Abstract
Exposure to polychlorinated biphenyls (PCBs) can activate inflammatory responses in vascular endothelial cells. Activation of peroxisome proliferator-activated receptors (PPARs) by nutrients or synthetic agonists has been shown to block pro-inflammatory responses both in vitro and in vivo. Here we demonstrate that activation of PPARα by synthetic agonists can reduce 3,3′4,4′-tetrachlorobiphenyl (PCB77)-induced endothelial cell activation. Primary vascular endothelial cells were pretreated with the PPARα ligands fenofibrate or WY14643 followed by exposure to PCB77. PPARα activation protected endothelial cells against PCB77-induced expression of the pro-inflammatory proteins vascular cell adhesion molecule-1 (VCAM-1), cycloxygenase-2 (COX-2), and PCB77-induced expression and activity of the aryl hydrocarbon receptor (AHR) responsive cytochrome P450 1A1 (CYP1A1). Furthermore, basal AHR expression was downregulated by fenofibrate and WY14643. We also investigated the possible interactions between PCBs, and basal PPAR activity and protein expression. Treatment with PCB77 significantly reduced basal mRNA expression of PPARα and the PPAR responsive gene CYP4A1, as well as PPARα protein expression. Also, PCB77 exposure caused a significant decrease in basal PPAR-dependent reporter gene expression in MCF-7 cells. Overall, these findings suggest that PPARα agonists can reduce PCB77 induction of endothelial cell activation by inhibition of the AHR pathway, and that coplanar PCB induced pro-inflammatory effects could be mediated, in part, by inhibition of PPARα expression and function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is substantial evidence from epidemiological studies that cardiovascular diseases are linked to environmental exposure to halogenated aromatic hydrocarbons (HAHs), such as dioxins and polychlorinated biphenyls (PCBs). For example, there was a significant increase in mortality from cardiovascular diseases among Swedish capacitor manufacturing workers exposed to PCBs for at least 5 years [1], and elevated plasma lipids and atherosclerotic plaques have been observed among dioxin exposed workers from the former Czechoslovakia [2]. A higher incidence of cardiovascular diseases, specifically chronic ischemic heart disease and chronic rheumatic heart disease, was detected in studies on the dioxin-exposed population of Seveso, Italy, after an industrial accident in 1976 [3, 4]. Furthermore, a recent study reported increased hospitalization rates for coronary heart disease in populations residing near areas contaminated with persistent organic pollutants [5].
Atherosclerotic lesions are thought to be initiated by vascular endothelial cell activation [6]. Since the endothelium is in immediate contact with the blood, endothelial cells are particularly susceptible to the effect of pro-inflammatory agents, such as cytokines and environmental contaminants present in the bloodstream [7]. We have previously reported that coplanar PCBs such as PCB77 can activate the aryl hydrocarbon receptor (AHR), the pro-inflammatory transcription factor nuclear factor kappa B (NF-κB), increase oxidative stress, and induce expression of adhesion molecules and cytokines such as vascular cell adhesion molecule-1 (VCAM-1) and interleukin-6 (IL-6) in vascular endothelial cells [8, 9]. Increased expression of adhesion molecules and cytokines play a critical role in endothelial cell activation and vascular disease [10, 11]. Furthermore, cell culture studies using U937 macrophages have shown that exposure to dioxin, can increase the expression of matrix degrading metalloproteinases, cyclooxygenase-2 (COX-2), and interleukin 1β, and promote foam cell formation [12]. The expression of adhesion molecules and cytokines further enhances the inflammation by recruiting monocytes, and facilitating their binding to and migration through the endothelium. This loss of the endothelial barrier function can increase the accumulation of foam cells in the subendothelial space, subsequently leading to the formation of fatty streaks and advanced atherosclerosis [7, 13]. Studies with both in vivo and in vitro models have shown that many of the pro-inflammatory effects induced by coplanar PCBs are dependent on AHR function [14, 15]. In contrast to dioxin or dioxin-like compound-induced toxicity through abnormal or prolonged AHR activation [16, 17], it has been proposed that intervention using nutritional or pharmaceutical AHR inhibitors could potentially reduce toxicity caused by xenobiotic AHR ligands [18].
The peroxisome proliferator-activated receptors (PPARs) are ligand-activated transcription factors that form part of the nuclear receptor superfamily [19]. There are three genes that belong to the PPAR family: PPARα, PPARγ, and PPARβ/δ. Upon activation, PPARs control gene expression by forming a heterodimer with the retinoid × receptor that can recognize specific DNA sequences known as PPAR response elements (PPREs) [20]. PPARα expression is localized in tissues with a high metabolic rate (e.g., liver, kidney, and skeletal muscle), and in various cell types in the vascular wall such as smooth muscle cells, endothelial cells, and monocytes/macrophages [21]. Nutritional and pharmaceutical PPARα agonists have been shown to be protective against atherosclerosis by downregulating underlying pro-inflammatory signaling pathways [22, 23]. PPARα has been shown to negatively interfere with NF-κB, and activator protein-1 (AP-1) signaling pathways [24], and can therefore prevent the induction of inflammatory genes such as adhesion molecules and cytokines controlled by these transcription factors. Indeed, clinical and experimental evidence suggests that PPARα activation decreases the incidence of cardiovascular diseases [21, 23].
