Abstract
Delayed cerebral ischemia (DCI) is a common and severe complication after subarachnoid hemorrhage (SAH). Logistic regression (LR) is the primary method to predict DCI, but it has low accuracy. This study assessed whether other machine learning (ML) models can predict DCI after SAH more accurately than conventional LR. PubMed, Embase, and Web of Science were systematically searched for studies directly comparing LR and other ML algorithms to forecast DCI in patients with SAH. Our main outcome was the accuracy measurement, represented by sensitivity, specificity, and area under the receiver operating characteristic. In the six studies included, comprising 1828 patients, about 28% (519) developed DCI. For LR models, the pooled sensitivity was 0.71 (95% confidence interval [CI] 0.57–0.84; p < 0.01) and the pooled specificity was 0.63 (95% CI 0.42–0.85; p < 0.01). For ML models, the pooled sensitivity was 0.74 (95% CI 0.61–0.86; p < 0.01) and the pooled specificity was 0.78 (95% CI 0.71–0.86; p = 0.02). Our results suggest that ML algorithms performed better than conventional LR at predicting DCI.
Trial Registration: PROSPERO (International Prospective Register of Systematic Reviews) CRD42023441586; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=441586
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Delayed cerebral ischemia (DCI) is one of the most frequent complications after subarachnoid hemorrhage (SAH) and is sometimes a determinant of poor prognosis due to late diagnosis [1, 2]. The early identification of DCI can either interfere with the patient’s prognosis or reduce the costs of intensive care.
Logistic regression (LR) is the conventional method for predicting DCI, but it has limitations including low precision and complexity in the use of data, given the multicollinearity between the variables [3]. For this reason, machine learning (ML) algorithms appear as a potential alternative for the analysis of clinical data, because in addition to being able to process large amounts of data, they can learn the parameters, optimizing the obtained results [4].
Some studies involving DCI prediction through clinical data suggest that ML models have greater predictive power than LR [5,6,7]. Other studies that have applied ML algorithms using heterogeneous data (including both clinical information and imaging tests) have shown positive results in both the diagnosis of Alzheimer’s disease [8] and the prediction of the risk of aortic stenosis [9].
Therefore, we aimed to perform a systematic review and meta-analysis comparing the effectiveness of ML models versus LR models to predict DCI after SAH, specifically interested in parameters such as sensitivity, specificity, and area under the receiver operating characteristic (AUROC).
Methods
Protocol and Registration
This systematic review and meta-analysis were reported based on recommendations from the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement guidelines. The review protocol was registered with PROSPERO (CRD42022383937).
Eligibility Criteria
We screened studies by title, abstract, and full text using the eligibility criteria defined by the elements of our question: population, intervention, control, and outcomes. The essential items consisted of the following:
-
1.
Population men or women with SAH.
-
2.
Intervention classic ML algorithms, such as random forest, support vector machine, and artificial neural networks.
-
3.
Control conventional LR.
-
4.
Outcomes accuracy measurement (sensitivity, specificity, AUROC, and accuracy).
We only selected studies that reported outcome measures related to the effectiveness of DCI predictive models, such as sensitivity, specificity, accuracy, confusion matrix, and so on. We excluded the following types of articles: reviews, case reports, editorials, correspondences, studies without peer review, and abstracts.
Search Strategy and Data Extraction
We searched PubMed, Embase, and Web of Science up to December 2022. No publication period limits were applied. The following search terms were included: (“subarachnoid hemorrhage” or “SAH” or “subarachnoid hemorrhages”) AND (“delayed cerebral ischemia” or “DCI”) AND ((“machine learning” or “ML”) or (“logistic regression” or “LR”)). This search strategy was applied to all databases.
In addition to the main outcome measurements, the following baseline characteristics were collected: (1) number of patients, (2) sex distribution, (3) mean age, (4) hypertension, (5) proportion of patients with diabetes, (6) Hunt and Hess grade, and (7) modified Fisher scale. These data were extracted by two authors independently following predefined search criteria and quality assessment.
End Point
The main outcome was the accuracy measurement (sensitivity, specificity, AUROC, and accuracy) of the DCI prediction models.
