Abstract
Astrogliosis and microgliosis in hippocampal sclerosis (HS) are widespread and are postulated to contribute to the pro-excitatory neuropathological environment. This study aimed to establish if seizure burden at the time of surgery or post-surgical outcome were correlated with the extent of gliosis in HS. As a secondary aim, we wanted to determine if the degree of gliosis could be predicted by pre-operative neuroimaging.
Children and adults who underwent epilepsy surgery for HS between 2002 and 2011 were recruited (n = 43), and age-matched autopsy controls obtained (n = 15). Temporal lobe specimens were examined by DAB immunohistochemistry for astrocytes (glial fibrillary acidic protein (GFAP)) and microglia (CD68). Cell counting for GFAP and CD68 was performed and quantitative densitometry undertaken for GFAP. Seizure variables and outcome (Engel) were determined through medical record and patient review. Seizure frequency in the 6 months prior to surgery was measured to reflect the acute seizure burden. Duration of seizures, age at onset and age at operation were regarded to reflect chronic seizure burden. Focal, lobar and generalized atrophy on pre-operative MRI were independently correlated with the degree of cortical gliosis in the surgical specimen.
In HS, both acute and chronic seizure burden were positively correlated with the degree of gliosis. An increase in reactive astrocyte number in CA3 was the strongest predictor of poor post-operative seizure outcome at 1 and 3 years post-operatively in this cohort. Changes in lower cortical astrocyte and upper cortical microglial number also correlated with post-operative outcome at 1 year. Post-surgical seizure outcome (1, 3 and 5 years) did not otherwise correlate with GFAP immunoreactivity (GFAP-IR) or CD68 immunoreactivity (CD68-IR). Increased microglial activation was detected in patients with pre-operative bilateral convulsive seizures, compared to those without convulsive seizures. Furthermore, focal, lobar and generalized atrophy on pre-operative neuroimaging were independently correlated with the degree of cortical gliosis in the surgical specimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hippocampal sclerosis is a common neuropathological finding in intractable epilepsy requiring surgery. Disappointingly, despite significant technological advances in imaging and technical procedures over the last decade, one third of patients continue to have seizures after surgery [1]. Certain factors have been linked to seizures continuing post-operatively, including widespread and incompletely resected pathology [2–5].
Neuronal loss and gliosis of the hippocampus and surrounding regions are pathological hallmarks of HS [6], but gliosis also occurs in extra-temporal cortical regions, independent of hippocampal projection pathways [7]. A new classification of hippocampal sclerosis was recently published defining patterns of neuronal loss and gliosis [8] and noted the co-occurrence with other pathologies, including focal cortical dysplasia and tumour. Atypical patterns of neuronal loss have been documented as having poorer outcomes post-surgery and were highlighted in this new classification [8].
Atrophy on MRI is frequently reported in neuroimaging studies of temporal lobe epilepsy (TLE) [7–11]. Although the pathological basis of the volume loss is unclear, some authors have suggested that it may be due to acquired pathologies, such as gliosis, which is also known to be widely distributed in TLE [7]. No previous studies have correlated MRI atrophy with pathological increases in gliosis.
On pathological examination of the cortex of patients with seizures associated with acute and chronic injury, there is an increase in both astrogliosis and microgliosis [12–15]. Acute and subacute responses to central nervous system (CNS) injury include both microglial proliferation and migration and reactive astrocytosis. In reactive astrocytes, morphological changes are evident with upregulation of glial fibrillary acidic protein (GFAP), astrocyte hypertrophy, proliferation and overlap of astrocyte domains [16, 17]. Similar morphological changes also occur in microglial activation, with thickening of processes and cell bodies [18]. These acute changes can resolve when the trigger is removed [19, 20]. There is growing evidence that reactive glia in seizure foci are both pro-excitatory and pro-inflammatory, and it has been suggested that such inflammation contributes to the perpetuation of disease development and severity [21].
In chronic CNS injury, glial scarring occurs, with a dense network of intermingled GFAP-labelled processes, persisting long after the triggering injury has resolved [8, 14, 20]. Within a glial scar, fibromeningeal cells and astrocytes predominate with tightly interdigitating processes forming a physical barrier [20, 22]. Particularly in cortical and spinal cord injuries, a glial scar has been demonstrated to form both a physical and chemical barrier, which while acting to isolate the damaged area, inhibits further axonal regeneration [17, 20, 22, 23]. The hypertrophy and hyperplasia of astrocytes seen in acute injury are less apparent in chronic scarring [24]. Dense fibrous astrogliosis has been described in HS since early pathological descriptions [6].
There have been few studies examining the relationship between seizures in HS and the extent of gliosis in surgically resected neuropathological specimens. However, microglial numbers have been positively correlated with the duration of epilepsy and the frequency of seizures in other types of lesions, for example, focal cortical dysplasia [25], but there has been a lack of consensus to date in HS. Blanc et al. [7] demonstrated increased cortical immunostaining for GFAP and CD68 in six post-mortem cases with HS, but there was no significant correlation with the duration of epilepsy or frequency of seizures in this small adult cohort. By contrast, another small study of 12 patients with HS showed a positive correlation between seizure frequency and increased numbers of reactive astrocytes, but no correlation was found between epilepsy duration and GFAP expression [26]. Animal studies have found similar results regarding seizure frequency and reactive astrocytosis [19]. The relationship between the degree of gliosis and post-surgical outcome has received little attention to date. The only post-operative study, conducted by Spencer et al. [27], examined glial density in 62 patients with mesial TLE and found no correlation with seizure freedom.
