Abstract
Recent advances in diagnostic and treatment strategies for various cancers suggest that the number of cancer survivors will continue to grow over the next few decades. Coupled with the aggressiveness of new chemotherapy regimens, emergence of molecularly targeted agents, frequent use of dual modality treatments that combine systemic therapy with radiation, the incidence of treatment-related side effects will also likely continue to increase. Due, in part, to its diverse clinical manifestations and significant morbidity burden, prompt diagnosis and effective management of cardiotoxicity can be particularly challenging for members of the cancer care team. In order to optimize care and follow-up for the growing population of cancer patients and survivors, a basic understanding of the risk factors, treatments, and outcomes for the various cardiac toxicities is absolutely essential. Herein, the cardiotoxicity profiles of several relevant classes of anticancer agents are discussed, with emphasis on anthracyclines, trastuzumab, molecularly targeted agents, and radiotherapy. A brief outline of the causes and underlying pathophysiology as well as management and prognosis of the different cardiac manifestations is introduced and explored.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Cancer and cardiovascular disease are by far the two leading causes of death in the developed countries. Modern developments in diagnostic and treatment strategies within all aspects of cancer management—medical, surgical, and radiation oncology—mean that an increasing number of patients who are diagnosed with cancer today will live to become long-term cancer survivors. The majority of these individuals would have received some form of anticancer treatment during the course of their illness as a means to control their cancer or manage their symptoms. Because many systemic therapeutic agents as well as radiation techniques can be associated with acute, early, or late cardiac toxicities, a significant number of patients with a prior history of cancer are at risk of developing cardiovascular complications. Manifestations are diverse and can span the full spectrum of cardiac diseases such as cardiac arrhythmias, cardiomyopathies, and ischemic heart diseases. In addition to worsening overall quality of life, these conditions are not infrequently irreversible or fatal; therefore, they highlight the importance for members of the cancer care team to share a basic awareness of the potential risk factors, causes, and management of these various cardiac toxicities. Additionally, recent advances in basic and translational cancer research have led to an explosion in the use of mechanistically based therapies many of which have been shown to cause cardiovascular complications.
Cancer survivors who develop cardiac dysfunction as a result of their treatment could face devastating consequences and worse survival [1]. Consequently, early identification, monitoring, and prevention are essential to minimize irreversible damage. Chemotherapy-related cachexia, emesis, and myelosuppression are dose-limiting toxicities which in the past have prevented the administration of chemotherapy doses that are sufficiently high enough to cause cardiac toxicities. Over the last decade, however, advances in symptom control and supportive care measures, including the frequent use of 5-HT3 antagonists (e.g., ondansetron, granisetron) and granulocyte colony-stimulating factors, have not only improved patient tolerability toward chemotherapy, but they have also allowed clinicians to deliver more intensive and prolonged courses of treatment in an effort to maximize cancer control. With the uptake of more aggressive systemic treatment regimens, cardiac complications are increasingly recognized in a growing population of cancer patients and survivors. The more widespread availability of imaging facilities coupled with recent improvements in radiographic modalities has further resulted in the detection of more subclinical cardiac abnormalities. Conversely, newer radiation techniques are designed to limit unnecessary exposure to vital organs, such as the heart. Such efforts have decreased the incidence of radiation-related cardiac dysfunction, but some degree of risk remains.
At the cellular level, the effect of antineoplastic drugs on cardiomyocytes has been divided into two main categories: type I cardiotoxicity , as seen with anthracyclines, is characterized by structural changes in cardiomyocytes leading to apoptosis and death. This process is dose dependent and irreversible. Conversely, in type II cardiotoxicity , myocardial dysfunction and loss of contractility (stunning) occur with minimal structural changes. Classically seen with trastuzumab , type II injury is not dose dependent and is often reversible with discontinuation of the drug. Cardiac toxicities have traditionally been classified as “acute” (e.g., those that occur during or immediately after chemotherapy administration), “early” (typically within the first year after treatment), or “late/delayed” (e.g., years to decades after chemotherapy or radiation exposure). Recent evidence suggests, at least with anthracyclines, that cardiotoxicity represents a continuum that begins with subclinical decline in LVEF that can progress to symptomatic heart failure [2, 3]. As clinicians develop a higher vigilance for the risk of treatment-related cardiac toxicities, a variety of strategies have been employed to minimize this serious risk without unnecessarily compromising treatment efficacy. These various strategies include modifying the schedule of drug administration or radiation exposure, altering the actual drug molecule or the vehicle for drug delivery, or using adjunctive “cardioprotective” agents during active treatment. Unfortunately, none of these approaches have proven to be completely successful, thereby underscoring the ongoing need to closely monitor patients who are either currently receiving or have previously received potentially cardiotoxic agents.
In this chapter, the cardiotoxicity profiles of several pertinent, commonly used classes of anticancer agents, including anthracyclines (e.g., doxorubicin, epirubicin), molecularly targeted drugs (e.g., trastuzumab), and radiotherapy will be introduced and discussed. There will be an emphasis on anthracyclines since they are the most frequently implicated agents for cancer treatment-related cardiac dysfunction. Potential cardiovascular side effects of hormonal anticancer treatments are beyond the scope of this review.
Anthracyclines
Background
A class of chemotherapy drugs widely used in oncology to treat a variety of solid tumors and hematologic malignancies, anthracyclines exert their cytocidal activity by several mechanisms including inhibition of DNA and RNA synthesis by directly binding to the DNA of replicating cells, impairing DNA repair by inhibition of the enzyme topoisomerase II and generation of cytotoxic free radicals. Because cancer cells are rapidly proliferating, these various actions of anthracyclines can confer effective antitumor activity. The exact mechanisms by which anthracyclines contribute to cardiac dysfunction and myocardial damage are not entirely understood and might differ from its anticancer effects, particularly since myocytes of the heart are not actively replicating. One possible mechanism for their cardiotoxicity is that anthracyclines cause an increase in the generation of reactive oxygen species as well as a decrease in endogenous levels of antioxidant enzymes that are normally responsible for scavenging oxygen free radicals throughout the body. This can lead to an increase in oxidative stress, which may then result in irreversible myocardial damage [4, 5]. More recent evidence suggests that anthracyclines form a complex with the topoisomerase II beta enzyme present in cardiomyocytes leading to DNA double-strand breakage and cell death [6].
