Abstract
Background
Transcranial Doppler ultrasonography (TCD) is a portable, bedside, noninvasive diagnostic tool used for the real-time assessment of cerebral hemodynamics. Despite the evident utility of TCD and the ability of this technique to function as a stethoscope to the brain, its use has been limited to specialized centers because of the dearth of technical and clinical expertise required to acquire and interpret the cerebrovascular parameters. Additionally, the conventional pragmatic episodic TCD monitoring protocols lack dynamic real-time feedback to guide time-critical clinical interventions. Fortunately, with the recent advent of automated robotic TCD technology in conjunction with the automated software for TCD data processing, we now have the technology to automatically acquire TCD data and obtain clinically relevant information in real-time. By obviating the need for highly trained clinical personnel, this technology shows great promise toward a future of widespread noninvasive monitoring to guide clinical care in patients with acute brain injury.
Methods
Here, we describe a proposal for a prospective observational multicenter clinical trial to evaluate the safety and feasibility of prolonged automated robotic TCD monitoring in patients with severe acute traumatic brain injury (TBI). We will enroll patients with severe non-penetrating TBI with concomitant invasive multimodal monitoring including, intracranial pressure, brain tissue oxygenation, and brain temperature monitoring as part of standard of care in centers with varying degrees of TCD availability and experience. Additionally, we propose to evaluate the correlation of pertinent TCD-based cerebral autoregulation indices such as the critical closing pressure, and the pressure reactivity index with the brain tissue oxygenation values obtained invasively.
Conclusions
The overarching goal of this study is to establish safety and feasibility of prolonged automated TCD monitoring for patients with TBI in the intensive care unit and identify clinically meaningful and pragmatic noninvasive targets for future interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transcranial Doppler ultrasonography (TCD) is a portable, bedside, noninvasive diagnostic tool used for the real-time assessment of cerebral hemodynamics. The application of TCD in clinical practice was first described by Rune Aaslid et al. [1] in 1982 for real-time dynamic monitoring of cerebral blood flow (CBF) velocity (CBFV) using low frequency ultrasound probes. TCD measurement of CBFV provides a noninvasive surrogate of CBF and distal cerebrovascular resistance in the basal cerebral arteries. Seminal work from Brauer et al. [2] demonstrated a strong linear relationship between CBFV and CBF measured using xenon-enhanced computed tomography. This introduced TCD to clinical applications in the critical care settings because of its ability to identify dynamic pathophysiological changes that could indicate imminent secondary brain injury in patients with acute brain injury, such as the traumatic brain injury (TBI) [3, 4] or subarachnoid hemorrhage (SAH) [5]. Portable continuous TCD monitoring allows for multimodal assessment and frequent evaluation of trends in cerebral hemodynamics and thus has the potential to guide individualized targets for clinical management guided by noninvasive assessments of intracranial pressure (ICP), cerebral perfusion pressure (CPP), cerebral autoregulation (CA), and critical closing pressure (CrCP).
Real-time, automated software platforms have allowed for the integration of different clinical and systemic neuromonitoring modalities in neurocritical care research. For example, the Intensive Care Monitor, ICM + software (Cambridge Enterprise, Cambridge, UK), implemented in the early 2000s, is one such commonly used software platform that enables the monitoring and integration of multimodal bedside data, such as ICP, CPP, arterial blood pressure (ABP), brain tissue oxygenation (PbtO2), CBF, brain temperature, and microdialysis among other modalities, and provides clinically relevant parameters, such as pressure reactivity indices (PRx) [6,7,8], CrCP [9], brain compensatory reserve [10], and optimal CPP [11], using automated computerized algorithms. Such measures of continuous autoregulatory indices in acute TBI, including PRx [7, 12], and TCD-based indices—such as mean flow index (Mx), mean flow index Mx (Mx_a), systolic flow index (Sx), and systolic flow index Sx (Sx_a) [8]—have been shown to strongly correlate with 6-month outcomes and show promise as potential targets for goal-directed therapy (GDT) [6, 7, 13]. Further, Mx/Mx_a and Sx/Sx_a have shown good correlations with invasive PRx and can be used as noninvasive surrogates for this parameter [8]. CrCP is yet another TCD-derived parameter [9, 26] that is related to the vasomotor tone of the small cerebral vasculature and can provide useful information regarding the state of the cerebral hemodynamics and reflect changes in CPP [9, 24, 25, 27]. Because CPP is directly related to PbtO2, the study of CrCP could provide valuable correlation data with potential for clinical use.
