Abstract
Helicobacter pylori (H. pylori) infection can interfere with the absorption of most elements, and the variations of some element levels are related to the incidence of gastric cancer. However, there have been conflicting results concerning the influence of H. pylori infection on serum element levels. The present study aimed to compare the serum element concentrations of H. pylori-infected local residents with uninfected residents from Lujiang County with high gastric cancer risk in Eastern China. We used data and serum samples from the H. pylori screening-survey program which was a cross-sectional study. We took 155 samples randomly from the screening survey, identified 74 H. pylori-positive residents and 81 H. pylori-negative residents by a serological test. The serum concentrations of 15 elements (calcium, magnesium, iron, zinc, selenium, copper, molybdenum, chromium, cobalt, nickel, lead, cadmium, mercury, arsenic, and aluminum) were determined using inductively coupled plasma mass spectrometry. Serum cobalt was found at higher levels in the H. pylori-infected residents than the H. pylori-uninfected residents (0.246 vs 0.205 μg/L, P = 0.022), but no statistically significant differences in the serum levels of other elements were found. This is the first study to report the serum concentrations of 15 elements and their relationships with the infection status of H. pylori among local residents from Lujiang County with high gastric cancer risk. Although the International Agency for Research on Cancer has classified cobalt and other soluble cobalt salts as possibly carcinogenic to human beings, our results may provide a clue to the relationships between cobalt, H. pylori, and gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, the incidence and mortality of gastric cancer has been observed to have an overall decreasing trend over the past decades; however, the health burden of gastric cancer is still high in Eastern Asia (particularly in China, Korea, Mongolia, and Japan), Central and Eastern Europe, and South America [1]. Of note, in China, the incidence rate of gastric cancer was 52.3 per 100,000 as well as the mortality was 31.3 per 100,000 according to the data from a large cohort study during 2008–2013 [2]. There is an obvious clustering of the geographical distribution of gastric cancer in China, with the highest mortality being mostly located in rural areas, especially in Gansu, Henan, Hebei, Shanxi, and Anhui Provinces [3, 4]. Lujiang County is located in Anhui Province in Eastern China. In this county, the incidence of gastric cancer adjusted by the Chinese standard population was 68.32 per 100,000 during 2010–2012 according to the data from the local Center for Disease Control and Prevention [5]. In fact, Lujiang County has been known as a county with high gastric cancer risk in which the average annual mortality of gastric cancer has always been above 65.00 per 100,000 since the 1990s [4].
Such high incidence rates may be explained by the fact that this county has a number of gastric cancer risk factors which have been known for a long time. These risks include being a rural region with low economic income, having traditional eating habits of salty foods, and using too much pesticide and fertilizer (as a major agricultural county) which has probably led to contaminated drinking water. On the other hand, it is well known that chronic infection with Helicobacter pylori (H. pylori) is the strongest identified risk factor for gastric cancer, with about 90% of new cases of non-cardia gastric cancer worldwide attributed to this bacteria [6]. H. pylori screening and treatment is a recommended gastric cancer risk reduction strategy in high-risk populations. However, at the Lujiang site, the status of H. pylori infection in 40- to 69-year-old local residents was unclear until we carried out screening work for this infection.
H. pylori have the unique ability to persist in the human stomach, causing nutritional insufficiencies in the host by competing for the acquisition of essential nutrients. Furthermore, the chronic inflammatory response of the gastric mucosa to H. pylori infection can interfere with the absorption of most micronutrients [7], by reducing the secretion of hydrochloric acid and enzymes. In the case of essential minerals, this can prevent them from becoming soluble and affect their absorption, although the absorption process does not take place in the stomach. The variations in some mineral levels are related to the incidence of gastric cancer. For example, some studies showed an inverse relationship between baseline serum selenium concentrations and the risk of mortality from gastric cardia cancer [8, 9]. In addition, there has been evidence that suggested iron deficiency could increase oxidative stress and DNA damage, which might increase the risk of carcinogenesis especially in the gastrointestinal tract [10]. A deficiency of molybdenum may also be one of the risk factors in gastric cancer [11]. However, there have been conflicting results on the influence of H. pylori infection on serum element levels. Some studies observed that there was no obvious difference in serum element levels between the individuals infected with H. pylori and those uninfected, for example, zinc [12], magnesium [13], and selenium [12]. In contrast, some studies have shown that there were differences in the serum concentrations of elements between individuals infected with H. pylori and those uninfected, such as copper [14], zinc [15, 16], and magnesium [15].