Risk Factors
Several clinical factors have been identified that predispose individuals to an elevated risk of developing anthracycline-induced cardiac toxicities such as dose of the drug, age, female gender, prior mediastinal radiation, use of other cardiotoxic agents, and preexisting cardiac conditions. One of the strongest and most reliable predictors is the cumulative dose of anthracycline drug delivered. With doxorubicin, for example, a combined analysis of three prospective trials showed that congestive heart failure (CHF) occurred in 5%, 26%, and 48% of patients who have received a cumulative dose of 400 mg/m2, 550 mg/m2, and 700 mg/m2, receptively [7]. Based on these observations, it is recommended that the cumulative dose of doxorubicin not exceed 400–500 mg/m2. While for epirubicin, the maximal cumulative dose is set at 900 mg/m2. While these cumulative dose thresholds serve as a general guideline for clinicians and patients, treatments should be individualized. With the availability of noninvasive surveillance techniques, such as echocardiograms and MUGA scans that can assess cardiac function, therapy should be stopped at much lower cumulative doses if there is early evidence of cardiac dysfunction. Conversely, treatment to higher cumulative doses may also be considered if there are no signs of cardiac toxicities and anthracyclines are clinically indicated for maintaining tumor control.
Extremes of age is another well-established risk factor. Children have been consistently shown to develop cardiac toxicities at much lower cumulative doses than in adults. A similar relationship is observed in older patients, many of whom have preexisting hypertension or heart conditions. The precise reasons for this age-related association are unclear, but it is possible that the very young and very old age groups have less functional cardiac reserve to accommodate the strain that anthracyclines place on myocytes [8]. In a similar manner, a prior history of radiotherapy also increases susceptibility to cardiotoxic effects, possibly because of diminished cardiac reserve caused by previous radiation exposure. This is particularly evident for those who have received mediastinal or chest wall irradiation. Such exposures probably introduce moderate degrees of damage to the cardiac endothelium and coronary blood vessels, and subsequent treatment with anthracyclines results in further insults to the heart [9]. Likewise, the use of cardiotoxic nonanthracycline agents in combination with anthracyclines often poses a synergistic toxic effect. One common example would be the concurrent or sequential administration of taxanes and trastuzumab, both of which are cardiotoxic, along with anthracyclines for the management of both early- and advanced-stage breast cancers [10, 11].
The risk of cardiac toxicity after anthracycline exposure is variable between different individuals suggesting that genetic disposition is in play. Polymorphism in genes encoding several proteins involved in tissue remodeling, protection from oxidative damage, and drug efflux have been suggested [4, 12].
Clinical Manifestations
The clinical presentation, the severity of dysfunction, as well as the onset of cardiac toxicities are highly variable. Acute toxicities may present as rhythm disturbances (such as atrial fibrillation), constitutional symptoms from pericarditis or myocarditis, chest discomfort due to cardiac ischemia, or dyspnea as a result of heart failure. Fortunately, early cardiac events are rare, and many are actually subclinical in nature with minimal sequelae. Therefore, formal cardiac monitoring is usually not warranted during the initial administration of anthracyclines, unless there are pertinent findings on patient history, physical examination, or recent cardiac tests that suggest a heightened risk for complications. While acute cardiac dysfunction may occur, the peak time for the appearance of cardiac toxicities is typically about 3–6 months after the last anthracycline dose, at which point serial monitoring of cardiac function should be considered. If early symptoms and signs of possible cardiomyopathy are left undetected or untreated, mortality can exceed 50% [13].
Chronic cardiac toxicity is most commonly seen within the first year following chemotherapy and ranges from asymptomatic left ventricular (LV) dysfunction to CHF. In one prospective study, the vast majority of LV dysfunction (98%) occurred within the first year2. Nonetheless, the onset of cardiac dysfunction can rarely occur more than 10 years after the last dose of anthracycline administered, as evidenced by cases of serious heart failure found among long-term childhood cancer survivors, who were previously treated with high doses of anthracyclines as part of their chemotherapy regimens. In most of these situations, the cardiac abnormality presents as nonischemic dilated cardiomyopathy. Interestingly, the risk of such late cardiac problems appears to be lower among young women with early-stage breast cancers who have received only a short, adjuvant course of anthracycline-based chemotherapy , with the proviso that the cumulative dose did not exceed 300 mg/m2 [9]. This finding further emphasizes the strong dose–response pattern that exists between the cumulative dose administered and the risk of cardiac toxicities. One important consideration remains: when compared to those receiving chemotherapy without anthracyclines or those not given any chemotherapy at all, the overall cardiac risk remains higher in patients who have previously been treated with any anthracyclines, irrespective of dose.
Minimizing the Risk
First and foremost, to minimize the risk, limit the lifetime cumulative dose as described above. Several other approaches have been introduced to potentially lower the risk of anthracycline-induced cardiac toxicities, including (1) altering the mode of drug administration, (2) encapsulating the anthracycline drug molecule within liposomes, and (3) using adjunctive “cardioprotective” agents during treatment. Along with these strategies, intensive and serial monitoring with noninvasive cardiac imaging techniques has also been advocated to detect the earliest possible evidence of cardiotoxicity, at which point prompt and necessary measures can be taken to prevent the development of more severe forms of cardiac dysfunction.
A continuous infusion of anthracycline over the course of 48–96 h may lower the incidence of cardiotoxicity. This potential benefit has been suggested based on small observational studies, which showed that patients treated with prolonged infusions of anthracyclines were less likely to develop heart problems, defined as >10% reduction in left ventricular ejection fraction, when compared to those who received the conventional bolus treatment [14]. Infusional delivery, however, is less practical and resource intensive and might be associated with worse outcomes. For these reasons, anthracyclines are still typically administered by the bolus route.
There are also ongoing efforts aimed at modifying the anthracycline molecule to minimize cardiotoxic effects, while maintaining its antitumor efficacy. A prime example of this strategy is the incorporation of anthracyclines into liposomes, which has been shown in studies to have a similar efficacy as free, unbound anthracyclines. In addition, this formulation is appealing because it lowers the incidence of cardiac dysfunction and also permits substantially higher cumulative doses to be delivered [15].