Despite the proven role of TCD in clinical management and prognostication in diseases such as SAH and TBI [14, 15] and the integration of TCD-derived parameters using multimodality data analysis platforms such as ICM+, utilization continues to be low outside of a few specialized centers with technical and clinical expertise in neurosonography. For example, routine vasospasm screening with TCD is recommended in aneurysmal SAH (aSAH), but only 2% of hospitalized patients with aSAH undergo such evaluation, according to a nationwide survey from 2002 through 2011 [16]. Such low rates of TCD use for the management of acute brain injury such as aSAH and TBI are largely driven by the lack of robust scalable monitoring protocols and the lack of technical and clinical expertise required to perform and interpret the examination. Research so far in this field has been limited to algorithms that monitor a brief snapshot of fluctuating cerebrovascular hemodynamics, thereby limiting clinical utility in guiding care for these dynamic disease processes.
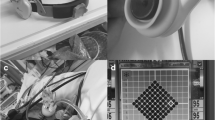
Recent innovations in TCD devices using robotic probes have facilitated the automated insonation of the middle cerebral artery (MCA). New technology provides the autocorrection of signal acquisition in real time, allowing access to automated prolonged monitoring of TCD parameters in facilities that would otherwise lack the resources and technical expertise required to perform and interpret these examinations [17, 18]. This technology provides real-time data visualization of clinically relevant variables that represent cerebral hemodynamics and obviate the need for a bedside, dedicated TCD technician. The artificial intelligence-guided technology automatically adjusts for high quality signal acquisition in case of displacements caused by movement, facilitating prolonged monitoring and is well suited to capture temporal fluctuations in cerebrovascular hemodynamics that correspond with the underlying dynamic pathobiological processes in TBI.
Although the overall safety of TCD monitoring technology has been well established, automated robotic TCD technology has only been tested in single center studies (Cambridge, UK) [17, 18], in patients with severe TBI undergoing multimodal neuromonitoring. Despite the general safety and feasibility, the effect of prolonged monitoring on brain temperature has not yet been investigated. In the United States, although automated robotic TCD monitoring device have demonstrated feasibility of a time-limited study in critically ill patients with aSAH with concomitant external ventricular drain and central venous lines [19], the safety profile with regards to the dislodgement of other concomitant invasive neuromonitors have not been investigated widely. The overall scalability and safety of this technology in obtaining clinically meaningful data across sites with varying TCD expertise has also yet to be explored. A widespread implementation of monitoring-based intervention protocols using automated TCD, particularly in resource-limited settings with a lack of invasive monitoring and neurosonography expertise, has the potential to bring a paradigm shift in the management of patients with acute TBI. Automated TCD data can inform TBI care, as protocols evolve from “one-size-fits-all” to patient-based precision medicine, guided by individual hemodynamics and cerebral physiology.
Evaluating the feasibility and safety of TCD-based prolonged cerebrovascular hemodynamic monitoring in critically ill patients with TBI and studying the TCD correlations with clinical parameters derived from standard, surgically implanted monitoring devices is the logical next step toward assessing the scalability, safety, and efficacy of prolonged automated TCD monitoring in patients with severe TBI. The overarching hypothesis of this project is that prolonged automated TCD monitoring is safe and feasible in the severe TBI population and can be used as a surrogate non-invasive measure of PbtO2.
Methods
Study Design
We propose an observational multicenter trial in patients with severe TBI admitted to critical care units in the United States performing invasive ICP, PbtO2, and brain temperature monitoring as part of the standard of care with varying degrees of TCD availability and experience. We seek to study the safety and feasibility of prolonged automated robotic TCD monitoring in patients with acute severe TBI and evaluate the correlations of TCD parameters (such as Sx/Sx_a, Mx/Mx_a, and CrCP) with the invasive PbtO2 values. We plan to implement the protocol on an intended sample size of a total of 100 patients. Safety and feasibility will be analyzed after the enrollment of the first 25 patients. Further enrollment will be contingent on established safety and feasibility of prolonged TCD monitoring.
