Abstract
Low bone mineral density (BMD) is a strong risk factor for low trauma fractures in the postmenopausal population without known chronic kidney disease (CKD). In stage 1–3 CKD, low BMD can also be used to predict fracture risk with the gradient of risk similar to patients without CKD even though patients with stage 3 CKD have an approximate doubling of risk compared with age-matched patients without CKD. This greater risk of fracture in stage 3 CKD is not calculated in the current FRAX model. In stage 4–5 CKD, BMD by dual-energy x-ray absorptiometry (DXA) is a poor predictor of fracture risk probably related to the severe derangements in bone metabolism in severe CKD, which alter bone quality and strength not measured by DXA. Serial BMD by DXA, however, may be useful in all stages of CKD to monitor for potential loss of BMD or effect of pharmacological agents to improve BMD. Newer radiological technologies, particularly high-resolution peripheral quantitative computerized tomography (HRpQcT) of the radius and tibia show promise to define the microstructural changes in bone that explain the greater risk of fracture observed in patients with CKD versus patients without CKD. BMD by DXA may still be of value across the spectrum of CKD, but physicians should realize its limitations and understand the greater risk of fracture in patients in all stages of CKD as compared to age-matched and BMD-matched patients without CKD.
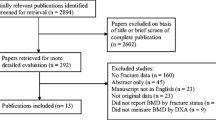
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Measurements of bone mineral density (BMD) by a number of methodologies have advanced the science and clinical management of metabolic bone diseases. Most notably, BMD measurements have provided the framework for the diagnosis of postmenopausal and male osteoporosis before a fracture occurs, have been validated as one of the strongest risk factors for the prediction of fracture risk in the postmenopausal and male osteoporosis populations, and are valuable for monitoring either the natural biology of change in BMD or change induced by pharmacological therapy for osteoporosis [1–29].
The United States Surgeon General Office and the United States Prevention Services Task Force (USPSTF) recommend population screening for early detection of osteoporosis in all postmenopausal women aged 65 years and older without any additional risk factors for osteoporosis, and in all postmenopausal women with even one additional risk factor for osteoporosis [30, 31].
The Bone Mass Measurement Act (BMMA) of 1995, a congressional statute to expand the indications for bone mass measurements in the postmenopausal population, provided even stronger United States government support for facilitating widespread use of bone mass measurements for the diagnosis of osteoporosis and for monitoring patients on Food and Drug Administration (FDA) approved therapies [32]. Since all worldwide populations are living longer and renal function declines with aging, it is inevitable that nephrologists will increasingly be faced with management decisions in the chronic kidney disease (CKD) population who also have BMD determinations. In the National Health and Nutrition Examination Survey (NHANES), the prevalence of CKD and osteoporosis is clearly increasing [33, 34].
The 1994 publication of the World Health Organization (WHO) criteria for the diagnosis of postmenopausal osteoporosis (PMO) or osteopenia are not predicated on any known level of renal function [3]. In addition, the 9 population trials that constituted the data used by the WHO to validate the 10-year risk factors for fracture in untreated postmenopausal and male populations (FRAX™), and renal function by any methodology was not captured in an adequate sample size to become a validated factor for fracture risk prediction [17, 21]. Diagnosis, fracture risk prediction, and management of patients at high risk of fractures will increasingly become important management considerations for the nephrologist for a number of reasons:
-
1.
Populations are aging.
-
2.
Age is an independent risk factor for fracture at equivalent levels of BMD (Fig. 1) [12, 13, 15, 20–23].
Fig. 1 The relationship between bone mineral density, age, and fracture risk [9]
-
3.
Glomerular filtration rate (GFR) declines with increasing age [35–37].
-
4.
Stage 3 CKD, (GFR <60 ml/min), is the largest growing stage of CKD in the worldwide population [33–37].
-
5.
Risk of all fractures doubles by stage 3 CKD at the same level of BMD, age, and body mass index (BMI) as compared to those without CKD [38–42].
Thus, risks of fragility fractures are greater in patients with CKD at the same BMD than in those without CKD. There are many pathophysiological disturbances associated with CKD that make these patients more likely to break bones compared with patients without CKD, despite having the same bone mass measurement. These biochemical interactions are outlined in Fig. 2 [43]. Phosphorus retention, secondary hyperparathyroidism, elevated fibroblast growth factor 23 (FGF-23), chronic metabolic acidosis, and disorders of vitamin D metabolism singularly or collectively could alter bone metabolism and contribute to decreases in bone quality and thus bone strength beyond the contribution provided by low BMD per se [43–48].
The biochemical interactions between bone, kidney, parathyroid glands, gastrointestinal tract, and vascular tissue that regulate serum phosphorus, bone turnover, and vascular calcification (adapted from [43])
It is inevitable that the question is “What is the predictability of BMD measurements by dual X-ray absorptiometry (DXA) to predict fracture risk in stage 3 CKD?” Equally important for the nephrology community is the question of “How well are BMD measurements by DXA in predicting risk of fracture in more severe CKD (stage 4–5 CKD), that is, patients with GFR values of <30 ml/min?”
This manuscript will examine data and put into real-world perspective the applicability of using BMD by DXA to diagnose PMO or to predict fracture risk across the spectrum of CKD.
How the WHO Established the “T-score”
The data that led to the establishment of the WHO diagnostic criteria for defining the T-score were derived predominately from 2 separate postmenopausal populations: Olmstead County, Rochester, Minnesota, USA, and Sheffield, UK [3, 8, 15]. From these 2 populations, where renal function was not assessed, the data related the T-score (defined as the number of standard deviations {SD} the patient’s BMD was above or below the average BMD for a healthy 30-year-old Caucasian woman), to the lifetime risk of hip fracture. The diagnostic cutoff value (T-score > −2.5) was chosen since the lifetime risk of hip fracture in untreated Caucasian postmenopausal women (20%) matched the average T-score across this population (50–85 years) at the femoral neck [49]. From this data, the initial quantification suggested that the relative risk (RR) of lifetime fracture was approximately 2× greater for each SD that a patient’s BMD is below the average for the young normal healthy population. The development of the T-score launched bone densitometry into clinical medicine since it provided clinicians with a simple and fast way to make a diagnosis of PMO in a non-fractured patient and a simple single number to assess fracture risk by a noninvasive means [50].
