Opinion statement
Convulsive status epilepticus (CSE) is a medical emergency with an associated high mortality and morbidity. It is defined as a convulsive seizure lasting more than 5 min or consecutive seizures without recovery of consciousness. Successful management of CSE depends on rapid administration of adequate doses of anti-epileptic drugs (AEDs). The exact choice of AED is less important than rapid treatment and early consideration of reversible etiologies. Current guidelines recommend the use of benzodiazepines (BNZ) as first-line treatment in CSE. Midazolam is effective and safe in the pre-hospital or home setting when administered intramuscularly (best evidence), buccally, or nasally (the latter two possibly faster acting than intramuscular (IM) but with lower levels of evidence). Regular use of home rescue medications such as nasal/buccal midazolam by patients and caregivers for prolonged seizures and seizure clusters may prevent SE, prevent emergency room visits, improve quality of life, and lower health care costs. Traditionally, phenytoin is the preferred second-line agent in treating CSE, but it is limited by hypotension, potential arrhythmias, allergies, drug interactions, and problems from extravasation. Intravenous valproate is an effective and safe alternative to phenytoin. Valproate is loaded intravenously rapidly and more safely than phenytoin, has broad-spectrum efficacy, and fewer acute side effects. Levetiracetam and lacosamide are well tolerated intravenous (IV) AEDs with fewer interactions, allergies, and contraindications, making them potentially attractive as second- or third-line agents in treating CSE. However, data are limited on their efficacy in CSE. Ketamine is probably effective in treating refractory CSE (RCSE), and may warrant earlier use; this requires further study. CSE should be treated aggressively and quickly, with confirmation of treatment success with epileptiform electroencephalographic (EEG), as a transition to non-convulsive status epilepticus is common. If the patient is not fully awake, EEG should be continued for at least 24 h. How aggressively to treat refractory non-convulsive SE (NCSE) or intermittent non-convulsive seizures is less clear and requires additional study. Refractory SE (RSE) usually requires anesthetic doses of anti-seizure medications. If an auto-immune or paraneoplastic etiology is suspected or no etiology can be identified (as with cryptogenic new onset refractory status epilepticus, known as NORSE), early treatment with immuno-modulatory agents is now recommended by many experts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The operational definition of status epilepticus (SE) describes an abnormally prolonged state of self-perpetuating seizure activity. The International League Against Epilepsy (ILAE) recently established a new definition of SE, as follows:
“Status epilepticus is a condition resulting either from the failure of the mechanisms responsible for seizure termination or from the initiation of mechanisms, which lead to abnormally, prolonged seizures (after time point t1). It is a condition, which can have long-term consequences (after time point t2), including neuronal death, neuronal injury, and alteration of neuronal networks, depending on the type and duration of seizure.” [1•]
For tonic-clonic seizures, t 1 describes the duration of seizure activity after which it is likely to continue if not treated—i.e., when it should be considered abnormally prolonged (or continuous) and requiring treatment. The second time point, or t 2, defines the length of continuous seizure activity after which there is a risk of long-term consequences. For generalized convulsive status epilepticus (CSE), t 1 is estimated to be 5 min, and t 2 30 min. For focal SE, t 1 is considered 10 min, and t 2 >60 min [1•].
Generally, SE is divided into convulsive and non-convulsive subtypes. Non-convulsive SE (NCSE) presents with variable levels of altered awareness in association with epileptiform electroencephalographic (EEG) patterns, but lacks a clinically obvious convulsive component. CSE can potentially evolve to NCSE, with 14 to 20 % of patients treated for CSE losing their clinical component, yet remaining in NCSE [2, 3]. Within 24 h of monitoring after CSE, about half (48 %) of patients will have non-convulsive seizures [2].
SE is the second most common neurologic emergency with an annual incidence of 10 to 41 cases per 100,000 persons, depending on geographic location [4–6]. Of these cases, anywhere from 45 to 74 % are classified in the convulsive subtype of SE [7].
In a recent review of the US hospital discharge diagnoses from 1979 to 2010, the incidence of SE increased from 3.5 to 12.5/100,000 people [8]. Dham et al. found the highest incidence of SE was in patients less than 10 years of age and those older than 50 (14.3/100,000 and 28.4/100,00, respectively). The mortality rate ranges from 7.2 % to nearly 20 % [8–10].
