Abstract
Multipotent mesenchymal stem/stromal cells (MSCs) have regenerative and immunomodulatory properties to restore and repair injured tissues, making them attractive candidates for cell-based therapies. Experimental and clinical evidence has demonstrated the effectiveness of MSC transplantation in managing diabetes mellitus (DM). Autologous MSCs are assumed to be favorable because patient-derived cells are readily available and do not entail sustained immunosuppressive therapy. DM is associated with hyperglycemia, oxidative stress and altered immune responses and inflammation. It may thus alter the biological characteristics and therapeutic qualities of human MSCs (hMSCs). Several studies have explored the effect of DM or the diabetic microenvironment on the engraftment and efficacy of transplanted MSCs, which are determined by proliferation, differentiation, senescence, angiogenesis supportive effect, migration, anti-oxidative capacity and immunomodulatory properties. This review aims to present the available data on how DM impacts MSC biology and functionality and identify future perspectives for autologous MSC-based therapy in diabetics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is the most common metabolic disease with a rapid annual increase worldwide [1, 2]. DM leads to many life-threatening complications affecting major organs, especially the kidneys, heart and eyes [3]. The global healthcare expenditure on diabetic patients was estimated to be 850 billion USD in 2017 [4]. Type 1 DM (DMT1) is an autoimmune disease characterized by insulin deficiency due to T cell-mediated destruction of insulin-secreting beta (β-) cells [5]. Type 2 DM (DMT2), on the other hand, is the predominant type of diabetes and is characterized by metabolically abnormal and inflamed adipose tissue (AT) and adipocytokine imbalance. DMT2 is also associated with oxidative and endoplasmic reticulum stress [6]. All of these factors contribute to insulin resistance and β-cell apoptosis and exhaustion [7]. Gestational DM (GDM) is an impaired glucose tolerance that develops during pregnancy as a result of obesity or advanced maternal age and confers an increased risk for complications for both mother and offspring [8].
Dietary control, oral hypoglycemic agents, and insulin are the current treatment options; however, these options cannot achieve long-term blood glucose homeostasis [9]. Whole pancreas or islet transplantation is effective in achieving posttransplantation insulin discontinuation [10, 11]. However, surgery-associated risks, the need for lifelong immunosuppression, and the scarcity of organ donors all limit the clinical applicability of these regimens [12]. A cure for DM requires correcting metabolic dysregulation and resetting immune homeostasis. In addition to dietary control, oral hypoglycemic agents, and insulin, significant research is ongoing to develop stem cell therapy in an effort to cure diabetes [13].
Mesenchymal stem/stromal cells (MSCs) have been used in several experimental and clinical therapeutic approaches for DM treatment. MSCs are multipotent progenitors that have been isolated from many tissues, including the bone marrow (BM) [14], AT [15], umbilical cord (UC) matrix [16] and blood [17], dental pulp [18] and periodontal ligaments [19]. MSCs are able to self-renew, differentiate into mesodermal [14] and nonmesodermal [20] tissues and exhibit regenerative and immunomodulatory properties [21].
MSCs have been reported to successfully adopt an insulin-secreting phenotype in vitro [22, 23] and in vivo [24, 25]. In experimental DM, administration of MSCs was found to reverse hyperglycemia [25,26,27,28,29,30,31,32,33,34]. Such an anti-hyperglycemic effect was achieved via several mechanisms that include selective homing and engraftment into damaged pancreatic tissues [27], inducing the regeneration of new functional insulin-producing β-cells from endogenous progenitors and increasing the number of pancreatic islets [26, 31]. Other mechanisms include enhancing the survival and self-replication of pre-existing β-cells [2] and stimulating revascularization of damaged islets [26], in addition to improving insulin sensitivity in peripheral tissues [31]. Furthermore, MSCs were found to play a role in regulating hepatic glucose metabolism [33] and managing exacerbated autoimmune responses [28, 29] and inflammation [34]. However, the latter was partially achieved by inducing regulatory immune phenotypes [29, 30] to protect endogenous cells from further destruction and apoptosis.
MSCs modify the pancreatic microenvironment and achieve reparative properties via secretion of a wide range of trophic factors [35]. Factors such as vascular endothelial growth factor (VEGF), hepatocyte growth factor (HGF), epidermal growth factor (EGF), fibroblast growth factor(s), angiopoietin-1 (Ang-1) and angiopoietin-2 (Ang-2) mediate angiogenesis-supportive and anti-apoptotic potentials of MSCs [36, 37]. Indoleamine oxygenase (IDO), interleukin-10 (IL-10), prostaglandin E2 (PGE2), tumor necrosis factor-stimulated gene 6 (TSG6), human leukocyte antigen G (HLA-G) and transforming growth factor β(TGFβ), among others, contribute to MSC regulatory actions on diverse immune cell subsets [25, 38].
Despite low immunogenicity due to the lack of expression of major histocompatibility class II (MHC-II) and costimulatory molecules [39], allogeneic MSCs can still be recognized and rejected by the recipient’s immune system [40, 41]. Generation of the immune response after allogeneic transplantation is still a confounding factor that requires investigation [40]. Autologous stem cell transplantation has thus become more preferred than allogeneic transplantation and may be the safest approach to clinical cellular therapy. However, while autologous transplantation may be effective in BM disorders, its usefulness in a metabolic disease such as DM is still disputed [13].
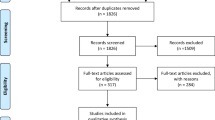
The diabetic microenvironment is characterized by hyperglycemia, altered immune responses, and oxidative stress, all of which were found to alter BMSC properties and functions [42]. We summarize the published studies on the impact of the diabetic microenvironment in T1DM, T2DM, and GDM on different human tissue-derived MSCs in terms of phenotype, cell viability, stemness, proliferation, multipotency, glucose metabolism, angiogenic potential, migration, immunomodulation and β-cell regenerative ability (Table 1). Table 2 summarizes the effects of diabetic milieu (hyperglycemia and hypoxia) in culture conditions on the same MSC properties. In Table 3, we review the clinical studies that evaluated the efficacy of autologous MSCs in the management of hyperglycemia and insulin sensitivity in diabetic patients. Finally, strategies to improve the survival and therapeutic efficacy of MSCs in diabetic patients are recommended. Abbreviations are listed in a supplementary file.
MSC Number and Colony Formation in the Diabetic Microenvironment
DM, even in the presence of a vascular disease, did not significantly alter the efficiency of isolation of AT-derived stromal cells (ASCs), as evaluated by the number of isolated cells per gram of AT. AT from diabetic donors yielded 224,028 ± 20,231 cells/g and 259,345 ± 15,441 cells/g from nondiabetic subjects (p > 0.05) [55]. Another study investigated how the diabetic microenvironment modified the stromal vascular fraction (SVF) (mononuclear cells that were initially obtained after the enzymatic digestion of AT and centrifugation of the isolate). Neither advanced age nor the presence of comorbidities, including diabetes, obesity, perivascular disease (PVD) or end stage renal disease, significantly affected the number of cells in the SVF. Similarly, the number of ASC populations (depleted of CD31+/endothelial and CD45+/monocyte cells) was not affected by the diabetic microenvironment [46]. However, diabetes tended to decrease the SVF and ASC counts, whereas PVD tended to increase ASC yield.
Due to AT dysfunction in DM [93], Harris et al. attributed the poor stem cell availability to chronic glycosylation of their surface proteins. This has led to the attenuated ability of collagenase to release the cells during the isolation procedure [46]. In contrast, the number of ASCs recovered from visceral AT was significantly higher in diabetic cultures than in healthy cultures [50]. This result was suggested to be a result of high glucose (HG) concentrations in the diabetic adipose stem cell niche promoting OCT4-mediated dedifferentiation of ASCs [50].
A colony-forming unit (CFU) assay was used in several studies to assess the “stemness” potential of diabetic MSCs. Davies et al. explored the effect of early- and late-diagnosed DMT1 on the colony forming capacity of BM-derived stem cells [60]. The authors reported an age-related decline in the number of mononuclear cells (BM-MNCs) isolated from diabetic or healthy donors, irrespective of the disease status. No significant difference in the colony-forming ability of DMT1-MSCs was evident compared with healthy BMSCs [60]. Similarly, a comparable MSC colony count was reported in cultures of healthy cells or cells from diabetic and ischemic subjects [59]. In contrast, Cramer et al. reported that the colony count was lower for ASCs isolated from both nondiabetic (ND) and diabetic (D) subjects when cultured in a medium supplemented with a HG concentration. Insulin treatment increased CFUs in both HG-treated ND-ASCs and D-ASCs [45].
Lee et al. reported attenuated clonogenic potential of SVF cells isolated from diabetic patients with critical limb ischemia (CLI) compared with healthy subjects. However, this finding was correlated with fewer ASCs and lower density in the diabetic SVF [48]. Decreased clonogenic potential was detected for placenta-derived MSCs (P-MSCs) obtained from women with GDM [71]. In accordance with these data, compromised colony forming efficiency of ASCs from DMT2 was recently reported and was improved after culture treatment with a low concentration of basic fibroblast growth factor (bFGF) [66].
Phenotype of MSCs
According to the International Society for Cellular Therapy, MSCs are positive for CD73, CD90, CD105 and HLA-I markers, whereas they lack expression of CD14, CD34, CD45 and HLA-II markers [94]. The immunophenotype of MSCs isolated from diabetic patients was characterized by several investigators [38, 44, 46, 50,51,52, 54, 56, 59,60,61,62, 66]. In comparison to healthy counterparts, a comparable phenotype was exhibited by MSCs isolated from patients with DMT2 [44, 56, 62, 66] or recently diagnosed with DMT1 [38, 60, 61]. The copresence of diabetes and coronary artery disease (CAD) did not affect the uniform mesenchymal phenotype of BMSCs (CD44+, CD29+, CD34− and CD45−) or ASCs (CD73+, CD90, CD105, NG2+, PDGFRB+, CD14low/−, CD19low/−, CD34low/−, CD45low/− and CD279low/−) [52]. Furthermore, Brewster et al. reported that BMSCs isolated from amputated ischemic limbs of diabetic patients retained the mesenchymal immunophenotype [59].
However, few studies have reported changes in MSC immunophenotypes in the diabetic microenvironment [50, 54]. ASCs isolated from DMT2 patients exhibited levels of the mesenchymal markers CD29 and CD44 similar to those of normal cells. However, levels of stemness markers CD105 and CD90 higher than those derived from healthy subjects were reported [50]. Koci et al. assessed the expression levels of a considerable number of cell surface markers, including CD29, CD73, CD90, CD105, CD271, anti-human fibroblast surface protein, CD31, CD45, CD146, HLA-ABC, CD133, CD235a, and VEGFR2. ASCs isolated from ATs of distal ischemic limbs of diabetic patients were compared to those isolated from nondiabetic controls [54]. Both ND-and ischemic D-ASCs exhibited comparable phenotypes [95, 96]. However, ischemic diabetic ASC cultures were contaminated with a high ratio of fibroblasts (40%, based on the expression of anti-fibroblast protein) compared to 20% in nondiabetic cultures. Inverse correlation was evident between the expression levels of CD105 and the anti-fibroblast protein. These results indicate that AT from ischemic limbs may not yield a fibroblast-free ASC population, especially in the presence of DM [54]. This finding should be considered when selecting autologous ASCs for stem cell therapy in DM.
Glucose concentration in cell culture medium is another factor that modulates stem cell phenotype. A concentration of 5.5 mmol/l in culture medium is considered low, while a concentration of 11 mmol/l or above is considered high [76]. Concentrations of 25 mmol/l and 30 mM D-glucose were commonly used to represent the diabetic hyperglycemic state. Human MSCs (hMSCs) isolated from subcutaneous fat, omental fat and BM were extensively cultured in HG (25 mmol/l) culture medium and analyzed for the expression profile of diverse surface markers [76]. These markers included those of hematopoietic stem cells (HSCs), such as CD34, CD45 and HLA-DRl; MSCs, such as CD90, CD105, and CD73; cell adhesion molecules, such as CD29, CD44 and CD106; surface enzymes, such as CD13; aldehyde dehydrogenase (ALDH); and pluripotent markers, such as stage-specific embryonic antigen 4 (SSEA4). MSCs from the three sources exhibited comparable immunophenotypes, which were seemingly unaltered by HG culture conditions [76].
Viability, Senescence, and Stemness of MSCs
DM adversely affects the viability and induces senescence and/or apoptosis of hMSCs derived from different sources, including BM [51], AT [45, 62, 66] and UC [69, 70]. DMT2-ASCs showed higher levels of cellular senescence and apoptosis than did ND-ASCs in LG or HG culture conditions. HG was found to induce apoptosis via activation of extrinsic caspase pathways in ND-ASCs and the intrinsic pathway in D-ASCs. Importantly, cell treatment with insulin was able to recover HG-induced apoptosis in ND- and D-ASC cultures; however, the latter were less responsive [45]. GDM was found to induce premature senescence in UC-MSCs most likely via disrupting mitochondrial functions as presented, among others, by reduced mRNA levels of mitochondrial-related genes, altered mitochondrial membrane integrity and potential, and enhanced mitochondrial superoxide generation [70]. In support of these data, HG treatment induced the generation of reactive oxygen species (ROS) in normal ASCs, resulting in mitochondrial dysfunction. This defect was represented by decreased mitochondrial membrane potential and changes in mitochondrial morphology. This deviation in mitochondrial functioning was suggested to be an early sign of apoptosis [83]. Cell viability was also significantly reduced in hMSCs incubated with DMT2 sera [86,87,88]. Moreover, induced apoptotic cell response and cell damage have been reported [86, 87]. Kim et al. demonstrated that HG in culture was found to induce the replicative senescence of hASCs via inducing microRNA (miR)-486-5p expression, which in turn downregulated the expression of silent information regulator 1 (SIRT1) [75]. SIRT1, a NAD-dependent deacetylase, regulates the expression of genes involved in the cell cycle, senescence, apoptosis and metabolism [97], as well as insulin sensitivity in target tissues [98]. SIRT1 expression was downregulated in DMT2-ASCs and was associated with upregulated levels of its target, P53, which is an apoptosis-inducing marker [66]. Importantly, stimulation of D-ASCs in that study with bFGF was found to upregulate SIRT1 mRNA and to suppress senescence and apoptosis. In contrast to previous studies, Lafosse et al. reported that ND-ACSs and DMT2-ASCs exhibited comparable survival rates, even in an in vitro diabetic wound microenvironment (hypoxia and hyperglycemia) [63].
To investigate the influence of the diabetic microenvironment on stemness-related markers, two recent studies reported that DMT2-ASCs isolated from visceral [50] or subcutaneous [62] ATs exhibited significantly upregulated levels of pluripotency regulators, such as OCT4 and NANOG, compared with ND-ASCs. These data indicate that D-ASCs are more dedifferentiated/immature than ND-ASCs. In vitro culture of human BMSCs derived from healthy donors in a HG vs. low glucose (LG) culture medium (25 mmol/dl vs 5 mmol/dl D-glucose, respectively) for 72 h did not affect the gene expression of the pluripotency markers OCT4 and FOXD3 but increased that of SOX-2, suggesting that hMSCs are able to maintain the undifferentiated state under HG stress [74]. However, the enhanced stemness in D-MSCs or HG-treated cells may be associated with premature senescence and impaired regenerative potential. It has been thus proposed that early passages of MSCs are preferable for clinical purposes [62].