Given that gliosis is known to be common and widely distributed in HS and may be an active pro-excitatory component of the neuropathology, we aimed to establish if seizure burden at the time of surgery or post-surgical outcome were correlated with the extent of gliosis in a large group of adults and children with HS. As a secondary aim, we also wanted to determine if the degree of gliosis could be predicted by pre-operative neuroimaging.
Materials and Methods
Cohort
Participants were children and adults who underwent TLE surgery at Sydney Children’s Hospital (SCH) or Prince of Wales Hospital (POWH) between January 2002 and December 2011. Research ethics approval was granted by the Sydney Children’s Hospitals Network Human Research Ethics Committee. All patients were at least 1-year post-surgery at the time of recruitment. Pathological review of specimens from the group with TLE (n = 73)Footnote 1 was undertaken to confirm a smaller cohort who had HS.
Pathological Review and Quantitation of Gliosis
Review of Pathology
The original histopathological sections of the surgically resected lesion were reviewed by a neuropathologist and neurologist. In those patients confirmed to have HS, suitable blocks were selected from hippocampus (one block) and temporal cortex (one block) on the basis of orientation, location and satisfactory completeness and integrity of the section. If several operations had occurred and tissue was available from more than one procedure, the block with the most representative pathology was chosen. If tissue that was available from the hippocampus or temporal lobe was considered inadequate by the neuropathologist, the patient was not included in the study.
In the temporal cortex, mid-temporal blocks were chosen in preference to anterior or posterior temporal blocks. Sections were judged to be well-orientated if the cortical ribbon appeared to be of normal thickness, was not cut tangentially and included a straight section of the cortical ribbon, not at the crest of a gyrus or deep in a sulcus. Previous studies have noted the importance of achieving non-tangential cuts in accurately assessing cortical measures and suggested assessing cortical sections where the section was perpendicular to the cortical surface [7, 29]. Cortical thickness was measured for each of the orientated cortical ribbons, using a 2.5× objective. The median cortical width was 2.5 mm (interquartile range (IQR) = 0.85) for the majority of specimens, with only one outlier (4 mm), indicating non-tangential orientation.
In the hippocampus, blocks were selected on the basis of orientation and specimen completeness, displaying all subfields where possible. If the hippocampus was infiltrated by tumour, the specimen was not used for the study.
Pathological categories were based on recent definitions for HS, tumour and focal cortical dysplasia (FCD) IIIA [1, 8, 30–34]
Immunohistochemistry
Paraffin blocks of hippocampus and temporal lobe were sectioned at a thickness of 6 μm. The same microtome (Leica, 2035 Biocut. Reichert-Jung, Fabr Number 004119) was used for the study to maintain consistency of section thickness.
GFAP, CD68 and NeuN immunostaining was performed using a Leica Bond III automated immunostainer (Leica Autostainer XL, Leica Microsystems, Newcastle, UK) following the manufacturer’s protocol. Following de-paraffinization and rehydration and prior to peroxidase blocking, enzymatic antigen retrieval was performed for 10 min (GFAP and CD68) or heat retrieval was performed for 30 min (NeuN). Sections were then incubated with either a primary (rabbit) polyclonal antibody against GFAP (Reference Z0334, Lot 00087880, 1 in 4000, DAKO), a primary (mouse) monoclonal antibody against CD68 (Clone PG-M1, 1 in 500, DAKO) or a primary (mouse) monoclonal antibody against NeuN (clone A60, biotin conjugated, MAB377B lot LV1770323, 1 in 200, Millipore) for 30 min. Antibody binding was detected using the respective Bond Polymer Refine Detection Kit (Leica Microsystems), which uses HRP-conjugated (Horseradish peroxidase) secondary antibodies and DAB (3,3' diaminobenzidine tetrahydrochloride) as the chromagen. Mayer’s haematoxylin was used as the counterstain. NeuN immunostaining to detect neuronal cell bodies was only performed in the epilepsy group, as it could not be used in control specimens due to incompatibility with the fixation methods. Histochemistry and immunohistochemistry were otherwise performed on both cohort and control specimens.
Quantitation
Sections were examined using a motorized Axioplan2 microscope (Zeiss, Göttingen, Germany), and digital images acquired using an AxioCamHR digital camera using Axiovision software. Quantitation of glial number and immunoreactivity in the epilepsy cohort and controls were measured by density of immunoreactivity and cell counts. All counting was performed by the same operator to maximize consistency.
Immunostaining with antibodies directed against GFAP is the most accepted current methodology for examining both reactive astrocytes and the formation of glial scarring [35]. GFAP is a specific marker for astrocytes, as it labels intermediate filaments in the main processes and body of the cell, producing the typical star-shaped appearance [20, 24]. Acute injury increases production of GFAP so that previously immunonegative cells may become immunopositive, as well as causing physical hypertrophy of the cell body and its processes [20, 24]. Elevated expression of GFAP is now regarded as a sensitive and reliable marker of reactive astrocytes that are responding to CNS injuries. Limitations of the use of GFAP include a lack of expression by a proportion of normal astrocytes in the CNS and its expression exhibiting both regional and local variability by immunostaining [20].