The variables of interest are listed in Supplementary Table 1. Data will be encrypted and stored in a secure server and will not be available for real-time decision making in this observational study. The results from this study will help determine the utility of TCD-derived parameters in predicting cerebral hypoxia in severe TBI patients. The study findings will be shared through publications and conference presentations. If the technology is successful, this protocol will help derive non-invasive targets for goal directed therapy (GDT) in patients with severe non-penetrating TBI. Additionally, findings from this study could facilitate development of future prognostic studies using non-invasive TCD monitoring.
Patient Population
Adult patients with severe blunt head trauma with Glasgow Coma Scale (GS) score ≤ 8 and invasive ICP and PbtO2 monitoring will be included. Unstable patients and those who are unable to tolerate device placement will be excluded. Specific inclusion and exclusion criteria for the study are summarized in Table 1. All procedures performed in the study shall be in accordance with the ethical standards of the participating institution as well as the 1964 Helsinki declaration and related amendments. Informed consent will be obtained from all participants enrolled in the study.
Study Objectives, Hypothesis, and Approach
The objectives of this study are threefold:
Aim 1: to determine the feasibility of prolonged automated robotic TCD monitoring in critically ill patients with severe TBI across multiple clinical sites with varying levels of TCD availability and experience.
-
Hypothesis: we hypothesize that all eligible patients will be able to successfully undergo up to 4 h of continuous TCD monitoring per day without any related adverse events, and clinically meaningful data will be acquired > 50% of the time per monitoring session.
-
Approach: upon informed consent, patients will undergo daily automated robotic TCD monitoring sessions for up to 4 h a day for a total duration of 5 days. TCD monitoring of bilateral MCA CBFV will be performed by using a robotic TCD system equipped with bilateral 2-MHz Doppler probes for continuous bilateral extended duration recording of MCA CBFV, using robotically controlled TCD probes.
-
Data acquisition: demographic data will be gathered for each patient, along with clinical variables, which are listed in Supplementary Table 1. Key factors and events precluding initiation or continuation of the study will also be recorded. Data will be gathered on the feasibility of bilateral monitoring given the possibility of limited temporal windows and technical factors that could limit insonation on one side. In case of unilateral insonation, data will be gathered on limiting factors including patient factors and technical issues with device or software issues. Additionally, a five-question provider survey (Table 2) will be administered at each participating site to obtain bedside nurse and clinician feedback on the perceived safety and feasibility of protocol implementation.
Aim 2: To determine the safety of prolonged automated robotic TCD monitoring in critically ill patients with severe TBI.
-
Hypothesis: we hypothesize that brain temperature measured by invasive intracranial probe will show < 1 ºC absolute rise attributable to TCD monitoring after adjusting for systemic temperature in patients monitored for up to 4 h. Additionally, we hypothesize that automated TCD monitor application is safe in eligible patients with severe TBI without unintended adverse events.
-
Approach: we will evaluate real-time brain temperature using the standard of care, invasive brain temperature probe during prolonged automated TCD monitoring and consider brain temperature rise of > 1 °C as the primary safety end point. We will define the safe duration of TCD monitoring as the total maximum duration of monitoring (up to 4 h) that is possible without rise in brain temperature more than 1 °C.
-
Data acquisition: We will gather data on continuous brain temperature using invasive monitoring and systemic core temperature to adjust for systemic fevers or body temperature rise during monitoring. Data will be gathered on absolute change in brain temperature as well a change in brain temperature divided by the change in core body temperature during the same time period. Assuming that a subset of patients may not have successful bilateral TCD monitoring due to limited temporal windows or technical issues, data will be gathered on laterality of temperature probe in relation to TCD insonation. As a secondary safety end point, we will monitor (1) patient discomfort (defined by change in heart rate > 20 points and systolic blood pressure > 20 mm Hg within the first 30 min of TCD initiation that is not attributed to routine clinical fluctuation), (2) dislodgement of invasive intracranial device as a result of TCD application, and (3) skin irritation or breakdown at the site of probe contact.
Aim 3: To evaluate the correlation between noninvasive cerebral hemodynamic parameters (systolic CBFV, mean CBFV, and corresponding Mx/Mx_a, Sx/Sx_a, and CrCP) derived from TCD and the PbtO2 values measured by invasive monitor. We will explore similar correlations between PRx and PbtO2, both derived by using invasive monitors.
