 2 cases, ACTH had no marked effect prior to thymectomy or before splenectomy [7].
Schmid et al. reported 4 cases of pure red cell aplasia associated with thymoma and none of them attained complete remission, either after thymectomy or following steroids and testosterone propionate. All 4 patients continued to have multiple blood transfusions [8].
Masaoka et al. studied seventeen cases of PRCA with thymoma clinically, histologically, and immunologically. Sixteen patients had thymectomies; one patient was unresectable due to tumor invasion. Operative procedures consisted of six simple thymectomies and ten extended thymectomies. Therapeutic effects of the operations on PRCA were evaluated. The effects were studied in 6 patients. Most of them responded to steroids, which were ineffective before surgery [9].
Charles et al. evaluated 37 PRCA patients at the University of Washington between 1982 and 1992. All patients fulfilled standard criteria for PRCA and had anemia with reticulocytopenia (reticulocyte count of < l%), normal white cell counts, normal differential counts, and normal platelet counts. Among these 37 patients, 3 patients had PRCA associated with thymoma. One patient had complete remission following thymectomy, and another had a complete remission following thymectomy along with prednisone therapy. Third patient died of Myocardial infarction (MI) 1 month after thymectomy [4].
Thompson et al. did a single institutional study at the Mayo Clinic, and they reported 13 patients treated for PRCA associated with thymoma over 50 years at their institution. All but one patient underwent surgical excision of the thymoma. The patient who did not undergo resection had significant medical co-morbidities that precluded operative intervention. None of the12 patients in their series who underwent surgery experienced complete anemia remission (complete remission, defined as hemoglobin concentration of > 11 g/dl without transfusions) after resection alone. Subsequent therapeutic interventions included danazol, corticosteroids, other immunosuppressants (cyclosporin, anti-thymocyte globulin (ATG), and azathioprine), cytotoxic agents (low-dose cyclophosphamide), androgens, splenectomy, and rituximab. One patient received multiple cytotoxic agents and mediastinal irradiation without effect, due to initial incorrect diagnosis of lymphoma at another institution. They concluded that surgical resection of the thymoma was insufficient for normalization of erythropoiesis in all cases. Cyclosporin and anti-thymocyte globulin were effective adjuvant treatments. However, treatment-related morbidity was high, with frequent infectious complications [10].
Hirokawa et al. conducted a nationwide cohort study in Japan and found 48 patients had both thymoma and PRCA. One patient who had undergone autologous hematopoietic stem cell transplantation for recurrent malignant thymoma before the onset of PRCA was excluded from this study, so 41 patients were finally selected for analysis of thymoma-associated PRCA. Thymectomy was performed in 36 patients, while four patients did not undergo surgery. The initial treatment for these patients included cyclosporine (n = 20), corticosteroids (n = 13), cyclophosphamide (n = 1), and an anabolic steroid (n = 1). Six patients did not receive any medication. Cyclosporine produced complete remission or partial remission in 19/20 patients (95%). Corticosteroids produced complete remission or partial remission in 6/13 patients (46%). Cyclophosphamide was administered to one patient who had a complete response. The time to response from the start of therapy was unknown. The one patient treated with an anabolic steroid did not achieve remission. So thymoma-associated PRCA showed an excellent response to cyclosporine-containing regimens that were effective in preventing relapse of anemia [6].
Moriyama et al. retrospectively reviewed all PRCA patients who underwent surgical resection of thymoma at Nagoya City University Hospital from April 1, 2004, to December 31, 2015. They found eight patients with PRCA among 146 patients who underwent surgical resection of thymoma. There were five males and three females, with a mean age at the surgical resection of 59 (range 45–80 years old). Five patients received preoperative chemotherapy using cytotoxic agents (n = 1) and high-dose steroids (n = 4). Extended thymectomy (n = 4) and thymectomy (n = 4) were performed in eight patients with thymoma. Complete resection was achieved macroscopically in only five patients. Cyclosporine was used to treat PRCA in six patients with or without corticosteroids, and immunosuppressive agents were not used in the other two patients, who only received an occasional transfusion. Three patients (including two who died) obtained complete remission of anemia by cyclosporine with or without corticosteroids [11].
Parry et al. reported a case of pure red cell aplasia and a benign thymic tumor in whom thymectomy had no effect on the anemia. Subsequently, prednisone therapy was followed by the restoration of normal erythropoiesis [12].
Freeman reported a case of thymoma and pure red cell anemia in which he found even after removal of the tumor that there was no improvement in the blood picture up to the time of death 18 days later [13].
Milnes et al. reported a case of thymoma and pure red cell aplasia, wherein the patient had an excess of lymphocytes in his bone marrow and high numbers of T8-positive cells in peripheral blood before treatment. Thymectomy followed by immunosuppression with prednisolone and cyclophosphamide effected a considerable reduction in T8-positive cells and clinical remission [14].
Fujimura et al. reported 3 cases of thymoma associated with PRCA. Case 1, a patient with pure red blood cell aplasia and hypogammaglobulinemia, was treated after surgery with immunosuppressive agents. She did not show any remission and died 8 months after the operation. Case 2, a patient with pure red blood cell aplasia alone, showed transient erythropoiesis only in the early postoperative period and died 1 year and 7 months after the operation. Patient 3 had pure red blood cell aplasia alone before surgery and was treated after surgery with prednisolone and fluoxymesterone. He showed good remission from the aplasia after these treatments [15].
