Abstract
Cancer therapies, especially anthracyclines and monoclonal antibodies, have been linked with increased rates of cardiotoxicity. The development of some cardiac side effects happens over several months, and changes in ejection fraction can be detected long before permanent damage or disability occurs. Advanced heart failure could be averted with better and earlier detection. Methodologies for early detection of cardiac changes include stress echocardiograms, cardiac velocity measurements, radionuclide imaging, cardiac MRI and several potential biomarkers. Many agents have been described for prophylaxis of cardiac events precipitated by cancer therapy. Prophylactic use of beta-blockers and ACE inhibitors may be considered for use with trastuzumab in breast cancer as tolerated. Recovery of cardiac function is possible early after the injury from a cancer therapy. Late complications for coronary artery disease, hypertension and arrhythmia are underappreciated. Treatments for severe cancer therapy-related cardiac complications follow the existing paradigms for congestive heart failure and coronary artery disease, although outcomes for cancer patients differ from outcomes for non-cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiotoxicity and cancer treatments
Cardiotoxicity caused by cancer therapies spans several classes of drugs and results in surprisingly high rates of adverse events. Cancer therapy-related cardiac dysfunction results in 2–3 % rates of symptoms in randomized trials and up to 26 % in observational studies [1]. At present, cardiotoxicity has been observed from the anthracyclines, monoclonal antibodies, tyrosine kinase inhibitors, proteasome inhibitors, anti-angiogenesis agents and most recently some of the checkpoint immunotherapy agents. The mechanisms of cardiac toxicity are fully elucidated only for a minority of these drug classes. Given the rapid growth in the fields of oncology and cardiooncology, there is a need for an update of recent advances in this field. This review summarizes the most recent updates and recommendations relevant to cardiac effects of cancer therapy.
Cardiac links to cancer therapy can be traced to the development of the anthracycline chemotherapy family in the late 1960s by Pharmitalia Research Laboratories in Italy. Since then, anthracyclines have been used for treatment of many types of cancer [2], and they were soon found to cause cardiac side effects. Likewise, since the FDA approvals of trastuzumab in 1998 and imatinib in 2003, the use and breadth of agents with putative cardiotoxicity has rapidly expanded [3]. There are currently three approved Her2-targeted antibody therapies and a dozen tyrosine kinase inhibitors which all may have relevant cardiac effects. Additionally, bevacizumab and other angiogenesis agents are approved in several cancer types and with important cardiac implications for clinicians to be aware of.
Historically, cardiac monitoring in cancer patients consisted only of clinical symptom assessment and examination findings. In the intervening decades since the 1960s, a series of criteria for measurement and categorization of cardiotoxicity have been developed. Simultaneously, a variety of imaging tests, blood tests and even catheter-based assessments have been developed to quantify the very earliest cardiac changes associated with cancer therapy [2].
Mechanisms and types of cardiac toxicities
At this point in time, it is best understood that anthracyclines cause cellular damage by free radical production, intercalation into DNA and altered intracellular signaling. Anthracycline-induced cardiotoxicity involves cardiomyocyte histological changes, mitochondrial apoptosis, fibrin deposition, alterations in the left ventricular ejection fraction and eventually systolic and/or diastolic heart failure. Rarely, there are cases of early arrhythmias and myocarditis/pericarditis syndromes for which the mechanism of insult is less clear. For drug classes beyond anthracyclines, the direct toxic effects on cardiomyocytes are generally less clear at this time. Several lines of research implicate fibroblasts, lymphocytes, oxidative stress, pro-apoptotic signaling, calcium transport, stromal interactions and mitochondrial apoptosis as some of the more likely explanations for cardiotoxicity [4].
Hypertension, arrhythmia and coronary artery disease are the other leading cardiovascular complications of cancer therapy. The VEGF acting drugs are well known to cause hypertension and microvascular changes. Arrhythmias are reported with anthracyclines, several of the small molecule inhibitors, taxanes, vinca alkaloids, platinums, arsenic, thalidomide, antimetabolites and IL-2. The most common arrhythmia is atrial fibrillation although ventricular tachycardia is also well reported. The rates of arrhythmia are generally under 10 % for these classes of drugs, with the exception of intraperitoneal cisplatin which has been reported to cause atrial fibrillation in 18–32 % of patients [5].
Coronary artery disease has been the subject of much debate as cancer survivorship has improved over the last few decades. The largest datasets come from pediatric cancer survivors who are well followed after their cancer diagnoses and who seem to have increased rates of coronary artery disease. Also, the breast and prostate cancer patients, who are treated with hormone deprivation therapies for many years, appear to have slightly higher rates of coronary artery disease than the general population [6–8]. Finally, patients treated with other cancer therapies may experience increased rates of late coronary artery disease due to other factors such as increased systemic inflammation either due to the underlying disease, the treatments, the stress of treatment, or perhaps even due to changes in the microbiome that accompany a cancer diagnosis and treatment. Other effects on valve disease, pericardial disease and sudden cardiac death have been reviewed elsewhere [9].
Definitions and dose dependence
In recent years, “clinically significant chemotherapy-induced cardiotoxicity” has been defined as a decrease in the left ventricular ejection fraction (LVEF) more than 10 % to a final value of less than 50 % [10, 11]. Declines in LVEF which do not result in a final LVEF below 50 % have generally not been classified as clinically significant, although as discussed below, early subclinical declines in LVEF may have greater predictive value than was originally appreciated when the definitions were first agreed upon.
In the late 1970s, the seminal study was published by Von Hoff et al. [12]. They followed 4018 patients receiving doxorubicin and observed a 2.2 % incidence of congestive heart failure (CHF). In that study, CHF was determined by clinical signs and symptoms. It was noted that the incidence rate of CHF increased as the cumulative dose of doxorubicin increased. The CHF incidence rate was 3 % for patients with a cumulative dose of 400 mg/m2, 7 % for those with a cumulative dose of 550 mg/m2 and 18 % for those with a cumulative dose of 700 mg/m2. For the subset of patients developing CHF symptoms, the mortality due to CHF was 71 %. They suggested that up to 80 % of the population that survived cancer had late cardiac symptoms.