-
Hypothesis: we hypothesize that noninvasive TCD values correlate with the PbtO2 measured by invasive monitors. We will explore the possibility that certain TCD thresholds of Mx/Mx_a, Sx/Sx_a, and CrCP can inform the presence of cerebral hypoxia and serve as a noninvasive surrogate measure of brain tissue hypoxia (defined as PbtO2 < 20 mm Hg for 5 min) in critically ill patients with severe TBI. Similarly, we hypothesize that certain thresholds of PRx can inform the presence of cerebral hypoxia in patients with acute TBI.
-
Approach: TCD assessment of bilateral MCA CBFV will be obtained via a robotic TCD system. All recorded signals will be digitized and integrated via an analog–digital converter, sampled at a frequency of 500 Hz using ICM + software and stored for offline analysis. The ICM + software includes a calculation engine that allows easy configuration and online trending of complex physiological parameters and multimodal monitoring of brain parameters. The program records raw signals with built in feature for artifact extraction and calculates time trends of summary parameters. Configuration and analysis utilize arithmetic expressions of signal processing functions to calculate various statistical properties for each signal, frequency spectrum, and derivatives, as well as correlations/cross-correlations between signals. This allows the multiparametric information coming off the bedside monitors to be summarized in a concise fashion and presented to medical and nursing staff in a simplified way that alerts them to the development of various pathological processes. The system provides a universal tool for clinical and academic purposes. Its flexibility and advanced signal processing are specialized for the needs of multidisciplinary brain monitoring. ICM + software will be available to all participating centers for data collection and signal processing. Of note, because a delay is expected between change in CBFV and related change in PbtO2, we will monitor the delay between these parameters.
-
Data acquisition: continuous vitals and pertinent hemodynamic and cerebrovascular parameters will be collected as noted in Supplementary Table 1. Post-acquisition processing of the above-described signals will be conducted using ICM + software. Continuous data will be gathered from concomitant ICP monitor using external ventricular drains or bolt, PbtO2 using invasive brain tissue oxygen monitor, mean ABP (MAP) using invasive ABP and the ETCO2 using the end-tidal CO2 monitor. CPP will be determined as the following: CPP = MAP–ICP (in mm Hg). Ten-second moving averages (updated every 10 s to avoid data overlap) will be calculated for all recorded signals: ICP, ABP (which will produce MAP), CPP, and systolic, diastolic, and mean CBFV. The autoregulation/cerebrovascular reactivity indices will be derived in a similar fashion including PRx and TCD-derived parameters Sx, Mx, Sx_a, and Mx_a. Details on each index calculation is presented in Table 3. Previously described thresholds for outcome analysis are presented in Table 4.
Statistical Analysis
We will evaluate correlations between each of the TCD-derived parameters and PbtO2 in comparison to correlation between PRx (derived invasively) and PbtO2. Associations will be evaluated using a general linear mixed model, accounting for the longitudinal data capture and the potential for site effects. We will assess if adjustment for age, sex, GCS, ICP and CPP affects these correlations. We will evaluate if TCD-derived CA parameters like Sx/Sx_a, Mx/ Mx_a, and CrCP can predict cerebral hypoxic burden as defined by PbtO2 < 20 mm Hg for > 5 min. We will also explore if the predictive value of TCD parameters to determine hypoxic burden differ between patients with intact autoregulation and those with impaired autoregulation, as defined by published PRx threshold for autoregulation [7]. A positive PRx signifies a positive gradient of the regression line between the slow components of MAP and ICP, which we hypothesize to be associated with the passive behavior of a nonreactive vascular bed. A negative value of PRx reflects a normally reactive vascular bed, as MAP waves provoke inversely correlated waves in ICP.
Discussion
Day-to-day neurocritical care environment requires analysis of a vast amount of data from a variety of sources including physical examination, systemic hemodynamic variables, imaging, and continuous physiological multimodal sensors such as electroencephalography and other neuromonitoring devices. Clinicians are routinely tasked with rapid evaluation and explication of multimodal data to make expeditious critical medical decisions. The sheer volume of continuously emerging critical data requiring complex interpretations is quite daunting and often preclude a comprehensive analysis and intervenable interpretation in routine clinical settings. The use of clinical decision support systems that allow ergonomic display of clinically useful data is the critical step toward wide applications of multimodal neuromonitoring [20]. Bedside clinicians need monitoring devices that are low maintenance with regard to data acquisition and provide clinical information in a simple usable format. Noninvasive monitoring using robotic TCDs with data display using automated software could be one such plausible solution for widespread use of neuromonitoring [21].
