Abstract
Purpose
To evaluate the potential benefit of adding a low frequency vascular probe to the conventional pre-operative ultrasound examination of patients with primary hyperparathyroidism.
Methods
A prospective cohort of 136 patients with primary hyperparathyroidism underwent a conventional ultrasound examination of the neck with a high frequency ( > 10 MHz) linear ultrasound probe, followed by an add-on examination with a low frequency vascular probe. For each ultrasound probe, and for every potential parathyroid lesion, the presence of a feeding vessel, a polar placement of the feeding vessel, and the presence of a vascular arch was recorded.
Results
A total of 146 ultrasound lesions were evaluated for vascularity by each probe. For both ultrasound probes, the odds of a hyperfunctioning parathyroid gland being correctly identified increased with the number of visible vascular features. The vascular probe identified a significantly higher number of vascular features among ultrasound true positive glands compared with the conventional probe (p < 0.0001). Among histopathologically verified pathological parathyroid glands, the vascular probe identified 20% more feeding vessels, 27% more polar placements of the feeding vessel, and 65% more vascular arches than the high frequency probe. However, the diagnostic confidence score for true positive glands did not differ significantly between the probes (p = 0.11).
Conclusion
The addition of a low frequency vascular probe increases the number of visible vascular features in hyperfunctioning parathyroid glands, which facilitates their preoperative detection. Whether or not this can increase the diagnostic confidence of ultrasound examiners has yet to be substantiated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Most patients with primary hyperparathyroidism (PHPT) have a single hyperfunctioning parathyroid gland (89%), while a minority have multiple gland hyperplasia (6%), or double adenomas (4%) [1]. The definitive cure for PHPT is surgical removal of all hyperfunctioning parathyroid tissue [2]. Surgical planning is facilitated by pre-operative imaging, which attempts to determine both the location and number of enlarged parathyroid glands. If the pre-operative localization is successful, surgeons can perform a minimally invasive procedure in patients with single gland disease or plan the least extensive bilateral procedure for patients with multiple gland disease [3].
Pre-operative imaging regimens vary between institutions, but ultrasound (US) is the recommended technology, as it enables a simultaneous evaluation of the thyroid gland [2, 4]. Although US has a high sensitivity for the detection of enlarged parathyroid glands in experienced hands [5], many diagnostic set-ups involve a parallel acquisition of US and a radiation-based imaging modality, such as 99mTc-sestamibi subtraction scintigraphy, single-photon emission computed tomography (SPECT), SPECT/CT, four-dimensional CT, or positron emission tomography (PET)-CT with a radiolabelled tracer [2, 6, 7]. To avoid superfluous imaging procedures, however, a number of centers with experienced parathyroid ultrasound examiners have abandoned parallel imaging acquisition in favor of a stepwise regimen, in which an upfront US examination determines the need for additional procedures [8, 9].
Upfront US places high demands on the quality of the US examination and the ability of the US probe to visualize the typical sonographic features of a parathyroid adenoma: A hypoechoic and sharply delineated lesion with an enlarged feeding artery entering the pole and continuing around the periphery in a 90 to 270 degree vascular arch [10, 11]. In general, high frequency ( > 10 MHz) US probes are used to evaluate hyperfunctioning parathyroid glands and current guidelines on parathyroid ultrasound do not suggest using a separate transducer for the detection of vascular features [10, 12]. However, when our tertiary referral center recently performed a study comparing US and contrast-enhanced ultrasound (CEUS) with scintigraphy [13], we experienced that the lower frequency range (3–11 MHz) peripheral vascular probe dedicated to CEUS could reveal parathyroid vascular features that had not been visible with the high frequency probe, even without the addition of a contrast agent. Therefore, we hypothesized that the conventional ultrasound examination of patients with PHPT would benefit from the addition of a lower frequency dedicated vascular probe in terms of revealing more vascular features.
