Abstract
Autoimmune liver diseases (AILDs) are potentially life-threatening chronic liver diseases which include autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, and recently characterized IgG4-related sclerosing cholangitis. They are caused by immune attack on hepatocytes or bile ducts, with different mechanisms and clinical manifestations. The etiologies of AILDs include a susceptible genetic background, environment insults, infections, and changes of commensal microbiota, but remain complicated. Understanding of the underlying mechanisms of AILDs is mandatory for early diagnosis and intervention, which is of great importance for better prognosis. Thus, animal models are developed to mimic the pathogenesis, find biomarkers for early diagnosis, and for therapeutic attempts of AILDs. However, no animal models can fully recapitulate features of certain AILD, especially the late stages of diseases. Certain limitations include different living condition, cell composition, and time frame of disease development and resolution. Moreover, there is no IgG4 in rodents which exists in human. Nevertheless, the understanding and therapy of AILDs have been greatly advanced by the development and mechanistic investigation of animal models. This review will provide a comprehensive overview of traditional and new animal models that recapitulate different features and etiologies of distinct AILDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human liver is a tolerogenic organ [1]. It continuously receives insults from the blood circulation and maintains an environment of tolerance [2, 3]. However, the liver is also the effector site of many systemic immune reactions which may result in chronic liver inflammation and the development of autoimmune liver diseases (AILDs). AILDs include autoimmune hepatitis (AIH), primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), and recently characterized IgG4-related sclerosing cholangitis (IgG4-SC). They can progress into liver dysfunction, such as cholestasis, fibrosis, cirrhosis, and liver cancer. Although the etiologies remain to be clarified, AILDs are thought to develop with a susceptible genetic background and further environmental insults such as infections and chemicals [4].
AILDs often develop imperceptibly; thus, early diagnosis and understanding of the disease processes are very important for prognosis and disease management [5,6,7]. Animal models are powerful tools to understand the immunopathogenesis of AILDs and discover serological markers for early diagnosis and immunological checkpoints as targets for treatment [8]. Thus, many transgenic, chemical-induced, infection-induced animal models are developed, which greatly advance the knowledge of distinct AILDs and overlap syndromes. In this review, we will give a comprehensive overview of commonly used and newly developed animal models of human AILDs, as well as the limitations and challenges of these models. As most of the models are induced in mice and rats, we focus on murine models of AILDs in this review.
AIH
AIH is a female predominant chronic and self-perpetuating inflammatory disease [9]. It affects all ages and races. AIH usually starts with an episode of acute hepatitis [7, 10,11,12]. Elevation of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and immunoglobulins especially IgG in the serum is detected in AIH, which are used for the definition of biochemical remission [12]. In addition, autoantibodies including antinuclear antibodies (ANAs), smooth muscle antibodies (SMAs), anti-LMK1, and anti-cytochrome P4502D6 (CYP2D6) antibodies can be detected in the serum of AIH patients [7]. Inflammatory damage to the liver is an essential feature of AIH [13], with other non-AIH-specific features such as lymphoplasmacytic infiltrates, hepatocyte resetting, and emperipolesis [14]. Current treatment of AIH is prednisolone alone or in combination with azathioprine, which are immunosuppressants [15]. Although the etiology of AIH is unknown, both genetic and environmental triggers are possibility involved [16]. The genetic association, especially human leukocyte antigen (HLA) region, is so strong that some genes like HLA-DR3 (DRB1*03:01) and HLA-DR4 (DRB1*04:01) are considered susceptibility factors of AIH [7]. To further understand the liver immunology and pathological mechanisms of AIH, several animal models are developed (Table 1 and Fig. 1). Knowledge gained from these models will help to identify novel therapeutic targets for AIH [17].
Animal models of AIH and disease characteristics. AIH can be induced in animals through surrogate antigen inoculation, liver homogenate immunization, genetic modification, liver autoantigen induction, and virus infection. Con A can bind to LSECs and macrophages which can induce activation of T cells and NKT cells. T cells and NKT cells can induce apoptosis of hepatocytes and LSECs through IFN-γ and TNF-α production. α-GalCer can induce TNF-α production by NKT cells, which can induce apoptosis of hepatocytes. Homogenate proteins can be presented to expand autoreactive T cells which can recognize self-antigens and promote the production of autoantibodies. PD-1 knockout mice with thymectomy lack Treg cells which results in spontaneous activation of T cells. Infection of mice with adenovirus which express liver autoantigens such as CYP2D6 and FTCD can also induce the activation of autoreactive T cells and production of autoantibodies. MHV A259 infection can generate FAH analogue which induce FAH-specific T cells and the development of autimmune hepatitis
Spontaneous Models
NTxPD-1−/− mice are reported to be the first mouse model of spontaneous fatal AIH, resembling acute-onset AIH presenting as fulminant hepatic failure in humans [18]. NTxPD-1−/− mice have a concurrent loss of naturally arising regulatory T (Treg) cells and PD-1-mediated signaling, which results in T cell activation and infiltration into liver parenchyma, massive lobular necrosis, and generation of ANA. Similar to human AIH, administration of dexamethasone prevents disease development, while dexamethasone removal leads to relapse of AIH [19]. In this model, dysregulated generation of follicular helper T cells, which migrate to the liver through expressing CCR6, is critical for disease development [20]. Moreover, CD8+ T cells infiltrating in the liver also contribute to liver injury through producing inflammatory cytokines, such as INF-γ [21] and TNF-α [22]. However, due to the massive destruction of the parenchyma of the liver, these mice start to die as early as 2 weeks of age, with most dying by 4 weeks. In summary, NTxPD-1−/− mice represent the first mouse model of spontaneous fatal AIH, but the short lifespan limits its application for more mechanistic studies.
Models Induced by Surrogate Antigens
Concanavalin A–Induced Hepatitis
Concanavalin A (ConA) induces acute immune-mediated liver injury, by activation of antigen non-specific T cells and macrophages in a dose-dependent manner [23]. ConA mainly accumulates in the liver and binds to mannose-rich glycoproteins on liver sinusoidal endothelial cells (LSECs) and Kupffer cells, which can further induce firm cellular arrest of T cells [24]. T cells, especially NKT cells, secrete inflammatory cytokines such as IFN-γ and TNF-α, which subsequently recruit and active other cells and induce apoptotic cell death of LSECs and hepatocytes [25, 26]. IFN-γ may also upregulate TNF receptors on hepatocytes, potentiating TNF-induced DNA fragmentation and hepatotoxicity [27]. In summary, ConA-induced hepatitis is a valuable model for highly specific activation of T cells, and has extensive applications in investigating the mechanisms of T cell function in AIH. However, it is a cytokine-dependent and antigen-independent model of liver injury, and is acute rather than chronic.
α-Galactosylceramide–Induced Hepatitis
α-Galactosylceramide (α-GalCer) is a synthetic glycolipid which can be recognized by invariant NKT cells through CD1d [28]. It is reported that α-GalCer can induce hepatic injury that resemble human acute AIH [29, 30]. Mice injected with α-GalCer show necrosis of hepatocytes and lymphocytic infiltration in the liver, with increased ALT, AST, and ANA levels in the serum. In this model, TNF-α but not Kupffer cells mediate α-GalCer-induced liver injury [31]. Activation of NKT cells results in their secretion of IL-4 and IFN-γ, which differentially regulate neutrophil accumulation and hepatitis development [32]. It is also reported that IL-17 protects liver injury in this model possibly through regulating NKT chemoattractant chemokines [33]. However, whether activation of NKT cells is the cause of human AIH remains unknown.
Models Induced by Liver Autoantigens
Liver Homogenate–Induced Hepatitis
Administration of liver extracts can successfully break the liver tolerance and induce pathological features of AIH, which is called experimental autoimmune hepatitis. Monthly injection of syngeneic liver homogenate together with the polysaccharide of Klebsiella pneumoniae 03:K1 as adjuvant induces infiltration of mononuclear cells consisting mainly of lymphocytes in portal areas and piecemeal necrosis in mice [34]. Significantly, transfer of splenocytes from AIH-like mice into naive recipients can induce features of AIH. Another model is generated by intraperitoneal immunization of male C57BL/6 mice with the 100,000×g supernatant of syngeneic liver homogenate (S-100) emulsified in Freund’s adjuvant. This results in inflammatory infiltrates and hepatocyte necrosis and generation of S-100 protein-specific T cells [35]. This approach is simple and has been used widely in searching for the mechanisms of AIH, like the important role of the mitogen-activated protein kinase p38 [36], and CD11b+ regulatory B cells [37]. However, the real identity of both the triggering antigen as well as the target liver autoantigens remains known. In summary, these models are generated by injection of liver extracts with largely unknown compositions.
Liver Autoantigen–Induced Hepatitis
CYP2D6, mainly aa193–212, is the immunodominant and possibly the best characterized autoantigen recognized by T cells from patients with AIH-2 [38]. Thus, CYP2D6 is considered as a model antigen of AIH [39]. The CYP2D6 model is generated by infecting wild-type FVB mice with an adenovirus encoding human CYP2D6 (Ad-2D6) [40]. Infection with Ad-2D6 results in two distinct phases of liver damage: an acute hepatic inflammation, characterized by transient elevation of serum aminotransferase levels and minor cellular infiltration, followed by chronic AIH-like disease characterized by massive hepatocellular damage, strong cellular infiltration, high titer anti-CYP2D6 antibodies, and extensive hepatic fibrosis [41]. It is interesting that the T cell epitopes are located in regions of intermediate homology between the triggering hCYP2D6 and the target mouse Cyp homologs, which indicates molecular mimicry rather than identity breaks T cell tolerance [42]. Although lymphocytes are involved in destruction and continuous inflammation, activated hepatic stellate cells play an essential role in periportal and especially subcapsular fibrosis through producing massive amounts of extracellular matrix proteins such as collagen I and α-smooth muscle actin [40]. In summary, the CYP2D6 model displays persistent cellular infiltration and liver fibrosis, offering the opportunity for a detailed investigation of the mechanisms of chronic autoimmune-mediated liver fibrogenesis. Besides, the direct delivery of CYP2D6 by an adenovirus guarantees both direct targeting of the liver and local inflammation that promotes the breakdown of tolerance.
Besides CYP2D6, the target of LC1 antibodies, hepatic autoantigen formiminotransferase cyclodeaminase (FTCD), has also been used to generate murine model of AIH [43, 44]. In this model, non-obese diabetic (NOD) mice infected with Ad-FTCD develop a chronic AIH-like disease after an initial transient acute hepatitis. However, hepatitis can only be induced in NOD mice but not wild-type FVB/N or C57BL/6 mice, suggesting that a genetic predisposition is required in this model [43]. Notably, immunization with a plasmid expressing both CYP2D6 and FTCD generates high titer of both anti-LKM1 and anti-LC1 antibodies in mice [45].
Mouse Hepatic Virus A59 Infection–Induced Hepatitis
Another model of AIH is induced by infecting wild-type C57BL/6 mice with MHV A59, which generates autoantibodies to fumarylacetoacetate hydrolase (FAH), a soluble cytosolic enzyme present in the liver and kidneys [46]. MHV A59 infection results in hepatitis associated with transient hypergammaglobulinemia, elevated transaminases, and autoantibodies against various liver proteins, which resemble human fulminant hepatitis [47]. In this model, neutrophils contribute to the development of hepatits through their expression of macrophage scavenger receptor 1 and activation of the complement system [48].
PBC
PBC is characterized by the presence of antimitochondrial antibodies (AMAs) in the serum and the destruction of intrahepatic bile ducts accompanied by portal inflammation, which in turn leads to progressive cholestasis, liver fibrosis, and, severely, cirrhosis [49,50,51]. The incidence of PBC predominates among middle-aged women, with a male-to-female ratio of approximately 1:9 [52]. A number of important observations have greatly advanced the approach to PBC pathogenesis [49]. First, AMAs, particularly antibody against pyruvate dehydrogenase complex-E2 (PDC-E2), can be detected several years before the clinical diagnosis of the disease [53, 54]. Second, the proportions of autoreactive CD4+T and CD8+T cells in the liver are significantly increased, especially around the small bile ducts [49, 55]. Third, patients manifest elevated levels of serum pro-inflammatory cytokines such as IFN-γ and TNF-α [56]. Fourth, the proportion and number of functional Treg cells in PBC patients are decreased [57].