Quality Assessment and Risk of Bias
This article used the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) criteria to evaluate the risk of bias. Domains included patient selection, index test, reference standard, and flow and timing. In line with the recommendations from the QUADAS-2 guidelines, questions per domain were tailored for this article and can be found in “Supplemental Materials, Adapted QUADAS-2 questions.” If one of the questions was scored at risk of bias, the domain was scored as high risk of bias. At least one domain at high risk of bias resulted in an overall score of high risk of bias, and only one domain scored as unclear risk of bias resulted in an overall score of unclear risk of bias for that article. Quality assessment was performed by two investigators (JBCD, LSS) independently. Disagreements between the two investigators were solved through a consensus after a discussion among the authors and senior author.
Summary measures
Because of the diversity of data reported by the models under study, we chose to compare the AUROCs of each article. When the study did not report the AUROC, we estimated the metric using sensitivity and specificity (Eq. 1). Only one study [15] provided information on the time point at which the AUROCs were calculated, which is crucial for assessing the time-sensitivity of the features. In that study, the time point with the highest performance was chosen, specifically 7 days before the onset of DCI.
Statistical Analysis
We extracted information on the true positives, true negatives, false positives, and false negatives and entered the data into Review Manager 5.4.1 (Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) to calculate pooled measures of sensitivity and specificity, as well as the corresponding 95% confidence intervals (CIs). We also used R (R Foundation for Statistical Computing, Vienna, Austria, 2021) to perform a meta-analysis of the tests’ performance.
Results
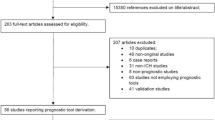
As illustrated by Fig. 1, a total of 1130 records were initially retrieved from three literature databases. Following the removal of duplicated records and the exclusion of studies that were not related to the topic of this meta-analysis, 37 studies remained for the full review. From those, six studies were deemed eligible.
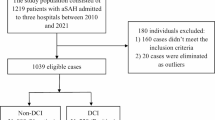
In this meta-analysis, we enlisted a nonoverlapping sample of 1828 participants, of whom 519 (28%) developed DCI. The studies reported 627 male patients and 1255 female patients, with a mean age ranging from 53 to 55 years. More details regarding the characteristics of the eligible studies are presented in Table 1. Of the 29 models identified in this review, the majority of employment was represented by LR (11 models) and random forest (RF) (5 models), as represented in Table 2.
Regarding DCI diagnostic criteria, the majority of studies relied on a combination of clinical and radiographic findings, including alterations in the Glasgow Coma Scale (GCS) score, the emergence of new focal neurological deficits, and the presence of ischemic infarcts on computed tomography (CT) or magnetic resonance imaging scans. In the context of prediction, a variety of covariates or predictors were employed, typically encompassing age, sex, clinical grades (Hunt–Hess and World Federation of Neurological Surgeons scale), treatment of aneurysms, and laboratory test results (hemoglobin, sodium, white blood cell count, platelet count, and creatinine levels). Furthermore, certain studies integrated specific features associated with subarachnoid hemorrhage, such as CT values and the presence of cerebral edema. Table 3 displays the covariates and diagnostic criteria for DCI used in the models.
The ML models exhibited better overall performance than the LR models, as evidenced by the pooled sensitivity and specificity, based on the data of five studies. One study was excluded of this analysis as it provided only the AUROC and lacked data of the confusion matrix [15]. For the LR models, sensitivity and specificity values were corresponding to 0.71 (95% CI 0.57–0.84; Fig. 2) and 0.63 (95% CI 0.42–0.85; Fig. 3), respectively, whereas the equivalent values for the ML models were 0.74 (95% CI 0.61–0.86; Fig. 4) and 0.78 (95% CI 0.71–0.86; Fig. 5). As depicted in Tables 4 and 5, ML models showed higher AUROC values than those obtained by LR models. This superiority is also supported by the scatter plot of AUROC values grouped by models (Fig. 6), and the forest plots (Supplement Figs. 3 and 4). Further comparisons between the algorithms are provided in Tables 4 and 5.
