Abstract
Purpose
To assess the role of transcatheter arterial chemoembolization (TACE) and percutaneous ethanol injection (PEI) in patients with hepatocellular carcinoma (HCC) and transjugular intrahepatic portosystemic shunts (TIPS).
Methods
Between January 1999 and September 2004, 6 patients with HCC and TIPS were treated with either TACE (n = 3) or TACE in combination with PEI (n = 3). One patient had a known advanced, untreated HCC prior to TIPS. In the remaining 5 patients HCC was diagnosed 14, 17, 51, 69, and 76 months respectively after elective TIPS. TACE was performed using a mixture of 30–60 mg of epirubicin and 10 ml of lipiodol following superselective catheterization of tumor-feeding vessels. PEI was performed under CT guidance.
Methods
The mean follow-up time after treatment of HCC was 26.2 months (range 7–46 months). During follow-up, all patients were free of rebleeding. Two patients died 7 and 38 months after one session of TACE and PEI (77 months after TIPS) and three sessions of TACE (91 months after TIPS), respectively. The cause of death was liver failure (Child-Pugh class C) and peritonitis, respectively. A third patient underwent liver transplantation 24 months after TIPS and several sessions of TACE. In the remaining 3 patients, the HCC is well controlled 13, 30, and 46 months after repetitive percutaneous treatment without signs of hepatic deterioration or metastasis.
Conclusion
Transcatheter arterial superselective chemoembolization and percutaneous ethanol injection seems to be beneficial even in HCC patients treated with TIPS, provided that the liver function is adequate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Variceal bleeding, refractory ascites, and encephalopathy represent the most frequent, difficult, and alarming complications of cirrhosis. The annual risk for hepatocellular carcinoma (HCC) among carriers of the hepatitis B surface antigen (HbsAg) is 0.06–0.3%. The relative risk increases to 0.8% in patients with chronic hepatitis and to 1.5–6.6% in those with cirrhosis [1]. The incidence of HCC is rising in developed western countries, and in the United States there has been an increase of about 80% in the annual incidence rate during the past 20 years [2, 3]. The care of the subgroup of patients who have cirrhosis complicated by HCC is very challenging. Transcatheter arterial embolization (TAE) performed alone or in combination with chemotherapy (TACE) in unselected patients is a controversial treatment strategy for patients with unresectable HCC [4, 5]. Hemorrhage associated with varices in patients with HCC is often fatal. Ho et al. determined that more than 45% of 287 patients with HCC died acutely from variceal bleeding [6]. The management of the small group of patients with a history of portal decompression (surgical or intrahepatic shunting) followed by the occurrence of HCC is even more challenging: portal decompression may increase the arterioportal shunting and, thereby, decrease nutrient hepatic blood flow and lead to further hepatic dysfunction. Recently, there have been preliminary reports and a few case reports of combining transjugular intrahepatic portosystemic shunt (TIPS) and TACE in patients suffering from cirrhosis and HCC [7–9]. One paper reported long-term observation of 2 patients with HCC and TIPS [10].
The purpose of this study was to investigate the local therapeutic effect of TACE and percutaneous ethanol injection (PEI) in patients with HCC and TIPS, and to analyze the long-term survival rates of treated patients.
Materials and Methods
Patients
Between January 1999 and September 2004, 6 patients with HCC and TIPS were treated with either TACE (n = 3) or TACE in combination with PEI (n = 3). All patients were suffering from portal hypertension due to cirrhosis, and were primarily admitted with acute bleeding from ruptured gastroesophageal varices (n = 4), refractory ascites (n = 1), or both (n = 1). The clinical profile before TIPS is listed in Table 1. All patients were staged using the Child-Pugh classification [11]. The patients suffering from severe bleeding had failed to respond to endoscopic sclerotherapy of esophageal varices. One patient had a known advanced, untreated HCC of nodular type prior to TIPS and had experienced two massive upper gastrointestinal hemorrhages (Fig. 1). Sclerotherapy failed to control the bleeding, so he was treated on an emergency basis within 48 hr of admission. All the other patients were prepared for treatment by carrying out a variety of clinical and laboratory tests including color Doppler sonography and computed tomography (CT). CT was used to define the anatomy, with emphasis on the relation between the portal vein and hepatic vein, vascular patency, and ruling out the presence of HCC. All patients were evaluated for possible surgical shunting, and a final decision was made to perform TIPS after an interdisciplinary conference between the gastroenterologist, the surgeon, and the radiologist. All patients were informed about the procedure in detail, and they gave their written informed consent according to the guidelines of the local ethics committee.