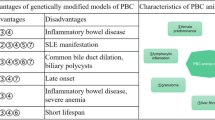
The typical course of PBC has changed a lot with the introduction of ursodeoxycholic acid (UDCA), which can significantly improve non-graft survival in PBC patients [58]. However, approximately 40% of patients do not respond to it [50, 51]. Obeticholic acid, a farnesoid X-receptor agonist, is another approved drug that can significantly reduce ALP activity and total bilirubin level, which are associated with the risk of liver transplantation or death [59, 60]. On the other hand, it is relatively disappointing treating PBC with conventional immunosuppressive drugs, indicating that the exact immunopathogenesis of PBC remains unclear. PBC is a chronic disease that can be symptom-free for many years, and the access to patients’ liver samples is difficult, especially the early stage of disease. So the use of animal models is very valuable for elucidating the pathogenesis of PBC and further drug target development [61,62,63]. A variety of PBC animal models have been reported, which can be divided into two major categories: spontaneous models and xenobiotic immunized/infection-triggered models [61, 62, 64]. Although these animal models show immune characteristics very similar to human PBC, all of them have substantial limitations [65,66,67]. However, the knowledge gained from these models has greatly contributed to our understanding of the immune pathways and the etiology of PBC (Fig. 2 and Table 2).
Animal models of PBC and disease characteristics. Current animal models that spontaneously develop cholangitis that resemble human PBC mainly include NOD.c3c4, dnTGF-βRII, IL-2Rα−/−, ARE-Del−/−, Scurfy, and Ae2a,b−/− mice. Other models include xenobiotic/infectious-induced models including 2-OA, and BDP immunized and N. aromaticivorans and E. coli-infected mice. Each model has its unique pathogenesis and phenotype. The main pathogenesis of PBC is focused on bile duct; abnormal or excessive activation of T cells including CD4+T cells and CD8+T cells directly or indirectly attacks bile duct epithelial cells (BECs), causing autoimmune cholangitis. Specific AMAs against PDC-E2 and increased inflammatory cytokines can be detected in serum
Spontaneous Models
NOD.c3c4 and NOD.c3c4-Derived Mouse Lines
NOD mice is a model of spontaneous autoimmune type 1 diabetes, in which there are at least 20 insulin-dependent diabetes (Idd) locus modifications [68]. NOD.c3c4 mice are generated by introgressing chromosome 3 and 4 B6/B10-derived genomic regions on NOD background, which are completely free of autoimmune diabetes but developed PBC-like autoimmune symptoms. These mice have liver infiltration of CD4+T and CD8+T cells and eosinophils, formation of hepatic granuloma, and production of anti-mitochondrial antibody against PDC-E2 [69, 70]. Although T cells are critical in disease development, Igμ−/− NOD.c3c4 mice that deficient in B cells exhibited a reduced number of non-B cells in the liver and alleviated liver inflammation, indicating that B cells participate in aggravating biliary tract disease in this model [71].
However, this model has limitations. There are damage of extrahepatic bile ducts and more extensive biliary hyperplasia and biliary cyst than humans. In addition, anti-Smith autoantibodies specific to systemic lupus erythematosus (SLE) patients present in more than 50% mice [62, 70]. There is another strain, the NOD.ABD strain, which is generated by crossing NOD.c3c4 mice with NOD.B6 Idd10/18 (NOD 1101). These mice harbor congenic segments of B6 chromosome 3 and B10 chromosome 4 including recombinant mouse–type I IFN regions [69]. Histologically, NOD.ABD mice and NOD.c3c4 mice are indistinguishable. However, NOD.ABD mice produce AMAs as typical of human PBC, but no anti-nuclear or anti-Smith autoantibodies [69].
Dominant-Negative TGF-β Receptor II Mice
Transforming growth factor beta (TGF-β) is one of the key regulators of immune homeostasis [72]. Transgene expression of a dominant negative form of human TGF-β receptor type II under the mouse CD4 promoter (dnTGF-βRII) leads to the abrogation of TGF-β signaling pathway in CD4+T as well as CD8+T cells and the development of autoimmune diseases [73]. It is further found that dnTGF-βRII mice have the closest serological characteristics to human PBC [74], including serum cytokine profiles; high titers of AMAs against mitochondrial autoantigens PDC-E2, BCOADC-E2, and OGDC-E2 [53]; and antinuclear antibodies against gp210 and sp100 [75]. Histologically, dnTGF-βRII mice develop portal inflammation and liver lymphocytic infiltration, but no eosinophil infiltration and granuloma. The presence of these immunopathological features indicates that TGF-β signaling pathway in T cells is closely related to the pathogenesis of PBC [76].
dnTGF-βRII mice have extensive liver infiltration of CD4+T and CD8+T lymphocytes. However, adoptive transfer of CD8+T but not CD4+T cells into Rag1−/− recipient mice leads to PBC-like changes in the liver [77], indicating a prominent role of CD8+T cells in the pathogenesis of PBC. This is consistent with PBC patients, in which PDC-E2-specific CD8+T cells may play an important role in bile duct destruction and disease progression [78, 79]. Further experiments prove that clonal expansion of autoreactive CD8+T cells and defective TGF-β signaling in these T cells are both required for the induction of autoimmune cholangitis [74, 77]. On the other hand, in the presence of pathogenic CD8+T cells, a “corrected” subset of CD4+T cells, which contain normal Treg cells, is effective in the treatment of autoimmune cholangitis [80]. Treg cells in dnTGF-βRII mice show a downregulated expression of key transcription factors and an activated Th1-like phenotype, leading to their abnormal function [81]. This highlights the role of Treg cells in PBC and their functional dysregulation in dnTGF-βRII mice.
Another T cell subset that account for a large proportion of mouse liver immune cells is natural killer T (NKT) cells [3], and their TGF-β signaling is also blocked in dnTGF-βRII mice. In PBC patients, CD1d expression and CD1d-restricted NKT cells are reported to increase in the liver, and bacterial infection may induce NKT cell activation and liver pathology [82, 83]. CD1d−/− TG mice which lack invariant NKT cells exhibited significantly reduced hepatic lymphocytic infiltration and milder bile duct inflammation [84]. Interestingly, in young but not older dnTGF-βRII mice, α-galactosylceramide-induced IFN-γ production in hepatic CD1d-restricted NKT cells was significantly increased, indicating that CD1d-restricted NKT cells participate in PBC development in an age-dependent effect.
Liver contains high proportion of innate immune cells, including NK cells that account for 10–20% of hepatic lymphocytes [85]. They participate in many liver diseases, including hepatitis B [86] and autoimmune hepatitis [87], and their function is controversial. In dnTGF-βRII mice, DX5−CD11chi liver-resident NK cells upregulate negative regulation-related functional genes in the inflammatory microenvironment, colocalize with CD4+T cells, and inhibit their proliferation to limit the development of PBC-like disease [88].
In addition to T cells, B cells also contribute to PBC development. Igμ−/− dnTGF-βRII mice develope more severe bile duct injury than control mice, and the proportion of activated CD4+T and CD8+T cells in the liver increased significantly, with elevated pro-inflammatory cytokines and decreased Treg cells [89]. Similarly, depletion of B cells with anti-CD20/CD79 antibodies eliminated the production of PDC-E2-specific antibodies, but exacerbated cholangitis [90]. When B cells are depleted at early age of dnTGF-βRII mice, liver inflammation is alleviated, with decreased intrahepatic CD8+T cells. However, treating mice with anti-CD20 antibody at 20–22 weeks of age fails to improve liver disease [91]. These results are different from NOD.c3c4 mice, indicating that the role of B cells in PBC mouse model remains controversial and still needs to be further explored.
dnTGF-βRII mice have similar serum cytokine profile with PBC patients, including increased IL-12p40, IFN-γ, TNF-α, and IL-6. The contributions of these cytokines on autoimmune cholangitis are investigated in dnTGF-βRII mice. The disease phenotype in IFN-γ−/− dnTGF-βRII mice including liver immunopathology is similar to dnTGF-βRII mice [92], suggesting that IFN-γ contributes little to PBC disease in dnTGF-βRII mice. However, knockout of CXCR3, a Th1-associated chemokine receptor, in dnTGF-βRII mice exacerbates autoimmune cholangitis through promoting pathogenic CD8+T cell activation [93]. On the other hand, IL-12p40−/− dnTGF-βRII mice have significantly reduced autoimmune biliary inflammation and hepatic proinflammatory cytokines, with no difference in serum AMAs compared with control mice. This suggests the importance of IL-12p40 signaling in autoimmune cholangitis [92]. IL-12p40 is a shared subunit of IL-12 and IL-23 [94]; however, IL-23p19−/− dnTGF-βRII mice show unchanged biliary tract lesions [95]. Besides, as a major effector cytokine produced by IL-23-dependent Th17 cells, deletion of IL-17A in dnTGF-βRII mice does not affect the severity of cholangitis. In addition, IL-6 is thought to promote inflammation, and activation of the hepatocyte IL-6/STAT3 pathway is associated with pathological regulation in acute liver failure, liver regeneration, and concanavalin A–induced liver inflammation [96]. IL-6−/− dnTGF-βRII mice exhibit significantly aggravated autoimmune cholangitis, including elevated hepatic inflammatory cytokines TNF-α and IFN-γ, increased number of activated T cells, and worsening of liver pathology [97]. These results indicate that IL-6 has a protective role of autoimmune cholangitis in dnTGF-βRII mice. However, the mechanism needs further investigation.
A recent report demonstrated that administration of antibiotics significant reduced biliary pathology in dnTGF-βRII mice. However, TLR2-deficient dnTGF-βRII mice exhibited exacerbation of autoimmune cholangitis partly due to increased gut permeability and microbiota translocation to the liver. This effect can be reduced by antibiotics, suggesting a role of gut microbiota translocation in biliary pathogenesis of dnTGF-βRII mice [98].
Although dnTGF-βRII mice emphasize the importance of TGF-β in PBC-like diseases, it is worth noting that TGF-β signaling is not completely abolished in these T cells, which explains why dnTGF-βRII mice have a normal life span as wild-type mice [61].
IL-2Rα−/− and IL-2Rα−/−-Derived Murine Models
PBC predominantly affects middle-aged woman and has never been described in childhood, until a male child at age 5 with IL-2 receptor α subunit (IL-2Rα) deficiency was reported to have hepatic dysfunction accompanied by PBC-like serological markers [99]. This patient develops an intense mononuclear cell infiltration in the intrahepatic portal area and a decrease in CD3+CD4+T lymphocytes in the blood and anti-PDC-E2 antibody in the serum. IL-2Rα is a marker of Treg cells, and IL-2 signaling is key to the development, expansion, and maintenance of Treg cells [100]; thus, this case demonstrates that the dysfunction of CD4+CD25+Treg cells leads to susceptibility to PBC. Actually, Treg cells from PBC patients showed phenotypic and functional alterations [57, 100, 101], and scurfy mice that genetically deficient in Foxp3 develop phenotypes of human PBC [102].
Based on this observation, IL-2Rα−/− mice are investigated for the appropriateness to be a mouse model of PBC [103]. In addition to portal inflammation and bile duct injury, serum indicators reflect the bias of Th1-type cytokines and increased serum IgG, IgA, PDC-E2-specific AMAs, all of which are similar to human PBC. With Treg dysfunction in IL-2Rα−/− mice, CD8+T cells mediate bile duct injury, whereas CD4+T cells mediate colon-specific autoimmune responses [104]. On the other hand, IL-2 not only plays a key role in the induction of effector T cells and Treg cells but also inhibits IL-17 producing T cells [105]. In this murine model, IL-17A plays a protective role in autoimmune cholangitis and promotes inflammatory bowel disease [106, 107]. These results are of particular importance for the potential use of anti-IL-17A therapy in patients with PBC.