However, it soon became clear that measurements of BMD had limited ability to predict the true risk of either hip fractures or all fractures (“global”). This was due to the recognition that there are other factors that contribute to bone fragility that are not captured by BMD. This group of factors found a new name, “bone quality,” to explain the non-BMD components of bone strength that may lead to fractures. While intense investigative efforts continue to define these non-BMD aspects of bone and have led to the quantification of independent variables that constitute bone quality (cortical porosity, stress-risers, remodeling space, remodeling rates, etc.), measurement of bone quality factors in clinical practice has escaped refinement [51–53]. Many of these bone quality factors are being differentiated in the CKD population from the osteoporotic population as independent contributors to bone strength, and will be discussed in the next section of this manuscript.
In the osteoporotic population, the first non-BMD-independent factor to be defined as a risk factor for fracture was increasing age [12]. Even before the WHO T-score was developed, it was published by the University of Indiana group that fracture risk approximately doubles by each decade above 50 years at the equivalent BMD. The reasons for this greater fracture risk as age increases are still not well defined but may have to do, in part, with alterations in bone quality with aging and with a greater risk of falling as age increases.
The second most robust risk factor for future fracture independent of the prevailing BMD is the number and/or type of prior low trauma fracture [1, 2, 17, 21, 23]. Exceptional data from multiple population, cohort, or placebo groups of osteoporosis pharmacological clinical trials have validated, for example, that the risk of any fracture is greater in a patient with 3 versus 1 prevalent vertebral fracture or is greater in a patient with a severe (grade 3) versus mild (grade 1) vertebral fracture [48, 54–59]. Prior vertebral fracture (or wrist fracture) [60, 61] not only predict a greater risk of future vertebral fractures, but also future non-vertebral fractures. The exact reason for this greater risk of fractures at sites distant from the initial fracture and independent of the T-score remains unclear. It might be that a low trauma fracture conveys some symbol of systemic skeletal fragility—another bone quality issue.
As it became clear that factors independent of BMD contributed to fracture risk, a number of international population studies were initiated to prospectively examine how risk factors independently and collectively contribute to future fracture risk prediction. These population studies led to the creation and implementation of the Fracture Risk Assessment Modeling (FRAX™) [32]. FRAX™ is the most robust longitudinal data acquired validating risk factors for fragility fractures in the postmenopausal and male populations over age 50. In addition, FRAX™ defined how independent risk factors interact to enhance risk prediction over 10 years in untreated populations. The risk factors captured and validated in FRAX™ are shown in Fig. 3, which is a template of how the input of the risk factors appears on the DXA or smartphone devices. FRAX™ calculates the 10-year risk of “all major” (clinical spine, hip, humerus, pelvis, and femur) or hip only fractures. FRAX™ sets “treatment thresholds” of 20% (major) or 3% (hip) which were based on health-economic data based on pharmacological therapy that costs ~$600 US/year. It is obvious that for osteoporosis drugs that cost less or more than the pharmacological costs calculated for cost-effectiveness in FRAX™ and that the intervention threshold for treatment will differ. Furthermore, FRAX™ did not capture a group of additional known independent risk factors for fracture (listed below) that also contribute to fracture risk and increase risk above and beyond that risk captured by the current FRAX™ model. This is not a criticism of the FRAX™ data but simply a function of the fact that when FRAX™ was initiated, these latter independent risk factors were not known. These separate risk factors that the clinician can assess clinically can be added to the risk calculated by FRAX™, though these “newer” risk factors have not been validated in the populations used to develop the “FRAX™ score.” They can, however, be a part of clinical judgment when deciding whether or not to treat an individual patient, especially in borderline cases where FRAX™ per se shows an uncertain risk. These other risk factors are as follows:
-
1.
Rate of bone turnover as assessed by biochemical markers of bone turnover
-
2.
Morphometric vertebral compression fractures
-
3.
Lumbar spine BMD
-
4.
Doses of glucocorticoids
-
5.
Frailty and fall risk
-
6.
Chronic kidney disease
The National Osteoporosis Foundation’s Clinician’s Guide for the utilization of FRAX™ in the United States health care system does include lumbar spine T-score of −2.5 or below or the presence of morphometric vertebral fractures that should be considered as independent factors for consideration of treatment [5]. In addition, the International Osteoporosis Foundation and the International Society for Clinical Densitometry recently published their Position Development Guidelines that addressed how to incorporate these other risk factors into the FRAX™ model [62]. These professional organizations have provided different levels of evidence on how to consider these other risk factors in the total risk calculation—with the exception of CKD.
Bone Mineral Density for Diagnosis and Risk Prediction in Patients with Reduced GFR
The osteoporosis and renal communities have just begun to come to an understanding as it relates to the utilization of BMD measurements by DXA in patients across the spectrum of CKD. This alignment is driven by a number of key developments:
-
1.
There were a number of the elderly patients in the FRAX™ populations who did have reduced GFR, though the sample size was inadequate to validate fracture risk by the level of GFR to be included in the FRAX™ model.
-
2.
The FDA approval for pharmacological therapies for PMO-randomized patients 60–90 years of age with known GFR down to 30 ml/min (i.e., stage 3 CKD).
-
3.
The US Surgeon General and the USPSTF both endorsed population screening of the elderly (65 years and older) postmenopausal population by DXA, which as a simple function of aging will include persons with reduced GFR.
Hence, it became important to the National Kidney Foundation working through the evidence provided by the Kidney Disease Improving Global Outcome (KDIGO) working group on bone metabolism across the spectrum of CKD that some agreement be achieved in how to apply the WHO criteria to these populations with known CKD.