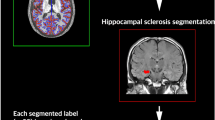
Density of GFAP immunoreactivity (GFAP-IR) was performed using a ‘densitometric mean’ (DSM, Axiovision software). Areas with dense immunoreactivity gave a lower DSM (minimum value measured = 3814.9) than areas with minimal immunoreactivity (maximum value measured = 10281.4). Cells were counted as being GFAP-immunoreactive astrocytes if the morphology was stellate in appearance, and there was at least a rim of IR around the nucleus or the nucleus appeared to be positive (see Fig. 1). If no nucleus was visible, the cell was not counted. Astrocytes adherent to blood vessel walls were not included in the overall counts. If the cell was on the edge of the region of interest, at least half of the cell nucleus had to be visible in order for it to be counted.
Morphology of GFAP-immunoreactive cells. Some of the various morphologies of GFAP-immunoreactive cells are illustrated and indicated by arrowheads: a a typical reactive astrocyte in CA4; b a reactive astrocyte in CA4 where no nucleus was visible in section, so not included in cell counts; c a reactive astrocyte in CA1 with a nucleus surrounded by dense fibrillary gliosis; d a reactive astrocyte in CA1 surrounded by gliosis where no nucleus was visible in section, so not included in cell counts. Scale bar shown in d equals 12.5 μm for a–d. Control cases illustrated in a and b. Epilepsy specimen demonstrated in c and d, showing HS ILAE class I with maximal neuronal loss and gliosis in CA1 and CA4
CD68 is the commonest marker used in studies immunolocalizing microglia in human epilepsy surgical specimens [7, 25, 36], though other markers for cells of microglial/macrophage lineage have also included HLA-DR (human leukocyte antigen complex) [25] and mGluR1α (metabotropic glutamate receptor) [37]. These markers are non-specific as they do not differentiate between intrinsically activated microglia or trafficking macrophage/monocytes [38, 39]. Perivascular and luminal immunoreactive cells would be the best representatives of this second group, with ongoing turnover from bone marrow-derived monocytes [40].
CD68 immunoreactivity (CD68-IR) was distributed sparsely and was considered to be more accurately measured through cell counts than overall staining density, in contrast to GFAP. Cells were counted as being CD68-immunoreactive microglia if their morphology showed immunoreactive projections from a nucleus, which often appeared to also have a rim of immunoreactivity (see Fig. 2). If no nucleus was visible, the cell was not counted. If the cell was on the edge of the region of interest, at least half of the cell nucleus had to be visible in order for it to be counted. Perivascular and luminal CD68-positive cells were not counted as microglia, as they have been shown to represent bone marrow-derived monocytes rather than intrinsic CNS microglia [40].
Morphology of CD68-immunoreactive cells. CD68 immunoreactivity is demonstrated in epilepsy cases, with HS ILAE class I, indicated by arrowheads: a in CA4, a clearly CD68-immunoreactive cell with thickened processes, which was counted as a reactive microglial cell. b In contrast, when clearly CD68 immunoreactive processes were seen in the parenchyma as here, presumably with their cell body excluded from the plane of section, they were not included in counts. c Immunoreactivity associated with blood vessel endothelium was not counted. Scale bar shown in c equals 12.5 μm in a–b, 25 μm in c
Multiple fields were examined in both the hippocampus and temporal neocortex, to allow for variability in immunoreactivity between anatomical structures. Three measures were taken from each anatomical location (non-overlapping fields) to allow for variation and a mean value calculated for each measurement. Regions of interest were photographed avoiding, where possible, artefacts from the staining or mounting process, large vessels or significant haemorrhage.
Hippocampal measures (high power field = 40× objective) were taken in all subfields (CA1, CA2, CA3, CA4 and dentate). In the temporal neocortex, measures were taken in the upper cortex, lower cortex and white matter. Upper cortical measures were orientated so the region of interest was parallel to the cortical surface, and the upper margin was placed mid-way through layer II. For GFAP (acquired using 10× objective), the upper cortical measure encompassed layer II (part), III and IV (part). The lower cortical measure for GFAP was contiguous to the initial measure, encompassing layer IV (part), V and VI. If white matter was included in the field, it was excluded from measures of DSM and cell counts. For CD68 (acquired using 20× objective), the upper cortical measure encompassed layer II (part) and layer III. The lower cortical measure for CD68 was taken adjacent to, but not including the white matter, and encompassed layers V and VI. White matter measures were taken in interdigitate matter, where available, or in deeper white matter not including any cortical tissue.
Clinical Review and Outcome
Clinical data were collated from the medical records. For those patients undergoing more than one surgical procedure, clinical details were determined prior to the first surgery where tissue was available. Data included age at first seizure, age at operation, duration of seizures prior to operation and seizure frequency (average number of seizures per month for 6 months prior to surgery). Pre-operative seizure frequency was classified as reflecting the acute seizure burden. Variables considered to be associated with the chronicity of the seizures included early age at the onset of seizures, long epilepsy duration and older age at operation. The types of seizure experienced by each patient were recorded. Seizure classification was based upon the most recent seizure and epilepsy classification from the International League Against Epilepsy (ILAE) [41]. Status epilepticus was defined in accordance with published definitions [42, 43]. Post-operative seizure outcome was recorded according to the Engel classification [44]. Outcome was calculated for 1, 3 and 5 years post-operatively, where possible.