The other seminal study on a dose relationship for anthracyclines was published in 1973 and showed that of 399 patients with advanced carcinomas treated with doxorubicin, there were 11 patients (2.8 %) who developed CHF [13]. Eight out of the 11 CHF patients died from cardiac decompensation. In that study, the population was divided into two groups: The first group was 366 patients that received a doxorubicin dose of less than 550 mg/m2 and the second group was 33 patients that received a dose of more than 550 mg/m2 of the same drug. Only one case developed signs of CHF out of the 366 patients in the first group (0.27 %), while ten out of 33 patients developed signs of CHF in the second group (30 %). Together, the Von Hoff study and this Lefrak study confirmed the existence of a dose relationship for anthracyclines in the development of cardiac dysfunction.
In clinical practice currently, most clinicians limit the cumulative dose of doxorubicin to 400–450 mg/m2, but considerable cardiac damage is now known to occur at cumulative dosages below this level. Indeed, cardiac toxic effects have been reported with doses starting at 250–350 mg/m2. Even more concerning is a study suggesting toxicity in doses less than 250 mg/m2 at least for childhood malignancy [3, 9].
Long-term outcomes
Long-term cardiac outcomes, at least for anthracyclines and trastuzumab, are recently well studied and reported. Most recently, a study of the cardiac complications in long-term cancer survivors was reported in 2016. It found that 60 % of anthracycline-treated children would develop evidence of echocardiographic dysfunction and that 10 % of these children would experience CHF symptoms within 20 years of initial chemotherapy. It also concluded that up to 12 % of adults treated with trastuzumab might develop cardiotoxicity. In the modern era, where cardiac monitoring is performed, the trastuzumab-induced cardiac changes were often captured early and were usually reversible. Likewise, an estimated 20 % of patients receiving the combination of an anthracycline with trastuzumab were reported to develop any cardiotoxicity within 5 years [9].
In another large study, there were 14,358 cancer survivors enrolled in a retrospective cohort study to analyze long-term effects on the heart. By comparison, survivors of cancer were significantly more likely than siblings to report CHF (HR 5.9, 95 % CI 3.4–9.6; p < 0.001), myocardial infarction (HR 5.0, 95 % CI 2.3–10.4; p < 0.001), pericardial disease (HR 6.3, 95 % CI 3.3–11.9; p < 0.001) or valve abnormalities (HR 4.8, 95 % CI 3.0–7.6; p < 0.001). Exposure to cumulative doses of 250 mg/m2 or more of an anthracycline increased the risk of CHF, pericardial disease and valve abnormalities by two to five times compared with survivors who had not been exposed to an anthracycline. The study also concluded that the subset of 1500 patients that were exposed to radiotherapy and anthracyclines showed a twofold to sixfold increased risk for developing cardiotoxic events compared with non-irradiated patients [9, 14].
Combination of anthracycline and trastuzumab
Slamon et al. [15] first observed evidence of cardiac dysfunction for the combination of trastuzumab and anthracycline in the pivotal 2001 trial. Since then, several prospective studies have further confirmed an increased toxicity signal for this combination of agents. Further confirmation was published in 2016 from a population-based retrospective cohort study of 18,540 women with breast cancer [1]. The women (median age 54 years; 79 % under 65 years) had stage I to III breast cancer between 2007 and 2012 in Ontario. The treatment regimens were categorized as follows: anthracycline-based chemotherapy without trastuzumab, trastuzumab with taxanes, sequential therapy (anthracycline followed by trastuzumab) and other chemotherapy. The study concluded that the incidence rate of emergency department visits and hospitalizations due to anthracycline-induced congestive heart failure was 3.08 % (95 % confidence interval 2.81–3.36 %), but was only 0.96 % (95 % CI 0.89–1.04 %) in a 92,000-woman age-matched sample from Ontario. An additional conclusion was that the regimens containing both anthracycline and trastuzumab were the highest risk regimens for cardiac outcome. The adjusted rate of major cardiac events was highest in dual-agent therapy (HR 3.96; 95 % CI 3.01–5.22). Even trastuzumab without anthracycline generated more cardiac hospital visits than the healthy comparator group (HR 1.76; 95 % CI of 1.19–2.60).
Finally, to further confirm the prospective studies, a meta-analysis of more than 29,000 women with breast cancer was published in 2016. It found that trastuzumab use increased survival, but was associated with small, but relevant rate of cardiotoxicity. Severe cardiotoxicity was found to occur in 3.00 % (95 % CI 2.41–3.64) of the overall population within 3 years of therapy and in 3.14 % (95 % CI 2.12–4.37) of the patients with metastatic early breast cancer. Like the prior studies, this meta-analysis observed an increased rate of severe cardiotoxicity when early-stage breast cancer patients were treated with both anthracyclines and trastuzumab (2.90 % for dual therapy vs. 0.92 % for trastuzumab only) [16].
A study of the FDA adverse event reporting system (FAERS) database from January 2004 through September 2012 regarding cardiotoxicity in targeted therapy for breast cancer was recently reported [17]. A total of 59,739 adverse event reports of cardiotoxicity were found during that eight-year period. After analysis of the potential causative agents, trastuzumab was found to have the highest number of cardiotoxic reports followed by bevacizumab and lapatinib. Trastuzumab was reported to be the suspected cardiotoxic agent in 937 cases of cardiomyopathy or cardiac failure. Like the above studies, the combination of anthracycline and trastuzumab had a high odds ratio for cardiac events (ROR 17.84; 95 % CI 13.77–23.11). On the other hand, the ROR for cardiotoxicity for lapatinib was low at 1.20 (95 % CI 1.01–1.41) even when used in combination therapies.
