Abstract
Persistent inflammation in intensive care unit (ICU) survivors is associated with higher long-term mortality and poorer mobility. However, it is unknown if inflammatory markers are associated with other dysfunctions observed in survivors of critical illness. Thus, it was investigated if plasma levels of interleukin (IL)-6 and IL-10 at hospital discharge were associated with long-term functional and cognitive performance after ICU discharge. Adult patients admitted for > 48 h to a 20-bed mixed ICU in a University Hospital had blood collected within 48 h before hospital discharge to measure IL-6 and IL-10 levels. After a median time of 48 months, cognitive status was determined by the Mini-Mental State Examination (MMSE), and functional status was determined by the Barthel Index. Patients at the higher 25th percentile of both IL-6 and IL-10 had a worse long-term cognitive performance, but not worse functional status, even when adjusted for confounders after long-term follow-up. In conclusion, elevated circulating IL-6 and IL-10 concentrations at hospital discharge were associated with long-term cognitive dysfunction in ICU survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that 13 to 20 million people annually require life support in intensive care units (ICUs) worldwide [1]. Survivors of critical illness suffer loss of muscle mass, nerve dysfunction, and resultant weakness and functional disability that represent important and lasting morbidities [2]. The inflammatory nature of most critical illness raises the possibility that persisting inflammation could directly interfere with neuromuscular regeneration and brain function [2, 3] as the inflammatory response might persist at hospital discharge, even though clinical signs have resolved and subjects seemed stable for discharge [4].
In animal models that mimic long-term dysfunction-associated with critical illness, we and others have demonstrated persistent brain inflammation and muscle dysfunction [5,6,7,8]. Persistent inflammation, defined as higher circulating levels of IL-6 and IL-10 at hospital discharge after community-acquired pneumonia (CAP), was associated with all-cause and cause-specific mortality over 1 year, despite resolution of clinical signs of acute infection [4]. Recently, Griffith and cols demonstrated that poorer mobility 3 months after ICU discharge was associated with different inflammatory markers [3]. This persisted even after adjusting for measures of pre-existing comorbidity and acute illness severity [3]. However, it is unknown if inflammatory markers are associated with other dysfunctions observed in survivors of critical illness after ICU discharge. Thus, our study aims to determine if plasma levels of IL-6 and IL-10 at hospital discharge were associated with long-term functional and cognitive performance after ICU discharge.
Material and Methods
Ethics Approval and Consent to Participate
The institutional review board at Hospital São José (number 61541616.7.0000.5364) approved the study, and a written informed consent was obtained from all participants or their proxies.
Patients
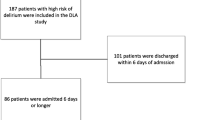
From January 2008 to December 2011, all consecutive adult patients admitted for > 48 h to a 20-bed mixed ICU in a University hospital were followed for different studies from our group and had blood collected within 48 h before hospital discharge. Since these were delirium-related studies, patients who could not be assessed for delirium at any time during the study period (patients with Richmond Agitation and Sedation Scale (RASS) scores − 4 or − 5 during the study period) and patients admitted because of brain trauma, delirium, or other neurological reason (e.g., stroke or subarachnoid hemorrhage) were excluded. From a median time of 48 months (percentile 25 26 months, percentile 75: 52 months, minimum 20 months, maximum 64 months), patients were evaluated to assess long-term dysfunctions (see below).
Procedures
Demographic variables and disease characteristics were collected for all admitted patients. Long-term dysfunctions were evaluated in the University outpatient clinic or in the patient home depending on patient convenience. Cognitive status was determined by the Mini-Mental State Examination (MMSE), and impaired performance was defined as a cutoff score of fewer than 24 points [9]. Functional status was determined by the Barthel Index (Basic Activities of Daily Life—BADL) [10]. Impaired functional status was defined as a cutoff score of fewer than 90 points. Comorbidities were evaluated by the Adult Comorbidity Evaluation-27 (ACE-27) and considered clinically relevant when the score was higher than 2.