MRI Review
Pre-operative MRIs (majority 1.5 T) were independently reviewed by a neuroradiologist and neurologist, blinded to the original report. These studies were analyzed for extra-hippocampal atrophy and the location of the atrophy. Atrophy was grouped into generalized atrophy, hemispheric atrophy (extra-temporal atrophy involving ipsilateral hemisphere), temporal atrophy (involving majority of temporal lobe) or focal atrophy involving the anterior temporal pole. Each of these types of atrophy was regarded as an independent variable, so that a patient’s MRI could be classified as having several different types of atrophy (e.g., both focal and generalized).
Disagreement between investigators was resolved through consensus. For five patients, no pre-operative MRI was available.
Control Specimens
Post-mortem controls (n = 15) were received from the Neuropathologisches Institut, Erlangen, Germany, as 6 μm paraffin-embedded, mounted sections, with no significant difference in age between this group and the epilepsy cohort (age at death for controls compared to age at operation for epilepsy cohort (p = 0.898)). For each control patient, the whole brain had been fixed for at least 2 weeks in 4 % formalin prior to being processed, embedded in paraffin and sectioned. Control specimens were from hippocampus and temporal neocortex (middle or inferior temporal gyrus, 2 cm posterior to anterior pole). This location was chosen to avoid parcellation at the anterior pole. Control specimens underwent the same histochemistry and immunohistochemistry as the epilepsy cohort, except for NeuN immunostaining which could not be performed in the control group due to incompatibility with the fixation method.
Statistical Analysis
Statistical relationships between specific clinical features and outcome (both continuous and categorical variables) and the degree of gliosis (continuous variable) were assessed. Non-parametric data were assessed using the Mann–Whitney U test or two-tailed bivariate correlations (Kendall’s tau-b or Spearman’s). Parametric data were assessed using independent samples t test or two-tailed bivariate correlations (Pearson’s). Mean or median were quoted as a measure of central tendency depending upon the distribution of values (parametric or non-parametric, respectively). Normality of data was assessed using the Kolmogorov–Smirnov statistic. Levene’s test was used to assess equality of variance. Logistic regression was used to assess the impact of multiple factors upon outcome.
Interrater agreement regarding MRI findings was assessed using observed concordance. Observed concordance for MRI atrophy in the available scans (n = 38) was 83.6 % with complete agreement after discussion.
Statistical analysis was performed using IBM SPSS Statistics for Mac (version 20.0). Random identification numbers were generated for the epilepsy cohort using an online tool (www.randomizer.org/form/htm). Each number remained unique, and the list was unsorted prior to application to the cohort.
Results
Cohort Details
Forty-three patients were included in the TLE surgery with HS cohort (see Table 1). Thirty patients had isolated HS, and 13 had HS with co-pathology (nine with FCD IIIA, four with tumour). Six patients required a repeat operation for ongoing seizures. Patients with bilateral convulsive seizures had a significantly longer duration of epilepsy (median = 18.1 years, IQR = 25.1 years) than those without convulsive seizures (median = 6.8 years, IQR = 19.7 years, p = 0.018). No significant relationship was found between post-operative outcome and any clinical variables in this cohort.
Differences in Gliosis Between Epilepsy Cohort and Controls
There was a significant difference in astrocyte counts and density and microglial counts between controls and the epilepsy cohort. Figure 1 shows examples of reactive gliosis determined by GFAP-IR for epilepsy cases and controls. Figure 2 illustrates the morphology of CD68-IR cells. CD68-IR cell counts were significantly higher in all hippocampal subregions (CA4, CA3, CA2, CA1 and dentate) and temporal lobe regions (upper cortex, lower cortex and white matter) in epilepsy cases compared to controls (see Fig. 3). Epilepsy cases were found to have significantly higher levels of GFAP-IR density and fibrillary gliosis (increased density in all hippocampal subregions and temporal lobe regions) but decreased reactive astrocyte number in CA4, CA3 and dentate compared to controls (see Fig. 4) (Fig. 5).