TIPS Procedure
The treatment was performed with the patient under general anesthesia in the angiography suite. The technique of placing a transjugular intrahepatic stent to establish a portosystemic shunt has been described previously [12, 13]. Four patients were treated with TIPS alone, and two with TIPS combined with adjunctive embolotherapy of gastroesophageal collaterals using sclerosing agents [4% benzylalcohol (Varigloban, Kreussler Pharma, Wiesbaden-Biebrich, Germany) or sodium amidotrizoate (Ethibloc, Ethicon GmbH, Norderstedt, Germany)] and coils. The embolotherapy was performed immediately after TIPS (at the same session via the transjugular vein). The rationale of embolotherapy was to use long-acting occluding agents embolizing proximal and peripheral collateral veins by combining liquid and mechanical materials in order to prevent collateralization and reperfusion.
After dilation of the intrahepatic tract, the patency of the TIPS shunt in the patient suffering from an advanced, untreated HCC prior to TIPS (Fig. 1) was guaranteed by deployment of a 4 cm long stent-graft (Jomed, Haan, Germany) in combination with a Wallstent (Boston Scientific Europe). In the other patients, the patency of TIPS shunts was guaranteed by deployment of bare stents: tantalum Strecker stent (Boston Scientific Europe), 9 mm/6 cm (n = 1), Wallstents (n = 3), and a combination of a balloon-expandable Palmaz stent (Cordis Endovascular, Haan, Germany) and a Wallstent (n = 1).
A 51-year-old man suffering from portal hypertension due to cirrhosis (chronic hepatitis). Prior to TIPS he had experienced two massive upper gastrointestinal hemorrhages within a few weeks. In October 2000 he was admitted with life-threatening hemorrhage and was treated with TIPS on an emergency basis. A MR scan (T1-weighted, fat suppression) about 6 weeks before TIPS shows a HCC (7.5 cm in diameter) of the nodular type in segment 4. B Superselctive lipiodol embolization (posteroanterior view) immediate before TIPS. The tip of the 3 Fr microcatheter is placed in a branch of the left hepatic artery. C Direct splenoportography (right anterior oblique, 20°) after catheterization of the splenal artery. The pressure gradient was 17.5 mmHg (24 cm H2O). D TIPS shunt (lateral view) after deployment of a 4 cm long stent-graft and an overlapping bare Wallstent, and after variceal embolization using coils and Ethibloc. E Result after TIPS and variceal embolization (right anterior oblique, 25°). The pressure gradient was reduced to 9 mmHg (12 cm H2O).
TACE/PEI Procedure
Prior to each treatment session a dual-phase spiral CT scan of the liver was done to assess the extent of the HCC, and to check the patency of the TIPS tract and portal vein flow. Renal and liver function tests, electrolytes, and coagulation studies were performed. All tumors were staged using the TNM classification [14] and the method of Okuda et al. [15]. Transfemoral angiography (different-shaped 5 Fr catheters) of the celiac axis and superior mesenteric artery (SMA) was performed in all patients to outline the vascular anatomy and to identify the arteries contributing to the blood supply of the tumor. All treatments were performed with the patient under local anesthesia. All patients were informed about the procedure in detail, and gave their written informed consent according to the guidelines of the local ethics committee.