In the nephrology community, the renal metabolic bone diseases associated with progressive CKD are given the name renal osteodystrophy when defined by quantitative histomorphometry [63–65] or CKD-MBD (chronic kidney disease-mineral and bone disorder) (Table 1) when defined by the abnormalities in bone turnover, mineralization, and volume, which are mediated by changes in parathyroid hormone, phosphorus retention, FGF-23, and metabolic acidosis [45]. The pathophysiological processes involved in CKD-MBD may explain the greater risk of fracture in the CKD population than seen in age-matched persons without CKD and in part, explain why DXA underestimates fracture risk in the CKD population.
Diagnosis of Osteoporosis and Prediction of Fracture Risk in Patients with Stage 1–3 CKD
While there is a greater risk of fracture even in stage 3 CKD (GFR 60–30 ml/min) than in age-matched patients without CKD, it is acceptable to use the WHO criteria for the diagnosis of osteoporosis in stage 1–3 CKD as it is in populations without known CKD. This criterion is predicated in the absence of any biochemical abnormalities that might suggest the concomitant presence of CKD-MBD: hyperphosphatemia and/or hyperparathyroidism, for example [45]. A recent study reported on 211 men and women with stages 3–5 CKD. There were 74 fractures in this group, and the numbers of subjects were distributed equally into stages 3, 4, and 5 CKD. Mean serum levels of parathyroid hormone (PTH) and phosphate were slightly above the normal reference range for all stages of CKD. The authors reported that BMD by DXA was able to discriminate fracture status but due to limited power could not comment on differences in fracture risk prediction by stage of CKD or biochemical abnormalities [66]. It is also important that the nephrology community recognizes that just because a PTH might be elevated in a patient with CKD, that the 2 may not be linked; for example, there are other causes of elevated serum PTH that could be unrelated to CKD [67] (Table 2). Hence, before concluding that osteoporosis by WHO criteria cannot be used in a patient with stage 3 CKD because they also have an elevated serum PTH and, therefore, have CKD-MBD, it is important to first exclude other non-renal related causes of elevated PTH; one of the most common and treatable causes being vitamin D insufficiency [68].
A word of clinical guidance about risk prediction using DXA in stage 3 CKD: while the standard rule for risk prediction in the general postmenopausal population using DXA is that RR is increased ~2× for each SD reduction in BMD, that risk will be higher in stage 3 CKD for reasons previously cited. Hence, the risk calculated by FRAX™ will also be higher in patients with stage 3 CKD than in comparable patients without stage 3 CKD. The exact magnitude of that greater risk is not validated but the clinician should take this greater risk into consideration when deciding on management strategies to reduce fracture risk in those with CKD.
Diagnosis of Osteoporosis and Prediction of Fracture Risk in Patients with Stage 4–5 CKD
The abnormalities in bone metabolism associated with CKD become far more manifested in stages 4–5 CKD. Phosphorus retention is greater, PTH levels are often higher (or lower if patients are receiving agents {vitamin D analogues or cinacalcet} that suppress PTH production), FGF-23 levels are higher, metabolic acidosis is more severe, and vitamin D metabolism is more deranged [45, 46, 69–73]. Because of this, BMD and bone strength may be modified by factors that are not present in postmenopausal or elderly male patients who do not have CKD. Due to the presence and severity of these multiple metabolic derangements in stage 4–5 CKD, it is not acceptable to use the WHO criteria for the diagnosis of osteoporosis. In addition, since all forms of renal osteodystrophy have reduced bone strength and are at greater risk of fragility fracture, low trauma fractures cannot be used to diagnose osteoporosis in severe CKD [74–81]. While osteoporosis, as defined by the National Institute of Health Consensus statement on osteoporosis [82], may also be a component of the aberrant bone metabolism observed in severe CKD, the additional metabolic abnormalities of bone defined within the defects encompassing CKD-MBD contribute independent negative effect on bone mineral content and bone strength that limit the use of DXA for diagnosis or risk prediction. The diagnosis of osteoporosis in stage 4–5 CKD is one of exclusion. By excluding the other histomorphometric forms of renal osteodystrophy in a patient with fragility fractures or low BMD, osteoporosis remains as the one metabolic bone disease that can also cause fractures in this population.
The gold standard test for exclusion is double tetracycline-labeled quantitative bone histomorphomery by transiliac bone biopsy [83–86]. Quantitative bone histomorphometry has established normative reference data created by The American Society for Bone and Mineral Research (ASBMR) [63] and is the only objective, scientific means of distinguishing among the different forms of renal osteodystrophy including: osteomalacia, osteitis fibrosa cystica (hyperparathyroid bone disease), mixed renal bone disease, and adynamic bone disease. If a patient with low trauma fractures does not have one of these 4 renal bone diseases, then the diagnosis of osteoporosis can be made. While bone biopsy is a safe procedure with little to no morbidity when performed by trained individuals, it is not readily accessible at this time. Even more limiting are the fewer competent quantitative histomorphometrists to read the biopsy for clinical purposes. Currently, a working group made up of many physicians skilled in performing and reading biopsies has been created to work toward improving access and reimbursement for quantitative biopsies. In the absence of quantitative histomorphometry, biochemical markers of bone turnover may have some, though limited, value to discriminate among the different forms of renal bone disease (Fig. 4) [87–94]. The markers that are not cleared by the kidney are the resorption marker tartrate-resistant acid phosphatase (TRAP5b) and the formation markers osteocalcin, bone-specific alkaline phosphatase (BSAP), and trimer form of propeptide type I collagen (PINP). Despite this physiological data on cleared versus non-cleared bone turnover markers, there is a paucity of data on how they correlate to a specific form of renal bone disease. Nevertheless, using biochemical markers such as PTH and BSAP to differentiate among the various forms of renal osteodystrophy do have some value, though they are insensitive and non-specific [95–100]. Biochemical markers cannot be used to diagnose osteoporosis, but PTH and/or BSAP may be able to provide some help with regard to what type of renal bone disease may be present. In patients not on agents that inhibit PTH synthesis, an intact PTH <150 pg/ml is strongly suggestive and <100 pg/ml highly suggestive of adynamic renal bone disease. This includes aluminum bone disease where aluminum also accumulated in the parathyroid gland, inhibiting PTH secretion [44]. An elevated BSAP excludes adynamic renal bone disease unless there has been a recent fracture. An elevated BSAP, however, may be due to other causes of increased BSAP, such as Paget’s disease, metaststic cancer to bone, hyperparathyroid bone disease, or osteomalacia. A low normal (lower quartile) BSAP is suggestive of low bone turnover; however, it does not have strong positive predictive value for this discrimination as much as a low PTH does (Fig. 5).