With regard to toxic metals, some have been classified as certain or probable carcinogens by the International Agency for Research on Cancer (IARC), for example, lead, cadmium, mercury, and arsenic. Furthermore, numerous investigations have revealed an association between the exposure to these toxic metals and the incidence and mortality of gastric cancer [17]. Our previous work conducted in Anhui Province also showed statistically significant correlations of topsoil lead concentration with the incidence of human gastric cancer, and mercury in grain has been correlated with human liver cancer [18].
Based on the aforementioned information, the objective of this cross-sectional study was to characterize exposure to 15 elements (calcium, Ca; magnesium, Mg; iron, Fe; zinc, Zn; selenium, Se; copper, Cu; molybdenum, Mo; chromium, Cr; cobalt, Co; nickel, Ni; lead, Pb; cadmium, Cd; mercury, Hg; arsenic, As; aluminum, Al) in the blood serum samples (N = 155) from our H. pylori screening work in Lujiang County, assess the infection status of H. pylori among these local residents, and examine the associations between element concentrations in the serum and the H. pylori infection status.
Materials and Methods
Participates and Samples
From July 2015 to December 2016, a total of 1196 40- to 69-year-old local residents in Lujiang County in China were recruited to the H. pylori screening-survey program. The screening survey included a questionnaire interview and blood collection. In this study, serum concentrations of 15 elements were detected in local residents (N = 155) using random sampling from the screening survey. Information on socio-demographics, alcohol and tobacco use, and source of drinking water was obtained by a structured questionnaire administered by trained interviewers and undertaken face-to-face. Approximately 5 mL of venous blood was collected into an element-free vacuum blood tube without anticoagulation. After centrifugation, serum samples were prepared and preserved at a temperature of − 20 °C prior to analyses.
The exclusion criteria included any one of the following: individuals who were not local residents (settlement in local for less than 5 years), were aged less than 40 years or more than 69 years, had taken mineral supplements during the previous 3 months, were diagnosed with chronic wasting diseases (e.g., hepatic diseases, kidney diseases, diabetes mellitus, and cancers), or were pregnant.
The study received ethical approval from the Ethics Institutional Review Board from the Anhui Medical University. Written informed consents were obtained from all participants before taking part in the study.
Measurement of H. pylori Infection
The measurement of H. pylori infection was by a serological test to qualitative determine the IgG antibody of H. pylori. This test is an indirect solid-phase immunochromatographic assay. For all participants recruited in our H. pylori screening-survey program, one drop of serum was sent to Dian Diagnostics Ltd. (Hefei, China) where the serological test was performed.
Detection of the Concentrations of 15 Elements
Serum concentrations of 15 elements were analyzed using inductively coupled plasma mass spectrometry (ICP-MS; Perkin Elmer NexION 350X, USA). The details of this method were described in previous work by one of the authors, Liang [19].
Statistical Analyses
Statistical analysis was performed using SPSS version 10 (SPSS Inc., Chicago, USA). The chi-square test was used for categorical variables. The Mann-Whitney U test was used to assess the difference in element levels between H. pylori-infected residents and uninfected residents. Spearman’s correlation was performed for correlation analysis among the element concentrations. A P value of 0.05 or lower was considered significant.
Results
H. pylori Seropositivity of 155 Local Residents
According to the results of the serological test, there were 74 local residents infected with H. pylori, which was indicated by positive result of the IgG antibody to H. pylori. The remaining participants (N = 81) were never infected with H. pylori which was indicated by negative result for the IgG antibody.
There was no significant difference observed between the H. pylori-infected group and the uninfected group regarding any of the characteristics measured (Table 1). However, the H. pylori seropositivity reached 51.4% in the 60–69-year-age group, higher among females (52.6%) than males (42.9%), and higher among overweight individuals (58.3%) and those with obesity (55.0%) than those with normal weight (40.2%). As other researchers have reported, the H. pylori seropositivity was lower in those who had the highest incomes (40.4%) and education levels (41.5%). In this county, nearly half (48.4%) of the participants still drank water from the local well, and of whom 40.0% were H. pylori-infected, which was lower than those drinking tap water (55.0%).