Differences in CD68 immunoreactivity between controls and epilepsy cohort. Controls (a, c) and epilepsy cases (b, d) imaged in CA4. An obvious increase in the number of CD68-IR cells is seen in epilepsy cases. Large neurons (black arrow) in controls are less frequent in epilepsy cases, as is typical for HS. Scale bar shown in d equals 50 μm in a–d
Relationship Between Gliosis and Pre-Operative Seizure Variables
Variables associated with chronic seizure burden (age at onset of epilepsy, duration of epilepsy prior to surgery, age at operation) were considered with regard to pathological factors consistent with fibrillary gliosis (increased GFAP-IR density and decreased astrocyte count). There was shown to be a strong correlation between duration of epilepsy prior to surgery and age at operation (Pearson coefficient 0.631, p < 0.0005), but other correlations were only weak or moderate. A significantly higher GFAP-IR density in CA1 (n = 30, r = 0.445, p = 0.001) and CA4 (n = 43, r = 0.350, p = 0.021) was associated with an earlier age of epilepsy onset. A longer duration of epilepsy was significantly associated with lower numbers of astrocytes in CA1 (n = 30, r = −0.32, p = 0.019) and in the dentate (n = 41, r = −0.345, p = 0.004). These variables were also significant on multivariate analysis (B = −0.04, 95 % CI −0.074 to −0.005, p = 0.025; B = −0.13, 95 % CI −0.024 to −0.003, p = 0.015, respectively). Patients who were older at operation had a significantly increased GFAP-IR density in the upper cortex (n = 43, r = −0.308, p = 0.045), lower cortex (n = 43, r = −0.378, p = 0.01) and white matter (n = 43, r = −0.311, p = 0.043), with only lower cortex (B = −23.246, 95 % CI = −40.26 to −6.233, p = 0.009) and white matter (B = −14.9, 95 % CI −29.4 to −0.392, p = 0.044) significant on multivariate analysis. Age was not correlated with neocortical GFAP-IR density in controls (upper cortex p = 0.108, lower cortex p = 0.439 and white matter p = 0.257). Other comparisons were not found to yield significant correlations.
A high seizure frequency was significantly associated with reactive astrogliosis defined by higher levels of GFAP-IR density in CA1 (n = 30, r = −0.331, p = 0.013) and higher astrocyte numbers in CA2 (n = 29, r = 0.443, p = 0.016). Other regions did not show a significant relationship between GFAP-IR and seizure frequency.
Microglial cell numbers determined by CD68-IR cell count was also used as a marker of acute/subacute injury. Patients with pre-operative bilateral convulsive seizures had significantly higher numbers of microglia in the upper cortex (n = 30, mean = 19.9, SD = 5.7) and in CA2 (n = 20, mean = 12.5, SD = 6.3) compared to those without convulsive seizures (upper cortex n = 13, mean = 15.4, SD = 6.2, p = 0.023; CA2 n = 11, mean = 7.8, SD = 3.7, p = 0.013). Patients with pre-operative status epilepticus had a significantly higher number of microglia in the dentate (n = 5, median = 5.7, IQR = 14.8) compared to those without status (n = 34, median = 4, IQR = 2.5, p = 0.049). Other locations did not show a significant correlation between CD68-IR and seizure type.
Relationship Between MRI Findings and Gliosis
Twenty patients (52.6 %) had atrophy on their MRI (locations shown in Table 1, see Fig. 5 for examples), with six patients displaying more than one sort of atrophy (15.8 %). In those patients where the MRI showed focal atrophy, there was a significantly higher number of microglial cells in the white matter of the temporal neocortex (n = 9, mean = 43.9, SD = 11.2) compared to those patients with no focal atrophy (n = 29, mean = 36.3, SD = 9.4, p = 0.047). Generalized atrophy on MRI was significantly associated with higher density of GFAP-IR in the upper cortex (p = 0.033) and lower cortex (p = 0.049) of the temporal lobe. Lobar atrophy on MRI was significantly associated with lower numbers of reactive astrocytes in the upper cortex of the temporal lobe (n = 6, median (Mdn) = 1.8, IQR = 5.8) compared to those patients without lobar atrophy (n = 32, Mdn = 9.5, IQR = 15.6, p = 0.046). Other comparisons between MRI atrophy and neocortical measures for GFAP-IR and CD68-IR were not found to yield significant correlations.
Relationship Between Gliosis and Post-Surgical Seizure Outcome
Patients with poor seizure outcome (Engel III or IV at 1 year post-operatively) had significantly higher numbers of astrocytes in CA3 and reduced numbers of lower cortical astrocytes and upper cortical microglia (see Table 2). On logistic regression, this model was a good predictor of outcome (p < 0.0005, χ 2 = 20.7, df = 3) but failed to meet significance for individual variables. High CA3 astrocyte count was the strongest predictor of poor seizure outcome on logistic regression. Furthermore, at 3 years, an increased number of astrocytes in CA3 was the only significant predictor of poorer outcome (Engel II–IV, p = 0.029). Fewer patients (n = 27 and n = 14) had post-operative outcome available at later time measures (3 and 5 years, respectively). Other comparisons between post-surgical seizure outcome (1, 3 and 5 years) and GFAP-IR or CD68-IR were not found to yield significant correlations.
Discussion
This study supports a relationship between the degree of hippocampal and cortical gliosis and clinical measures of seizure burden in a large group of children and adults with HS. Acute pre-operative seizure variables correlated with hippocampal reactive astrocytosis. Bilateral convulsive seizures and status epilepticus were correlated positively with microglial activation determined by CD68 immunostaining. Variables involved with chronicity of seizure activity (age at onset, seizure duration, age at operation) correlated with fibrillary gliosis. A relationship was also noted between MRI atrophy and the degree of cortical gliosis. Importantly, post-operative outcome was linked to both cortical and hippocampal gliosis, which is a novel finding.