Finally, the use of adjunctive cardioprotective agents, such as dexrazoxane, in conjunction with anthracyclines may reduce cardiotoxicity. Dexrazoxane is an EDTA-like chelator [16] believed to prevent cardiac damage by binding to iron stores that are released from intracellular storage during oxidative stress. It has been shown in randomized controlled trials to reduce the incidence of anthracycline-associated heart failure and subclinical cardiac toxicity [17, 18]. While this cardioprotective agent can be helpful, it is imperfect due to concerns about its potential to interfere with cancer therapy, its apparent association with lower treatment response rates, and its possible exacerbation of anthracycline-induced myelosuppression [19]. Unfortunately, data in these areas have been inconsistent; thus, it is currently unclear whether the benefits of dexrazoxane truly outweigh its risks. At the present time, the American Society of Clinical Oncology endorses the use of dexrazoxane only for patients who have received a cumulative dose of doxorubicin ≥300 mg/m2 or an equivalent dose of epirubicin for the treatment of metastatic disease. Given its potential detrimental impact on antitumor efficacy as well as on myelosuppression, dexrazoxane is not recommended for use in the adjuvant setting when the goal of therapy is cure. The use of dexrazoxane does not entirely eliminate the risk of cardiotoxicity. As such, patients who receive dexrazoxane should continue on regular cardiac monitoring.
Preliminary research points toward a possible benefit of concurrently administering β-blockers and ACE inhibitors with anthracyclines as a primary preventive measure against cardiotoxicity. In some of these prior studies, the prophylactic use of β-blockers, ACE inhibitors, or both was associated with better preservation of left ventricular ejection fraction [20,21,22]. Definitive conclusions, however, are difficult to draw as data in this regard have been based on retrospective analyses or small randomized trials. Whether benefit from prophylactic use of these agents is clinically meaningful remains to be seen.
Cardiac Monitoring
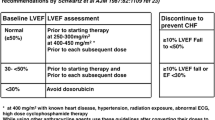
Serial noninvasive cardiac monitoring continues to be an essential component in the ongoing management of anthracycline-treated patients so that the earliest possible evidence of cardiotoxicity can be detected. A variety of monitoring techniques that mostly rely on measuring changes in LV ejection fraction have been employed; and guidelines have been developed for monitoring and drug discontinuation by expert groups. One set of proposed guidelines is shown in Table 11.1. These guidelines are mostly based on consensus rather than evidence. Echocardiography is perhaps the most frequently used noninvasive strategy for evaluating left ventricular ejection fraction. This modality is currently endorsed by the American College of Cardiology for monitoring anthracycline-induced cardiotoxicity. Owing to its widespread availability and its lack of radiation exposure, echocardiograms remain a popular standard. Disadvantages, however, include its poor reproducibility and variability in interpretation among clinicians. In addition, it can be occasionally difficult to accurately quantify the global ventricular function.
Radionuclide imaging , using multi-gated cardiac blood pool imaging (MUGA scan), has become a common technique for monitoring cardiac dysfunction because it provides results that are highly reproducible making it ideal for serial measurements. It also can detect subtle changes in systolic and diastolic function. As a result of such early detection, some cardiac abnormalities may be potentially reversible. Disadvantages of MUGA scans, however, include limited ability to assess structural cardiac abnormalities (such as valvular heart disease), small radiation exposure, and the need for intravenous access.
There is also an emerging interest in exploring newer approaches to cardiac monitoring. Cardiac magnetic resonance (CMR) imaging , for instance, may be particularly useful when other imaging modalities yield suboptimal images. CMR can also demonstrate subclinical changes such as myocardial edema prior to the onset of LV dysfunction [23]. Alternately, there is ongoing research to clarify the role of cardiac biomarkers, such as troponin and natriuretic peptide. The hypothesis is that these biomarkers may provide earlier signs of cardiac damage than any standard imaging techniques. In preliminary studies, elevations in troponin and natriuretic peptide were associated with the severity of myocardial damage secondary to anthracyclines, correlated with the degree of decrease in left ventricular ejection fraction, and were predictive of subsequent cardiac-related morbidity and mortality [24]. Whether early elevations in these biomarkers predict any protective benefit from the prophylactic use of conventional therapeutic agents for heart failure, such as β-blockers and ACE inhibitors, is uncertain. Overall, these early data are promising for identifying early anthracycline-related cardiotoxicity, but there is insufficient evidence to support their routine use at the present time.
Finally, it is important to recognize that the “gold standard” of assessing anthracycline cardiotoxicity is the endomyocardial biopsy since this method allows for direct evaluation of both the presence and the degree of cardiac damage [25]. Characteristic features of chemotherapy-related injury include depletion of myofibrillary bundles, evidence of myofibrillar lysis, mitochondrial disruption, and intramyocyte vacuolization. Understandably, this procedure is invasive and itself carries the risk of complications, such as arrhythmias and bleeding. Furthermore, the interpretation of the biopsy specimens requires special expertise in histology and pathology. For these reasons, endomyocardial biopsy has typically been reserved for patients in whom a definitive diagnosis is required or for those in whom noninvasive imaging modalities fail to provide adequate information regarding the cardiac functional status.
Prognosis and Management
The short- and long-term prognosis of individuals affected by anthracycline-induced cardiac toxicities appears to depend heavily on the severity and stage of cardiac symptoms at the time when dysfunction is initially diagnosed. This observation further underscores the importance of prompt and early detection. Patients who manifest with clinical symptoms at diagnosis have a worse outcome when compared with those who present with an asymptomatic decrease in left ventricular ejection fraction. In a prospective study of 2625 women treated with anthracyclines for a variety of solid tumors, 226 (9%) developed cardiac toxicity of whom full or partial recovery of LVEF was observed in 82% of cases after prompt initiation of enalapril, either alone or in conjunction with a β-blocker [2]. These data indicate significant potential for reversibility with early detection and treatment and challenge the concept of irreversible myocardial damage. However, the potential for spontaneous recovery in asymptomatic patients is unclear.
Currently, anthracycline-associated cardiac dysfunction is treated in a similar fashion to other causes of LV dysfunction with the use of medical therapy, such as β-blockers and ACE inhibitors. At least one study suggests that ACE inhibitors should be considered as first-line treatment for both asymptomatic left ventricular dysfunction and symptomatic heart failure. In this small series of women with metastatic breast cancer who received epirubicin, 7 of 8 women treated with ACE inhibitors had an increase in ejection fraction ≥15% whereas only 1 of 33 women without ACE inhibitor therapy demonstrated a similar response [26]. Until more evidence becomes available, medical management of chemotherapy-related heart failure should incorporate the use of these medications. To this end, most experts also concur that for patients in whom anthracycline-induced cardiotoxicity is refractory to standard medical therapy, interventions such as cardiac resynchronization therapy should at the very least be considered in the appropriate setting.
