Abstract
The aim of present investigation is to explore the molecular mechanisms of vasculogenic mimicry (VM) induced by hypoxia. Hepatocellular carcinoma cell lines were treated with CoCl2, and the VM-related parameters were assayed by real-time qPCR, Western blotting and immunofluorescence. Matrigel tube structure was also detected. We demonstrated that the expression of pMEK, MEK, pERK1/2 and ERK1/2 had a positive correlation with VM induced by hypoxia in MHCC97H while HepG2 signified VM under normoxia condition. PD98059 was negatively while epidermal growth factor positively participated in the increased tubes and area of VM. At the meaning time, the increased VM-related genes VE-cadherin, MMP2, MMP9, EphA2 and LAMC2 in hypoxia group were down-regulated by PD98059 in a dose-dependent manner. Furthermore, we elucidated that PKA, but not PKC, mediated the MEK/ERK pathway in a negative manner in VM. In conclusion, MEK/ERK pathway is positively involved in VM in hepatocellular carcinoma cell line, which was mediated by PKA negatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Blood flow dynamics are essential for the growth, metastasis and invasion of malignant tumors and can be an important indicator in deciding on a treatment strategy [1, 2]. Vasculogenic mimicry (VM) is a newly discovered blood supply system for malignant tumors, which is independent of blood vessel endothelium [3, 4]. VM is a pipe-like functional microcirculation structure mainly established by malignant tumor cells. VM reflects the plasticity of aggressive tumor cells in many malignancies including hepatocellular carcinoma (HCC), one of the most common causes of cancer mortality worldwide [5, 6].
Through surgical resection for HCC is the best treatment strategy for cancer patients in clinical, the 5-year survival rate is relatively low and mainly resulted from tumor metastasis. So the pathogenesis and metastasis mechanisms of HCC must cause serious attention. The overall poor prognosis in HCC has a close relationship with vascular enrichment in liver, and the presence of VM explains the poor effect of antitumor drugs designed only on the target of endothelium-dependent vascular formation partly [7, 8].
Abnormal cellular signal transduction is one of the most important reasons for carcinogenesis and angiogenesis [9, 10]. Emerging date demonstrated that mitogen-activated protein kinase (MAPK) pathway was involved in the pathogenesis of some malignant tumors. Mitogen extracellular kinase (MEK), key member of MAPK signaling pathway, participates in the proliferation and differentiation in malignant tumors by regulating transcription factor in nucleus. ERK1/2, a dual phosphorylation on serine and tyrosine in ERK signaling pathway, mediating by MEK, usually regulates the transcription factors directly, such as c-fos, c-Jun, STATs, c-myc and so on.
Hypoxia is a common pathological process and generally involved in malignant tumor progression by activating hypoxia-inducible factor-1α (HIF-1α) [11, 12]. As an activator of angiogenesis, hypoxia increases the gene expression of multiple drug resistance (MDR) and inhibits tumor suppressor genes p53 and Bax, therefore resulting in an invalid effect of chemotherapy drugs on cancer cells. HIF-1α is an internal indicator of tissue hypoxia and exerts an essential function in the process of adaptation to hypoxia in tumor cells. Emerging data have showed that hypoxia-induced VM occurred in glioma, ovarian carcinoma melanoma while few reports in HCC [13–15]. In present study, we hypothesized that MEK/ERK pathway was involved in the hypoxia-induced HCC cell VM formation, which is mediated by protein kinase A.