Genome-wide association study (GWAS) data indicate a key role for IL-12 and its subunits in the development of PBC [108]. IL-12p40 is reported to promote autoimmune cholangitis in dnTGF-βRII mice [92]. However, p40−/-IL-2Rα−/− mice exhibited more severe portal inflammation and bile duct damage, including signs of portal hypertension and liver fibrosis with improved colitis [106]. The mechanism of different effects of IL-12p40 in dnTGF-βRII and IL-2Rα−/− mice needs further investigation. IL-2Rα−/− mice also exhibited enhanced Th1 cytokine production. Consistent with dnTGF-βRII mice, deletion of CXCR3 in IL-2Rα−/− mice leads to increased inflammation of the liver with increased hepatic CD4+T and CD8+T cells, especially the effector memory CD8+T cells [109]. However, colitis is improved. Thus, CXCR3 regulates the function of T cells in PBC, but the regulation maybe organ specific.
IFN-γ ARE-Del−/− Mice
Although Th1 mediated inflammatory response appears to be critical in the loss of tolerance, the role of IFN-γ in autoimmunity is controversial [110]. IFN-γ level is increased in PBC patients; however, in dnTGF-βRII and IL-2Rα−/− mice, IFN-γ seems to play little role in PBC development [92, 106]. The protein level of IFN-γ is regulated by the adenylate uridine–rich element in the 3′ untranslated region of IFN-γ mRNA, which is conserved in mice and human and can mediate its degradation [111]. Deletion of this element (IFN-γ ARE-Del−/−) in mice results in chronic IFN-γ expression and autoimmunity [112]. Interestingly, IFN-γ ARE-Del−/− mice develop liver lesions and portal lymphocytic infiltration similar to human PBC [113]. Serum levels of bile acid, aspartate aminotransferase, and ALT increased significantly, as well as autoantibodies against PDC-E2, BCOADC-E2, and OGDC-E2. Importantly, there is a significant female predominance in PBC-like symptoms in ARE-Del−/− mice [113]. Therefore, ARE-Del−/− mice can be studied as a new PBC mouse model with their significant female bias and close pathological features to human PBC.
ARE-Del−/− mice have enhanced not only type II IFN signaling but also intense and sustained type I IFN signaling. ARE-Del−/-IFN-αR1−/− mice show a significant remission of liver pathology and a loss of gender bias compared with ARE-Del−/− mice. In addition, knockout of IFN-α receptor in female ARE-Del−/− mice corrected germinal center abnormalities including abnormal follicular structures [114]. These results suggest that type I IFN signaling may be the initiator of the disease and plays a crucial role in the gender bias of autoimmune cholangitis, highlighting that targeting type I IFN signaling pathway has therapeutic potential at the early stages of PBC.
Ae2a,b−/− Mice
PBC is a cholestasis disease, in which bile duct destruction results in bile acid accumulation in the liver. Cl−/HCO3− anion exchanger 2 (AE2) is a critical mediator of biliary bicarbonate secretion by cholangiocytes, which is important for maintaining an alkaline pH around hepatocytes and cholangiocytes [115]. Further, it is found that the bicarbonate biliary “umbrella” protects cholangiocytes from protonated glycine-conjugated bile salt–induced apoptosis, especially when the level of bile salts increases in cholestasis conditions [116, 117]. In PBC patients, decreased expression of AE2 gene is found in liver biopsy specimens and blood mononuclear cells, and the expression of AE2 is associated with prognosis of PBC patients under UDCA treatment [118,119,120]. Thus, AE2 knockout mice (Ae2a,b−/− mice) were generated to mimic the human PBC [118]. About one third of Ae2a,b−/− mice show infiltration of CD4+T and CD8+T cells in the portal area and around the damaged bile ducts, and mild fibrosis around the bile duct obstruction area. Most Ae2a,b−/− mice are AMA positive, with elevated serum IgM and IgG and ALP levels. These results suggest that defective expression of AE2 in the liver alters pH homeostasis in immune cells and gene expression profile in BECs, and may be involved in the pathogenesis of PBC [118]. However, the disadvantage of Ae2a,b−/− mouse model is that there are differences in histological characteristics with human PBC. Many mice showed no changes of liver histology, and they have difficulty reproducing.
Models Induced by Xenobiotic and Infectious Agents
The development of PBC is influenced not only by genetic background but also by environmental factors such as xenobiotic and infectious agents [121, 122]. The loss of tolerance to PDC-E2 through molecular mimicry with environmental chemicals and infectious agents is considered to be the immanent cause of PBC [123,124,125]. A large number of immunoassays for PDC-E2 structural analogs demonstrate this hypothesis and illustrate the importance of structural integrity of PDC-E2 lipoyl domain in AMA recognition [126, 127]. Exposure to an infectious agent that have structural similarity with PDC-E2 can lead to the loss of tolerance to PDC-E2, resulting in the occurrence of PBC. The following models use this method to establish PBC animal models, which can simulate the pre-existing conditions of PBC with strong practicability.
2-Octynoic Acid-BSA–Immunized Mice
2-Octynoic acid (2-OA) is a non-naturally occurring, artificially synthesized xenobiotic compound widely used in food flavorings and cosmetics with the potential to modify PDC-E2 in vivo [126]. The time required for AMA-positive reaction and biliary lesions induced by 2-OA is just a few weeks [128]. Serum IgG, lgM, lgA, TNF-α, and IFN-γ are significantly increased, with mild lymphocyte infiltrations around the damaged bile ducts, and reduced hepatic CD4/CD8 ratio. Furthermore, ductopenia is observed, and epithelioid granulomas are scattered within some portal tracts and hepatic parenchyma, which resemble pathological features of human PBC.
In 2OA-BSA-immunized murine model, Th1 cells and IFN-γ are major contributors to the initial stage and apparently may have different effects as the disease progresses [129]. Besides, several gene knockout mice were used to study the IL-12/Th1 and IL-23/Th17 pathway in this model [130]. Deletion of the Th17 cytokines IL-17A and IL-22 but not IL-17F reduced biliary tract damage; deletion of IL-17A reduced AMA levels. Th17 cytokine-deficient mice had significantly reduced IFN-γ in the liver, whereas the ability of T cells to produce IFN-γ was not affected, suggesting that the lack of the Th17 pathway inhibits the accumulation of IFN-γ producing cells in the early liver of cholangitis. Cholangitis disappears only in IL-20p40−/− but not IL-23p19−/− and IL-12p35−/− mice, with decreased portal infiltration of mononuclear cells including CD4+ and CD8+T cells. In summary, IL-12/Th1 and IL-23/Th17 are involved in the development of cholangitis, among them IL-12/Th1 signaling pathway plays an important role in liver pathological induction, while IL-23/Th17 pathway is enhanced the immunopathology mediated by IL-12/IFN-γ.
Besides adaptive immunity, anti-NK1.1 antibody is used in 2OA-BSA before immunization to study the role of NK cells and NKT cells, which compose a large part of innate immune cells in the liver [131]. The levels of AMA and cytokines in serum significantly decreased after treatment, but the degree of portal inflammation does not change, indicating that NK and NKT cells play an important role in triggering the loss of tolerance [132]. Further, α-GalCer treatment leads to aggravated autoimmune cholangitis even fibrosis. Meanwhile, CD1d−/− mice show reduced portal infiltration and AMA responses after immunization [133], suggesting that iNKT cells can be activated by overlapping and/or promiscuous pathways. What is more, CD4 and CD8 knockout mice immunized with 2OA-BSA have symptoms like PBC and are augmented by α-GalCer [134]. In summary, all of the models illustrate the important role of innate immunity, like iNKT cells, in PBC, especially in the early stages.
Bile Duct Protein–Immunized Mice
While the above immunized mouse model focuses on the molecular simulation of the E2 subunit of PDC-E2, another study has explored the breaking of tolerance with self-tissue. In this model, mice immunized with syngeneic bile duct protein (BDP) develop a variety of key features similar to human PBC, including liver-specific inflammation, increased number of activated CD4+T and CD8+T cells as well as 100% AMAs [135].
Bacteria-Infected Mice
Novosphingobium aromaticivorans is a gram-negative bacteria which present in human mucus surfaces and feces [136]. It expresses proteins that share high molecular homology with human PDC-E2 epitope [137]. Strikingly, PBC patients express antibodies against N. aromaticivorans, and the reactivity is much higher than E. coli [136, 137]. N. aromaticivorans belongs to the family of Sphingomonas whose glycosphingolipids on the cell wall can be specifically presented to NKT cells by CD1d, causing mutual activation of NKT cells and dendritic cells and the release of a large amount of cytokines and chemokines [83]. Various mouse strains infected by N. aromaticivorans including C57BL/6, NOD, and SJL exhibited increased AMAs, as well as bile duct damage and granuloma similar to human PBC [138]. In this model, chronic liver inflammation is dependent on CD1d and NKT cells, illustrating the importance of early microbial activation of NKT cells in the initiation of autonomous, organ-specific autoimmunity.
Besides, several epidemiological studies have demonstrated that patients with PBC have a higher incidence of urinary tract infections, and the most common isolates from the patient’s urine are E. coli [139]. TCRβ repertoire analysis of memory T cells from PBC patients also reveals a potential role of E. coli in the pathogenesis of PBC [140]. In NOD1101 mice, with E. coli infection induced more serious biliary disease similar with human PBC than N. aromaticivorans, and interestingly, the titer of AMA was higher [141]. PDC-E2 is highly conserved between mammals and bacteria, and six E. coli peptide sequences mimic the human PDC-E2 autoepitope with six to eight identical amino acid residues [142], suggesting that E. coli immunogenic mimics may account for the dominance of the major PDC-E2 autoepitope. In summary, these models may be useful to study the relationship between environmental bacteria and the development of PBC.
PSC
PSC is a rare, chronic cholestatic liver dysfunction characterized by an impairment of the bile flow and intrahepatic or/and extrahepatic bile duct stricture with biliary fibrosis [143, 144]. The cause and pathogenesis are extremely complicated, and the specific pathophysiology remains unclear. The incidence of PSC is high among young individuals, with predominance in young men. The development of PSC undergoes four stages (Fig. 3): (i) portal edema; (ii) mild portal inflammation, lymphocytic infiltration, and bile duct hyperplasia; (iii), portal vein fibrosis, degeneration, and disappearance of bile ducts; and (iv) cirrhosis, even neoplasms. The clinical development of PSC is unpredictable, and the most terrible complications are cholangiocarcinoma and colorectal cancer, which can occur at any stage of the disease. PSC is strongly associated with inflammatory bowel disease (IBD); 70% of patients with PSC develop IBD, whereas 5–10% of patients with colitis develop PSC [143, 144]. PSC patients have fecal dysbiosis and is distinct from IBD signatures, suggesting that intestinal microbiota may be an important factor in the pathogenesis [145]. Besides, increased ALP and a variety of autoantibodies have been detected in PSC including perinuclear antineutrophil cytoplasmic antibodies, ANAs, and SMAs [146, 147].
Animal models of PSC and pivotal characteristics. Animal models of human PSC have been reported to fall into two broad categories: spontaneous models (Mdr2−/− mice) and chemically induced cholangitis models (DDC-fed, TNBS-fed, LCA-fed). The pathology of PSC under each model is derived from different pathogenesis and mechanism (left). Different PSC animal models can mimic certain stages of human PSC (numbers labeled). The main four stages of human PSC include initial portal edema and biliary stricture and dilution, inflammation progression, fibrosis, and finally tumorigenic stage. The ideal PSC animal model can progress to “onion skin-type” periductal fibrosis of intrahepatic bile ducts, immune cell infiltration, bile duct replacement by a scar formation, and subsequent development of bile duct hyperplasia (right)
Currently, no treatment slows or reverses progression of PSC, while only liver transplantation achieves good outcome in advanced stages, reflecting the poor understanding of disease pathogenesis. Thus, animal models of PSC are needed to develop new treatment strategies. Current animal models include spontaneous models and chemically induced models (Table 3 and Fig. 3), which mimic some important characteristics for mechanistic and therapeutic studies, but all of them have substantial limitations.
