Abstract
Background
Conflicting data exist regarding the association of perihematomal edema (PHE) with outcomes after intracerebral hemorrhage (ICH). We performed a post hoc analysis of the ICH Deferoxamine trial to examine whether an early change in ventricular size (VS), as a composite measure of PHE growth and mass effect, intraventricular hemorrhage, and hydrocephalus, is a more accurate predictor of outcome than PHE measures alone.
Methods
Computerized tomography scans were performed at baseline and after 72–96 h. We evaluated measures of PHE and change in VS as predictors of outcome, assessed by a dichotomized modified Rankin Scale score (0–2 versus 3–6), primarily at 90 days and secondarily at 30 days. A multivariable logistic regression model was fitted for each predictor, with adjustment for the same confounders.
Results
A total of 248 participants were included after we excluded those requiring external ventricular drains. On univariate analyses, older age, female sex, lower Glasgow Coma Scale score and baseline temperature, greater ICH volume, absolute PHE volume, edema extension distance at presentation, lesser changes in relative PHE volume and edema extension distance, and an increase in VS were associated with poor outcome. In multivariable analyses, only the increase in VS was associated with lower odds of modified Rankin Scale scores 0–2 at 90 days (odds ratio 0.927, 95% confidence interval 0.866–0.970, p = 0.001) and 30 days (odds ratio 0.931, 95% confidence interval 0.888–0.975, p = 0.003).
Conclusions
Within the context of a randomized controlled trial with standardized imaging and functional assessments, we did not find significant associations between measures of PHE and outcome but documented an independent association between early increase in VS and lower odds of good clinical outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Various clinical markers have been proposed for outcome prognostication in patients with intracerebral hemorrhage (ICH) on the basis of the pathophysiology of the injury, including age, hematoma volume and growth, ICH location, and presence of intraventricular hemorrhage (IVH) [1,2,3,4,5,6,7]. Emerging evidence in recent years suggests that perihematomal edema (PHE) may be a potential predictor of functional outcome as well. However, studies examining the relationship between PHE and outcomes after ICH have yielded conflicting results [8,9,10,11]. These inconsistent observations may be related to variabilities in study design, patient selection, parameters used to measure PHE, and the time points of PHE and outcome assessments. This prompted us to investigate the relationship between PHE, along with its associated measures, and clinical outcomes within the context of the ICH Deferoxamine (iDEF) trial, a randomized, double-blind, multicenter study with uniform and standardized imaging and clinical assessment procedures [12]. We hypothesized that change in ventricular size (VS), resulting from PHE growth, presence of IVH, and hydrocephalus, is a more accurate predictor of outcome than PHE measures alone.
Methods
Study Design and Participants
The iDEF trial was a prospective, multicenter, multinational, placebo-controlled, double-blind phase two clinical trial that recruited 294 patients with primary, spontaneous, and supratentorial ICH; details of the study design, methods, and main results have been published elsewhere [12]. Briefly, participants were randomized 1:1 to receive deferoxamine (32 mg/kg/day) or placebo (saline) infusions for three consecutive days, starting within 24 h of the onset of ICH. A computerized tomography (CT) scan of the brain was performed for all eligible participants on presentation to confirm the diagnosis of ICH, and a second CT scan of the brain was obtained within 24 h of completion of the last infusion (i.e., within 72–96 h from ICH onset). The modified Rankin Scale (mRS) was assessed at various time points, including 30 and 90 days after ICH, by qualified investigators certified in mRS administration and blinded to treatment assignment. The trial was approved by the institutional review boards at participating sites, and written informed consent was obtained from each participant or legally authorized representative. Eligible participants were aged 18–80. The main exclusion criteria included infratentorial ICH, suspected secondary causes of the hemorrhage, kidney failure or coagulopathy, planned hematoma evacuation, and pre-existing do not resuscitate or do not intubate status or anticipation of withdrawal of medical care within the first 72 h after presentation. For the present analysis, we excluded patients who had an external ventricular drainage (EVD) system placed at any point because EVD can influence the VS and confound relevant measurements. Both patients and controls for the iDEF study were included in this study.