Materials and methods
Chemical reagents and antibodies
Matrigel (BD Biosciences), fetal bovine serum (Gibco), cell culture media (DMEM and MEM), PD980509 (a specific MEK/ERK pathway inhibitor), FSK (a specific PKA activator), H89 (a specific PKA inhibitor), H7 (a specific PKC inhibitor), PMA (a specific PKC activator) and EGF (a specific MEK/ERK pathway activator) (Sigma-Aldrich), 4′,6-diamidino-2-phenylindole (DAPI) (Sigma-Aldrich), primer synthesis (Invitrogen), monoclonal rabbit anti-ERK1/2, pERK1/2, VE-cadherin (Cell Signaling), monoclonal mice anti-MEK, pMEK, HIF-1α, β-actin and secondary antibodies (Santa Cruz), Sodium dodecyl sulfide, bis-acrylamide, ammonium persulfate, N,N,N′,N′-tetramethylethylenediamine and nitrocellulose membrane (Sigma-Aldrich), 3-(5′-hydroxumethyl-2′-furyl)-1-benzylindazole (YC-1) (Amresco), CoCl2 (Sigma-Aldrich).
Cell culture
HepG2 and MHCC97H cell lines were purchased from the Cell Bank of the Chinese Academy of Sciences. HepG2 cell line was cultured in MEM while MHCC97H cell line in DMEM with 10 % FBS antibiotics (100 U/mL of penicillin and 100 mg/mL of streptomycin), respectively. All the cultures were incubated in a humidified atmosphere at 37 °C and 5 % CO2.
Hypoxia medication
Cell culture plates were incubated at 37 °C and 5 % CO2, and hypoxia conditions were duplicated by adding CoCl2 to a final concentration of 100 μmol/L (with the dissolution of DMSO) for 24 h. Control group (normoxia) cells received same dose of DMSO. The inhibition or activation effect of drugs were studied by adding culture media containing corresponding drugs into the wells after cell seeding to a certain concentration for 24 h.
Matrigel tube structure formation assay
The Matrigel tube structure formation detection is adopted for the determination of VM formation capacity of cancer cells in vitro. The plate well was coated with 100 μL (10 mg/mL) Matrigel and then incubated at 37 °C for 60 min. About 200 μL MHCC97H or HepG2 cells (at a concentration of 2 × 104/100 μL) was seeded into the prepared wells and incubated in a humidified atmosphere at 37 °C and 5 % CO2. The effect of the inhibitor or activator on the tube structure formation was studied by adding culture medium containing drugs into the cells to a final concentration of 2, 20 or 100 μM (PD98059) and 2, 20 or 100 mg/L (EGF).
cDNA generation and real-time quantitative PCR (qPCR)
Total RNA and cDNA were generated from cells using TRIzol reagent (Invitrogen) according to the manufacturer’s instructions. The mRNA expression of MMP2, MMP9, VE-cadherin, EphA2 and LAMC2 were examined by quantitative real-time PCR (ABI 7700). The primer sequences used for real-time qPCR were as follows: VE-cadherin forward: 5′-GATTTGTGTGCCTGAAGAC-3′, reverse: 5′-ATGGTGAAAGCGCCTGGTA-3′; MMP9 forward: 5′-CGACATAGACGGCATCCAG-3′, reverse: 5′-CTGTCGGCTGTGGTTCAGT-3′; EphA2 forward: 5′-CCCGGAGGACGTTTACTTCT-3′, reverse: 5′-GGATGGATGATTCGGTAG-3′; LAMC2 forward: 5′-AATTCCTGCCTAGACAC-3′, reverse: 5′-TCCCTGTCAGTTGCCTCCAT-3′; GAPDH forward: 5′-GGGAAATCGTGCGTGACAT-3′, reverse 5′-CAGGAGGAGCAATGATCTT-3′
Western blotting
Cell samples were prepared for Western blotting analysis. Equal amount of protein in each group was subjected to 10 % SDS-PAGE and then transferred to a NC membrane. The membrane was blocked by 5 % nonfat milk. Then, the blocked membrane was incubated with primary antibody in 4 °C overnight. After washing three times with PBS, the membrane was incubated with horseradish peroxide (HRP)-conjugated secondary antibody. The signal strength was calculated by normalizing the strength of β-actin abundance.
