Abstract
To assess the evidence for improved outcomes in hepatocellular carcinoma (HCC) with transarterial chemoembolization (TACE) plus percutaneous ethanol injection (PEI). A systematic search of MEDLINE, EMBASE, the Cochrane library, Chinese biomedicine literature database, Chinese scientific full-text database, and Chinese journal full-text database was undertaken for relevant articles. The computer search was supplemented with a manual search of reference lists for all available review articles, primary studies, and books to identify other studies not found in the computer search. The initial search identified seven randomized trials that included 623 patients. Meta-analysis results are as follows: the 6-month, 1-, 2-, and 3-year survival rates were significantly better in patients with the TACE + PEI group than TACE group; in the decline rates of the AFP level and the reduction rates of tumor size (>50%), the TACE + PEI group has better effects than TACE group; as adverse effects, TACE + PEI group has lower incidence rates than TACE group. In patients with HCC, the efficacy of TACE combined with PEI is significantly better than that of TACE alone. Although there is convincing evidence to confirm the results mentioned, they still need to be confirmed by large sample, multicenter, randomized, controlled trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignant tumors with an increasing incidence in the industrialized countries. It is the sixth most common neoplasm in the world, with more than half a million new cases annually [1]. According to the World Health Organization (WHO), most cases of hepatocellular carcinoma occur in Asia. East Asia particularly has a very high incidence (over 20 cases per 100,000 population). Another region of concern is sub-Saharan Africa, and particularly the western region of Africa [2].
Many risk factors can contribute to hepatocellular carcinoma occurring, mainly hepatitis B and C virus infection, cirrhosis, and aflatoxin B1 ingestion. Cirrhosis is the strongest predisposing factor in hepatocellular carcinoma.
Early diagnosis of hepatocellular carcinoma is rare, and the majority of individuals present with locally advanced disease [3]. Treatments for HCC have been conventionally divided into curative treatment and palliative treatment. Curative treatments, such as resection, liver transplantation, and percutaneous ablation[4] and surgical resection is the main method, but because of lacking early symptoms most patients with liver cancer who received treatment are at the advanced stages and lose the opportunity to operation, after curative resection, recurrence is common and is the main cause of death so most patients are suitable only for receiving palliative treatments, such as radiotherapy, systemic chemotherapy, immunotherapy, embolization ethanol injection and so on. In many countries, transarterial chemoembolization (TACE) has been shown to improve survival, but it also has many disadvantages. Percutaneous ethanol injection (PEI) can be a curative therapy for small HCC (<3 cm). Using TACE plus PEI is either to reduce the size of larger tumors in order to subsequently apply percutaneous treatment or to combine the necrotizing effects of both procedures in order to achieve a more complete tumor necrosis [5].Therefore, this article sets onto determine the efficacy and safety of TACE plus PEI and TACE alone for patients with HCC.
Materials and methods
Literature search
We searched EMBASE, PubMed, the Cochrane Library, Chinese biomedicine literature database, Chinese scientific full-text database, and Chinese journal full-text database for randomized controlled trials comparing TACE + PEI with TACE by means of the keywords “hepatocellular carcinoma” “liver cell carcinoma” “transarterial chemoembolization” “percutaneous ethanol injection” and “randomized controlled trial”. No language limitation was imposed. We hand-searched key Chinese magazines of related fields, used search engines to search related references on the Internet, and searched the references of included studies. In addition, we contacted experts to identify potentially eligible trials, published, and unpublished.
Inclusion and exclusion
We considered all published and unpublished randomized controlled trials if they were randomized controlled trials comparing TACE + PEI with TACE; untreated patients with HCC; confirmed histologically or diagnosed HCC by means of pathologic examination of biopsy or autopsy specimens in all patients; and no evidence for extrahepatic metastases.
Evaluation method
The search strategy described was used to obtain titles and abstracts of randomized controlled trials that were relevant to this review. Two reviewers independently assessed the titles and abstracts of all identified trials to confirm fulfillment of inclusion criteria, with disagreements settled through consensus opinion reached using the other investigator. Data were independently extracted by two investigators and checked by the other authors. The quality of included studies was assessed independently by two reviewers without blinding to authorship or journal. Discrepancies were resolved by discussion with the third investigator. The quality items assessed were randomization, allocation concealment, blinding (participants, investigators, outcome assessors, and data analysis), and completeness of follow-up.
Statistical analysis
We analyzed the data using Review Manager (version 5.0) and extracted and pooled data for summary estimates. We expressed results for dichotomous outcomes as relative risk (RR) with 95% confidence intervals (CIs) and continuous outcomes as weighted mean difference (WMD) or standard mean difference (SMD). We used the χ2 statistic to assess heterogeneity between trials and the I2 statistic to assess the extent of inconsistency. We used a fixed-effect model for calculations of summary estimates and their 95% CI unless there was significant heterogeneity, in which case results were confirmed using a random-effects statistical model. Subgroup analyses were intended to explore important clinical differences among trials that might be expected to alter the magnitude of treatment effect.