Growth and Proliferation
Some reports showed that DM did not impair the growth or in vitro expansion of MSCs isolated from different sources [47, 55, 59,60,61]. D-ASCs exhibited proliferative activity similar to that of ND-ASCs under normoxia. However, in response to hypoxia, D-ASCs showed attenuated proliferation [47]. DM, even in the presence of a vascular disease, did not seem to alter the proliferation of ASCs [55]. Compared to healthy BMSCs, MSCs from BM aspirates from the tibia of ischemic amputated limbs exhibited comparable proliferation at early passages. However, diminished proliferation at late passages, with a more remarkable attenuation in the presence of DM, was observed [59]. Recently, no differences in proliferation capacity between ND-BMSCs and BMSCs from EDMT1 [60, 61] and LDMT1 [60] patients were detected. In accordance with these data and in an ex vivo-created diabetic microenvironment (hypoxia and HG culture conditions), DMT2-ASCs exhibited growth rates similar to those of healthy ASCs. These studies imply that a sufficient therapeutic number of diabetic MSCs could be expanded in a time frame similar to that of healthy cells [60]. Some studies have reported that culture of hMSCs in HG medium (25 mM) did not acutely affect [72, 73, 76, 83] or enhance [50, 74, 99] cell proliferation. Deeper insight into the mechanisms underlying the HG-stimulatory effect on MSC proliferation revealed that HG induced the expression of the cell cycle regulatory proteins cyclin D1 and cyclin E in hBMSCs through the upregulation of TGFβ1 expression via the activation of the Ca+2/PKC/MAPK and PI3K/Akt/mTOR signaling pathways [74]. Dentelli et al. identified that HG was able to induce NADPH oxidase-dependent generation of nontoxic levels of ROS, in addition to activating AKT kinases in visceral ASCs [50]. ROS and AKT were thus proposed to be crucial regulators for stem cell biology and fate [100].
In contrast, several studies reported that DM impaired the proliferation of MSCs isolated from BM [44, 51], AT [45, 48, 62], cardiac auricles [56], and UC [69, 70]. Gene expression and/or protein studies demonstrated that DM-induced decline in MSC proliferation was associated with diminished levels of proliferation markers such as Bcl2 [51]. There was also attenuation of phosphorylation of serine 10 on histone H3 (H3S10P) and/or the histone variant H3.3, a marker of active cell cycle S phase [56]. By investigating the epigenetic modifications that may be associated with DM-induced alterations in MSC characteristics, Vecellio et al. identified reduced mRNA levels of two epigenetic enzymes, Aurora B and C kinases, involved in cell cycle progression in diabetic cardiac auricle MSCs (D-cMSCs). In addition, several modifications known to be associated with closed chromatin structure and transcription repression were found in histones 3 and 4 in D-cMSCs. These modifications included decreased histone acetylation but increased methylation [56]. Deeper mechanistic insight demonstrated that some histone methylases were overexpressed. However, two Gcn5-related N-acetyltransferases (GCN5A and PCAF) [101] were significantly reduced in D-cMSCs [56].
Treatment with SPV106/pentadecylidenemalonate 1b reversed DM-induced epigenetic changes in cMSCs. SPV106/pentadecylidenemalonate 1b is a pro-acetylation pharmacological compound that acts via activation of the GCN5A/PCAF members of the GNAT family. This activation promotes the acetylation of histones and histone proteins and accesses the transcription of proliferation promoting markers and cell cycle control elements [102].
GDM was found to decrease proliferation of UC-MSCs and upregulate expression of cyclin-dependent kinase inhibitor transcripts p16 and p27. This was attributed to impaired mitochondrial functions and enhanced ROS generation to toxic levels [70]. In another study, enhanced proliferation and shorter telomere length were detected in ASCs derived from patients with DMT2-associated CAD [52].
Telomere shortening is a marker of replicative senescence and might reflect chronic pathologies associated with depletion of stem cells and progenitor compartments [52]. A recent global DNA methylation analysis was performed to determine epigenetic changes in DMT2- cardiac MSCs (CMSCs) and to investigate the role of α-ketoglutarate (αKG) in the control of DNA demethylation in these cells [67]. The accumulation of 5 methylated cytosine (5mC) and its oxidized products 5 hydroxymethylated cytosine (5hmC) and 5 formyl cytosine (5fC) occurred in the DNA of human CMSCs derived from DMT2 patients. To determine whether elevated DNA methylation in DMT2-CMSCs was associated with transcriptional repression, transcriptome analysis followed by functional analysis was carried out. Downregulated transcripts significantly enriched in cell metabolism, cell replication, mismatch and base excision repair were identified in DMT2-CMSCs. Monitoring the activity of two epigenetic DNA demethylation enzymes, thymine DNA glycosylase (TDG) and ten eleven translocation 1 (TET), demonstrated compromised functioning in DMT2-CMSCs [103]. These data were paralleled by the evidence of a weak association between TET1 and TDG to form a complex required for further TDG activation. These findings suggested inhibited the DNA demethylation process in metabolically compromised CMSCs.
In DMT2-CMSCs, a significant reduction was observed in the intracellular content of αKG and the activity of isocitrate dehydrogenase (IDH), the enzyme responsible for αKG synthesis. Importantly, exogenous addition of αKG was found to trigger TET1/TDG complex formation and TDG activation, eventually reducing global DNA methylation and restoring compromised functions in D-CMSCs as cell proliferation [67].
Several studies showed that culture in HG medium impaired proliferation of different tissue-derived MSCs [45, 62, 75, 80, 82, 104]. This compromised proliferation was likely attributed to the HG modulatory effect on signaling pathways that regulate MSC proliferation and stemness, such as JAK2/STAT3, P38 MAPK or AKT kinases [62, 82]. It is worth mentioning that the two studies were performed with a relatively similar design but showed contradictory results. While Dentelli et al. reported a stimulatory effect of HG on visceral ASCs [50], Cheng et al. reported an inhibitory effect of HG on subcutaneous ASCs [62]. Surprisingly, these findings were attributed to HG-induced ROS generation leading to AKT activation in visceral ASCs but to its inhibition in subcutaneous ASCs. These contradictory results may be related to variability in the inherent biological properties and responses of the two ASC populations used in the two studies, based on different anatomical origins of AT.
Multipotency
Mesodermal Differentiation Potential
A number of studies have reported that diabetes alone [44, 50, 58] or with other comorbidities [52, 59] did not alter the multipotency of hMSCs. Through exposure to the corresponding lineage-specific differentiation medium, commitment of DMT2-BMSCs [61], EDMT1-BMSCs [38, 60, 61] or LDMT1-BMSCs to differentiate into adipocytes, osteocytes or chondrocytes was comparable to that of ND-BMSCs. Maintained adipogenic potential of DMT2-ASCs was also reported [50, 58]. When DMT2-ASCs were induced to differentiate and mature into adipocytes in three-dimensional bioreactors, there were no significant differences in the metabolic activity, functionality and architecture of adipocytes generated from both diabetic and nondiabetic ASCs [58]. These findings suggest that once ASCs were removed from the hyperglycemic and hyperinsulinemic milieu of DMT2, they retained no memory of the diseased state [58].
Other studies, however, found that DM alone or associated with one of its complications could dysregulate MSC adipogenesis [45, 56, 68], osteogenesis [45, 54, 57], or both [70]. DMT2 has been associated with excessive fat mass in the BM at the expense of hematopoietic tissue [105]. Using an in vitro approach, a diabetic feedback loop was recently proposed. BMSCs were constitutively primed to generate adipocytes that fueled BMSC differentiation into new fat via monocyte chemoattractant protein-1 (MCP-1). Importantly, pharmacological inhibition of MCP-1 signaling contrasted this vicious cycle restoring, at least in part, the balance between adipogenesis and hematopoiesis in DMT2- BM [68]. MCP-1 signals through the CCR2 receptor to induce the transcription of MCP-1-induced protein (MCPIP). The latter promotes adipogenic differentiation in a peroxisome proliferator-activated receptor γ (PPARγ)-independent manner [106]. In contrast, attenuated osteogenic potency was identified for ASCs derived from subcutaneous AT of ischemic lower limbs of diabetic patients [54].
GDM was also found to impair the osteogenic potency of UC-MSCs [70]. The copresence of diabetes and periodontitis compromised the osteogenic potential of periodontal ligament stem cells (PDLSCs) in vitro and in vivo [57]. Activated canonical Wnt signaling was shown to have an inhibitory role in the osteogenic differentiation of PDLSCs under inflammatory conditions [107]. Thus, the addition of Dickkopf-1 (DKK-1), a soluble inhibitor of Wnt/β-catenin signaling [108], significantly improved the osteogenic and bone-forming ability of defective PDLSCs derived from patients with diabetes-induced periodontitis [57]. These findings diverge with data showing that activation of Wnt/β-catenin signaling promoted the osteogenesis of MSCs [109]. Impaired mitochondrial biogenesis and functions and altered energetic status contribute to deteriorated osteogenic differentiation of ASCs derived from equine metabolic syndrome via predominance of autophagy over selective mitophagy [110].
Several in vitro studies have explored the effect of HG culture on the mesodermal differentiation capabilities of hMSCs [45, 82, 111]. HG was found to skew the differentiation potential of MSCs into adipocyte lineage in favor of osteogenic and chondrogenic lineages [111]. This effect was proposed to be mediated via the inhibitory effect of HG on Wnt/β-catenin signaling, which acts as a brake for adipogenic differentiation [112]. Aguiari et al. showed that culture of human ASCs and muscle-derived stem cells in a dynamic perfusion system under HG conditions stimulated the spontaneous differentiation and trans-differentiation of these cells into mature adipocytes. The latter successfully formed a viable and vascularized AT in vivo [113]. HG is a state of oxidative stress that activates the generation of ROS via NADPH oxidase [114], xanthine oxidase [115], or the mitochondrial respiratory chain [116]. However, Aguiari et al. proposed that the generated levels of ROS were enough to induce differentiation, not toxicity. ROS in turn activate PKCβ, which is an effector kinase mediating the adipogenic-differentiation potential of HG [113]. Similarly, it was reported that HG induced adipogenic differentiation of MSCs derived from BM and gestational tissues, including the chorion, placenta and UC. This differentiation was associated with upregulated expression of key adipogenic markers, such as PPARγ and lipoprotein lipase (LPL), in BMSCs and adiponectin and LPL [82].
On the other hand, data showed that HG had a detrimental effect on the osteogenic differentiation of MSCs [45, 77,78,79,80, 85, 104]. This was manifested by attenuated calcium deposition, reduced alkaline phosphatase activity and/or downregulated expression of osteogenic markers such as run-related gene 2 (Runx2), osterix (Osx), osteopontin (OPN), and osteocalcin (OCN) [77,78,79,80]. The anti-osteogenic effect was attributed to several factors, including HG-induced oxidative damage/stress [77, 79, 104] and elevated global DNA methylation [78]. Mechanisms included suppression of PI3K/AKT [77, 79] and/or Wnt/β-catenin [77, 78] pathways and activation of the inflammatory pathway nuclear factor kappa (NF-Kβ) [80]. Very recently, Qu et al. found that miR-449 was significantly upregulated during osteogenic differentiation of hBMSCs in the presence of HG and free fatty acid (FFA) [85]. On the molecular level, miR-449 directly suppressed bone formation by SIRT1, [117] by binding to its 3’-UTR during osteogenic differentiation [85]. Furthermore, miR-449 overexpression decreased the mRNA and protein levels of Fra-1, a c-fos-related protein that plays an essential role in osteogenesis [118]. Importantly, SIRT1 overexpression reversed the miR-449 inhibitory effect on Fra-1 expression. Thus, miR-449 overexpression inhibited osteogenic differentiation of HG-FFA-treated hBMSCs by suppressing the Sirt1/Fra-1 axis. These findings might explain the mechanism underlying DM-induced osteoporosis and suggest modulating miR-449 as a possible intervention strategy in diabetic osteoporosis [85].
Neurogenic Differentiation Potential
Sawangmake et al. investigated the neurogenic differentiation of hPDLSCs with or without HG by employing a two-stage protocol that comprises neuroprogenitor (neurosphere) formation and neuronal cell maturation. HG was found to attenuate neurosphere formation efficiency by hPDLSCs in terms of morphology and neurogenic marker expression but without adversely affecting cell viability. In contrast, HG did not affect the maturation of neurospheres into neuronal cells that exhibited characteristics comparable to those maturing in normal neurogenic culture conditions. In this study, HG downregulated glucose transporter expression and glucose uptake during neurosphere formation but not neuronal maturation [19]. In contrast, Cheng et al. demonstrated that when HG-pretreated ND-ASCs and DMT2-ASCs were cultured in an appropriate induction medium, they exhibited significantly enhanced neurogenic differentiation compared to that of LG–pretreated counterparts. Neurogenic differentiation was determined by increased expression of the neurogenic markers nestin and microtubule-associated protein 2 (MAP2). These findings were compatible with the upregulation of stemness markers in HG-treated normal ASCs, indicating that they were reprogrammed to induce ground state pluripotent stem cells with enhanced plasticity [62]. Some discrepancies in the results of the two studies may be attributed to differences in induction protocols and MSC sources and necessitate further investigation.
Angiogenic Potential
Diabetes did not seem to affect the potential of ASCs to acquire endothelial traits after culture in endothelial differentiation medium [46, 50]. The expression of the endothelial-specific marker CD31 and formation of vessel-like network upon seeding on Matrigel were not altered in D- vs ND- ASCs [46]. Compared to ND-counterparts, MSCs from diabetic patients exhibited similar expression levels of proangiogenic factors, including VEGF [48, 59], HGF [48, 59], MCP-1, and stromal derived factor-1α (SDF-1α) [59]. In the ex vivo diabetic wound microenvironment (hypoxia and hyperglycemia), VEGF secretion by ASCs was not altered, while the release of keratinocyte growth factor (KGF) was significantly depleted [63]. A recent study showed that ASCs were more resistant to oxidative stress-induced senescence and hypoxia-induced apoptosis. Furthermore, ASCs possess higher angiogenic potential than BMSCs [119]. Taken together, these data may favor AT as a promising source for autologous cell-based therapy for ischemic diabetic wounds.
Weil et al. reported that culture of human BMSCs in HG conditions had no effect on proangiogenic factor secretion, even in the presence of a stressor such as hypoxia or inflammation. BMSCs were shown to maintain the functionality of the JAK2/STAT3 and P38 MAPK signaling pathways [73], which are involved in MSC growth factor production [120, 121]. In another study, long-term (7-day) culture of hASCs in HG culture medium did not affect their pericystic function to support vascular network formation, suggesting that ASCs are resistant to glucose toxicity [83].