Cell apoptosis and viability assessment
DAPI staining was adopted to assess morphological changes in chromatin structure in MHCC cells undergoing apoptosis. MHCC cells were digested with trypsin gently, mounted on bacteria-free glass slides. Then, the cells were fixed in paraformaldehyde (4 % in volume) for 0.5 h and stained with 1 μg/mL DAPI for 30 min. Apoptosis was characterized by chromatin condensation and fragmentation, which were visualized under a fluorescence microscopy. The length and area of VM of HMCC97H cell lines were assayed by Image-Pro Plus software (Media Cybernetics).
Gelatin zymography
The cells were centrifuged at 4 °C, 2,000 rpm for 10 min. Equal amount of protein in each group was quantified by BCA. Gelatin zymography was conducted as previously reported [16].
Immunofluorescence
Cells were fixed with cold acetone (−20 °C) for 10 min and dried in a clean bench for 30 min. Cellular membrane permeability was increased by incubating with 1 % Triton-100 for 60 min. Then, cells were sealed with bovine serum albumin (BSA, 2 %) and then incubated overnight with the first antibody. After washing with PBS, cells were incubated with FITC-conjugated secondary antibody. Finally, cells were photographed under a fluorescence microscopy (IX83, Olympus).
Statistical analysis
Data were expressed as the mean ± SD, and statistical difference was evaluated by one-way ANOVA. Differences were considered significant at P values <0.05.
Results
Abnormal MEK and ERK1/2 were related with hypoxia-induced VM formation
The involvement of ERK pathway in hypoxia-induced VM formation was examined in two hepatoma carcinoma cell lines: HMCC97H and HepG2. Both MHCC97H and HepG2 had the capacity of VM formation in vitro, but only MHCC97H showed a significant difference between control (normoxia) and hypoxia medication for 24 h while HepG2 showed VM formation in either condition (Fig. 1a).
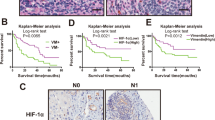
Abnormal MEK and ERK1/2 proteins were related with hypoxia-induced VM formation capacity. a MHCC97H cell line revealed VM formation induced by hypoxia medication while HepG2 cell line showed VM formation in both normoxia and hypoxia conditions. b, c The up-regulated VE-cadherin and HIF-1α expression in hypoxia group was normalized by YC-1 in MHCC97H cell lines. d, e The expression of ERK pathway key regulators pMEK, MEK, pERK1/2 and ERK1/2 was consistent with VE-cadherin in MHCC97H cell lines. Data are presented as mean ± SD. *P < 0.05; **P < 0.01 versus control, # P < 0.05; ## P < 0.01 versus hypoxia. Scale bars presented 500 μm
It was found that HIF-1α was up-regulated greatly in hypoxia group in both MHCC97H and HepG2 cell lines, but VM-associated marker VE-cadherin expression signified no statistical differences in hypoxia group when compared with control in HepG2 cell lines (Fig. 1b, c). The result also demonstrated that the expression of ERK pathway key parameters ERK1/2, pERK1/2, MEK and pMEK were increased dramatically in hypoxia group, which is consistent with the change of VE-cadherin. And these abnormalities were alleviated by YC-1, a specific HIF-1α compound (Fig. 1d, e).
MEK/ERK agonist promotes while inhibitor inhibits VM formation
PD98059 and EGF were used as inhibitor or agonist of MEK/ERK pathway to determine the participation of it in VM formation in vitro. In was found that the number of VM was increased under hypoxia condition and PD98059 inhibited the number in a dose-dependent manner (Fig. 1a). The increased length and area of VM in hypoxia group were decreased by PD98059 interventions greatly while EGF increased the parameters significantly (P < 0.01, Table 1). The results also showed that the enhanced expression of VM formation associated marker VE-cadherin and tube structure number in hypoxia group was alleviated by PD98059 dramatically (Fig. 2b, c). Consistent with the previous results, these abnormalities were enhanced by EGF medication in a dose-dependent manner (Fig. 2b, c).