Imaging Analyses
All CT scans were sent to the iDEF core imaging laboratory (Beth Israel Deaconess Medical Center, Boston, MA) for central review by experienced raters blinded to clinical data and treatment assignment to confirm the ICH location and presence of IVH and to perform volumetric measurements of ICH, PHE, and ventricles using an imaging analysis software (Analyze 11.0 Visualization and Analysis Software for Medical Imaging; AnalyzeDirect, Overland Park, KS). Areas of the hemorrhage and PHE were automatically delineated by imaging analysis software with the use of density thresholds on each slice, followed by manual correction using a semiautomated edge detection tool up to an absolute maximum of 35 HU to obtain the best delineation of the PHE. The boundaries of the PHE area were adjusted further after inspection of the three orthogonal planes in the software’s volume edit module, which allows for better assessment of the location and distribution of each lesion beyond the two-dimensional axial plane. When delineating PHE, the following additional principles were applied to avoid potential artifacts related to old infarcts or leukoaraiosis: (1) the PHE area should be more hypodense than the corresponding region in the contralateral hemisphere, and (2) the most hypodense areas immediately surrounding the hemorrhage should be used. The software provided total volume measurements for ICH, IVH, and PHE by summing up the volumes from all respective slices. The interrater and intrarater reliability of this methodology have been previously validated [13]. The total ventricular volume (lateral, third, and fourth ventricles) was measured, and we calculated the following parameters for PHE: absolute PHE (aPHE), defined as the sum total of pixels of the perihematomal lesion; relative PHE (rPHE), the ratio of aPHE to hematoma lesion; and edema extension distance (EED), the difference between the radius of a sphere equal to the aPHE volume and the radius of a sphere equal to the ICH volume alone [11, 14].
Statistical Analysis
Continuous variables were summarized with the mean and standard deviation for normally distributed variables and median and interquartile range for variables not following a normal distribution. Categorical variables were reported as absolute counts and percentages of the total. In univariable analyses, we used Student’s t-test and the Wilcoxon rank-sum test for normally and nonnormally distributed continuous variables, respectively. For categorical variables, the χ2 test was used. The primary outcome measure was good clinical outcome, defined as a dichotomized mRS score of 0–2 at day 90. We fitted a multivariable logistic regression model for VS and various measures of PHE, adjusting for the variables that reached statistical significance in independent univariable analyses: age, female sex, presence of IVH, baseline hematoma volume, prior use of antiedema medication (hypertonic saline and/or mannitol), Glasgow Coma Scale (GCS) score at presentation, and baseline temperature. We also performed similar secondary analyses using an mRS score of 0–2 at day 30 as early good clinical outcome. To account for multiple testing, the significance threshold for the multivariable analyses was set at 0.0056 using the Bonferroni correction. All statistical analyses were performed using JMP Pro 15.0.0.
Results
Of the 254 study participants without an EVD placement, a total of 248 participants were included in the primary analysis, and 252 were included in the secondary analysis because six study participants did not have mRS scores available at 90 days and two study participants did not have mRS scores available at 30 days. In the primary analysis, the mean age was 60.8 ± 11.6 years, and 95 (37.4%) study participants were women. Supplemental Table 1 summarizes the baseline characteristics of the participants who were included (those without EVD placement) and excluded (those with EVD placement). Of the patients who were excluded (n = 39), 34 had EVD placement before the repeat CT scan on day 4 and five had EVD placement sometime after the repeat scan. Expectedly, higher proportions of included patients were not on antiedema medications prior to randomization and had higher GCS scores on presentation, lower prevalence and smaller volume of IVH, smaller VS on the baseline scan and change in VS on the repeat scan, and greater change in rPHE from baseline to repeat scans. Age, female sex, and prevalence of comorbidities were comparable between included and excluded cohorts.