Other studies, however, reported that DM induced differences in some angiogenic functions of hMSCs. Gu et al. showed that DM profoundly impaired the potential of ASCs to promote endothelial cell proliferation in response to a hypoxic stimulus. In addition, VEGF transcript and secreted protein levels were significantly lower in diabetic ASCs than in control cultures under normoxic and hypoxic conditions. However, hypoxia was sufficient to significantly upregulate VEGF expression in both ASC types. Injecting control or diabetic ASCs in a model of flap ischemia similarly induced neovascularization and improved the flap survival. These results were attributed to the potential of diabetic ASCs to secrete HGF at high levels under normoxic and hypoxic conditions. These data indicate that although diabetic ASCs were impaired in their ability to promote angiogenesis in vitro, this potential may be improved under ischemic conditions in vivo. The authors thus proposed using ASCs to treat ischemic lesions in diabetic patients [47].
Policha et al. reported that DM delayed the acquisition of endothelial-specific markers after culture of ASCs in a specific endothelial differentiation medium. This was due to inhibition of PI3K signaling [55], a crucial pathway in endothelial differentiation and angiogenesis of human ASCs [122, 123]. Policha et al. also investigated the potential of diabetic ASCs to form durable tissue-engineered vascular grafts. Both diabetic and control ASCs were differentiated into endothelial-like-cells, seeded on a vascular scaffold and exposed to shear force linear flow conditioning. Both cell populations showed comparable potential for proliferation and retention on the vascular scaffold. Showing that DM has no deleterious effect on ASCs led the authors to propose ASCs as an endothelial cell substitute in vascular tissue engineering for the treatment of diabetic patients with microvascular diseases [55].
In another report, DMT2 compromised the vessel-like structure formation potential of cardiac auricle-derived MSCs cultured in endothelial differentiation medium and seeded on Matrigel [56]. The coexistence of DMT2 and CAD was found to significantly compromise the ability of ASC-conditioned medium (CM) to stimulate capillary-like formation by endothelial cells seeded on Matrigel [52]. The expression of pro-angiogenic factors such as HGF and platelet-derived growth factor (PLGF), as well as that of the anti-angiogenic mediators thrombospondin-1 and plasminogen activator inhibitor 1 (PAI-1), was found to be higher in the CM of diabetic cultures than in the control. Importantly, neutralizing PAI-1 in the CM was found to partially restore the tube-like-formation potential of diabetic ASCs. The authors deduced that the imbalance between the level of pro-and anti-angiogenic mediators was in favor of angiogenesis inhibition. This imbalance mediated the observed impairment in angiogenic activity of ASCs from patients with chronic pathologies. The use of allogenic ASCs from young healthy donors for cell therapy in patients with cardiovascular and metabolic diseases was recommended, taking into consideration the immunological issues associated with allogeneic transplantation [52].
A vascular complication of GDM is hypervascularization, which is a feature of diabetic extraembryonic tissues as a result of hyperinsulinemia and hyperglycemia [124]. Wajid et al. reported that GDM promoted the angiogenic activity of Wharton’s jelly-derived MSCs (WJMSCs) as presented by elevated expression of VEGFA protein [69]. In contrast, GDM- placenta-derived MSCs exhibited a decrease in tube formation ability and a significant downregulation in the expression of bFGF and VEGF [71].
Culture of hMSCs in HG conditions was found to impair the angiogenic activity of hMSCs and downregulate the expression of the proangiogenic stem cell factor (SCF) through upregulated expression of miR-34c [81]. Kang et al. [81] determined that downregulated expression of SCF, not upregulated miR-34c expression, increased the anti-angiogenic mediator Kruppel-like factor-4 (KLF-4) [125] and its downstream effector PAI-1 [126]. The authors thus suggested that HG-induced miR-34c expression attenuated the angiogenic activity of MSCs via dysregulating SCF/KLF-4/PAI-1 signaling. In a step closer to the in vivo scenario, Rezabakhsh et al. incubated CD133+-enriched human BMSCs with normal and diabetic serum for 7 days and evaluated their potential to form tube-like structures when seeded on Matrigel. The data showed that diabetes impaired the tubulogenic potential of BMSCs. This impairment was associated with aberrant autophagic status inside the cells and overexpression of the factor P62 at both transcriptome and protein levels [86]. Autophagy is a self-degradative process that plays a housekeeping role in the quality control of macromolecules and organelles [127]. It is a survival mechanism that senses cell metabolism and redox status [127, 128]. Activation of autophagy was reported to induce the angiogenic capacity of MSCs [129]. However, the accumulation of the autophagic factor P62 was correlated with inhibited autophagy and aberrant angiogenesis [130]. Using appropriate bioinformatics tools, Rezabakhsh et al. showed that interleukin-1 β (IL-1β)-induced expression in DM might cause bulk production of P62, which in turn aberrantly affects autophagy and angiogenesis [86]. Others reported that DMT2 sera-treated MSCs exhibited reduced secreted protein levels of VEGF [87], Ang-1 and Ang-2 [88]. They also exhibited abnormal physical interaction with endothelial cells and limited endothelial and pericyte differentiation potential [88]. Although diabetes impairs MSC intrinsic function, these cells may still have angiogenic potential [47]. Transplantation of autologous ASCs in the diabetic foot of three CLI patients resulted in significant improvement in ischemia symptoms [48].
Fibrinolytic/Anti-Thrombotic Potential
A clinical trial (ClincalTrials.gov identifier: NCT01257776) was conducted to evaluate the feasibility and safety of autologous ASCs treatment of diabetic patients with critical limb ischemia (CLI). Two diabetic patients developed distal microthrombosis, raising the possibility that the diabetic milieu might alter the well-known anti-thrombotic properties of MSCs [131]. This was evident in a study by Acosta et al., which showed altered expression of two fibrinolytic determinants in diabetic ASCs from patients with CLI. Compared to non-diabetic counterparts, from subjects with or without CLI, ACSs from diabetic patients promoted thrombosis [49]. These factors included tissue plasminogen activator (tPA), fibrinolysis promoting factor and its inhibitor (tPAI) [132]. The study assessed also the anti-fibrosis potential of D- and ND- ASCs, embedded in fibrin clots. The cells were cultured in the presence or absence of diabetic serum, and the level of formed D-dimer (byproduct of fibrin degradation) was then determined [49]. Both D-ASCs, and ND-ASCs cultured in diabetic serum, exhibited compromised potential to degrade the fibrin gel. These data indicated that the diabetic milieu adversely affected the fibrinolysis potential of ASCs and this altered potency was not reverted by normal culture conditions. The authors recommended the need to include safety tests, as D-dimer quantity and/or tPA-to-PAI-1 ratio to assess the clinical applicability of autologous ASC product in the inflammatory disease [49].
Ex vivo-expanded human MSCs were reported to induce instant blood-mediated inflammatory reaction (IBMIR) both in vitro and in vivo [133]. IBMIR is characterized by complement/coagulation cascade activation, platelet consumption and rapid lysis of cells by innate immune system [133]. Recently, Davies et al. assessed the blood compatibility of BMSCs derived from early and lately diagnosed DMT1 patients. The surface expression of three complement inhibitors; CD46, CD55 and CD59 were analyzed from healthy, EDMT1 and LDMT1-BMSCs. Similar clot formation and comparable levels of complement activation products were detected in all groups. While both healthy and DMT1 MSC groups expressed CD46, CD59 was significantly downregulated in the diabetic groups. The expression of CD55 was also significantly elevated in LDMT1 BMSCs, leading to the conclusion that LDMT1-BMSCs demonstrated favorable blood compatibility. This conclusion was confirmed by the lower platelet consumption and thrombin formation in the same group [60].
Migration and Homing Potential
Diabetes can induce mobilopathy, a phenomenon characterized by retention of stem/progenitor cells in the bone marrow, and contributing to development of secondary complications [42]. The molecular mechanism underlying this mal-mobilization is thought to involve altered dipeptidyl peptidase-4/stromal derived factor-1 alpha (DPP-4/SDF-1α) axis [134]. This axis is essential to establish chemotactic SDF-1α gradient towards the peripheral blood by degrading bone marrow SDF-1α. This is mediated by the protease activity of DPP-4, and ultimately favors the migration of bone marrow stem cells to the site of injury [42]. Limited data is available on the engraftment capacity of diabetic MSCs ex vivo [54, 60, 61, 64].
MSC homing is mediated by chemokine-related genes, such as C-X-C chemokine receptor type 4 (CXCR4) and C-X-C Motif Chemokine Ligand 12 (CXCL12)/SDF1. These chemockines were found to be downregulated in ASCs derived from diabetic CLI patients, when compared to non-diabetic CLI-free donors [135]. These data suggest possible impaired homing and recruitment for MSCs derived from diabetic adipose tissues of ischemic limbs. This source may thus be not suitable for auologus cell therapy [54].
In accordance with these data, Cheng et al. reported that HG-treated ASCs exhibited decreased cell migration in vitro. The migrated LG-treated group covered a significantly greater area than the HG-treated ASCs [62]. Two other recent studies showed that DMT2 sera blunted hMSC migration toward various chemotactic agents as VEGF and SDF-1α [86, 88]. This was attributed to distinct modulation of mir-1-3p and mir-15-5p in diabetic conditions, and consequent decrease in expression of VEGFR-2 and CXCR-4 receptors [88].
Whole genome microarray analysis for BMSCs derived from healthy and DMT1 patients, with early and late onsets, revealed limited genomic discrepancies in EDMT1-MSCs. LDMT1-BMSCs on the other hand have shown wider discrepancies compared to healthy counterparts. These data suggest that a disease memory state may exist in the late diabetic MSCs [60]. Wound healing response genes, including FOS and bone morphogenetic protein-2 (BMP-2) were significantly dysregulated in LDMT1-BMSCs. To determine whether these genotypic discrepancies between healthy and LDMT1- BMSCs were associated with different response to injury, in vitro migration assay was performed. Microscopic monitoring for the rate and extent of wound closure throughout 24 h period revealed no significant difference between the two MSC populations. In addition, the expression of dysregulated wound response genes was normalized in LDMT1-BMSCs 24 h post-scratching. These findings indicated that chronic diabetes had not altered wound healing function of MSCs. Delayed wound healing in diabetes was attributed to fibroblast dysfunction and/or impaired MSC-stromal crosstalk in diabetic tissues [60]. Two recent studies reported elevated basal migration and invasion capacities in DMT2-ASCs [64] and BMSCs of recently diagnosed DMT1 [61]. This was associated with increased expression of the invasion-related factors; matrix metalloproteinases-2 and -9. Compared to LG-treated cells, HG-treated bone marrow multipotent progenitors showed a similar migration response to the chemoattractant fetal bovine serum (FBS), but a significantly reduced expression of matrix protein genes (collagen 1, 3, 4 and fibronectin) [111].
Immunomodulatory Properties
Mancini et al. addressed the potential of ASCs from DMT2 patients without or with atherosclerosis (ATH) to suppress the proliferation of activated allogeneic CD4+ T cells. The compromised T cell anti-proliferative effect of ASCs observed in DMT2 was more profound in the presence of ATH [65]. In accordance with these data, Serena et al. showed that the immunosuppressive effect of ASCs was significantly altered by DMT2. Firstly, mRNA and protein of TGFβ, a crucial MSC immunomediator, was significantly reduced in DMT2-ASCs. In addition, diabetic ASCs showed a decreased potential to inhibit T and B cell proliferation and to activate the anti-inflammatory macrophage (M2) phenotype. This impaired immunosuppressive potential of DMT2-ASCs was attributed to inflammasome-mediated IL-1β secretion in these cells. Importantly, pretreatment of DMT2-ASCs with TGFβ and interleukin-1 receptor antagonist (IL-1RA) together restored their immunosuppressive properties [64]. de Lima et al. performed global transcriptome analysis to monitor the expression of immunoregulatory molecules, such as adhesion molecules, chemokines, and growth factors and their receptors, in BMSCs of early/newly diagnosed DMT1 (EDMT1) and controls [61]. Several adhesion molecules were found to be differentially expressed in T1D compared to control cells. Of these, vascular cell adhesion molecule-1 (VCAM-1), LAMA3, and ITGA7 were downregulated while SEMA4A was upregulated. VCAM-1 plays a central role in the immunosuppressive action of MSCs by contributing to adhesion of MSCs to activated T cells [136]. Accordingly, de Lima et al. proposed that this cell contact-dependent immunosuppressive action may be affected by DMT1 [61]. Some immunomodulatory chemokines, such as C-C Motif Chemokine Ligand 2 (CCL2) and CXCL12, were downregulated in BMSCs from diabetics. In silico functional gene analysis showed preferential enrichment of canonical pathways related to sympathetic hyperactivity, and upregulation of the β3-adrenergic receptor-encoding geneADRB3 [61]. This was associated with negative regulation of important hematopoietic stem cell maintenance factors such as CXCL12 and VCAM-1 [137]. These studies support proper characterization of MSC immunological and immunomodulatory properties for successful autologous therapy in diabetes.
Other studies however demonstrated that DMT1 had no deleterious effect on immunosuppressive properties of human MSCs [38, 60]. Similar to their healthy counterparts, EDMT1-BMSCs exerted anti-proliferative activity on allogeneic CD3+ T cells in a dose-dependent manner. Microarray analysis showed no significant difference in expression of immunomodulatory mediators such as PDL1, NOS2, LI-10, TGFβ, and PDL2 between the healthy and EDMT1-BMSCs. Similarly, other mediators such as HLA-G, TGS6, and factors involved in MSC licensing as IFNGR2, TNFR1, IFNGR1, TNFR2, TLR4 and TLR3 showed no significant difference [38]. Davies et al. demonstrated comparable immunomodulatory functions of EDMT1- and LDMT1-BMSCs, which were similar to normal healthy cells. DMT1-BMSCs suppressed the expression and function of CD25, and reduced the secretion of pro-inflammatory cytokines [60]. Treatment of MSCs with pro-inflammatory cytokines such as interferon gamma (IFNγ) and tumor necrosis factor (TNF) induced MSCs to acquire anti-inflammatory phenotype [138].
Davies et al. explored the secretion of a number of immunoregulatory cytokines and chemokines after stimulation of BMSCs with pro-inflammatory stimuli. At baseline, comparable levels of IL-6, PGE2, CXCL1, CXCL6 and IDO were reported in healthy and DMT1 MSC groups. Interestingly, HGF baseline was significantly lower in EDMT1-BMSCs compared with LDMT1-cells, but not in healthy counterparts. Different responses to inflammation were reported in the secretome of the three MSC types. Treatment of cells with IFNγ and TNF induced similarly significant upregulation in IDO activity and IL-6 secretion by all cell types. In response to priming, CXCL1 upregulated expression was significantly higher in the two DMT1 groups compared to control. However, CXCL6 was significantly higher in primed EDMT1-BMSCs compared with the other two groups. DMT1 thus seems to have no effect on the responsiveness of BMSCs to priming. Primed diabetic MSCs may exhibit a comparable or even increased ability to recruit immune cells compared to healthy counterparts [60].