Materials and methods
This prospective, paired cohort study is based on a larger non-inferiority study of 172 patients, which compares conventional US and CEUS with scintigraphy, as previously reported [13]. The study is registered at ClinicalTrials.gov (NCT04305561) and has been approved by the Regional Committees on Health Research Ethics for Southern Denmark (project ID S-20190077). The study was carried out in accordance with the ethical principles described in the 1964 Declaration of Helsinki and its later amendments. The inclusion of the current subgroup started on December 19, 2019, and ended on February 25, 2021 at the Department of Otorhinolaryngology, Head & Neck Surgery, and Audiology at Odense University Hospital, Denmark. Participants signed an informed consent document and formed a consecutive series. The reporting guideline Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) was used [14].
Study participants
Eligible patients were adults ( ≥ 18 years) with PHPT who were referred for parathyroidectomy. Patients were excluded if they were not legally competent; were pregnant/nursing; could not read/speak Danish; had prior parathyroid or thyroid surgery; had an ongoing malignant neoplasm; did not undergo scintigraphy or CEUS in the Region of Southern Denmark; had contraindications to CEUS; or were not booked for surgery [13].
Setup and blinding
All patients underwent a dual-tracer 99mtechnetium-pertechnetate/99mtechnetium-sestamibi subtraction scintigraphy with 99mtechnetium-sestamibi SPECT/CT (dtSM SPECT/CT) prior to an in-office consultation with one of three experienced parathyroid surgeon-sonographers. The surgeon-sonographer was blinded to the result of the dtSM SPECT/CT until all US examinations had been performed and documented.
Notation of localization, diagnostic confidence, and vascular features
Each ultrasound probe had its own scoring sheet featuring a coronal illustration of the thyroid gland, which had been divided into quadrants as well as a 10-part classification (Fig. 1). Potential pathological glands were drawn on the illustration, and each predefined position was assigned a confidence score from a 5-point Likert-type scale. Low scores of 1 or 2 were assigned to imaging negative positions, and high scores of 4 or 5 were assigned to imaging positive positions. If no potential pathological gland was identified anywhere, a neutral score of 3 was assigned to all positions, categorizing the examination as non-localizing.
A high suspicion of pathology was indicated with score 5 for the given location combined with score 1 for all remaining negative positions. A moderate suspicion was indicated with score 4 for the given location combined with score 1 for all remaining negative positions. A low suspicion was indicated with score 4 for the given location combined with score 2 for all remaining negative positions.
All imaging-positive lesions were evaluated for the presence/absence of three vascular features: i. a feeding artery, ii. polar placement of the feeding artery, iii. a vascular arch.
Conventional high frequency ultrasound
The conventional US examination was carried out on a Canon® Aplio a450 US machine, version 1.3 (Canon Medical Systems, Japan) with a PLT-1005BT (14L5) linear transducer with center frequency pre-sets of 8.0, 11.0, and 14.0 MHz. Patients were placed in a supine position with their neck extended. First, the probe was placed on a central part of the thyroid gland in the transversal plane to optimize settings. The highest frequency providing visualization of the longus colli muscle was chosen, and the depth was adjusted to show the thyroid gland and underlying longus colli muscle. The focus was set on the dorsal border of the thyroid gland, but could be adjusted once a potential pathological parathyroid gland was encountered. Scanning commenced cranial to the thyroid gland in the transverse plane and continued caudally to the clavicle, where the probe was tilted until the subclavian artery or vein was visualized. The probe was then rotated 90 degrees clockwise, and scanning continued in the longitudinal plane [15]. All potential parathyroid lesions were evaluated for vascularity with Advanced Dynamic Flow and Superb Microvascular Imaging. The location, diagnostic confidence, and number of visible vascular features were documented before the ensuing examination with the low frequency vascular probe was conducted.