Element Concentrations in Serum
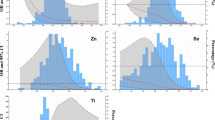
Fifteen element concentrations in serum are shown in Tables 2 and 3. In the H. pylori-uninfected group, the concentrations of nickel and copper were normally distributed. In the H. pylori-infected group, the concentrations of copper, zinc, and magnesium were normally distributed. Other element concentrations in serum were not normally distributed and showed wide scatter, and the medians are listed.
Although there were differences of element concentrations in serum between the H. pylori-infected group and the uninfected group (Fig. 1), only the difference in concentration of cobalt achieved statistical significance (P = 0.022). The median of cobalt concentration was higher in the infected group compared with the uninfected group (0.246 vs 0.205 μg/L).
To explore associations among the multiple element concentrations between the H. pylori-uninfected group and infected group, Spearman’s correlations were calculated in Tables 4 and 5 for most element concentrations in this study were not in normal distribution. In Tables 4 and 5, the symbol of element represented the variables “element concentrations in serum” for expressing succinctly. For example, the iron concentration in serum was expressed by “Fe”. In Table 4, there were positive relationships in the uninfected group between Fe and Pb (rs = 0.428, P < 0.01), Cd and Al (rs = 0.300, P < 0.01), Se and Cu (rs = 0.298, P < 0.01), and Co and Ca (rs = 0.230, P < 0.05), as well as a negative relationship between Mg and Hg (rs = − 0.307, P < 0.05), Se and Al (rs = − 0.297, P < 0.01), Se and Mo (rs = − 0.255, P < 0.05), and Mg and Pb (rs = − 0.239, P < 0.05); however, these correlations in the infected group in Table 5 showed no significant difference.
On the other hand, in Table 5, positive relationships appeared in the H. pylori-infected group between Cr and Al (rs = 0.413, P < 0.01), Hg and Zn (rs = 0.391, P < 0.01), Ni and Se (rs = 0.337, P < 0.01), Hg and Ca (rs = 0.295, P < 0.05), Hg and Ni (rs = 0.279, P < 0.05), Ca and Cr (rs = 0.252, P < 0.05), Ca and Pb (rs = 0.252, P < 0.05), Cu and Pb (rs = 0.240, P < 0.05), and Al and Ni (rs = 0.234, P < 0.05). While in the uninfected group in Table 4, these correlations showed no significant difference or even negative relationships.
Discussion
Lujiang is a county of Anhui Province in Eastern China which has had extremely high incidence and mortality rates of gastric cancer for a long time. Although several attempts have been made to explain what causes such a high incidence of gastric cancer in Lujiang [20, 21], there had been no general survey of the Helicobacter pylori (H. pylori) infection status in local residents until our team began the screening work in 2015. There had also not been any investigation of the influence of H. pylori infection on serum levels of elements. To the best of our knowledge, this is the first study to report the serum concentrations of 15 elements and their relationships with the infection status of H. pylori among local residents from Lujiang County.