Oxidative Stress and Inflammatory Status
Oxidative stress is dysregulated production and/or scavenging of reactive oxygen and nitrogen species. ROS are kept at nontoxic concentrations to maintain cell biology and functions by a variety of anti-oxidant mechanisms [139]. However, elevated ROS levels, as a result of stress, cause damage to lipid, proteins, DNA and results in cellular dysfunction and death [140]. It is well-established that hyperglycemia induces formation of advanced glycation end products (AGEs). AGEs are formed by reducing sugars nonenzymatically with proteins, and interact with specific receptors (RAGE) expressed on many cell types including MSCs [141]. AGEs-RAGE interaction activates pathways involved in ROS generation and inflammatory cytokine production [142].
Reportedly, oxidative stress negatively impacts MSC survival and function, limiting their clinical applications [137]. Few studies investigated the level of ROS generation by diabetic MSCs from different sources [50, 66, 70, 104]. Dentelli et al. reported that visceral DMT2-ASCs, both freshly recovered and CD31/CD45-depleted, generated higher levels of NADPH oxidase-dependent ROS than normal cells [50]. Consequently, increased levels of IL-6 and IL-8 production by DMT2-ASCs were reported. In another study, altered redox state was evident in the form of elevated mitochondrial-dependent generation of ROS in DMT2-ASCs [66]. However, quantification of secreted extracellular superoxide dismutase (SOD) showed similar activity of this crucial anti-oxidant enzyme in both diabetic and healthy ASCs.
Others reported increased malondialdehyde, a marker for lipid peroxidation, in GDM-WJMSCs [69]. Reduced MSC survival was observed due to reduced activities [69] or low levels [87] of anti-oxidant enzymes SOD, glutathione reductase (GSH) and catalase.
A recent study compared the inflammatory response of ASCs from subcutaneous (SAT) and visceral adipose tissue and (VAT), of age-matched lean, obese and DMT2 donors [64]. Both types of cells exhibited higher levels of inflammatory markers such as IL-1β, IL-6, TNF and MCP-1 compared to normal cells. Importantly, ASCs and mature adipocytes of DMT2 patients (from VAT and SAT) showed higher expression levels of IL-1β than their obese-derived counterparts. Given that inflammasome signaling mediates IL-1β secretion [143], protein expression of some inflammasome components were performed. The researchers investigated NLRP3, IL-1β and apoptosis-associated speck-like protein containing a CARD (ASC) in subcutaneous and visceral ASCs. The results showed that ASC were significantly higher in DMT2- subcutaneous ASCs than lean or even obese counterparts, while NLRP3 and IL-1β levels were not changed. However, NLRP3, IL-1β, and ASC protein levels were significantly higher in DMT2-visceral ASCs than in lean ones Interestingly, NLRP3 showed also a higher protein level in visceral DMT2-ASCs. It was concluded that the inflammasome-mediated inflammatory response activation in DMT2-ASCs derived from visceral AT is dependent on body mass index as well as insulin resistance [64]. Another study reported that culture of human periodontal ligament stem cells in HG conditions activated NF-Kβ pathway, the major inflammation signaling pathway [144]. This in turn enhanced IL-6 and IL-8 expression [80].
Metabolic Activity and Insulin Sensitivity
Limited reports investigated the metabolic activity of diabetic MSCs [56, 64]. The metabolic profile including glycolysis, mitochondrial respiration and ATP content was investigated in ND- and DMT2- cMSCs [56]. To measure mitochondrial respiration capacity, oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) were detected. No significant differences were reported between both cell populations regarding glycolysis and mitochondrial respiration under basal and stress conditions. However, ATP content was higher in D-cMSCs [56]. Increased ATP level was associated with insulin resistance and predisposition to DMT2 in obese patients [145]. Defective oxidative phosphorylation and altered respiratory capacity in mitochondria of GDM-UC-MSCs compared to ND-UC cells was reported. These mitochondrial dysfunctions were suggested to be associated with insulin resistance [70].
Recently, Serena et al. investigated the metabolic gene expression profile of both subcutaneous and visceral ASCs derived from lean, obese and DMT2 donors. Both visceral and subcutaneous ASCs from obese and DMT2 donors exhibited glycolytic phenotype. Another study by Moon et al. also reported that glycolysis stimulated the immune responses, and was associated with NLRP3 inflammasome activation. Similarly, significant upregulation of gene expression of glycolytic factors including hexokinase (HK), phosphofructokinase (PFKM), and lactate dehydrogenase B (LDHB) was reported in obese and DMT2-ASCs. This increased metabolic activity was attributed to the continuous need of these cells to ATP to maintain their proliferative, migratory, invasive and inflammatory activities [64].
When investigating the effect of HG on glucose metabolism and bioenergetics of ASCs, Hajmouse et al. reported a significant decline in glucose uptake by HG compared to LG-ASCs. Bioenergetics studies revealed that mitochondria in HG-treated ASCs displayed similar basal respiration to LG-ASCs, although with lower maximal respiratory capacity. HG-treated ASCs similarly exhibited diminished glycolysis that was not reversed by insulin stimulation [83].
Molecular studies were performed to determine the changes induced by diabetes or in ASCs and how they may impair their regenerative properties [45]. The Adipo/AdipoR1/AdipoR2/APPL1 axis was found to be significantly downregulated in HG-treated ASCs and D-ASCs [45]. Adiponectin (Adipo) is an adipokine that acts as insulin-sensitizer in insulin target tissues, to promote insulin action and ameliorate insulin resistance [146]. It also displays anti-inflammatory activities via promoting macrophage M2 phenotype [147]. Upon binding to its receptors, (AdipoR1 and AdipoR2), Adipo activates APPL1, which mediates metabolic energy regulation and insulin signaling [146]. This may explain the finding that HG-treated ASCs and D-ASCs were less prone to insulin recovery, by being less prone to insulin signaling, at least partially due to DM-related downregulation in the Adipo/AdipoR1/AdipoR2/APPL1 axis. Moreover, transcriptome analysis in the same study also revealed 28 genes that were differentially expressed in ND compared to DMT2-ASCs. Those included gene clusters associated with insulin resistance (GDP1, CEACAM1, IL-10, IL12 and IL-6), and those associated with glucose metabolism (GCG, GCK, INSR, FBP1, CEBPA and IGFBP5). HG treatment of ND- and DMT2-ASCs resulted in further changes in the regulation of genes linked to insulin resistance. The changes in IFNG, TNF, resistin, PPARG family genes and ADRB3 CEBP were more pronounced in HG-treated DMT2-ASCs. Importantly, insulin treatment uregulated some insulin resistance and glucose metabolism genes more profoundly in HG-treated ND- than DMT2-ASCs. This may indicate that DMT2-induced gene alterations were most likely irreversible, and associated with permanent ASC dysfunction [45]. Elevated global DNA methylation in DMT2- ASCs [66], and also in cardiac MSCs [67], was associated with increased risk of insulin resistance [148]. Similarly, compared to normal placenta (P)-MSCs, GDM-P-MSCs were proposed to be likely insulin-resistant. This was evident by decreased glucose consumption, compromised glucose uptake and reduced glycogen storage [71].
β-Cell Regenerative Potential
Few studies reported that human MSCs from diabetic patients could differentiate into cells of pancreatic endocrine phenotype in vitro [43, 44, 53, 89, 149]. Sun et al. provided evidence that the β-cell differentiation capacity of BMSCs in diabetic patients was intact. In this study, MSCs harvested from bone marrow samples of DMT1 and DMT2 patients were induced to differentiate into insulin-producing cells (IPCs). The three-stage differentiation protocol included activin A, among other stimulants, as key β-cell differentiating agent. Generation of IPCs was confirmed by the gene expression of typical β-cell markers as PDX-1 and insulin. Importantly, these IPCs secreted insulin in response to glucose stimulation in vitro [43]. Phadnis et al. demonstrated that unlike healthy cells, DMT2-BMSCs were able to differentiate rapidly into islet-like-aggregates expressing endocrine hormones including insulin, glucagon and somatostatin. This differentiation was demonstrated upon culture in a HG serum-free medium supplemented with fetal pancreatic extract. It is noteworthy that transcriptome studies revealed that undifferentiated DMT2-BMSCs, not the healthy ones, expressed pancreatic progenitor markers, such as ISL-1, PAX6, NKX6.1, and PAX4. These findings supported the potential use of initially expanded D-BMSCs as pancreatic progenitors that can be easily differentiated into functional endocrine pancreatic lineage [44]. Thakkar et al. reported successful differentiation of ASCs cultured in a high glucose medium, containing growth factors and supplement with nicotinamide, Activin A, exendin, pentagastrin and HGF. ASCs from DMT1 patients successfully generated glucose-responsive, insulin-secreting cells expressing insulin,-specific markers PAX-6, PDX-1 and ISL-1 [89]. Gabr et al. also demonstrated that DMT2-BMSCs were successfully differentiated in vitro into islet clusters using a glucose-rich medium supplemented with B27, betacellulin, Activin A and nicotinamide. Insulin secretion profile of diabetic MSCs was significantly higher than their non-diabetic counterparts [53]. Unique factors in the diabetic microenvironment may have contributed to these differences [12]. Importantly, while islet transplantation under the kidney capsule of diabetic animals, restored normoglycemia, undifferentiated MSCs did not. However, in another study, administration of undifferentiated DMT1-MSCs reversed hyperglycemia and prevented disease progression in streptozotocin (STZ)-induced diabetes [38]. In that study, BMSCs from healthy and recently diagnosed DMT1 donors were directly injected in the spleen of diabetic mice in the chronic phase of the disease. Both MSC populations equally reversed hyperglycemia, increased β-cell mass and insulin production and induced glucose tolerance in 67% of treated mice. The mechanisms underlying the MSC beneficial effect in these mice was determined to be via decreasing the production of pro-inflammatory cytokines in the pancreatic tissues leading to constraining pancreatic inflammation/insulitis, preventing β-cell death and promoting β- cell regeneration. However, it did not affect the frequency of CD4+CD25+Foxp3+ Treg cells in spleens and pancreatic lymph nodes. Conclusively, MSCs from recently diagnosed DMT1 did not present β-cell reparative functional abnormalities, supporting the use of autologous MSCs in the treatment of DMT1 patients [38, 90].
Despite these promising experimental results, gene expression studies revealed DM-related gene alterations, which may suggest attenuated β-cell regenerative potential of MSCs. Examples of these alterations included significant downregulation of HGF in EDMT1-MSCs [38, 60, 61]. HGF is a pleiotropic cytokine that signals through the tyrosine kinase transmembrane receptor c-Met [150]. The HGF/c-Met signaling pathway is important for β-cell protection and proliferation in metabolic stress conditions [151]. Similarly, epidermal growth factor receptor (EGFR) and fibroblast growth factor receptor (FGFR) genes were downregulated in EDMT1-MSCs [61], suggesting loss of stemness, cell growth and tissue repair ability of MSCs [152, 153]. Recently, Rezaie et al. reported that CM from diabetic hMSCs induced lipid accumulation in intracellular spaces and decreased insulin secreting potential of β-cells. These findings show that DMT2 might attenuate the β-cell restorative ability of hMSCs [88]. These data suggest the need for larger scale preclinical studies to determine the wide-ranging factors that may influence the efficacy of diabetic MSC-based therapy in DM.
Clinical Studies
Few investigators applied autologous MSCs to treat DMT1 [89, 90] or DMT2 patients [91, 92] (Table. 3). Thakkar et al. compared the efficacy of infusion of autologous or allogeneic insulin-secreting adipose-derived mesenchymal stromal cells (IS-ASCs) in DMT1 management. In this study, IS-ASCs were co-administered with bone marrow-derived hematopoietic stem cell (BM-HSC) in portal and thymic circulation, and in subcutaneous tissue. The first group received autologous 2.65 ± 0.8 X 104 ISCs/kg body wt. along with CD34+ and CD45−/90+/73+ cells, while, the second group was administered allogenic2.07 ± 0.67 X 104 ISCs/kg body wt, along with CD34+ and CD45−/90+/73+ cells. Sustained improvement in fasting and post-prandial blood sugar, glycated hemoglobin (HbA1c) and serum C-peptide were achieved in both groups. A decrease in mean glutamic acid decarboxylase (GAD) antibodies and insulin doses were observed in recipients of both stem cell groups over the follow-up period. Serum C-peptide was better improved in the recipients of the autologous stem cells compared to the allogeneic transplant. Diabetes control was also better in the first group, where HbA1c was reduced from 10.99% at baseline to 7.75 ± 1.05, compared to 11.93 to 8.01 ± 1.04 in the second group. The study concluded that co-infusion of autologous IS-ASCs along with BM-HSCs offered a favorable long-term control of hyperglycemia compared with the allogeneic transplant [89].
Carlsson et al. investigated the therapeutic effect of in vitro expanded autologous BMSCs on newly diagnosed DMT1 patients. In comparison to insulin treatment alone, intravenous administration of autologous BMSCs within 3 weeks of DMT1 diagnosis was found to preserve or even improve C-peptide response for one-year follow up. No significant differences however were observed between insulin-treated and MSC-treated patients in levels of HbA1c, fasting C-peptide, insulin doses and frequency of GAD 65 or islet antigen 2 (IA2) antibodies. Autologous MSC transplantation thus offered a promising and safe approach to intervene in DMT1 progression and preserve residual β-cell function [90].
Dang et al. evaluated the safety and therapeutic effect of transplantation of in vitro expanded autologous ASCs for DMT2. ASCs were transfused at a dose of 1 × 106 cells/kg body weight, and patients evaluated for fever and blood glucose level (BGL) every 2 weeks. No adverse reactions were detected and decreased BGL was recorded suggesting the potential of autologous expanded ASC transfusion to manage DMT2 [91]. Recently, Bhansali et al. compared the efficacy and safety of administering autologous BMSC compared to bone marrow mononuclear cell (BM-MNC) in DMT2. Over one-year follow up, both autologous BMSCs and BM-MNCs resulted in significant reduction in exogenous insulin requirement by ≥50%, while maintaining HbA1c <7.0% (<53.0 mmol/mol) in almost 60% of the patients. This was accompanied by augmented C-peptide response in the MNCs group and improved insulin sensitivity in MSCs group. Gene expression analysis showed enhanced expression of insulin receptor substrate-1 (IRS-1) in the MSC-treated patients. These data suggested that insulin sensitivity most likely improved through an IRS-1-dependent mechanism. It is noteworthy that no adverse events were noted. Despite the small sample size and short duration of follow-up, the authors recommend combined autologous BMSCs and BM-MNCs for better control of DMT2 [92].
A recent meta-analysis demonstrated that autologous stem cell transplantation can be a safe and effective approach for treatment of DM patients, although with some limitations [13]. The study reported the paucity of the available trials on autologous MSC therapy for DM. Larger sample size, the number of cells infused, route of infusion, and the type of stem cells were all reported as inconsistent and limiting factors in determining the best outcome. Longer follow-up time, conventional therapies-treated and placebo controls, standard follow-up measures and metabolic studies to ensure the efficacy and safety are also needed.
Strategies to Improve the Efficacy and Function of Diabetic MSCs
Strategies to improve the therapeutic efficacy of MSCs from diabetic patients for treatment of diabetes included preconditioning strategies and genetic manipulation strategies.