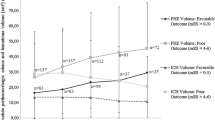
Table 1 summarizes the baseline clinical and imaging characteristics of included study participants on the basis of mRS scores, dichotomized into 0–2 versus 3–6 at 90 and 30 days. On univariate analyses, younger age, male sex, absence of prior use of antiedema agents, lower National Institutes of Health Stroke Scale (NIHSS) score at screen and post infusion, higher GCS score at screen and post infusion, lower baseline temperature, smaller baseline ICH volume, decrease in VS, greater changes in rPHE volume and EED between admission and follow-up scans, and smaller aPHE volume and EED at presentation were associated with good clinical outcome at 90 days. At 30 days, lower NIHSS score at screen and post infusion, higher GCS score at post infusion, smaller baseline ICH volume, lower proportion of presence of IVH, decrease in VS, and smaller aPHE volume at presentation were associated with good clinical outcome. Table 2 shows the location of ICH in patients with increase in VS and decrease/no change in VS. Although higher proportions of study participants had thalamic or deep/nonthalamic locations of ICH, this did not reach statistical significance. Figures 1 and 2 illustrate the distributions mRS scores at 30 and 90 days in the increase in VS versus decrease/no change in VS. Only the increase in VS from admission to 72- to 96-h scans was independently associated with lower odds of good clinical outcome on multivariable logistic regression analysis at 90 days (odds ratio 0.927; 95% confidence interval 0.886–0.970) and at 30 days (odds ratio 0.931; 95% confidence interval 0.888–0.975) (Table 3). None of the measures of PHE was significantly associated with 90-day clinical outcome on multivariable analyses.
Discussion
In this post hoc analysis of the iDEF trial of patients with spontaneous ICH without EVD placement, early increase in VS within 96 h of ICH onset was associated with lower odds for good clinical outcome at 90 and 30 days. Conversely, we did not find an independent association between early growth of PHE, using several measures and parameters, and clinical outcome at either 90 or 30 days. These findings suggest that change in VS may be a more accurate predictor of outcome than PHE after ICH.
VS is influenced by several pathophysiological processes, which impact clinical outcomes after ICH. These include mass effect from the hematoma and PHE, presence and volume of IVH, and resulting hydrocephalus. Therefore, it is logical that the prognostic significance of VS exceeds that of these individual factors. We cannot exclude the possibility that the observed association between VS and clinical outcome may be related to the IVH-mediated inflammatory response or secondary injury mediated by blood and its degradation products in the hematoma region and intraventricular space. However, because PHE is often considered as a surrogate radiological measure of secondary injury after ICH, the lack of an association between various measures of PHE and outcome suggests that VS played a greater role in our study; the sum may be better than its parts.
Previous studies have shown that increased ventricular compression and midline shift as indirect markers of mass effect are associated with poor outcomes and mortality after ischemic stroke and ICH [9,10,11]. Our main finding of an association between VS enlargement, as opposed to compression, and poor clinical outcome may seem discordant with these observations. However, these studies only assessed the displacement of the outer wall or the volume of the lateral ventricle ipsilateral to the lesion and not the entire VS. We postulate that our findings may represent early hydrocephalus, which may be attributed to obstruction of cerebrospinal fluid outflow by the presence of IVH. ICH locations influence the development of hydrocephalus, with thalamic and deep/nonthalmic hemorrhages causing obstructive hydrocephalus via mass effect on the third ventricle or with association with IVH, leading to communicating hydrocephalus. Mortality and poor functional outcomes are associated with ICH in posterior internal capsule, thalamus, and infratentorial locations, likely related to their tendencies to lead to hydrocephalus [15, 16]. Similar findings can be seen among the included study participants of our study. Though not statistically significant, a higher proportion of those with positive VS change had thalamic or deep/nonthalamic locations of ICH. The mechanism seen in the included study participants may be from communicating hydrocephalus because compared with those with decrease in VS from screening to repeat scan, those with increase in VS had higher proportions of the presence of IVH, which trended toward significance (Supplemental Table 2). This is consistent with previous reports, indicating that the presence of IVH is associated with increased mortality and poor clinical outcomes [15, 16].
We noted a small increase of approximately 2 cm3 in VS in the poor outcome group. This may seem too modest to result in worsening outcomes. There are several potential explanations. First, the direction of change, rather than the absolute difference in VS, may be more relevant. Second, the location of the increase in VS may be significant because an increase in the third or fourth ventricle could suggest more significant hydrocephalus than a similar increase in the lateral ventricles. Third, we only assessed VS on baseline and day 4 scans; therefore, one cannot rule out that the observed early increase in VS may have been a marker of subsequent continued growth in VS, which in turn impacted long-term 90-day outcomes. Fourth, the observed association between increased VS and poor outcome may be partly related to the secondary consequences of IVH-mediated inflammatory response and secondary injury [17].