Cardiotoxicity from other agents
As mentioned above, cardiotoxicity has been observed to some degree with almost all the cancer therapies currently available. Cardiac side effects for the tyrosine kinase inhibitors and other small molecule inhibitors and immunotherapy agents have been reported elsewhere and are beyond the scope of this review [18, 19]. The vascular endothelial growth factor receptor (VEGFR) inhibitors represent a major class of cancer therapeutic with significant cardiac toxicity. These agents (both antibodies and kinase inhibitors) are known to cause hypertension, endothelial dysfunction and increased platelet aggregation. There have been several studies and two meta-analyses regarding cardiotoxicity from bevacizumab. The largest and most recent meta-analysis assessed the risk of congestive heart failure in cancer patients treated with bevacizumab. It compared outcomes by the dose of the bevacizumab and the cancer type. The analysis concluded that the use of bevacizumab significantly increased the risk of high-grade congestive heart failure in cancer patients (RR 1.98, 95 % CI 1.30–3.02, p = 0.002), but not for all-grade CHF (RR 1.14, 95 % CI 0.87–1.49, p = 0.33). The relative risk for patients receiving bevacizumab doses of 5 mg/kg/week and 2.5 mg/kg/week was 2.25 (95 % CI 1.43–3.56) and 1.00 (95 % CI 0.33–3.05), respectively. Regarding the incidence rate of CHF in relation to the cancer type, it was found that only breast cancer was statistically significantly related to the development of CHF (RR 2.43, 95 % CI 1.48–3.98). Finally, it was concluded that bevacizumab in combination with taxanes significantly increased the risk of high-grade CHF.
Risk factors for treatment-related cardiotoxicity
There are multiple factors that can increase the likelihood of cancer treatment-induced cardiotoxicity. These factors include cumulative dose, age (extremes of age), radiotherapy of the left side of the chest, previous exposure to cardiotoxins and co-administration of anthracyclines and trastuzumab. Traditional cardiac risk factors including hypertension, dyslipidemia, smoking and diabetes mellitus are thought to be predictors of chemotherapy-related cardiac toxicity [12, 20, 21]. It remains unclear whether ethnicity is a risk factor, although there was one study which suggested that African-Americans may be at increased risk of cardiac toxicity of cancer therapy [22].
In a lymphoma study with 208 patients, hypertension was the strongest predictive factor for clinically significant LVEF decline with R-CHOP chemotherapy (19.7 vs 6.6 %, p = 0.004) [23]. Other studies have failed to confirm that any of those risk factors associated with anthracycline cardiotoxicity are predictive of trastuzumab cardiotoxicity [24]. Intriguingly, there was one small Italian study (N = 45), suggesting that in young Her2-positive breast cancer patients that lower body mass index might have a negative impact [25]. This finding has not been substantiated in a larger study yet.
Cardiac monitoring
There are many methods to detect subtle cardiac side effects in cancer patients undergoing therapy. Assessments include noninvasive imaging to estimate change in LVEF, invasive cardiac catheterization and invasive cardiac biopsy methods to determine histological changes in myocardium [26, 27].
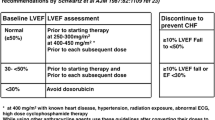
The prevailing noninvasive tool to measure cardiac function is echocardiography, though MRI and radionuclide imaging are also heavily used. Schwartz et al. [28] proposed guidelines for echocardiographic monitoring of cardiac function in anthracycline-treated patients. Schwartz et al. also recommended obtaining a baseline ejection fraction by equilibrium radionuclide imaging, with subsequent imaging studies before consideration of any additional doses. They also provided specific criteria for drug discontinuation based on interval change in LV function. Cardiotoxicity was defined as a decline of the LVEF more than 10 % and to a level below 50 %. For patients with a baseline LVEF of less than 50 %, significant change was defined as decline more than 10 % or to a level <30 %.
The study recommended interval calculations of the LVEF before administration of 100 mg/m2 of doxorubicin. They recommend another assessment after the use of 250–300 mg/m2 and a third assessment after the use of 400 mg/m2 in patients with known cardiac risk factors. For the patients who did not have a history of any cardiac risk factors, then an echocardiogram needs to be performed only if the cumulative dose exceeds 450 mg/m2. The conservative suggestion from Schwartz et al. [28] was that anthracycline or trastuzumab should be discontinued if the decline in the LVEF is more than 10 % and the LVEF value decreases to a level below 50 %. The proposed guidelines suggest that patients with baseline LVEF <50 % should carefully weigh risk versus benefit before starting a potentially cardiotoxic agent. If the LVEF is <30 %, then cardiotoxic agents should not be considered at all. For patients with LVEF between 30 and 50 %, repeat cardiac assessment should be obtained prior to each cycle and therapy withheld for a decline approaching 10 % [28, 29]. The same guidelines were also validated in the Delphi study which concluded that “When LVEF decreases, there has already been considerable myocardial damage” [30, 31].
A prospective registry study of the role of echocardiography and multigated acquisition scan (MUGA) tested the actual clinical impact of routine baseline cardiac testing before cancer therapy. The study assessed 600 eligible patients to detect baseline cardiac abnormalities using echocardiograms and MUGA before the administration of anthracyclines and/or trastuzumab. Thirteen patients out of 600 (2.2 %, 1.2–3.7 %) proved to have abnormal imaging. Only nine of them had LVEF <55 %. On the follow-up of the study (mean 4.0 years; range 0–8.3), only 15 patients developed cardiac events and none of these 15 patients had any abnormality on baseline screening using echo/MUGA. The study concluded that baseline echo/MUGA did not alter the treatment plan [28, 31].
Echocardiography and MUGA are perhaps the most frequently used tools for cardiac monitoring. There are advantages and limitations to the use of two-dimensional (2D) echocardiography. The limitations are inter-observer and intra-observer variability and the concern that 2D echo is likely to detect late changes in LVEF that are less likely to be reversible [32]. A benefit of echocardiography beyond estimation of the LVEF is the ability to evaluate valve lesions and pericardial pathology. For example, new-onset mitral regurgitation and asymmetry of the papillary muscle leading to dyssynchrony has been described during treatment with trastuzumab [33, 34]. Also the echocardiographic finding of endocardial calcification has been described in a case of restrictive cardiomyopathy [35]. A potential downside of 2D echocardiography is the tendency to underestimate the decline in the ejection fraction. MUGA imaging remains a generally safe and easily reproducible alternative to echocardiography, with the only significant downsides being the radiation exposure and longer time required for dosing [27, 32, 33].