Preconditioning of MSCs
Insulin pretreatment of DMT2-ASCs was found to improve cell survival and proliferation [45]. FGF has been suggested as a potential therapeutic agent for improving stem cell-based approaches for the treatment of diabetes mellitus and its complications [66]. Conditioning of DMT2-ASCs with bFGF reversed the detrimental effects of DM on MSC viability and proliferation. Importantly, stimulation with bFGF at a concentration of 5 ng/ml markedly enhanced GLUT-4 gene and protein expression and reduced the global DNA methylation in DMT2-ASCs. These findings were associated with insulin sensitizing effect of bFGF. In addition, bFGF treatment attenuated intracellular ROS level in diabetic ASCs [66]. Insulin and bFGF were proposed to act via activation of PI3K/AKT pathway [153, 154], which contributed to maintaining MSC stemness and proliferation [155]. Recently, Guo et al. proposed that exendin-4 treatment could improve the proliferation of human PDLSCs under HG conditions [104]. Platelet lysate supplementation of cultured media improved the expansion potential of diabetic BMSC cultures, derived from ischemic amputated limbs [59]. Prior to transplantation, MSCs could be treated with heme oxygenase (HO-1) inducer to decrease the levels of superoxide anion and inflammatory factors [156]. This treatment might contribute to ameliorating oxidative stress and improving survival and functions of diabetic MSCs. However designing HO-1-inducing compounds with clinical applicability is still needed [156].
Some preconditioning compounds were introduced to counteract the deleterious effect of DM or HG on osteogenic differentiation of MSCs. These include hespertin, a polyphenolic compound that acts as ROS scavenger with osteoinductive activity [77], and silbinin, a medicinal plant extract with anti-oxidative and bone-remodeling activities [79, 157]. Insulin [45], and 5-aza-2-deoxycytidine (5-aza-dC), a DNA methyltransferase inhibitor were used to decrease the elevated DNA methylation induced by HG [78]. Exendin-4, a glucagon-like peptide-1 with radical scavenging activity [104], and a specific inhibitor to the NF-Kβ pathway [80], are other applied ROS scavengers.
Glucose reduction in the culture medium was found to increase MSC proliferation and osteogenesis, and to decrease MSC senescence and adipogenesis [158]. This effect was associated with reduced anaerobic glycolysis and shift in ATP production from glycolysis to mitochondrial oxidative phosphorylation. Elevated expression of anti-oxidant defense enzymes such as MnSOD and catalase was also documented. This might indicate cell ability to counteract the undesirable levels of ROS, produced as a consequence of increased aerobic respiration [158].
Critical preconditioning by short-term exposure to oxygen, and serum and glucose deprivation were able to enhance the angiogenic secretome and therapeutic potential of apical papilla-derived MSCs [159]. Furthermore, hypoxia preconditioning provided a protective shelter for transplanted MSCs from apoptosis. This effect was mediated via hypoxia-inducible factor-1 alpha (HIF-1α)-dependent pathway [160]. Apelin 13, a ligand for G protein coupled APJ receptor, provided protective effect for BMSCs from apoptosis by reducing ROS level via MAPK/ERK1/2 and PI3K/AKT signaling pathways [161]. Pre-treatment of MSCs by hypoxia and apelin 13 could thus provide a strategy to rescue cells transplanted in diabetic conditions [160] and maybe a conceivable regimen to potentiate autologous diabetic MSC-based therapy.
Recently, Fromer et al. employed an approach to improve hASC-based therapy in diabetic wounds, by priming them with CM of HG-treated human umbilical vein endothelial cells (HUVECs). Compared to unprimed counterparts, primed HG-treated hASCs exhibited increased proliferation, enhanced endothelial differentiation and tube formation, in addition to improved therapeutic effect. CM of HUVECs contained an array of angiogenic cytokines and growth factors including IL-8, VEGF-A, C and D, FGF-1, FGF-2 and HGF. The HUVEC secretome priming of ASCs could be used to overcome the deleterious effects of diabetes on angiogenic capacity of this cell population [84].
Treatment of MSCs with pro-inflammatory cytokines has been reported to induce MSCs to acquire an anti-inflammatory phenotype [138]. Davies et al. demonstrated that priming of DMT1-BMSCs with IFNγ and TNF potentiated their immunomodulatory properties and enhanced expression of immunoregulatory factors and chemokines. However, further studies are required to define the appropriate priming conditions required to achieve maximum therapeutic recovery of diabetic MSCs in experimental models [60].
Genetic Manipulation
Recently, it was demonstrated that modulating sirtuin expression and/or activity may be a potential method to reduce oxidative stress in MSCs [139]. Sirtuins (1–7) are protein deacetylases that play several roles in extension of lifespan and protection against metabolic diseases [162]. Few studies explored expression of sirtuins and their contribution to MSC biology and functions [66, 163, 164]. Additional studies are needed to investigate expression of sirtuins in MSCs in a diabetic microenvironment. Manipulation of theses sitruins, especially those known to regulate ROS generation as SIRT3 [165] and SIRT4 [166], could alleviate DM-induced oxidative stress and cell dysfunction.
MiR-486-5p and its target sirtuin1 (SIRT1) were found to regulate MSC replicative senescence under HG conditions [75]. Overexpression of HO-1 gene might promote the survival and angiogenic function of diabetic MSCs transplanted in diabetic microenvironment [156]. SIRT-1/Fra-1 axis was found to be downregulated in diabetic MSCs by miR-449 overexpression blunting its osteogenic differentiation [85]. Moreover, SCF/KLF-4 proangiogenic factors were downregulated in HG-treated MSCs and their expression could be enhanced by down regulation of miR-34c [81]. PAI-1, anti-angiogenic factor, acts through regulating endothelial cell migration by inhibiting urokinase plasminogen activator (uPA), which is a crucial angiogenesis promotor [167]. PAI-1 is one of the potential targets that can be manipulated in diabetic ASCs to potentiate their angiogenic and anti-thrombotic properties before autologous transplantation [49, 52]. Under ischemic conditions, upregulation of the anti-apoptotic factor Bcl-2 significantly enhanced the levels of angiogenic and mitogenic paracrine factors such as VEGF, HGF and bFGF ASCs [168]. However, overexpression of Bcl-2 under diabetic conditions (hypoxia and hyperglycemia) needs to be investigated.
Adiponectin (Adipo) is an adipokine that acts as insulin-sensitizer in insulin target tissues [146] and exerts anti-inflammatory activities [147]. Adiponectin was downregulated in insulin-resistant DMT2-ASCs [45], thus upregulating adiponectin level in these cells may improve their response to insulin and regulate energy metabolism. To improve engraftment and regenerative properties of diabetic MSCs, it is recommended to genetically modulate downexpressed growth factors and their receptors as well as chemokines receptors. Among those growth factors are HGF [38, 60, 61], FGF3 [61], growth factor receptors are EGFR and FGFR [61], and chemoattractant receptors, VEGFR-2 and CXCR-4. Expression of the latter gene set could also be manipulated by regulating mir-1-3p and mir-15-5p levels [88].
Concluding Remarks and Future Perspectives
MSCs are a promising cell therapy approach to treat DM due to their regenerative and immunomodulatory properties. Despite their ability to escape immune recognition, autologous MSC transplantation was found to be more favorable than allogeneic transplantation in some cases. This is especially important to avoid immune-suppressive regimens that are difficult for already compromised diabetic patients to tolerate. Many studies have shown that DM and its associated hyperglycemia may induce MSC apoptosis and premature senescence and diminish clonogenicity, cell proliferation and osteogenic differentiation capacity. To optimize the use of MSCs for transplantation, the early passages of expanded MSCs are thus recommended for clinical purposes. MSCs may be treated with anti-oxidative and/or growth-stimulating agents to augment their therapeutic potential.
Several studies have shown inconclusive data on the compromised and abnormal functions of MSCs after prolonged exposure to the diabetic microenvironment. Among the altered functions were migration and engraftment abilities, anti-thrombotic potential, angiogenesis supportive effect and immunomodulatory properties. The available studies, however, have not uniformly shown that altered functions do indeed interfere with the therapeutic outcome of stem cells.
Other studies, however, demonstrated that diabetic MSCs displayed compromised functions and metabolic pathways. For example, enhanced oxidative stress, increased pro-inflammatory markers, altered signaling pathways, especially the PI3K/AKT pathway, and disturbed mitochondrial integrity and functions were all documented. These altered functions may contribute to the reduced efficacy of the transplanted cells. Unfortunately, very limited data are available to demonstrate the functionality of hMSCs from recently diagnosed DMT1 patients to regenerate β-cells or restore normoglycemia in diabetic animal models. Clinical trials have demonstrated more promising outcomes. Autologous MSC transplantation in diabetic patients improved blood sugar and C-peptide levels and decreased HbA1c. Importantly, MSC administration improved hyperglycemia in response to glucose challenge and reduced the required daily insulin doses. The current knowledge on how DM impacts the biology and functions of MSCs lack standardization. Clinical parameters such as the patient’s age, disease duration, level of glycated hemoglobin, BMI value and presence of comorbidities or other therapies are widely variable in clinical trials. MSC-related issues, including cell source, isolation methods and culture conditions, as well as experimental designs and analysis techniques, are not unified. Standardization of protocols that involve injection of naive or differentiated stem cells, optimum doses, site of injections and preconditioning regimens would accelerate effective clinical applications. Other factors that need consideration include the need for repeated injections, survival of the cells, homing and engraftment duration, and the need for immune suppression.
More uniform experimental and preclinical studies are also required to understand the molecular basis and signaling molecules that regulate MSC function under diabetic conditions. Studies to elucidate the mechanisms regulating energy metabolism in MSCs in diabetic conditions are urgently required. Additionally, studies that identify the mechanisms underlying DM-related decline in mitochondrial respiratory capacity, ROS generation and the anti-oxidative capacity of MSCs will be beneficial. Specific assays, such as D-dimer quantity and/or tPA-to-PAI-1 ratio, to predict the safety and potency of autologous MSCs in DM should be available. Data from these studies would facilitate accurate evaluation of the efficacy of the treatment and more precise inclusion and exclusion criteria to properly select diabetic patient groups that would best benefit from the treatment.
References
Scully, T. (2012). Diabetes in numbers. Nature, 485(7398), S2–S3.
Berezin, A. E. (2017). New trends in stem cell transplantation in diabetes mellitus type I and type II. In P. Pham (Ed.), Pancreas, kidney and skin regeneration (pp. 73–88). Cham: Springer.
Forbes, J. M., & Cooper, M. E. (2013). Mechanisms of diabetic complications. Physiological Reviews, 93(1), 137–188.
Cho, N. H., Shaw, J. E., Karuranga, S., Huang, Y., da Rocha Fernandes, J. D., Ohlrogge, A. W., & Malanda, B. (2018). IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Research and Clinical Practice, 138, 271–281.
Atkinson, M. A. (2012). The pathogenesis and natural history of type 1 diabetes. Cold Spring Harbor Perspectives in Medicine, 2(11).
Alicka, M., & Marycz, K. (2018). The effect of chronic inflammation and oxidative and endoplasmic reticulum stress in the course of metabolic syndrome and its therapy. Stem Cells International, 2018, 4274361–4274313. https://doi.org/10.1155/2018/4274361.
Donath, M. Y., & Shoelson, S. E. (2011). Type 2 diabetes as an inflammatory disease. Nature Reviews. Immunology, 11(2), 98–107.
Chiefari, E., Arcidiacono, B., Foti, D., & Brunetti, A. (2017). Gestational diabetes mellitus: An updated overview. Journal of Endocrinological Investigation, 40(9), 899–909.
Fanelli, C. G., Porcellati, F., Pampanelli, S., & Bolli, G. B. (2004). Insulin therapy and hypoglycaemia: The size of the problem. Diabetes/Metabolism Research and Reviews, 20(Suppl 2), S32–S42.
Cefalu, W. T. (2012). American diabetes association-European association for the study of diabetes position statement: Due diligence was conducted. Diabetes Care, 35(6), 1201–1203.
Health Quality, O. (2015). Pancreas islet transplantation for patients with type 1 diabetes mellitus: A clinical evidence review. Ont Health Technol Assess Ser, 15(16), 1–84.
El-Badri, N., & Ghoneim, M. A. (2013). Mesenchymal stem cell therapy in diabetes mellitus: Progress and challenges. Journal of Nucleic Acids, 2013, 194858–194857. https://doi.org/10.1155/2013/194858.
El-Badawy, A., & El-Badri, N. (2016). Clinical efficacy of stem cell therapy for diabetes mellitus: A meta-analysis. PLoS One, 11(4), e0151938.
Pittenger, M. F., Mackay, A. M., Beck, S. C., Jaiswal, R. K., Douglas, R., Mosca, J. D., Moorman, M. A., Simonetti, D. W., Craig, S., & Marshak, D. R. (1999). Multilineage potential of adult human mesenchymal stem cells. Science, 284(5411), 143–147.
Zuk, P. A., Zhu, M., Ashjian, P., de Ugarte, D. A., Huang, J. I., Mizuno, H., Alfonso, Z. C., Fraser, J. K., Benhaim, P., & Hedrick, M. H. (2002). Human adipose tissue is a source of multipotent stem cells. Molecular Biology of the Cell, 13(12), 4279–4295.
Romanov, Y. A., Svintsitskaya, V. A., & Smirnov, V. N. (2003). Searching for alternative sources of postnatal human mesenchymal stem cells: Candidate MSC-like cells from umbilical cord. Stem Cells, 21(1), 105–110.
Bieback, K., Kern, S., Kluter, H., & Eichler, H. (2004). Critical parameters for the isolation of mesenchymal stem cells from umbilical cord blood. Stem Cells, 22(4), 625–634.
Gronthos, S., Mankani, M., Brahim, J., Robey, P. G., & Shi, S. (2000). Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proceedings of the National Academy of Sciences of the United States of America, 97(25), 13625–13630.
Sawangmake, C., Pavasant, P., Chansiripornchai, P., & Osathanon, T. (2014). High glucose condition suppresses neurosphere formation by human periodontal ligament-derived mesenchymal stem cells. Journal of Cellular Biochemistry, 115(5), 928–939.
Krampera, M., Franchini, M., Pizzolo, G., & Aprili, G. (2007). Mesenchymal stem cells: From biology to clinical use. Blood Transfusion, 5(3), 120–129.
Rohban, R., & Pieber, T. R. (2017). Mesenchymal stem and progenitor cells in regeneration: Tissue specificity and regenerative potential. Stem Cells International, 2017, 5173732.
Chandra, V., Swetha, G., Muthyala, S., et al. (2011). Islet-like cell aggregates generated from human adipose tissue derived stem cells ameliorate experimental diabetes in mice. PLoS One, 6(6), e20615.
Kim, S. J., Choi, Y. S., Ko, E. S., Lim, S. M., Lee, C. W., & Kim, D. I. (2012). Glucose-stimulated insulin secretion of various mesenchymal stem cells after insulin-producing cell differentiation. Journal of Bioscience and Bioengineering, 113(6), 771–777.