On the univariate analysis, those with better functional outcome (mRS score ≤ 2) both at 90 and 30 days had lower initial ICH volume, a previously shown parameter correlated with functional outcome [1]. Accordingly, study participants with better functional outcome on both days also had lower aPHE volume at screen but not consistently with other related measures of PHE, such as rPHE and EED. Furthermore, ICH volume at screen was included in the multivariable model as a confounder. This leads us to believe that the higher odds of poor outcome for those with higher change in VS is beyond just secondary injury mechanism related to PHE pathophysiology. The initial injury and mass effect from hematoma expansion likely contributed to our findings because change in ICH volume from screen to postinfusion scan trended toward significance in the multivariable model.
Though expected, patients with poor clinical outcomes at 90 and 30 days showed interim improvements from screen to post infusion but still maintained lower GCS scores and higher NIHSS scores compared with those who achieved good outcomes. Similarly, there was no significant differences in the IVH volume at screen and change in IVH volume from screen to post infusion. We believe that these findings may be secondary to the exclusion of those who required EVD placement. Although these findings may seem to contradict previous findings that only large IVH volumes portend poor clinical outcomes in those with ICH, the presence of any IVH was also shown to be associated with poor clinical outcomes [6, 15, 18].
We did not find significant associations between various measures of PHE and clinical outcomes. This contrasts with findings from some previous studies, albeit in line with the overall conflicting body of literature on the relationship between PHE and clinical outcomes [1,2,3,4,5,6,7,8,9,10,11]. These inconsistent reports may be related to variabilities in study design, patient selection, parameters and methods used to measure PHE, lack of adjustments for the use of antiedema agents, and the time points of PHE and outcome assessments between various studies. Our radiographic measures of PHE were based on CT scans because magnetic resonance imaging was not required in the iDEF trial. The delineation of PHE may be more accurate on magnetic resonance imaging, and this may have influenced quantitative PHE measures in some cases. However, we used a systematic and semiautomated Hounsfield unit threshold-based approach to minimize this limitation [19, 20]. Though it may not ultimately affect the clinical outcome, hyperosmolar therapy (e.g., hypertonic saline, mannitol) reduces the development of cerebral edema and is commonly used to manage increased intracranial pressure in the setting of cerebral edema [21]. Because the iDEF trial did not record the study participant’s sodium levels and distinguish between those who received hyperosmolar therapy and which type, it remains a possibility that serum sodium and osmolarity could have confounded the result, although the use of hyperosmolar therapy (labeled as “antiedema therapy” in the main trial) was one of the confounding variables included in our analyses.
Our analyses of PHE were conducted within the context of a prospective trial with standardized imaging and clinical assessment procedures by experienced and blinded assessors. Furthermore, we simultaneously examined various parameters of PHE within the same cohort. Our findings suggest that the association between PHE and its growth and clinical outcome is modest at best. However, these findings should be interpreted with caution for the following reasons. First, our study is a post hoc analysis, and the iDEF trial was not specifically powered to examine the association between PHE and clinical outcomes. Second, the impact of treatment with deferoxamine on our findings cannot be excluded. Previous studies have shown that treatment with deferoxamine can reduce the growth of PHE and resolution of hematoma [22]. However, we previously reported that treatment with deferoxamine had no effect on relative PHE growth in the iDEF trial [12].
In addition to the preceding limitations, the main trial was not powered to address the main hypothesis of the current analysis. The iDEF trial excluded patients in whom there was an indication that care may be withdrawn within the first 72 h after ICH. This, together with the exclusion of enrolled patients with EVD placements from this analysis, may have introduced some bias and limits the generalizability of our findings. Patients included in this study were relatively young, in their 60 s, and had relatively small-to-moderate-sized hemorrhages, which further limits generalizability to older patients with larger ICHs. We only assessed PHE evolution up to 96 h after ICH onset. Thus, there lies a possibility of having missed the ability to assess the full spectrum of PHE evolution and more delayed consequences, although observational studies have shown that PHE growth peaks by the second week [19]. In addition, other studies have shown that (1) PHE growth is fastest during the first 2 days, (2) early PHE growth correlates with early neurological worsening (within the first few days), and (3) delayed PHE growth does not correlate with long-term outcomes [19, 23]. Although we adjusted our analyses for multiple testing, the potential impact of multiplicity on reported findings cannot be ruled out. Our results, therefore, are considered hypothesis generating. The strengths of our study lie in the vigorous methodology of the main trial and its standardized assessments within a prespecified protocol and central blinded analyses of all imaging data by experienced raters.