TACE was performed after superselectively introducing a 3 Fr microcatheter into the segmental branches of the hepatic artery and injecting a mixture of 10 ml iodized oil and 30–60 mg epirubicin hydrochloride (Farmorubicin, Farmitalia, Carlo Erba, Freiburg, Germany), mixed with the pumping method immediately before injection. The dosage was proportional to liver function and tumor size: 60 mg epirubicin hydrochloride was given to patients 1, 3, 4, and 5; 45 mg epirubicin hydrochloride to patient 6, and 30 mg epirubicin hydrochloride to patient 2 (Table 2). The injection was performed under fluoroscopic control, and was interrupted if flow ceased or retrograde flow occurred. If the flow did not cease after injection of the above mixture, the injection was continued with a mixture of 10 ml iodized oil and 10 ml NaCl. After injection of the mixture of lipiodol and epirubicin, we did not use gelfoam sponge or other embolic material to stop the arterial flow. During the procedure an antiemetic (i.e., ondansetron) was given and continued for 12–24 hr after TACE. An opiate analgesic (i.e., piritramide) was administered if necessary. If possible, TACE was repeated after a minimum time interval of 8 weeks, and up to five times.
PEI was carried out under CT guidance. After intratumoral positioning of a 22 cm long, 21gauge needle (Bard, Karlsruhe, Germany) without sideholes, a mixture of absolute ethanol, local anesthetic (Scandicain), and a nonionic contrast medium in the ratio 8:1:1 respectively was injected at a dosage of 6–9 ml per session, depending on ethanol distribution, patient compliance, and lesion size [16]. If possible, PEI was repeated after a minimum time interval of 8 weeks.
Evaluation of Treatment Response
Follow-up imaging for shunt surveillance and liver parenchyma consisted of ultrasonography (US) and color Doppler US at discharge and at 3, 6, and 12 months after the procedure and 6-monthly thereafter. A shunt insufficiency was diagnosed when the reduction in maximum portal vein flow velocity was below 20 cm/sec or reduction of the early increment of the portal vein flow velocity was more than 50%. Follow-up visits were scheduled prospectively. All suspected shunt abnormalities were evaluated by direct portography and pressure measurement after transjugular TIPS shunt catheterization.
On US scans, every discrete solid lesion was considered as a possible HCC, and was an indication for dual-phase spiral CT and/or magnetic resonance imaging (MRI). If the lesion detected at US clearly matched a lesion showing the characteristic features of HCC, including arterial hypervascularization at dual-phase spiral CT or MRI, biopsy confirmation was considered unnecessary, according to the current noninvasive criteria devised by the European Association for the Study of the Liver [17].
The results of US, color Doppler US, and the enhanced CT scan of the liver were used for evaluation of tumor response before the next TACE/PEI session. Tumor response was classified according to the World Health Organization classification [18]: an increase in tumor mass of more than 25% and/or appearance of new tumor foci was classified as progressive disease (PD); a decrease in tumor mass of less than 50% or an increase of less than 25% as stable disease (SD); a decrease in tumor mass of more than 50% as a partial response (PR); and complete disappearance of the tumor manifestations as complete remission (CR).
Further follow-up data were based on findings from outpatient examinations, periodic blood tests, and telephone interviews with the patients and their primary physicians. The patients were followed up until death, liver transplantation, or November 2004.
Results
TIPS
The mean portosystemic pressure gradient (PPG) was 22.1 mmHg (range 16–38 mmHg) before shunting and 11.1 mmHg (range 7.5–13 mmHg) after the procedure (paired t-test, p < 0.0001), with a mean balloon diameter of 8.8 mm (range 8–10 mm). During follow-up, all patients were free of rebleeding. Duplex scanning and shunt venograms revealed shunt dysfunction in all patients due to stenosis (n = 5) and occlusion (n = 1), which was successfully treated by percutaneous transluminal angioplasty (PTA) and stent implantation. One patient showed a small amount of ascites prior to dilation of the shunt stenosis. The total number of reinterventions necessary to maintain TIPS patency was 1.6 (range 1–3).
TACE/PEI
As mentioned above, one patient had a known advanced, untreated HCC of nodular type prior to TIPS. In 5 patients HCC of nodular type were diagnosed 14, 17, 51, 69, and 76 months after elective TIPS (Table 2). Alphafetoprotein (AFP) was >10 ng/dl in 4 patients (mean 105 ng/dl; range 45–165 ng/dl), <10 ng/dl in 1 patient, and unknown in 1 patient. The diagnosis of HCC was confirmed histologically in 2 of the 6 patients. Seventeen TACE procedures were performed in the 6 patients, an average of 2.8 per patient (range 1–5), and 5 PEI procedures were performed in 3 patients (average 1.6; range 1–2). All interventions were technically successful.