Results
Search results
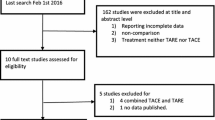
We identified 882 potentially eligible trials and subsequently excluded 875 trials for the following reasons: 444 were not randomized; 96 were about drug therapy; 120 were review; 113 were missing test group or control group; 102 were abstracts referring exclusively to limited-stage disease or treatments other than TACE or PEI; and seven randomized controlled trials totaling 623 patients were included. Finally, the trials all reported the effective about the comparison with TACE + PEI and TACE, and the analysis of the survival rates. Similarity of comparison groups at baseline was ensured by stratified randomization based on age at entry and sex in all of the included studies.
The quality and characteristics of included studies
The quality and characteristics of included studies are shown in Table 1.
Meta-analysis results
Six-month survival rates
We identified three trials (388 participants) with outcome measurement of 6-month survival rates. There is no heterogeneous among the trials included, using fixed-effects model (RR, 1.84; 95% CI, 1.06–3.18), the results are shown in Fig. 1.
One-year survival rates
We identified six trials (566 participants) with outcome measurement of 1-year survival rates. There is no heterogeneous among the trials included, using sing fixed-effects model (RR, 3.32; 95% CI, 2.32–4.75), the results are shown in Fig. 2.
Two-year survival rates
We identified five trials (518 participants) with outcome measurement of 2-year survival rates. There is no heterogeneous among the trials included, using fixed-effects model (RR, 2.75; 95% CI, 1.87–4.04), the results are shown in Fig. 3.
Three-year survival rates
We identified three trials (154 participants) with outcome measurement of 3-year survival rates. There is no heterogeneous among the trials included, using fixed-effects model (RR, 3.43; 95% CI, 1.65–7.13), the results are shown in Fig. 4.
The decline rates of the AFP level
We identified three trials (415 participants) with outcome measurement of the decline rates of the AFP level. There is no heterogeneous among the trials included, using fixed-effects model (RR, 3.72; 95% CI, 2.44–5.66), the results are shown in Fig. 5.
The reduction rates of tumor size (>50%)
We identified four trials (470 participants) with outcome measurement of the reduction rates of tumor size (>50%). There is no heterogeneous among the trials included, using fixed-effects model (RR, 1.80; 95% CI, 1.51–2.14), the results are shown in Fig. 6.
Side effects
In both groups, there was no obvious treatment-related complication occurred. After TACE treatment or TACE plus PEI treatment, most patients showed symptoms of a mild postembolization syndrome: fever, mild nausea and wild abdominal pain, but all were self-limited postembolization syndrome. And these side effects were transient and disappeared within a short time.
Discussion
TACE has become one of the most common forms of interventional therapy. But because of the periphery of the massive hepatocellular carcinoma more portal blood supply, simple TACE treatment is not to achieve complete necrosis of the main tumors, and the recurrence rate post-TACE is still high, the long-term survival is unsatisfactory. It is a challenge to postpone disease progression and prolong survival of inoperable HCC [13]. It is well known that improving the overall therapeutic effects of HCC depends on the combined therapies. PEI is the seminal technique, it is also widely used and is an effective means of treating HCC, and its advantages and limitations were widely reported. It is inexpensive, safe, and easy to perform and has few adverse effects. But the effectiveness of PEI has been limited to small HCC lesions, the tumor less than 3 cm in diameter [14]. In lesions larger than 3 cm in diameter, it is difficult to inject ethanol throughout the entire tumor. Compared with TACE, the combination of TACE and PEI can get more complete necrosis rates of tumor and prolong overall survival [15]. Therefore, the combination of TACE and PEI should be a better treatment option for inoperable HCCs than TACE alone. Adding PEI after TACE has been expected to obtain adequate control of this tumor and to alter the texture of the tumor parenchyma, so that a large volume of ethanol can be administered to penetrate entire tumor lesions resulting in a complete necrosis [12].
The aim of the meta-analysis was to review the available evidence to estimate the effectiveness and safety of TACE plus PEI. This meta-analysis of data from the including studies have shown the 6-month, 1-, 2-, and 3-year survival rates: the decline rates of the AFP level and the reduction rates of tumor size(>50%) and the side effects. There are some limitations to this meta-analysis. Because the trials we found were of generally poor methodological quality, so it might not allow for a reliable conclusion. Of these including studies, few studies [7, 12] were mentioned double blinding, which can produce high performance bias and measuring bias. Another potential limitation is that not all studies were mentioned allocation concealment, two studies [9, 10] were not mentioned. This might bring selective bias in these trials, because it was possible for those responsible for recruiting the participant to alter their assignment if allocation was concealed. Some included [6–8] trials were not mentioned the Child’s class and the mean diameter of main tumor, these will influence the results of the meta-analysis. And most studies were come from China, so publication bias may have occurred.