Effect of MEK/ERK pathway agonist and inhibitor on VM formation. a Interrupted tube numbers induced by hypoxia and drug interventions. b, c Increased expression of VE-cadherin induced by hypoxia and drug restorations. Data are presented as mean ± SD. *P < 0.05; **P < 0.01 versus control; # P < 0.05, ## P < 0.01 versus hypoxia
ERK1/2 was consistent with VE-cadherin in different hypoxia exposure times
The consistency of ERK1/2 and VE-cadherin was tested by Western blotting in different times of hypoxia medication (0, 12, 24 and 48 h). The expression of pERK1/2 and ERK1/2 was consisted of the VM formation marker VE-cadherin in hypoxia-induced MHCC97H cells as shown in Fig. 3, further demonstrating the participation of MEK/ERK signaling pathway in hypoxia-induced VM formation in MHCC97H cells.
ERK1/2 expressions were consistent with VE-cadherin in different hypoxia times. a Western blotting showed that ERK1/2, pERK1/2 and VE-cadherin were consistent in different hypoxia times. b Quantification of MEK/ERK pathway signaling parameters. Data are presented as mean ± SD. *P < 0.05, **P < 0.01 versus control; # P < 0.05, ## P < 0.01 versus hypoxia
PD98059 resulted in a robust alteration in gene expression profiles related to VM
To further present the VM formation mechanism, real-time qPCR was conducted to test VM-related profiles after hypoxia incubation and PD98059 intervention. Hypoxia incubation resulted in increased mRNA of VM-associated genes VE-cadherin, MMP2, MMP9, EphA2 and LAMC2 in HMCC97H while PD95059 inhibited these abnormal mRNA dramatically in a dose-dependent manner (Fig. 4a). We also found that PD98059 alleviated the activity of MMP2 and MMP9, which was enhanced by hypoxia through gelatin zymography test (Fig. 4b, c). The expression of VE-cadherin, EphA2 and LAMC2 was enhanced in immunofluorescence assay, and PD98059 attenuated the intensity in a dose-dependent manner (Fig. 4d), which is consistent with qPCR result. Taken together, these results demonstrated that PD98059 had the potential to affect MHCC97H cell VM formation, manifesting the involvement of MEK/ERK pathway in the formation of VM.
PD98059 results in a robust alteration in gene expression profiles related to hypoxia-induced VM. a Hypoxia-induced abnormal mRNA expression of VM-related genes and alleviations by PD98059. b, c The enhanced activity of MMP2 and MMP9 induced by hypoxia and attenuations by PD98059 was analyzed by gelatin zymography. d Immunofluorescence assay of VE-cadherin, EphA2 and LAMC. Data are presented as mean ± SD. *P < 0.05, **P < 0.01 versus control; # P < 0.05, ## P < 0.01 versus hypoxia. Scale bars presented 50 μm
PD98059 and EGF medication alone did not result in apoptosis or viability
DAPI staining and tubes structure number counting were performed to assess apoptosis and viability of MHCC97H cell line. Results showed that no apoptosis or viability (no statistical differences) was occurred after PD98059 or EGF medication, indicating that activation or inhibition of MHCC97H cell did not result in apoptosis or viability (Fig. 5).
MEK/ERK signaling pathway was mediated by PKA but not PKC
It was found that PKA agonist FSK decreased the content of VE-cadherin, pERK1/2 and ERK1/2 while H89, the inhibitor of PKA, increased the expression of those proteins in a dose-dependent manner, strongly demonstrating the negative regulations of PKA in the hypoxia-induced VM formation (Fig. 6a, b). However, the activation or blockade of PKC by H7 or PMA showed no obvious effects on VE-cadherin, p-ERK1/2 or ERK1/2 expression (Fig. 6c, d). PKA but not PKC plays a negative regulation on hypoxia-induced VM formation.