Conclusions
Within the context of a randomized controlled trial with standardized imaging and functional assessments, we did not find significant associations between various measures of PHE growth during the first 96 h after ICH and functional outcomes but documented an independent association between early increase in VS and lower odds of favorable outcome. Further investigations are required to confirm our findings and to determine whether the treatment of even a minor ventricular enlargement during the first few days after ICH is warranted to influence outcomes.
Source of Support
The iDEF trial was funded by the National Institute of Neurological Disorders and Stroke (U01 NS074425). Dr. Magdy Selim receives funding from the National Institute of Neurological Disorders and Stroke and National Institute on Aging (U01 NS102289 and UF1 NS120871). Dr. Vasileios-Arsenios Lioutas receives funding from National Institute of Neurological Disorders and Stroke grants U01 NS102289 and R01 NS017950.
References
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral haemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24(7):987–93. https://doi.org/10.1161/01.str.24.7.987.
Davis SM, Broderick J, Hennerici M, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66(8):1175. https://doi.org/10.1212/01.wnl.0000208408.98482.99.
Brian TA, Bennie WC, Walter LO, Lawrence HP. The effect of intracerebral hematoma location on the risk of brain-stem compression and on clinical outcome. J Neurosurg. 1988;69(4):518–22. https://doi.org/10.3171/jns.1988.69.4.0518.
Sreekrishnan A, Dearborn JL, Greer DM, et al. Intracerebral Hemorrhage location and functional outcomes of patients: a systematic literature review and meta-analysis. Neurocrit Care. 2016;25(3):384–91. https://doi.org/10.1007/s12028-016-0276-4.
Christensen Michael C, Mayer S, Ferran J-M. Quality of Life After Intracerebral Hemorrhage. Stroke. 2009;40(5):1677–82. https://doi.org/10.1161/STROKEAHA.108.538967.
Roeder SS, Sprügel MI, Sembill JA, et al. Influence of the extent of intraventricular hemorrhage on functional outcome and mortality in intracerebral hemorrhage. Cerebrovasc Dis. 2019;47(5–6):245–52. https://doi.org/10.1159/000501027.
Delcourt C, Huang Y, Arima H, et al. Hematoma growth and outcomes in intracerebral hemorrhage. Neurology. 2012;79(4):314. https://doi.org/10.1212/WNL.0b013e318260cbba.
Ironside N, Chen CJ, Ding D, Mayer SA, Connolly ES Jr. Perihematomal edema after spontaneous intracerebral hemorrhage. Stroke. 2019;50(6):1626–33. https://doi.org/10.1161/strokeaha.119.024965.
Murthy SB, Moradiya Y, Dawson J, et al. Perihematomal edema and functional outcomes in intracerebral hemorrhage. Stroke. 2015;46(11):3088–92. https://doi.org/10.1161/STROKEAHA.115.010054.
Grunwald Z, Beslow LA, Urday S, et al. Perihematomal edema expansion rates and patient outcomes in deep and lobar intracerebral hemorrhage. Neurocrit Care. 2017;26(2):205–12. https://doi.org/10.1007/s12028-016-0321-3.
Urday S, Beslow LA, Dai F, et al. Rate of perihematomal edema expansion predicts outcome after intracerebral hemorrhage. Crit Care Med. 2016;44(4):790–7.
Selim M, Foster LD, Moy CS, et al. Deferoxamine Mesylate in patients with intracerebral haemorrhage: a multi-center, randomised, double-blind, placebo-controlled, Phase II Trial. Lancet Neurol. 2019;18(5):428–38. https://doi.org/10.1016/S1474-4422(19)30069-9.
Mehdiratta M, Kumar S, Hackney D, Schlaug G, Selim M. Association between serum ferritin level and perihematoma edema volume in patients with spontaneous intracerebral hemorrhage. Stroke. 2008;39(4):1165–70. https://doi.org/10.1161/strokeaha.107.501213.