Emerging cardiac monitoring methodologies
Some newer and more accurate methods include tissue Doppler imaging (TDI) and myocardial strain imaging [29]. A TDI study of the left ventricle, inter-ventricular septum and the right ventricle was performed in long-term survivors of childhood leukemia. The study enrolled 60 patients with acute lymphoblastic leukemia that were in remission for a period of at least two years (median age of 11.7 years) and also included 30 healthy controls. The patients were followed for a median period of four years. All patients were treated with a low cumulative dose of doxorubicin (100 mg/m2) according to the St. Jude Total-XIIIA protocol. The LVEF and the myocardial shortening were found to be normal in patient and control groups although slightly lower in the patient group (69.5 ± 2.3 vs. 72.7 ± 3 %, p < 0.01). On the other hand, the myocardial systolic, early diastolic and late diastolic velocities were found to be decreased in the patient group (p < 0.01 for all of myocardium segments). The study concluded that lower velocities were associated with decreased systolic contraction, delayed relaxation and restriction of the myocardium. It was further concluded that TDI detected cardiac changes “earlier than conventional echocardiography” and better delineated diastolic dysfunction. Finally, it was suggested that detection prior to the onset of symptoms was critical for prevention of longer-term adverse effects [36].
Another tissue Doppler study of 32 pediatric malignancy survivors and 22 healthy children assessed fractional shortening, stroke volume, cardiac index, and peak velocity of early rapid filling by echo. The peak velocity of early filling on TDI was lower in cancer patients than in healthy patients (p < 0.05), and the ratio of early peak velocity of rapid filling on pulse Doppler to tissue Doppler (E/E′) values was statistically higher in the patient group than in the control group (p < 0.05) [36, 37].
Global myocardial strain and the strain rate are proposed improvements for cardiac assessment. A study of these methods enrolled 111 cancer survivors and 107 healthy controls. The global strain parameters of survivors were compared with the same parameters in controls. Strain parameters were related to conventional echocardiographic parameters, N-terminal pro-natriuretic peptide (NT-pro-BNP) levels and clinical parameters. The study concluded that global myocardial strain, strain rate and time to peak systolic strain in asymptomatic survivors of childhood cancer were significantly lower compared with healthy controls (p < 0.0001) and were related to systolic and diastolic left ventricular parameters [38].
An unrelated myocardial strain study in adults with Her2-positive breast cancer followed 42 patients from 2007 to 2009 [36]. Troponin T, CRP and BNP were assessed and did not show any change in the follow-up period. However, over the 3 months of adjuvant therapy, a significant difference in the systolic annular velocity of the lateral left ventricular wall was observed between the normal cohort and the 25 % of patients who went on to develop clinically relevant LVEF declines (9.1 ± 1.6 and 6.4 ± 0.6 cm/s, respectively, p < 0.05). Additionally, the peak global longitudinal and radial strain decreased up to 3 months prior to the eventual finding of LVEF decline by conventional echo. It was concluded from the study that tissue velocity index and strain imaging were able to detect preclinical changes in the left ventricular systolic function even before changes in the LVEF were detected by conventional echocardiography [36, 39].
Cardiac magnetic resonance imaging (cMRI) is another evolving imaging modality. cMRI is able to assess both the functional and structural components of the myocardium. In a prospective study of 81 childhood cancer patients [40], the primary finding was a significant increase in left atrial volume by cMRI. A mild increase in myocardial scaring was also observed. The authors concluded that cMRI and left atrial volume might be early markers of diastolic dysfunction and markers of myocardial fibrosis [40, 41].
An innovation in imaging technology that failed to improve surveillance was stress echocardiography. Stress echo was studied in 80 childhood cancer survivors. They were classified into high risk (12), moderate risk (23), low risk (24) or no risk (21) as defined by the Children’s Oncology Group Long-Term Follow-Up Guidelines version 3.0 and assessed by stress echo [42]. Peak aerobic capacity in all groups was similar. Compared with controls at rest, the high-risk group had evidence of diastolic dysfunction with lower E/A ratios (1.4 vs. 2.0, p = 0.008) and nonsignificant difference in septal early diastolic velocities (E/E′) of 11.7 versus 9.9 (p = 0.165). With exercise, this difference resolved and myocardial contractile reserve was preserved. These findings suggest that routine stress echocardiography may not be a useful surveillance tool [42].
Biomarkers of cardiotoxicity
Biomarker screening for early detection of cardiotoxicity has been a major interest due to their promising roles in the early detection of cardiac events during chemotherapy treatment. Troponin increases due to cardiomyocyte damage and B-type natriuretic peptide (BNP) increases due to elevation of filling pressure are often observed in anthracycline-treated patients [43]. Troponin I (TnI) and BNP were used as screening measures along with imaging echocardiography in a recent prospective study [44]. The biomarkers were measured before and 24 h after each cycle, and cardiac imaging was performed at baseline and after completion of the chemotherapy course. Out of 109 patients, 11 (10.1 %) suffered cardiac events. All of these 11 patients had at least one BNP test value of more than 11 pg/ml prior to the occurrence of the cardiac event. Only three of the patients that developed cardiac events had LVEF decline. The authors made a suggestion for the serial use of cardiac biomarkers for earlier detection of cardiac events [43, 44].
Similarly, a multicenter cohort study of 78 breast cancer patients undergoing doxorubicin and trastuzumab therapy examined a series of eight biomarkers. The eight biomarkers were measured at baseline and every 3 months. The biomarkers included high-sensitivity cardiac troponin I (hs-cTnI), high-sensitivity C-reactive protein (hs-CRP), N-terminal pro-B-type natriuretic peptide (NT-pro-BNP), growth differentiation factor 15 (GDF-15), myeloperoxidase (MPO), placental growth factor (PlGF), soluble fms-like tyrosine kinase receptor-1 (sFlt-1) and galectin 3 (gal-3). The study observed that six out of the eight biomarkers increased as early as 3 months, while NT-pro-BNP and gal-3 did not. The observed increases persisted at 15 months. The study found that MPO, GDF-15 and gal-3 increased prior to a decline in LVEF [45]. Further biomarker development was the ultimate conclusion of this study.
A smaller study of 19 patients with Her2-positive breast cancer was assessed by serial high-sensitivity troponin T (hs-TnT) levels [46]. The study population was divided into two groups: the first group that represented nine patients that had decline in the LVEF >5 % and the second group representing the rest of the study population that had LVEF decline <5 %. The hs-TnT level at six months was significantly higher in the first group than in the second group (11.0 ± 7.8 vs. 4.0 ± 1.4 pg/mL, p < 0.01). The hs-TnT level at 6 months had 78 % sensitivity and 80 % specificity for predicting a reduction in LVEF at 15 months [45, 46].