Ho, J. H., Tseng, T. C., Ma, W. H., Ong, W. K., Chen, Y. F., Chen, M. H., Lin, M. W., Hong, C. Y., & Lee, O. K. (2012). Multiple intravenous transplantations of mesenchymal stem cells effectively restore long-term blood glucose homeostasis by hepatic engraftment and beta-cell differentiation in streptozocin-induced diabetic mice. Cell Transplantation, 21(5), 997–1009.
Tsai, P. J., Wang, H. S., Lin, G. J., Chou, S. C., Chu, T. H., Chuan, W. T., Lu, Y. J., Weng, Y. J., Su, C. H., Hsieh, P. S., Sytwu, H. K., Lin, C. H., Chen, T. H., & Shyu, J. F. (2015). Undifferentiated Wharton's jelly mesenchymal stem cell transplantation induces insulin-producing cell differentiation and suppression of T-cell-mediated autoimmunity in nonobese diabetic mice. Cell Transplantation, 24(8), 1555–1570.
Hess, D., Li, L., Martin, M., Sakano, S., Hill, D., Strutt, B., Thyssen, S., Gray, D. A., & Bhatia, M. (2003). Bone marrow-derived stem cells initiate pancreatic regeneration. Nature Biotechnology, 21(7), 763–770.
Lee, R. H., Seo, M. J., Reger, R. L., Spees, J. L., Pulin, A. A., Olson, S. D., & Prockop, D. J. (2006). Multipotent stromal cells from human marrow home to and promote repair of pancreatic islets and renal glomeruli in diabetic NOD/scid mice. Proceedings of the National Academy of Sciences of the United States of America, 103(46), 17438–17443.
Ezquer, F. E., Ezquer, M. E., Parrau, D. B., Carpio, D., Yanez, A. J., & Conget, P. A. (2008). Systemic administration of multipotent mesenchymal stromal cells reverts hyperglycemia and prevents nephropathy in type 1 diabetic mice. Biology of Blood and Marrow Transplantation, 14(6), 631–640.
Bassi, E. J., Moraes-Vieira, P. M., Moreira-Sa, C. S., et al. (2012). Immune regulatory properties of allogeneic adipose-derived mesenchymal stem cells in the treatment of experimental autoimmune diabetes. Diabetes, 61(10), 2534–2545.
Ezquer, F., Ezquer, M., Contador, D., Ricca, M., Simon, V., & Conget, P. (2012). The antidiabetic effect of mesenchymal stem cells is unrelated to their transdifferentiation potential but to their capability to restore Th1/Th2 balance and to modify the pancreatic microenvironment. Stem Cells, 30(8), 1664–1674.
Si, Y., Zhao, Y., Hao, H., Liu, J., Guo, Y., Mu, Y., Shen, J., Cheng, Y., Fu, X., & Han, W. (2012). Infusion of mesenchymal stem cells ameliorates hyperglycemia in type 2 diabetic rats: Identification of a novel role in improving insulin sensitivity. Diabetes, 61(6), 1616–1625.
Kono, T. M., Sims, E. K., Moss, D. R., Yamamoto, W., Ahn, G., Diamond, J., Tong, X., Day, K. H., Territo, P. R., Hanenberg, H., Traktuev, D. O., March, K. L., & Evans-Molina, C. (2014). Human adipose-derived stromal/stem cells protect against STZ-induced hyperglycemia: Analysis of hASC-derived paracrine effectors. Stem Cells, 32(7), 1831–1842.
Xie, M., Hao, H. J., Cheng, Y., Xie, Z. Y., Yin, Y. Q., Zhang, Q., Gao, J. Q., Liu, H. Y., Mu, Y. M., & Han, W. D. (2017). Adipose-derived mesenchymal stem cells ameliorate hyperglycemia through regulating hepatic glucose metabolism in type 2 diabetic rats. Biochemical and Biophysical Research Communications, 483(1), 435–441.
Xie, Z., Hao, H., Tong, C., Cheng, Y., Liu, J., Pang, Y., Si, Y., Guo, Y., Zang, L., Mu, Y., & Han, W. (2016). Human umbilical cord-derived mesenchymal stem cells elicit macrophages into an anti-inflammatory phenotype to alleviate insulin resistance in type 2 diabetic rats. Stem Cells, 34(3), 627–639.
Caplan, A. I., & Dennis, J. E. (2006). Mesenchymal stem cells as trophic mediators. Journal of Cellular Biochemistry, 98(5), 1076–1084.
Watt, S. M., Gullo, F., van der Garde, M., Markeson, D., Camicia, R., Khoo, C. P., & Zwaginga, J. J. (2013). The angiogenic properties of mesenchymal stem/stromal cells and their therapeutic potential. British Medical Bulletin, 108, 25–53.
Khubutiya, M. S., Vagabov, A. V., Temnov, A. A., & Sklifas, A. N. (2014). Paracrine mechanisms of proliferative, anti-apoptotic and anti-inflammatory effects of mesenchymal stromal cells in models of acute organ injury. Cytotherapy, 16(5), 579–585.
Yaochite, J. N., de Lima, K. W., Caliari-Oliveira, et al. (2016). Multipotent mesenchymal stromal cells from patients with newly diagnosed type 1 diabetes mellitus exhibit preserved in vitro and in vivo immunomodulatory properties. Stem Cell Research & Therapy, 7, 14.
Klyushnenkova, E., Mosca, J. D., Zernetkina, V., Majumdar, M. K., Beggs, K. J., Simonetti, D. W., Deans, R. J., & McIntosh, K. R. (2005). T cell responses to allogeneic human mesenchymal stem cells: Immunogenicity, tolerance, and suppression. Journal of Biomedical Science, 12(1), 47–57.
Griffin, M. D., Ryan, A. E., Alagesan, S., Lohan, P., Treacy, O., & Ritter, T. (2013). Anti-donor immune responses elicited by allogeneic mesenchymal stem cells: What have we learned so far? Immunology and Cell Biology, 91(1), 40–51.
Nauta, A. J., Westerhuis, G., Kruisselbrink, A. B., Lurvink, E. G., Willemze, R., & Fibbe, W. E. (2006). Donor-derived mesenchymal stem cells are immunogenic in an allogeneic host and stimulate donor graft rejection in a nonmyeloablative setting. Blood, 108(6), 2114–2120.
van de Vyver, M. (2017). Intrinsic mesenchymal stem cell dysfunction in diabetes mellitus: Implications for autologous cell therapy. Stem Cells and Development, 26(14), 1042–1053.
Sun, Y., Chen, L., Hou, X. G., et al. (2007). Differentiation of bone marrow-derived mesenchymal stem cells from diabetic patients into insulin-producing cells in vitro. Chinese Medical Journal, 120(9), 771–776.
Phadnis, S. M., Ghaskadbi, S. M., Hardikar, A. A., & Bhonde, R. R. (2009). Mesenchymal stem cells derived from bone marrow of diabetic patients portrait unique markers influenced by the diabetic microenvironment. The Review of Diabetic Studies, 6(4), 260–270.
Cramer, C., Freisinger, E., Jones, R. K., Slakey, D. P., Dupin, C. L., Newsome, E. R., Alt, E. U., & Izadpanah, R. (2010). Persistent high glucose concentrations alter the regenerative potential of mesenchymal stem cells. Stem Cells and Development, 19(12), 1875–1884.
Harris, L. J., Zhang, P., Abdollahi, H., Tarola, N. A., DiMatteo, C., McIlhenny, S. E., Tulenko, T. N., & DiMuzio, P. J. (2010). Availability of adipose-derived stem cells in patients undergoing vascular surgical procedures. The Journal of Surgical Research, 163(2), e105–e112.
Gu, J. H., Lee, J. S., Kim, D. W., Yoon, E. S., & Dhong, E. S. (2012). Neovascular potential of adipose-derived stromal cells (ASCs) from diabetic patients. Wound Repair and Regeneration, 20(2), 243–252.
Lee, H. C., An, S. G., Lee, H. W., Park, J. S., Cha, K. S., Hong, T. J., Park, J. H., Lee, S. Y., Kim, S. P., Kim, Y. D., Chung, S. W., Bae, Y. C., Shin, Y. B., Kim, J. I., & Jung, J. S. (2012). Safety and effect of adipose tissue-derived stem cell implantation in patients with critical limb ischemia: A pilot study. Circulation Journal, 76(7), 1750–1760.
Acosta, L., Hmadcha, A., Escacena, N., Perez-Camacho, I., de la Cuesta, A., Ruiz-Salmeron, R., Gauthier, B. R., & Soria, B. (2013). Adipose mesenchymal stromal cells isolated from type 2 diabetic patients display reduced fibrinolytic activity. Diabetes, 62(12), 4266–4269.
Dentelli, P., Barale, C., Togliatto, G., Trombetta, A., Olgasi, C., Gili, M., Riganti, C., Toppino, M., & Brizzi, M. F. (2013). A diabetic milieu promotes OCT4 and NANOG production in human visceral-derived adipose stem cells. Diabetologia, 56(1), 173–184.
Liu, Y., Li, Z., Liu, T., Xue, X., Jiang, H., Huang, J., & Wang, H. (2013). Impaired cardioprotective function of transplantation of mesenchymal stem cells from patients with diabetes mellitus to rats with experimentally induced myocardial infarction. Cardiovascular Diabetology, 12, 40.
Dzhoyashvili, N. A., Efimenko, A. Y., Kochegura, T. N., Kalinina, N. I., Koptelova, N. V., Sukhareva, O. Y., Shestakova, M. V., Akchurin, R. S., Tkachuk, V. A., & Parfyonova, Y. V. (2014). Disturbed angiogenic activity of adipose-derived stromal cells obtained from patients with coronary artery disease and diabetes mellitus type 2. Journal of Translational Medicine, 12, 337.
Gabr, M. M., Zakaria, M. M., Refaie, A. F., Ismail, A. M., Abou-el-Mahasen, M. A., Ashamallah, S. A., Khater, S. M., el-Halawani, S. M., Ibrahim, R. Y., Uin, G. S., Kloc, M., Calne, R. Y., & Ghoneim, M. A. (2013). Insulin-producing cells from adult human bone marrow mesenchymal stem cells control streptozotocin-induced diabetes in nude mice. Cell Transplantation, 22(1), 133–145.
Koci, Z., Turnovcova, K., Dubsky, M., et al. (2014). Characterization of human adipose tissue-derived stromal cells isolated from diabetic patient's distal limbs with critical ischemia. Cell Biochemistry and Function, 32(7), 597–604.
Policha, A., Zhang, P., Chang, L., Lamb, K., Tulenko, T., & DiMuzio, P. (2014). Endothelial differentiation of diabetic adipose-derived stem cells. The Journal of Surgical Research, 192(2), 656–663.
Vecellio, M., Spallotta, F., Nanni, S., Colussi, C., Cencioni, C., Derlet, A., Bassetti, B., Tilenni, M., Carena, M. C., Farsetti, A., Sbardella, G., Castellano, S., Mai, A., Martelli, F., Pompilio, G., Capogrossi, M. C., Rossini, A., Dimmeler, S., Zeiher, A., & Gaetano, C. (2014). The histone acetylase activator pentadecylidenemalonate 1b rescues proliferation and differentiation in the human cardiac mesenchymal cells of type 2 diabetic patients. Diabetes, 63(6), 2132–2147. https://doi.org/10.2337/db13-0731.
Liu, Q., Hu, C. H., Zhou, C. H., Cui, X. X., Yang, K., Deng, C., Xia, J. J., Wu, Y., Liu, L. C., & Jin, Y. (2015). DKK1 rescues osteogenic differentiation of mesenchymal stem cells isolated from periodontal ligaments of patients with diabetes mellitus induced periodontitis. Scientific Reports, 5, 13142.
Minteer, D. M., Young, M. T., Lin, Y. C., et al. (2015). Analysis of type II diabetes mellitus adipose-derived stem cells for tissue engineering applications. J Tissue Eng, 6, 2041731415579215.
Brewster, L., Robinson, S., Wang, R., Griffiths, S., Li, H., Peister, A., Copland, I., & McDevitt, T. (2017). Expansion and angiogenic potential of mesenchymal stem cells from patients with critical limb ischemia. Journal of Vascular Surgery, 65(3), 826–838 e821.
Davies, L. C., Alm, J. J., Heldring, N., Moll, G., Gavin, C., Batsis, I., Qian, H., Sigvardsson, M., Nilsson, B., Kyllonen, L. E., Salmela, K. T., Carlsson, P. O., Korsgren, O., & le Blanc, K. (2016). Type 1 diabetes mellitus donor mesenchymal stromal cells exhibit comparable potency to healthy controls in vitro. Stem Cells Translational Medicine, 5(11), 1485–1495.
de Lima, K. A., de Oliveira, G. L., Yaochite, J. N., Pinheiro, D. G., de Azevedo, J. T., Silva, W. A., Jr., … Malmegrim, K. C. (2016). Transcriptional profiling reveals intrinsic mRNA alterations in multipotent mesenchymal stromal cells isolated from bone marrow of newly-diagnosed type 1 diabetes patients. Stem Cell Research & Therapy, 7(1), 92.
Cheng, N. C., Hsieh, T. Y., Lai, H. S., & Young, T. H. (2016). High glucose-induced reactive oxygen species generation promotes stemness in human adipose-derived stem cells. Cytotherapy, 18(3), 371–383.
Lafosse, A., Dufeys, C., Beauloye, C., Horman, S., & Dufrane, D. (2016). Impact of hyperglycemia and low oxygen tension on adipose-derived stem cells compared with dermal fibroblasts and keratinocytes: Importance for wound healing in type 2 diabetes. PLoS One, 11(12), e0168058.
Serena, C., Keiran, N., Ceperuelo-Mallafre, V., et al. (2016). Obesity and type 2 diabetes alters the immune properties of human adipose derived stem cells. Stem Cells, 34(10), 2559–2573.
Mancini, O. K., Shum-Tim, D., Stochaj, U., Correa, J. A., & Colmegna, I. (2017). Erratum to: Age, atherosclerosis and type 2 diabetes reduce human mesenchymal stromal cell-mediated T-cell suppression. Stem Cell Research & Therapy, 8(1), 35.
Nawrocka, D., Kornicka, K., Szydlarska, J., & Marycz, K. (2017). Corrigendum to "basic fibroblast growth factor inhibits apoptosis and promotes proliferation of adipose-derived mesenchymal stromal cells isolated from patients with type 2 diabetes by reducing cellular oxidative stress". Oxidative Medicine and Cellular Longevity, 2017, 1083618.
Spallotta, F., Cencioni, C., Atlante, S., Garella, D., Cocco, M., Mori, M., Mastrocola, R., Kuenne, C., Guenther, S., Nanni, S., Azzimato, V., Zukunft, S., Kornberger, A., Sürün, D., Schnütgen, F., von Melchner, H., di Stilo, A., Aragno, M., Braspenning, M., van Criekinge, W., de Blasio, M. J., Ritchie, R. H., Zaccagnini, G., Martelli, F., Farsetti, A., Fleming, I., Braun, T., Beiras-Fernandez, A., Botta, B., Collino, M., Bertinaria, M., Zeiher, A. M., & Gaetano, C. (2018). Stable oxidative cytosine modifications accumulate in cardiac mesenchymal cells from Type2 diabetes patients: Rescue by alpha-ketoglutarate and TET-TDG functional reactivation. Circulation Research, 122(1), 31–46.