With regard to the essential elements, other than cobalt (Co), there were no statistical differences in serum concentrations between the H. pylori-infected local residents and those uninfected with H. pylori in the current study. However, we will focus on three essential minerals associated with gastric cancer. The first is selenium (Se) which functions through selenoproteins. Several of the selenoproteins are oxidant-defense enzymes, such as the selenium-dependent glutathione peroxidase which defends the body against oxidative stress. Many studies have indicated that high selenium exposure had a protective effect on cancer risk [22]. A general population nutrition intervention trial conducted in Linxian County suggested that the participants who received supplementation with vitamins and minerals (including selenium) had lower overall mortality and gastric cancer mortality than individuals who did not receive the supplements [23]. Linxian County is also a rural area with high gastric cancer risk, which is located in Henan Province in Central China. In our study, the mean Se concentration of the total 155 participants was high when compared with that found in the Linxian population [9] (96.475 μg/L compared with 73 μg/L, respectively). In general, Se deficiency is considered to occur when the serum Se concentration is below 70 μg/L [24]. On the basis of this criterion, only 4.5% of our participants (7/155) were considered to be selenium deficient, which means that in the present study, most individuals had no selenium deficiency. The second essential mineral important to consider is iron (Fe), which is an indispensable trace element critical for motor and cognitive development. However, the ability of Fe to cycle between the oxidized and reduced forms also renders it capable of contributing to free radical formation. Therefore, Fe can contribute to both tumor initiation and tumor growth [25]. One result available from a large cohort of more than 300,000 adults in Taiwan suggested that the relationship between serum Fe and cancer risk was a J-shaped one, with higher cancer risk at both ends, either lower than 600 μg/L or higher than 1200 μg/L [26]. In our research, there were 7.1% of the participants (11/155) whose serum Fe levels were lower than 600 μg/L, as well as 52.9% (82/155) higher than 1200 μg/L. If the above thresholds were reliable, it means nearly two-thirds of the participants have a higher carcinogenesis risk. The third essential element of particular interest is molybdenum (Mo) which is also an element that enters the body primarily from dietary sources. In humans, Mo is a cofactor for three enzyme classes—sulfite oxidase, aldehyde dehydrogenase, and xanthine oxidase [27]. It has been suggested for some time that deficiency of molybdenum may be one of the risk factors in gastric cancer. Luo et al. [28] observed in rats that the addition of Mo to drinking water significantly inhibited N-nitrososarcosine ethyl ester-induced forestomach carcinogenesis. Another study performed in humans showed that serum molybdenum levels of patients with gastric cancer were lower than those of healthy controls [11]. In the current study, the serum Mo concentrations tended to be lower in H. pylori-infected participants than those uninfected (1.514 vs 1.651 μg/L). But the difference did not achieve statistical significance (P > 0.05). However, the available epidemiological data are scant, and the appropriate amount of molybdenum in human serum is unknown.
With regard to potentially toxic elements, in the current study, there were also no statistical differences in serum concentrations between the H. pylori-infected participants and those uninfected. Compared to the presentations in the previous reports [29, 30], our results were lower. Meanwhile, continuous biomonitoring studies about these potentially toxic elements are needed. Because more and more research has suggested that low to moderate exposure of some toxic metals, such as arsenic (As) [31] and cadmium (Cd) [32], for a long duration may play a key role in tumorigenesis. Moreover, in our previous work, we also observed statistically significant correlations of topsoil lead (Pb) concentration with human gastric cancer [18]. In other words, it may not be necessary to accumulate a high concentration of some toxic metals during tumorigenesis.
As a constituent of cobalamin, Co is beneficial for humans at the low-dose exposure. The general population is mainly exposed to low levels of Co by breathing, eating, drinking water, or by skin contact. Food and drinking water are the largest sources of exposure to Co for the general population. The low-dose exposures of Co from food and drinking water would not cause organ or tissue damage. In a survey assessing the correlation between cancer mortality and trace metal levels in water supplies throughout the USA, no correlation was found between cancer mortality and the level of Co in the water [33].
However, exposure to high levels of Co may result in lung and heart adverse effects and dermatitis, and even some kind of cancers. Some individuals may develop a high level of Co from their daily lifestyle, which causes an elevated Co concentration in their bodies. These include patients who receive joint prostheses that are fabricated from cobalt alloys [34], workers who perform electroplating, refine or process alloys, use hard metal cutting tools or use diamond-polishing wheels that contain cobalt metal [35], and farmers who use fertilizers containing cobalt. There is evidence that soluble cobalt cations exert a genotoxic and carcinogenic activity from in vitro and in vivo experimental systems [36, 37]. In human studies, most have focused on the association between Co and lung cancer. An industry-wide study of hard-metal workers in France observed an increased mortality from lung cancer [38]. But, a cohort study which comprised Finnish male cobalt production workers between 1969 and 2013 suggested that occupational exposure to Co is not associated with an increased overall cancer risk or lung cancer risk among these workers [39]. Although there is a lack of definitive evidence in human studies, the International Agency for Research on Cancer (IARC) has classified cobalt and other soluble cobalt salts as possibly carcinogenic to humans.