Finally, a prospective study of NT-proBNP was performed in 100 patients with breast cancer who were treated with anthracyclines, taxanes and trastuzumab. The analysis revealed significant increases in the levels of the NT-pro-BNP (p = 0.0001) at 3 and 6 months which preceded the detection of LVEF decline by echocardiography. As with the studies above, further validation is needed before these biomarkers are ready for routine clinical use [43, 47].
Cardioprotection during cancer therapy
At the same time that many studies were working on the early detection of anthracycline- and trastuzumab-induced cardiotoxicity, other studies focus on mitigation of toxic effects either by altering the drug properties of the chemotherapeutic agent or by prophylaxis against the cardiac toxic effects of these medications (Table 1). We will review dexrazoxane, vitamin E, liposomal formulations, statins, beta-blockers and angiotensin-blocking agents. Exercise interventions and other dietary interventions have been studied, but are beyond the scope of this review.
Liposomal doxorubicin formulations of anthracyclines were developed for multiple reasons, one of which was to improve the toxicity profiles. Two formulations have been approved in Europe and Canada and one in the USA (Myocet and Doxil). It is fairly clear that liposomal formulations have gentler toxicity profiles compared with conventional doxorubicin [48]. Indeed, a head-to-head comparison of 509 metastatic breast cancer patients with normal cardiac functions randomized them to receive either pegylated liposomal doxorubicin or conventional doxorubicin. The LVEF was assessed at multiple occasions to determine the effect of each medication on the cardiac function. The study concluded that the progression-free survival rate was 6.9 versus 7.8 months (HR 3.6, 95 % CI 1.58–6.31, p < 0.001). Likewise, it concluded that the cardiotoxicity risk was higher with doxorubicin than with PLD (HR 3.16; 95 % CI 1.58–6.31; p < 0.001). There were less alopecia, nausea, vomiting and neutropenia with liposomal doxorubicin. Palmar-plantar erythrodysesthesia, stomatitis and mucositis were more common with liposomal doxorubicin than with doxorubicin. The study concluded that PLD has less toxicity, but similar efficacy compared with doxorubicin [48, 49].
The cardioprotective effect of vitamin E has been the topic of multiple studies due to its antioxidant effect. A study in female BalbC/NIH mice treated with vitamin E at 24 h before bolus doses of doxorubicin or doxorubicin and cyclophosphamide (intraperitoneal) assessed cardiac biopsy and blood markers at 1.5 and 3 months after treatment [50]. It was concluded from the study that vitamin E failed to prevent the occurrence of anthracycline-induced cardiotoxicity, though it might have mitigated late progression of cardiac damage at least in the doxorubicin only group. A human pilot study of 13 chemotherapy patients failed to detect a difference between patients treated with vitamin E and patients treated without vitamin E [50–52].
The protective effect of dexrazoxane has been fairly well studied in humans. Several studies confirmed its role in decreasing the cardiac risks in patients treated with anthracycline chemotherapy. Two multicenter studies were performed, in which patients were randomized to receive either FAC (fluorouracil, doxorubicin and cyclophosphamide) with placebo or FAC plus dexrazoxane. The overall incidence of congestive heart failure in the placebo group was 22 % but in the dexrazoxane group was 3 %. This suggested a cardioprotective role of dexrazoxane in patients receiving cumulative doses of anthracycline over 300 mg/m2 [53]. Currently, dexrazoxane is not used in clinical practice in the USA, and there are concerns for differences in effects across differing cohorts of patients, differing cancer types and divergent treatment regimens. A concern for second malignancies has been raised but is not yet confirmed outside of a single trial.
B-blockers, angiotensin antagonists and statins
Chief among the cardioprotective agents are the B-blockers and angiotensin agents (ACEIs and ARBs). Several agents in these categories were studied with chemotherapy in older studies and hints of benefit were seen, but definitive practice-changing conclusions were not rendered [54, 55]. More recently, the PRADA and MANTICORE studies were presented and have impacted on practice patterns in the field of breast cancer therapy (though not universally). Both recent studies were prospective assessments on prevention of cardiotoxicity from anthracyclines and trastuzumab specifically in early-stage breast cancer [54]. The PRADA study, a double-blinded randomized clinical trial, assigned 130 women with early-stage breast cancer to candesartan cilexetil, metoprolol succinate or matching placebos in parallel with adjuvant anticancer therapy. Cardiac magnetic resonance imaging was used to assess the LVEF. The overall decline in the LVEF was 2.6 % (95 % CI 1.5, 3.8) in the placebo group but 0.8 % (95 % CI −0.4, 1.9) in the group treated with the ARB and B-blocker along with chemotherapy. The study concluded that in patients with early-stage breast cancer treated with anthracyclines chemotherapy, that metoprolol did not effect the overall decline of the LVEF but candesartan provided protection against early decline of LVEF [54, 56–58]. MANTICORE on the other hand appears to show a benefit for both perindopril and bisoprolol in preventing deceases in LVEF during trastuzumab treatment.
To keep these exciting findings of PRADA and MANTICORE in perspective, it should be pointed out that the six preceding cardioprotection studies showed wide variation in the impact of beta-blockers, ACEI and ARB agents on the eventual development of LVEF in cancer patients [59, 60]. Two attempts at meta-analysis described below attempt to solve this question, but they suffer from patient and treatment heterogeneity. Additionally, the side effects of the cardiac drugs are significant and especially difficult to deal with during the time of chemotherapy. Side effects led to sub-optimal compliance in nearly every trial to date. Editorials from several experts in the field urge caution before adoption of the prophylactic use of ACEI and beta-blockers for all anthracycline- and trastuzumab-treated patients.