Previously reported pathological markers of poor outcome in TLE have included atypical patterns of neuronal loss in HS [1, 30] and incomplete resection of pathology [3, 4]. This is the first report where an acquired pathological change was predictive of poor post-operative outcome, and this therefore has important implications regarding the management of seizures in the post-surgical period. Previous studies of gliosis in HS have not found a link between the degree of gliosis and outcome [27].
Previous studies in human HS, however, have demonstrated activation of pathological pathways consistent with glial activation [21]. Both animal and human studies in HS have demonstrated links between the degree of gliosis and the frequency of seizures [19, 26]. No relationship has previously been described between the degree of gliosis and the duration of epilepsy pre-operatively, as in other pathologies such as FCD [25].
In our study, absolute cell counts for GFAP and CD68 were used, with the acknowledgment that this methodology may have some limitations [26]. Whilst cell counts can be affected by tissue atrophy or surgical processing, many other variables could also potentially affect absolute cell counts, including tissue oedema, tangential cutting and the differences in autopsy specimen fixation compared with epilepsy cases. Due to the many variables that could potentially influence cell count in one or another direction, cell counts were not adjusted. Tangential cuts were minimized through careful selection of the cortical regions analyzed, and the cortical width was considered to be within normal limits for the majority of patients.
Post-operative outcome was correlated with hippocampal glial activation (CA3 astrocytes were increased in poor outcome) and cortical reactive gliosis (astrocytes were decreased in poor outcome). It can be hypothesized that increased reactivity in CA3 reflects increased reactivity in hippocampal projection pathways, as this subregion is an important part of the trisynaptic circuit, involved with outflow of activity from the hippocampus (through CA1 and entorrhinal cortex) [45, 46]. By contrast, cortical reactive gliosis was increased in patients with good seizure outcome, though this was a less significant factor on logistic regression. The correlation with good outcome may possibly be due to the complete resection of an active seizure focus. Alternately, the difference in cortical glial numbers could be due to differences in reactive cell migration, with increased glial migration into the active hippocampal circuit in patients with poor outcome. This finding has potential clinical application regarding surgical outcome prediction and could help guide management post-operatively.
Patients with a longer duration of seizures were more likely to have developed bilaterally convulsive seizures. Although the presence of pre-operative bilaterally convulsive seizures was not found to be significantly associated with post-operative outcome in this series, it has been found to be linked to poorer post-operative outcome in other TLE series [47, 48]. The link between long duration of seizures, pre-operative bilaterally convulsive seizures and poor post-operative outcome supports the idea of performing early surgery for TLE.
Previous studies of MRI findings in TLE have noted widespread atrophy affecting many cortical regions [9], with progressive extra-hippocampal atrophy over time [10, 11]. Blanc et al. [7] noted that the pathological basis for volume loss has not been firmly established, and postulated MRI changes were due to acquired pathology secondary to cortical injury. Blanc et al. [7] also established that cortical gliosis was widespread. No studies have directly correlated MRI atrophy with pathological increases in gliosis prior to this work. In our study, there was a significant relationship between pre-operative, extra-hippocampal MRI atrophy and the degree of cortical gliosis. Further confirmation of these relationships would require sampling of multiple regions with MRI localization and quantitation using voxel-based morphometry. Quantitated MRI measures were not available for many of our patients, and this is a limitation of this retrospective study.
Conclusion
In HS, both acute and chronic seizure burden were positively correlated with the degree of gliosis. An increase in reactive astrocyte number in CA3 was the strongest predictor of poor post-operative seizure outcome in this cohort. Increased microglial activation was detected in patients with pre-operative bilateral convulsive seizures, compared to those without convulsive seizures. Furthermore, atrophy on pre-operative neuroimaging was correlated with the degree of cortical gliosis.
Notes
The larger cohort with TLE is reported in Johnson et al. [28].