Blood was obtained for cytokine assays within the last 48 h before hospital discharge and in the long-term follow-up. Blood was immediately centrifuged at 3000×g for 10 min, and the plasma collected and stored at − 80 °C until assayed. Plasma levels of IL-6 and IL-10 were determined by ELISA according to the manufacturer’s instructions (Quantikine, R&D Systems, Minneapolis, MN, USA).
Statistical Analysis
Standard descriptive statistics were used to characterize the study population. Continuous variables were presented as a median and interquartile interval. Differences in baseline characteristics and cytokine levels and long-term outcomes were tested using chi-square or Mann-Whitney test. IL-6 and IL-10 entered in most of the analyses (except in the multivariate linear regression) as the odds among patients at the highest 25th percentile of each cytokine levels versus all other quartiles combined. Multivariate linear and logistic regression analyses were performed to examine the independent association between variables and outcomes (MMSE and BADL entered the multivariate linear regression as a continuous variable and the logistic regression as a dichotomous variable). Variables yielding P values below 0.2 by univariate analysis entered in the linear and logistic regression models. For the logistic regression, since the number of events was low, it was additionally performed models that included variables yielding p values below 0.1 or 0.05. All these three models had a similar performance so it was decided to include in the final logistic regression only variables yielding p values below 0.05. Thus, it was created one model to the MMSE that included years of formal education, age, APACHE score and cytokine levels, and one model to the BADL that included years of formal education, age, APACHE score, ACE-27, and cytokine levels. Despite the fact that delirium and the time of cognitive and functional assessment did not reach the p value to be included in the regression analysis, they were forced in the regression since they are clinically relevant variables.
Results
Of the 663 subjects enrolled, 215 (32%) patients were dead at the time of recruitment. Of the remaining 487 subjects, 369 (76%) patients were not found after 3 phone call attempts, and 19 (4%) subjects denied participation. Thus 60 subjects were analyzed.
Table 1 describes baseline characteristics of included subjects. The median age of subjects was 60 years, 75% were male, and 20% had delirium during the ICU stay. Median hospital stay was 12 days. Thirteen subjects (22%) were admitted to the ICU after coronary bypass graft surgery, and two survivors had sepsis.
The median of IL-6 and IL-10 concentrations at hospital discharge for all subjects was 5.0 and 12 pg/ml, respectively (Table 1). The relation between IL-6 and IL-10 and long-term dysfunctions are presented in Table 2. Patients at the higher 25th percentile of both IL-6 (High IL-6) and IL-10 (High IL-10) had a worse performance in the MMSE. Actually, these were the only variables independently associated with MMSE. This was also true when delirium and the time of cognitive assessment were forced into the regression.
However, this was not true to the BADL. Despite the fact that IL-6 and IL-10 were associated with worse performance in the univariate analysis, after correcting to confounders only, APACHE II and ACE-27 scores were independently associated with impaired functional status (Table 2). Even if MMSE was forced in the regression, there was no independent association between IL-6, IL-10, and BADL. In addition, MMSE was not independently associated with impaired functional status, nor the presence of delirum and the time of functional assessment were forced into the regression.
Since the logistic regression could be overfitted due to the low numbers of events, it was also performed a linear regression (Fig. 1a–d) and multiple linear regression that would allow a more reliable result (Table 3). In the linear regression, cytokines significantly correlated only to MMSE, but not BADL scores (Fig. 1a–d). This was also true in the multiple linear regression. Higher values of IL-6 and IL-10 were significantly associated with lower scores on MMSE (Table 3), but not with BADL scores. Plasma levels of IL-6 and IL-10 collected during follow-up visit were not associated with long-term performance (data not shown).
Correlation between cytokines and the performance on Mini-Mental State Examination and basic activities of daily life. a Correlation between IL-6 plasma levels and MMSE performance. R2 = 0.32, p < 0.0001. b Correlation between IL-10 plasma levels and MMSE performance. R2 = 0.20, p = 0.0003. c Correlation between IL-6 plasma levels and BADL performance. R2 = 0.002, p = 0.25. d Correlation between IL-10 plasma levels and BADL performance. R2 = 0.001, p < 0.79
Discussion
We demonstrated that higher concentrations of plasma inflammatory markers at hospital discharge were associated with long-term cognitive dysfunction, but not impaired functional status, in ICU survivors.