The objective of the current study was to determine interactions between the PPARα and AHR pathways in the vascular endothelium. We hypothesized that PPARα agonists can block PCB77 activation of pro-inflammatory responses in endothelial cells and that PCBs could alter basal PPARα function. Our results suggest that PPARα can interfere with PCB77 activation of the AHR pathway, and that PCBs can reduce function and expression of PPARα. Since PPARα plays a critical role in inflammation, the negative PCB effects on PPARα expression and function may increase susceptibility to other kinds of pro-inflammatory stimuli in exposed individuals.
Materials and Methods
Cell Culture and Experimental Media
Endothelial cells were isolated from porcine pulmonary arteries, as described earlier [25]. Arteries obtained during routine slaughter were donated from the College of Agriculture, University of Kentucky. Endothelial cells from passages 5–10 were used in the current experiments. MCF-7 cells, stably transfected with a luciferase gene driven by a triple repeat of the PPAR response element (PPRE), were utilized for selected experiments. Cells were subcultured in medium 199 (endothelial cells) and DMEM (MCF-7 cells) containing 10% (v/v) fetal bovine serum (FBS, HyClone Laboratories, Logan, UT, USA) using standard techniques.
The experimental media contained 1% (v/v) FBS. PCB 77 (0.001–3.4 μM) and PPARα agonists (10–20 μM) were added from stock solutions prepared in dimethyl sulfoxide (DMSO; Sigma, St. Louis, MO, USA). The PPARα agonists’ fenofibrate and WY14643 were purchased from Sigma (St. Louis, MO, USA) and Cayman Chemical (Ann Arbor, MI, USA), respectively. These two different agonists were used to verify that the observed effects were PPARα specific. PCB77 was kindly provided by Dr. Larry W. Robertson, University of Iowa. PCB77 was used at a concentration, which was previously shown to promote endothelial cell activation, and is based on previously reported serum concentrations occurring after acute exposure [8, 9, 26]. All treatment groups contained an equal amount of DMSO. The final DMSO concentration in the media never exceeded 0.05% (v/v) in all treatment groups. Cells were treated with PPARα agonists and with PCBs for 6–18 h.
CYP1A1 Activity: Ethoxyresorufin-o-Deethylase (EROD)
Cellular cytochrome P450 1A1 (CYP1A1) activity or ethoxyresorufin-o-deethylase (EROD) activity was measured in 48 well plates (Costar, Corning Incorporated, NY, USA) using 7-ethoxyresorufin (Sigma, St. Louis, MO, USA) as a CYP1A1 substrate, as described previously [14, 27]. Briefly, cells were rinsed with phosphate buffered serum (PBS; 37°C) followed by the addition of 7-ethoxyresorufin (2 μM final concentration). The reaction was measured using a Cytofluor 4000 (PE Biosystems, Foster City, CA, USA) containing excitation and emission filters for 530 and 590 nm, respectively.
Measurement of VCAM-1, COX-2, CYP1A1, AHR, β-actin, and PPARα protein expression
Total cellular protein was extracted, as described previously [8]. Cell monolayers were scraped and washed in cold PBS, pelleted, and incubated in 110 μl of lysis buffer containing 20 mM Tris, 150 mM NaCl, 1 mM EDTA, 0.5 mM dithiothreitol, 0.5 mM phenylmethanesulfonyl fluoride (PMSF), 1 μg/ml leupeptin, 1 μg/ml pepstatin, 0.1% nonidet P-40, and 0.5% Triton X-100. Protein extracts were electrophoresed on 12% SDS–polyacrylamide gels transferred to nitrocellulose membranes. Proteins were probed with commercial rabbit and goat antibodies for VCAM-1, COX-2, CYP1A1, AHR (goat polyclonal IgG isotype, Santa Cruz Biotechnology, Santa Cruz, CA, USA), PPARα (rabbit polyclonal IgG isotype, Cayman Chemical, Ann Arbor, MI, USA), and β-actin (rabbit polyclonal IgG, Sigma, St. Louis, MO, USA). β-actin was used as a loading control for normalizing expression of proteins of interest. Antibodies were diluted 1:1,000 or 1:3,000 in blocking buffer. Blots were developed with an Image Station 2000R (KODAK Molecular Imaging Systems, New Haven, CT, USA) using ECL (GE Healthcare, Piscataway, NJ, USA) for chemiluminescent detection.