Statin therapy represents another area of cardiovascular medicine that has been studied both prospectively and retrospectively. Statins have different side effect profiles from ACEI/B-blockers and have been shown to have a protective effect against chemotherapy-induced cardiotoxicity [61]. The most relevant prospective study was a double-blinded randomized clinical trial which enrolled 40 patients and divided them into two groups. Patients with heart failure, left ventricular dysfunction or history of coronary artery disease were excluded. The first group received atorvastatin 40 mg/day before chemotherapy for 6 months regardless of their lipid profile. Echocardiography then was performed before and six months after chemotherapy. The statin-treated group did not show any elevation of the high-sensitivity CRP after chemotherapy, but it was elevated in the control group (3.84 ± 0.89 vs. 5.43 ± 1.78 mg/dl, p < 0.0001). Regarding the LVEF assessments, there was no decline in the LVEF in the statin group (61.3 ± 7.9 vs. 62.6 ± 9.3 %, p = 0.144), but there was a statistically significant decline in the LVEF in the control group (62.9 ± 7.0 vs. 55.0 ± 9.5 %, p < 0.0001). Only one patient in the statin group was observed with LVEF <50 %, but there were five patients in the control group with LVEF decline below 50 %. The study concluded that in the statin group, there was no decline in the LVEF or change in the end-systolic (30.3 ± 5.4 vs. 32.3 ± 5.4 mm, p < 0.0001) nor in the end-diastolic (47.2 ± 5.2 and 49.2 ± 6.2 mm, p < 0.013) parameters [61]. A separate retrospective study of statin use prior to and during anthracycline therapy showed a hazard ratio of 0.3 for heart failure hospitalization in patients taking uninterrupted statin therapy versus those without statin use [62, 63].
A meta-analysis of 14 published articles of cardioprotective drugs representing 12 clinical trials and two observational studies provided cross-study data for both pediatric and adult patients. The agents included dexrazoxane, statins, B-blockers and angiotensin antagonists. The analysis showed that in the control group there have been 304 cardiac events, but the cardiac events rate was only 83 in the patient group treated with any of the prophylactic agents. All agents showed favorable relative risk improvements across the meta-analysis. The magnitudes of protection were: dexrazoxane (RR 0.35 [95 % CI 0.27–0.45], p < 0.00001), beta-blockade (RR 0.31 [95 % CI 0.16–0.63], p = 0.001), statin (RR 0.31 [95 % CI 0.13–0.77], p = 0.01) and angiotensin antagonists (RR 0.11 [95 % CI 0.04–0.29], p < 0.0001) [64]. We conclude that there are roles for cardioprotective agents prophylactically in oncology, although there is equipoise regarding which agents are superior for which patient populations. Most of our trastuzumab-treated patients are offered prophylactic beta-blockers, and most have tolerated this therapy well.
Management of cancer related heart failure
As mentioned above, congestive heart failure remains the most common and most discussed cardiac complication of cancer therapy, although there are other known complications. There is currently nothing particularly unique to the management of symptomatic heart failure when the causative agent is a cancer drug. Routine clinical heart failure management strategies remain the accepted standard. Cornerstones of standard therapy include ACE inhibitors, B-blockers, diuretics, implantable defibrillators and even cardiac transplantation and mechanical circulatory support [65, 66].
The early-stage clinical outcomes for heart failure therapy when caused by cancer agents are slightly better than the outcomes for heart failure from ischemia, but once patients progress to stage C or D heart failure, the cancer patients appear to do a little worse than ischemic or idiopathic heart failure patients (HR 2.64 for death or transplant) [67].
In terms of early-stage heart failure, recovery or long-term stability is possible. For example, in 201 anthracycline-treated patients with LVEF decline below 45 %, the prompt treatment with ACEIs and B-blockers seemed to support recovery. Those patients were followed every 3 months for 2 years and then every 6 months for 36 months. The study showed that 85 patients (42 % of the patients) had complete recovery of the LVEF to baseline; 26 patients (13 % of the patients) had partial LVEF recovery; and 90 patients (45 %) had no recovery of LVEF. The rate of recovery or response increased as the time between the end of chemotherapy and the start of heart failure therapy decreased. The study also observed a lack of late recoveries beyond 6 months from LVEF decline. It was also noted that recovery patients showed a lower rate of cumulative cardiac events than partial and non-recovery patients (5, 31, and 29 %, respectively; p < 0.001).
Multiple studies corroborate that the best cardiac outcomes occur when LVEF decline is detected early and heart failure therapy is initiated promptly [54, 56, 65, 66]. For monoclonal antibody therapy, the recovery may even be superior to other agents. For example, in 38 patients with Her2-positive breast cancer with trastuzumab-induced cardiotoxicity, the mean LVEF was 61 ± 13 %, and the LVEF decreased to 43 ± 16 % after trastuzumab (p < 0.0001). After withdrawal of trastuzumab, the LVEF increased to 56 ± 11 %. Mean time to recovery of LVEF was 1.5 months and was temporally associated with medical treatment in 32 (84 %) of the 38 patients but occurred without treatment in six patients (16 %). Hence, the recovery of the LVEF occurred in 37 of the 38 patients. A total of 25 of the 37 patients were retreated with trastuzumab. Three out of these 25 patients developed recurrence of the cardiac dysfunction, but the other 22 patients did not. It was worth mentioning that the 25 patients that were re-challenged with trastuzumab received concurrent standard heart failure medical therapy. Nine of the study population underwent myocardial biopsy, and the histopathological analysis did not show any ultrastructural changes [68]. Another study similarly assessed 95 patients and found 19 patients (20 %) with evidence of cardiotoxicity after anthracycline and trastuzumab. Partial or complete recovery was seen in 13 patients (68 %) [39].
Conclusion
Cancer treatments have been linked with increased rates of cardiac side effects, the most common of which is decline of the LVEF. The risk of decline appears to be highest for the concurrent or sequential use of trastuzumab and anthracyclines. There is clinically significant and relevant cardiac risk even for regimens trastuzumab without anthracyclines. Other cancer agents are known to cause cardiotoxicity, especially the VEGFR inhibitors. Several cardioprotective measures can be used to decrease the toxic effects of chemotherapy on the heart. Among these measures, B-blockers, ACEIs, ARBs, dexrazoxane and the use of vitamin E are all studied, but so far, the only agents recommended for routine prophylaxis are angiotensin antagonists and B-blockers which are maybe considered in the setting of trastuzumab therapy. The early detection of declines in the LVEF during the course of treatment for cancer appears to be the best way to mitigate cardiac damage. Cardiac imaging historically relied upon 2D echocardiography and radionuclide imaging, but more recent 3D echocardiography, strain pattern, Doppler technology and cardiac MRI all have potential to further refine and accelerate the time to detection of cardiac changes from cancer therapy. Early detection and the use of cardioprotective measures may allow for partial or even complete recovery of cardiac function and ultimately lead to better quality of life and better survival for cancer patients.