Along with age, the etiology of SE has been acknowledged as the most predictive prognostic factor. The etiologies of SE can be divided between acute symptomatic versus remote etiologies, such as stroke, central nervous infection, neoplasm, or traumatic brain injury [11].
Prolonged convulsive seizures have widespread detrimental systemic consequences both acutely and chronically [12]. A recent study found that 18 of 32 patients treated for CSE in the ICU setting met criteria for stress cardiomyopathy (Takotsubo cardiomyopathy) [13]. Manno et al. found in 2005 that patients who [14] died from SE had myocardial contraction band necrosis at a higher rate than controls [15]. Sub-acute complications include rhabdomyolysis, renal failure, pulmonary edema, and increased intracranial pressure [7, 16]. Muscle enzymes should always be checked the day after CSE (even if fairly brief) to make sure they are not markedly elevated; if they are, treatment and monitoring for renal failure are important.
Treatment
Early intervention to suppress seizure activity is the first priority of care, often warranting aggressive treatment. Delaying treatment leads to further refractoriness, as was shown by Kapur et al. They found that rats chemically induced into SE responded to diazepam easily if treated within 10 min of seizure onset. However, response to diazepam after 45 min of sustained seizure activity required nearly ten times the dose [17]. There is convincing evidence that this loss of effectiveness with delayed treatment occurs in humans as well, as shown in Fig. 1 [18, 19].
Cardiopulmonary support may be required when treating CSE. Stopping SE is the best way to avoid respiratory failure. Alldredge et al. found that giving pre-hospital benzodiazepines (BNZs) to treat CSE terminated seizures 43–59 % of the time on route to the hospital, versus 21 % for those who received placebo. Patients no longer in CSE upon arrival at the emergency room required significantly less respiratory support, with only 32 % requiring admission to the ICU versus 73 % for those still seizing [19]. Overall, respiratory failure was more common in patients randomized to placebo (16 %) than to either diazepam (9 %) or lorazepam (11 %). If neuromuscular blockade is needed for intubation, a short-acting non-depolarizing agent such as rocuronium bromide is preferred.
Pharmacological treatment
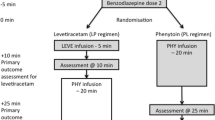
Modern treatment protocols take a staged approach. In 2012, the Neurocritical Care Society (NCS) guidelines for the evaluation and management of SE addressed the need for “emergent, targeted treatment to reduce patient morbidity and mortality.” They described the treatment of SE in three phases: emergent initial, urgent, and refractory therapies. Treatment of super-refractory SE can be considered the fourth stage of treatment [20••, 21].
Early SE calls for BNZs, preferably intravenous (IV); otherwise, intramuscular (IM), nasal, or buccal administration is acceptable if IV access is not available. One should not delay treatment while trying to obtain IV access [22••]. If seizures are refractory to treatment with BNZs, “established SE” is reached. Therapy with non-benzodiazepine IV anti-epileptic drugs (AEDs) is then indicated, usually with phenytoin or valproate; some protocols include IV phenobarbital, levetiracetam, or lacosamide as options. Many treatment protocols propose bypassing this step or simultaneously proceeding directly to anesthetic doses of BNZ, barbiturates, or propofol. If seizures continue despite full doses of two appropriate parenteral AEDs (including a BNZ), the patient is considered to be in refractory status epilepticus (RSE). At this point, anesthetic doses of medications are the standard of care [7, 20••, 21]. Continued SE beyond 24 h from seizure onset, despite anesthetic doses of medications, is considered super-refractory SE (SRSE). A suggested treatment algorithm (an updated version of the 2012 protocol at Yale-New Haven Hospital) is shown in Fig. 2.
Stage 1
Benzodiazepines
BNZ enhances neurotransmission of GABA at the GABAA receptor, increasing the frequency of chloride ion channel opening in response to GABA. IV lorazepam is generally the favored agent. Midazolam is the preferred medication for IM, nasal or buccal injection, and diazepam for rectal administration (and possibly nasal) [19]. Side effects are similar for most BNZ and include sedation (compounded by other CNS depressants), dizziness, weakness, unsteadiness, respiratory depression, and hypotension. Respiratory depression is more common in patients with underlying pulmonary disease [23•, 24].