HER-2-Targeted Therapy
Trastuzumab
Background
Trastuzumab is a humanized monoclonal antibody that targets the human epidermal growth factor receptor-2 (HER-2), a receptor tyrosine kinase that is overexpressed in up to 25% of breast cancer patients. Binding of trastuzumab to the extracellular domain of HER-2 results in inhibition of downstream signal transduction, thereby resulting in cellular growth inhibition. This molecularly targeted agent has led to dramatic improvement in outcomes and has become a critical component in the management of both adjuvant and metastatic HER-2-positive breast cancer. These benefits must be carefully weighed against the added risk of cardiac toxicities from trastuzumab treatment.
The precise mechanisms underlying trastuzumab-associated cardiac dysfunction are as yet unclear. Of note, considering that many patients who receive trastuzumab have also been previously treated with anthracyclines, it was once postulated that potentiation of prior anthracycline-induced cardiac damage was the most responsible factor. However, histopathological studies from endomyocardial biopsy specimens from individuals with trastuzumab-related cardiac dysfunction have refuted this hypothesis, since anthracycline-based structural changes were not always observed. Moreover, trastuzumab dysfunction can develop even in the setting of anthracycline-naïve patients. Preliminary studies indicate that trastuzumab cardiotoxicity may be directly related to HER-2 blockade (on-target toxicity) [27]. Early animal models, for instance, suggest that HER-2 signaling is an important step in embryonic cardiac development. It also participates in protecting the heart from potential cardiotoxins where studies show that HER-2 gene knockout mice are more likely to develop dilated cardiomyopathy and their myocytes demonstrate increased susceptibility to anthracycline-induced cell death [28]. In further support, serum HER-2 levels appear to be increased in patients with chronic heart failure with levels correlating inversely with left ventricular function [29].
The following section briefly reviews the clinical manifestations of trastuzumab cardiotoxicity, the guidelines for monitoring cardiac function during treatment, and the management of patients who experience cardiotoxicity as a result of trastuzumab exposure.
Risk Factors
The overall incidence of cardiac dysfunction in trastuzumab-treated patients ranges between 3% and 19%, while the incidence of symptomatic heart failure is 2–4%. Cardiac toxicity is modest when trastuzumab is used alone, but the rate becomes significantly higher among individuals who receive trastuzumab concurrently with other potentially cardiotoxic agents, especially anthracyclines [30]. In the pivotal phase III trial that evaluated the benefit of adding trastuzumab to conventional cytotoxic chemotherapy for metastatic breast cancer, the incidence of any cardiac dysfunction was 27% for trastuzumab plus doxorubicin and cyclophosphamide (AC) vs. 8% for AC alone and 13% for trastuzumab plus paclitaxel vs. 1% for paclitaxel alone. As expected, the incidence of severe heart failure, consisting of either class III or IV symptoms, was substantially lower: 16% with trastuzumab plus AC vs. 4% for AC alone and 2% with trastuzumab plus paclitaxel vs. 1% for paclitaxel alone [11]. These findings resulted in the recommendation that concurrent delivery of anthracyclines and trastuzumab be generally avoided or used with great caution in favor of sequential therapy because of the increased risk of cardiotoxicity associated with concurrent administration. Subsequent trials employing frequent cardiac monitoring showed lower incidence of LV dysfunction and symptomatic heart failure with trastuzumab use in combination with anthracyclines and to much lower extent with the use of taxanes. The precise mechanisms underlying the additive cardiotoxicity of anthracyclines and trastuzumab are unclear, but upregulation of HER-2 blockade by anthracyclines is thought to be at least partially responsible for this synergistic effect.
Aside from concurrent anthracycline use, additional risk factors have been proposed to identify individuals with a higher likelihood of developing trastuzumab-related cardiotoxicity including older age, preexisting LV dysfunction, use of antihypertensive medications, higher body weight, prior chest radiation, and prior therapy with anthracyclines.
Clinical Manifestations
Unlike the adverse events observed with anthracyclines, trastuzumab-related cardiac toxicities tend to manifest as asymptomatic reductions in ejection fraction as opposed to overt heart failure. In further contrast, trastuzumab-associated cardiac disease is not dependent on the cumulative dose of drug administered. It is commonly reversible with treatment cessation and frequently amenable to treatment rechallenge if cardiac function recovers after a planned treatment break.
Because of these differences, chemotherapy-related cardiac abnormalities are categorized by some experts into type I and type II dysfunction [31]. The former “type I” refers to anthracycline-associated injury, which results in permanent myocyte destruction and clinical heart failure. Conversely, the latter “type II” refers to trastuzumab-associated damage, which is more often associated with transient loss of cardiac contractility and less likely to involve myocyte death or clinical heart failure. Owing to its somewhat transient nature, this form of dysfunction may be reversible.
Minimizing the Risk
At least in the adjuvant setting, several approaches have been proposed as potential ways to lower the risk of trastuzumab-related cardiotoxicity. First, attempts at shortening the duration of trastuzumab treatment were examined in clinical trials. Most adjuvant breast cancer trials involving trastuzumab have administered the agent over the course of 12 months. In the FinHer trial, an anthracycline- and taxane-containing regimen was compared to the same chemotherapy regimen plus a 9-week course of trastuzumab [32]. The trastuzumab arm showed a 35% improvement in distant disease-free survival (DFS), albeit nonsignificant. No cardiac dysfunction was observed in the trastuzumab study arm, suggesting that a decrease in the duration of exposure to trastuzumab may confer substantially less cardiac risk. However, the large phase III trial PHARE that involved 3384 patients failed to demonstrate non-inferiority with a shorter 6-month duration of trastuzumab compared with 12 months [33]. Therefore, despite more cardiac events, the currently recommended duration of adjuvant trastuzumab remains 12 months.
Another method is integrating trastuzumab into nonanthracycline-containing adjuvant regimens. One example consists of docetaxel and carboplatin, plus trastuzumab (TCH). Indeed, results from the BCIRG 006 trial, in which one of the three arms utilized the nonanthracycline-containing TCH adjuvant chemotherapy regimen, are promising with respect to lowering cardiac risk [34]. However, the anthracycline-containing regimen showed a nonsignificant trend toward improvement in survival. Until further evidence, anthracycline-based chemotherapy in combination with trastuzumab is preferred for locally advanced HER-2-positive breast cancer with larger tumors or involvement of locoregional lymph nodes. TCH is an acceptable alternative in select patients with small tumors.