For a more specific evaluation, we conducted subanalyses of individual algorithms that presented a satisfactory amount of data (Supplemental Figs. 5–14). The extreme gradient boosting (XGBoost) model achieved the highest pooled sensitivity (0.89; 95% CI 0.80–0.89; Supplemental Fig. 13), whereas the artificial neural network (ANN) model had the highest specificity (0.81; 95% CI 0.71–0.92; Supplemental Fig. 6). In other subanalyses, only retrospective studies were included to reduce heterogeneity (Supplemental Figs. 15–18). Again, the ML models demonstrated better results than the LR models in terms of sensitivity (0.74; 95% CI 0.64–0.85; Supplemental Fig. 17) and specificity (0.77; 95% CI 0.72–0.82; Supplemental Fig. 18). The LR models had lower sensitivity (0.68; 95% CI 0.60–0.77; Supplemental Fig. 15) and specificity (0.51; 95% CI 0.27–0.75; Supplemental Fig. 16) when compared with the ML models.
Comparative Analysis: Strengths and Weaknesses
Regarding the strengths and weaknesses of the ML models employed, a detailed comparison of each algorithm’s characteristics is provided in Table 6. ANN demonstrates exceptional capabilities in capturing intricate patterns and nonlinear relationships. However, their utilization can be computationally demanding, and their inherent black-box nature makes interpretation challenging [16]. Decision tree models offer simplicity and robustness against outliers but are susceptible to overfitting and struggle with high-dimensional datasets. Ensemble classifiers improve prediction accuracy by combining multiple models, yet they require careful configuration and may lack interpretability [17]. Group-based trajectory modeling identifies distinct subgroups and provides valuable insights into population dynamics, albeit relying on predetermined trajectory groups [18]. K-nearest neighbor presents an intuitive approach for capturing complex relationships, yet computational demands can increase with larger datasets [19]. Multilayer perceptron exhibits nonlinear modeling capabilities, albeit at the cost of interpretability [20]. RF effectively handles nonlinear relationships and missing values, yet interpretation can be challenging [21]. Support vector machine excels at capturing nonlinear relationships but necessitate careful parameter tuning [22]. Lastly, XGBoost showcases proficiency in capturing complex patterns but requires meticulous parameter tuning and may have limited interpretability [23].
Key Variables in High-Performing ML Models
One study [12] employed the XGBoost algorithm with Boruta feature selection and aneurysm type as predictors. The inclusion of aneurysm type as a predictor is of utmost importance due to its provision of valuable information about anatomical characteristics and the risk of rupture. The XGBoost algorithm is renowned for its capability to capture intricate interactions and nonlinear relationships among variables, which likely contributed to its enhanced performance in this study.
Two studies [7, 14] achieved the best performance by employing ANN models. In the study by Hu et al. [14], significant predictors were CT value of subarachnoid hemorrhage, white blood cell count, neutrophil count, CT value of cerebral edema, and monocyte count. Similarly, Savarraj et al. [7] attained the highest results by incorporating a combination of electronic medical record variables, such as age, hemoglobin, sodium, white blood cell count, platelets, creatinine, and the clinician-derived Hunt–Hess score, in their ANN model.
LR model revealed that high-middle cerebral artery velocity collected on day 3 after SAH was a more influential predictor for DCI compared with epileptiform abnormalities (day 3) [23]. However, the Hunt–Hess score alone did not perform as well as other features. Among the ML models, the multitrajectory feature (day 3) outperformed the epileptiform abnormalities trajectory feature (day 3). These findings highlight the importance of high-middle cerebral artery velocity and multitrajectory in DCI prediction, suggesting their superiority over Hunt–Hess score and epileptiform abnormalities trajectory features.
One study [15] observed promising results in the application of RF and ensemble classifier. The model’s training incorporated standard vital sign measurements (heart rate, blood pressure, respiratory rate, and oxygen saturation) alongside routine demographic data collected for clinical purposes, such as age, sex, modified Fisher score, World Federation of Neurological Surgeons scale, Hunt–Hess grade, and GCS at Neurological Intensive Care Unit Admission.
Finally, one study [5] combined clinical variables with extracted image features using RFc (random forest classifier). The most relevant features, in order of importance, included image features, total brain volume, presence of intraparenchymal blood, time from ictus to CT, age, aneurysm height, presence of subdural blood, aneurysm width, and GCS.
Timing Impact on DCI Prediction Model Performance
With respect to the relationship between the timing of DCI prediction and the performance of models, five studies did not provided information on the relationship between the timing of DCI prediction and the performance of the DCI prediction models [5, 7, 12, 14, 34]. However, one study reported that the model using data from the DCI to 12 h before the onset of DCI had the best performance [15].