PPARα and CYP4A1 mRNA Expression Real Time Polymerase Chain Reaction (PCR)
RNA was extracted using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s directions. Specific primers for porcine CYP4A1, PPARα, and β-actin mRNAs were designed using Primer Express 3.0 software (Applied Biosystems, Foster City, CA, USA). The following primers were employed; CYP4A1 forward: 5′ GGA ATC ATC CTC TCG CTC TTCA 3′, reverse: 5′ GCA GAA CCC GGT GCA AAC 3′, PPARα forward: 5′ TCG CCA TGC TGT CCT CTG T 3′, reverse: 5′ AAG GGT TTC CTC AGG CTC TTG 3′, β-actin forward: 5′ TCA TCA CCA TCG GCA ACG 3′, reverse: 5′ TTC CTG ATG TCC ACG TCG 3′. Real time PCR was conducted with the 7300 Real Time PCR System (Applied Biosystems) and using Sybr Green (Applied Biosystems) to measure gene expression according to manufacturer instructions. The CYP4A1 and PPARα expression data obtained for individual samples were normalized to the corresponding β-actin expression.
PPAR Reporter Gene Studies
Since primary endothelial cells are difficult to transfect with high efficiency, a well-established model, previously used to study PPAR function, was used to study PPAR-dependent reporter gene expression [28]. The human breast cancer epithelial cell line MCF-7 was transfected with pGL3 vector (Promega, Madison, WI, USA) containing a triple repeat of PPRE in the promoter region driving luciferase gene expression and a HSV-TK-driven renilla. Transfected cells were selected using G418. Cells were plated in 48 well plates and exposed to PCBs 6 h prior to cell lysis. Cell lysis and reporter gene assay was performed using the dual reporter assay kit (Promega, Madison, WI, USA). Values were expressed as a luciferase/renilla ratio.
Statistical Analysis
All experiments were performed in triplicate. Comparisons between treatments were made by one-way or two-way ANOVA. Post-hoc comparisons of the means were made by Tukey tests. Statistical probability of P < 0.05 was considered significant. All statistical analyses were performed with Sigmastat (Systat Software, San Jose, CA, USA).
Results
PPARα Agonists Downregulate the PCB77-Induced Expression of the Pro-inflammatory Proteins COX-2 and VCAM-1
Previous studies have demonstrated that exposure to coplanar PCBs and halogenated aromatic hydrocarbons (HAHs) can lead to increased expression of pro-inflammatory genes associated with endothelial activation and atherosclerosis [8, 12]. To determine if PPARα can block PCB77-induced expression of the pro-inflammatory proteins COX-2 and VCAM-1, porcine endothelial cells were pretreated with fenofibrate (FF) followed by exposure to PCB77, and total cellular proteins were extracted, followed by immunoblots. PCB77 significantly induced COX-2 protein expression, but pretreatment with FF significantly blocked this effect (Fig. 1). To determine if PPARα activation can interfere with PCB77 induction of VCAM-1, endothelial cells were pretreated with FF or WY14643 followed by exposure to PCB77. PCB77 significantly induced VCAM-1 protein expression, which was partially blocked by pretreatment with FF or WY14643 (Fig. 2a and b). Basal COX-2 and VCAM-1 protein expression was not altered by treatment with either PPAR ligand.
Expression of COX-2 protein after pretreatment with the PPARα ligand fenofibrate (FF; 1 or 10 μM) followed by exposure to PCB77 (3.4 μM). Cell cultures were pretreated with FF for 8 h followed by exposure to vehicle (DMSO), or PCB77 for 18 h followed by immunoblots. COX-2 densitometry values were normalized to β-actin signal. Blots represent one of the three replicates. Bars represent % of control values ± SEM (n = 3); *Statistically significant difference (P < 0.05) relative to the control group
(a and b): Expression of VCAM-1 protein after pretreatment with the PPARα ligands fenofibrate (FF) or WY14643 (WY) at a final concentration of 10 and 20 μM, respectively, followed by exposure to PCB77 (3.4 μM). Cell cultures were pretreated with FF (a) or WY (b) for 8 h followed by exposure to vehicle (DMSO), or PCB77 for 18 h followed by immunoblots. VCAM-1 densitometry values were normalized to β-actin signal. Blots represent one of the three replicates. Bars represent % of control values ± SEM (n = 3); *Statistically significant difference (P < 0.05) relative to the control group
PPARα Agonists Block PCB77 Induction of CYP1A1 and Reduce Basal AHR Protein Expression
The majority of the pro-inflammatory effects of coplanar HAHs and PCBs are associated with activation of the AHR pathway [15, 29]. To determine if PPARα can alter AHR pathway activation, protein expression and activity of the AHR responsive microsomal enzyme cytochrome P450 1A1 (CYP1A1) was measured in endothelial cells pretreated with PPARα ligands followed by PCB77 exposure. CYP1A1 is a monooxygenase enzyme that is highly inducible by AHR ligands such as coplanar PCBs [27, 30]. Endothelial cell pretreatment with FF resulted in a significant reduction in PCB77-induced CYP1A1 activity (Fig. 3a). Furthermore, treatment with WY14643 significantly reduced CYP1A1 protein induction by PCB77 (Fig. 3b). To determine if PPARα activation affected AHR protein expression, endothelial cells were treated with FF prior to measurement of AHR expression by immunoblots. Treatment with FF resulted in a significant reduction of AHR protein expression (Fig. 4a), which was confirmed using the PPARα ligand WY14643 (Fig. 4b). These results suggest that PPARα activation disrupts the AHR pathway in endothelial cells by reducing AHR protein expression.