Comparison of HRpQCT between two age-matched and BMD-matched patients with and without chronic kidney disease [104]
In an attempt to try to add more scientific understanding to the greater reduction in bone strength across the spectrum of CKD that is not explained by low BMD by DXA, a great deal of investigation has used high-resolution peripheral quantitative computerized tomography (HRpQCT) to examine the microstructure of bone in patients with and without CKD [101–105]. HRpQCT has the capacity to discriminate between cortical and trabecular bone and can measure at a high resolution (~82 um). Measurements obtained from HRpQCT include: total volumetric BMD, total area, cortical area and trabecular area, cortical volumetric BMD, trabecular volumetric BMD, cortical thickness, trabecular thickness, and trabecular separation. The reproducibility (root-mean-square coefficient of variation) for density measurements at the distal radius is from 0.46 to 0.70%. There are significant differences between cortical and trabecular microarchitecture between aged-matched and BMD-matched patients with and without CKD. In patients with stage 5 CKD on dialysis (stage 5D), cortical HRpQCT measurements are strongly associated with fractures while no association is seen between BMD by DXA or HRpQCT trabecular parameters and fracture. However, a recent study comparing fracture prediction by DXA versus HRpQCT parameters (cortical thickness and total volumetric BMD in a stage 3–5, pre-dialysis population) did not show any significant discriminatory ability of one technique over the other [103]. In addition, receiver operator curves (ROC) in this study demonstrated that either a lower BMD by DXA or low cortical measures by HRpQCT were capable of discriminating non-fractured from fractured patients but that the two techniques were equally robust in fracture discrimination. These differences in the stage 5D and 3–5 pre-dialysis populations in HRpQCT discriminatory capacity may reflect the different forms of CKD-MBD in stage 3–5 pre-dialysis versus 5D populations.
The science is moving forward to measure and define the aspects of bone quality in people with and without CKD to explain the approximately 50% of fracture risk that is not captured by BMD by DXA in the PMO population without known CKD and even the larger proportion of risk not captured by DXA in the more severe CKD population. This does not discount the tremendous value that DXA provides in the assessment and management of patients with metabolic bone diseases––especially postmenopausal, male and glucocorticoid-induced osteoporosis [1, 2]. The issues surrounding DXA that are important in order to use it competently in patient management are defined below and include proper quality control and interpretation.
Mistakes Common in the Use of DXA in CKD:
-
1.
Comparing DXA results among different DXA manufacturers
-
2.
Not using the same region of interest (ROI) even with the same DXA manufacturer
-
3.
Monitoring patients with DXA without knowing the in vivo least significant change (LSC) or monitoring using T-scores rather than absolute BMD
-
4.
Underestimation of fracture risk when calculating risk using FRAX™
The International Society of Clinical Densitometry (ISCD.ORG) was created with the mission of educating both physicians and technologists in the science and clinical applications of DXA. The ISCD has developed well-respected international certification courses in bone mass measurements and published Position Development Conferences considering variable applications of DXA in various situations such as use in younger persons, using different reference population databases for development of T-scores, and many other clinical and research situations. A multispecialty organization, ISCD embraces other professional societies and organizations to try to bring standardization in DXA performance and interpretation. By doing so ISCD hopes to proactively mitigate errors in DXA utilization.
While there are many ways that DXA can be misused leading to incompetent results, diagnosis, and interpretation, there are 3 that the nephrologists should be cognizant of:
-
1.
Comparing DXA results among different DXA manufacturers
The 3 DXA manufacturers in the United States are Lunar-GE (Madison, Wisconsin), Hologic (Boston, Mass), and Nordland (Ft. Atkinson, Wis). All 3 of these DXA machines are excellent machines. However, they calibrate even the same bone ROI differently leading to different results (gram/cm²) even in the same patient. This fact has to do with many technological issues that have been well described [106]. The point is that measuring patients on DXA machines by different manufacturers will lead to different conclusions, especially when monitoring patients. For example, in the same patient the average BMD will be ~20% higher for the L1–L4 vertebral bodies on a Lunar-GE than a Hologic instrument. If one is not cognizant of this issue, patients can been told that they have lost (or gained) 20% of their BMD, when in fact it might not have changed at all if measured on another machine by the same manufacturer. This is just one of many examples of knowing how to use DXA will lead to correct management decisions.
-
2.
Not using the same ROI even with the same DXA manufacturer
The DXA machines have automatic edge detection systems for defining a particular ROI such as L1–L4, L1–L2, total hip, or femoral neck, for example. The DXA technologist can manually move the ROI at will if she/he does not agree with the automatic computer-generated ROI. Both approaches are correct, but it is vital that for proper interpretation of serial BMD measurements that the exact ROIs be compared. Comparing inconsistent ROIs leads to incorrect conclusions when monitoring either the basic biology of changes in bone over time or in response to pharmacological therapy.
-
3.
Monitoring patients with DXA without knowing the in vivo LSC or monitoring using T-scores rather than absolute BMD
In the serial measurements of any biological tests, there are errors in measurement. In part, these errors are biological and some are related to assays variability. In the case of serial measurements of BMD using DXA, the daily measurement of a phantom is part of the manufacturer-recommended quality control. In plotting the change in BMD with phantom scanning, the DXA technologists plot changes over time to see whether there are trends in precision errors which might suggest that, for example, the strength of the photon source is weakening. However, phantoms do not move and patients do. Therefore, if a competent DXA facility is to report serial BMD changes over time in human beings, it must perform in vivo precision studies. If in vivo precision studies are not done by a DXA facility, they have no means of knowing whether a change over time in DXA measurements is significant or not. There are published instructions on how to perform an in vivo precision study [18, 19, 28, 29, 107–111]. These instructions are also available on the ISCD website (ISCD.ORG). In clinical practice, more management errors are made in monitoring patients when the in vivo LSC.