Ferland-McCollough, D., Maselli, D., Spinetti, G., et al. (2018). MCP-1 feedback loop between adipocytes and mesenchymal stromal cells causes fat accumulation and contributes to hematopoietic stem cell rarefaction in the bone marrow of patients with diabetes. Diabetes, 67(7), 1380–1394.
Wajid, N., Naseem, R., Anwar, S. S., Awan, S. J., Ali, M., Javed, S., & Ali, F. (2015). The effect of gestational diabetes on proliferation capacity and viability of human umbilical cord-derived stromal cells. Cell and Tissue Banking, 16(3), 389–397.
Kim, J., Piao, Y., Pak, Y. K., Chung, D., Han, Y. M., Hong, J. S., Jun, E. J., Shim, J. Y., Choi, J., & Kim, C. J. (2015). Umbilical cord mesenchymal stromal cells affected by gestational diabetes mellitus display premature aging and mitochondrial dysfunction. Stem Cells and Development, 24(5), 575–586.
Mathew, S. A., & Bhonde, R. (2017). Mesenchymal stromal cells isolated from gestationally diabetic human placenta exhibit insulin resistance, decreased clonogenicity and angiogenesis. Placenta, 59, 1–8.
Li, Y. M., Schilling, T., Benisch, et al. (2007). Effects of high glucose on mesenchymal stem cell proliferation and differentiation. Biochemical and Biophysical Research Communications, 363(1), 209–215.
Weil, B. R., Abarbanell, A. M., Herrmann, J. L., Wang, Y., & Meldrum, D. R. (2009). High glucose concentration in cell culture medium does not acutely affect human mesenchymal stem cell growth factor production or proliferation. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, 296(6), R1735–R1743.
Ryu, J. M., Lee, M. Y., Yun, S. P., & Han, H. J. (2010). High glucose regulates cyclin D1/E of human mesenchymal stem cells through TGF-beta1 expression via Ca2+/PKC/MAPKs and PI3K/Akt/mTOR signal pathways. Journal of Cellular Physiology, 224(1), 59–70.
Kim, Y. J., Hwang, S. H., Lee, S. Y., Shin, K. K., Cho, H. H., Bae, Y. C., & Jung, J. S. (2012). miR-486-5p induces replicative senescence of human adipose tissue-derived mesenchymal stem cells and its expression is controlled by high glucose. Stem Cells and Development, 21(10), 1749–1760.
Dhanasekaran, M., Indumathi, S., Rajkumar, J. S., & Sudarsanam, D. (2013). Effect of high glucose on extensive culturing of mesenchymal stem cells derived from subcutaneous fat, omentum fat and bone marrow. Cell Biochemistry and Function, 31(1), 20–29.
Kim, S. Y., Lee, J. Y., Park, Y. D., Kang, K. L., Lee, J. C., & Heo, J. S. (2013). Hesperetin alleviates the inhibitory effects of high glucose on the osteoblastic differentiation of periodontal ligament stem cells. PLoS One, 8(6), e67504.
Liu, Z., Chen, T., Sun, W., et al. (2016). DNA demethylation rescues the impaired osteogenic differentiation ability of human periodontal ligament stem cells in high glucose. SciRep, 6, 27447.
Ying, X., Chen, X., Liu, H., Nie, P., Shui, X., Shen, Y., Yu, K., & Cheng, S. (2015). Silibinin alleviates high glucose-suppressed osteogenic differentiation of human bone marrow stromal cells via antioxidant effect and PI3K/Akt signaling. European Journal of Pharmacology, 765, 394–401.
Kato, H., Taguchi, Y., Tominaga, K., Kimura, D., Yamawaki, I., Noguchi, M., Yamauchi, N., Tamura, I., Tanaka, A., & Umeda, M. (2016). High glucose concentrations suppress the proliferation of human periodontal ligament stem cells and their differentiation into osteoblasts. Journal of Periodontology, 87(4), e44–e51.
Kang, H. J., Kang, W. S., Hong, M. H., Choe, N., Kook, H., Jeong, H. C., Kang, J., Hur, J., Jeong, M. H., Kim, Y. S., & Ahn, Y. (2015). Involvement of miR-34c in high glucose-insulted mesenchymal stem cells leads to inefficient therapeutic effect on myocardial infarction. Cellular Signalling, 27(11), 2241–2251.
Hankamolsiri, W., Manochantr, S., Tantrawatpan, C., Tantikanlayaporn, D., Tapanadechopone, P., & Kheolamai, P. (2016). The effects of high glucose on Adipogenic and osteogenic differentiation of gestational tissue-derived MSCs. Stem Cells International, 2016, 9674614.
Hajmousa, G., Elorza, A. A., Nies, V. J., Jensen, E. L., Nagy, R. A., & Harmsen, M. C. (2016). Hyperglycemia induces bioenergetic changes in adipose-derived stromal cells while their Pericytic function is retained. Stem Cells and Development, 25(19), 1444–1453.
Fromer, M. W., Chang, S., Hagaman, A. L. R., Koko, K. R., Nolan, R. S., Zhang, P., Brown, S. A., Carpenter, J. P., & Caputo, F. J. (2018). The endothelial cell secretome as a novel treatment to prime adipose-derived stem cells for improved wound healing in diabetes. Journal of Vascular Surgery, 68(1), 234–244.
Qu, B., Gong, K., Yang, H. S., Li, Y. G., Jiang, T., Zeng, Z. M., Cao, Z. R., & Pan, X. M. (2018). MiR-449 overexpression inhibits osteogenic differentiation of bone marrow mesenchymal stem cells via suppressing Sirt1/Fra-1 pathway in high glucose and free fatty acids microenvironment. Biochemical and Biophysical Research Communications, 496(1), 120–126.
Rezabakhsh, A., Cheraghi, O., Nourazarian, A., Hassanpour, M., Kazemi, M., Ghaderi, S., Faraji, E., Rahbarghazi, R., Avci, Ç. B., Bagca, B. G., & Garjani, A. (2017). Type 2 diabetes inhibited human mesenchymal stem cells Angiogenic response by over-activity of the Autophagic pathway. Journal of Cellular Biochemistry, 118(6), 1518–1530.
Ali, F., Aziz, F., & Wajid, N. (2017). Effect of type 2 diabetic serum on the behavior of Wharton's jelly-derived mesenchymal stem cells in vitro. Chronic Dis Transl Med, 3(2), 105–111.
Rezaie, J., Mehranjani, M. S., Rahbarghazi, R., & Shariatzadeh, M. A. (2018). Angiogenic and restorative abilities of human mesenchymal stem cells were reduced following treatment with serum from diabetes mellitus type 2 patients. Journal of Cellular Biochemistry, 119(1), 524–535.
Thakkar, U. G., Trivedi, H. L., Vanikar, A. V., & Dave, S. D. (2015). Insulin-secreting adipose-derived mesenchymal stromal cells with bone marrow-derived hematopoietic stem cells from autologous and allogenic sources for type 1 diabetes mellitus. Cytotherapy, 17(7), 940–947.
Carlsson, P. O., Schwarcz, E., Korsgren, O., & Le Blanc, K. (2015). Preserved beta-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes, 64(2), 587–592.
Dang, L., Phan, N., & Truong, K. (2017). Mesenchymal stem cells for diabetes mellitus treatment: New advances. Biomedical Research and Therapy, 4(1), 1062–1081.
Bhansali, S., Dutta, P., Kumar, V., Yadav, M. K., Jain, A., Mudaliar, S., Bhansali, S., Sharma, R. R., Jha, V., Marwaha, N., Khandelwal, N., Srinivasan, A., Sachdeva, N., Hawkins, M., & Bhansali, A. (2017). Efficacy of autologous bone marrow-derived mesenchymal stem cell and mononuclear cell transplantation in type 2 diabetes mellitus: A randomized, placebo-controlled comparative study. Stem Cells and Development, 26(7), 471–481.
Hajer, G. R., van Haeften, T. W., & Visseren, F. L. (2008). Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. European Heart Journal, 29(24), 2959–2971.
Dominici, M., Le Blanc, K., Mueller, I., Slaper-Cortenbach, I., Marini, F., Krause, D., … Horwitz, E. (2006). Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy, 8(4), 315–317.
Alt, E., Yan, Y., Gehmert, S., Song, Y. H., Altman, A., Gehmert, S., Vykoukal, D., & Bai, X. (2011). Fibroblasts share mesenchymal phenotypes with stem cells, but lack their differentiation and colony-forming potential. Biology of the Cell, 103(4), 197–208.
Konno, M., Hamabe, A., Hasegawa, S., Ogawa, H., Fukusumi, T., Nishikawa, S., Ohta, K., Kano, Y., Ozaki, M., Noguchi, Y., Sakai, D., Kudoh, T., Kawamoto, K., Eguchi, H., Satoh, T., Tanemura, M., Nagano, H., Doki, Y., Mori, M., & Ishii, H. (2013). Adipose-derived mesenchymal stem cells and regenerative medicine. Development, Growth & Differentiation, 55(3), 309–318.
Zhang, F., Cui, J., Liu, X., Lv, B., Liu, X., Xie, Z., & Yu, B. (2015). Roles of microRNA-34a targeting SIRT1 in mesenchymal stem cells. Stem Cell Research & Therapy, 6, 195.
Rutanen, J., Yaluri, N., Modi, S., Pihlajamaki, J., Vanttinen, M., Itkonen, P., Kainulainen, S., Yamamoto, H., Lagouge, M., Sinclair, D. A., Elliott, P., Westphal, C., Auwerx, J., & Laakso, M. (2010). SIRT1 mRNA expression may be associated with energy expenditure and insulin sensitivity. Diabetes, 59(4), 829–835.
Kanafi, M. M., Ramesh, A., Gupta, P. K., & Bhonde, R. R. (2013). Influence of hypoxia, high glucose, and low serum on the growth kinetics of mesenchymal stem cells from deciduous and permanent teeth. Cells, Tissues, Organs, 198(3), 198–208.
Bigarella, C. L., Liang, R., & Ghaffari, S. (2014). Stem cells and the impact of ROS signaling. Development, 141(22), 4206–4218.
Salah Ud-Din, A. I., Tikhomirova, A., & Roujeinikova, A. (2016). Structure and functional diversity of GCN5-related N-acetyltransferases (GNAT). International Journal of Molecular Sciences, 17(7).
Milite, C., Castellano, S., Benedetti, R., Tosco, A., Ciliberti, C., Vicidomini, C., Boully, L., Franci, G., Altucci, L., Mai, A., & Sbardella, G. (2011). Modulation of the activity of histone acetyltransferases by long chain alkylidenemalonates (LoCAMs). Bioorganic & Medicinal Chemistry, 19(12), 3690–3701.
Bochtler, M., Kolano, A., & Xu, G. L. (2017). DNA demethylation pathways: Additional players and regulators. Bioessays, 39(1), 1–13.
Guo, Z., Chen, R., Zhang, F., Ding, M., & Wang, P. (2018). Exendin-4 relieves the inhibitory effects of high glucose on the proliferation and osteoblastic differentiation of periodontal ligament stem cells. Archives of Oral Biology, 91, 9–16.
Ambrosi, T. H., Scialdone, A., Graja, A., Gohlke, S., Jank, A. M., Bocian, C., Woelk, L., Fan, H., Logan, D. W., Schürmann, A., Saraiva, L. R., & Schulz, T. J. (2017). Adipocyte accumulation in the bone marrow during obesity and aging impairs stem cell-based hematopoietic and bone regeneration. Cell Stem Cell, 20(6), 771–784 e776.
Younce, C., & Kolattukudy, P. (2012). MCP-1 induced protein promotes adipogenesis via oxidative stress, endoplasmic reticulum stress and autophagy. Cellular Physiology and Biochemistry, 30(2), 307–320.
Liu, W., Konermann, A., Guo, T., Jager, A., Zhang, L., & Jin, Y. (2014). Canonical Wnt signaling differently modulates osteogenic differentiation of mesenchymal stem cells derived from bone marrow and from periodontal ligament under inflammatory conditions. Biochimica et Biophysica Acta, 1840(3), 1125–1134.
Li, X., Shan, J., Chang, W., Kim, I., Bao, J., Lee, H. J., Zhang, X., Samuel, V. T., Shulman, G. I., Liu, D., Zheng, J. J., & Wu, D. (2012). Chemical and genetic evidence for the involvement of Wnt antagonist Dickkopf2 in regulation of glucose metabolism. Proceedings of the National Academy of Sciences of the United States of America, 109(28), 11402–11407.
Gaur, T., Lengner, C. J., Hovhannisyan, H., Bhat, R. A., Bodine, P. V. N., Komm, B. S., Javed, A., van Wijnen, A. J., Stein, J. L., Stein, G. S., & Lian, J. B. (2005). Canonical WNT signaling promotes osteogenesis by directly stimulating Runx2 gene expression. The Journal of Biological Chemistry, 280(39), 33132–33140.
Marycz, K., Kornicka, K., Maredziak, M., Golonka, P., & Nicpon, J. (2016). Equine metabolic syndrome impairs adipose stem cells osteogenic differentiation by predominance of autophagy over selective mitophagy. Journal of Cellular and Molecular Medicine, 20(12), 2384–2404. https://doi.org/10.1111/jcmm.12932.
Keats, E., & Khan, Z. A. (2012). Unique responses of stem cell-derived vascular endothelial and mesenchymal cells to high levels of glucose. PLoS One, 7(6), e38752.
Jeon, M., Rahman, N., & Kim, Y. S. (2016). Wnt/beta-catenin signaling plays a distinct role in methyl gallate-mediated inhibition of adipogenesis. Biochemical and Biophysical Research Communications, 479(1), 2227.
Aguiari, P., Leo, S., Zavan, B., Vindigni, V., Rimessi, A., Bianchi, K., Franzin, C., Cortivo, R., Rossato, M., Vettor, R., Abatangelo, G., Pozzan, T., Pinton, P., & Rizzuto, R. (2008). High glucose induces adipogenic differentiation of muscle-derived stem cells. Proceedings of the National Academy of Sciences of the United States of America, 105(4), 1226–1231.
Atashi, F., Modarressi, A., & Pepper, M. S. (2015). The role of reactive oxygen species in mesenchymal stem cell adipogenic and osteogenic differentiation: A review. Stem Cells and Development, 24(10), 1150–1163.
Kelley, E. E., Khoo, N. K., Hundley, N. J., Malik, U. Z., Freeman, B. A., & Tarpey, M. M. (2010). Hydrogen peroxide is the major oxidant product of xanthine oxidase. Free Radical Biology & Medicine, 48(4), 493–498.
Turrens, J. F. (2003). Mitochondrial formation of reactive oxygen species. The Journal of Physiology, 552(Pt 2), 335–344.