Low frequency vascular probe
The vascular ultrasound examination was performed as an add-on to conventional ultrasound and consisted of the initial steps of a CEUS examination, before the injection of contrast. Because CEUS requires a dedicated vascular probe, an integrated part of the procedure is to re-identify – with the vascular probe and before contrast injection – all suspected pathological parathyroid glands visualized during conventional ultrasound. This examination was undertaken by one of two surgeon-sonographers trained in CEUS, using a PLT-705BT (11L3) peripheral vascular linear transducer with center frequency pre-sets of 6.0, 7.0, and 8.0 MHz. Settings were optimized and suspected parathyroid lesions were re-identified and scored for diagnostic confidence and the number of visible vascular features, as described above. This additional documentation step was scored separately from the ensuing CEUS examination.
Surgery
If a potential parathyroid adenoma had been preoperatively identified, a minimally invasive approach was chosen. If preoperative imaging results were discordant, the surgeon autonomously decided which location to target first, guided by the respective confidence scores. Two pre-incision parathyroid hormone (PTH) plasma levels were measured at the beginning of surgery. A ≥ 50% drop in plasma PTH from the highest pre-incision level, measured ten minutes after the excision of a potential parathyroid gland, signaled that no further exploration was necessary [16]. The in vivo location of excised tissue was documented according to the specifications described above (Fig. 1) combined with the Perrier classification, which is a nomenclature covering the most frequent anatomical locations of parathyroid adenomas [17]. All specimens underwent histopathological evaluation.
Follow-up
After surgery, patients were referred to their local department of endocrinology, where they were followed with blood tests for at least six months [13]. A minority of patients (19 of 136 [14%]) finalized follow-up with their family physician after showing stable normocalcemia for a median of 122 days (IQR 85–148) at the local department of endocrinology. Individuals in this group were assumed to have remained normocalcemic if they had not been re-referred to the hospital by the end of the study, i.e. December 31, 2021.
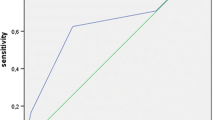
Outcome measures
For obvious reasons, pathological parathyroid glands that were overlooked on ultrasound could not be evaluated for vascularity. The main outcome measure was the number of vascular features identified by each probe. Exploratory analyses furthermore assessed the association between the number of visible vascular features and the number of true/false positive glands for each probe, the association between the number of visible vascular features and the diagnostic confidence, and the diagnostic confidence reached by each probe. For reference purposes, we also calculated the per-patient sensitivity ( ≥ 1 true positive quadrant per patient) and the per-quadrant sensitivity, specificity, positive predictive value, and negative predictive value. These results are available in Online Resource 1. Since a diagnosis of PHPT was an inclusion criterion, calculating the specificity per patient was not meaningful.
The reference standard consisted of the in vivo surgical localization and histopathology of the excised specimen combined with long-term cure (normocalcemia 6 months after surgery). If a specimen was located in-between two quadrants (i.e. in the middle of the thyroid gland), the 10-part classification served as a reference [13]. Patients with residual disease at follow-up were conservatively categorized as having had one pathological parathyroid gland in each quadrant at the time of surgery, representing the maximum possible number of pathological glands that the ultrasound examiner could have overlooked. A true positive quadrant had been correctly categorized on ultrasound as harboring a diseased gland (adenoma or hyperplasia on histopathology). A true negative quadrant had been correctly categorized as free from pathology in a patient who achieved long-term cure. A false positive quadrant had been categorized as harboring a diseased gland on ultrasound, but no pathological tissue was removed from it during surgery - in a patient who achieved long-term cure. A false negative quadrant had been categorized as free from pathology on ultrasound, but an adenomatous or hyperplastic gland was either excised from it during surgery or assumed in residual disease.
Sample size
The sample size of 136 patients was predetermined by the sample size of the overall cohort [13]. Regarding the main outcome measure, we made an a priori calculation of the discordant proportions necessary to reach a power >80% and a significance level of 0.05 when using McNemar’s test, two correlated proportions, and a sample size of 136. Assuming that the conventional ultrasound probe could identify 5% of vascular features that were not visible on the vascular probe, the power would be >80%, provided that the vascular probe could identify at least 16% of vascular features not visible on the conventional ultrasound probe.