MEK/ERK signaling pathway was mediated by PKA. a, b Expression analysis of VE-cadherin, pERK1/2 and ERK1/2 induced by hypoxia and interventions of PKA inhibitor or agonist. c, d Expression analysis of VE-cadherin, pERK1/2 and ERK1/2 induced by hypoxia and interventions of PKC inhibitor or agonist. Data are presented as mean ± SD. *P < 0.05, **P < 0.01 versus control; # P < 0.05, ## P < 0.01 versus hypoxia
Discussion
VM reflects the plasticity of aggressive tumor cells and has become a prognostic factor for poor clinical outcomes [17, 18]. In present study, we demonstrated that the expression of MEK and ERK1/2 was consisted of the VM formation in MHCC97H cell lines induced by hypoxia medication in vitro. In addition, PKA, but not PKC, played a critical role in the MEK/ERK pathway-mediated VM formation in MHCC97H. Moreover, the expression level of MEK/ERK was in line with the expression intensity of VM-related parameters, confirming the participation of MEK/ERK pathway in hypoxia-induced VM formation.
The rapid growth of malignant tumor tissue requires adequate oxygen supply. HIF-1α, a transcription factor induced by hypoxia medication, exhibited over-expression in various kinds of malignant tumors and had a close relationship with the proliferation, differentiation, apoptosis and metastasis of cancer cell. In this research, we found that HIF-1α was activated after CoCl2 medication in MHCC97H cell line, which was consistently matched with the findings of VM structure number and activated MEK/ERK signaling pathway. The previous studies also showed that hypoxia promoted VM formation in ovarian carcinoma and melanoma [13, 15]. Emerging data also demonstrated that Rac1 mediated hypoxia-induced HIF-1α expression in MCF-7 breast cancer cells, which was regulated by ERK signaling pathway [19]. ERKs also played a pivotal role in the hypoxia medication induced death resistance and invasiveness in glioblastoma cells [20]. Though few reports on the relationship between VE-cadherin and ERK signaling pathway in malignant tumors, VE-cadherin, the VM-associated marker was markedly decreased in hypoxia/oxygenation process and was partly mediated by ERK pathway in heart [21]. Based on the results of the present study, it is reasonable to conclude that the activated MEK and ERK1/2 promotes the expression of VE-cadherin and therefore result in the VM formation.
The key physiological character of VM formation is featured as VE-cadherin co-localization and up-regulation of EphA2, MMPs and LAMC2. The activation of EphA2 induces the increase of MMP14, which subsequently leads to MMP2 activation [22]. Besides mediating extracellular matrix degradation and recombination, MMPs promote LAMC2 cleave to γ2′ and γ2 × fragments [22, 23], which are involved in migration and invasion of tumors and ultimately lead to VM formation. In this part, it was found that hypoxia medication enhanced the expression of EphA2, LAMC2, MMP2 and MMP9 level, indicating the VM formation induced by hypoxia was involved in extracellular matrix degradation and recombination process in MHCC97H cell line, consistent with previous reports [24, 25]. In the meantime, MEK/ERK pathway inhibitor PD98059 normalized the aberrant content of VM-related parameters in a dose-dependent manner, providing further evidence that VM formation was regulated by MEK/ERK pathway. Meanwhile, previous study proved that ephrinA/EphA proteins facilitated myogenesis by inhibiting Ras-ERK1/2 cascade [26]. A recent study revealed that EphA2 receptor over-expressed in glioblastoma multiforme and showed contributions to cell transformation, tumor initiation, progression and maintenance while down-regulation exerted anti-tumor effects [27]. Lema et al. [27] also showed that alanine substitution led to down-regulated EphA2 expression, which was in agreement with suppressed pERK content, signifying similar regulatory network in this article. The increased migration and invasion of malignant tumors are key events in the development of metastasis, in which process ERK pathway-regulated MMPs played a crucial role [28–30]. Tubular structure network formation is closely linked to MMP over-expressions [31], and curcumin exerted VM inhibition function by down-regulating EphA2/PI3K/MMP pathway in a melanoma model [24]. It was also reported that MMP2 was related with VM formation and expression of laminin5 gamma2 chain in melanoma tumor [25]. However, a research focused on TGF-beta exerting cell proliferation, differentiation and invasion effect in advanced carcinomas (MCF10A human breast epithelial cells) came up with an idea that p38MAPK but not ERK signaling was involved MMP2 and MMP9 process [32]. Our findings in present study showed that MMP2/9, EphA2, LAMC2 and VM-associated marker VE-cadherin regulated hypoxia-induced VM formation by activating MEK/ERK pathway.