In the context of TBI, the underpinnings of secondary brain injury are quite complex and involve the interplay of several factors including cerebral hypoperfusion, neuronal inflammation and excitotoxicity [22]. Impaired CA with early phase of cerebral hypoperfusion followed by hyperemia leading to rise in ICP, has been proposed as one of the possible mechanisms of secondary brain injury [22]; therefore, a prime objective of TBI management in the acute period is the prevention of secondary brain injury by optimizing cerebral perfusion and oxygenation [23]. Unfortunately, there has been little advancement in the management strategies over the past few decades [23,24,25,26,28]. Because the impairment of normal cerebrovascular hemodynamics in TBI have serious prognostic implications [29], a GDT approach targeting optimization of cerebral hemodynamics such as the CPP, PbtO2, and ICP—or its noninvasive surrogates—can improve clinical outcomes by preventing the secondary injury cascade [28,29,31]. In terms of outcomes, established data from invasive monitoring of vasoreactivity capacity such as the PRx has already provided metrics with prognostic relevance and demonstrated good correlation with its noninvasive counterparts. This deserves further evaluation and exploration of avenues for routine clinical implementation.
The PRx is derived as the moving Pearson’s correlation coefficient between time averaged signals of ICP and MAP that allows determination of optimal CPP for individualized therapy and aids in determination of prognostic trajectory [7, 31,32,33,34,36]. It is one of the few CA indices supported by experimental data that allows measurement of the lower limit of autoregulation during arterial hypotension and intracranial hypertension [37]. Various thresholds of positive values of PRx have been identified within the literature to suggest impaired autoregulation, with PRx values ≥ 0.25 associated with mortality and PRx > 0.05 associated with unfavorable functional outcome [7]. Implementation of GDT using such parameters assessing cerebral hemodynamics is the cornerstone of precision medicine and allows for standardization of care across populations.
Bedside TCD can generate similar useful physiological intervenable information regarding cerebrovascular hemodynamics such as CPP [38], and TCD-derived PRx that have shown prognostic relevance [18]. The flow-based indices (Mx/Mx_a and Sx/Sx_a) can be derived noninvasively by using TCD, and studies have shown a close association between PRx and the noninvasive systolic flow index (Sx_a: moving Pearson’s correlation between systolic CBFV and MAP) and the mean flow index (Mx_a: moving Pearson’s correlation between the mean CBFV and MAP) [8, 18, 39]. Studies have also identified thresholds for each of these indices, which define populations with an increased risk for mortality or poor functional outcome. Mx threshold of 0.30 has been associated with mortality and unfavorable functional outcome, whereas Mx_a > 0.30 was only associated with unfavorable functional outcome [6]. For Sx, threshold of < − 0.15 was reported to correlate with unfavorable outcome and < − 0.20 for mortality. For Sx_a, thresholds of > 0.05 and < − 0.10 were associated with mortality and unfavorable outcomes, respectively [8].
Another TCD-based parameter with promise for clinical application in the evaluation of cerebral hemodynamics is the CrCP. The parameter represents the lower threshold of ABP, below which CPP is inadequate to prevent cerebral microvascular collapse, thereby resulting in the cessation of CBF. The concept of CrCP was first introduced by Burton’s model, described as the sum of ICP and vascular wall tension [40, 41]. The wall tension represents active cerebral vasomotor tone, which when combined with ICP determines the CrCP. Alternatively, CrCP can be assessed noninvasively by using the pulsatile waveforms of CBFV and ABP [9, 42]. Given the relationship with the vasomotor tone of small blood vessels, CrCP can provide useful information regarding the state of cerebral hemodynamics and reflect changes in CPP [9, 40, 41, 43]. Because CPP is directly associated with PbtO2, study of CrCP in the setting of invasive PbtO2 monitoring could provide valuable correlation data with potential for clinical utility.