Lorazepam
High-potency, intermediate-duration, 3-hydroxy BNZ is often used to treat anxiety disorders [25].
- Standard dose :
-
Initial dose of 0.1 mg/kg IV at a maximum of 2 mg/min; stop administering if seizures stop. Alternative dosing regimen for adults: 4 mg IV over 2 min; repeat once if still seizing.
- Contraindication to use :
-
Respiratory distress (if patient is still seizing and developing respiratory distress may need to intubate to enable safe administration).
- Main drug interactions :
-
Scopolamine—hallucinations and sedation; Valproate—reduces clearance of lorazepam.
- Common side effects :
-
See general BNZ side effects above.
- Special points :
-
Well-designed double-blinded studies established lorazepam as the initial drug of choice in treating CSE [3, 26], although IV diazepam is a reasonable alternative.
Midazolam
A short-acting BNZ.
- Standard dose :
-
IV—0.2 mg/kg bolus or 10 mg; repeat boluses until seizures stop.
IM—0.2 mg/kg or 10 mg once [27].
Nasal/buccal—0.2 mg/kg or 10 mg [28].
- Contraindications to use :
-
Include hypersensitivity. Caution must be observed with patients in hypotensive states, such as septic shock [29, 30].
- Main drug interactions :
-
CYP3A4 inhibiting medications such as erythromycin, diltiazem, ketoconazole, and cimetidine cause increased sedation.
- Common side effects :
-
See general BNZ side effects. The half-life is normally short (∼3 h), but with prolonged use, it increases, causing delayed arousal and potentially increased duration of ventilator support [31]. CNS depression is partly attributed to metabolite 1-hydroxymidazolam, which accumulates after hepatic oxidation [29, 30, 32].
- Special points :
-
In 2012, a double-blinded study done in the pre-hospital setting called RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial) was conducted. It randomized patients in CSE en route to the hospital to 10 mg of IM midazolam versus 4 mg of IV lorazepam. The study concluded IM midazolam was superior to IV lorazepam in subjects with CSE. The longer time to therapeutic effect and therapeutic serum concentrations for IM midazolam was more than offset by the time required to obtain IV access [22••, Class 1, level A]. Lorazepam has poor stability in unrefrigerated conditions, but midazolam does not [33]. The pediatric subgroup analysis of RAMPART showed both treatments were equally effective [34].
A recent retrospective review of non-IV treatments for CSE found IM and intranasal midazolam had the shortest times for treatment initiation and CSE termination when compared to other modalities [35•]. Additional studies support intranasal and buccal midazolam as effective abortive agents for terminating SE [14, 28, 36].
Diazepam
A long acting BNZ.
- Standard dose :
-
IV—0.15–0.4 mg/kg over 2 min or 10 mg IV over 2 min repeat if still seizing.
Nasal—adult, 10 mg, may repeat if still seizing [37].
- Main drug interactions :
-
See general BNZ side effects.
- Contraindications to use :
-
Severe liver disease. IV diazepam solution contains polyethylene glycol, which can contribute to metabolic acidosis [32].
- Special points :
-
Intranasal versus IV diazepam in a small cohort of stroke patients in CSE was recently reviewed. The intranasal group was administered diazepam nine times faster than the IV group (1 vs. 9.5 min), and seizure cessation was three times faster in the intranasal group (3 vs. 9.5 min) [37].
Stage 2
Second-line treatment in CSE
After BNZ are administered for emergent treatment of CSE, patients receive additional AEDs for maintenance therapy or as escalation in treatment to stop continued seizures. The NCS refers to these second-agent therapies as the “urgent treatment” phase of care [20••].
Large-scale and high-quality evidence is limited with regard to the particular agent of choice. In most recent guidelines, valproate reached evidence class IIa, evidence level A, with phenytoin class IIa, level B, and levetiracetam only at class IIb, level C ([20••], see [38] for classification details). Prospective, randomized controlled studies (level IIa, class B) on in-hospital treatment for CSE from the past decade are listed in Table 1.