The mean follow-up time after treatment of HCC was 26.2 months (range 7–46 months). Two patients died 7 and 38 months after one session of TACE and PEI (77 months after TIPS) and three sessions of TACE (91 months after TIPS), respectively. Causes of death were liver failure and peritonitis, respectively. One patient underwent liver transplantation 24 months after TIPS and several sessions of TACE (Fig. 2). In the other patients HCC is well controlled 13, 30, and 46 months after repetitive percutaneous treatment without signs of hepatic deterioration or metastasis. A summary of the patient data is given in Table 2.
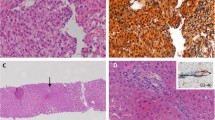
Same patient as in Fig. 1. Between November 2000 and September 2002 the HCC was controlled by TACE (five sessions). All TACE procedures were performed using a superselective chemoembolization technique. A Follow-up angiography (posteroanterior view) about 13 months after the first treatment, and after three sessions of TACE, shows a new tumor focus (segment 6). There is an aberrant origin of the right hepatic artery from the superior mesenteric artery. B Superselective catheterization of the segmental artery (posteroanterior view). C Result after chemoembolization, with no vascularization of the tumor. D Native CT scan (coronal planar reconstruction) after chemoembolization shows the distribution of the iodized oil. E Two years after TIPS the patient went to liver transplantation. Serial macroscopic and microscopic analysis of the liver (posterior view) proved total necrosis of both tumor foci, and a patent stent-graft with complete endothelialization.
Complications
TIPS
Procedure-related complications with clinical sequelae occurred in 3 patients (encephalopathy: n = 1; fever and abdominal pain: n = 2). These patients were treated successfully with medical therapy (lactulose in combination with limits on protein, and antibiotics, respectively) without any long-term sequelae.
TACE/PEI
After TACE, all patients showed symptoms of a mild postembolization syndrome (fever <39°C, mild nausea, and mild abdominal pain), but all were able to be discharged without delay. We did not observe any complications during the PEI procedures.
Discussion
The evidence-based indications for TIPS are discussed by Shiffman et al. [19] and Haskal et al. [20]. Whereas Haskal et al. conclude that accepted indications for TIPS include uncontrollable or recurrent variceal hemorrhage, portal hypertensive gastropathy, refractory hypertensive portal ascites or hydrothorax, and Budd-Chiari syndrome, Shiffman et al. discuss accepted indications (+++), potential indications (++), and experimental indications (+). Further, Shiffman et al. discuss indications not accepted (−), and absolute contraindications (− −) for TIPS.
Five of our 6 patients were treated either on the basis of accepted (n = 4) or potential (n = 1) indications for TIPS, and at the time of diagnosing HCC (mean follow-up of 45 months after TIPS) these patients were free of rebleeding. The ascites patient showed minor ascites (ultrasound) with no fluid-related symptoms. Altogether the efficacy of portal decompression in these 5 patients was obvious.
The absolute contraindications to TIPS placement include severe hepatic failure, uncontrolled hepatic encephalopathy, right heart failure, and uncontrolled systemic infection. Indications not accepted or relative contraindications include primary or secondary hepatic malignancy, and polycystic liver disease. In several publications the presence of hepatic malignancy was one of the exclusion criteria [21, 22]. Wallace et al. have recently published their experience with TIPS that traversed the tumor of patients with advanced primary and secondary hepatic malignancies [23]. They conclude that TIPS can be created safely in patients with hepatic malignancy without increased technical complications, but they observed a high rate of acute shunt occlusion. In our patient with HCC prior to TIPS we avoided traversing the tumor by using pre-TIPS superselective lipiodolembolization, transfemoral splenoportography in two planes, and fluoroscopy to plan the transhepatic puncture and to find the optimal route for traversing the region and puncture site (Fig. 1). The theoretical rationale for using a stent-graft was to create a physical barrier between the tumor and the shunt lumen. During follow-up, we observed a shunt stenosis after 8 months, but the PTA was successful and the shunt stayed open until the patient underwent a liver transplantation 2 years later (Fig. 2).