The use of automated TCD can spontaneously capture such continuous data points generating multivariate time series that chronicles the longitudinal changes in cerebral hemodynamics. Having a dynamic window to the brain for each patient fosters precision medicine. The feasibility of the point of care TCD to guide clinical care has already been demonstrated both in the prehospital and hospital settings [3, 5, 44, 45]. Notably, the available literature and multidisciplinary consensus endorse the benefit of continuous measures of cerebrovascular reactivity to guide individualized therapy in patients with TBI [12, 34]. Nevertheless, the logistical challenges of ergonomic data acquisition and display have been a bottleneck in integrating TCD as a valuable and accessible tool in the treatment of patients with critically ill TBI. These challenges mainly pertain to deficit in technical and clinical expertise as well as inability to continuously measure clinically relevant parameters that can guide management in real time. Availability of automated robotic TCD in conjunction with automated software that can produce clinically useful data in real time could bridge the existing barriers that hinder routine clinical use of TCD for the treatment of critically ill patients with TBI.
This era of emerging concerted global efforts to cure coma [46, 47] is an opportune time to venture into novel ways to integrate and leverage the power of innovative technology for data acquisition and automated algorithms for data monitoring and interpretation. However, as we embark on this endeavor, it is also important to recognize some possible limitations related to the study aims. For example, for cases in which invasive PbtO2 monitors are placed away from the ischemic zone, the PbtO2 value may appear falsely normal. Similarly, because the automated TCD insonates only the MCAs, focal changes in CBFV away from the probe are unlikely to be detected. Furthermore, the distance between the site of TCD insonation and invasive monitors (PbtO2 and brain temperature) may preclude accurate correlation analysis. Although there are several challenges to overcome and account for, with this study using a robotic automated TCD acquisition equipment and a data processing software, we aim to identify clinically meaningful and pragmatic targets for future interventions that can pave a path toward improving outcomes in critically ill patients with TBI.
References
Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982;57(6):769–74.
Brauer P, Kochs E, Werner C, et al. Correlation of transcranial Doppler sonography mean flow velocity with cerebral blood flow in patients with intracranial pathology. J Neurosurg Anesthesiol. 1998;10(2):80–5.
Ract C, Le Moigno S, Bruder N, Vigué B. Transcranial Doppler ultrasound goal-directed therapy for the early management of severe traumatic brain injury. Intensive Care Med. 2007;33(4):645–51.
Sokoloff C, Williamson D, Serri K, et al. Clinical usefulness of transcranial Doppler as a screening tool for early cerebral hypoxic episodes in patients with moderate and severe traumatic brain injury. Neurocrit Care. 2020;32(2):486–91.
Budohoski KP, Czosnyka M, Smielewski P, et al. Impairment of cerebral autoregulation predicts delayed cerebral ischemia after subarachnoid hemorrhage: a prospective observational study. Stroke. 2012;43(12):3230–7.
Sorrentino E, Budohoski KP, Kasprowicz M, et al. Critical thresholds for transcranial Doppler indices of cerebral autoregulation in traumatic brain injury. Neurocrit Care. 2011;14(2):188–93.
Sorrentino E, Diedler J, Kasprowicz M, et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care. 2012;16(2):258–66.
Zeiler FA, Cardim D, Donnelly J, et al. Transcranial Doppler systolic flow index and ICP-derived cerebrovascular reactivity indices in traumatic brain injury. J Neurotrauma. 2018;35(2):314–22.
Varsos GV, Richards H, Kasprowicz M, et al. Critical closing pressure determined with a model of cerebrovascular impedance. J Cereb Blood Flow Metab. 2013;33(2):235–43.
Calviello L, Donnelly J, Cardim D, et al. Compensatory-reserve-weighted intracranial pressure and its association with outcome after traumatic brain injury. Neurocrit Care. 2018;28(2):212–20.
Beqiri E, Smielewski P, Robba C, et al. Feasibility of individualised severe traumatic brain injury management using an automated assessment of optimal cerebral perfusion pressure: the COGiTATE phase II study protocol. BMJ Open. 2019;9(9):e030727.
Czosnyka M, Smielewski P, Kirkpatrick P, et al. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41(1):11–7;discussion 7–9.
Zeiler FA, Ercole A, Cabeleira M, et al. Univariate comparison of performance of different cerebrovascular reactivity indices for outcome association in adult TBI: a CENTER-TBI study. Acta Neurochir (Wien). 2019;161(6):1217–27.