A recent prospective pilot study comparing phenytoin, valproate, and levetiracetam following lorazepam in management of CSE, with 50 patients in each arm, concluded that all three AEDs were safe and roughly equally efficacious [43]. Three cases of postictal psychosis were seen, all in the levetiracetam arm. Yasiry and Shorvon compared the efficacy of 5 AED’s in BNZ-resistant CSE in a meta-analysis of prior studies. Valproate, levetiracetam and phenobarbital showed similar efficacy as first-line therapy. Authors concluded AED choice should depend on patient comorbidities and medication side effects. Their study did not support first-line use of phenytoin, and insufficient evidence existed to recommend using or avoiding lacosamide [44•].
Phenytoin and fosphenytoin
Phenytoin is a hydantoin-derivative AED that blocks voltage gated sodium channels. It is also a class 1b antiarrhythmic medication [45].
- Fosphenytoin :
-
A phosphate ester pro-drug of phenytoin developed as an alternative to IV phenytoin. Fosphenytoin is water-soluble allowing easier and faster administration. It is dephosphorylated in the blood to phenytoin with a 15-min conversion half-life.
- Standard dose :
-
18–20 mg/kg IV of phenytoin, or phenytoin-equivalents for fosphenytoin. Maximal phenytoin infusion is 50 mg/min, while fosphenytoin is given up to 150 mg/min.
- Contraindications to use :
-
Bradycardia, sino-atrial block, second- and third-degree atrio-ventricular block [46, 47]. A black box warning exists for cardiovascular risk with rapid infusions.
- Main drug interaction :
-
Strong inducer of CYP3A4 and CYP2C19, affecting metabolism of steroids, chemotherapeutic agents, immuno-suppressants, HIV medications, statins and anti-hypertensives, among many others [46].
- Common side effects :
-
Infusion rate-related hypotension, ataxia, dizziness, diplopia.
- Special points :
-
Overall fosphenytoin is preferable to phenytoin for IV use in SE as it is more rapidly infused, causes hypotension less commonly, does not necrotize tissue if it extravasates, is compatible with all IV fluids, and results in therapeutic free phenytoin levels slightly faster. IM fosphenytoin is not recommended in SE due to slow absorption, but is otherwise useful [48].
Valproate
Valproate is an organic acid compound that prolongs sodium channel inactivation, attenuates calcium mediated transient currents and augments GABA. Its efficacy in treating CSE is well established [20••, 49], with equal [40, 42, 43] or superior [39, 50] efficacy versus IV phenytoin in prospective, randomized trials.
- Standard dose :
-
20–40 mg/kg IV bolus at 6 mg/kg/min; we recommend the higher dose of 40 mg/kg for CSE, which typically results in a peak level just over 100. An additional 20 mg/kg bolus can be given as well. A prior study found loading doses as high as 79 mg/kg had no related adverse effects [51].
- Contraindications to use :
-
Pregnancy, mitochondrial disease, pre-existing acute or chronic liver dysfunction, porphyria and urea cycle disorder thrombocytopenia, and possibly recent or potentially ongoing intracranial bleeding [52].
- Main drug interactions :
-
Topiramate—risk of hypothermia, hyperammonemia, and hepatic failure in conjunction with valproate [53]; Salicylic acid—decreases valproate metabolism; Carbapenem antibiotics and P450 inducing medications such as phenytoin, carbamazepine, phenobarbital, and rifampin lower valproate levels, sometimes dramatically. Valproate decreases metabolism of lamotrigine, warfarin, and others.
- Common side effects :
-
Hepatic dysfunction, hyperammonemia (often asymptomatic), gastrointestinal symptoms, hormonal disturbances and weight gain [52]. Valproate is associated with teratogenicity, lower IQ and autism in children exposed in utero [54]. Can cause dose-dependent thrombocytopenia, and possibly increased bleeding despite normal platelet count. We try to avoid valproate in patients with intracranial bleeding or those requiring neurosurgical intervention.