In terms of evidenced-based medicine, the indications for TACE when administered to unselected patients with unresectable HCC are not clarified [5]. However, the two most recent high-quality trials showed a significant survival benefit in a stringently selected subgroup of patients [24, 25]. The aims of chemoembolization are to synergistically combine a highly concentrated dose of chemotherapy to tumor cells with embolization of the artery feeding a tumor, which results in ischemia within the tumor and subsequent tumor necrosis. The extent of tumor necrosis after chemoembolization has been reported to range from 60% to 100% [26]. Prognostic factors influencing the survival of patients with HCC treated with TACE were found to be tumor type (nodular vs. infiltrating), tumor size, Child-Pugh class (A vs. B vs. C), and grade of vascularization [15, 27]. Our experience and results confirm these findings: (a) one of our patients with advanced HCC (all patients had tumor of the nodular type) underwent liver transplantation 24 months after TIPS and several sessions of TACE, and the serial macroscopic and microscopic analysis of the liver proved total necrosis of both tumor foci, showing the efficacy of repetitive and superselective chemoembolization of HCC of the nodular type (Fig. 2); (b) our patient with the highest Child-Pugh class before treatment (Table 2) died 7 months later due to liver failure.
PEI has been indicated as an effective alternative to surgery for small HCC nodules, since complete necrosis of lesions less than 3 cm in diameter has been achieved [28]. According to the guidelines of the European Association for the Study of the Liver, PEI should be considered the standard technique for percutaneous treatment of small HCC [17]. In patients with small HCC, it has recently been reported that radio-frequency thermal ablation (RF ablation) is superior to PEI with respect to local recurrence-free survival rates [29]. As a result of difficulties in obtaining homogeneous alcohol perfusion in larger tumors, patients with large HCC are usually treated with TACE [30]. There are several reports evaluating the combined therapy of TACE and PEI for patients with HCC [31–34], but only one of these is a randomized controlled study [33]. The results of these studies may allow us to conclude that combination therapy with TACE and PEI is superior to monotherapy in terms of recurrence-free survival. Among patients with HCC tumors measuring less than 2 cm, Koda et al. found that the survival rates in the group treated with TACE and PEI group were significantly better than the survival rates in the group treated with PEI alone [33]. Bartolozzi et al. concluded that the combination of TACE and PEI was an effective treatment even in patients with large HCC [31]. We combined TACE and PEI in 3 patients, all of whom had tumors 4 cm or less in diameter. One patient died 7 months later due to liver failure unrelated to treatment. The other patients showed stable disease 30 and 46 months after two sessions with combined therapy together with one session of TACE, respectively. Using the life table method, our overall 1-, 2-, and 3-year survival rates are 83%, 63%, and 45%, respectively.
The main challenge and potentially the most crucial aspect of TACE is to preserve as much functional liver tissue as possible, and thus avoid deterioration of liver function [35]. Due to decreased portal blood flow and the potential decrease in arterial nutrient hepatic blood flow, this challenge is maximized in patients with portosystemic shunts. To our knowledge there are four case reports of combining TIPS and TACE in patients suffering from cirrhosis and HCC [7–10]. Following the same strategy as ours with superselective chemoembolization, they report that HCC was well controlled without hepatic deterioration, but long-term follow-up [10] is reported only in 2 cases (22 and 58 months after therapy).
In conclusion, transcatheter arterial chemoembolization and percutaneous ethanol injection seems to be useful even in patients with TIPS, provided there is good liver function and superselective catheterization of segmental branches for the chemoembolization leaves the normal liver parenchyma virtually unaffected. Further research is warranted to clarify whether newer methods of tissue ablation, such as RF ablation, are superior with respect to survival rates.
