Abstract
In order to examine whether symptoms of iron deficiency anemia are due to the iron deficiency itself or the associated anemia, 34 patients with polycytemia vera (PV) treated with venesectio, who had iron deficiency but normal hemoglobin (Hb) levels, were given a questionnaire covering symptoms of iron deficiency including the international RLS-scale and the Fact-fatigue quality of life scale (QoL). We found a prevalence of pica of 11.7%, mouth paresthesias of 5.8% and rest-less legs 29.6% (RLS “normal” prevalence 10%). Thus, the prevalence of RLS is significantly higher in our population. We also saw a significant difference in QoL between patients with and without RLS (P = 0.015) and QoL correlated with the severity of RLS (R = 0.85). In conclusion, RLS seems to be a frequent and serious problem for PV patients treated with venesectio according to standard guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with polycytemia vera (PV) have an abnormal production of erythrocytes leading to an elevated hemoglobin level, red cell volume, and hematocrit. Venesectio is the standard treatment for this condition in order to bring erythrocytes out of the blood and diminish the red cell volume, reducing Hct and thereby reducing the risk for thromboembolic events [1]. Another effect of this treatment is loss of iron which induces a state of iron deficiency. This reduces the bone marrow production of erythrocytes and the need for frequent phlebotomies.
Patients with anemia secondary to iron deficiency develop symptoms like fatigue, parestesias, pica, restless legs, and mouth symptoms such as burning or stinging sensations. It is unclear whether these symptoms are due to the anemia per se or due to iron deficiency. The patients with PV treated with venesectio develop iron deficiency but not anemia. For this reason it would be of interest to examine whether or not these patients express the symptoms described above.
There are indications that iron metabolism is involved in the pathophysiology of the restless legs syndrome (RLS) [2] and high prevalence of restless legs symptoms in our population would support this theory. Also, we wanted to examine whether the standard treatment for PV is as harmless as is assumed.
Data supporting an association between iron deficiency anemia and thyroid dysfunction [3] gave us reason to investigate the thyroid status of the patients.
Patients and methods
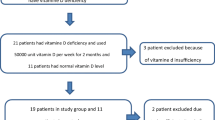
We enrolled patients for the study from the university hospital of Uppsala and the regional rural hospitals of Eskilstuna and Västerås in Sweden. All patients with the diagnosis of PV treated with venesectio were asked to participate in the study. Blood samples were analysed for hemoglobin (Hb) level, hematocrit, ferritin, transferrin saturation (Tsat), and thyroid function. Patients with anemia and patients with normal iron status were excluded from the study. Some patients had concomitant treatment with hydroxyurea.
Participating patients were asked to fill in a questionnaire, consisting of three parts: one part asked for traditionally recognized symptoms of iron deficiency like pica, mouth sores, and burning sensations from the mouth. Another part consisted of the Fact-fatigue quality of life scale (including the original 13 fatigue-related and the 7 functional well-being items) [4] and part three was the International restless legs scale [5].
Descriptive statistical analysis was used to calculate the prevalence of the different symptoms. Furthermore, we wanted to study the impact of RLS on quality of life. We used a t-test-analysis to see if there was a significant difference in quality of life for patients with or without RLS and a correlation-analysis to see if the severity of restless legs symptoms correlated with quality of life.
Ethical approval was obtained from the ethical committee at the University of Uppsala. Patients gave consent before blood sampling and answering the questionnaire.
Results
We enrolled in total 41 PV patients on phlebotomy treatment with the treatment goal of Hct < 45%. One patient was excluded because of anemia and six patients were excluded because of normal iron status. Remaining 34 patients were thus with iron deficiency and normal Hb levels. Hct levels in most patients were 44–47% with occasional patients above that, since the questionnaire was given the same day as a phlebotomy. The mean s-ferritin was 11.2 (range 3.7–23), mean Tsat 7.7 (range 3–29), mean MCV 79.9 (range 62–114). A normal or high MCV was caused by concomitant hydroxyurea treatment in some patients.
Ten out of the 34 patients (29.4%) expressed symptoms of rest-less legs with the median severity of 17 on the international restless legs scale. Two patients (5.8%) reported mouth symptoms and four patients (11.7%) had pica (Table 1). The median quality of life score for all included patients was 87 on the Fact-fatigue scale. The subgroup of patients who suffered from restless legs show a quality of life value of 68.5 while the patients without restless legs show a value of 93 (Table 2). The difference between these two groups was significant (P = 0.015) There was a correlation between the severity of restless legs symptoms and quality of life with a correlation coefficient of 0.85 (Fig. 1). No patient showed any sign of thyroid dysfunction.
Discussion
The purpose of our study was to investigate the prevalence and severity of symptoms recognized as symptoms of iron deficiency anemia in PV patients treated according to standard principles with phlebotomy. This is a population of patients with iron deficiency but no anemia.
There are, to our knowledge, no studies in the literature concerning the prevalence of pica or mouth symptoms in a normal population. We believe that the prevalence in our population (11.7 and 5.6%, respectively) is elevated compared to what we would expect from a normal population which would support the theory that these symptoms are true symptoms of iron deficiency. It would be of interest to compare the prevalence from our population with a normal population.