Spontaneous Models
Mdr2−/− Mice
The multidrug resistance 2 (Mdr2) gene encodes phosphatidylcholine translocase that is essential for the secretion of phospholipids from hepatocytes into bile [148]. Deficiency of Mdr2 in mice leads to complete loss of phospholipids in bile and increased concentration of non-micelle components of free bile acids, which is a detergent on the cell membrane of BECs [148]. This causes the destruction of both tight junctions and the basement membrane, leading to bile leakage inside the portal tract. Inflammation around the gallbladder and ROS production by Mdr2-deficient cells lead to activation of myofibroblasts accompanied by fibrotic deposition around the inflamed ducts, and may have subsequent pro-tumorigenic functions [64, 149, 150]. Similar to human PSC, Mdr2−/− mice have increased macrophages. Thus, Mdr2−/− mice are often used as sclerosing cholangitis model [151]. 24-Norursodeoxycholic acid, a side chain–modified UDCA derivative, can significantly revert cholangitis and biliary fibrosis in Mdr2−/− mice [152].
However, Mdr2−/− mice have limitations in mirroring some pivotal characteristics of PSC. Liver fibrosis is prone to occur at the age of 4–6 months, and the tumor nodules are similar in pathology to hepatocellular carcinoma rather than cholangiocarcinoma [153], which is inconsistent with human PSC. Besides, there is no accompanying IBD phenomenon. So, dextran sulfate sodium (DSS) is used to induce IBD in Mdr2−/− mice as a new PSC-IBD model. Mdr2−/−/DSS model displays increased weight loss, shortened colon length, and increased histological damage of the colon. On the other hand, DSS-induced enteritis aggravates the progression of PSC, accompanied by the appearance of bile duct reactions and bridging fibrosis, with increased pro-inflammatory cytokines [154]. The Mdr2−/−/DSS model suggests a role for the interdependent signaling pathways of the liver-intestine crosstalk in mediating disease, and is considered a novel murine model of PSC-IBD.
The close relationship between PSC and IBD is at the heart of the pathogenesis of PSC. From animal models, we learned that intestinal bacteria and bacterial products drive chronic bile duct injury. Increased Lactobacillus gasseri in the liver of Mdr2−/− mice can stimulate the production of IL-17A by γδ TCR+ cells and promote liver inflammation and fibrosis [155]. However, germ-free Mdr2−/− mice develop aggravated PSC phenotypes compared with conventional control, including higher serum ALP, AST, and bilirubin, and more severe fibrosis, biliary tract reaction, and bile duct loss [156]. These symptoms disappear after administration by UDCA, along with elimination of biliary cell senescence [157]. These results demonstrate the importance of normal commensal bacteria and their metabolites in the prevention of bile duct injury, which provides new ideas for future research on PSC biotherapy and intervention. Actually, fecal microbiota transplantation has proven to be safe and may improve ALP level in PSC patients [158].
Chemically Induced Models
3,5-Diethoxycarbonyl-1,4-Dihydrocollidine–Fed Mice
3,5-Diethoxycarbonyl-1,4-dihydrocollidine (DDC) acts as a chemical poison to stimulate chemical bile secretion of porphyrins, and mice fed with DDC develop progressive cholestatic liver injury [159, 160]. The specific phenotypes include small bile duct blockade, brisk ductular proliferation, and intense pericholangitis associated with “onion skin-type” periductal fibrosis, which are similar to human PSC [161, 162]. Interestingly, there is no change in bile flow and cholesterol and phospholipid excretion in the bile compared with Mdr2−/− mice. In addition, DDC feeding does not alter bile acid composition [162]. The establishment of this model is helpful in studying the mechanism of xenobiotic-induced chronic cholangiopathic disease and its sequelae. Compared with human PSC, a crucial difference in DDC-fed mice is the lacking of biliary stricture and dilations of the large extrahepatic bile ducts. However, this mouse model exhibits typical periductal fibrosis, which mainly affects intrahepatic bile ducts. Therefore, this condition can serve as a “small bile duct” PSC model [153].
2,4,6-Trinitrobenzene Sulfonic Acid–Fed Rats
2,4,6-Trinitrobenzene sulfonic acid (TNBS) acts as a hapten with a strong affinity for the lysine group of the intestinal epithelial membrane protein, triggering a cell-mediated immune response [163]. In rats, a single TNBS injection through bile duct results in a significant increase in serum levels of ALP and bilirubin, with increased inflammatory cell infiltration in the portal and bile duct [164]. The TNBS-related model exhibits a variety of features consistent with PSC, including irregular intrahepatic and extrahepatic bile ducts. Portal mononuclear cell infiltration mainly include macrophages and T lymphocytes. Simultaneously, it is serologically accompanied by the production of perinuclear antineutrophil cytoplasmic antibody (pANCA) and SMA. Unexpectedly, although the toxicity of TNBS to intestinal epithelial cells is recognized, it is bile duct specific in this rat model and does not cause symptoms of IBD. Furthermore, the main limitation of this model is the high mortality rate, mainly due to complications of surgery/chemical combination.
Lithocholic Acid–Fed Mice
Bile acids are thought to be less toxic to mice than humans because they tend to replace the bile acid pool with more hydrophilic bile acids [165]. Therefore, in order to understand the potential hepatotoxicity of hydrophobic bile acids in cholestatic liver injury, several studies have used monohydroxy bile acid lithocholic acid (LCA) as a prototype of toxic bile acids [166, 167]. As expected, LCA feeding results in biliary infarction followed by destructive cholangitis with activation and proliferation of perivascular fibroblasts. Cholestatic effects are evident after LCA feeding, which involves changes in the biochemical properties of the bile canalicular membrane, and the formation of crystalline plugs in bile ducts due to little solubility [166]. Importantly, the potential toxic bile acids may affect the integrity of the cell membranes of liver cells and biliary cells, which is very similar to Mdr2−/− mice [64]. Histologically, LCA fed mice developed portal bile duct injury, cholestasis, destructive cholangitis, and perivascular fibrosis [168]. However, because animals cannot take this drug for a long time, it is not a suitable model for studying the development of chronic bile duct injury.
IgG4-SC
IgG4-SC is the biliary manifestation of IgG4-related disease (IgG4-RD), which is a multi-system autoimmune disorder characterized by increased IgG4 in the plasma with unknown etiology [169, 170]. Although IgG4 exist only in human, mouse IgG1 resembles the function of human IgG4. Recently, a LatY136F knock-in mouse model was reported to mimic human IgG4-RD, which has increased Th2 effector cells, polyclonal B cell activation with IgG1 and IgE production and non-resolving inflammation and autoimmunity [171]. Although liver involvement was observed in LatY136F knock-in mice, whether they develop sclerosing cholangitis remains unknown. New animal models that mimic IgG4-RD and IgG4-SC are needed to study the pathogenic mechanisms and for drug screening.
Concluding Remarks
It is clear that AILDs develop with a disease-prone genetic background, epigenetic regulation, environment, and immunological factors, but the exact pathogenesis needs further illustration [172,173,174]. Although various animal models of AILDs have been reported, it is very challenging to summarize the complex immunological damages and local tissue interactions in a single model; thus, researchers are still puzzled on the underlying mechanisms and the etiologies at the induction of the disease process. Besides, AILDs have overlapped features and patients develop overlapped syndrome such as PBC-AIH and PSC-AIH [172].
Even so, many studies utilizing murine models have provided pathogenetic insights, diagnostic improvements, and therapeutic advances for AILDs. For example, molecular mimicary by environmental factors has been demonstrated in murine models of AIH and PBC. GWAS-identified risk factors such as IL-12A have been proved to contribute to disease development in murine models of PBC. In AIH and PBC, T cells are reported to be critical effector cells, suggesting that suppressing T cell activation and induction of T cell exhaustion may be possible managing strategies [8, 9]. In AIH, the role of TNF, B cells, and Treg cells in disease development have led to launch of clinical trails using anti-TNF, anti-CD20, anti-BAFF, and adoptive Treg transfer for disease treatment [9]. Many experimental therapies and clinical trials against PBC have also been launched based on the disease mechanisms revealed in animal models, such as B cell depletion, interleukin modulation, microbiome transfer, and anti-viral therapies [15, 175, 176]. Clinical trails using fecal microbiota transplantation has been launched for the treatment of PSC.
However, there are a lot of investigations that need to be done using murine models of AILDs. For example, the roles of many of the GWAS identified genes in AILDs can be investigated using transgenic mice. Moreover, unassessed pathways that have been implicated in other diseases, the underlying mechanisms of self-sustained immune reactivity in AILDs, and possible therapeutic strategies in other immune-mediated diseases still need more investigations in murine models.
On the other hand, one concern about utilizing murine models in AILD research is that laboratory mice do not reflect relevant aspects of the human immune system, which may result in failures to translate disease treatments from bench to bedside like other diseases [177]. This is mainly contributed by differences of physiology and genetics between mice and humans; however, recent studies have shown that natural environmental conditions especially microbiota are also important [177,178,179]. Mice from wild environment but not specific pathogen-free condition phenocopied human immune system and immune reactions. Thus, in the future, mice conditioned in wild environment may help to develop models more similar to human AILDs and to find new therapeutic targets.