(a and b): CYP1A1 activity (a) and protein expression (b) after pretreatment with the PPARα ligands fenofibrate (FF) or WY 14643 (WY) at a final concentration of 10 and 20 μM, respectively, followed by exposure to PCB77 (3.4 μM). Cell cultures were pretreated with FF (a) or WY (b) for 8 h followed by exposure to vehicle (DMSO), or PCB77 for 18 h followed by EROD assay or immunoblots. CYP1A1 densitometry values were normalized to β-actin signal. Blots represent one of the three replicates. Bars represent CYP1A1 activity or protein expression (% of control values) ± SEM (n = 3); * and ** represent statistically significant difference (P < 0.05) from vehicle and PCB treated cells, respectively
Expression of AHR protein after treatment with the PPARα ligands: fenofibrate (FF; 10 μM) (a) or WY14643 (20 μM) (b). Cell cultures were treated with FF or WY14643 for 18 h followed by immunoblots. AHR densitometry values were normalized to β-actin signal. Blots represent one of the three replicates. Bars represent % of control values ± SEM (n = 3); *Statistically significant difference (P < 0.05) relative to the control group
PCBs Decrease PPAR Transcriptional Function, Responsive Gene Expression, and Protein Expression
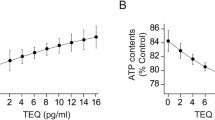
It has been previously shown that PPARα expression and activity are attenuated during inflammation [31, 32]. To determine if PCB77 exposure can affect basal PPARα function in endothelial cells, mRNA expression of PPARα and the PPAR responsive gene CYP4A1 were measured after treating cells with increasing concentrations of PCB77. Treatment with PCB77 significantly reduced PPARα and CYP4A1 mRNA expression at the lowest concentration used in these experiments (1 nM) (Fig. 5). We then measured the effects of PCB77 on PPARα protein expression. Treatment with PCB77 led to a dose-dependent decrease in PPARα protein expression (Fig. 6). To determine if PCB77 can affect PPAR transcriptional function, a PPAR responsive element driven reporter gene (luciferase) was used in MCF-7 cells. Treatment with PCB77 significantly reduced reporter gene expression (Fig. 7). These results suggest that PCB77 treatment reduced PPARα expression and transcriptional activity.
Effects of PCB77 (0.001–1 μM) on mRNA expression of PPARα and the PPARα responsive gene CYP4A1. Cells were exposed to increasing concentrations of PCB77 for 6 h. mRNA expression was measured by real time PCR using SYBR Green for detection. PPARα and CYP4A1 expression was normalized to β-actin signal. Bars represent % control values ± SEM (n = 3); * and # represent statistically significant differences (P < 0.05) from the respective control groups
Effects of PCB77 (0.01–1 μM) on PPARα protein expression. Cells were exposed to increasing concentrations of PCB77 for 18 h followed by immunoblots. PPARα densitometry values were normalized to β-actin signal. Blots represent one of the three replicates. Bars represent % of control values ± SEM (n = 3 replicates per treatment); * and ** represent statistically significant differences (P < 0.05) relative to the control group, and different PCB77 concentrations
Effects of PCB77 (3.4 μM) on PPAR transcriptional activity in MCF-7 cells stably transfected with a luciferase reporter gene driven by a triple repeat of PPRE. Cells were exposed to PCB77 for 6 h. Luciferase readings were normalized by readings obtained from measuring the CMV-driven renilla. Bars represent means ± SEM (n = 3). *Statistically significant difference (P < 0.05) relative to the control group
Discussion
The results from this study demonstrate that PPARα activation can protect endothelial cells from PCB-induced damage by decreasing expression of AHR protein and subsequent inhibition of the AHR pathway, and that coplanar PCBs can negatively affect PPAR function, and decrease PPARα mRNA and protein expression. It has been shown, in both cell culture and whole animal models that many of the pro-inflammatory and cardiotoxic effects of coplanar HAHs, including PCBs, are mediated by the AHR pathway [29], and the downstream activation of pro-inflammatory signaling cascades [15]. The results from the experiments described above suggest that activation of PPARα blocked PCB77 induction of the responsive pro-inflammatory proteins COX-2 and VCAM-1. Both of these proteins play an important role in endothelial cell activation and the pathogenesis of atherosclerosis. Induced COX-2 activity leads to increased production of prostaglandins, and reactive oxygen species [33, 34], while VCAM-1 is a cell surface receptor recognized by immune cells (monocytes and T lymphocytes) that promotes cell migration to the site of vascular injury [7]. These two proteins have been previously shown to be induced by HAHs [9, 12], and their upregulation is dependent on the presence of a functional AHR [9, 35].