The prevalence of RLS in a normal population has been investigated in several studies and has been estimated to be around 10% [6–10]. Two studies have been performed in the same geographical area of middle Sweden and showed prevalence in males of 5.8% and women of 11.4% [6, 10]. In our population, the prevalence is significantly higher (29.4%). Our data also show that the prevalence of RLS significantly reduces QoL with a correlation between the severity of RLS and reduced QoL. This correlation indicates that in patients with RLS, this symptom is important for QoL. There is a theoretical possibility that untreated PV patients may have an increased prevalence of RLS, however, there are no such reports in the literature. Neither has RLS been reported as a side effect of HU treatment.
There were problems finding an appropriate control group for this study. PV patients who no longer need phlebotomies and so are not iron deficient have a more advanced disease and therefore are unsuitable as controls. It is also questionable if newly diagnosed PV patients who have just started phlebotomy treatment and still are iron replete would be appropriate as a control group, since their Hct still is high and they also suffer from the psychological effects of recent information that they have a malignant disease. The patients in this study were all in a stable situation with regular phlebotomy treatment. It has been generally assumed that the iron deficiency caused by phlebotomy treatment of PV patients is innocent, not causing symptoms of iron deficiency, since the patients are not anemic. However, this study shows that a proportion of iron deficient PV patients have typical symptoms of iron deficiency, some experiencing pica, mouth sore and other classical but less disturbing symptoms, but as many as 29% meeting the diagnostic criteria for restless legs syndrome with a QoL reduction. This indicates that the treating physician should be aware of the problem, asking for symptoms of iron deficiency, including RLS.
A discussion is needed whether patients with symptoms of iron deficiency should be treated with cytoreduction in order to avoid phlebotomy. This would seem reasonable in view of the recent findings of reduction of the JAK2 V617F mutation expression during interferon and hydroxyurea treatment [11, 12]. Another option would be to give iron supplementation. However, the ordinary doses used for treatment of iron deficiency may cause a rapid increase in Hct that could be potentially harmful for the patients. Further studies are needed to investigate whether low dose iron supplementation under strict monitoring of the Hct level eliminates the iron deficiency symptoms without causing risk for the patients. Any iron supplementation may be expected to increase the need for phlebotomy.
Conclusion
Phlebotomy-treated, iron deficient PV patients without anemia show typical symptoms of iron deficiency, including a 29% prevalence of RLS.
References
McMullin MF, Reilly JT, Campbell P, et al. Amendment to the guideline for diagnosis and investigation of polycythaemia/erythrocytosis. Br J Haematol. 2007;138:821–2. doi:10.1111/j.1365-2141.2007.06741.x.
Allen R. Dopamine and iron in the pathophysiology of restless legs syndrome (RLS). Sleep Med. 2004;5:385–91. doi:10.1016/j.sleep.2004.01.012.
Eftekhari MH, Keshavarz SA, Jalali M, Elguero E, Eshraghian MR, Simondon KB. The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls. Asia Pac J Clin Nutr. 2006;15:50–5.
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13:63–74. doi:10.1016/S0885-3924(96)00274-6.
Walters AS, Le Brocq C, Dhar A, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–32. doi:10.1016/S1389-9457(02)00258-7.
Ulfberg J, Nystrom B, Carter N, Edling C. Prevalence of restless legs syndrome among men aged 18 to 64 years: an association with somatic disease and neuropsychiatric symptoms. Mov Disord. 2001;16:1159–63. doi:10.1002/mds.1209.
Winkelman JW, Finn L, Young T. Prevalence and correlates of restless legs syndrome symptoms in the Wisconsin Sleep Cohort. Sleep Med. 2006;7:545–52. doi:10.1016/j.sleep.2006.01.004.
Tison F, Crochard A, Leger D, Bouee S, Lainey E, El Hasnaoui A. Epidemiology of restless legs syndrome in French adults: a nationwide survey: the INSTANT Study. Neurology. 2005;65:239–46. doi:10.1212/01.wnl.0000168910.48309.4a.
Bjorvatn B, Leissner L, Ulfberg J, et al. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. 2005;6:307–12. doi:10.1016/j.sleep.2005.03.008.
Ulfberg J, Nystrom B, Carter N, Edling C. Restless Legs Syndrome among working-aged women. Eur Neurol. 2001;46:17–9. doi:10.1159/000050750.
Kiladjian JJ, Cassinat B, Chevret S, et al. Pegylated Interferon-alfa-2a induces complete hematological and molecular responses with low toxicity in Polycythemia Vera. Blood. 2008;112:3065–72.
Ricksten A, Palmqvist L, Johansson P, Andreasson B. Rapid decline of JAK2V617F levels during hydroxyurea treatment in patients with polycythemia vera and essential thrombocythemia. Haematologica. 2008;93(8):1260–1. doi:10.3324/haematol.12801.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tobiasson, M., Alyass, B., Söderlund, S. et al. High prevalence of restless legs syndrome among patients with polycytemia vera treated with venesectio. Med Oncol 27, 105–107 (2010). https://doi.org/10.1007/s12032-009-9180-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-009-9180-5