References
Thom M, Liagkouras I, Elliot KJ, Martinian L, Harkness W, McEvoy A, Caboclo LO, Sisodiya SM (2010) Reliability of patterns of hippocampal sclerosis as predictors of postsurgical outcome. Epilepsia 51:1801–1808
Hamiwka L, Jayakar P, Resnick T, Morrison G, Ragheb J, Dean P, Dunoyer C, Duchowny M (2005) Surgery for epilepsy due to cortical malformations: ten-year follow-up. Epilepsia 46:556–560
Krsek P, Maton B, Jayakar P, Dean P, Korman B, Rey G, Dunoyer C, Pacheco-Jacome E, Morrison G, Ragheb J, Vinters HV, Resnick T, Duchowny M (2009) Incomplete resection of focal cortical dysplasia is the main predictor of poor postsurgical outcome. Neurology 72:217–223
Lerner JT, Salamon N, Hauptman JS, Velasco TR, Hemb M, Wu JY, Sankar R, Donald Shields W, Engel J, Fried I, Cepeda C, Andre VM, Levine MS, Miyata H, Yong WH, Vinters HV, Mathern GW (2009) Assessment and surgical outcomes for mild type I and severe type II cortical dysplasia: a critical review and the UCLA experience. Epilepsia 50:1310–1335
Park C-K, Kim S-K, Wang K-C, Hwang Y-S, Kim KJ, Chae JH, Chi JG, Choe G-Y, Kim NR, Cho BK (2006) Surgical outcome and prognostic factors of pediatric epilepsy caused by cortical dysplasia. Childs Nerv Syst 22:586–592
Penfield W, Humphreys S (1940) Epileptogenic lesions of the brain: a histologic study. Arch Neurol Psychiatry 43:240–261
Blanc F, Martinian L, Liagkouras I, Catarino C, Sisodiya SM, Thom M (2011) Investigation of widespread neocortical pathology associated with hippocampal sclerosis in epilepsy: a postmortem study. Epilepsia 52:10–21
Blümcke I, Thom M, Aronica E, Armstrong DD, Bartolomei F, Bernasconi A, Bernasconi N, Bien CG, Cendes F, Coras R, Cross JH, Jacques TS, Kahane P, Mathern GW, Miyata H, Moshé SL, Oz B, Ozkara C, Perucca E, Sisodiya S, Wiebe S, Spreafico R (2013) International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: a Task Force report from the ILAE Commission on Diagnostic Methods. Epilepsia 54:1315–1329
Keller SS, Roberts N (2008) Voxel-based morphometry of temporal lobe epilepsy: an introduction and review of the literature. Epilepsia 49:741–757
Alhusaini S, Doherty CP, Scanlon C, Ronan L, Maguire S, Borgulya G, Brennan P, Delanty N, Fitzsimons M, Cavalleri GL (2012) A cross-sectional MRI study of brain regional atrophy and clinical characteristics of temporal lobe epilepsy with hippocampal sclerosis. Epilepsy Res 99:156–166
Bernhardt BC, Worsley KJ, Kim H, Evans AC, Bernasconi A, Bernasconi N (2009) Longitudinal and cross-sectional analysis of atrophy in pharmacoresistant temporal lobe epilepsy. Neurology 72:1747–1754
Belluardo N, Mudo G, Jiang XH, Condorelli DF (1996) Induction of astroglial gene expression by experimental seizures in the rat: spatio-temporal patterns of the early stages. Glia 16:174–186
Borges K, Gearing M, McDermott DL, Smith AB, Almonte AG, Wainer BH, Dingledine R (2003) Neuronal and glial pathological changes during epileptogenesis in the mouse pilocarpine model. Exp Neurol 182:21–34
Devinsky O, Vezzani A, Najjar S, De Lanerolle NC, Rogawski MA (2013) Glia and epilepsy: excitability and inflammation. Trends Neurosci 36:174–184
Ravizza T, Gagliardi B, Noé F, Boer K, Aronica E, Vezzani A (2008) Innate and adaptive immunity during epileptogenesis and spontaneous seizures: evidence from experimental models and human temporal lobe epilepsy. Neurobiol Dis 29:142–160
Sofroniew MV, Vinters HV (2010) Astrocytes: biology and pathology. Acta Neuropathol 119:7–35
Verkhratsky A, Sofroniew MV, Messing A, deLanerolle NC, Rempe D, Rodríguez JJ, Nedergaard M (2012) Neurological diseases as primary gliopathies: a reassessment of neurocentrism. ASN Neuro 4 doi: 10.1042/AN20120010
Belarbi K, Rosi S (2013) Modulation of adult-born neurons in the inflamed hippocampus. Front Cell Neurosci 7:145
Oberheim NA, Tian GF, Han X, Peng W, Takano T, Ransom B, Nedergaard M (2008) Loss of astrocytic domain organization in the epileptic brain. J Neurosci 28:3264–3276
Sun D, Jakobs TC (2012) Structural remodeling of astrocytes in the injured CNS. Neurosci Rev 18:567–588
Das A, Wallace GC 4th, Holmes C, McDowell ML, Smith JA, Marshall JD, Bonilha L, Edwards JC, Glazier SS, Ray SK, Banik NL (2012) Hippocampal tissue of patients with refractory temporal lobe epilepsy is associated with astrocyte activation, inflammation, and altered expression of channels and receptors. Neuroscience 220:237–246
Herrmann JE, Imura T, Song B, Qi J, Ao Y, Nguyen TK, Korsak RA, Takeda K, Akira S, Sofroniew MV (2008) STAT3 is a critical regulator of astrogliosis and scar formation after spinal cord injury. J Neurosci 28:7231–7243
Okada S, Nakamura M, Katoh H, Miyao T, Shimazaki T, Ishii K, Yamane J, Yoshimura A, Iwamoto Y, Toyama Y, Okano H (2006) Conditional ablation of Stat3 or Socs3 discloses a dual role for reactive astrocytes after spinal cord injury. Nat Med 12:829–834
Norton WT, Aquino DA, Hozumi I, Chiu FC, Brosnan CF (1992) Quantitative aspects of reactive gliosis: a review. Neurochem Res 17:877–885
Boer K, Spliet WGM, van Rijen PC, Redeker S, Troost D, Aronica E (2006) Evidence of activated microglia in focal cortical dysplasia. J Neuroimmunol 173:188–195