References
Thavendiranathan P, et al. Breast cancer therapy-related cardiac dysfunction in adult women treated in routine clinical practice: a population-based cohort study. J Clin Oncol. 2016;34(19):2239–46.
Di Marco A, Cassinelli G, Arcamone F. The discovery of daunorubicin. Cancer Treat Rep. 1981;65(Suppl 4):3–8.
Amiri-Kordestani L, et al. First FDA approval of neoadjuvant therapy for breast cancer: pertuzumab for the treatment of patients with HER2-positive breast cancer. Clin Cancer Res. 2014;20(21):5359–64.
Geisberg CA, Sawyer DB. Mechanisms of anthracycline cardiotoxicity and strategies to decrease cardiac damage. Curr Hypertens Rep. 2010;12(6):404–10.
Guglin M, et al. Introducing a new entity: chemotherapy-induced arrhythmia. Europace. 2009;11(12):1579–86.
Curigliano G, et al. Cardiotoxicity of anticancer treatments: epidemiology, detection, and management. CA Cancer J Clin. 2016. doi:10.3322/caac.21341.
Haque R, et al. Cardiovascular disease after aromatase inhibitor use. JAMA Oncol. 2016. doi:10.1001/jamaoncol.2016.0429.
Khan NF, et al. Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: a database study. Br J Cancer. 2011;105(Suppl 1):S29–37.
Nathan PC, Amir E, Abdel-Qadir H. Cardiac outcomes in survivors of pediatric and adult cancers. Can J Cardiol. 2016;32(7):871–80.
Jones RL, Swanton C, Ewer MS. Anthracycline cardiotoxicity. Expert Opin Drug Saf. 2006;5(6):791–809.
Gaudin PB, et al. Myocarditis associated with doxorubicin cardiotoxicity. Am J Clin Pathol. 1993;100(2):158–63.
Von Hoff DD, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91(5):710–7.
Lefrak EA, et al. A clinicopathologic analysis of adriamycin cardiotoxicity. Cancer. 1973;32(2):302–14.
Mulrooney DA, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ. 2009;339:b4606.
Slamon DJ, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Mantarro S, et al. Risk of severe cardiotoxicity following treatment with trastuzumab: a meta-analysis of randomized and cohort studies of 29,000 women with breast cancer. Intern Emerg Med. 2016;11(1):123–40.
Wittayanukorn S, et al. Cardiotoxicity in targeted therapy for breast cancer: a study of the FDA adverse event reporting system (FAERS). J Oncol Pharm Pract. 2015. doi:10.1177/1078155215621150.
Qi WX, et al. Bevacizumab increases the risk of severe congestive heart failure in cancer patients: an up-to-date meta-analysis with a focus on different subgroups. Clin Drug Investig. 2014;34(10):681–90.
Chen Z, Ai D. Cardiotoxicity associated with targeted cancer therapies. Mol Clin Oncol. 2016;4(5):675–81.
Zambetti M, et al. Long-term cardiac sequelae in operable breast cancer patients given adjuvant chemotherapy with or without doxorubicin and breast irradiation. J Clin Oncol. 2001;19(1):37–43.
Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet. 2000;355(9217):1757–70.
Hasan S, et al. Doxorubicin cardiotoxicity in African Americans. J Natl Med Assoc. 2004;96(2):196–9.
Szmit S, et al. Pre-existing arterial hypertension as a risk factor for early left ventricular systolic dysfunction following (R)-CHOP chemotherapy in patients with lymphoma. J Am Soc Hypertens. 2014;8(11):791–9.
da Fonseca LG, et al. Cardiac safety of (neo)adjuvant trastuzumab in the community setting: a single-center experience. Breast Care (Basel). 2014;9(4):255–60.
Pizzuti L, et al. Neoadjuvant sequential docetaxel followed by high-dose epirubicin in combination with cyclophosphamide administered concurrently with trastuzumab: the DECT trial. J Cell Physiol. 2016. doi:10.1002/jcp.25432.
Cascales A, et al. Association of anthracycline-related cardiac histological lesions with NADPH oxidase functional polymorphisms. Oncologist. 2013;18(4):446–53.
Stoddard MF, et al. Prolongation of isovolumetric relaxation time as assessed by Doppler echocardiography predicts doxorubicin-induced systolic dysfunction in humans. J Am Coll Cardiol. 1992;20(1):62–9.
Schwartz RG, et al. Congestive heart failure and left ventricular dysfunction complicating doxorubicin therapy. Seven-year experience using serial radionuclide angiocardiography. Am J Med. 1987;82(6):1109–18.
Piotrowski G, et al. Role of echocardiography in monitoring of cardiac toxicity of cancer pharmacotherapy. Expert consensus statement of the Polish clinical forum for cardiovascular imaging. Kardiol Pol. 2014;72(6):558–75.
Gavila J, et al. Evaluation and management of chemotherapy-induced cardiotoxicity in breast cancer: a Delphi study. Clin Transl Oncol. 2016. doi:10.1007/s12094-016-1508-y.
Truong SR, et al. Evaluating the utility of baseline cardiac function screening in early-stage breast cancer treatment. Oncologist. 2016;21(6):666–70.
Yoon GJ, et al. Left ventricular dysfunction in patients receiving cardiotoxic cancer therapies are clinicians responding optimally? J Am Coll Cardiol. 2010;56(20):1644–50.
Karabay CY, et al. Mitral regurgitation due to papillary muscle dyssynchrony during trastuzumab treatment. Cardiology. 2010;117(4):296–300.
Jiji RS, Kramer CM, Salerno M. Non-invasive imaging and monitoring cardiotoxicity of cancer therapeutic drugs. J Nucl Cardiol. 2012;19(2):377–88.
Guendouz S, et al. Restrictive cardiomyopathy associated with left ventricle and left atria endocardial calcifications following chemotherapy. J Am Coll Cardiol. 2011;57(15):1633.
Bayram C, et al. Evaluation of cardiotoxicity by tissue Doppler imaging in childhood leukemia survivors treated with low-dose anthracycline. Pediatr Cardiol. 2015;36(4):862–6.
Karakurt C, Kocak G, Ozgen U. Evaluation of the left ventricular function with tissue tracking and tissue Doppler echocardiography in pediatric malignancy survivors after anthracycline therapy. Echocardiography. 2008;25(8):880–7.