The including studies were not inadequate, so we suggest that the outcome measurements should include multiple end-points in the future trails: 1. Future research should clearly show the detailed methods of how to implement blinding; 2. The enroll patients should be included in the analysis of the outcomes using an intention-to-treat analysis to determine the overall cost-utility of a treatment; 3. Quality of life would be an important additional outcome, so the quality of life should be administered at regular time intervals so that quality-adjusted life year and cost-utility analysis can be performed; 4. Future study should pay attention to the impact of geographic differences. Therefore, we still need more high quality, multicenter, randomized, well-designed randomised clinical trials from other countries and regions.
In conclusion, the combination of TACE and PEI compared with TACE alone improved the 6-month, 1-, 2-, and 3-year survival rates of patients and showed a clearly better outcome with respect to tumor size, AFP level. Side effects were mild in the TACE + PEI group. But because the most including studies were Chinese, the bias in the surgical approach, the difference in the doses of the ethanol injection and the number of injections. So further prospective, randomized trials investigating the more outcomes of combined TACE and PEI versus TACE alone in a large number of patients are warranted.
References
Llovet JM, Di Bisceglie AM, Bruix J, et al. Design and endpoints of clinical trials in hepatocellular carcinoma. J Natl Cancer Inst. 2008;100:698–711.
Samuel M, Chow PK, Chan Shih-Yen E, et al. Neoadjuvant and adjuvant therapy for surgical resection of hepatocellular carcinoma (Review). The Cochrane Library. 2009, Issue 3.
Oliveri RS, Gluud C. Transcatheter arterial embolisation and chemoembolisation for hepatocellular carcinoma (Protocol). The Cochrane Library. 2009; Issue 3.
Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907–17.
Marelli L, Stigliano R, Triantos C, et al. Treatment outcomes for hepatocellular carcinoma using chemoembolization in combination with other therapies. Cancer Treat Rev. 2006;32:594–606.
Li HB, Qiu SM. Analysis of combination of hepatic arterial chemoembolization and percutaneous ethanol injection for treatment of primary liver cancer. Med Sci Edi. 2008;27:368–70.
Li XY, Yang LZ. Analysis of transcatherter arterial chemoembolization combined with percutaneous ethanol injection for hepatoma. Chin J Interv Imaging Ther. 2007;4:269–72.
Zhao XL, Zhao ZJ, Zhou Q, et al. Combination of transcatheter arterial chemoembolization and percutaneous ethanol injection for treatment of huge unresectable hepatocellular carcinoma under ultrasound. J Fourth Mil Med Univ. 2004;25:1382.
Kato T, Saito Y, Niwa M, et al. Combination therapy of transcatheter chemienbolization and percutaneous wthanol injection therapy for unresectable hepatocellualar carcinoma. Cancer Chemother Pharmacol. 1994;33:115–8.
Qu ZQ, Qian GJ, Chen H. Therapeutic effect of transcatheter arterial chemoembolization combined with percutaneous ethanol injection in hepatocellular carcinoma. Chinese–German J Clin Oncol. 2002;1:28–9.
Bartolozzi C, Lencioni R, Caramella D, et al. Treatment of large HCC: transcatheter arterial chemoembolization combined with percutaneous ethanol injection versus repeated transcatheter arterial chemoembolization. Radiology. 1995;197:812–8.
Becker G, Soezgen T, Olschewski M, et al. Combined TACE and PEI for palliative treatment of unresectable hepatocellular carcinoma. World J Gastroenterol. 2005;11:6104–9.
Liu SB, Hu DY, Huang YY, et al. The double intervention clinical value and application research of TACE with PAI on massive hepatocellular carcinoma. Chinese–German J Clin Oncol. 2008;7:128–30.
Tesdal IK, Wikström M, Flechtenmacher C, et al. Percutaneous treatment of hepatocellular carcinoma in patients with transjugular intrahepatic portosystemic shunts. Cardiovasc Intervent Radiol. 2006;29:778–84.
Chen XM, Luo PF, Lin HH. Long-term result of combination of transcatheter arterial chemoembolization and percutaneous ethanol injection for treatment of hepatocellular carcinoma. Chin J Cancer. 2004;23:829–32.
Conflict of interest statement
The authors made no disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, N., Guan, Q., Wang, K. et al. TACE combined with PEI versus TACE alone in the treatment of HCC: a meta-analysis. Med Oncol 28, 1038–1043 (2011). https://doi.org/10.1007/s12032-010-9620-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-010-9620-2