Quality Assessment and Risk of Bias
Regarding quality assessment and risk of bias, the results according to QUADAS-2 guidelines are shown in “Supplemental Table 1.” Only one study [14] had a low overall risk of bias. Three [5, 12, 15] out of six articles received an unclear risk of bias score for not clarifying whether the index test results were interpreted without knowledge of the results of the reference standard. Two studies [7, 13] had a high risk of bias because they failed to describe their study population (patient selection) or had inappropriate exclusions. However, apart from that, the majority of the four domains scored low risk of bias in all studies.
Discussion
We conducted a prospectively registered systematic review and meta-analysis of literature comparing LR and ML algorithms for predicting DCI with SAH in a cohort of 1828 patients. Our results suggest that ML models show promise for outperforming LR models. ML models exhibited slightly higher pooled sensitivity and specificity, which indicate that they may be more effective in identifying at-risk patients. Additionally, some ML models achieved substantially higher AUROC values, implying greater overall accuracy.
ML algorithms are a relevant and promising theme not only for neurosurgery but also for the entirety of medicine, seeing that it might provide a stronger approach to guide clinical decision-making. Despite the use of LR in predicting DCI, its use in analyzing complex and large datasets is limited, as this method assumes a linear association between predictors and the outcome variable, which is not always applicable [10]. Although ML algorithms, such as RF and ANN, have been proposed as an alternative to LR for prognosticating mortality in sepsis, their application in DCI predictions needs more research. Most previous studies investigating the use of ML for predicting DCI have not conducted a comprehensive analysis encompassing comparisons with LR. As an illustration, De Jong et al. [6] and Tanioka et al. [11] analyzed the diagnostic of DCI after SAH using ML algorithms but they did not provide a comparison with the performance of LR. To the best of our knowledge, this is the first systematic review and meta-analysis directly comparing LR and ML forecasting performance in the context of DCI following SAH.
The discussion of specific scenarios or contexts in which certain models may exhibit greater effectiveness than others is critical. The choice of ML or regression models should align with the characteristics and variables available in the study setting. For instance, one study identified CT value of SAH, white blood cell count, neutrophil count, CT value of cerebral edema, and monocyte count as significant predictors [14]. Similarly, three studies underscored the relevance of specific clinical variables such as clinical scores, aneurysm treatment, middle cerebral artery peak systolic velocities, and the presence of epileptiform abnormalities. In both cases, employing nonlinear ML models, specifically ANN, is more appropriate for accommodating the intricacies associated with these clinical predictors [5, 12, 23]. Conversely, one study highlighted the significance of demographic and laboratory test variables, including age, hemoglobin, sodium, white blood cell count, platelets, and creatinine [7]. Within this particular context, linear regression models offer enhanced suitability in capturing the linear relationships between these variables and the occurrence of DCI. Furthermore, some models employed specific clinical variables such as clinical scores, aneurysm treatment, middle cerebral artery peak systolic velocities, and the presence of epileptiform abnormalities [5, 12, 23]. In such cases, the incorporation of these variables into ML models, particularly ANN, is more appropriate for accommodating the intricacies associated with these clinical predictors.
Despite our significant findings, this study has some limitations related to the heterogeneity of the results, whose potential sources were identified by a meta-regression analysis. First, the selected studies have different designs; some are retrospective [5, 7, 12] whereas others are prospective [13,14,15]. Second, they have a lot of differences in their patient populations, including variations in the number of patients involved, the type of SAH (aneurysmal or nonaneurysmal), and the location of medical centers involved, which can impact heterogeneity through differences in inclusion criteria, characteristics of populations, health care systems, environmental factors, and treatment protocols. Third, there is a significant difference in the time point of DCI prediction, DCI diagnostic criteria, and the covariates used for it among the studies.
Notwithstanding these limitations, the combined analysis of nearly 2000 patients from six studies represents a considerable increase in statistical power when compared with individual studies, as it provides a more comprehensive and robust evaluation of the predictive performance of LR and ML algorithms for predicting DCI after SAH. To advance the application of predictive models for DCI, various research directions should be explored. Firstly, it is imperative to standardize the time frame for prediction and the selection of variables across studies, ensuring comparability and reproducibility of findings. Additionally, the timing of DCI prediction should be reported, as this information can provide valuable insights into the temporal sensitivity of the included features.