- Special points :
-
In a randomized prospective study comparing IV phenytoin and IV valproate in SE, valproate aborted SE 66 % of the time and phenytoin in 42 % of cases (p = 0.046) when used as first-line treatment without use of BNZ. When crossed over after failing the other drug, valproate was effective in 79 % of patients, whereas phenytoin was effective 25 % of the time (p = 0.004). Side effects between the two groups did not differ. The study concluded that valproate may be preferred in CSE [39]. A second prospective randomized trial compared IV valproate versus IV phenytoin in benzodiazepine refractory CSE. They found similar efficacy between the two AEDs; however, the valproate dose was only 20 mg/kg IV. No statistical difference in adverse effects was seen [40]. A systematic review comparing IV phenytoin and IV valproate in treating CSE concluded similar findings [55]. Valproate was the most effective agent in a retrospective study comparing phenytoin, valproate and levetiracetam in patients who failed initial treatment for CSE with a standardized BNZ protocol. Authors found valproate failed to stop seizures 25.4 % of the time, compared to phenytoin (41.4 %) and levetiracetam (48.3 %) [50].
Levetiracetam
Levetiracetam binds to synaptic vesicle glycoprotein SV2A, inhibiting presynaptic calcium channels, thereby reducing neurotransmitter release [56]. Levetiracetam enhances supply rate depression on presynaptic vesicle trafficking, regulating synaptic activity during times of increased activation [57].
- Standard dose :
-
1500–4000 mg IV as a loading dose in adults [20••]; we prefer 2500–4000 mg [58].
- Contraindications to use :
-
None; possibly psychiatric history.
- Main drug interactions :
-
None.
- Common side effects :
-
Dizziness, irritability, somnolence, agitation, depression [27].
- Special points :
-
A prospective, randomized study compared levetiracetam to lorazepam in CSE as first-line treatment. They concluded that levetiracetam is an effective alternative to lorazepam, and may be preferred in patients with respiratory failure or severe hypotension [23•]. Phenytoin was compared to levetiracetam for second-line treatment of CSE in a prospective, randomized trial. Authors found levetiracetam was similarly effective as phenytoin, with the advantage of easier administration, favorable adverse effect profile and pharmacokinetics [41].
A prospective observational study assessed the effectiveness of IV levetiracetam after BNZ use. They concluded that IV levetiracetam is suitable as second-line treatment after BNZ in treating SE, given its efficacy, ease of usage and safety [59]. A meta-analysis by Zeid and Shorvon found no statistical difference between levetiracetam, valproate and phenobarbital at terminating SE. The efficacy rates were 68.5, 75.7 and 73.6 %, respectively [44•].
Phenobarbital
Phenobarbital is a long-acting barbiturate that binds to the GABA receptor, increases chloride conductivity and decreases neuronal excitability. It may also directly block excitatory glutamate signaling by antagonizing NMDA receptors [11, 60].
- Standard dose :
-
20 mg/kg IV bolus up to 50 mg/min.
- Contraindications :
-
Acute intermittent porphyria, family history of porphyria, prior barbiturate dependence, severe respiratory insufficiency, severe hypotension, poor cardiac output, myxedema, Addison’s disease, hepatic disease [32, 46].
- Main drug interactions :
-
Induces the CYP P450 system. Caution with medications metabolized via this mechanism, as discussed in the phenytoin section [46]. Valproate increases serum levels. Additive sedation and respiratory drive reduction with CNS depressants, such as BNZ, narcotics, and phenothiazines.
- Common side effects :
-
Sedation, rash, respiratory depression and hypotension [20••, 46]. Acid-base disturbances can occur with continuous infusions as propylene glycol is in the IV formulation [61]. Its half-life of 53–118 h can prolong sedation, length of stay, and ventilator dependence [46].
- Special points :
-
The double-blinded and randomized VA Cooperative Study showed no difference in controlling SE between phenobarbital and lorazepam or the combination of phenytoin plus diazepam [3].
A prospective study comparing IV valproate to IV phenobarbital for treatment of pediatric CSE found that phenobarbital terminated seizure activity 77 % of the time, while valproate was successful in 90 % of cases. Adverse effects were experienced in 74 % of phenobarbital treated patients, and only 24 % of valproate patients [42]. A review in 2013 compared IV valproate versus IV phenobarbital for treating CSE. They found similar efficacy at terminating seizure activity, with a better adverse effect profile for valproate [62].
Lacosamide
Lacosamide is a functionalized amino acid that enhances slow inactivation of voltage-gated sodium channels [63].
- Standard dose :
-
200–400 mg IV is a common bolus dose. [64].