Recent findings offered the insights that PKA-enhanced GTP-Rac-mediated MEK/ERK signaling transduction in nuclear [33] and PKC inhibitors caused cancer cell apoptosis, which was also correlated with the ability of sustained ERK activation [34]. PKC–MEK–ERK signaling pathway was also activated in the enhanced cell invasion and metastasis in mouse melanoma [35]. But in more cases, ERK pathway had a cross talk with both PKA and PKC [36–38]. Strikingly, we found that only PKA was involved in hypoxia-related MEK/ERK activation and VM formation induced by hypoxia in this part while PKC showed no obvious effect in this process. Our results are consistent with the finding that PKA inhibited melanoma cell VM formation by inactivating ERK [39]. So it can be concluded that PKA induced the activated MEK/ERK signal transduction mediates VM formation of MHCC97H cell line induced by hypoxia medication.
In brief, our results signifying that enhanced MEK/ERK signaling transduction is involved in hypoxia-induced VM formation in HCC cell line MHCC97H, which was mediated by PKA negatively.
Abbreviations
- DAPI:
-
4′,6-Diamidino-2-phenylindole
- EGF:
-
Epidermal growth factor
- EphA2:
-
Ephrin A receptor 2
- ERK:
-
Extracellular regulated kinase
- HCC:
-
Hepatocellular carcinoma
- HIF-1α:
-
Hypoxia-inducible factor-1α
- LAMC2:
-
Laminin subunit gamma-2
- MAPK:
-
Mitogen-activated protein kinase
- MDR:
-
Multiple drug resistance
- MEK:
-
Mitogen extracellular kinase
- MMP:
-
Matrix metalloproteinase
- PBS:
-
Phosphate-buffered saline
- PKA/C:
-
Proteinase A/C
- VM:
-
Vasculogenic mimicry
References
Barinaga M. A face-off over tumor blood supply. Science. 2000;287(783):785.
Kudo M, Tochio H. Intranodular blood supply correlates well with biological malignancy grade determined by tumor growth rate in pathologically proven hepatocellular carcinoma. Oncology. 2008;75(Suppl 1):55–64.
Francescone R, Scully S, Bentley B, et al. Glioblastoma-derived tumor cells induce vasculogenic mimicry through flk-1 protein activation. J Biol Chem. 2012;287:24821–31.
Vartanian AA. Signaling pathways in tumor vasculogenic mimicry. Biochemistry. 2012;77:1044–55.
Sun T, Sun BC, Zhao XL, et al. Promotion of tumor cell metastasis and vasculogenic mimicry by way of transcription coactivation by Bcl-2 and Twist1: a study of hepatocellular carcinoma. Hepatology. 2011;54:1690–706.
Sun T, Zhao N, Zhao XL, et al. Expression and functional significance of Twist1 in hepatocellular carcinoma: its role in vasculogenic mimicry. Hepatology. 2010;51:545–56.
Li Y, Cai W, Yi Q, et al. Lipid droplets may lay a spacial foundation for vasculogenic mimicry formation in hepatocellular carcinoma. Med Hypotheses. 2014;83:56–9.