Abbreviations
- ABD:
-
Autoimmune biliary disease
- AE2:
-
Anion exchanger 2
- α-GalCer:
-
α-Galactosylceramide
- AIH:
-
Autoimmune hepatitis
- AILD:
-
Autoimmune liver disease
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AMAs:
-
Antimitochondrial antibodies
- ANAs:
-
Antinuclear antibodies
- AU-rich:
-
Adenylate uridine-rich
- BCOADC-E2:
-
Branched chain 2-oxo acid dehydrogenase complex-E2
- BDP:
-
Bile duct protein
- BEC:
-
Bile duct epithelial cell
- BSA:
-
Bovine serum albumin
- ConA:
-
Concanavalin A
- CTLA-4:
-
Cytotoxic T lymphocyte-associated protein 4
- CYP2D6:
-
Cytochrome P4502D6
- dnTGF-βRII:
-
Dominant-negative TGF-β receptor II
- DDC:
-
3,5-Diethoxycarbonyl-1,4-dihydrocollidine
- DSS:
-
Dextran sulfate sodium
- E. coli :
-
Escherichia coli
- FAH:
-
Fumarylacetoacetate hydrolase
- FTCD:
-
Formiminotransferase cyclodeaminase
- GWAS:
-
Genome-wide association study
- HLA:
-
Human leukocyte antigen
- IBD:
-
Inflammatory bowel disease
- Idd:
-
Insulin-dependent diabetes
- iNKT:
-
Invariant natural killer T
- IL-2Rα:
-
Interleukin-2 receptor α
- IgG4-RD:
-
Immunoglobulin G4–related disease
- LCA:
-
Lithocholic acid
- LPS:
-
Lipopolysaccharide
- LSEC:
-
Liver sinusoidal endothelial cells
- LSP:
-
Liver-specific membrane protein
- MHV:
-
Mouse hepatic virus
- NOD:
-
Non-obese diabetic
- N. aromaticivorans :
-
Novosphingobium aromaticivorans
- NTx:
-
Neonatal thymectomy
- OGDC-E2:
-
2-Oxoglutarate dehydrogenase complex-E2
- 2-OA:
-
2-Octyl acid
- pANCA:
-
Perinuclear antineutrophil cytoplasmic antibodies
- PBC:
-
Primary biliary cholangitis
- PDC-E2:
-
Pyruvate dehydrogenase complex-E2
- PSC:
-
Primary sclerosing cholangitis
- SLE:
-
Systemic lupus erythematosus
- SMAs:
-
Smooth muscle antibodies
- TNBS:
-
2,4,6-Trinitrobenzene sulfonic acid
- Tregs:
-
Regulatory T cells
- UDCA:
-
Ursodeoxycholic acid
References
Doherty DG (2016) Immunity, tolerance and autoimmunity in the liver: a comprehensive review. J Autoimmun 66:60–75
Horst AK, Neumann K, Diehl L, Tiegs G (2016) Modulation of liver tolerance by conventional and nonconventional antigen-presenting cells and regulatory immune cells. Cell Mol Immunol 13(3):277–292
Crispe IN (2009) The liver as a lymphoid organ. Annu Rev Immunol 27:147–163
Mattner J (2011) Genetic susceptibility to autoimmune liver disease. World J Hepatol 3(1):1–7
Cristoferi L, Nardi A, Ronca V, Invernizzi P, Mells G, Carbone M (2018) Prognostic models in primary biliary cholangitis. J Autoimmun 95:171–178
Terziroli Beretta-Piccoli B et al (2019) The challenges of primary biliary cholangitis: what is new and what needs to be done. J Autoimmun:102328
Liberal R, Grant CR, Mieli-Vergani G, Vergani D (2013) Autoimmune hepatitis: a comprehensive review. J Autoimmun 41:126–139
Huang C et al (2019) Immune checkpoint molecules. Possible future therapeutic implications in autoimmune diseases. J Autoimmun 104:102333
Mieli-Vergani G et al (2018) Autoimmune hepatitis. Nat Rev Dis Primers 4:18017
Manns MP, Lohse AW, Vergani D (2015) Autoimmune hepatitis—update 2015. J Hepatol 62(1 Suppl):S100–S111
Christen U (2019) Animal models of autoimmune hepatitis. Biochim Biophys Acta Mol basis Dis 1865(5):970–981
Manns MP, Czaja AJ, Gorham JD, Krawitt EL, Mieli-Vergani G, Vergani D, Vierling JM, American Association for the Study of Liver Diseases (2010) Diagnosis and management of autoimmune hepatitis. Hepatology 51(6):2193–2213
Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, Bittencourt PL, Porta G, Boberg KM, Hofer H, Bianchi FB, Shibata M, Schramm C, Eisenmann de Torres B, Galle PR, McFarlane I, Dienes HP, Lohse AW, International Autoimmune Hepatitis Group (2008) Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology 48(1):169–176
Gatselis NK, Zachou K, Koukoulis GK, Dalekos GN (2015) Autoimmune hepatitis, one disease with many faces: etiopathogenetic, clinico-laboratory and histological characteristics. World J Gastroenterol 21(1):60–83
European Association for the Study of the, L (2015) EASL Clinical Practice Guidelines: autoimmune hepatitis. J Hepatol 63(4):971–1004
Floreani A et al (2018) Etiopathogenesis of autoimmune hepatitis. J Autoimmun 95:133–143
Taubert R et al (2018) Novel therapeutic targets in autoimmune hepatitis. J Autoimmun 95:34–46
Kido M, Watanabe N, Okazaki T, Akamatsu T, Tanaka J, Saga K, Nishio A, Honjo T, Chiba T (2008) Fatal autoimmune hepatitis induced by concurrent loss of naturally arising regulatory T cells and PD-1-mediated signaling. Gastroenterology 135(4):1333–1343
Maruoka R et al (2013) Splenectomy prolongs the effects of corticosteroids in mouse models of autoimmune hepatitis. Gastroenterology 145(1):209–220.e9
Aoki N et al (2011) Dysregulated generation of follicular helper T cells in the spleen triggers fatal autoimmune hepatitis in mice. Gastroenterology 140(4):1322–1333.e1–5
Iwamoto S, Kido M, Aoki N, Nishiura H, Maruoka R, Ikeda A, Okazaki T, Chiba T, Watanabe N (2012) IFN-γ is reciprocally involved in the concurrent development of organ-specific autoimmunity in the liver and stomach. Autoimmunity 45(2):186–198
Iwamoto S, Kido M, Aoki N, Nishiura H, Maruoka R, Ikeda A, Okazaki T, Chiba T, Watanabe N (2013) TNF-α is essential in the induction of fatal autoimmune hepatitis in mice through upregulation of hepatic CCL20 expression. Clin Immunol 146(1):15–25
Tiegs G, Hentschel J, Wendel A (1992) A T cell-dependent experimental liver injury in mice inducible by concanavalin A. J Clin Invest 90(1):196–203
Gantner F, Leist M, Lohse AW, Germann PG, Tiegs G (1995) Concanavalin A-induced T-cell-mediated hepatic injury in mice: the role of tumor necrosis factor. Hepatology 21(1):190–198
Heymann F, Hamesch K, Weiskirchen R, Tacke F (2015) The concanavalin A model of acute hepatitis in mice. Lab Anim 49(1 Suppl):12–20
Takeda K, Hayakawa Y, van Kaer L, Matsuda H, Yagita H, Okumura K (2000) Critical contribution of liver natural killer T cells to a murine model of hepatitis. Proc Natl Acad Sci U S A 97(10):5498–5503
Küsters S, Gantner F, Künstle G, Tiegs G (1996) Interferon gamma plays a critical role in T cell-dependent liver injury in mice initiated by concanavalin A. Gastroenterology 111(2):462–471
Rossjohn J, Pellicci DG, Patel O, Gapin L, Godfrey DI (2012) Recognition of CD1d-restricted antigens by natural killer T cells. Nat Rev Immunol 12(12):845–857
Osman Y, Kawamura T, Naito T, Takeda K, van Kaer L, Okumura K, Abo T (2000) Activation of hepatic NKT cells and subsequent liver injury following administration of alpha-galactosylceramide. Eur J Immunol 30(7):1919–1928
Matsumoto H, Kawamura T, Kobayashi T, Kanda Y, Kawamura H, Abo T (2011) Coincidence of autoantibody production with the activation of natural killer T cells in alpha-galactosylceramide-mediated hepatic injury. Immunology 133(1):21–28
Biburger M, Tiegs G (2005) Alpha-galactosylceramide-induced liver injury in mice is mediated by TNF-alpha but independent of Kupffer cells. J Immunol 175(3):1540–1550
Wang H, Feng D, Park O, Yin S, Gao B (2013) Invariant NKT cell activation induces neutrophil accumulation and hepatitis: opposite regulation by IL-4 and IFN-gamma. Hepatology 58(4):1474–1485
Wondimu Z, Santodomingo-Garzon T, le T, Swain MG (2010) Protective role of interleukin-17 in murine NKT cell-driven acute experimental hepatitis. Am J Pathol 177(5):2334–2346
Kuriki J, Murakami H, Kakumu S, Sakamoto N, Yokochi T, Nakashima I, Kato N (1983) Experimental autoimmune hepatitis in mice after immunization with syngeneic liver proteins together with the polysaccharide of Klebsiella pneumoniae. Gastroenterology 84(3):596–603
Lohse AW, Dienes HP, Meyer zum Buschenfelde KH (1998) Suppression of murine experimental autoimmune hepatitis by T-cell vaccination or immunosuppression. Hepatology 27(6):1536–1543
Ma X, Jia YT, Qiu DK (2007) Inhibition of p38 mitogen-activated protein kinase attenuates experimental autoimmune hepatitis: involvement of nuclear factor kappa B. World J Gastroenterol 13(31):4249–4254
Liu X, Jiang X, Liu R, Wang L, Qian T, Zheng Y, Deng Y, Huang E, Xu F, Wang JY, Chu Y (2015) B cells expressing CD11b effectively inhibit CD4+ T-cell responses and ameliorate experimental autoimmune hepatitis in mice. Hepatology 62(5):1563–1575
Ma Y et al (2006) Polyclonal T-cell responses to cytochrome P450IID6 are associated with disease activity in autoimmune hepatitis type 2. Gastroenterology 130(3):868–882
Christen U, Holdener M, Hintermann E (2010) Cytochrome P450 2D6 as a model antigen. Dig Dis 28(1):80–85
Hintermann E, Ehser J, Bayer M, Pfeilschifter JM, Christen U (2013) Mechanism of autoimmune hepatic fibrogenesis induced by an adenovirus encoding the human liver autoantigen cytochrome P450 2D6. J Autoimmun 44:49–60
Holdener M, Hintermann E, Bayer M, Rhode A, Rodrigo E, Hintereder G, Johnson EF, Gonzalez FJ, Pfeilschifter J, Manns MP, Herrath Mv, Christen U (2008) Breaking tolerance to the natural human liver autoantigen cytochrome P450 2D6 by virus infection. J Exp Med 205(6):1409–1422
Ehser J, Holdener M, Christen S, Bayer M, Pfeilschifter JM, Hintermann E, Bogdanos D, Christen U (2013) Molecular mimicry rather than identity breaks T-cell tolerance in the CYP2D6 mouse model for human autoimmune hepatitis. J Autoimmun 42:39–49
Hardtke-Wolenski M, Fischer K, Noyan F, Schlue J, Falk CS, Stahlhut M, Woller N, Kuehnel F, Taubert R, Manns MP, Jaeckel E (2013) Genetic predisposition and environmental danger signals initiate chronic autoimmune hepatitis driven by CD4+ T cells. Hepatology 58(2):718–728
Dywicki J, Buitrago-Molina LE, Pietrek J, Lieber M, Broering R, Khera T, Schlue J, Manns MP, Wedemeyer H, Jaeckel E, Hardtke-Wolenski M (2020) Autoimmune hepatitis induction can occur in the liver. Liver Int 40(2):377–381
Lapierre P et al (2004) A murine model of type 2 autoimmune hepatitis: xenoimmunization with human antigens. Hepatology 39(4):1066–1074
Duhalde-Vega M, Loureiro ME, Mathieu PA, Retegui LA (2006) The peptide specificities of the autoantibodies elicited by mouse hepatitis virus A59. J Autoimmun 27(3):203–209
Aparicio JL, Peña C, Retegui LA (2011) Autoimmune hepatitis-like disease in C57BL/6 mice infected with mouse hepatitis virus A59. Int Immunopharmacol 11(10):1591–1598