Statistical methods
Descriptive statistics were derived according to data type; continuous variables were described with median (minimum-maximum), categorical variables with frequencies and respective percentages. The Wilcoxon signed rank test was used to compare the ultrasound probes (conventional vs. vascular) regarding the number of visualized vascular features and the diagnostic confidence of true positive glands. A logistic regression was used to assess the relationship between the number of visible vascular features and the number of true/false positive glands. A Kruskal-Wallis test and Cuzick’s test of trend were used to assess the relationship between the number of vascular features in true positive glands and the confidence score. McNemar’s test was used to compare the probes at the level of each individual vascular feature and to assess patient-based sensitivity. Quadrant-based analyses for diagnostic accuracy measures were performed as a regression of the binary outcome (e.g. for sensitivity: true positives vs. false negatives) on modality, with cluster-robust standard errors to account for the four quadrants within each patient [18]. Ninety-five percent confidence intervals were supplemented for respective point estimates. Two-sided p-values < 0.05 were considered statistically significant.
Study data were managed with REDCap® electronic data capture tools hosted at Odense University Hospital [19, 20]. Statistical calculations were performed in Stata/BE: release 18 (StataCorp LLC) and Microsoft Excel® 2016.
Results
Out of 158 eligible patients, 22 were excluded, leaving 136 patients for inclusion in the study (Fig. 2). Two patients (1.5%) did not achieve long-term cure, while the remaining 134 patients (98.5%) were relieved of hyperparathyroidism post-surgery. A total of 146 hypoechoic ultrasound lesions in 125 patients were considered to be “ultrasound positive” by at least one probe and consequently evaluated for vascularity. The remaining 11 patients had non-localizing ultrasound scans. Patient characteristics are listed in Table 1.
Vascular features
For both ultrasound probes, the odds of a gland being true positive increased with the number of visible vascular features (Table 2). The vascular probe identified a significantly higher number of vascular features among ultrasound true positive glands compared with the conventional probe (p < 0.0001, Table 2). This was also the case when each individual vascular feature was assessed (Table 3). The vascular probe identified 20% more feeding vessels, 27% more polar placements of the feeding vessel, and 65% more vascular arches among true positive glands than the high frequency probe Fig. 3.
Effect of vascular features on confidence score
For both probes, a Kruskal-Wallis test indicated that at least one level of vascular features had an effect on the confidence score (p = 0.0001). A post hoc Cuzick test showed a statistically significant trend for increasing confidence scores across the four levels of vascular features (p < 0.0001, Table 4). However, the diagnostic confidence score for true positive glands did not differ significantly between the probes (Wilcoxon signed rank test p = 0.11).
Discussion
Previous studies have shown that ultrasound is a valid first line test for localizing enlarged parathyroid glands in patients with primary hyperparathyroidism [13, 21]. In this context, optimizing the conventional ultrasound examination is a logical next step. To our knowledge, this is the first study comparing the visibility of vascular features in hyperfunctioning parathyroid glands using different ultrasound probes.
The most common mimics of hyperfunctioning parathyroid glands on ultrasound are cervical lymph nodes and thyroid nodules [22, 23]. These structures, however, may be distinguished from hyperfunctioning parathyroid glands by their vascular patterns [22]. Lymph nodes have a central vascular hilum, whereas thyroid nodules show peri- and intralesional vascularization from an internal thyroid vessel [22, 24]. Hyperfunctioning parathyroid glands, on the other hand, typically display a prominent extrathyroidal polar feeding vessel and a peripheral vascular arch [10].