References
Koteish A, Thuluvath PJ (2002) Screening for hepatocellular carcinoma. J Vasc Interv Radiol 13:185–190
El-Serag HB, Mason AC (1999) Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 340:745–750
El-Serag HB, Davila JA, Petersen NJ, McGlynn KA (2003) The continuing increase in the incidence of hepatocellular carcinoma in the United States: An update. Ann Intern Med 139:817–823
Camma C, Schepis F, Orlando A, Albanase M, Shahied L, Trevisani F, Andreone P, Craxi A, Cottone M (2002) Transarterial chemoembolization for unresectable hepatocellular carcinoma: Meta-analysis of randomized controlled trials. Radiology 224:47–54
Myers RP (2003) Meta-analysis of transarterial embolization in patients with unresectable hepatocellular carcinoma. Radiology 227:611–612
Ho J, Wu PC, Kung TM (1981) An autopsy study of hepatocellular carcinoma in Hong Kong. Pathology 13:409–415
Sakaguchi H, Uchida H, Maeda M, Matsuo N, Kichikawa K, Ohishi H, Nishida H, Ueno K, Nishimine K, Rosch J (1995) Combined transjugular intrahepatic portosystemic shunt and segmental lipiodol hepatic artery embolization for the treatment of esophagogastric varices and hepatocellular carcinoma in patients with cirrhosis: Preliminary report. Cardiovasc Intervent Radiol 18:9–15
Mingoli A, Modini C, Salvatori F, Bezzi M, Sgarzini G, Nardacchione F, Marzano M (1995) Emergency transjugular intrahepatic portosystemic shunt in patients with variceal bleeding and hepatocellular carcinoma. Ital J Gastroenterol 27:309–312
Serafini FM, Zwiebel B, Black TJ, Carey LC, Rosemurgy AS (1997) Transjugular intrahepatic portasystemic stent shunt in the treatment of variceal bleeding in hepatocellular carcinoma. Dig Dis Sci 42:59–65
Tazawa J, Sakai Y, Yamana M, Kakinuma S, Maeda M, Suzuki K, Miyasaka Y, Nagayama K, Kusano F, Sato C (2000) Long-term observation after transjugular intrahepatic portosystemic stent shunt in two patients with hepatocellular carcinoma. J Clin Gastroenterol 31:262–267
Pugh RNH, Murray-Lyon M, Dawson JL, Pietroni MC, Williams R (1973) Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 8:646–649
Rössle M, Haag K, Ochs A, Sellinger M, Nöldge G, Perarnau J-M, Berger E, Blum U, Gabelmann A, Hauenstein KH, Langer M, Gerok W (1994) The transjugular intrahepatic portosystemic shunt. N Engl J Med 330:165–171
Tesdal IK, Jaschke W, Bühler M, Adamus R, Filser T, Holm E, Georgi M (1997) Transjugular intrahepatic portosystemic shunting (TIPS) with balloon-expandable and self-expanding stents: Technical and clinical aspects after 3 1/2 years experience. Cardiovasc Intervent Radiol 20:29–37
International Union Against Cancer (1998) TNM atlas, 4th edn. Springer, Berlin Heidelberg New York, pp 115–123
Okuda K, Ohtsuki T, Obata H, Tomimatsu M, Okazaki N, Hasegawa H, Nakajima Y, Ohnishi K (1985) Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Cancer 56:918–928
Adamus, Tesdal IK, Georgi M (1997) Perkutane Alkoholinstillationstherapie (PAI) und Chemoembolisation bei einem ausgedehnten hepatozellulären Karzinom (HCC). Fortschr Rontgenstr 166:173–175
Bruix J, Sherman M, Llovet JM, et al (2001) for the EASL Panel of Experts on HCC Clinical management of hepatocellular carcinoma: Conclusions of the Barcelona-2000 EASL conference. J Hepatol 35:421–430
Häussler MD, Pfeifer T, Safi F, Friedrich JM, Bargon G (1993) CT-Monitoring bei regionaler Chemotherapie von Lebermetastasen. In: Reiser M, Streudel A, Hirner A, Kania U (eds) Lebertumoren und portale Hypertension: Radiologische und chirurgische Aspekte. Springer, Berlin Heidelberg New York, pp 241–247
Shiffman ML, Jeffers L, Hoofnagle JH, Tralka TS (1995) The role of transjugular intrahepatic portosystemic shunt for treatment of portal hypertension and its complications: A conference sponsored by the National Digestive Diseases Advisory Board. Hepatology 22:1591–1597