- Contraindications :
-
Cardiac arrhythmia [46, 65] PR interval prolongation. However, a recent randomized, double blinded, placebo controlled study compared healthy volunteers on up to 800 mg lacosamide per day and found no significant change in QTc or PR interval [65].
- Main drug interactions :
-
Valproate increases serum levels. Calcium channel and β-blockers may potentiate PR interval prolongation.
- Common side effects :
-
Dizziness, ataxia, nausea, diplopia.
- Special points :
-
A review from 2013 analyzed reports of the use of lacosamide in RSE. Lacosamide terminated RSE in 76/136 (56 %) of all cases, and ceased refractory CSE (RCSE) in 5/8 (63 %) patients. Lacosamide doses were not standardized and the adverse effect profile was favorable [66]. A second review compared IV lacosamide to IV phenytoin for RSE. Authors found that lacosamide was equally effective as phenytoin in terminating RSE. RCSE was diagnosed in 12 of 46 patients, but no subgroup analysis was performed. The patients on phenytoin had significant adverse effects 27 % of the time versus none in the lacosamide group [67]. A multi-center, prospective study investigated lacosamide as add-on treatment in RSE, but only included 1 of 34 patients in RCSE. For other types of RSE (i.e., non-convulsive), authors found lacosamide to be efficacious and safe [68].
In a preliminary report of a recent prospective, randomized trial of fosphenytoin versus lacosamide for recurrent non-convulsive seizures (the TRENdS trial), lacosamide was shown to be non-inferior to fosphenytoin in controlling seizures (controlled in 62 % with lacosamide versus 50 % with fosphenytoin, not statistically significant), and equally well tolerated [69].
Refractory status epilepticus and super-refractory status epilepticus
RSE is defined as ongoing or recurrent seizures without recovery of consciousness or return to baseline for at least 30 min, persisting after first- and second-line AEDs. RSE accounts for 35–40 % of SE cases [70]. Super-refractory status epilepticus is defined as SE that continues or recurs 24 h or more after the onset of anesthetic therapy [21] .
Midazolam
A benzodiazepine used as first-line treatment for RSE, as described above. Tachyphylaxis may occur [11, 71].
- Standard dose :
-
0.2 mg/kg bolus IV, repeated 5 min until seizures stop (max of 10 boluses), then maintenance infusion of 0.1 mg/kg/h – 2.9 mg/kg/h.
- Special points :
-
A retrospective observational study compared 2 treatment protocols for continuous IV midazolam infusions, including low (maximum 0.4 mg/kg/h median 0.2 mg/kg/h) versus high dose (maximum 2.9 mg/kg/h median 0.4 mg/kg/h) regimens. Authors found equivalent safety of both treatment regimens, lower seizure recurrence after midazolam discontinuation in the high dose group, and significantly lower mortality in the high dose group. This study provides Class III evidence that midazolam at higher infusion rates (when necessary for seizure control) is associated with reduced seizure recurrence and possibly lower mortality [72•].
Propofol
Propofol is a short-acting IV anesthetic/hypnotic agent. It activates GABAA receptors, inhibits NMDA receptors and modulates calcium influx through slow calcium ion channels [32, 73].
- Standard dose :
-
1–2 mg/kg IV push, repeated every 3–5 min until seizures stop (maximum 10 mg/kg) followed by 33 μg/kg/min (1.98 mg/kg/h) initial IV infusion rate. Maintenance dose of 17–250 μg/kg/min (1.02–15 mg/kg/h) [11, 20••].
- Common side effects :
-
Hypotension, transient apnea following bolus, myoclonus, and innate immune system dysfunction [32, 74, 75].
- Contraindications :
-
The respiratory effects of propofol are potentiated by other respiratory depressants.
- Main drug interactions :
-
Fentanyl may cause bradycardia. Vasoconstrictors, corticosteroids, and inotropes increase the chance of propofol infusion syndrome (PRIS). Carbonic anhydrase inhibitors (including zonisamide, topiramate, acetazolamide)—increase the risk of severe acidosis.
- Special points :
-
PRIS includes cardio-circulatory collapse, lactic acidosis, hypertriglyceridemia and rhabdomyolysis, occurring with prolonged use especially in children. If used for more than a few hours monitor pH, CK, and triglycerides, among other parameters [32, 71, 73]. We try to avoid use of more than 5 mg/kg for more than 24–48 h due to the risk of PRIS. Combining propofol with a benzodiazepine infusion may enable use of lower doses, thereby increasing efficacy and lowering risk of PRIS.