Liu WB, Xu GL, Jia WD, et al. Prognostic significance and mechanisms of patterned matrix vasculogenic mimicry in hepatocellular carcinoma. Med Oncol. 2011;28(Suppl 1):S228–38.
Wang LJ, Zhao Y, Han B, et al. Targeting slit-roundabout signaling inhibits tumor angiogenesis in chemical-induced squamous cell carcinogenesis. Cancer Sci. 2008;99:510–7.
Wen ZH, Su YC, Lai PL, et al. Critical role of arachidonic acid-activated mtor signaling in breast carcinogenesis and angiogenesis. Oncogene. 2013;32:160–70.
Ammirante M, Shalapour S, Kang Y, et al. Tissue injury and hypoxia promote malignant progression of prostate cancer by inducing CXCL13 expression in tumor myofibroblasts. Proc Natl Acad Sci USA. 2014;111:14776–81.
Yoo YG, Christensen J, Gu J, et al. HIF-1α mediates tumor hypoxia to confer a perpetual mesenchymal phenotype for malignant progression. Sci Signal. 2011;4:pt4.
Du J, Sun B, Zhao X, et al. Hypoxia promotes vasculogenic mimicry formation by inducing epithelial-mesenchymal transition in ovarian carcinoma. Gynecol Oncol. 2014;133:575–83.
Huang M, Ke Y, Sun X, et al. Mammalian target of rapamycin signaling is involved in the vasculogenic mimicry of glioma via hypoxia-inducible factor-1α. Oncol Rep. 2014;32:1973–80.
Sun B, Zhang D, Zhang S, et al. Hypoxia influences vasculogenic mimicry channel formation and tumor invasion-related protein expression in melanoma. Cancer Lett. 2007;249:188–97.
Toth M, Sohail A, Fridman R. Assessment of gelatinases (MMP-2 and MMP-9) by gelatin zymography. Methods Mol Biol. 2012;878:121–35.
Lin P, Wang W, Sun BC, et al. Vasculogenic mimicry is a key prognostic factor for laryngeal squamous cell carcinoma: a new pattern of blood supply. Chin Med J (Engl). 2012;125:3445–9.
Wang SY, Ke YQ, Lu GH, et al. Vasculogenic mimicry is a prognostic factor for postoperative survival in patients with glioblastoma. J Neurooncol. 2013;112:339–45.
Du J, Xu R, Hu Z, et al. PI3K and ERK-induced Rac1 activation mediates hypoxia-induced HIF-1α expression in MCF-7 breast cancer cells. PLoS One. 2011;6:e25213.
Kim JY, Kim YJ, Lee S, et al. The critical role of erk in death resistance and invasiveness of hypoxia-selected glioblastoma cells. BMC Cancer. 2009;9:27.
Lee SW, Won JY, Lee HY, et al. Angiopoietin-1 protects heart against ischemia/reperfusion injury through VE-cadherin dephosphorylation and myocardiac integrin-β1/ERK/caspase-9 phosphorylation cascade. Mol Med. 2011;17:1095–106.
Zhang JG, Li XY, Wang YZ, et al. Rock is involved in vasculogenic mimicry formation in hepatocellular carcinoma cell line. PLoS One. 2014;9:e107661.
Lu XS, Sun W, Ge CY, et al. Contribution of the PI3K/MMPS/Ln-5γ2 and EphA2/FAK/Paxillin signaling pathways to tumor growth and vasculogenic mimicry of gallbladder carcinomas. Int J Oncol. 2013;42:2103–15.
Chen LX, He YJ, Zhao SZ, et al. Inhibition of tumor growth and vasculogenic mimicry by curcumin through down-regulation of the EphA2/PI3K/MMP pathway in a murine choroidal melanoma model. Cancer Biol Ther. 2011;11:229–35.
Hess AR, Seftor EA, Seftor RE, et al. Phosphoinositide 3-kinase regulates membrane Type 1-matrix metalloproteinase (MMP) and MMP-2 activity during melanoma cell vasculogenic mimicry. Cancer Res. 2003;63:4757–62.