As outlined previously, concurrent administration of trastuzumab with anthracyclines conferred a high rate of cardiac events and should be avoided.
Cardiac Monitoring
Heart function should be evaluated prior to the instigation of trastuzumab therapy as well as regularly during treatment. Patients with a normal baseline ejection fraction based on imaging, and neither symptoms nor signs of heart failure on history and physical examination, respectively, should be considered eligible for trastuzumab therapy. Patients with LVEF 40–50% may be considered on a case-by-case basis and warrant careful monitoring. While the following are not contraindications to therapy, special caution should be taken when patients with a prior history of hypertension, coronary artery disease, and valvular heart disease are receiving trastuzumab.
Currently, there are no universal recommendations on the optimal methods or schedules for monitoring patients for trastuzumab cardiotoxicity. However, clinical guidelines have been proposed by expert groups and major organizations. Expert consensus by the American Society of Echocardiography and the European Association of Cardiovascular Imaging [35] recommends a baseline assessment with history and physical examination and a cardiac imaging test. Additionally, measurement of troponin level is desirable. Patients should also undergo follow-up cardiac imaging every 3 months while on trastuzumab therapy.
Likewise, guidelines for the management of cardiac complications during trastuzumab therapy have been developed. A set of proposed guidelines is outlined in Table 11.2.
Prognosis and Management
In contrast to anthracyclines, data indicate that trastuzumab-related cardiac toxicities are frequently reversible in the majority of cases. Moreover, early evidence suggests that reintroduction of trastuzumab appears to be safe as long as cardiac abnormalities that develop while receiving the drug have resolved. In the phase III trial by Slamon et al., for instance, 33 patients continued trastuzumab for a median of 26 weeks despite developing an asymptomatic decline in ejection fraction. The cardiac status of 85% improved or remained the same, while symptoms were reversible for 75% of those who received standard medical therapy for heart failure [11]. Similarly, in a retrospective review from MD Anderson Cancer Center, the majority of those who stopped trastuzumab after developing symptomatic heart failure recovered with appropriate medical therapy, which consisted of β-blockers and ACE inhibitors [38]. While recovery was not universal, treatment was reinitiated in more than half of patients who interrupted trastuzumab for either an asymptomatic or symptomatic cardiac event, of whom most remained free of subsequent cardiac problems.
Other HER-2-Targeted Agents
A number of HER-2-targeted agents are now approved for the treatment of HER-2-positive breast cancer such as lapatinib, pertuzumab, and ado-trastuzumab emtansine (T-DM1). Each has a unique mechanism of action that differs from trastuzumab. Preliminary results from clinical trials have suggested that these agents have a favorable cardiac safety profile compared to trastuzumab. For example, in a pooled analysis of over 3600 patients using lapatinib, an oral small molecule tyrosine kinase inhibitor that affects both HER-2 and epidermal growth factor receptor (EGFR), cardiac events occurred in only 1.6% of patients, and mostly were asymptomatic declines in LV function [39]. Similarly, only 1.7% had a cardiac event in a phase III trial using T-DM1 which is an antibody-drug conjugate composed of trastuzumab linked to an antimitotic agent [40]. Nonetheless, these trials included highly selected patients, and the experience with these agents has been less extensive.
More recently, combining trastuzumab with other HER-2-targeted therapy was associated with improved outcomes. In the Cleopatra trial, combining pertuzumab with trastuzumab and docetaxel for first-line treatment in women with metastatic HER-2-positive breast cancer has resulted in an impressive 15-month improvement in OS establishing this regimen as the new standard in this setting. This combination was not associated with significantly worse cardiac toxicity.
Similar to trastuzumab, cardiac monitoring with use of these agents is recommended at baseline and at regular intervals.
Radiation Therapy
Background
Radiation therapy, which can be applied either by itself or in combination with systemic treatment agents, has contributed to significant improvements in the survival of patients with specific cancers, including the breast, Hodgkin disease, as well as malignancies involving the thorax (e.g., lung, esophagus). Such advances have resulted in a higher prevalence of cancer survivors, who are now at increased risk for late complications of radiation treatment, which can frequently involve the heart. Most of the data pertaining to the cardiovascular toxicities of radiation therapy are derived primarily from survivors of breast cancer and Hodgkin lymphoma, since these are diseases in which radiation is a frequent component of initial management and for which survival is often prolonged to a significant degree.
Radiation, if administered in sufficiently high doses or large volumes, can potentially damage any and all aspects of the heart, including the pericardium, myocardium, heart valves, coronary blood vessels, and conduction system. Pericarditis is a common manifestation of acute radiation injury, while chronic pericardial disease, coronary artery disease, restrictive cardiomyopathy, valvular disease, and conduction abnormalities can present years or decades after the original treatment. All of these conditions can potentially result in significant morbidity and mortality. The increasing recognition of radiation-induced cardiac toxicities has led to the development of improved radiotherapy techniques that aim to minimize the dose and volume of exposure to the heart. These contemporary measures appear to have drastically reduced the incidence of radiation-related cardiac complications, although there is still some residual risk.
Risk Factors
Several factors increase the risk for developing radiation-induced cardiac toxicities. These include the total radiation dose administered, the dose per fraction, the volume of heart irradiated, and the concurrent delivery of cardiotoxic systemic therapeutic agents, such as anthracyclines and trastuzumab [41]. In breast cancer, for example, the older generation of radiation techniques used in the management of this disease has almost always involved irradiation to the chest wall and surrounding lymph nodes. This classically resulted in a relatively high dose of radiation being delivered to a substantial volume of the heart. There is abundant evidence that this form of radiation delivery was associated with excess cardiovascular morbidity and mortality. Modern techniques currently deliver much less radiation to the heart and appear to have reduced the number of cases and degree of associated cardiotoxicity. In many of these cases, however, longer follow-up is required to confirm these safety findings.
Patient dependent factors, such as younger age at the time of initial radiation exposure and the presence of other personal risk factors for coronary heart disease, including hypertension, high serum cholesterol, and smoking history, may also increase the risk of radiation-associated cardiac dysfunction [41].