Haskal ZJ, Martin L, Cardella JF, Cole PE, Drooz A, Grassi CJ, McCowan TC, Meranze SG, Neithamer CD, Oglevie SB, Roberts AC, Sacks D, Silverstein MI, Swan TL, Towbin RB, Lewis CA (2001) Quality improvement guidelines for transjugular intrahepatic portosystemic shunts. SCVIR Standards of practice committee. J Vasc Interv Radiol 12:131–136
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31:864–871
Hidajat N, Vogl T, Stobbe H, Schmidt J, Wex C, Lenzen R, Berg T, Neuhaus P, Felix R (2000) Transjugular intrahepatic portosystemic shunt. Experience at a liver transplantation center. Acta Radiol 41:474–478
Wallace M, Swaim M (2003) Transjugular intrahepatic portosystemic shunts through hepatic neoplasms. J Vasc Interv Radiol 14:501–507
Llovet JM, Real MI, Montana X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart J, Sola R, Rodes J, Bruix J (2002) Arterial embolization or chemoembolization versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: A randomized, controlled trial. Lancet 359:1734–1739
LO CH, Ngan H, Tso W-K, Liu C-L, Lam C-M, Poon RT-P, Fan S-T, Wong J (2002) Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35:1164–1171
Ramsey DE, Kernagis LY, Soulen MC, Geschwind JFH (2002) Chemoembolization of hepatocellular carcinoma. J Vasc Interv Radiol 13:211–221
Huppert PE, Lauchart W, Duda SH, Torkler C, Kloska SP, Weinlich M, Benda N, Pereira P, Claussen CD (2004) Chemoembolisation des hepatozellulären Karzinoms: Welche Faktoren bestimmen Therapieansprechen und Überleben? Fortschr Rontgenstr 176:375–385
Livraghi T, Bolondi L, Buscarini L, Cottone M, Mazziotti A, Morabito A, Torzilli G (1995) No treatment, resection and ethanol injection in hepatocellular carcinoma: A retrospective analysis of survival in 391 patients with cirrhosis. J Hepatol 22:522–526
Lencioni RL, Allgaier H-P, Cioni D, Olschewski M, Deibert P, Crocetti L, Frings H, Laubenberger J, Zuber I, Blum HE, Bartolozzi C (2003) Small hepatocellular carcinoma in cirrhosis: Randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology 228:235–240
Bartoluzzi C, Lencioni R (1996) Ethanol injection for the treatment of hepatic tumors. Eur Radiol 6:682–696
Bartolozzi C, Lencioni R, Caramella D, Vignali C, Cioni R, Mazzeo S, Carrai M, Maltinti G, Capria A, Conte PF (1995) Treatment of large HCC: Transcatheter arterial embolization combined with PEI versus repeated TACE. Radiology 197:812–818
Dohmen K, Shirahama M, Shigematsu H, Miyamoto Y, Torii Y, Irie K, Ishibashi H (2001) Transcatheter arterial chemoembolization therapy combined with percutaneous ethanol injection for unresectable large hepatocellular carcinoma: An evaluation of the local therapeutic effect and survival rate. Hepatogastroenterology 48:1409–1415
Koda M, Murawaki Y, Mitsuda A, Mitsuda A, Oyama K, Okamoto K, Idobe Y, Suou T, Kawasaki H (2001) Combination therapy with transcatheter arterial chemoembolization and percutaneous ethanol injection compared with percutaneous ethanol injection alone for patients with small hepatocellular carcinoma: A randomized controlled study. Cancer 92:1516–1524
Lubienski A, Bitsch RG, Schemmer P, Grenacher L, Düx M, Kauffmann GW (2004) Langzeitergebnisse der interventionellen Therapie von großen, inoperablen hepatozellulären Karzinome (HCC): signifikanter Überlebnsvorteil von transarterieller Chemoembolisation (TACE) und perkutaner Ethanolinjektion (PEI) gegenüber der TACE-Monotherapie. Fortschr Rontgenstr 176:1794–1802
Acunas B, Rozanes I (1999) Hepatocellular carcinoma: Treatment with transcatheter arterial chemoembolization. Eur J Radiol 32:86–89
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tesdal, I.K., Wikström, M., Flechtenmacher, C. et al. Percutaneous Treatment of Hepatocellular Carcinoma in Patients with Transjugular Intrahepatic Portosystemic Shunts. Cardiovasc Intervent Radiol 29, 778–784 (2006). https://doi.org/10.1007/s00270-005-0063-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-005-0063-7