Tang Y, Li H, Li J, Liu Y, Li Y, Zhou J, Zhou J, Lu X, Zhao W, Hou J, Wang XY, Chen Z, Zuo D (2018) Macrophage scavenger receptor 1 contributes to pathogenesis of fulminant hepatitis via neutrophil-mediated complement activation. J Hepatol 68(4):733–743
Hirschfield GM, Gershwin ME (2013) The immunobiology and pathophysiology of primary biliary cirrhosis. Annu Rev Pathol 8:303–330
Carey EJ, Ali AH, Lindor KD (2015) Primary biliary cirrhosis. Lancet 386(10003):1565–1575
Selmi C, Bowlus CL, Gershwin ME, Coppel RL (2011) Primary biliary cirrhosis. Lancet 377(9777):1600–1609
Sun Y, Haapanen K, Li B, Zhang W, van de Water J, Gershwin ME (2015) Women and primary biliary cirrhosis. Clin Rev Allergy Immunol 48(2–3):285–300
Oertelt S et al (2006) Anti-mitochondrial antibodies and primary biliary cirrhosis in TGF-beta receptor II dominant-negative mice. J Immunol 177(3):1655–1660
Moritoki Y et al (2007) AMA production in primary biliary cirrhosis is promoted by the TLR9 ligand CpG and suppressed by potassium channel blockers. Hepatology 45(2):314–322
Bernuzzi F, Fenoglio D, Battaglia F, Fravega M, Gershwin ME, Indiveri F, Ansari AA, Podda M, Invernizzi P, Filaci G (2010) Phenotypical and functional alterations of CD8 regulatory T cells in primary biliary cirrhosis. J Autoimmun 35(3):176–180
Mao TK, Lian ZX, Selmi C, Ichiki Y, Ashwood P, Ansari AA, Coppel RL, Shimoda S, Ishibashi H, Gershwin ME (2005) Altered monocyte responses to defined TLR ligands in patients with primary biliary cirrhosis. Hepatology 42(4):802–808
Lan RY et al (2006) Liver-targeted and peripheral blood alterations of regulatory T cells in primary biliary cirrhosis. Hepatology 43(4):729–737
Bosch A, Dumortier J, Maucort-Boulch D, Scoazec JY, Wendum D, Conti F, Morard I, Rubbia-Brandt L, Terris B, Radenne S, Abenavoli L, Poupon R, Chazouillères O, Calmus Y, Boillot O, Giostra E, Corpechot C (2015) Preventive administration of UDCA after liver transplantation for primary biliary cirrhosis is associated with a lower risk of disease recurrence. J Hepatol 63(6):1449–1458
Hirschfield GM, Mason A, Luketic V, Lindor K, Gordon SC, Mayo M, Kowdley KV, Vincent C, Bodhenheimer HC Jr, Parés A, Trauner M, Marschall HU, Adorini L, Sciacca C, Beecher-Jones T, Castelloe E, Böhm O, Shapiro D (2015) Efficacy of obeticholic acid in patients with primary biliary cirrhosis and inadequate response to ursodeoxycholic acid. Gastroenterology 148(4):751–761 e8
Nevens F, Andreone P, Mazzella G, Strasser SI, Bowlus C, Invernizzi P, Drenth JP, Pockros PJ, Regula J, Beuers U, Trauner M, Jones DE, Floreani A, Hohenester S, Luketic V, Shiffman M, van Erpecum K, Vargas V, Vincent C, Hirschfield GM, Shah H, Hansen B, Lindor KD, Marschall HU, Kowdley KV, Hooshmand-Rad R, Marmon T, Sheeron S, Pencek R, MacConell L, Pruzanski M, Shapiro D, POISE Study Group (2016) A placebo-controlled trial of obeticholic acid in primary biliary cholangitis. N Engl J Med 375(7):631–643
Katsumi T, Tomita K, Leung PS, Yang GX, Gershwin ME, Ueno Y (2015) Animal models of primary biliary cirrhosis. Clin Rev Allergy Immunol 48(2–3):142–153
Wang J et al (2014) Animal models of primary biliary cirrhosis. Semin Liver Dis 34(3):285–296
Webb GJ, Hirschfield GM (2017) Primary biliary cholangitis in 2016: high-definition PBC: biology, models and therapeutic advances. Nat Rev Gastroenterol Hepatol 14(2):76–78
Mariotti V, Cadamuro M, Spirli C, Fiorotto R, Strazzabosco M, Fabris L (2019) Animal models of cholestasis: an update on inflammatory cholangiopathies. Biochim Biophys Acta Mol basis Dis 1865(5):954–964
Tanakaa A, Leung PS, Young HA, Gershwin ME (2017) Toward solving the etiological mystery of primary biliary cholangitis. Hepatol Commun 1(4):275–287
Pollheimer MJ, Fickert P (2015) Animal models in primary biliary cirrhosis and primary sclerosing cholangitis. Clin Rev Allergy Immunol 48(2–3):207–217
Ueno Y et al (2010) Murine models of autoimmune cholangitis. Curr Opin Gastroenterol 26(3):274–279
Aoki CA, Borchers AT, Ridgway WM, Keen CL, Ansari AA, Gershwin ME (2005) NOD mice and autoimmunity. Autoimmun Rev 4(6):373–379
Yang GX et al (2011) CD8 T cells mediate direct biliary ductule damage in nonobese diabetic autoimmune biliary disease. J Immunol 186(2):1259–1267
Irie J, Wu Y, Wicker LS, Rainbow D, Nalesnik MA, Hirsch R, Peterson LB, Leung PS, Cheng C, Mackay IR, Gershwin ME, Ridgway WM (2006) NOD.c3c4 congenic mice develop autoimmune biliary disease that serologically and pathogenetically models human primary biliary cirrhosis. J Exp Med 203(5):1209–1219
Moritoki Y, Tsuda M, Tsuneyama K, Zhang W, Yoshida K, Lian ZX, Yang GX, Ridgway WM, Wicker LS, Ansari AA, Gershwin ME (2011) B cells promote hepatic inflammation, biliary cyst formation, and salivary gland inflammation in the NOD.c3c4 model of autoimmune cholangitis. Cell Immunol 268(1):16–23
Lucas PJ et al (2006) Dysregulation of IL-15-mediated T-cell homeostasis in TGF-beta dominant-negative receptor transgenic mice. Blood 108(8):2789–2795
Sawada S, Scarborough JD, Killeen N, Littman DR (1994) A lineage-specific transcriptional silencer regulates CD4 gene expression during T lymphocyte development. Cell 77(6):917–929
Kawata K et al (2013) Clonality, activated antigen-specific CD8(+) T cells, and development of autoimmune cholangitis in dnTGFbetaRII mice. Hepatology 58(3):1094–1104
Yang CY, Leung PS, Yang GX, Kenny TP, Zhang W, Coppel R, Norman GL, Ansari AA, Mackay IR, Worman HJ, Gershwin ME (2012) Epitope-specific anti-nuclear antibodies are expressed in a mouse model of primary biliary cirrhosis and are cytokine-dependent. Clin Exp Immunol 168(3):261–267
Tsuda M, Zhang W, Yang GX, Tsuneyama K, Ando Y, Kawata K, Park O, Leung PS, Coppel RL, Ansari AA, Ridgway WM, Gao B, Lian ZX, Flavell R, He XS, Gershwin ME (2013) Deletion of interleukin (IL)-12p35 induces liver fibrosis in dominant-negative TGFbeta receptor type II mice. Hepatology 57(2):806–816
Yang GX, Lian ZX, Chuang YH, Moritoki Y, Lan RY, Wakabayashi K, Ansari AA, Flavell RA, Ridgway WM, Coppel RL, Tsuneyama K, Mackay IR, Gershwin ME (2008) Adoptive transfer of CD8(+) T cells from transforming growth factor beta receptor type II (dominant negative form) induces autoimmune cholangitis in mice. Hepatology 47(6):1974–1982
Kita H, Lian ZX, van de Water J, He XS, Matsumura S, Kaplan M, Luketic V, Coppel RL, Ansari AA, Gershwin ME (2002) Identification of HLA-A2-restricted CD8(+) cytotoxic T cell responses in primary biliary cirrhosis: T cell activation is augmented by immune complexes cross-presented by dendritic cells. J Exp Med 195(1):113–123
Kita H et al (2002) Quantitative and functional analysis of PDC-E2-specific autoreactive cytotoxic T lymphocytes in primary biliary cirrhosis. J Clin Invest 109(9):1231–1240
Yang JB et al (2016) Successful treatment of murine autoimmune cholangitis by parabiosis: implications for hematopoietic therapy. J Autoimmun 66:108–117
Wang YH, Yang W, Yang JB, Jia YJ, Tang W, Gershwin ME, Ridgway WM, Lian ZX (2015) Systems biologic analysis of T regulatory cells genetic pathways in murine primary biliary cirrhosis. J Autoimmun 59:26–37
Zeissig S, Peuker K, Iyer S, Gensollen T, Dougan SK, Olszak T, Kaser A, Blumberg RS (2017) CD1d-restricted pathways in hepatocytes control local natural killer T cell homeostasis and hepatic inflammation. Proc Natl Acad Sci U S A 114(39):10449–10454
Mattner J, Debord KL, Ismail N, Goff RD, Cantu C 3rd, Zhou D, Saint-Mezard P, Wang V, Gao Y, Yin N, Hoebe K, Schneewind O, Walker D, Beutler B, Teyton L, Savage PB, Bendelac A (2005) Exogenous and endogenous glycolipid antigens activate NKT cells during microbial infections. Nature 434(7032):525–529
Chuang YH, Lian ZX, Yang GX, Shu SA, Moritoki Y, Ridgway WM, Ansari AA, Kronenberg M, Flavell RA, Gao B, Gershwin ME (2008) Natural killer T cells exacerbate liver injury in a transforming growth factor beta receptor II dominant-negative mouse model of primary biliary cirrhosis. Hepatology 47(2):571–580
Gao B (2016) Basic liver immunology. Cell Mol Immunol 13(3):265–266
Dunn C, Brunetto M, Reynolds G, Christophides T, Kennedy PT, Lampertico P, Das A, Lopes AR, Borrow P, Williams K, Humphreys E, Afford S, Adams DH, Bertoletti A, Maini MK (2007) Cytokines induced during chronic hepatitis B virus infection promote a pathway for NK cell-mediated liver damage. J Exp Med 204(3):667–680
Hudspeth K, Pontarini E, Tentorio P, Cimino M, Donadon M, Torzilli G, Lugli E, Della Bella S, Gershwin ME, Mavilio D (2013) The role of natural killer cells in autoimmune liver disease: a comprehensive review. J Autoimmun 46:55–65
Zhao ZB et al (2019) Liver-resident NK cells suppress autoimmune cholangitis and limit the proliferation of CD4(+) T cells. Cell Mol Immunol
Moritoki Y, Zhang W, Tsuneyama K, Yoshida K, Wakabayashi K, Yang GX, Bowlus C, Ridgway WM, Ueno Y, Ansari AA, Coppel RL, Mackay IR, Flavell RA, Gershwin ME, Lian ZX (2009) B cells suppress the inflammatory response in a mouse model of primary biliary cirrhosis. Gastroenterology 136(3):1037–1047
Dhirapong A, Lleo A, Yang GX, Tsuneyama K, Dunn R, Kehry M, Packard TA, Cambier JC, Liu FT, Lindor K, Coppel RL, Ansari AA, Gershwin ME (2011) B cell depletion therapy exacerbates murine primary biliary cirrhosis. Hepatology 53(2):527–535
Moritoki Y, Lian ZX, Lindor K, Tuscano J, Tsuneyama K, Zhang W, Ueno Y, Dunn R, Kehry M, Coppel RL, Mackay IR, Gershwin ME (2009) B-cell depletion with anti-CD20 ameliorates autoimmune cholangitis but exacerbates colitis in transforming growth factor-beta receptor II dominant negative mice. Hepatology 50(6):1893–1903
Yoshida K, Yang GX, Zhang W, Tsuda M, Tsuneyama K, Moritoki Y, Ansari AA, Okazaki K, Lian ZX, Coppel RL, Mackay IR, Gershwin ME (2009) Deletion of interleukin-12p40 suppresses autoimmune cholangitis in dominant negative transforming growth factor beta receptor type II mice. Hepatology 50(5):1494–1500
Ma HD, Ma WT, Liu QZ, Zhao ZB, Liu MZ, Tsuneyama K, Gao JM, Ridgway WM, Ansari AA, Gershwin ME, Fei YY, Lian ZX (2017) Chemokine receptor CXCR3 deficiency exacerbates murine autoimmune cholangitis by promoting pathogenic CD8(+) T cell activation. J Autoimmun 78:19–28