This study found that the median of levels of serum Co was 0.246 μg/L in the H. pylori-infected local residents, which was significantly higher than the level in H. pylori-uninfected participates (0.205 μg/L, P < 0.05). However, the serum Co level we observed in uninfected participants was quite different from other research reported in healthy people. In China, Lei Cai et al. [29] reported that the median of Co was 0.485 μg/L in 110 Chinese healthy adults. Among 79 Korean healthy adults, the median of serum Co was 0.15 μg/L [40]. In Turkey, Karadas [41] reported the level was 0.036 ± 0.019 μg/L. However, the serum Co level which Mohmand et al. [42] reported approached to 1.5 μg/L in 30 individuals from areas of the Punjab in Pakistan. The present status of the literature does not provide an adequate basis for formulating baseline serum Co concentrations. Therefore, results from selected investigations are listed here for information only. Considering the many routes of exposure to Co that we have described previously, the differences in serum Co concentration between the present study and other studies may be related to variation in exposure level to Co in different areas. The differences in detection method and sample size should also be considered.
Thus far, little has been known about the association between the serum level of Co and H. pylori infection, although several meta-analyses indicate that H. pylori infection is associated with reduced levels of cobalamin, supported by the positive effect of eradication treatment [7]. The key mineral in the large cobalamin molecule is Co, and in the general population without occupational exposure, the Co level is assumed to be decreased as a result of reduced levels of cobalamin associated with H. pylori infection. However, in the current study among the H. pylori-infected individuals, the Co concentration was higher than the level in uninfected participants. This is theoretically possible because a few studies have reported that some cobalt complexes have effective urease inhibitory activity [43, 44]. When an individual is infected with H. pylori, the urease that is synthesized by this organism is present at very high levels. This enzyme produces NH3 from gastric fluid urea and is essential for gastric infection or survival in acid. Therefore, followed the reactions between urease and cobalt complexes, it is possible that the Co concentration in the H. pylori-infected individuals will rise. However, studies on urease inhibition by cobalt complexes are lacking.
In the current study, we cannot come to a conclusion that elevated serum concentration of Co is caused by H. pylori infection, without consideration of the following three limitations. Firstly, few local residents of this study might be under the occupational exposure to Co. However, we could not assess the occupational exposure precisely because inaccurate information about the workplace and type of work might exist and could not be found out just by inquiring the subjects. Secondly, in the current study, there were 52.9% (82/155) local residents who were still doing farm work. In Lujiang County, farmers keep the tradition of growing rice twice per year, with a large consumption of fertilizers. After a long exposure to some fertilizers containing Co, one cannot rule out the possibility that the level of Co in the soil may be elevated. Thirdly, we could not provide the intake level of the minerals from food. Actually, a frequency questionnaire about staple foods was included in our questionnaire of the H. pylori screening-survey program. The dietary intake frequencies were compared roughly between the H. pylori-infected and uninfected local residents, but there were no statistically significant differences found (data has not yet been published). We could not further assess the dietary intake levels of the minerals precisely considering the incompleteness and inaccuracy of the food frequency questionnaire. However, there were no significant differences found in the intake frequencies of staple foods between the H. pylori-infected and uninfected subjects. So, we considered the food intake levels of the two groups similar to each other. On the other hand, it was unnecessary in this study to compare the mineral intake information from mineral supplements and drinking water. Because the local residents we detected had not taken mineral supplements during the previous 3 months which mentioned in exclusion criteria. And there was no significant difference in the source of drinking water (Table 1) between the H. pylori-infected and uninfected subjects.