Iyer, S., Han, L., Bartell, S. M., Kim, H. N., Gubrij, I., de Cabo, R., O'Brien, C. A., Manolagas, S. C., & Almeida, M. (2014). Sirtuin1 (Sirt1) promotes cortical bone formation by preventing beta-catenin sequestration by FoxO transcription factors in osteoblast progenitors. The Journal of Biological Chemistry, 289(35), 24069–24078.
Yu, S., Geng, Q., Sun, F., Yu, Y., Pan, Q., & Hong, A. (2013). Osteogenic differentiation of C2C12 myogenic progenitor cells requires the Fos-related antigen Fra-1 - a novel target of Runx2. Biochemical and Biophysical Research Communications, 430(1), 173–178.
El-Badawy, A., Amer, M., Abdelbaset, R., et al. (2016). Adipose stem cells display higher regenerative capacities and more adaptable electro-kinetic properties compared to bone marrow-derived mesenchymal stromal cells. Scientific Reports, 6, 37801.
Wang, M., Crisostomo, P. R., Herring, C., Meldrum, K. K., & Meldrum, D. R. (2006). Human progenitor cells from bone marrow or adipose tissue produce VEGF, HGF, and IGF-I in response to TNF by a p38 MAPK-dependent mechanism. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, 291(4), R880–R884.
Wang, M., Zhang, W., Crisostomo, P., Markel, T., Meldrum, K. K., Fu, X. Y., & Meldrum, D. R. (2007). STAT3 mediates bone marrow mesenchymal stem cell VEGF production. Journal of Molecular and Cellular Cardiology, 42(6), 1009–1015.
Cao, Y., Sun, Z., Liao, L., Meng, Y., Han, Q., & Zhao, R. C. (2005). Human adipose tissue-derived stem cells differentiate into endothelial cells in vitro and improve postnatal neovascularization in vivo. Biochemical and Biophysical Research Communications, 332(2), 370–379.
Karar, J., & Maity, A. (2011). PI3K/AKT/mTOR pathway in angiogenesis. Frontiers in Molecular Neuroscience, 4, 51.
Lassance, L., Miedl, H., Absenger, M., Diaz-Perez, F., Lang, U., Desoye, G., & Hiden, U. (2013). Hyperinsulinemia stimulates angiogenesis of human fetoplacental endothelial cells: A possible role of insulin in placental hypervascularization in diabetes mellitus. The Journal of Clinical Endocrinology and Metabolism, 98(9), E1438–E1447.
Zheng, X., Li, A., Zhao, L., Zhou, T., Shen, Q., Cui, Q., & Qin, X. (2013). Key role of microRNA-15a in the KLF4 suppressions of proliferation and angiogenesis in endothelial and vascular smooth muscle cells. Biochemical and Biophysical Research Communications, 437(4), 625–631.
Bajou, K., Herkenne, S., Thijssen, V. L., D'Amico, S., Nguyen, N. Q. N., Bouché, A., Tabruyn, S., Srahna, M., Carabin, J. Y., Nivelles, O., Paques, C., Cornelissen, I., Lion, M., Noel, A., Gils, A., Vinckier, S., Declerck, P. J., Griffioen, A. W., Dewerchin, M., Martial, J. A., Carmeliet, P., & Struman, I. (2014). PAI-1 mediates the antiangiogenic and profibrinolytic effects of 16K prolactin. Nature Medicine, 20(7), 741–747. https://doi.org/10.1038/nm.3552.
Wani, W. Y., Boyer-Guittaut, M., Dodson, M., Chatham, J., Darley-Usmar, V., & Zhang, J. (2015). Regulation of autophagy by protein post-translational modification. Laboratory Investigation, 95(1), 14–25.
Glick, D., Barth, S., & Macleod, K. F. (2010). Autophagy: Cellular and molecular mechanisms. The Journal of Pathology, 221(1), 3–12.
Liu, J., Hao, H., Huang, H., Tong, C., Ti, D., Dong, L., Chen, D., Zhao, Y., Liu, H., Han, W., & Fu, X. (2015). Hypoxia regulates the therapeutic potential of mesenchymal stem cells through enhanced autophagy. The International Journal of Lower Extremity Wounds, 14(1), 63–72.
Burke, R. M., & Berk, B. C. (2015). The role of PB1 domain proteins in endothelial cell dysfunction and disease. Antioxidants & Redox Signaling, 22(14), 1243–1256.
Prockop, D. J., & Oh, J. Y. (2012). Mesenchymal stem/stromal cells (MSCs): Role as guardians of inflammation. Molecular Therapy, 20(1), 14–20.
Neuss, S., Schneider, R. K., Tietze, L., Knuchel, R., & Jahnen-Dechent, W. (2010). Secretion of fibrinolytic enzymes facilitates human mesenchymal stem cell invasion into fibrin clots. Cells, Tissues, Organs, 191(1), 36–46.
Moll, G., Rasmusson-Duprez, I., von Bahr, L., Connolly-Andersen, A. M., Elgue, G., Funke, L., Hamad, O. A., Lönnies, H., Magnusson, P. U., Sanchez, J., Teramura, Y., Nilsson-Ekdahl, K., Ringdén, O., Korsgren, O., Nilsson, B., & le Blanc, K. (2012). Are therapeutic human mesenchymal stromal cells compatible with human blood? Stem Cells, 30(7), 1565–1574.
Fadini, G. P., Albiero, M., Vigili de Kreutzenberg, S., Boscaro, E., Cappellari, R., Marescotti, M., Poncina, N., Agostini, C., & Avogaro, A. (2013). Diabetes impairs stem cell and proangiogenic cell mobilization in humans. Diabetes Care, 36(4), 943–949.
Hocking, A. M. (2015). The role of chemokines in mesenchymal stem cell homing to wounds. Advances in Wound Care (New Rochelle), 4(11), 623–630.
Ren, G., Zhang, L., Zhao, X., Xu, G., Zhang, Y., Roberts, A. I., Zhao, R. C., & Shi, Y. (2008). Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell, 2(2), 141–150.
Mendez-Ferrer, S., Michurina, T. V., Ferraro, F., et al. (2010). Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature, 466(7308), 829–834.
Bernardo, M. E., & Fibbe, W. E. (2013). Mesenchymal stromal cells: Sensors and switchers of inflammation. Cell Stem Cell, 13(4), 392–402.
Denu, R. A., & Hematti, P. (2016). Effects of oxidative stress on mesenchymal stem cell biology. Oxidative Medicine and Cellular Longevity, 2016, 2989076.
Schieber, M., & Chandel, N. S. (2014). ROS function in redox signaling and oxidative stress. Current Biology, 24(10), R453–R462.
Kume, S., Kato, S., Yamagishi, S., Inagaki, Y., Ueda, S., Arima, N., Okawa, T., Kojiro, M., & Nagata, K. (2005). Advanced glycation end-products attenuate human mesenchymal stem cells and prevent cognate differentiation into adipose tissue, cartilage, and bone. Journal of Bone and Mineral Research, 20(9), 1647–1658.
Yang, K., Wang, X. Q., He, Y. S., et al. (2010). Advanced glycation end products induce chemokine/cytokine production via activation of p38 pathway and inhibit proliferation and migration of bone marrow mesenchymal stem cells. Cardiovascular Diabetology, 9, 66.
Grant, R. W., & Dixit, V. D. (2013). Mechanisms of disease: Inflammasome activation and the development of type 2 diabetes. Frontiers in Immunology, 4, 50.
Tornatore, L., Thotakura, A. K., Bennett, J., Moretti, M., & Franzoso, G. (2012). The nuclear factor kappa B signaling pathway: Integrating metabolism with inflammation. Trends in Cell Biology, 22(11), 557–566.
Ye, J. (2013). Mechanisms of insulin resistance in obesity. Frontiers in Medicine, 7(1), 14–24.
Ruan, H., & Dong, L. Q. (2016). Adiponectin signaling and function in insulin target tissues. Journal of Molecular Cell Biology, 8(2), 101–109.
Ohashi, K., Parker, J. L., Ouchi, N., Higuchi, A., Vita, J. A., Gokce, N., Pedersen, A. A., Kalthoff, C., Tullin, S., Sams, A., Summer, R., & Walsh, K. (2010). Adiponectin promotes macrophage polarization toward an anti-inflammatory phenotype. The Journal of Biological Chemistry, 285(9), 6153–6160.
Zhao, J., Goldberg, J., Bremner, J. D., & Vaccarino, V. (2012). Global DNA methylation is associated with insulin resistance: A monozygotic twin study. Diabetes, 61(2), 542–546.
Sebok, D., Eberhardt, M., Barbero, A., Linscheid, P., Timper, K., Martin, I., Keller, U., Muller, B., & Zulewski, H. (2007). Bone marrow derived mesenchymal stem cells isolated from patients with diabetes mellitus type 1 are able to induce a pancreatic endocrine genes in vitro. J Stem Cells Regen Med, 2(1), 102–103.
Ilangumaran, S., Villalobos-Hernandez, A., Bobbala, D., & Ramanathan, S. (2016). The hepatocyte growth factor (HGF)-MET receptor tyrosine kinase signaling pathway: Diverse roles in modulating immune cell functions. Cytokine, 82, 125–139.
Alvarez-Perez, J. C., Ernst, S., Demirci, C., Casinelli, G. P., Mellado-Gil, J. M. D., Rausell-Palamos, F., Vasavada, R. C., & Garcia-Ocana, A. (2014). Hepatocyte growth factor/c-met signaling is required for beta-cell regeneration. Diabetes, 63(1), 216–223.
Krampera, M., Pasini, A., Rigo, A., Scupoli, M. T., Tecchio, C., Malpeli, G., Scarpa, A., Dazzi, F., Pizzolo, G., & Vinante, F. (2005). HB-EGF/HER-1 signaling in bone marrow mesenchymal stem cells: Inducing cell expansion and reversibly preventing multilineage differentiation. Blood, 106(1), 59–66.
Coutu, D. L., Francois, M., & Galipeau, J. (2011). Inhibition of cellular senescence by developmentally regulated FGF receptors in mesenchymal stem cells. Blood, 117(25), 6801–6812.
Shukla, A., Grisouard, J., Ehemann, V., Hermani, A., Enzmann, H., & Mayer, D. (2009). Analysis of signaling pathways related to cell proliferation stimulated by insulin analogs in human mammary epithelial cell lines. Endocrine-Related Cancer, 16(2), 429–441.
Chen, J., Crawford, R., Chen, C., & Xiao, Y. (2013). The key regulatory roles of the PI3K/Akt signaling pathway in the functionalities of mesenchymal stem cells and applications in tissue regeneration. Tissue Engineering. Part B, Reviews, 19(6), 516–528.
Raffaele, M., Li Volti, G., Barbagallo, I. A., & Vanella, L. (2016). Therapeutic efficacy of stem cells transplantation in diabetes: Role of Heme oxygenase. Frontiers in Cell and Development Biology, 4, 80.
Kawamura, N., Kugimiya, F., Oshima, Y., Ohba, S., Ikeda, T., Saito, T., Shinoda, Y., Kawasaki, Y., Ogata, N., Hoshi, K., Akiyama, T., Chen, W. S., Hay, N., Tobe, K., Kadowaki, T., Azuma, Y., Tanaka, S., Nakamura, K., Chung, U. I., & Kawaguchi, H. (2007). Akt1 in osteoblasts and osteoclasts controls bone remodeling. PLoS One, 2(10), e1058.
Lo, T., Ho, J. H., Yang, M. H., & Lee, O. K. (2011). Glucose reduction prevents replicative senescence and increases mitochondrial respiration in human mesenchymal stem cells. Cell Transplantation, 20(6), 813–825.
Bakopoulou, A., Kritis, A., Andreadis, D., Papachristou, E., Leyhausen, G., Koidis, P., Geurtsen, W., & Tsiftsoglou, A. (2015). Angiogenic potential and Secretome of human apical papilla mesenchymal stem cells in various stress microenvironments. Stem Cells and Development, 24(21), 2496–2512.
Rekittke, N. E., Ang, M., Rawat, D., Khatri, R., & Linn, T. (2016). Regenerative therapy of type 1 diabetes mellitus: From pancreatic islet transplantation to mesenchymal stem cells. Stem Cells International, 2016, 3764681.
Mottaghi, S., Larijani, B., & Sharifi, A. M. (2012). Apelin 13: A novel approach to enhance efficacy of hypoxic preconditioned mesenchymal stem cells for cell therapy of diabetes. Medical Hypotheses, 79(6), 717–718.
Guarente, L. (2007). Sirtuins in aging and disease. Cold Spring Harbor Symposia on Quantitative Biology, 72, 483–488.
Yuan, H. F., Zhai, C., Yan, X. L., Zhao, D. D., Wang, J. X., Zeng, Q., Chen, L., Nan, X., He, L. J., Li, S. T., Yue, W., & Pei, X. T. (2012). SIRT1 is required for long-term growth of human mesenchymal stem cells. J Mol Med (Berl), 90(4), 389–400.
Shakibaei, M., Shayan, P., Busch, F., Aldinger, C., Buhrmann, C., Lueders, C., & Mobasheri, A. (2012). Resveratrol mediated modulation of Sirt-1/Runx2 promotes osteogenic differentiation of mesenchymal stem cells: Potential role of Runx2 deacetylation. PLoS One, 7(4), e35712.
Fu, Y., Kinter, M., Hudson, J., Humphries, K. M., Lane, R. S., White, J. R., Hakim, M., Pan, Y., Verdin, E., & Griffin, T. M. (2016). Aging promotes Sirtuin 3-dependent cartilage superoxide dismutase 2 acetylation and osteoarthritis. Arthritis & Rhematology, 68(8), 1887–1898.
Jeong, S. M., Hwang, S., & Seong, R. H. (2016). SIRT4 regulates cancer cell survival and growth after stress. Biochemical and Biophysical Research Communications, 470(2), 251–256.
Wu, J., Strawn, T. L., Luo, M., Wang, L., Li, R., Ren, M., Xia, J., Zhang, Z., Ma, W., Luo, T., Lawrence, D. A., & Fay, W. P. (2015). Plasminogen activator inhibitor-1 inhibits angiogenic signaling by uncoupling vascular endothelial growth factor receptor-2-alphaVbeta3 integrin cross talk. Arteriosclerosis, Thrombosis, and Vascular Biology, 35(1), 111–120.
Cui, Z., Zhou, H., He, C., Wang, W., Yang, Y., & Tan, Q. (2015). Upregulation of Bcl-2 enhances secretion of growth factors by adipose-derived stem cells deprived of oxygen and glucose. Bioscience Trends, 9(2), 122–128.
Acknowledgements
This manuscript was funded in part by the Science and Technology Development Fund, STDF grant #5300, Center of Excellence for Stem Cells and Regenerative Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Mahmoud, M., Abu-Shahba, N., Azmy, O. et al. Impact of Diabetes Mellitus on Human Mesenchymal Stromal Cell Biology and Functionality: Implications for Autologous Transplantation. Stem Cell Rev and Rep 15, 194–217 (2019). https://doi.org/10.1007/s12015-018-9869-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-018-9869-y