Clinical Manifestations
The main mechanism for radiation-related cardiac toxicities involves radiation damage to coronary blood vessels. This injury is believed to subsequently lead to the production of reactive oxygen species that disrupts DNA strands, which then results in secondary inflammatory changes and ultimately fibrosis. The classic hallmarks of radiation-induced cardiotoxicity consist of diffuse fibrosis of the myocardium coupled with narrowing of arterial and capillary lumens [42]. The ratio of capillaries to cardiac myocytes decreases by 50%, which contributes to cell death, cardiac ischemia, and further fibrosis. Collagen replaces the normal adipose tissue that usually forms around the outer layer of the heart, leading to pericardial fibrosis, effusion, and possibly tamponade. All of these changes can culminate in various forms of coronary artery diseases, valvular heart diseases, pericardial diseases, diastolic dysfunction, and dysrhythmias.
There are subtle differences between chemotherapy-related cardiac dysfunction and radiation-induced cardiac toxicities. First, irradiation causes fibrosis of the myocardium, which can lead to a restrictive cardiomyopathy. This appears to have a greater impact on diastolic rather than systolic cardiac function. This contrasts with the general effects of anthracyclines, which predominantly cause systolic dysfunction. Second, radiotherapy (specifically mediastinal irradiation) has been associated with an increased risk of clinically significant valvular abnormalities. Of potential clinical importance, many of the common abnormalities found in mediastinal irradiated patients are slowly progressive and may necessitate lifelong follow-up, some of which may also require antibiotic prophylaxis for endocarditis. Third, radiation can cause fibrosis of the conduction pathways in the heart, potentially leading to life-threatening arrhythmias and conduction defects that develop years after initial radiation therapy. Examples of such dysfunction include bradycardia and sick sinus syndrome, as well as complete and lesser degrees of heart block.
Additional Aspects
Unlike chemotherapy-induced cardiotoxicity, cardiac dysfunction related to radiation may be more challenging to manage in part because of its diverse manifestations. Improvements in radiotherapeutic techniques have been the primary means of decreasing the cardiac risk by minimizing the amount of radiation received by the heart. It is noteworthy that cardiovascular complications still appear more frequently in patients with left-sided than right-sided tumors, providing some evidence that the risk associated with radiation has not been completely eliminated with the newer generation of methods for radiotherapy.
Awareness of key factors that modify the risk of cardiovascular toxicity is another channel in which complications can be reduced. The size of the radiation field and the dose of exposure, for instance, determine the amount of incidental irradiation to the heart. Studies that compared breast cancer patients who received internal mammary lymph node irradiation were noted to have an increased risk of cardiovascular complications compared to those in whom the internal mammary lymph nodes were not included in the field [43]. Thus, radiation field and radiation dose are parameters that should be minimized, whenever possible. Care must also be taken to modify other risk factors for cardiovascular disease, such as hypertension, hyperlipidemia, and smoking, as well as to adequately manage preexisting coronary artery disease, since all of these variables may increase and potentiate radiation-related cardiotoxicity. Special attention is further warranted when radiation is used in patients who have or will receive known cardiotoxic agents, such as anthracyclines and trastuzumab.
Nonanthracycline Agents
Fluoropyrimidines
5-Fluorouracil is widely used in various chemotherapy regimens to fight a diverse array of cancers. Because of its frequent use, it is the second most common cause of chemotherapy-related cardiotoxicity after anthracyclines. The most frequent cardiac side effect from 5-fluorouracil is anginal chest pain. Myocardial infarction, acute pulmonary edema, and pericarditis can also occur, but these events are much rarer. The underlying mechanism for 5-flourouracil cardiotoxicity is thought to be due to coronary artery vasospasm. Its incidence is estimated to be around 8% [44]. The risk may be related to the mode of 5-flourouracil administration where infusional therapy is associated with a higher risk than bolus treatment. A prior history of coronary artery disease and concurrent use of cardiotoxic agents, including chemotherapy and radiation, also increase the risk. Fortunately, cardiac symptoms typically resolve with the cessation of 5-flourouracil treatment and the instigation of standard antianginal medical therapy. Rechallenging patients who have previously experienced 5-fluoruracil-related cardiac toxicities is somewhat controversial and generally not recommended due to high rates of recurrence. If rechallenge is being considered, it should be done under cardiac monitoring and close observation by specialized medical personnel. Alternatively, switching to non-fluoropyrimidine regimens is preferred. Furthermore, symptomatic patients should ideally undergo cardiac testing to rule out occult coronary ischemia.
Capecitabine is an oral fluoropyrimidine that is metabolized to 5-flourouracil, which is the active anticancer form of the drug. Thus, the cardiac toxicity profile of capecitabine is very similar to that observed for 5-flourouracil [45].
Taxanes
For taxanes such as paclitaxel, mild bradycardia and heart blocks can occur, although these are usually relatively asymptomatic. Overall, the incidence of these events is very low, and thus routine cardiac monitoring is not required for typical patients without risk factors. It is important to note that the nanoparticle albumin-bound paclitaxel (e.g., nab-paclitaxel) bodes the same cardiac toxicity profile as the regular, non-albumin-bound formulation. Similarly, conduction abnormalities and angina have been reported in users of docetaxel. Both paclitaxel and docetaxel also appear to potentiate the cardiotoxic effects of anthracyclines, as described previously [46].
Anti-angiogenic Agents
The vascular endothelial growth factor (VEGF) signaling pathway plays a critical role in tumor angiogenesis and has been a major target for cancer therapies leading to approval of more than a dozen drugs for a variety of cancers. Inhibition of the VEGF pathway can be achieved by several ways including the use monoclonal antibodies that block VEGF (such as bevacizumab) or its receptor (VEGFR2) such as ramucirumab or the use of VEGF-trap as in the case of aflibercept which acts as a decoy receptor for VEGF. Alternatively, sunitinib and pazopanib are examples of small molecule inhibitors of VEGF receptor tyrosine kinases (TKIs).
VEGF inhibitors have been associated with a variety of cardiovascular complications such as hypertension, thromboembolic events, cardiac arrhythmia, and cardiomyopathy, to name a few. Hypertension, in particular, is very common and ranges from 20% with bevacizumab to upward of 50% with some of the newer agents such as lenvatinib. This association is likely multifactorial. Inhibition of the VEGF pathway may result in an imbalance between vasodilators and vasoconstrictors and loss of capillary circulation [47]. Interestingly, the development of hypertension was associated with improved outcomes in some reports [48]. Active monitoring and management with standard antihypertensive therapy are recommended specially during the first few weeks of therapy.