Conclusions
We observed that there were no statistically significant differences in the serum concentrations of elements (other than cobalt) between the H. pylori-infected local residents and the H. pylori-uninfected ones. On the premise that cobalt and other soluble cobalt salts are possibly carcinogenic to human beings, our results may provide a clue to the relationships between cobalt, H. pylori, and gastric cancer.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108. https://doi.org/10.3322/caac.21262
Pan R, Zhu M, Yu C, Lv J, Guo Y, Bian Z, Yang L, Chen Y, Hu Z, Chen Z, Li L, Shen H (2017) Cancer incidence and mortality: a cohort study in China, 2008–2013. Int J Cancer 141(7):1315–1323. https://doi.org/10.1002/ijc.30825
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66(2):115–132. https://doi.org/10.3322/caac.21338
Yang L (2006) Incidence and mortality of gastric cancer in China. World J Gastroenterol 12(1):17–20
Hongyu C, Shuang J, Haiting C, Ran C, Xiaowen D, Guanglie H, Fen H (2015) Analysis of cancer prevalence in Lujiang county of Anhui Province during 2010–2012. Chin J Prevent Control Chronic Dis 23(2):113–115
Plummer M, Franceschi S, Vignat J, Forman D, de Martel C (2015) Global burden of gastric cancer attributable to Helicobacter pylori. Int J Cancer 136(2):487–490. https://doi.org/10.1002/ijc.28999
Lahner E, Persechino S, Annibale B (2012) Micronutrients (other than iron) and Helicobacter pylori infection: a systematic review. Helicobacter 17(1):1–15. https://doi.org/10.1111/j.1523-5378.2011.00892.x
Mark SD, Qiao YL, Dawsey SM, Wu YP, Katki H, Gunter EW, Fraumeni JF Jr, Blot WJ, Dong ZW, Taylor PR (2000) Prospective study of serum selenium levels and incident esophageal and gastric cancers. J Natl Cancer Inst 92(21):1753–1763
Wei WQ, Abnet CC, Qiao YL, Dawsey SM, Dong ZW, Sun XD, Fan JH, Gunter EW, Taylor PR, Mark SD (2004) Prospective study of serum selenium concentrations and esophageal and gastric cardia cancer, heart disease, stroke, and total death. Am J Clin Nutr 79(1):80–85
Pra D, Rech Franke SI, Pegas Henriques JA, Fenech M (2009) A possible link between iron deficiency and gastrointestinal carcinogenesis. Nutr Cancer 61(4):415–426. https://doi.org/10.1080/01635580902803701
Cao GH, Yan SM, Yuan ZK, Wu L, Liu YF (1998) A study of the relationship between trace element Mo and gastric cancer. World J Gastroenterol 4(1):55–56
Wu MC, Huang CY, Kuo FC, Hsu WH, Wang SS, Shih HY, Liu CJ, Chen YH, Wu DC, Huang YL, Lu CY (2014) The effect of Helicobacter pylori eradication on the levels of essential trace elements. Biomed Res Int 2014:513725–513725. https://doi.org/10.1155/2014/513725
Abbasciano V, Sartori S, Trevisani L, Girometti R, Ranzini M, Nielsen I, Mazzotta D, Vecchiatti G, Bononi A, Guglielmini C (2003) Comparison of magnesium concentration in serum, erythrocytes and gastric tissue in two groups of patients affected by chronic gastritis, Helicobacter pylori negative and positive. Magnes Res 16(4):281–286
Janjetic MA, Goldman CG, Balcarce NE, Rua EC, Gonzalez AB, Fuda JA, Meseri EI, Torti HE, Barrado J, Zubillaga MB, Lopez LB, Boccio JR (2010) Iron, zinc, and copper nutritional status in children infected with Helicobacter pylori. J Pediatr Gastroenterol Nutr 51(1):85–89. https://doi.org/10.1097/MPG.0b013e3181c2c2cd
Ozturk N, Kurt N, Ozgeris FB, Baygutalp NK, Tosun MS, Bakan N, Bakan E (2015) Serum zinc, copper, magnesium and selenium levels in children with helicobacter pylori infection. Eurasian J Med 47(2):126–129. https://doi.org/10.5152/eurasianjmed.2015.104
Dovhanj J, Kljaic K, Vcev A, Ilakovac V (2010) Helicobacter pylori and trace elements. Clin Lab 56(3–4):137–142