The case reported by Masuda et al. showed no beneficial effect after treating with prednisolone, thymectomy, and cyclophosphamide. After the initiation of cyclosporin therapy, the patient developed reticulocytosis. Another case of PRCA associated with malignant thymoma reported by Palmieri et al. attained complete clinical response with the combination of octreotide and prednisolone after thymectomy [16, 17].
Fujisao and Tsuda reported a case where after thymectomy, neutrophil and platelet counts quickly normalized and recovery of anemia and reticulocytosis followed. However, reticulocyte, neutrophil, and platelet counts soon declined again. Administration of cyclosporine was then started. Six weeks after the beginning of cyclosporine therapy, the patient achieved blood transfusion independence. Despite tapering off of cyclosporine therapy, the Hb remained at 12·0 g/dl in November 1997. At the last follow-up visit in June 1998, the patient was still in complete hematological remission, although a small maintenance dose of cyclosporine was still required [18].
Lahiri et al. reported a similar case, and after thymectomy, long-term corticosteroid was continued to attain remission [19].
The summary of the literature review is given in Table 1.
Summary
PRCA association with thymoma is rare. Anemia usually presents at the same time as the thymoma diagnosis, but anemia can also present years later. Though remission of anemia cannot be attained by thymectomy alone in all cases, still thymectomy is recommended. From the above literature review, though steroids, cyclophosphamide, ATG, and octreotide have been used after thymectomy, the rate of remission with cyclosporin is highest. So thymectomy followed by immunosuppression with the cyclosporin-containing regimen is currently the most effective treatment.
References
Ammus SS, Yunis AA. Acquired pure red cell aplasia. Am J Haematol. 1987;24:311–26.
Souadjian JV, Enriquez P, Silverstein MN, Pepin JM. The spectrum of diseases associated with thymoma. Coincidence or syndrome. Arch Intern Med. 1974;134:374–9.
Yip D, Rasko JE, Lee C, Kronenberg H, O’Neill B. Thymoma and agranulocytosis: two case reports and literature review. Br J Haematol. 1996;95:52–6.
Charles RJ, Sabo KM, Kidd PG, Abkowitz JL. The pathophysiology of pure red cell aplasia: implications for therapy. Blood. 1996;87:4831–8.
Mamiya S, Itoh T, Miura AB. Acquired pure red cell aplasia in Japan. Eur J Haematol. 1997;59:199–205.
Hirokawa M, Sawada K, Fujishima N, et al. Long-term response and outcome following immuno-suppressive therapy in thymoma-associated pure red cell aplasia: a nationwide cohort study in Japan by the PRCA collaborative study group. Haematologica. 2008;93:27–33.
Jacobs EM, Hutter RV, Pool JL, Ley AB. Benign thymoma and selective erythroid aplasia of the bone marrow. Cancer. 1959;12:47–57.
Schmid JR, Kiely JM, Harrison EG, Bayrd ED, Pease GL. Thymoma associated with pure red-cell agenesis. Review of literature and report of 4 cases. Cancer. 1965;18:216–30.
Masaoka A, Hashimoto T, Shibata K, Yamakawa Y, Nakamae K, Iizuka M. Thymomas associated with pure red cell aplasia. Histologic and follow- up studies. Cancer. 1989;64:1872–8.
Thompson CA, Steensma DP. Pure red cell aplasia associated with thymoma: clinical insights from a 50-year single-institution experience. Br J Haematol. 2006;135:405–7.
Moriyama S, Yano M, Haneda H, et al. Pure red cell aplasia associated with thymoma: a report of a single-center experience. J Thorac Dis. 2018;10:5066–72.
Parry EH, Kilipatrick GS, Hardisty RM. Red-cell aplasia and benign thymoma studies on a case responding to prednisone. Brit Med J. 1959;1:1154–6.
Freeman Z. Pure red-cell anaemia and thymoma: report of a case Br Med J. 1960;1:1390–2.
Milnes JP, Goorney BP, Wallington TB. Pure red cell aplasia and thymoma associated with high levels of the suppressor/cytotoxic T lymphocyte subset. Br Med J (Clin Res Ed). 1984;289:1333–4.
Fujimura S, Kondo T, Yamauchi A, Handa M, Nakada T. Experience with surgery for thymoma associated with pure red blood cell aplasia. Report of three cases. Chest. 1985;88:221–5.
Masuda M, Arai Y, Okamura T, Mizoguchi H. Pure red cell aplasia with thymoma: evidence of T-cell clonal disorder. Am J Hematol. 1997;54:324–8.
Palmieri G, Lastoria S, Colao A, et al. Successful treatment of a patient with a thymoma and pure red-cell aplasia with octreotide and prednisone. N Engl J Med. 1997;336:263–5.
Fujisao S, Tsuda H. Th1/Th2 balance alteration in the clinical course of a patient with pure red cell aplasia and thymoma. Br J Haematol. 1998;103:308–10.
Lahiri TK, Agrawal D, Agrawal K, Shukla J. Pure red cell aplasia associated with thymoma. Indian J Chest Dis Allied Sci. 2002;44:259–62.
Funding
Because it is not a research paper we did not require funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Human and animal rights disclosure
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
In this article, neither the name of the patient or the identity of the patient is revealed. So consent from the patient was not taken.
Ethical approval
Not required
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xavier, R.D., Devaraj, S., Sadasivam, V. et al. Thymoma associated with pure red cell aplasia: a case report and literature review. Indian J Thorac Cardiovasc Surg 36, 404–408 (2020). https://doi.org/10.1007/s12055-019-00875-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-019-00875-2