The results from this study suggest that PPARα activation can significantly reduce PCB77 effects by reducing AHR protein expression and the induction of AHR-regulated gene expression. It has been previously shown that PPARα activation can block pro-inflammatory signaling pathways by various mechanisms, which include inhibition of transcription factors AP-1 and NF-κB. This inhibition occurs through various mechanisms: direct interaction with these proteins [36], inducing expression of the NF-κB inhibitory protein IκBα [37], reducing basal expression of the pro-inflammatory transcription factors NF-κB and CAAT enhancer binding protein β (C/EBP-β) [38], and the IL-6 receptor complex IL-6R/gp80 and gp130 [39]. Our results are supportive of previous studies showing that PPARα activation can alter induction of AHR responsive genes, and reduce AHR expression in rat liver and HepG2 cells [40]. Specifically, we demonstrated in endothelial cells that PPARα activation could significantly reduce basal AHR expression, and CYP1A1 induction by PCB77. A recent study using rat liver epithelial cells showed that decreased AHR expression by siRNA targeted gene silencing can reduce CYP1A1 induction by the AHR ligands benzo-a-pyrene and benzo-b-fluoranthene [41]. However, studies using Caco-2 cells, a colorectal carcinoma cell line, suggest that PPARα activation can potentiate AHR expression and CYP1A1 induction [42]. Overall, these data suggest that the outcome of PPARα and AHR pathway interactions are tissue and cell type specific.
In the current study, we focused on PPARα. Both PPARs α and γ are expressed in the vasculature, including the endothelium, and there is evidence that treatment with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) can suppress PPARγ expression [43, 44]. Our data suggest that PCBs can decrease both PPARs α and γ basal protein expression [45]. Various mechanisms triggered by coplanar PCB exposure could be associated with downregulating expression and function of PPARs α and γ. Previous studies have demonstrated that during adipogenesis, TCDD can cause suppression of PPARγ expression through activation of MEK/ERK dependent mechanisms [43], and that these effects could be blocked by AHR inhibitors [46].
Another possible mechanism, by which PCBs decrease basal PPARα expression and function, is by promoting oxidative stress and the activation of pro-inflammatory signaling cascades. PPARα has been shown to be reduced by age-dependent and diet-induced oxidative stress, as well as exposure to pro-inflammatory cytokines [47–49]. Others and we have shown previously that exposure to coplanar PCBs such as PCB77 and PCB126 can activate NF-κB, induce pro-inflammatory cytokine production and oxidative stress [8, 9, 15]. Finally, PPARα downregulation by PCB77 could be due to AHR interference with transcription factors that regulate PPARα expression. It has been shown that the PPARα gene promoter contains multiple binding sites for Sp1 [50, 51], and AHR activation can affect Sp1 function to either promote or repress gene expression [52, 53].
The inhibitory effects of PCB exposure on the basal expression and function of the anti-inflammatory PPARα could increase susceptibility to other types of pro-inflammatory stimuli. Various PPAR knockout models have shown that genetic elimination of PPAR α or γ expression is associated with increased susceptibility to pro-inflammatory agents [54, 55]. Dioxins and coplanar PCBs have been shown to increase expression of genes associated with systemic inflammation and atherosclerosis [9, 12, 15]. These effects, coupled with a decrease in expression of protective PPARs, may increase the potential for PCB toxicity in the vascular endothelium.
Both cell culture and whole animal studies have previously shown that treatment with PPARα ligands can significantly reduce inflammation and atherosclerosis [24, 56]. The data presented in the current study show that PCBs can decrease basal expression and function of PPARα. Furthermore, our data demonstrate that PPARα agonists can inhibit PCB-mediated endothelial cell activation by downregulating AHR expression and function. These observations present a novel mechanism, by which endothelial cell activation and inflammation induced by chlorinated AHR ligands can be attenuated by PPAR agonists.
References
Gustavsson, P., & Hogstedt, C. (1997). A cohort study of Swedish capacitor manufacturing workers exposed to polychlorinated biphenyls (PCBs). American Journal of Industrial Medicine, 32, 234–239.
Pelclova, D., Fenclova, Z., Preiss, J., Prochazka, B., Spacil, J., Dubska, Z., Okrouhlik, B., Lukas, E., & Urban, P. (2002). Lipid metabolism and neuropsychological follow-up study of workers exposed to 2,3,7,8- tetrachlordibenzo-p-dioxin. International Archives of Occupational and Environmental Health, 75(Suppl), S60–S66.
Bertazzi, P. A., Bernucci, I., Brambilla, G., Consonni, D., & Pesatori, A. C. (1998). The Seveso studies on early and long-term effects of dioxin exposure: A review. Environmental Health Perspectives, 106(Suppl 2), 625–633.
Pesatori, A. C., Zocchetti, C., Guercilena, S., Consonni, D., Turrini, D., & Bertazzi, P. A. (1998). Dioxin exposure and non-malignant health effects: A mortality study. Occupational and Environmental Medicine, 55, 126–131.