Yuan W, Yang N, Li X (2016) Advances in understanding how heavy metal pollution triggers gastric cancer. Biomed Res Int 2016:7825432–7825410. https://doi.org/10.1155/2016/7825432
Zhao Q, Wang Y, Cao Y, Chen A, Ren M, Ge Y, Yu Z, Wan S, Hu A, Bo Q, Ruan L, Chen H, Qin S, Chen W, Hu C, Tao F, Xu D, Xu J, Wen L, Li L (2014) Potential health risks of heavy metals in cultivated topsoil and grain, including correlations with human primary liver, lung and gastric cancer, in Anhui province, Eastern China. Sci Total Environ 470-471:340–347. https://doi.org/10.1016/j.scitotenv.2013.09.086
Liang C, Li Z, Xia X, Wang Q, Tao R, Tao Y, Xiang H, Tong S, Tao F (2017) Determine multiple elements simultaneously in the sera of umbilical cord blood samples—a very simple method. Biol Trace Elem Res 177(1):1–8. https://doi.org/10.1007/s12011-016-0853-6
Yuehong W, Zhu G, Nong X, Yijia W, Hua L (2005) A case-control study on the relationship between self-made foods and gastric cancer in rural areas. Ji bing kong zhi za zhi [Chin J Dis Control Prev] 9(5):387–389
Matsuda T, Tao H, Goto M, Yamada H, Suzuki M, Wu Y, Xiao N, He Q, Guo W, Cai Z, Kurabe N, Ishino K, Matsushima Y, Shinmura K, Konno H, Maekawa M, Wang Y, Sugimura H (2013) Lipid peroxidation-induced DNA adducts in human gastric mucosa. Carcinogenesis 34(1):121–127. https://doi.org/10.1093/carcin/bgs327
Cai X, Wang C, Yu W, Fan W, Wang S, Shen N, Wu P, Li X, Wang F (2016) Selenium exposure and cancer risk: an updated meta-analysis and meta-regression. Sci Rep 6:19213. https://doi.org/10.1038/srep19213
Qiao YL, Dawsey SM, Kamangar F, Fan JH, Abnet CC, Sun XD, Johnson LL, Gail MH, Dong ZW, Yu B, Mark SD, Taylor PR (2009) Total and cancer mortality after supplementation with vitamins and minerals: follow-up of the Linxian General Population Nutrition Intervention Trial. J Natl Cancer Inst 101(7):507–518. https://doi.org/10.1093/jnci/djp037
Compounds IoMUPoDAaR (2000) Selenium. In: Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. National Academies Press (US), Washington (DC). https://doi.org/10.17226/9810
Manz DH, Blanchette NL, Paul BT, Torti FM, Torti SV (2016) Iron and cancer: recent insights. Ann N Y Acad Sci 1368(1):149–161. https://doi.org/10.1111/nyas.13008
Wen CP, Lee JH, Tai YP, Wen C, Wu SB, Tsai MK, Hsieh DP, Chiang HC, Hsiung CA, Hsu CY, Wu X (2014) High serum iron is associated with increased cancer risk. Cancer Res 74(22):6589–6597. https://doi.org/10.1158/0008-5472.CAN-14-0360
Kisker C, Schindelin H, Rees DC (1997) Molybdenum-cofactor-containing enzymes: structure and mechanism. Annu Rev Biochem 66:233–267. https://doi.org/10.1146/annurev.biochem.66.1.233
Luo XM, Wei HJ, Yang SP (1983) Inhibitory effects of molybdenum on esophageal and forestomach carcinogenesis in rats. J Natl Cancer Inst 71(1):75–80
Cai L, Chen T, Yang J, Zhou K, Yan X, Chen W, Sun L, Li L, Qin S, Wang P, Yang P, Cui D, Burmeister M, He L, Jia W, Wan C (2015) Serum trace element differences between Schizophrenia patients and controls in the Han Chinese population. Sci Rep 5:15013. https://doi.org/10.1038/srep15013
Ceylan OM, Can Demirdogen B, Mumcuoglu T, Aykut O (2013) Evaluation of essential and toxic trace elements in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Biol Trace Elem Res 153(1–3):28–34. https://doi.org/10.1007/s12011-013-9644-5
Garcia-Esquinas E, Pollan M, Umans JG, Francesconi KA, Goessler W, Guallar E, Howard B, Farley J, Best LG, Navas-Acien A (2013) Arsenic exposure and cancer mortality in a US-based prospective cohort: the strong heart study. Cancer Epidemiol Biomark Prev 22(11):1944–1953. https://doi.org/10.1158/1055-9965.EPI-13-0234-T