-
4.
Underestimation of fracture risk when calculating risk using FRAX™
As previously mentioned, the validated risk factors captured in the 10-year risk model by FRAX™ did not have an adequate sample size to incorporate CKD into the risk assessment. From the published population studies, it appears that fracture risk odds ratios ~ doubles when GFR is <60 ml/min. Since BMD measurements are often done in the elderly population, many of whom may also have reduced GFR, it would make sense that the validated FRAX™ calculations probably underestimate risk in these patients. While this additional risk may not be capable of being quantitated, it would seem reasonable to increase the patients risk to some degree above that risk calculated by FRAX™ if they also have stage 3 CKD.
Conclusions
Measurements of BMD by DXA have been the single greatest advancement in the past 25 years that have allowed clinical decisions to be made in the office setting for the diagnosis of osteoporosis, assessment of fracture risk, and monitoring pharmacological response. Knowledge of these applications led to the US government endorsing population screening using DXA. However, neither the development of the T-score nor the validation of FRAX™ for risk assessment included renal function. Since the populations that develop osteoporosis may also develop age-related reductions in renal function, it is important that all physicians, including nephrologists, think about how to incorporate BMD measurements by DXA. While WHO criteria and risk assessment can be used similarly between the PMO and CKD (stage 1–3) populations, it is important to consider that if patients have biochemical evidence of CKD-MBD that a different or concomitant metabolic bone disease, not just osteoporosis, may be present. In addition, even by stage 3 CKD the risk of fracture seems to be higher than the fracture risk calculated by FRAX™ alone. Neither the WHO diagnostic criteria nor risk assessment by DXA are valid in stage 4–5 CKD. BMD measurements may still have value in these more severe stages of CKD because baseline BMD values provide means of measuring change over time. In order for competent DXA measurements to provide accurate information to physicians managing patients with osteoporosis, there are education programs available that provide skills in performance of DXA measurements for physicians and technologists alike. Scientific efforts are very active to investigate other noninvasive means of quantitating the additional and independent bone quality factors that contribute to the greater risk of fragility fracture in the CKD population that are not captured by DXA. HRpQCT is the most advanced of these newer modalities at the current time.
References
Miller PD, Bonnick SL. Clinical application of bone densitometry. In: Favus MJ, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 4th edn. American Society for Bone and Mineral Research. Philadelphia, PA: Lippincott Williams & Wilkins; 1999.
Bonnick SL, Miller PD. Clinical use of bone densitometry. In: Marcus R, Rosen C, Feldman D, editors. Osteoporosis. Philadelphia, PA: Lippincott, Williams and Wilkons; 2012.
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser; Geneva; WHO. 1994;843:1–129.
ISCD 2007 official positions and pediatric official positions of the International Society for Clinical Densitometry. 2007. http://www.iscd.org/visitors/positions/OfficialPositionsText.cfm. Accessed 23 Nov 2011.
National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. Washington, DC: National Osteoporosis Foundation; 2010.
Watts NB, Bilezikian JP, Camacho PM, Greenspan SL, Harris ST, Hodgson SF, Kleerekoper M, Luckey MM, McClung MR, Pollack RP, Petak SM. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Prac. 2010;16(S3):1–37.
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstorm F, Rizzoli R. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19(4):399–428.
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42:467–75.
Kanis JA, Glüer CC, for the Committee of Scientific Advisors International Osteoporosis Foundation. An update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporos Int. 2000;11:192–202.
Kanis JA, Gianchi G, Bilezikian JP, Kaufman JM, Kholsa S, Orwoll E, Seeman E. Towards a diagnostic and therapeutic consensus in male osteoporosis. Osteoporos Int. 2011;22:2789–98.
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ III, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A. Predictive value of bone mineral density for hip and other fractures. J Bone Miner Res. 2005;20:1185–94.
Hui SL, Slemenda CW, Johnston CC. Baseline measurement of bone mass predicts fracture in white women. Ann Intern Med. 1989;111:355–61.
Gardsell P, Johnell O, Nilsson BE. The predictive value of bone loss for fragility fractures in women: a longitudinal study over 15 years. Calcif Tissue Int. 1991;49:90–4.
Black DM, Cummings SR, Genant HK, Nevitt MC, Palermo L, Browner W. Axial and appendicular bone density predict fractures in older women. J Bone Miner Res. 1992;7:633–8.
Melton LJ, Atkinson EJ, O’Fallon WM, Wahner HW, Riggs BL. Long-term fracture prediction by bone mineral assessed at different skeletal sites. J Bone Miner Res. 1993;8:1227–33.
Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM. Bone density at various sites for prediction of hip fracture. The study of osteoporotic fractures research group. Lancet. 1993;341:72–5.
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–97.
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, Hanley DA, Hodsman A, Jamal SA, Kaiser SM, Kvern B, Siminoski K, Leslie WD. Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–73.
Comptson J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M. Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Updated July 2010. http://www.shef.ac.uk/NOGG/downloads.html. Accessed 22 May 2011.
2010 Official positions of the ISCD/IOF on the interpretation and use of FRAX in clinical practice. 2010. http://www.iscd.org/Visitors/positions/OfficialPositionsText.cfm. Accessed 26 Nov 2011.
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, Cauley JA, Compston JE, Dawson-Hughes B, El-Hajj Fuleihan G, Johansson H, Leslie WD, Lewiecki EM, Luckey M, Oden A, Papapoulos SE, Poiana C, Rizzoli R, Wahl DA, McCloskey EV; Task Force of the FRAX Initiative. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22:2395–2411.
Siminoski K, Leslie WD, Frame H, Hodsman A, Josse RG, Khan A, Lentle BC, Levesque J, Lyons DJ, Tarulli G, Brown JP. Recommendations for bone mineral density reporting in Canada: a shift to absolute fracture risk assessment. J Clin Densitom. 2007;10:120–3.