A sustained decline in physical activity and muscle strength, long-term neurocognitive decline with an increased risk of developing dementia, and increased functional limitations are often observed in survivors of critical illness [11]. Plasma IL-6 and IL-10 concentrations were associated with subsequent mortality after CAP hospitalization [4]. This suggests that inflammatory response to infection persists even after infection resolution. In addition, 3 months after hospital discharge survivors from critical illness had a phenotype of persisting inflammation (elevated c-reactive protein, human neutrophil elastase, IL-6, IL-8, secretory leukocyte protease inhibitor and decreased transforming growth factor), and this phenotype was associated with poorer motor performance, even after adjustment for confounders [3]. Our results add to these published data that the degree of inflammation at hospital discharge is associated with long-term cognitive dysfunction. This was dissociated from a poorer functional status, suggesting that inflammation impacts on brain function, but not in other aspects that reflect on functional status. In this context, it was previously demonstrated that specific aspects of cognitive function (such as executive dysfunction), but not a global cognitive impairment or memory performance, were associated with poorer functional status [12]. Additionally, it is important to note that in our small sample size, the majority of patients had the maximum score in the BADL and this could at least in part explain these unexpected results.
Experimental studies suggest that persistent brain inflammation occurs after sepsis and major surgery [13, 14]. However, when blood was collected during critical illness, inflammatory markers were not correlated to long-term dysfunction [15], despite the fact that delirium is associated with accelerated cognitive decline [16]. Furthermore, plasma cytokines are possible indicators of neuroinflammation in Alzheimer’s disease (AD) and can be related to disease progression and conversion of mild cognitive impairment to AD [17]. Thus, our results have some biological plausibility, linking acute inflammation to sustained low-grade inflammation and the development of cognitive impairment.
There are some limitations to our study. We only studied cytokine levels taken at hospital discharge and at follow-up evaluation (median time 42 months). The evolution of systemic inflammation from hospital discharge and long-term evaluation was missed, and temporal patterns may yield additional information, like causality between inflammation and long-term dysfunction. Second, only IL-6 and IL-10 were measured, and this does not clearly represent the complexity of the inflammatory response. For example, in the Griffith and cols study, despite the fact that IL-6 was still increased 3 months after discharge, it was not correlated with motor dysfunction [3]. Third, this was a retrospective cohort study; thus, the majority of survivor patients could be contacted. This could be associated with selection bias, but when it was compared included and non-included patients, it was not found any clinically significant differences in the ICU-related variables, suggesting that these were similar populations. Fourth, ideally, these patients should be evaluated by a series of different tasks that measure different components of cognition, neuropsychiatric state, and quality of life to have a more complete picture of their limitations, but we preferred to make a more simple and quick evaluation that can miss some important aspects related to long-term impairment.
In conclusion, elevated circulating IL-6 and IL-10 concentrations at hospital discharge were associated with long-term cognitive in ICU survivors.