Fatima N, Shuaib A, Chughtai TS, Ayyad A, Saqqur M. The role of transcranial Doppler in traumatic brain injury: a systemic review and meta-analysis. Asian J Neurosurg. 2019;14(3):626–33.
Ziegler D, Cravens G, Poche G, Gandhi R, Tellez M. Use of transcranial Doppler in patients with severe traumatic brain injuries. J Neurotrauma. 2017;34(1):121–7.
Kumar G, Albright KC, Donnelly JP, Shapshak AH, Harrigan MR. Trends in transcranial Doppler monitoring in aneurysmal subarachnoid hemorrhage: a 10-year analysis of the Nationwide Inpatient Sample. J Stroke Cerebrovasc Dis. 2017;26(4):851–7.
Zeiler FA, Smielewski P. Application of robotic transcranial Doppler for extended duration recording in moderate/severe traumatic brain injury: first experiences. Crit Ultrasound J. 2018;10(1):16.
Zeiler FA, Smielewski P, Stevens A, et al. Non-invasive pressure reactivity index using Doppler systolic flow parameters: a pilot analysis. J Neurotrauma. 2019;36(5):713–20.
Clare K, Stein A, Damodara N, et al. Safety and efficacy of a novel robotic transcranial doppler system in subarachnoid hemorrhage. Sci Rep. 2022;12(1):2266.
Schmidt JMD, Georgia M. Multimodality monitoring: informatics, integration data display and analysis. Neurocrit Care. 2014;21(Suppl 2):S229–38.
Citerio G, Park S, Schmidt JM, et al. Data collection and interpretation. Neurocrit Care. 2015;22(3):360–8.
Werner C, Engelhard K. Pathophysiology of traumatic brain injury. Br J Anaesth. 2007;99(1):4–9.
DeWitt DS, Prough DS. Traumatic cerebral vascular injury: the effects of concussive brain injury on the cerebral vasculature. J Neurotrauma. 2003;20(9):795–825.
Narayan RK, Michel ME, Ansell B, et al. Clinical trials in head injury. J Neurotrauma. 2002;19(5):503–57.
Wright DW, Yeatts SD, Silbergleit R, et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371(26):2457–66.
Dewan Y, Komolafe EO, Mejía-Mantilla JH, et al. CRASH-3-tranexamic acid for the treatment of significant traumatic brain injury: study protocol for an international randomized, double-blind, placebo-controlled trial. Trials. 2012;13:87.
Edwards P, Arango M, Balica L, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet. 2005;365(9475):1957–9.
Clifton GL, Valadka A, Zygun D, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet Neurol. 2011;10(2):131–9.
Merck LH, Yeatts SD, Silbergleit R, et al. The effect of goal-directed therapy on patient morbidity and mortality after traumatic brain injury: results from the progesterone for the treatment of traumatic brain injury III clinical trial. Crit Care Med. 2019;47(5):623–31.
Okonkwo DO, Shutter LA, Moore C, et al. Brain oxygen optimization in severe traumatic brain injury phase-II: a phase II randomized trial. Crit Care Med. 2017;45(11):1907–14.
Zeiler FA, Beqiri E, Cabeleira M, et al. Brain tissue oxygen and cerebrovascular reactivity in traumatic brain injury: a collaborative European NeuroTrauma effectiveness research in traumatic brain injury exploratory analysis of insult burden. J Neurotrauma. 2020;37(17):1854–63.
Steiner LA, Czosnyka M, Piechnik SK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30(4):733–8.
Czosnyka M, Miller C. Monitoring of cerebral autoregulation. Neurocrit Care. 2014;21(Suppl 2):S95-102.
Le Roux P, Menon DK, Citerio G, et al. Consensus summary statement of the international multidisciplinary consensus conference on multimodality monitoring in neurocritical care: a statement for healthcare professionals from the neurocritical care society and the European Society of Intensive Care Medicine. Neurocrit Care. 2014;21(Suppl 2):S1-26.
Needham E, McFadyen C, Newcombe V, et al. Cerebral perfusion pressure targets individualized to pressure-reactivity index in moderate to severe traumatic brain injury: a systematic review. J Neurotrauma. 2017;34(5):963–70.