Mavinkurve-Groothuis AM, et al. Myocardial strain and strain rate in monitoring subclinical heart failure in asymptomatic long-term survivors of childhood cancer. Ultrasound Med Biol. 2010;36(11):1783–91.
Fallah-Rad N, et al. The utility of cardiac biomarkers, tissue velocity and strain imaging, and cardiac magnetic resonance imaging in predicting early left ventricular dysfunction in patients with human epidermal growth factor receptor II-positive breast cancer treated with adjuvant trastuzumab therapy. J Am Coll Cardiol. 2011;57(22):2263–70.
Lunning MA, et al. Cardiac magnetic resonance imaging for the assessment of the myocardium after doxorubicin-based chemotherapy. Am J Clin Oncol. 2015;38(4):377–81.
de Ville de Goyet M, et al. Prospective cardiac MRI for the analysis of biventricular function in children undergoing cancer treatments. Pediatr Blood Cancer. 2015;62(5):867–74.
Ryerson AB, et al. Assessing anthracycline-treated childhood cancer survivors with advanced stress echocardiography. Pediatr Blood Cancer. 2015;62(3):502–8.
Henri C, Heinonen T, Tardif JC. The role of biomarkers in decreasing risk of cardiac toxicity after cancer therapy. Biomark Cancer. 2016;8(Suppl 2):39–45.
Lenihan DJ, et al. The utility of point-of-care biomarkers to detect cardiotoxicity during anthracycline chemotherapy: a feasibility study. J Card Fail. 2016;22(6):433–8.
Putt M, et al. Longitudinal changes in multiple biomarkers are associated with cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. Clin Chem. 2015;61(9):1164–72.
Katsurada K, et al. High-sensitivity troponin T as a marker to predict cardiotoxicity in breast cancer patients with adjuvant trastuzumab therapy. Springerplus. 2014;3:620.
De Iuliis F, et al. Serum biomarkers evaluation to predict chemotherapy-induced cardiotoxicity in breast cancer patients. Tumour Biol. 2016;37(3):3379–87.
Lien MY, et al. Safety and efficacy of pegylated liposomal doxorubicin-based adjuvant chemotherapy in patients with stage I-III triple-negative breast cancer. Anticancer Res. 2014;34(12):7319–26.
O’Brien ME, et al. Reduced cardiotoxicity and comparable efficacy in a phase III trial of pegylated liposomal doxorubicin HCl (CAELYX/Doxil) versus conventional doxorubicin for first-line treatment of metastatic breast cancer. Ann Oncol. 2004;15(3):440–9.
Bjelogrlic SK, et al. Activity of d,l-alpha-tocopherol (vitamin E) against cardiotoxicity induced by doxorubicin and doxorubicin with cyclophosphamide in mice. Basic Clin Pharmacol Toxicol. 2005;97(5):311–9.
Berthiaume JM, et al. Dietary vitamin E decreases doxorubicin-induced oxidative stress without preventing mitochondrial dysfunction. Cardiovasc Toxicol. 2005;5(3):257–67.
Wagdi P, et al. Cardioprotection in patients undergoing chemo- and/or radiotherapy for neoplastic disease. A pilot study. Jpn Heart J. 1996;37(3):353–9.
Swain SM, et al. Delayed administration of dexrazoxane provides cardioprotection for patients with advanced breast cancer treated with doxorubicin-containing therapy. J Clin Oncol. 1997;15(4):1333–40.
Pituskin E, et al. Rationale and design of the Multidisciplinary Approach to Novel Therapies in Cardiology Oncology Research Trial (MANTICORE 101-Breast): a randomized, placebo-controlled trial to determine if conventional heart failure pharmacotherapy can prevent trastuzumab-mediated left ventricular remodeling among patients with HER2+ early breast cancer using cardiac MRI. BMC Cancer. 2011;11:318.
Yun S, Vincelette ND, Abraham I. Cardioprotective role of beta-blockers and angiotensin antagonists in early-onset anthracyclines-induced cardiotoxicity in adult patients: a systematic review and meta-analysis. Postgrad Med J. 1081;2015(91):627–33.
Gulati G, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016;37(21):1671–80.
Pituskin E, Mackey J, Koshman S. MANTICORE 101: multidisciplinary approach to novel therapies in cardio-oncology research. In: San Antonio breast cancer symposium. December 9–12, 2015: San Antonio, TX.
Liu L, et al. Preventive effect of low-dose carvedilol combined with candesartan on the cardiotoxicity of anthracycline drugs in the adjuvant chemotherapy of breast cancer. Zhonghua Zhong Liu Za Zhi. 2013;35(12):936–40.
Georgakopoulos P, et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin-treated lymphoma patients: a prospective, parallel-group, randomized, controlled study with 36-month follow-up. Am J Hematol. 2010;85(11):894–6.
Bosch X, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies). J Am Coll Cardiol. 2013;61(23):2355–62.
Seicean S, et al. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J Am Coll Cardiol. 2012;60(23):2384–90.
Acar Z, et al. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2011;58(9):988–9.
Chotenimitkhun R, et al. Chronic statin administration may attenuate early anthracycline-associated declines in left ventricular ejection function. Can J Cardiol. 2015;31(3):302–7.
Kalam K, Marwick TH. Role of cardioprotective therapy for prevention of cardiotoxicity with chemotherapy: a systematic review and meta-analysis. Eur J Cancer. 2013;49(13):2900–9.
Akolkar G, et al. The role of renin angiotensin system antagonists in the prevention of doxorubicin and trastuzumab induced cardiotoxicity. Cardiovasc Ultrasound. 2015;13:18.
Cardinale D, et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol. 2010;55(3):213–20.
Ryberg M, et al. Epirubicin cardiotoxicity: an analysis of 469 patients with metastatic breast cancer. J Clin Oncol. 1998;16(11):3502–8.
Ewer MS, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol. 2005;23(31):7820–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no conflict of interest related to this work.
Rights and permissions
About this article
Cite this article
Fanous, I., Dillon, P. Cancer treatment-related cardiac toxicity: prevention, assessment and management. Med Oncol 33, 84 (2016). https://doi.org/10.1007/s12032-016-0801-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-016-0801-5