Barbiturate (sodium thiopental and pentobarbital)
Sodium thiopental is a rapid-onset short-acting barbiturate general anesthetic.
- Standard dosage :
-
Thiopental loading dose is 1–2 mg/kg IV and 1–5 mg/kg/h maintenance dose [11].
Pentobarbital loading dose is 5 mg/kg IV and maintenance of 1–5 mg/kg/h [20••].
- Common side effects :
-
Similar adverse effects as phenobarbital.
- Contraindications :
-
Similar contraindications as phenobarbital.
- Main drug interactions :
-
Similar to the drug interactions of phenobarbital.
Ketamine
An N-methyl-d-aspartate (NMDA) receptor antagonist.
- Standard dosage :
-
Load: 1.5 mg/kg IV every 3–5 min until seizures stop (max 4.5 mg/kg). Initial infusion 1.2 mg/kg/h, maintenance 0.3–7.5 mg/kg/h.
- Common side effects :
-
Tachycardia, hypertension, possible increased intracranial pressure in patients with compromised cerebral auto-regulation [76]. Sedation with additional CNS depressant medications.
- Contraindications :
-
Neurotoxicity on CNS development in animal studies. Several retrospective studies found no statistically significant effect on neurodevelopment in human infants after ketamine was used in cardiac surgery [21, 77]. Elevated intracranial pressure.
- Main drug interactions :
-
None.
- Special points :
-
A handful of studies demonstrate efficacy and safety of ketamine for the treatment of RSE and SRSE [76, 78•]. Ketamine is not associated with cardiorespiratory depression and is used successfully in hemodynamically compromised patients.
A retrospective analysis found ketamine terminated RCSE in 14/19 (74 %) episodes in 13 patients. Importantly, 5/13 patients avoided traditional anesthetics and endotracheal intubation [79] .
A large multi-center trial retrospectively investigated efficacy and safety of IV ketamine for RSE from 1999 to 2012. Of 60 patients (46 adults, 12 children), 32 % achieved seizure control shortly after treatment. Adverse effects occurred in 36 (60 %) patients prior to ketamine infusion, and 18 (30 %) afterwards. Of those patients, raised intracranial pressure was seen in 3 (5 %) prior to receiving ketamine and 2 (3 %) after the infusion [78•].
Lidocaine
Sodium channel antagonist and class Ib anti-arrhythmic agent.
- Standard dosage :
-
Bolus of 100–400 mg IV followed by 1–3 mg/kg, or a continuous 2–4 mg/kg/h infusion without bolus [80].
- Common side effects :
-
Metallic taste, lightheadedness, confusion, tremors, shivering, tinnitus, bradycardia [81, 82]. Two reported cases of hypotension and two cases of cardiorespiratory arrest after bolus doses [80].
- Contraindications :
-
Allergy to amide anesthetic agents. Some centers include liver failure, severe heart failure, second- or third-degree heart block, systolic blood pressure >160 mmHg and hypokalemia [82].
- Main drug interactions :
-
Decreased clearance with β-blockers and cimetidine. Tocainide use with lidocaine may exacerbate seizures [83].
- Special points :
-
The majority of data studying lidocaine in the setting of SE is in the pediatric realm. A recent review found that adults responded well to lidocaine, and SE was terminated 70 % of the time. The vast majority of patients had phenytoin on board prior to infusing lidocaine. Authors concluded that further study is needed to evaluate the utility of lidocaine for RSE in adults [80].
Immuno-modulatory treatments
New onset refractory status epilepticus (NORSE) accounts for approximately 40 % of RSE cases. Gaspard et al. found that of 130 cases, 48 (37 %) were autoimmune or paraneoplastic in nature, 67 (52 %) remained cryptogenic after extensive evaluations, and a total of 19 (15 %) patients initially presented as RCSE [84•]. Khawaja et al. found of 11 patients diagnosed with NORSE, 8 treated with immuno-modulatory treatments had better outcomes than 3 patients not treated [85]. Early immuno-modulatory treatment, including high-dose parenteral corticosteroids, intravenous immunoglobulin, and plasmapheresis, is increasingly becoming a mainstay of treatment in these cases, in addition to traditional anti-epileptic agents [76]. These treatment modalities were discussed previously in Lopinto-Khoury and Sperlings review of autoimmune epilepsy in 2013 [86]. No randomized, double blinded case-control clinical trials currently exist.