LV dysfunction has been reported with several of these agents. For instance, in trials of sunitinib , a VEFG TKI commonly used in the treatment of metastatic renal cancer and gastrointestinal stromal tumors was associated with a decrease in LV function and overt heart failure in 10–3%, respectively [49]. Retrospective analyses suggest an even higher incidence of cardiovascular complications. Similar to trastuzumab , functional recovery of myocardial function is frequently (albeit not invariably) seen after their interruption suggesting a type II injury.
Arterial thromboembolic events such as stroke and myocardial infarction have also been linked to some of these agents such as bevacizumab (twofold increase in risk), whereas the association with venous thromboembolism has also been suggested but is less clear.
Small Molecule Tyrosine Kinase Inhibitors
TKIs block the function of tyrosine kinases which are enzymes responsible for the activation of several proteins integral in the signal transduction pathways responsible for cell growth, proliferation, and differentiation. These drugs have emerged as a major component in the treatment of several cancers, and their use has increased exponentially in the past few years. Unlike traditional chemotherapy, these agents are administered orally and often used for prolonged periods of time ranging from months to even years as in the case of imatinib and other ABL1 kinase inhibitors used in the treatment of chronic myeloid leukemia (CML) . These factors further emphasize the potential for being “overlooked” as a potential cause for cardiac diseases and underscores the importance of familiarity with their side effect profiles not only for oncologists but also for primary care physicians and cardiologists.
The range of cardiac complications seen with these small molecule inhibitors is wide; however, individual drugs have unique side effect profiles. For example, vandetanib , a multi-kinase inhibitor used to treat patients with medullary thyroid cancer, is known to cause prolongation of QTc in 16% of patients [50]. Torsades de pointes and sudden death have also been reported leading the Food and Drug Administration (FDA) to issue a US box warning. It should be avoided in patients using other drugs known to cause QT prolongation and in patients with electrolyte abnormalities.
A detailed discussion of these agents and their cardiac manifestations is beyond the scope of this chapter.
Cardio-oncology
As more cancer therapies become available, a growing number of cancer survivors face many challenges including the consequences of cancer treatment. The field of cardio-oncology addresses the cardiovascular issues arising from cancer therapy. It has evolved over the last decade in response to a massive expansion of novel therapies in cancer, many of which carry significant cardiac morbidity. In addition, the interplay between cancer and the cardiovascular system extends beyond toxicology as cancer by itself is associated with cardiovascular and metabolic complications [47]. Finally, cancer and the cardiovascular system seem to share common pathways which are not fully understood; therefore, cardio-oncology can serve as a novel platform for clinical and translational research to help cardiovascular drug discovery [51] and provides an excellent opportunity for collaboration between oncologists and cardiologists both in the care of patients and in clinical trial design.
Summary
In summary, advances in early detection and treatment strategies have prolonged the natural history of many cancers and contributed to an increasing prevalence of cancer survivors. Some of these patients are now faced with the sequelae of early and late treatment-related toxicities, many of which involve the cardiovascular system. Cardiotoxic chemotherapy, molecular targeted therapy, and radiation are increasingly incorporated into current treatment paradigms, but each agent is associated with a spectrum of cardiac side effects. As members of the cancer team, a basic awareness of the mechanisms, risk factors, management, and prognosis of these various treatment-associated cardiac toxicities is important for addressing the specific needs and optimizing care for present and future cancer survivors.
References
Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342(15):1077–84.
Cardinale D, Colombo A, Bacchiani G, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131(22):1981–8.
Groarke JD, Nohria A. Anthracycline cardiotoxicity: a new paradigm for an old classic. Circulation. 2015;131(22):1946–9.
Volkova M, Russell R 3rd. Anthracycline cardiotoxicity: prevalence, pathogenesis and treatment. Curr Cardiol Rev. 2011;7(4):214–20.
Elliott P. Pathogenesis of cardiotoxicity induced by anthracyclines. Semin Oncol. 2006;33(3 Suppl 8):S2–7.
Lyu YL, Kerrigan JE, Lin CP, et al. Topoisomerase II beta mediated DNA double-strand breaks: implications in doxorubicin cardiotoxicity and prevention by dexrazoxane. Cancer Res. 2007;67(18):8839–46.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79.
Hershman DL, McBride RB, Eisenberger A, et al. Doxorubicin, cardiac risk factors, and cardiac toxicity in elderly patients with diffuse B-cell non-Hodgkin's lymphoma. J Clin Oncol. 2008;26(19):3159–65.
Shapiro CL, Hardenbergh PH, Gelman R, et al. Cardiac effects of adjuvant doxorubicin and radiation therapy in breast cancer patients. J Clin Oncol. 1998;16(11):3493–501.
Bria E, Giannarelli D, Felici A, et al. Taxanes with anthracyclines as first-line chemotherapy for metastatic breast carcinoma. Cancer. 2005;103(4):672–9.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Wang X, Liu W, Sun CL, et al. Hyaluronan synthase 3 variant and anthracycline-related cardiomyopathy: a report from the children's oncology group. J Clin Oncol. 2014;32(7):647–53.
Nakamae H, Tsumura K, Terada Y, et al. Notable effects of angiotensin II receptor blocker, valsartan, on acute cardiotoxic changes after standard chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone. Cancer. 2005;104(11):2492–8.
van Dalen EC, van der Pal HJ, Caron HN, et al. Different dosage schedules for reducing cardiotoxicity in cancer patients receiving anthracycline chemotherapy. Cochrane Database Syst Rev. 2006;4:CD005008.
Gabizon AA, Lyass O, Berry GJ, et al. Cardiac safety of pegylated liposomal doxorubicin (Doxil/Caelyx) demonstrated by endomyocardial biopsy in patients with advanced malignancies. Cancer Investig. 2004;22(5):663–9.
Seifert CF, Nesser ME, Thompson DF. Dexrazoxane in the prevention of doxorubicin-induced cardiotoxicity. Ann Pharmacother. 1994;28(9):1063–72.
Smith LA, Cornelius VR, Plummer CJ, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer. 2010;10:337.
van Dalen EC, Caron HN, Dickinson HO, et al. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev. 2005;1:CD003917.