Froese L, Batson C, Gomez A, Dian J, Zeiler FA. The limited impact of current therapeutic interventions on cerebrovascular reactivity in traumatic brain injury: a narrative overview. Neurocrit Care. 2021;34(1):325–35.
Czosnyka M, Richards H, Pickard JD, Harris N, Iyer V. Frequency-dependent properties of cerebral blood transport—an experimental study in anaesthetized rabbits. Ultrasound Med Biol. 1994;20(4):391–9.
Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD. Cerebral perfusion pressure in head-injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg. 1998;88(5):802–8.
Zeiler FA, Smielewski P, Donnelly J, et al. Estimating pressure reactivity using noninvasive Doppler-based systolic flow index. J Neurotrauma. 2018;35(14):1559–68.
Michel E, Hillebrand S, vonTwickel J, Zernikow B, Jorch G. Frequency dependence of cerebrovascular impedance in preterm neonates: a different view on critical closing pressure. J Cereb Blood Flow Metab. 1997;17(10):1127–31.
Nichol J, Girling F, Jerrard W, Claxton EB, Burton AC. Fundamental instability of the small blood vessels and critical closing pressures in vascular beds. Am J Physiol. 1951;164(2):330–44.
Panerai RB. The critical closing pressure of the cerebral circulation. Med Eng Phys. 2003;25(8):621–32.
Puppo C, Camacho J, Yelicich B, et al. Bedside study of cerebral critical closing pressure in patients with severe traumatic brain injury: a transcranial Doppler study. Acta Neurochir Suppl. 2012;114:283–8.
Tazarourte K, Atchabahian A, Tourtier JP, et al. Pre-hospital transcranial Doppler in severe traumatic brain injury: a pilot study. Acta Anaesthesiol Scand. 2011;55(4):422–8.
Rasulo FA, Bertuetti R, Robba C, et al. The accuracy of transcranial Doppler in excluding intracranial hypertension following acute brain injury: a multicenter prospective pilot study. Crit Care. 2017;21(1):44.
Claassen J, Akbari Y, Alexander S, et al. Proceedings of the first curing coma campaign NIH symposium: challenging the future of research for coma and disorders of consciousness. Neurocrit Care. 2021;35(Suppl 1):4–23.
Provencio JJ, Hemphill JC, Claassen J, et al. The curing coma campaign: framing initial scientific challenges-proceedings of the first curing coma campaign scientific advisory council meeting. Neurocrit Care. 2020;33(1):1–12.
Acknowledgements
We would like to sincerely thank the Curing Coma Campaign Scientific Advisory Council for providing insights and feedback related to the project as well as Karen G. Hirsch and Jonathan Elmer for their insight and guidance on the research protocol.
Funding
The work reported in this publication was partially supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Numbers U24NS100659 and U24NS100655. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
SM: conceptualized and designed the research protocol and drafted and finalized the article. DC: conceptualized and designed the research protocol and drafted and finalized the article. AS: conceptualized and designed the research protocol and drafted and finalized the article. LM: significant contribution to the design and concept of the protocol and provided critical input and edits on the article. SY: significant contribution to the design and concept of the protocol and provided critical input and edits on the article. MC: significant contribution to the design and concept of the protocol and provided critical input and edits on the article. LS: significant contribution to the design and concept of the protocol and provided critical input and edits on the article. The authors approved of the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
SY: National Institute of Neurological disorders (NINDS) grant funds to institution related to Strategies to Innovate Emergency Care Clinical Trials Network (SIREN) Data Coordinating Center (DCC), Brain Oxygen Optimization in Severe TBI - Phase 3 (BOOST-3) study. MC: Receives licensing fee for ICM+ (Intensive Care Monitoring) software. The remaining authors have no conflicts to disclose.
Ethical approval/informed consent
This is a design and rationale article of an upcoming trial that will be conducted after appropriate ethical approval from participating sites. Informed consent will be used to enroll participants in this observational study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mainali, S., Cardim, D., Sarwal, A. et al. Prolonged Automated Robotic TCD Monitoring in Acute Severe TBI: Study Design and Rationale. Neurocrit Care 37 (Suppl 2), 267–275 (2022). https://doi.org/10.1007/s12028-022-01483-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01483-6