The enhancement of statistical power and the broadening of the generalizability of developed models can be achieved through the augmentation of sample size in future studies. Moreover, the exploration of additional predictors and variables beyond the currently employed demographic, clinical, and radiographic characteristics has the potential to offer valuable insights into the underlying mechanisms and risk factors of DCI.
Lastly, we highly recommend conducting clinical interventional trials following the Standard Protocol Items: Recommendations for Interventional Trials—Artificial Intelligence and Consolidated Standards of Reporting Trials—Artificial Intelligence guidelines to assess the effectiveness of ML-based decision support systems.
Conclusions
For patients with SAH, ML models performed slightly better than LR models. These findings imply that ML algorithms have the potential to surpass traditional statistical methods in this context. However, further research is required to explore the different techniques of ML and whether patients’ characteristics, data, and diagnostic criteria used for detection could affect their performance. Overall, this meta-analysis provides valuable insights into the use of artificial intelligence in medical research and highlights the potential benefits of these methods for improving patient outcomes.
References
Macdonald RL. Delayed neurological deterioration after subarachnoid haemorrhage. Nat Rev Neurol. 2014;10(1):44–58. https://doi.org/10.1038/nrneurol.2013.246.
Francoeur CL, Mayer SA. Management of delayed cerebral ischemia after subarachnoid hemorrhage. Crit Care. 2016;20(1):277. https://doi.org/10.1186/s13054-016-1447-6.
Tu JV. Advantages and disadvantages of using artificial neural networks versus logistic regression for predicting medical outcomes. J Clin Epidemiol. 1996;49(11):1225–31. https://doi.org/10.1016/s0895-4356(96)00002-9.
Jordan MI, Mitchell TM. Machine learning: trends, perspectives, and prospects. Science. 2015;349(6245):255–60. https://doi.org/10.1126/science.aaa8415.
Ramos LA, van der Steen WE, Sales Barros R, Majoie CBLM, van den Berg R, Verbaan D, Vandertop WP, Zijlstra IJAJ, Zwinderman AH, Strijkers GJ, Olabarriaga SD, Marquering HA. Machine learning improves prediction of delayed cerebral ischemia in patients with subarachnoid hemorrhage. J Neurointerv Surg. 2019;11(5):497–502. https://doi.org/10.1136/neurintsurg-2018-014258.
De Jong G, Aquarius R, Sanaan B, Bartels RHMA, Grotenhuis JA, Henssen DJHA, Boogaarts HD. Prediction models in aneurysmal subarachnoid hemorrhage: forecasting clinical outcome with artificial intelligence. Neurosurgery. 2021;88(5):E427–34. https://doi.org/10.1093/neuros/nyaa581.
Savarraj JPJ, Hergenroeder GW, Zhu L, Chang T, Park S, Megjhani M, Vahidy FS, Zhao Z, Kitagawa RS, Choi HA. Machine learning to predict delayed cerebral ischemia and outcomes in subarachnoid hemorrhage. Neurology. 2021;96(4):e553–62. https://doi.org/10.1212/WNL.0000000000011211.
Zhang D, Wang Y, Zhou L, Yuan H, Shen D. Alzheimer’s disease neuroimaging initiative. Multimodal classification of Alzheimer’s disease and mild cognitive impairment. Neuroimage. 2011;55(3):856–67. https://doi.org/10.1016/j.neuroimage.2011.01.008.
Syeda-Mahmood T, et al. Identifying patients at risk for aortic stenosis through learning from multimodal data. Medical Image computing and computer-assisted intervention—MICCAI 2016. MICCAI 2016. Lecture Notes in Computer Science(), vol 9902. Springer, Cham. https://doi.org/10.1007/978-3-319-46726-9_28
Ranganath R, Gerrish S, Blei DM. Deep survival analysis. In: Proceedings of the 32nd international conference on machine learning, 2016; pp. 2079–2088. https://cims.nyu.edu/~rajeshr/papers/Ranganath_DeepSurvival2016.pdf
Tanioka S, Ishida F, Nakano F, Kawakita F, Kanamaru H, Nakatsuka Y, Nishikawa H, Suzuki H, pSEED group. Machine learning analysis of matricellular proteins and clinical variables for early prediction of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Mol Neurobiol. 2019;56(10):7128–35. https://doi.org/10.1007/s12035-019-1601-7.