Minami M, Koyama T, Wakayama Y, et al. EphrinA/EphA signal facilitates insulin-like growth factor-I-induced myogenic differentiation through suppression of the Ras/extracellular signal-regulated kinase 1/2 cascade in myoblast cell lines. Mol Biol Cell. 2011;22:3508–19.
Lema Tome CM, Palma E, Ferluga S, et al. Structural and functional characterization of monomeric ephrina1 binding site to EphA2 receptor. J Biol Chem. 2012;287:14012–22.
Yu T, Wu Y, Helman JI, et al. CXCR4 promotes oral squamous cell carcinoma migration and invasion through inducing expression of MMP-9 and MMP-13 via the ERK signaling pathway. Mol Cancer Res. 2011;9:161–72.
Lakka SS, Jasti SL, Gondi C, et al. Downregulation of MMP-9 in ERK-mutated stable transfectants inhibits glioma invasion in vitro. Oncogene. 2002;21:5601–8.
Kim S, Choi JH, Lim HI, et al. EGF-induced MMP-9 expression is mediated by the JAK3/ERK pathway, but not by the JAK3/STAT-3 pathway in a SKBR3 breast cancer cell line. Cell Signal. 2009;21:892–8.
Karroum A, Mirshahi P, Faussat AM, et al. Tubular network formation by adriamycin-resistant MCF-7 breast cancer cells is closely linked to MMP-9 and VEGFR-2/VEGFR-3 over-expressions. Eur J Pharmacol. 2012;685:1–7.
Kim ES, Kim MS, Moon A. TGF-beta-induced upregulation of MMP-2 and MMP-9 depends on p38 MAPK, but not ERK signaling in MCF10A human breast epithelial cells. Int J Oncol. 2004;25:1375–82.
Bachmann VA, Riml A, Huber RG, et al. Reciprocal regulation of PKA and Rac signaling. Proc Natl Acad Sci USA. 2013;110:8531–6.
Pettersson F, Couture MC, Hanna N, et al. Enhanced retinoid-induced apoptosis of MDA-MB-231 breast cancer cells by PKC inhibitors involves activation of ERK. Oncogene. 2004;23:7053–66.
Matsuoka H, Tsubaki M, Yamazoe Y, et al. Tamoxifen inhibits tumor cell invasion and metastasis in mouse melanoma through suppression of PKC/MEK/ERK and PKC/PI3K/Akt pathways. Exp Cell Res. 2009;315:2022–32.
Hirota Y, Tsukazaki T, Yonekura A, et al. Activation of specific MEK–ERK cascade is necessary for TGFβ signaling and crosstalk with PKA and PKC pathways in cultured rat articular chondrocytes. Osteoarthr Cartil. 2000;8:241–7.
Zeni AL, Zomkowski AD, Maraschin M, et al. Involvement of PKA, CaMKII, PKC, MAPK/ERK and PI3K in the acute antidepressant-like effect of ferulic acid in the tail suspension test. Pharmacol Biochem Behav. 2012;103:181–6.
Hu HJ, Gereau RWT. ERK integrates PKA and PKC signaling in superficial dorsal horn neurons. II. Modulation of neuronal excitability. J Neurophysiol. 2003;90:1680–8.
Lissitzky JC, Parriaux D, Ristorcelli E, et al. Cyclic AMP signaling as a mediator of vasculogenic mimicry in aggressive human melanoma cells in vitro. Cancer Res. 2009;69:802–9.
Conflict of interest
The authors declare that they have no competing interests to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, B., Xiao, E. & Huang, M. MEK/ERK pathway is positively involved in hypoxia-induced vasculogenic mimicry formation in hepatocellular carcinoma which is regulated negatively by protein kinase A. Med Oncol 32, 408 (2015). https://doi.org/10.1007/s12032-014-0408-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0408-7