Swain SM, Whaley FS, Gerber MC, et al. Cardioprotection with dexrazoxane for doxorubicin-containing therapy in advanced breast cancer. J Clin Oncol. 1997;15(4):1318–32.
Gulati G, Heck SL, Ree AH, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016;37(21):1671–80.
Bosch X, Rovira M, Sitges M, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of malignant hEmopathies). J Am Coll Cardiol. 2013;61(23):2355–62.
Kalay N, Basar E, Ozdogru I, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006;48(11):2258–62.
Jiji RS, Kramer CM, Salerno M. Non-invasive imaging and monitoring cardiotoxicity of cancer therapeutic drugs. J Nucl Cardiol. 2012;19(2):377–88.
Kuittinen T, Husso-Saastamoinen M, Sipola P, et al. Very acute cardiac toxicity during BEAC chemotherapy in non-Hodgkin's lymphoma patients undergoing autologous stem cell transplantation. Bone Marrow Transplant. 2005;36(12):1077–82.
Cooper LT, Baughman KL, Feldman AM, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation. 2007;116(19):2216–33.
Jensen BV, Skovsgaard T, Nielsen SL. Functional monitoring of anthracycline cardiotoxicity: a prospective, blinded, long-term observational study of outcome in 120 patients. Ann Oncol. 2002;13(5):699–709.
Ewer MS, Vooletich MT, Durand JB, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol. 2005;23(31):7820–6.
Crone SA, Zhao YY, Fan L, et al. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat Med. 2002;8(5):459–65.
Perik PJ, de Vries EG, Gietema JA, et al. Serum HER2 levels are increased in patients with chronic heart failure. Eur J Heart Fail. 2007;9(2):173–7.
Seidman A, Hudis C, Pierri MK, et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol. 2002;20(5):1215–21.
Ewer MS, Lippman SM. Type II chemotherapy-related cardiac dysfunction: time to recognize a new entity. J Clin Oncol. 2005;23(13):2900–2.
Joensuu H, Kellokumpu-Lehtinen PL, Bono P, et al. Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med. 2006;354(8):809–20.
Pivot X, Romieu G, Debled M, et al. 6 months versus 12 months of adjuvant trastuzumab for patients with HER2-positive early breast cancer (PHARE): a randomised phase 3 trial. Lancet Oncol. 2013;14(8):741–8.
Robert NJ, Eiermann W, Pienkowski T, et al. BCIRG 006: Docetaxel and trastuzumab-based regimens improve DFS and OS over AC-T in node positive and high risk node negative HER2 positive early breast cancer patients: quality of life (QOL) at 36 months follow-up. J Clin Oncol. 2007;25(90180):19647.
Plana JC, Galderisi M, Barac A, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27(9):911–39.
Tan-Chiu E, Yothers G, Romond E, et al. Assessment of cardiac dysfunction in a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel, with or without trastuzumab as adjuvant therapy in node-positive, human epidermal growth factor receptor 2-overexpressing breast cancer: NSABP B-31. J Clin Oncol. 2005;23(31):7811–9.
Mackey JR, Clemons M, Cote MA, et al. Cardiac management during adjuvant trastuzumab therapy: recommendations of the Canadian Trastuzumab working group. Curr Oncol. 2008;15(1):24–35.
Guarneri V, Lenihan DJ, Valero V, et al. Long-term cardiac tolerability of trastuzumab in metastatic breast cancer: the M.D. Anderson Cancer Center experience. J Clin Oncol. 2006;24(25):4107–15.
Perez EA, Koehler M, Byrne J, et al. Cardiac safety of lapatinib: pooled analysis of 3689 patients enrolled in clinical trials. Mayo Clin Proc. 2008;83(6):679–86.
Verma S, Miles D, Gianni L, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–91.
Aleman BM, van den Belt-Dusebout AW, De Bruin ML, et al. Late cardiotoxicity after treatment for Hodgkin lymphoma. Blood. 2007;109(5):1878–86.
Hardenbergh PH, Munley MT, Bentel GC, et al. Cardiac perfusion changes in patients treated for breast cancer with radiation therapy and doxorubicin: preliminary results. Int J Radiat Oncol Biol Phys. 2001;49(4):1023–8.
Hooning MJ, Botma A, Aleman BM, et al. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst. 2007;99(5):365–75.
Akhtar SS, Salim KP, Bano ZA. Symptomatic cardiotoxicity with high-dose 5-fluorouracil infusion: a prospective study. Oncology. 1993;50(6):441–4.
Ng M, Cunningham D, Norman AR. The frequency and pattern of cardiotoxicity observed with capecitabine used in conjunction with oxaliplatin in patients treated for advanced colorectal cancer (CRC). Eur J Cancer. 2005;41(11):1542–6.
Malhotra V, Dorr VJ, Lyss AP, et al. Neoadjuvant and adjuvant chemotherapy with doxorubicin and docetaxel in locally advanced breast cancer. Clin Breast Cancer. 2004;5(5):377–84.
Moslehi JJ. Cardiovascular toxic effects of targeted cancer therapies. N Engl J Med. 2016;375(15):1457–67.
Dahlberg SE, Sandler AB, Brahmer JR, et al. Clinical course of advanced non-small-cell lung cancer patients experiencing hypertension during treatment with bevacizumab in combination with carboplatin and paclitaxel on ECOG 4599. J Clin Oncol. 2010;28(6):949–54.
Khakoo AY, Kassiotis CM, Tannir N, et al. Heart failure associated with sunitinib malate: a multitargeted receptor tyrosine kinase inhibitor. Cancer. 2008;112(11):2500–8.
Zang J, Wu S, Tang L, et al. Incidence and risk of QTc interval prolongation among cancer patients treated with vandetanib: a systematic review and meta-analysis. PLoS One. 2012;7(2):e30353.
Bellinger AM, Arteaga CL, Force T, et al. Cardio-oncology: how new targeted cancer therapies and precision medicine can inform cardiovascular discovery. Circulation. 2015;132(23):2248–58.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Samawi, H.H., Cheung, W.Y. (2018). Victims of Our Own Success: Cardiac Toxicities from Conventional and Emerging Cancer Therapies. In: Olver, I. (eds) The MASCC Textbook of Cancer Supportive Care and Survivorship. Springer, Cham. https://doi.org/10.1007/978-3-319-90990-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-90990-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-90989-9
Online ISBN: 978-3-319-90990-5
eBook Packages: MedicineMedicine (R0)