Leslie WD, Lix LM. Simplified 10-year absolute fracture risk assessment: a comparison of men and women. J Clin Densitom. 2010;13:141–6.
Leslie WD, Berger C, Langsetmo L, Lix LM, Adachi JD, Hanley DA, Ioannidis G, Josse RG, Kovacs CS, Towheed T, Kaiser S, Olszynski WP, Prior JC, Jamal S, Kreiger N, Goltzman D. Construction and validation of a simplified fracture risk assessment tool for Canadian women and men: results from the CaMos and Manitoba cohorts. Osteoporos Int. 2011;22:1873–83.
Simons LA, McCallum J, Simons J, Powell I, Ruys J, Heller R, Lebra C. The Dubbo study: an Australian prospective community study of the health of elderly. Aust NZ J Med. 1990;20:783–9.
Sandhu SK, Nguyen ND, Center JR, Pocock NA, Eisman JA, Nguyen TV. Prognosis of fracture: evaluation of predictive accuracy of the FRAX™ algorithm and Garvan nomogram. Osteoporos Int. 2010;21:863–71.
Langsetmo L, Nguyen TV, Nguyen ND, Kovacs CS, Prior JC, Center JR, Morin S, Josse RG, Adachi JD, Hanley DA, Eisman JA. Independent external validation of nomograms for predicting risk of low-trauma fracture and hip fracture. CMAJ. 2011;183:E107–14.
Bonnick SL, Shulman L. Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both? Am J Med. 2006;119:S25–31.
Miller PD. Monitoring osteoporosis therapies. Curr Osteoporos Rep. 2007;5:38–43.
Annals Int Med. 2010. http://www.ahrq.gov. USPSTF.
US Department of Health and Human Services. Bone health and osteoporosis: a report of the surgeon general. Rockville, MD: US Department of Health and Human Services, Office of the Surgeon General; 2004.
National Osteoporosis Foundation Clinician's Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation. Available at: http://www.nof.org/sites/default/files/pdfs/NOF_ClinicianGuide2009_v7.pdf. Accessed 14 Aug 2011.
Klawansky S, Komaroff E, Cavanaugh PF Jr, Mitchell DY, Gordon MJ, Connelly JE, Ross SD. Relationship between age, renal function and bone mineral density in the US population. Osteoporos Int. 2003;14:570–6.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van LF, Levey AS. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Glassock RJ, Winearls C. Ageing and the glomerular filtration rate: truths and consequences. Trans Am Clin Climatol Assoc. 2009;120:419–28.
Abdelhafiz AH, Brown SH, Bello A, El Nahas M. Chronic kidney disease in older people: physiology, pathology or both? Nephron Clin Pract. 2010;116(1):c19–24.
Duru OK, Vargas RB, Kermah D, Nissenson AR, Norris KC. High prevalence of stage 3 chronic kidney disease in older adults despite normal serum creatinine. J Gen Intern Med. 2009;24:86–92.
Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third national health and nutrition examination survey. Am J Kidney Dis. 2003;41(1):1–12.
Dukas L, Schacht E, Stahelin HB. In elderly men and women treated for osteoporosis a low creatinine clearance of < 65 ml/min is a risk factor for falls and fractures. Osteoporos Int. 2005;16(12):1683–90.
Ensrud KE, Lui L, Taylor BC, Ishani A, Shlipak MG, Stone KL, Cauley JA, Jamal SA, Antoniucci DM, Cummings SR. Renal function and risk of hip and vertebral fractures in older women. Arch Intern Med. 2007;167:133–9.
Fried LF, Biggs ML, Shlipak MG, Seliger S, Kestenbaum B, Stehman-Breen C, Sarnak M, Siscovick D, Harris T, Cauley J, Newman AB, Robbins J. Association of kidney function with incident hip fracture in older adults. J Am Soc Nephrol. 2007;18(1):282–6.
Nickolas TL, McMahon DJ, Shane E. Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol. 2006;17(11):3223–32.
Gal-Moscovici A, Sprague SM. Osteoporosis and chronic kidney disease. Semin Dial. 2007;20:423–30.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;2002(39):S1–266.
Moe S, the Kidney Disease Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD–MBD). Kidney Int. 2009;76(113):S1–130.
Jüppner H, Wolf M, Salusky IB. FGF-23: more than a regulator of renal phosphate handling? J Bone Miner Res. 2010;25(10):2091–7.
Isakova T, Wahl P, Vargas GS, Gutiérrez OM, Scialla J, Xie H, Appleby D, Nessel L, Bellovich K, Chen J, Hamm L, Gadegbeku C, Horwitz E, Townsend RR, Anderson CA, Lash JP, Hsu CY, Leonard MB, Wolf M. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 2011;79(12):1370–8.
Isakova T, Xie H, Yang W, Xie D, Anderson AH, Scialla J, Wahl P, Gutiérrez OM, Steigerwalt S, He J, Schwartz S, Lo J, Ojo A, Sondheimer J, Hsu CY, Lash J, Leonard M, Kusek JW, Feldman HI, Wolf M, Chronic Renal Insufficiency Cohort (CRIC) Study Group. Fibroblast growth factor 23 and risks of mortality and end-stage renal disease in patients with chronic kidney disease. JAMA. 2011;305(23):2432–9.
Melton LJ III, Chrischilles EA, Cooper C, Lane AW, Riggs BL. How many women have osteoporosis? JBMR anniversary classic. J Bone Miner Res. 2005;20(5):886–92.
Miller PD, Bonnick SL, Rosen CJ. Consensus of an international panel on the clinical utility of bone mass measurement in the detection of low bone mass in the adult population. Calcif Tissue Int. 1996;58:207–14.
Bouxsein ML. Non-invasive measurements of bone strength: promise and peril. J Musculoskelet Neuronal Interact. 2004;4:404–5.
Seeman E. Bone quality: the material and structural basis of bone strength. J Bone Miner Metab. 2008;26:1–8.