Abbreviations
- IL:
-
interleukin
- ICU:
-
intensive care unit
- CAP:
-
community-acquired pneumonia
- RASS:
-
Richmond Agitation and Sedation Scale
- MMSE:
-
Mini-Mental State Examination
- BADL:
-
basic activities of daily life
- ACE-27:
-
Adult Comorbidity Evaluation-27
- APACHE:
-
acute physiologic assessment and chronic health evaluation
- AD:
-
Alzheimer’s disease
References
Adhikari NK, Fowler RA, Bhagwanjee S et al (2010) Critical care and the global burden of critical illness in adults. Lancet 376:1339–1346
Herridge MS (2009) Legacy of intensive care unit-acquired weakness. Crit Care Med 37:S457–S461
Griffith DM, Lewis S, Rossi AG, Rennie J, Salisbury L, Merriweather JL, Templeton K, Walsh TS et al (2016) Systemic inflammation after critical illness: Relationship with physical recovery and exploration of potential mechanisms. Thorax 71:820–829
Yende S, D’Angelo G, Kellum JA et al (2008) Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med 177:1242–1247
Hill NE, Saeed S, Phadke R, Ellis MJ, Chambers D, Wilson DR, Castells J, Morel J et al (2015) Detailed characterization of a long-term rodent model of critical illness and recovery. Crit Care Med 43:e84–e96
Mina F, Comim CM, Dominguini D (2014) Il1-β involvement in cognitive impairment after sepsis. Mol Neurobiol 49:1069–1076
Schwalm MT, Pasquali M, Miguel SP, dos Santos JPA, Vuolo F, Comim CM, Petronilho F, Quevedo J et al (2014) Acute brain inflammation and oxidative damage are related to long-term cognitive deficits and markers of neurodegeneration in sepsis-survivor rats. Mol Neurobiol 49:380–385
Moraes CA, Santos G, de Sampaio E, Spohr TC et al (2015) Activated microglia-induced deficits in excitatory synapses through IL-1β: implications for cognitive impairment in sepsis. Mol Neurobiol 52:653–663
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Annane D, Sharshar T (2015) Cognitive decline after sepsis. Lancet Respir Med 3:61–69
Marshall GA, Rentz DM, Frey ME, Locascio JJ, Johnson KA, Sperling RA, Alzheimer's Disease Neuroimaging Initiative (2011) Executive function and instrimental activities of daily living in mild cognitive impairment and Alzheimer’s disease. Alzheimers Dement 7:300–308
Hennessy E, Gormley S, Lopez-Rodriguez AB, Murray C, Murray C, Cunningham C (2017) Systemic TNF-α produces acute cognitive dysfunction and exaggerated sickness behavior when superimposed upon progressive neurodegeneration. Brain Behav Immun 59:233–244
He HJ, Wang Y, Le Y et al (2012) Surgery upregulates high mobility group box-1 and disrupts the blood-brain barrier causing cognitive dysfunction in aged rats. CNS Neurosci Ther 18:994–1002
van den Boogaard M, Kox M, Quinn KL, van Achterberg T, van der Hoeven JG, Schoonhoven L, Pickkers P (2011) Biomarkers associated with delirium in critically ill patients and their relation with long-term subjective cognitive dysfunction; indications for different pathways governing delirium in inflamed and noninflamed patients. Crit Care 15:R297
Davis DH, Muniz-Terrera G, Keage HA et al (2017) Association of delirium with cognitive decline in late life: a neuropathologic study of 3 population-based cohort studies. Epidemiological clinicopathological studies in Europe (EClipSE) collaborative members. JAMA Psychiatry 74:244–251
Brosseron F, Krauthausen M, Kummer M, Heneka MT (2014) Body fluid cytokine levels in mild cognitive impairment and Alzheimer’s disease: a comparative overview. Mol Neurobiol 50:534–544
Funding
Supported by grants from the National Council for Scientific and Technological Development (CNPq), NENASC project (PRONEX program CNPq/FAPESC), PPSUS-FAPESC, and Universidade do Extremo Sul Catarinense.
Author information
Authors and Affiliations
Contributions
MM and SRB were involved in the conception and design, data acquisition, analysis and interpretation of the data, and drafting the manuscript. EBL, HD, RLD, and FV were involved in the conception and design and data acquisition. CDT, CR, and FD-P were involved in the conception and design, analysis and interpretation of the data, and drafting the manuscript.
Corresponding author
Ethics declarations
The institutional review board at Hospital São José (number 61541616.7.0000.5364) approved the study, and a written informed consent was obtained from all participants or their proxies.
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Maciel, M., Benedet, S.R., Lunardelli, E.B. et al. Predicting Long-term Cognitive Dysfunction in Survivors of Critical Illness with Plasma Inflammatory Markers: a Retrospective Cohort Study. Mol Neurobiol 56, 763–767 (2019). https://doi.org/10.1007/s12035-018-1166-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1166-x