In this study, we showed that the addition of a low-frequency vascular transducer significantly increased the number of detectable vascular features in pathological parathyroid glands compared to conventional ultrasound employing a high-frequency probe. Additionally, the odds of a gland being true positive increased with the number of visible vascular features. This finding is in line with a study by Lane et al., which found that the presence of an extrathyroidal feeding vessel increased the sensitivity for detecting parathyroid adenomas from 73% to 83% [25]. Similarly, a prospective study from 2003 reported a statistically significant increase in diagnostic accuracy when a feeding vessel was identified [26]. Even when it comes to the challenging detection of intrathyroidal parathyroid adenomas, a retrospective study from 2013 found a strong correlation between the presence of a polar feeding vessel and correct identification of an intrathyroidal parathyroid adenoma on ultrasound [27]. Consequently, the addition of a vascular probe to the conventional ultrasound examination could potentially help reduce the number of false positive findings on ultrasound and/or increase the sensitivity for detecting pathological parathyroid glands [26, 28].
While our exploratory analysis showed a statistically significant trend for increasing diagnostic confidence scores concurrently with increasing numbers of visible vascular features, there was no statistically significant difference between the confidence scores obtained with each probe. The reason for this is likely three-fold. First, the sample size was not designed to compare the confidence scores between the ultrasound probes. Second, by design the examiners had no option of indicating an improved diagnostic confidence with the addition of the vascular probe in cases where they had already given a maximum confidence score based on the conventional probe alone. Third, the examiners in this study were all experienced in parathyroid ultrasound. It may well be that less experienced examiners would benefit even more from the increased visibility of parathyroid vascular features [29].
Some limitations should be addressed. The idea for the present study arose during the pilot phase of a larger cohort study. The sample size and design were therefore constrained by a predefined protocol. This restricted the recording of diagnostic confidence, as mentioned above, but it did not influence the notation of the number of vascular features. Because the number of vascular features is an objective measure, whereas diagnostic confidence is subjective, we considered the number of visible vascular features to be the most reliable/reproducible measure of the effect of adding a vascular probe. Finally, we cannot be certain of the generalizability of our results to ultrasound probes from other manufacturers.
Future studies could aim to investigate the impact of the addition of a low frequency vascular probe on both the sensitivity of the ultrasound examination, the diagnostic confidence of the examiner, and the interobserver variability. Furthermore, the generalizability of our results to probes from other manufacturers should be investigated. In centers that employ upfront ultrasound, it would be interesting to examine the effect of a second-look ultrasound examination on the diagnostic sensitivity in cases where the initial ultrasound examination is negative, or the ultrasound examiner’s confidence in the result is low. Such an approach could potentially spare an even larger number of patients from radiation-based parathyroid imaging while making better use of the finite resources of the healthcare system [29, 30].
In conclusion, we have shown that the addition of a low frequency vascular probe increases the number of visible vascular features in hyperfunctioning parathyroid glands, which aids in their preoperative detection. Whether or not this can increase the diagnostic confidence of ultrasound examiners has yet to be substantiated.