Genant HK, Lang TF, Engelke K, et al. Advances in the noninvasive assessment of bone density, quality, and structure. Calcif Tissue Int. 1996;59(suppl 1):S10–5.
Adams JE, Lenchik L, Roux C, Genant HK. Radiologic assessment of vertebral fracture. Vertebral fracture initiative, part II. 2011. http://www.iofbonehealth.org/index.php?id=574. Accessed 25 Nov 2011.
Schousboe JT, Vokes T, Binkley N, Genant HK. Densitometric vertebral fracture assessment (VFA). Vertebral fracture initiative, part III. 2011. http://www.iofbonehealth.org/index.php?id=574. Accessed 25 Nov 2011.
Rea JA, Li J, Blake GM, Steiger P, Genant HK, Fogelman I. Visual assessment of vertebral deformity by X-ray absorptiometry: a highly predictive method to exclude vertebral deformity. Osteoporos Int. 2000;11:660–8.
Schousboe JT, DeBold CR, Bowles C, Glickstein S, Rubino RK. Prevalence of vertebral compression fracture deformity by X-ray absorptiometry of lateral thoracic and lumbar spines in a population referred for bone densitometry. J Clin Densitom. 2002;5:239–46.
Nevitt MC, Ross PD, Palermo L, Muslinger T, Genant HK, Thompson DE. Association of prevalent vertebral fractures, bone density and alendronate treatment with incident vertebral fractures: effect of number and spinal location. Bone. 1999;25(5):613–9.
Davis JW, Grove JS, Wasnich RD, Ross PD. Spatial relationships between prevalent and incident spine fractures. Bone. 1999;24:261–4.
Siris E, Miller P, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, Berger ML, Santora AC, Sherwood LM. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the national osteoporosis risk assessment. JAMA. 2001;286:2815–22.
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–39.
International Society for Clinical Densitometry-International Osteoporosis Foundation Position Development Conferences. J Clin Densit. 2011;14(3):171–243.
Parfitt AM, Drezner M, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR. Bone histomorphometry: standardization of nomenclature, symbols, and units. report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res. 1987;2:595–610.
Parfitt AM. Renal bone disease: a new conceptual framework for the interpretation of bone histomorphometry. Curr Opin Nephrol Hypertens. 2003;12:387–403.
Andress DL, Sherrard DJ. The osteodystrophy of chronic renal failure. In: Schrier RW, editor. Diseases of the kidney and urinary tract. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. p. 2431–53.
Jamal SA, West SL, Cheung AM, Lok CE. Tests of bone density and structure are associated with fractures in stage 3–5 chronic kidney disease. J Bone Miner Res. 2011;26(supplement 1 abstract book).
Malluche HH, Faugere MC. Renal osteodystrophy. N Engl J Med. 1989;321:317–8.
Lewiecki EM, Bilezikian JP, Khosla S, Marrcus R, McClung, Miller PD, Watts NB, Maricic M. Osteoporosis update from the 2010 Santa Fe Bone symposium. J Clin Densit. 2011;14(1):1–21.
Miller PD, Vitamin D. Calcium, and cardiovascular mortality: a perspective from a plenary lecture given at the annual meeting of the American Association of Clinical Endocrinologists. Endocr Pract. 2011;17(5):798–806.
Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, Andress DL. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007;71:31–8.
Vassalotti JA, Uribarri J, Chen SC, Li S, Wang C, Collins AJ, Calvo MS, Whaley-Connell AT, McCullough PA, Norris KC, Kidney Early Evaluation Program Investigators. Trends in mineral metabolism: kidney early evaluation program (KEEP) and the national health and nutrition examination survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 suppl 2):S56–S68.
Lehmann G, Ott U, Kaemmerer D, Schuetze J, Wolf G. Bone histomorphometry and biochemical markers of bone turnover in patients with chronic kidney disease stages 3–5. Clin Nephrol. 2008;70:296–305.
Hitt O, Jaworski ZF, Shimizu AG, Frost HM. Tissue-level bone formation rates in chronic renal failure, measured by means of tetracycline bone labeling. Can J Physiol Pharmacol. 1970;48:824–8.
Elder GJ, Mackun K. 25-Hydroxyvitamin D deficiency and diabetes predict reduced BMD in patients with chronic kidney disease. J Bone Miner Res. 2006;21(11):1778–84.
Jadoul M, Albert JM, Akiba T, Akizawa T, Arab L, Bragg-Gresham JL, Mason N, Prutz KG, Young EW, Pisoni RL. Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the dialysis outcomes and practice patterns study. Kidney Int. 2006;70:1358–66.
Nickolas TL, Leonard MB, Shane E. Chronic kidney disease and bone fracture: a growing concern. Kidney Int. 2008;74:721–31.
Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:396–9.
Ball AM, Gillen DL, Sherrard D, Weiss NS, Emerson SS, Seliger SL, Kestenbaum BR, Stehman-Breen C. Risk of hip fracture among dialysis and renal transplant recipients. JAMA. 2002;288:3014–8.
Stehman-Breen CO, Sherrard DJ, Alem AM, Gillen DL, Heckbert SR, Wong CS, Ball A, Weiss NS. Risk factors for hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:2200–5.
Wehrli FW, Leonard MB, Saha PK, Gomberg BR. Quantitative high resolution magnetic resonance imaging reveals structural implications of renal osteodystrophy on trabecular and cortical bone. J Magn Reson Imaging. 2004;20:83–9.
Coen G. Adynamic bone disease: an update and overview. J Nephrol. 2005;18:117–22.
Andress DL. Adynamic bone in patients with chronic kidney disease. Kidney Int. 2008;73(12):1345–54.
NIH Consensus Development Panel Osteoporosis Prevention Diagnosis and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–95.
Miller PD. The role of bone biopsy in patients with chronic renal failure. Clin J Am Soc Nephrol. 2008;3(suppl 3):S140–50.
Frost HM. Tetracycline-based histological analysis of bone remodeling. Calcif Tissue Res. 1969;3:211–37.