Garcia-Esquinas E, Pollan M, Tellez-Plaza M, Francesconi KA, Goessler W, Guallar E, Umans JG, Yeh J, Best LG, Navas-Acien A (2014) Cadmium exposure and cancer mortality in a prospective cohort: the strong heart study. Environ Health Perspect 122(4):363–370. https://doi.org/10.1289/ehp.1306587
Berg JW, Burbank F (1972) Correlations between carcinogenic trace metals in water supplies and cancer mortality. Ann N Y Acad Sci 199:249–264
Lhotka C, Szekeres T, Steffan I, Zhuber K, Zweymuller K (2003) Four-year study of cobalt and chromium blood levels in patients managed with two different metal-on-metal total hip replacements. J Orthop Res 21(2):189–195. https://doi.org/10.1016/S0736-0266(02)00152-3
Hutter HP, Wallner P, Moshammer H, Marsh G (2016) Dust and cobalt levels in the Austrian tungsten industry: workplace and human biomonitoring data. Int J Environ Res Public Health 13(9):931. https://doi.org/10.3390/ijerph13090931
Lison D, De Boeck M, Verougstraete V, Kirsch-Volders M (2001) Update on the genotoxicity and carcinogenicity of cobalt compounds. Occup Environ Med 58(10):619–625
Liu LZ, Ding M, Zheng JZ, Zhu Y, Fenderson BA, Li B, Yu JJ, Jiang BH (2015) Tungsten carbide-cobalt nanoparticles induce reactive oxygen species, AKT, ERK, AP-1, NF-kappaB, VEGF, and angiogenesis. Biol Trace Elem Res 166(1):57–65. https://doi.org/10.1007/s12011-015-0331-6
Moulin JJ, Wild P, Romazini S, Lasfargues G, Peltier A, Bozec C, Deguerry P, Pellet F, Perdrix A (1998) Lung cancer risk in hard-metal workers. Am J Epidemiol 148(3):241–248
Sauni R, Oksa P, Uitti J, Linna A, Kerttula R, Pukkala E (2017) Cancer incidence among Finnish male cobalt production workers in 1969–2013: a cohort study. BMC Cancer 17(1):340. https://doi.org/10.1186/s12885-017-3333-2
Choi R, Kim HT, Lim Y, Kim MJ, Kwon OJ, Jeon K, Park HY, Jeong BH, Koh WJ, Lee SY (2015) Serum concentrations of trace elements in patients with tuberculosis and its association with treatment outcome. Nutrients 7(7):5969–5981. https://doi.org/10.3390/nu7075263
Karadas S, Sayin R, Aslan M, Gonullu H, Kati C, Dursun R, Duran L, Gonullu E, Demir H (2014) Serum levels of trace elements and heavy metals in patients with acute hemorrhagic stroke. J Membr Biol 247(2):175–180. https://doi.org/10.1007/s00232-013-9621-0
Mohmand J, Eqani SA, Fasola M, Alamdar A, Mustafa I, Ali N, Liu L, Peng S, Shen H (2015) Human exposure to toxic metals via contaminated dust: bio-accumulation trends and their potential risk estimation. Chemosphere 132:142–151. https://doi.org/10.1016/j.chemosphere.2015.03.004
Bruggraber SF, French G, Thompson RP, Powell JJ (2004) Selective and effective bactericidal activity of the cobalt (II) cation against Helicobacter pylori. Helicobacter 9(5):422–428. https://doi.org/10.1111/j.1083-4389.2004.00264.x
Jing C, Wang C, Yan K, Zhao K, Sheng G, Qu D, Niu F, Zhu H, You Z (2016) Synthesis, structures and urease inhibitory activity of cobalt(III) complexes with Schiff bases. Bioorg Med Chem 24(2):270–276. https://doi.org/10.1016/j.bmc.2015.12.013
Funding
This study was funded by the National Natural Science Foundation of China (No. 81502806) and Grant for Scientific Research of BSKY from Anhui Medical University (No. XJ201523).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study received ethical approval from the Ethics Institutional Review Board from the Anhui Medical University. Written informed consents were obtained from all participants before taking part in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hu, A., Li, L., Hu, C. et al. Serum Concentrations of 15 Elements Among Helicobacter Pylori-Infected Residents from Lujiang County with High Gastric Cancer Risk in Eastern China. Biol Trace Elem Res 186, 21–30 (2018). https://doi.org/10.1007/s12011-018-1283-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1283-4