Alexopoulos G, Zhang J, Karampelas I, Khan M, Quadri N, Patel M, Patel N, Almajali M, Mattei TA, Kemp J, Coppens J, Mercier P. Applied forecasting for delayed cerebral ischemia prediction post subarachnoid hemorrhage: methodological fallacies. Inform Med Unlock. 2022;28:100817. https://doi.org/10.1016/j.imu.2021.100817.
Chen HY, Elmer J, Zafar SF, Ghanta M, Moura Junior V, Rosenthal ES, Gilmore EJ, Hirsch LJ, Zaveri HP, Sheth KN, Petersen NH, Westover MB, Kim JA. Combining transcranial doppler and EEG data to predict delayed cerebral ischemia after subarachnoid hemorrhage. Neurology. 2022;98(5):e459–69. https://doi.org/10.1212/WNL.0000000000013126.
Hu P, Li Y, Liu Y, Guo G, Gao X, Su Z, Wang L, Deng G, Yang S, Qi Y, Xu Y, Ye L, Sun Q, Nie X, Sun Y, Li M, Zhang H, Chen Q. Comparison of conventional logistic regression and machine learning methods for predicting delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage: a multicentric observational cohort study. Front Aging Neurosci. 2022;17(14):857521. https://doi.org/10.3389/fnagi.2022.857521.
Megjhani M, Terilli K, Weiss M, Savarraj J, Chen LH, Alkhachroum A, Roh DJ, Agarwal S, Connolly ES Jr, Velazquez A, Boehme A, Claassen J, Choi HA, Schubert GA, Park S. Dynamic detection of delayed cerebral ischemia: a study in 3 centers. Stroke. 2021;52(4):1370–9. https://doi.org/10.1161/STROKEAHA.120.032546.
Schmidt J, Marques MRG, Botti S, et al. Recent advances and applications of machine learning in solid-state materials science. N Engl J Med. 2019;5(1):83. https://doi.org/10.1038/s41524-019-0221-0.
Obermeyer Z, Emanuel EJ. Predicting the future: big data, machine learning, and clinical medicine. N Engl J Med. 2016;375(13):1216–9. https://doi.org/10.1056/NEJMp1606181.PMID:27682033;PMCID:PMC5070532.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. https://doi.org/10.1146/annurev.clinpsy.121208.131413.
Saadatfar H, Khosravi S, Joloudari JH, Mosavi A, Shamshirband S. A new K-nearest neighbors classifier for big data based on efficient data pruning. N Engl J Med. 2020;8(2):286. https://doi.org/10.3390/math8020286.
Reifman J, Feldman EE. Multilayer perceptron for nonlinear programming. Comput Oper Res. 2002;29(9):1237–50. https://doi.org/10.1016/S0305-0548(01)00027-2.
Strobl C, Boulesteix AL, Zeileis A, Hothorn T. Bias in random forest variable importance measures: illustrations, sources and a solution. BMC Bioinform. 2007;25(8):25. https://doi.org/10.1186/1471-2105-8-25.
Cortes C, Vapnik V. Support vector networks. Mach Learn. 1995;20(3):273–97. https://doi.org/10.1007/BF00994018.
Chen T, Guestrin C. XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining, 2016; pp. 785–794. https://doi.org/10.1145/2939672.2939785
Funding
This work was not supported by any grant.
Author information
Authors and Affiliations
Contributions
LSS: selection of studies, data collection, statistical analysis, and manuscript writing. JBCD: selection of studies, data collection, risk of bias, and manuscript writing. NNR: supervision and manuscript review. MJT: supervision and manuscript review. EGF: supervision and manuscript review. JPMT: statistical analysis, supervision, and manuscript review. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval/Informed Consent
All authors confirm adherence to ethical guidelines—no data, including images, have been falsified or manipulated to support our conclusions—and the use of a reporting checklist for systematic reviews and meta-analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santana, L.S., Diniz, J.B.C., Rabelo, N.N. et al. Machine Learning Algorithms to Predict Delayed Cerebral Ischemia After Subarachnoid Hemorrhage: A Systematic Review and Meta-analysis. Neurocrit Care 40, 1171–1181 (2024). https://doi.org/10.1007/s12028-023-01832-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01832-z