Teng MW, Bowman EP, McElwee J, Smyth MJ, Casanova JL, Cooper AM, Cua DJ (2015) IL-12 and IL-23 cytokines: from discovery to targeted therapies for immune-mediated inflammatory diseases. Nat Med 21(7):719–729
Ando Y, Yang GX, Tsuda M, Kawata K, Zhang W, Nakajima T, Tsuneyama K, Leung P, Lian ZX, Okazaki K, Ridgway WM, Norman GL, Ansari AA, He XS, Coppel RL, Gershwin ME (2012) The immunobiology of colitis and cholangitis in interleukin-23p19 and interleukin-17A deleted dominant negative form of transforming growth factor beta receptor type II mice. Hepatology 56(4):1418–1426
Klein C, Wüstefeld T, Assmus U, Roskams T, Rose-John S, Müller M, Manns MP, Ernst M, Trautwein C (2005) The IL-6-gp130-STAT3 pathway in hepatocytes triggers liver protection in T cell-mediated liver injury. J Clin Invest 115(4):860–869
Zhang W, Tsuda M, Yang GX, Tsuneyama K, Rong G, Ridgway WM, Ansari AA, Flavell RA, Coppel RL, Lian ZX, Gershwin ME (2010) Deletion of interleukin-6 in mice with the dominant negative form of transforming growth factor beta receptor II improves colitis but exacerbates autoimmune cholangitis. Hepatology 52(1):215–222
Ma HD, Zhao ZB, Ma WT, Liu QZ, Gao CY, Li L, Wang J, Tsuneyama K, Liu B, Zhang W, Zhou Y, Gershwin ME, Lian ZX (2018) Gut microbiota translocation promotes autoimmune cholangitis. J Autoimmun 95:47–57
Aoki CA, Roifman CM, Lian ZX, Bowlus CL, Norman GL, Shoenfeld Y, Mackay IR, Gershwin ME (2006) IL-2 receptor alpha deficiency and features of primary biliary cirrhosis. J Autoimmun 27(1):50–53
Chinen T, Kannan AK, Levine AG, Fan X, Klein U, Zheng Y, Gasteiger G, Feng Y, Fontenot JD, Rudensky AY (2016) An essential role for the IL-2 receptor in Treg cell function. Nat Immunol 17(11):1322–1333
Chen J, Hou X, Jia H, Cui G, Wu Z, Wang L, Lu C, Wu W, Wei Y, Uede T, Li L, Lian Z, Diao H (2017) Regulatory T cells with a defect in inhibition on co-stimulation deteriorated primary biliary cholangitis. Oncotarget 8(65):108406–108417
Zhang W, Sharma R, Ju ST, He XS, Tao Y, Tsuneyama K, Tian Z, Lian ZX, Fu SM, Gershwin ME (2009) Deficiency in regulatory T cells results in development of antimitochondrial antibodies and autoimmune cholangitis. Hepatology 49(2):545–552
Wakabayashi K, Lian ZX, Moritoki Y, Lan RY, Tsuneyama K, Chuang YH, Yang GX, Ridgway W, Ueno Y, Ansari AA, Coppel RL, Mackay IR, Gershwin ME (2006) IL-2 receptor alpha(−/−) mice and the development of primary biliary cirrhosis. Hepatology 44(5):1240–1249
Hsu W, Zhang W, Tsuneyama K, Moritoki Y, Ridgway WM, Ansari AA, Coppel RL, Lian ZX, Mackay I, Gershwin ME (2009) Differential mechanisms in the pathogenesis of autoimmune cholangitis versus inflammatory bowel disease in interleukin-2Ralpha(−/−) mice. Hepatology 49(1):133–140
Lan RY, Selmi C, Gershwin ME (2008) The regulatory, inflammatory, and T cell programming roles of interleukin-2 (IL-2). J Autoimmun 31(1):7–12
Yao Y, Yang W, Yang YQ, Ma HD, Lu FT, Li L, Tao YY, Tsuneyama K, Zhang W, Friedman S, Gershwin ME, Lian ZX (2014) Distinct from its canonical effects, deletion of IL-12p40 induces cholangitis and fibrosis in interleukin-2Ralpha(−/−) mice. J Autoimmun 51:99–108
Lan RY, Salunga TL, Tsuneyama K, Lian ZX, Yang GX, Hsu W, Moritoki Y, Ansari AA, Kemper C, Price J, Atkinson JP, Coppel RL, Gershwin ME (2009) Hepatic IL-17 responses in human and murine primary biliary cirrhosis. J Autoimmun 32(1):43–51
Liu X, Invernizzi P, Lu Y, Kosoy R, Lu Y, Bianchi I, Podda M, Xu C, Xie G, Macciardi F, Selmi C, Lupoli S, Shigeta R, Ransom M, Lleo A, Lee AT, Mason AL, Myers RP, Peltekian KM, Ghent CN, Bernuzzi F, Zuin M, Rosina F, Borghesio E, Floreani A, Lazzari R, Niro G, Andriulli A, Muratori L, Muratori P, Almasio PL, Andreone P, Margotti M, Brunetto M, Coco B, Alvaro D, Bragazzi MC, Marra F, Pisano A, Rigamonti C, Colombo M, Marzioni M, Benedetti A, Fabris L, Strazzabosco M, Portincasa P, Palmieri VO, Tiribelli C, Croce L, Bruno S, Rossi S, Vinci M, Prisco C, Mattalia A, Toniutto P, Picciotto A, Galli A, Ferrari C, Colombo S, Casella G, Morini L, Caporaso N, Colli A, Spinzi G, Montanari R, Gregersen PK, Heathcote EJ, Hirschfield GM, Siminovitch KA, Amos CI, Gershwin ME, Seldin MF (2010) Genome-wide meta-analyses identify three loci associated with primary biliary cirrhosis. Nat Genet 42(8):658–660
Liu QZ et al (2018) The CXC chemokine receptor 3 inhibits autoimmune cholangitis via CD8(+) T cells but promotes colitis via CD4(+) T cells. Front Immunol 9:1090
Arellano G et al (2015) Stage-specific role of interferon-gamma in experimental autoimmune encephalomyelitis and multiple sclerosis. Front Immunol 6:492
Bakheet T, Frevel M, Williams BR, Greer W, Khabar KS (2001) ARED: human AU-rich element-containing mRNA database reveals an unexpectedly diverse functional repertoire of encoded proteins. Nucleic Acids Res 29(1):246–254
Hodge DL, Berthet C, Coppola V, Kastenmüller W, Buschman MD, Schaughency PM, Shirota H, Scarzello AJ, Subleski JJ, Anver MR, Ortaldo JR, Lin F, Reynolds DA, Sanford ME, Kaldis P, Tessarollo L, Klinman DM, Young HA (2014) IFN-gamma AU-rich element removal promotes chronic IFN-gamma expression and autoimmunity in mice. J Autoimmun 53:33–45
Bae HR, Leung PS, Tsuneyama K, Valencia JC, Hodge DL, Kim S, Back T, Karwan M, Merchant AS, Baba N, Feng D, Park O, Gao B, Yang GX, Gershwin ME, Young HA (2016) Chronic expression of interferon-gamma leads to murine autoimmune cholangitis with a female predominance. Hepatology 64(4):1189–1201
Bae HR, Hodge DL, Yang GX, Leung PSC, Chodisetti SB, Valencia JC, Sanford M, Fenimore JM, Rahman ZSM, Tsuneyama K, Norman GL, Gershwin ME, Young HA (2018) The interplay of type I and type II interferons in murine autoimmune cholangitis as a basis for sex-biased autoimmunity. Hepatology 67(4):1408–1419
Beuers U, Hohenester S, de Buy Wenniger LJ, Kremer AE, Jansen PL, Elferink RP (2010) The biliary HCO(3)(−) umbrella: a unifying hypothesis on pathogenetic and therapeutic aspects of fibrosing cholangiopathies. Hepatology 52(4):1489–1496
Molinaro A, Marschall HU (2017) Why doesn’t primary biliary cholangitis respond to immunosuppressive medications? Curr Hepatol Rep 16(2):119–123
Hohenester S et al (2012) A biliary HCO3- umbrella constitutes a protective mechanism against bile acid-induced injury in human cholangiocytes. Hepatology 55(1):173–183
Salas JT, Banales JM, Sarvide S, Recalde S, Ferrer A, Uriarte I, Oude Elferink RP, Prieto J, Medina JF (2008) Ae2a,b-deficient mice develop antimitochondrial antibodies and other features resembling primary biliary cirrhosis. Gastroenterology 134(5):1482–1493
Melero S, Spirlì C, Zsembery A, Medina JF, Joplin RE, Duner E, Zuin M, Neuberger JM, Prieto J, Strazzabosco M (2002) Defective regulation of cholangiocyte Cl-/HCO3(−) and Na+/H+ exchanger activities in primary biliary cirrhosis. Hepatology 35(6):1513–1521
Poupon R, Ping C, Chrétien Y, Corpechot C, Chazouillères O, Simon T, Heath SC, Matsuda F, Poupon RE, Housset C, Barbu V (2008) Genetic factors of susceptibility and of severity in primary biliary cirrhosis. J Hepatol 49(6):1038–1045
Perricone C, Colafrancesco S, Mazor RD, Soriano A, Agmon-Levin N, Shoenfeld Y (2013) Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) 2013: unveiling the pathogenic, clinical and diagnostic aspects. J Autoimmun 47:1–16
Selmi C, Leung PS, Sherr DH, Diaz M, Nyland JF, Monestier M, Rose NR, Gershwin ME (2012) Mechanisms of environmental influence on human autoimmunity: a National Institute of Environmental Health Sciences expert panel workshop. J Autoimmun 39(4):272–284
Chen RC, Naiyanetr P, Shu SA, Wang J, Yang GX, Kenny TP, Guggenheim KC, Butler JD, Bowlus C, Tao MH, Kurth MJ, Ansari AA, Kaplan M, Coppel RL, Lleo A, Gershwin ME, Leung PS (2013) Antimitochondrial antibody heterogeneity and the xenobiotic etiology of primary biliary cirrhosis. Hepatology 57(4):1498–1508
Wakabayashi K et al (2009) Induction of autoimmune cholangitis in non-obese diabetic (NOD).1101 mice following a chemical xenobiotic immunization. Clin Exp Immunol 155(3):577–586
Rojas M, Restrepo-Jiménez P, Monsalve DM, Pacheco Y, Acosta-Ampudia Y, Ramírez-Santana C, Leung PSC, Ansari AA, Gershwin ME, Anaya JM (2018) Molecular mimicry and autoimmunity. J Autoimmun 95:100–123
Amano K et al (2005) Chemical xenobiotics and mitochondrial autoantigens in primary biliary cirrhosis: identification of antibodies against a common environmental, cosmetic, and food additive, 2-octynoic acid. J Immunol 174(9):5874–5883
Wang J et al (2013) Antimitochondrial antibody recognition and structural integrity of the inner lipoyl domain of the E2 subunit of pyruvate dehydrogenase complex. J Immunol 191(5):2126–2133
Wakabayashi K, Lian ZX, Leung PS, Moritoki Y, Tsuneyama K, Kurth MJ, Lam KS, Yoshida K, Yang GX, Hibi T, Ansari AA, Ridgway WM, Coppel RL, Mackay IR, Gershwin ME (2008) Loss of tolerance in C57BL/6 mice to the autoantigen E2 subunit of pyruvate dehydrogenase by a xenobiotic with ensuing biliary ductular disease. Hepatology 48(2):531–540
Syu BJ et al (2016) Dual roles of IFN-γ and IL-4 in the natural history of murine autoimmune cholangitis: IL-30 and implications for precision medicine. Sci Rep 6:34884
Kawata K, Tsuda M, Yang GX, Zhang W, Tanaka H, Tsuneyama K, Leung P, He XS, Knechtle S, Ansari AA, Coppel RL, Gershwin ME (2013) Identification of potential cytokine pathways for therapeutic intervention in murine primary biliary cirrhosis. PLoS One 8(9):e74225
Shimoda S, Tsuneyama K, Kikuchi K, Harada K, Nakanuma Y, Nakamura M, Ishibashi H, Hisamoto S, Niiro H, Leung PS, Ansari AA, Gershwin ME, Akashi K (2012) The role of natural killer (NK) and NK T cells in the loss of tolerance in murine primary biliary cirrhosis. Clin Exp Immunol 168(3):279–284
Wu SJ, Yang YH, Tsuneyama K, Leung PS, Illarionov P, Gershwin ME, Chuang YH (2011) Innate immunity and primary biliary cirrhosis: activated invariant natural killer T cells exacerbate murine autoimmune cholangitis and fibrosis. Hepatology 53(3):915–925
Chang CH, Chen YC, Zhang W, Leung PS, Gershwin ME, Chuang YH (2015) Innate immunity drives the initiation of a murine model of primary biliary cirrhosis. PLoS One 10(3):e0121320