Sergeev, A. V., & Carpenter, D. O. (2005). Hospitalization rates for coronary heart disease in relation to residence near areas contaminated with persistent organic pollutants and other pollutants. Environmental Health Perspectives, 113, 756–761.
Lusis, A. J. (2000). Atherosclerosis. Nature, 407, 233–241.
Libby, P. (2002). Inflammation in atherosclerosis. Nature, 420, 868–874.
Slim, R., Toborek, M., Robertson, L. W., & Hennig, B. (1999). Antioxidant protection against PCB-mediated endothelial cell activation. Toxicological Sciences, 52, 232–239.
Hennig, B., Meerarani, P., Slim, R., Toborek, M., Daugherty, A., Silverstone, A. E., & Robertson, L. W. (2002). Proinflammatory properties of coplanar PCBs: In vitro and in vivo evidence. Toxicology and Applied Pharmacology, 181, 174–183.
Kougias, P., Chai, H., Lin, P. H., Yao, Q., Lumsden, A. B., & Chen, C. (2005). Effects of adipocyte-derived cytokines on endothelial functions: Implication of vascular disease. The Journal of Surgical Research, 126, 121–129.
Colombo, P. C., Banchs, J. E., Celaj, S., Talreja, A., Lachmann, J., Malla, S., DuBois, N. B., Ashton, A. W., Latif, F., Jorde, U. P., Ware, J. A., & LeJemtel, T. H. (2005). Endothelial cell activation in patients with decompensated heart failure. Circulation, 111, 58–62.
Vogel, C. F., Sciullo, E., & Matsumura, F. (2004). Activation of inflammatory mediators and potential role of ah-receptor ligands in foam cell formation. Cardiovascular Toxicology, 4, 363–373.
Ross, R. (1999). Atherosclerosis—an inflammatory disease. The New England Journal of Medicine, 340, 115–126.
Ramadass, P., Meerarani, P., Toborek, M., Robertson, L. W., & Hennig, B. (2003). Dietary flavonoids modulate PCB-induced oxidative stress, CYP1A1 induction, and AhR-DNA binding activity in vascular endothelial cells. Toxicological Sciences, 76, 212–219.
Matsumura, F. (2003). On the significance of the role of cellular stress response reactions in the toxic actions of dioxin. Biochemical Pharmacology, 66, 527–540.
Shertzer, H. G., Nebert, D. W., Puga, A., Ary, M., Sonntag, D., Dixon, K., Robinson, L. J., Cianciolo, E., & Dalton, T. P. (1998). Dioxin causes a sustained oxidative stress response in the mouse. Biochemical and Biophysical Research Communications, 253, 44–48.
Celander, M., & Forlin, L. (1995). Decreased responsiveness of the hepatic cytochrome-P450 1a1 system in rainbow-trout (Oncorhynchus-Mykiss) after prolonged exposure to Pcb. Aquatic Toxicology, 33, 141–153.
Hennig, B., Ettinger, A. S., Jandacek, R. J., Koo, S., McClain, C., Seifried, H., Silverstone, A., Watkins, B., & Suk, W. A. (2007). Using nutrition for intervention and prevention against environmental chemical toxicity and associated diseases. Environmental Health Perspectives, 115, 493–495.
Issemann, I., & Green, S. (1990). Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature, 347, 645–650.
Tugwood, J. D., Issemann, I., Anderson, R. G., Bundell, K. R., McPheat, W. L., & Green, S. (1992). The mouse peroxisome proliferator activated receptor recognizes a response element in the 5′ flanking sequence of the rat acyl CoA oxidase gene. The EMBO Journal, 11, 433–439.
Israelian-Konaraki, Z., & Reaven, P. D. (2005). Peroxisome proliferator-activated receptor-alpha and atherosclerosis: From basic mechanisms to clinical implications. Cardiology, 103, 1–9.
Mishra, A., Chaudhary, A., & Sethi, S. (2004). Oxidized omega-3 fatty acids inhibit NF-kappaB activation via a PPARalpha-dependent pathway. Arteriosclerosis, Thrombosis, and Vascular Biology, 24, 1621–1627.
Zambon, A., Gervois, P., Pauletto, P., Fruchart, J. C., & Staels, B. (2006). Modulation of hepatic inflammatory risk markers of cardiovascular diseases by PPAR-alpha activators: Clinical and experimental evidence. Arteriosclerosis, Thrombosis, and Vascular Biology, 26, 977–986.
Delerive, P., Fruchart, J. C., & Staels, B. (2001). Peroxisome proliferator-activated receptors in inflammation control. The Journal of Endocrinology, 169, 453–459.
Toborek, M., Lee, Y. W., Kaiser, S., & Hennig, B. (2002). Measurement of inflammatory properties of fatty acids in human endothelial cells. Methods in Enzymology, 352, 198–219.
Jensen, A. A. (1989). Halogenated biphenyls, terphenyls, naphthalenes, dibenzodioxins and related products. Amsterdam: Elsevier Science Publishers.