References
J.M. Ruda, C.S. Hollenbeak, B.C. Stack Jr., A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol. Head. Neck Surg. 132(3), 359–372 (2005). https://doi.org/10.1016/j.otohns.2004.10.005
S.M. Wilhelm, T.S. Wang, D.T. Ruan et al. The American Association of Endocrine surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 151(10), 959–968 (2016). https://doi.org/10.1001/jamasurg.2016.2310
A.A. Khan, D.A. Hanley, R. Rizzoli et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos. Int. 28(1), 1–19 (2017). https://doi.org/10.1007/s00198-016-3716-2
T. Weber, C. Dotzenrath, H. Dralle et al. Management of primary and renal hyperparathyroidism: guidelines from the German Association of Endocrine Surgeons (CAEK). Langenbecks Arch. Surg. 406(3), 571–585 (2021). https://doi.org/10.1007/s00423-021-02173-1
D.L. Steward, G.P. Danielson, C.E. Afman, J.A. Welge, Parathyroid adenoma localization: surgeon-performed ultrasound versus sestamibi. Laryngoscope 116(8), 1380–1384 (2006). https://doi.org/10.1097/01.mlg.0000227957.06529.22
S.W. Lee, S.R. Shim, S.Y. Jeong, S.J. Kim, Direct comparison of preoperative imaging modalities for localization of primary hyperparathyroidism: a systematic review and network meta-analysis. JAMA Otolaryngol. Head. Neck Surg. 147(8), 692–706 (2021). https://doi.org/10.1001/jamaoto.2021.0915
A.O. Bergenfelz, P. Hellman, B. Harrison, A. Sitges-Serra, H. Dralle, Positional statement of the European Society of Endocrine Surgeons (ESES) on modern techniques in pHPT surgery. Langenbecks Arch. Surg. 394(5), 761–764 (2009). https://doi.org/10.1007/s00423-009-0533-5
C. Deutmeyer, M. Weingarten, M. Doyle, D. Carneiro-Pla, Case series of targeted parathyroidectomy with surgeon-performed ultrasonography as the only preoperative imaging study. Surgery 150(6), 1153–1160 (2011). https://doi.org/10.1016/j.surg.2011.09.041
B.R. Untch, M.A. Adam, R.P. Scheri et al. Surgeon-performed ultrasound is superior to 99Tc-sestamibi scanning to localize parathyroid adenomas in patients with primary hyperparathyroidism: results in 516 patients over 10 years. J. Am. Coll. Surg. 212(4), 522–529 (2011). https://doi.org/10.1016/j.jamcollsurg.2010.12.038
A. Kamaya, A. Quon, R.B. Jeffrey, Sonography of the abnormal parathyroid gland. Ultrasound Q 22(4), 253–262 (2006). https://doi.org/10.1097/01.ruq.0000237260.33509.4f
R.J. Wolf, J.J. Cronan, J.M. Monchik, Color Doppler sonography: an adjunctive technique in assessment of parathyroid adenomas. J. Ultrasound Med. 13(4), 303–308 (1994)
AIUM practice parameter for the performance of a thyroid and parathyroid ultrasound examination. J. Ultrasound Med. 35(9):1–11 (2016). https://doi.org/10.7863/ultra.35.9.1-c
S.H. Michaelsen, M. Bay, O. Gerke et al. Evaluation of surgeon-performed ultrasonography with or without contrast enhancement vs scintigraphy in patients with primary hyperparathyroidism. JAMA Otolaryngol. Head Neck Surg. (2023). https://doi.org/10.1001/jamaoto.2023.0389
E. von Elm, D.G. Altman, M. Egger, S.J. Pocock, P.C. Gøtzsche, J.P. Vandenbroucke, The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J. Surg. 12(12), 1495–1499 (2014). https://doi.org/10.1016/j.ijsu.2014.07.013
S.B. Reeder, T.S. Desser, R.J. Weigel, R.B. Jeffrey, Sonography in primary hyperparathyroidism: review with emphasis on scanning technique. J. Ultrasound Med. 21(5), 539–552 (2002). quiz 553-4
D.M. Carneiro, C.C. Solorzano, M.C. Nader, M. Ramirez, G.L. Irvin 3rd, Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery 134(6), 973–979 (2003). https://doi.org/10.1016/j.surg.2003.06.001
N.D. Perrier, B. Edeiken, R. Nunez et al. A novel nomenclature to classify parathyroid adenomas. World J. Surg. 33(3), 412–416 (2009). https://doi.org/10.1007/s00268-008-9894-0