Chang CH, Chen YC, Yu YH, Tao MH, Leung PS, Ansari AA, Gershwin ME, Chuang YH (2014) Innate immunity drives xenobiotic-induced murine autoimmune cholangitis. Clin Exp Immunol 177(2):373–380
Ma WT et al (2017) A mouse model of autoimmune cholangitis via syngeneic bile duct protein immunization. Sci Rep 7(1):15246
Selmi C, Balkwill DL, Invernizzi P, Ansari AA, Coppel RL, Podda M, Leung PS, Kenny TP, van de Water J, Nantz MH, Kurth MJ, Gershwin ME (2003) Patients with primary biliary cirrhosis react against a ubiquitous xenobiotic-metabolizing bacterium. Hepatology 38(5):1250–1257
Padgett KA, Selmi C, Kenny TP, Leung PS, Balkwill DL, Ansari AA, Coppel RL, Gershwin ME (2005) Phylogenetic and immunological definition of four lipoylated proteins from Novosphingobium aromaticivorans, implications for primary biliary cirrhosis. J Autoimmun 24(3):209–219
Mattner J, Savage PB, Leung P, Oertelt SS, Wang V, Trivedi O, Scanlon ST, Pendem K, Teyton L, Hart J, Ridgway WM, Wicker LS, Gershwin ME, Bendelac A (2008) Liver autoimmunity triggered by microbial activation of natural killer T cells. Cell Host Microbe 3(5):304–315
Parikh-Patel A, Gold EB, Worman H, Krivy KE, Gershwin ME (2001) Risk factors for primary biliary cirrhosis in a cohort of patients from the United States. Hepatology 33(1):16–21
Hou X, Yang Y, Chen J, Jia H, Zeng P, Lv L, Lu Y, Liu X, Diao H (2019) TCRbeta repertoire of memory T cell reveals potential role for Escherichia coli in the pathogenesis of primary biliary cholangitis. Liver Int 39(5):956–966
Wang JJ et al (2014) Escherichia coli infection induces autoimmune cholangitis and anti-mitochondrial antibodies in non-obese diabetic (NOD).B6 (Idd10/Idd18) mice. Clin Exp Immunol 175(2):192–201
Bogdanos DP, Baum H, Grasso A, Okamoto M, Butler P, Ma Y, Rigopoulou E, Montalto P, Davies ET, Burroughs AK, Vergani D (2004) Microbial mimics are major targets of crossreactivity with human pyruvate dehydrogenase in primary biliary cirrhosis. J Hepatol 40(1):31–39
Dyson JK, Beuers U, Jones DEJ, Lohse AW, Hudson M (2018) Primary sclerosing cholangitis. Lancet 391(10139):2547–2559
Lazaridis KN, LaRusso NF (2016) Primary sclerosing cholangitis. N Engl J Med 375(12):1161–1170
Sabino J, Vieira-Silva S, Machiels K, Joossens M, Falony G, Ballet V, Ferrante M, van Assche G, van der Merwe S, Vermeire S, Raes J (2016) Primary sclerosing cholangitis is characterised by intestinal dysbiosis independent from IBD. Gut 65(10):1681–1689
Hov JR, Boberg KM, Karlsen TH (2008) Autoantibodies in primary sclerosing cholangitis. World J Gastroenterol 14(24):3781–3791
Terziroli Beretta-Piccoli B, Mieli-Vergani G, Vergani D (2018) The clinical usage and definition of autoantibodies in immune-mediated liver disease: a comprehensive overview. J Autoimmun 95:144–158
Smit JJ et al (1993) Homozygous disruption of the murine mdr2 P-glycoprotein gene leads to a complete absence of phospholipid from bile and to liver disease. Cell 75(3):451–462
Tebbi A, Levillayer F, Jouvion G, Fiette L, Soubigou G, Varet H, Boudjadja N, Cairo S, Hashimoto K, Suzuki AM, Carninci P, Carissimo A, di Bernardo D, Wei Y (2016) Deficiency of multidrug resistance 2 contributes to cell transformation through oxidative stress. Carcinogenesis 37(1):39–48
Popov Y, Patsenker E, Fickert P, Trauner M, Schuppan D (2005) Mdr2 (Abcb4)−/− mice spontaneously develop severe biliary fibrosis via massive dysregulation of pro- and antifibrogenic genes. J Hepatol 43(6):1045–1054
Ikenaga N, Liu SB, Sverdlov DY, Yoshida S, Nasser I, Ke Q, Kang PM, Popov Y (2015) A new Mdr2(−/−) mouse model of sclerosing cholangitis with rapid fibrosis progression, early-onset portal hypertension, and liver cancer. Am J Pathol 185(2):325–334
Halilbasic E, Fiorotto R, Fickert P, Marschall HU, Moustafa T, Spirli C, Fuchsbichler A, Gumhold J, Silbert D, Zatloukal K, Langner C, Maitra U, Denk H, Hofmann AF, Strazzabosco M, Trauner M (2009) Side chain structure determines unique physiologic and therapeutic properties of norursodeoxycholic acid in Mdr2−/− mice. Hepatology 49(6):1972–1981
Fickert P, Pollheimer MJ, Beuers U, Lackner C, Hirschfield G, Housset C, Keitel V, Schramm C, Marschall HU, Karlsen TH, Melum E, Kaser A, Eksteen B, Strazzabosco M, Manns M, Trauner M, International PSC Study Group (IPSCSG) (2014) Characterization of animal models for primary sclerosing cholangitis (PSC). J Hepatol 60(6):1290–1303
Peng ZW, Rothweiler S, Wei G, Ikenaga N, Liu SB, Sverdlov DY, Vaid KA, Longhi MS, Kuang M, Robson SC, Popov YV (2017) The ectonucleotidase ENTPD1/CD39 limits biliary injury and fibrosis in mouse models of sclerosing cholangitis. Hepatol Commun 1(9):957–972
Tedesco D, Thapa M, Chin CY, Ge Y, Gong M, Li J, Gumber S, Speck P, Elrod EJ, Burd EM, Kitchens WH, Magliocca JF, Adams AB, Weiss DS, Mohamadzadeh M, Grakoui A (2018) Alterations in intestinal microbiota lead to production of interleukin 17 by intrahepatic gammadelta T-cell receptor-positive cells and pathogenesis of cholestatic liver disease. Gastroenterology 154(8):2178–2193
Tabibian JH, O’Hara SP, Trussoni CE, Tietz PS, Splinter PL, Mounajjed T, Hagey LR, LaRusso N (2016) Absence of the intestinal microbiota exacerbates hepatobiliary disease in a murine model of primary sclerosing cholangitis. Hepatology 63(1):185–196
Kotb MA (2012) Molecular mechanisms of ursodeoxycholic acid toxicity & side effects: ursodeoxycholic acid freezes regeneration & induces hibernation mode. Int J Mol Sci 13(7):8882–8914
Allegretti JR, Kassam Z, Carrellas M, Mullish BH, Marchesi JR, Pechlivanis A, Smith M, Gerardin Y, Timberlake S, Pratt DS, Korzenik JR (2019) Fecal microbiota transplantation in patients with primary Sclerosing cholangitis: a pilot clinical trial. Am J Gastroenterol 114(7):1071–1079
Fickert P et al (2007) A new xenobiotic-induced mouse model of sclerosing cholangitis and biliary fibrosis. Am J Pathol 171(2):525–536
Marzioni M, Saccomanno S, Agostinelli L, Rychlicki C, de Minicis S, Pierantonelli I, Trauner M, Fickert P, Müller T, Shanmukhappa K, Trozzi L, Candelaresi C, Baroni GS, Benedetti A (2013) PDX-1/Hes-1 interactions determine cholangiocyte proliferative response to injury in rodents: possible implications for sclerosing cholangitis. J Hepatol 58(4):750–756
Karlsen TH, Folseraas T, Thorburn D, Vesterhus M (2017) Primary sclerosing cholangitis—a comprehensive review. J Hepatol 67(6):1298–1323
Trauner M, Fickert P, Wagner M (2007) MDR3 (ABCB4) defects: a paradigm for the genetics of adult cholestatic syndromes. Semin Liver Dis 27(1):77–98
Erkes DA, Selvan SR (2014) Hapten-induced contact hypersensitivity, autoimmune reactions, and tumor regression: plausibility of mediating antitumor immunity. J Immunol Res 2014:175265
Mourelle M et al (1995) Induction of chronic cholangitis in the rat by trinitrobenzenesulfonic acid. J Hepatol 22(2):219–225
Chiang JY (2017, 2029) Recent advances in understanding bile acid homeostasis. F1000Res 6
Fickert P et al (2006) Lithocholic acid feeding induces segmental bile duct obstruction and destructive cholangitis in mice. Am J Pathol 168(2):410–422
Chiang JYL, Ferrell JM (2018) Bile acid metabolism in liver pathobiology. Gene Expr 18(2):71–87
Fabris L et al (2006) Effects of angiogenic factor overexpression by human and rodent cholangiocytes in polycystic liver diseases. Hepatology 43(5):1001–1012
Kamisawa T, Zen Y, Pillai S, Stone JH (2015) IgG4-related disease. Lancet 385(9976):1460–1471
Culver EL, Chapman RW (2016) IgG4-related hepatobiliary disease: an overview. Nat Rev Gastroenterol Hepatol 13(10):601–612
Yamada K, Zuka M, Ito K, Mizuguchi K, Kakuchi Y, Onoe T, Suzuki Y, Yamagishi M, Izui S, Malissen M, Malissen B, Kawano M (2018) LatY136F knock-in mouse model for human IgG4-related disease. PLoS One 13(6):e0198417
Liberal R, Grant CR (2016) Cirrhosis and autoimmune liver disease: current understanding. World J Hepatol 8(28):1157–1168
Larson L, James M, Gossard A (2016) Cholestatic liver injury: care of patients with primary biliary cholangitis or primary sclerosing cholangitis. AACN Adv Crit Care 27(4):441–452
Xie YQ, Ma HD, Lian ZX (2016) Epigenetics and primary biliary cirrhosis: a comprehensive review and implications for autoimmunity. Clin Rev Allergy Immunol 50(3):390–403
Chascsa D, Carey EJ, Lindor KD (2017) Old and new treatments for primary biliary cholangitis. Liver Int 37(4):490–499
Tanaka A (2019) Emerging novel treatments for autoimmune liver diseases. Hepatol Res 49(5):489–499
Beura LK, Hamilton SE, Bi K, Schenkel JM, Odumade OA, Casey KA, Thompson EA, Fraser KA, Rosato PC, Filali-Mouhim A, Sekaly RP, Jenkins MK, Vezys V, Haining WN, Jameson SC, Masopust D (2016) Normalizing the environment recapitulates adult human immune traits in laboratory mice. Nature 532(7600):512–516
Rosshart SP et al (2019) Laboratory mice born to wild mice have natural microbiota and model human immune responses. Science 365(6452)
Rosshart SP, Vassallo BG, Angeletti D, Hutchinson DS, Morgan AP, Takeda K, Hickman HD, McCulloch J, Badger JH, Ajami NJ, Trinchieri G, Pardo-Manuel de Villena F, Yewdell JW, Rehermann B (2017) Wild mouse gut microbiota promotes host fitness and improves disease resistance. Cell 171(5):1015–1028 e13
Funding
This work is supported by the Program for Guangdong Introducing Innovative and Enterpreneurial Teams (2017ZT07S054), the National Natural Science Foundation of China (81801607, 81873877, 81901652), China Postdoctoral Science Foundation (2018 M643095), and State Key Laboratory of Pathogenesis, Prevention, Treatment of Central Asian High Incidence Diseases Fund, China (SKL-HIDCA-2018-4).
Author information
Authors and Affiliations
Contributions
Shou-Pei, Zhen-Hua Bian, Zhi-Bin Zhao, Jinjun Wang, and Liang Li wrote the manuscript. Shou-Pei Liu, Zhen-Hua Bian, and Liang Li designed and drew the figures. Weici Zhang, Patrick S.C. Leung, and Zhe-Xiong Lian wrote and edited the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, SP., Bian, ZH., Zhao, ZB. et al. Animal Models of Autoimmune Liver Diseases: a Comprehensive Review. Clinic Rev Allerg Immunol 58, 252–271 (2020). https://doi.org/10.1007/s12016-020-08778-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-020-08778-6