Stegeman, J. J., Hahn, M. E., Weisbrod, R., Woodin, B. R., Joy, J. S., Najibi, S., & Cohen, R. A. (1995). Induction of cytochrome P4501A1 by aryl hydrocarbon receptor agonists in porcine aorta endothelial cells in culture and cytochrome P4501A1 activity in intact cells. Molecular Pharmacology, 47, 296–306.
Kilgore, M. W., Tate, P. L., Rai, S., Sengoku, E., & Price, T. M. (1997). MCF-7 and T47D human breast cancer cells contain a functional peroxisomal response. Molecular and Cell Endocrinology, 129, 229–235.
Korashy, H. M., & El-Kadi, A. O. (2006). The role of aryl hydrocarbon receptor in the pathogenesis of cardiovascular diseases. Drug Metabolism Reviews, 38, 411–450.
Whitlock, J. P., Jr. (1999). Induction of cytochrome P4501A1. Annual Review of Pharmacology and Toxicology, 39, 103–125.
Morishima, A., Ohkubo, N., Maeda, N., Miki, T., & Mitsuda, N. (2003). NFkappaB regulates plasma apolipoprotein A-I and high density lipoprotein cholesterol through inhibition of peroxisome proliferator-activated receptor alpha. The Journal of Biological Chemistry, 278, 38188–38193.
Reynders, V., Loitsch, S., Steinhauer, C., Wagner, T., Steinhilber, D., & Bargon, J. (2006). Peroxisome proliferator-activated receptor alpha (PPAR alpha) down-regulation in cystic fibrosis lymphocytes. Respiratory Research, 7, 104.
Leopold, J. A., & Loscalzo, J. (2005). Oxidative enzymopathies and vascular disease. Arteriosclerosis, Thrombosis, and Vascular Biology, 25, 1332–1340.
Burleigh, M. E., Babaev, V. R., Oates, J. A., Harris, R. C., Gautam, S., Riendeau, D., Marnett, L. J., Morrow, J. D., Fazio, S., & Linton, M. F. (2002). Cyclooxygenase-2 promotes early atherosclerotic lesion formation in LDL receptor-deficient mice. Circulation, 105, 1816–1823.
Puga, A., Hoffer, A., Zhou, S., Bohm, J. M., Leikauf, G. D., & Shertzer, H. G. (1997). Sustained increase in intracellular free calcium and activation of cyclooxygenase-2 expression in mouse hepatoma cells treated with dioxin. Biochemical Pharmacology, 54, 1287–1296.
Delerive, P., Martin-Nizard, F., Chinetti, G., Trottein, F., Fruchart, J. C., Najib, J., Duriez, P., & Staels, B. (1999). Peroxisome proliferator-activated receptor activators inhibit thrombin-induced endothelin-1 production in human vascular endothelial cells by inhibiting the activator protein-1 signaling pathway. Circulation Research, 85, 394–402.
Delerive, P., Gervois, P., Fruchart, J. C., & Staels, B. (2000). Induction of IkappaBalpha expression as a mechanism contributing to the anti-inflammatory activities of peroxisome proliferator-activated receptor-alpha activators. The Journal of Biological Chemistry, 275, 36703–36707.
Kleemann, R., Gervois, P. P., Verschuren, L., Staels, B., Princen, H. M., & Kooistra, T. (2003). Fibrates down-regulate IL-1-stimulated C-reactive protein gene expression in hepatocytes by reducing nuclear p50-NFkappa B-C/EBP-beta complex formation. Blood, 101, 545–551.
Gervois, P., Kleemann, R., Pilon, A., Percevault, F., Koenig, W., Staels, B., & Kooistra, T. (2004). Global suppression of IL-6-induced acute phase response gene expression after chronic in vivo treatment with the peroxisome proliferator-activated receptor-alpha activator fenofibrate. The Journal of Biological Chemistry, 279, 16154–16160.
Shaban, Z., El-Shazly, S., Ishizuka, M., Kimura, K., Kazusaka, A., & Fujita, S. (2004). PPARalpha-dependent modulation of hepatic CYP1A by clofibric acid in rats. Archives of Toxicology, 78, 496–507.
Andrysik, Z., Vondracek, J., Machala, M., Krcmar, P., Svihalkova-Sindlerova, L., Kranz, A., Weiss, C., Faust, D., Kozubik, A., & Dietrich, C. (2007). The aryl hydrocarbon receptor-dependent deregulation of cell cycle control induced by polycyclic aromatic hydrocarbons in rat liver epithelial cells. Mutation Research, 615, 87–97.
Fallone, F., Villard, P. H., Decome, L., Seree, E., Meo, M., Chacon, C., Durand, A., Barra, Y., & Lacarelle, B. (2005). PPARalpha activation potentiates AhR-induced CYP1A1 expression. Toxicology, 216, 122–128.