W. Vach (2013) Regression Models as a Tool in Medical Research. 1 ed. Chapman and Hall/CRC.
P.A. Harris, R. Taylor, R. Thielke, J. Payne, N. Gonzalez, J.G. Conde, Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42(2), 377–381 (2009). https://doi.org/10.1016/j.jbi.2008.08.010
P.A. Harris, R. Taylor, B.L. Minor et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inf. 95, 103208 (2019). https://doi.org/10.1016/j.jbi.2019.103208
G.M. Vitetta, A. Ravera, G. Mensa et al. Actual role of color-doppler high-resolution neck ultrasonography in primary hyperparathyroidism: a clinical review and an observational study with a comparison of (99m)Tc-sestamibi parathyroid scintigraphy. J. Ultrasound 22(3), 291–308 (2019). https://doi.org/10.1007/s40477-018-0332-3
A.M. Isidori, V. Cantisani, E. Giannetta et al. Multiparametric ultrasonography and ultrasound elastography in the differentiation of parathyroid lesions from ectopic thyroid lesions or lymphadenopathies. Endocrine 57(2), 335–343 (2017). https://doi.org/10.1007/s12020-016-1116-1
R. Centello, F. Sesti, T. Feola et al. The dark side of ultrasound imaging in parathyroid disease. J. Clin. Med. 12(7)(2023). https://doi.org/10.3390/jcm12072487
M. Ying, A. Ahuja, F. Brook, C. Metreweli, Power Doppler sonography of normal cervical lymph nodes. J. Ultrasound Med. 19(8), 511–517 (2000). https://doi.org/10.7863/jum.2000.19.8.511
M.J. Lane, T.S. Desser, R.J. Weigel, R.B. Jeffrey Jr., Use of color and power Doppler sonography to identify feeding arteries associated with parathyroid adenomas.AJR Am. J. Roentgenol. 171(3), 819–823 (1998). https://doi.org/10.2214/ajr.171.3.9725323
S. Rickes, J. Sitzy, H. Neye, K.W. Ocran, W. Wermke, High-resolution ultrasound in combination with colour-Doppler sonography for preoperative localization of parathyroid adenomas in patients with primary hyperparathyroidism. Ultraschall. Med. 24(2), 85–89 (2003). https://doi.org/10.1055/s-2003-38667
M.T. Heller, L. Yip, M.E. Tublin, Sonography of intrathyroid parathyroid adenomas: are there distinctive features that allow for preoperative identification? Eur. J. Radio. 82(1), e22–e27 (2013). https://doi.org/10.1016/j.ejrad.2012.08.001
A. Mohammadi, F. Moloudi, M. Ghasemi-rad, The role of colour Doppler ultrasonography in the preoperative localization of parathyroid adenomas. Endocr. J. 59(5), 375–382 (2012). https://doi.org/10.1507/endocrj.ej11-0351
S. Ilgan, B. Aydoğan, Ö Emer et al. Sonographic features of atypical and initially missed parathyroid adenomas: Lessons learned from a single center cohort. J. Clin. Endocrinol. Metab. (2023). https://doi.org/10.1210/clinem/dgad527
A. Chandramohan, K. Sathyakumar, A. Irodi, D. Abraham, M.J. Paul, Causes of discordant or negative ultrasound of parathyroid glands in treatment naïve patients with primary hyperparathyroidism. Eur. J. Radio. 81(12), 3956–3964 (2012). https://doi.org/10.1016/j.ejrad.2012.08.019
Funding
Dr Godballe reports a grant from “Doctor Sofus Carl Emil Friis and Wife Olga Doris Friis’ Grant” (a non-profit charitable foundation) to update the software licenses and ultrasound probes on two of the department’s ultrasound machines. The grant was received prior to the onset of the study. Open access funding provided by Odense University Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data acquisition, analysis, or interpretation was performed by all authors. The first draft of the manuscript was written by S.H.M. and O. Gerke. Author S.H.M. prepared all tables and figures. All authors contributed to the critical revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The study was carried out in accordance with the ethical principles of the 1964 Declaration of Helsinki and its later amendments. The study is registered at ClinicalTrials.gov (NCT04305561) and has been approved by the Regional Committees on Health Research Ethics for Southern Denmark (project ID S-20190077).
Consent to participate
Written informed consent was obtained from all participants in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Michaelsen, S.H., Bay, M., Gerke, O. et al. The detection of pathological parathyroid glands is facilitated by identifying vascular features on ultrasound: the potential benefit of a low-frequency vascular probe. Endocrine (2024). https://doi.org/10.1007/s12020-024-03986-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03986-y