Ferreira MA. Diagnosis of renal osteodystrophy: when and how to use biochemical markers and non-invasive methods; when bone biopsy is needed. Nephrol Dial Transplant. 2000;15(suppl 5):8–14.
Trueba D, Sawaya BP, Mawad H, Malluche HH. Bone biopsy: indications, techniques, and complications. Semin Dial. 2003;16:341–5.
Miller PD. Bone density and markers of bone turnover in predicting fracture risk and how changes in these measures predict fracture risk reduction. Curr Osteoporos Rep. 2005;3:103–10.
Miller PD, Hochberg MC, Wehren LE, Ross PD, Wasnich RD. How useful are measures of BMD and bone turnover? Curr Med Res Opin. 2005;21:545–54.
Chavassieux PM, Delmas PD. Bone remodeling: biochemical markers or bone biopsy? J Bone Miner Res. 2006;21:178–9.
Garnero P. Biomarkers for osteoporosis management: utility in diagnosis, fracture risk prediction and therapy monitoring. Mol Diagn Ther. 2008;12:157–70.
Meier C, Seibel MJ, Kraenzlin ME. Use of bone turnover markers in the real world: are we there yet? J Bone Miner Res. 2009;24:386–8.
Vasikaran S, Eastell R, Bruyere O, Foldes AJ, Garnero P, Griesmacher A, McClung MR, Morris HA, Silverman S, Trenti T, Wahl DA, Cooper C, Kanis JA, for the IOF-IFCC Bone Markers Standard Working Group. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int. 2011;22:391–420.
Adami S, Bianchi G, Brandi ML, Giannini S, Ortolani S, Dimunno O, Frediani B, Rossini M. Determinants of bone turnover markers in healthy premenopausal women. Calcif Tissue Int. 2008;82:341–7.
Baim S, Miller PD. Perspective: assessing the clinical utility of serum CTX in postmenopausal osteoporosis and its use in predicting risk of osteonecrosis of the jaw. J Bone Miner Res. 2009;24:561–73.
Barreto FC, Barreto DV, Moyses RM, Neves KR, Canziani ME, Draibe SA, Jorgetti V, Carvalho AB. K/DOQI-recommended intact PTH levels do not prevent low-turnover bone disease in hemodialysis patients. Kidney Int. 2008;73(6):771–7.
Rocha LA, Higa A, Barreto FC, dos Reis LM, Jorgetti V, Draibe SA, Carvalho AB. Variant of adynamic bone disease in hemodialysis patients:fact or fiction. Am J Kidney Dis. 2006;48(3):430–6.
Urena P, De Vernejoul MC. Circulating biochemical markers of bone remodeling in uremic patients. Kidney Int. 1999;55:2141–56.
Coen G, Ballanti P, Bonucci E, Calabria S, Centorrino M, Fassino V, Manni M, Mantella D, Mazzaferro S, Napoletano I, Sardella D, Taggi F. Bone markers in the diagnosis of low turnover osteodystrophy in haemodialysis patients. Nephrol Dial Transplant. 1998;13:2294–302.
Bervoets AR, Spasovski GB, Behets GJ, Dams G, Polenakovic MH, Zafirovska K, Van Hoof VO, De Broe ME, D’Haese PC. Useful biochemical markers for diagnosing renal osteodystrophy in predialysis end-stage renal failure patients. Am J Kidney Dis. 2003;41:997–1007.
Jamal SA, Hayden JA, Beyene J. Low bone mineral density and fractures in long-term hemodialysis patients: a meta-analysis. Am J Kidney Dis. 2007;49(5):674–81.
Jamal SA, Gilbert J, Gordon C, Bauer DC. Cortical PQCT measures are associated with fractures in dialysis patients. J Bone Miner Res. 2006;21:543–8.
Nickolas TL, Cremers S, Zhang A, Thomas V, Stein E, Cohen A, Chauncey R, Nikkel L, Yin MT, Liu XS, Boutroy S, Staron RB, Leonard MB, McMahon DJ, Dworakowski E, Shane E. Discriminants of prevalent fractures in chronic kidney disease. J Am Soc Nephrol. 2011;22(8):1560–72.
Nickolas TL, Stein E, Cohen A, Thomas V, Staron RB, McMahon DJ, Leonard MB, Shane E. Bone mass and microarchitecture in CKD patients with fracture. J Am Soc Nephrol. 2010;21:1371–80.
Leonard MB. A structural approach to skeletal fragility in chronic kidney disease. Semin Nephrol. 2009;29(2):133–43.
Fan B, Lu Y, Genant H, Fuerst T, Shepard J. Does standardized BMD still remove differences between Hologic and GE-Lunar state-of-the art DXA systems? Osteoporos Int. 2010;21(7):1227–36.
International Organization of Standardization. Accuracy (trueness and precision) of measurement methods and results—part 1: general principles and definition. 1st [ISO 5725-1]. Switzerland, ISO. International Standard. International Organization of Standardization. 1994. pp. 1–17.
Kiebzak GM, Morgan SL. Long-term versus short-term precision of dual-energy X-ray absorptiometry scans and the impact on interpreting change in bone mineral density at follow-up. J Clin Densitom. 2011;14:108–15.
Bonnick SL, Johnston CC Jr, Kleerekoper M, Lindsay R, Miller P, Sherwood L, Siris E. Importance of precision in bone density measurements. J Clin Densitom. 2001;4:105–10.
Lenchik L, Kiebzak GM, Blunt BA. What is the role of serial bone mineral density measurements in patient management? J Clin Densitom. 2002;5:S29–38.
Leslie WD, Moayyeri A. Minimum sample size requirements for bone density precision assessment produce inconsistency in clinical monitoring. Osteoporos Int. 2006;17:1673–80.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, P.D., Jamal, S.A. & West, S.L. Bone Mineral Density in Chronic Kidney Disease Use and Misuse. Clinic Rev Bone Miner Metab 10, 163–173 (2012). https://doi.org/10.1007/s12018-012-9130-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12018-012-9130-1