Hanlon, P. R., Ganem, L. G., Cho, Y. C., Yamamoto, M., & Jefcoate, C. R. (2003). AhR- and ERK-dependent pathways function synergistically to mediate 2,3,7,8-tetrachlorodibenzo-p-dioxin suppression of peroxisome proliferator-activated receptor-gamma1 expression and subsequent adipocyte differentiation. Toxicology and Applied Pharmacology, 189, 11–27.
Alexander, D. L., Ganem, L. G., Fernandez-Salguero, P., Gonzalez, F., & Jefcoate, C. R. (1998). Aryl-hydrocarbon receptor is an inhibitory regulator of lipid synthesis and of commitment to adipogenesis. Journal of Cell Science, 111(Pt 22), 3311–3322.
Hennig, B., Reiterer, G., Majkova, Z., Oesterling, E., Meerarani, P., & Toborek, M. (2005). Modification of environmental toxicity by nutrients: Implications in atherosclerosis. Cardiovascular Toxicology, 5, 153–160.
Cimafranca, M. A., Hanlon, P. R., & Jefcoate, C. R. (2004). TCDD administration after the pro-adipogenic differentiation stimulus inhibits PPARgamma through a MEK-dependent process but less effectively suppresses adipogenesis. Toxicology and Applied Pharmacology, 196, 156–168.
Poynter, M. E., & Daynes, R. A. (1998). Peroxisome proliferator-activated receptor alpha activation modulates cellular redox status, represses nuclear factor-kappaB signaling, and reduces inflammatory cytokine production in aging. The Journal of Biological Chemistry, 273, 32833–32841.
El Midaoui, A., Wu, L., Wang, R., & de Champlain, J. (2006). Modulation of cardiac and aortic peroxisome proliferator-activated receptor-gamma expression by oxidative stress in chronically glucose-fed rats. American Journal of Hypertension, 19, 407–412.
Kim, M. S., Sweeney, T. R., Shigenaga, J. K., Chui, L. G., Moser, A., Grunfeld, C., & Feingold, K. R. (2007). Tumor necrosis factor and interleukin 1 decrease RXRalpha, PPARalpha, PPARgamma, LXRalpha, and the coactivators SRC-1, PGC-1alpha, and PGC-1beta in liver cells. Metabolism, 56, 267–279.
Gearing, K. L., Crickmore, A., & Gustafsson, J. A. (1994). Structure of the mouse peroxisome proliferator activated receptor alpha gene. Biochemical and Biophysical Research Communications, 199, 255–263.
Chew, C. H., Samian, M. R., Najimudin, N., & Tengku-Muhammad, T. S. (2003). Molecular characterisation of six alternatively spliced variants and a novel promoter in human peroxisome proliferator-activated receptor alpha. Biochemical and Biophysical Research Communications, 305, 235–43.
Khan, S., Barhoumi, R., Burghardt, R., Liu, S., Kim, K., & Safe, S. (2006). Molecular mechanism of inhibitory aryl hydrocarbon receptor-estrogen receptor/Sp1 cross talk in breast cancer cells. Molecular Endocrinology, 20, 2199–2214.
Tsuchiya, Y., Nakajima, M., & Yokoi, T. (2003). Critical enhancer region to which AhR/ARNT and Sp1 bind in the human CYP1B1 gene. Journal of Biochemistry (Tokyo), 133, 583–592.
Delerive, P., De Bosscher, K., Besnard, S., Vanden Berghe, W., Peters, J. M., Gonzalez, F. J., Fruchart, J. C., Tedgui, A., Haegeman, G., & Staels, B. (1999). Peroxisome proliferator-activated receptor alpha negatively regulates the vascular inflammatory gene response by negative cross-talk with transcription factors NF-kappaB and AP-1. The Journal of Biological Chemistry, 274, 32048–32054.
Nakajima, A., Wada, K., Miki, H., Kubota, N., Nakajima, N., Terauchi, Y., Ohnishi, S., Saubermann, L. J., Kadowaki, T., Blumberg, R. S., Nagai, R., & Matsuhashi, N. (2001). Endogenous PPAR gamma mediates anti-inflammatory activity in murine ischemia-reperfusion injury. Gastroenterology, 120, 460–469.
Corti, R., Osende, J., Hutter, R., Viles-Gonzalez, J. F., Zafar, U., Valdivieso, C., Mizsei, G., Fallon, J. T., Fuster, V., & Badimon, J. J. (2007). Fenofibrate induces plaque regression in hypercholesterolemic atherosclerotic rabbits: In vivo demonstration by high-resolution MRI. Atherosclerosis, 190, 106–113.
Acknowledgments
This study was supported in part by grants from NIEHS/NIH (ES 07380), the KY AES, and the University of Kentucky Lyman T. Johnson Postdoctoral Fellowship. G. Reiterer is a recipient of the American Heart Association predoctoral fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arzuaga, X., Reiterer, G., Majkova, Z. et al. PPARα Ligands Reduce PCB-Induced Endothelial Activation: Possible Interactions in Inflammation and Atherosclerosis. Cardiovasc Toxicol 7, 264–272 (2007). https://doi.org/10.1007/s12012-007-9005-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-007-9005-8