Cohen-Gadol AA, Pan JW, Kim JH, Spencer DD, Hetherington HH (2004) Mesial temporal lobe epilepsy: a proton magnetic resonance spectroscopy study and a histopathological analysis. J Neurosurg 101:613–620
Spencer SS, Kim J, deLanerolle N, Spencer DD (1999) Differential neuronal and glial relations with parameters of ictal discharge in mesial temporal lobe epilepsy. Epilepsia 40:708–712
Johnson AM, Sugo E, Barreto D, Cunningham AM, Hiew C-C, Lawson JA, Somerville ER, Connolly AM, Bye AME (2014) Clinicopathological associations in temporal lobe epilepsy patients utilising the current ILAE focal cortical dysplasia classification. Epilepsy Res 108:1345–51
Blümcke I, Mühlebner A (2011) Neuropathological work-up of focal cortical dysplasias using the new ILAE consensus classification system—practical guideline article invited by the Euro-CNS Research Committee. Clin Neuropathol 30:164–177
Blümcke I, Pauli E, Clusmann H, Schramm J, Becker A, Elger C, Merschhemke M, Meencke H-J, Lehmann T, von Deimling A, Scheiwe C, Zentner J, Volk B, Romstöck J, Stefan H, Hildebrandt M (2007) A new clinico-pathological classification system for mesial temporal sclerosis. Acta Neuropathol 113:235–244
Blümcke I, Kistner I, Clusmann H, Schramm J, Becker AJ, Elger CE, Bien CG, Merschhemke M, Meencke H-J, Lehmann T, Buchfelder M, Weigel D, Buslei R, Stefan H, Pauli E, Hildebrandt M (2009) Towards a clinico-pathological classification of granule cell dispersion in human mesial temporal lobe epilepsies. Acta Neuropathol 117:535–544
Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, Jacques TS, Avanzini G, Barkovich AJ, Battaglia G, Becker A, Cepeda C, Cendes F, Colombo N, Crino P, Cross JH, Delalande O, Dubeau F, Duncan J, Guerrini R, Kahane P, Mathern G, Najm I, Özkara Ç, Raybaud C, Represa A, Roper SN, Salamon N, Schulze‐Bonhage A, Tassi L, Vezzani A, Spreafico R (2011) The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia 52:158–174
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Thom M, Blümcke I, Aronica E (2012) Long-term epilepsy-associated tumors. Brain Pathol 22:350–379
Ostergaard PJ, Jensen MB (2013) Histological quantification of astrocytosis after cerebral infarction: a systematic review. Int J Neurosci 123:439–443
Garbelli R, Milesi G, Medici V, Villani F, Didato G, Deleo F, D’Incerti L, Morbin M, Mazzoleni G, Giovagnoli AR, Parente A, Zucca I, Mastropietro A, Spreafico R (2012) Blurring in patients with temporal lobe epilepsy: clinical, high-field imaging and ultrastructural study. Brain 135:2337–2349
Geurts JJG, Wolswijk G, Bö L, van der Valk P, Polman CH, Troost D, Aronica E (2003) Altered expression patterns of group I and II metabotropic glutamate receptors in multiple sclerosis. Brain 126:1755–1766
Flügel A, Bradl M (2001) New tools to trace populations of inflammatory cells in the CNS. Glia 36: 125–136
Graeber MB, Scheithauer BW, Kreutzberg GW (2002) Microglia in brain tumors. Glia 40:252–259
Williams K, Alvarez X, Lackner AA (2001) Central nervous system perivascular cells are immunoregulatory cells that connect the CNS with the peripheral immune system. Glia 36:156–164
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde BW, Engel J, French J, Glauser TA, Mathern GW, Moshé SL, Nordli D, Plouin P, Scheffer IE (2010) Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 51:676–685
(1993) Guidelines for epidemiologic studies on epilepsy. Commission on Epidemiology and Prognosis, International League Against Epilepsy. Epilepsia 34: 592–596
Shinnar S, Hesdorffer DC (2010) Pediatric status epilepticus: should the diagnostic evaluation change? Neurology 74:624–625
Engel J Jr (1992) Update on surgical treatment of the epilepsies. Clin Exp Neurol 29:32–48
Andersen P (2007) The hippocampus book. Oxford University Press, New York
Jones MW, McHugh TJ (2011) Updating hippocampal representations: CA2 joins the circuit. Trends Neurosci 34:526–535
McIntosh AM, Kalnins RM, Mitchell LA, Fabinyi GCA, Briellmann RS, Berkovic SF (2004) Temporal lobectomy: long-term seizure outcome, late recurrence and risks for seizure recurrence. Brain 127:2018–2030
Spencer SS, Berg AT, Vickrey BG, Sperling MR, Bazil CW, Shinnar S, Langfitt JT, Walczak TS, Pacia SV (2005) Predicting long-term seizure outcome after respective epilepsy surgery: the multicentre study. Neurology 65:912–918
Acknowledgments
We have received support from Leica Biosystems with immunostaining. We acknowledge the support of Westfield Research Laboratories and Professor Jenny Peat (statistician). We thank Professor Ingmar Blümcke and Dr. Roland Coras (Neuropathologishes Institut, Univeresitatskilinkum Erlangen) for kindly providing us with control tissue for the project.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnson, A.M., Sugo, E., Barreto, D. et al. The Severity of Gliosis in Hippocampal Sclerosis Correlates with Pre-Operative Seizure Burden and Outcome After Temporal Lobectomy. Mol Neurobiol 53, 5446–5456 (2016). https://doi.org/10.1007/s12035-015-9465-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9465-y