Selim M, Norton C. Perihematomal edema: implications for intracerebral hemorrhage research and therapeutic advances. J Neurosci Res. 2020;98(1):212–8. https://doi.org/10.1002/jnr.24372.
Bhattathiri PS, Gregson B, Prasad KS, Mendelow AD. Intraventricular hemorrhage and hydrocephalus after spontaneous intracerebral hemorrhage: results from the STICH trial. Acta Neurochir Suppl. 2006;96:65–8. https://doi.org/10.1007/3-211-30714-1_16.
Delcourt C, Sato S, Zhang S, et al. Intracerebral hemorrhage location and outcome among INTERACT2 participants. Neurology. 2017;88(15):1408–14. https://doi.org/10.1212/wnl.0000000000003771.
Garton T, Keep RF, Wilkinson DA, et al. Intraventricular hemorrhage: the role of blood components in secondary injury and hydrocephalus. Transl Stroke Res. 2016;7(6):447–51. https://doi.org/10.1007/s12975-016-0480-8.
Tuhrim S, Horowitz DR, Sacher M, Godbold JH. Volume of ventricular blood is an important determinant of outcome in supratentorial intracerebral hemorrhage. Crit Care Med. 1999;27(3):617–21. https://doi.org/10.1097/00003246-199903000-00045.
Urday S, Beslow LA, Goldstein DW, et al. Measurement of perihematomal edema in intracerebral hemorrhage. Stroke. 2015;46(4):1116–9. https://doi.org/10.1161/strokeaha.114.007565.
Volbers B, Staykov D, Wagner I, et al. Semi-automatic volumetric assessment of perihemorrhagic edema with computed tomography. Eur J Neurol. 2011;18(11):1323–8. https://doi.org/10.1111/j.1468-1331.2011.03395.x.
Cook AM, Morgan Jones G, Hawryluk GWJ, et al. Guidelines for the acute treatment of cerebral edema in neurocritical care patients. Neurocrit Care. 2020;32(3):647–66. https://doi.org/10.1007/s12028-020-00959-7.
Yu Y, Zhao W, Zhu C, et al. The clinical effect of deferoxamine mesylate on edema after intracerebral hemorrhage. PLoS ONE. 2015;10(4):e0122371. https://doi.org/10.1371/journal.pone.0122371.
Inaji M, Tomita H, Tone O, Tamaki M, Suzuki R, Ohno K. Chronological changes of perihematomal edema of human intracerebral hematoma. Acta Neurochir Suppl. 2003;86:445–8. https://doi.org/10.1007/978-3-7091-0651-8_91.
Author information
Authors and Affiliations
Consortia
Contributions
Dr. Kun He Lee and Dr. Vasileios-Arsenios Lioutas made substantial contributions in the analysis and interpretation of data as well as in drafting and revising the manuscript. Dr. Sarah Marchina made significant contributions in acquisition of the data for the manuscript’s parent study, the iDEF trial, and critical revisions of the manuscript. Dr. Magdy Selim was critical in the conception and design of this study and made important contributions in the manuscript and its revisions. All authors approved the final version of the manuscript for its submission and publication and agreed to be accountable for the manuscript’s integrity and accuracy.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Magdy Selim receives grant funding from the National Institute of Neurological Disorders and Stroke (related to and outside of the current work) and royalties from Up to Date and Cambridge University Press. He serves on the Advisory Board of MedRhythms, Inc. Dr. Vasileios-Arsenios Lioutas receives grant funding from the National Institute of Neurological Disorders and Stroke (related to and outside of the current work) and consulting fees from Qmetis. Drs. Sarah Marchina and Kun He Lee declare no potential conflicts of interest.
Ethical Approval/Informed Consent
Institutional review board approval was obtained for this article’s parent study, the iDEF trial.
Clinical Trial Registration
ClinicalTrials.gov identifier: NCT02175225 (https://clinicaltrials.gov/ct2/show/NCT02175225).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, K.H., Lioutas, VA., Marchina, S. et al. The Prognostic Roles of Perihematomal Edema and Ventricular Size in Patients with Intracerebral Hemorrhage. Neurocrit Care 37, 455–462 (2022). https://doi.org/10.1007/s12028-022-01532-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01532-0