Emerging therapies
Pharmacological therapy
Allopregnanolone
Allopregnanolone is a neurosteroid that modulates synaptic and extra-synaptic GABAA receptors. Case reports in adults and children show efficacy in treating SRSE; however, none had documented CSE [87]. A clinical trial is currently underway.
Standard enteral treatments and studies worth mentioning
The ongoing Established Status Epilepticus Treatment Trial (ESETT) is comparing the effectiveness of valproate, phenytoin, and levetiracetam in treating established SE (trial number NCT01960075 at https://clinicaltrials.gov). Topiramate is a potent broad-spectrum AED that blocks ionotropic glutamatergic AMPA receptors, theorized to be a potent target for SE treatment. Enterically administered topiramate was used in studies to treat CSE. A total of 24 patients were treated of whom 6 (25 %) responded rapidly, and 11 (46 %) had a possible response within several hours of treatment [88, 89]. Topiramate showed good safety, tolerability, and had a limited side effect profile. Perampanel is a non-competitive AMPA-receptor antagonist theoretically effective at regulating the glutamate overload associated with RSE. Two retrospective analyses, totaling 21 patients, showed possible efficacy of perampanel in treating NCSE and epilepsia partialis continua, but none of the patients were in CSE [90, 91]. A few studies investigated the use of IV clonazepam (available in Europe) in SE showing effectiveness as first-line therapy [92–94]. Intravenous magnesium sulfate is a well-established treatment for convulsive seizures related to eclampsia. However, its utility for SE and RSE due to other etiologies remains unknown. A recent review found 50 % of patients had a reduced seizure rate or termination of their SE after infusion of magnesium sulfate [95]. A review of inhalational anesthetics found that isoflurane was highly effective at ceasing SE and inducing burst suppression [96]. Sivakumar et. al found that clobazam had effectiveness in controlling RSE in a recent review, where of 17 patients, 9 were in CSE and 7 had a good response to treatment [97]. Valnoctamide is a new, less teratogenic derivative of valproate in development; it suppresses electrographic seizures in animal models of SE. Valnoctamide acts through different binding sites than BZDs, which likely accounts for its effect on BZD-refractory SE [98, 99].
Non pharmacological therapy
Hypothermia
Hypothermia activates many anticonvulsant and neuroprotective mechanisms [100]. A recent systematic review found very low-grade evidence to support the use of therapeutic hypothermia in RSE [100]. Underlying seizure type was not described. The well-tolerated level of hypothermia used in humans has minimal effect on the EEG, and deeper levels, which are neuroprotective and strongly anti-seizure in animal models, may be unsafe.
Vagus nerve stimulation
In a review of the literature, 28 patients had VNS placed urgently in the setting of RSE. It is unclear what percentage had CSE. Authors found 76 % of patients with generalized SE had seizure control after VNS; however, only 25 % of patients in focal status epilepticus became controlled [101].
Resective surgery
Surgical procedures for SRSE were usually tailored focal cortical resections, but wider resections are viable treatment options in some patients with RSE due to focal pathologies, particularly cortical dysplasia [102]. In a study of children with RSE, seizures were terminated acutely by resective epilepsy surgery in all 10 patients with no mortality or substantial morbidity. At follow-up (median 7 months), 7 of 10 patients were seizure free, while 3 had significant improvement in their epilepsy [103]. A review article found 15 patients treated with resective surgeries for RSE, where all patients experienced cessation of their seizures. Neurologic deficits, including hemiparesis and dysphasia, occurred in four patients [104].
Ketogenic diet
Several studies have found success in treating adults and children for RSE in the inpatient setting [105, 106]. Thakur et al. found of nine patients, who achieved ketosis, all had seizure termination within 3 days of starting the diet. However, patients had already been treated with several AEDs and the average length of RSE prior to initiation of KD was 21 days. The type of SE was not specified. Further research is needed to assess the value of the KD in RCSE; preliminary results are promising.
Conclusion
Progress is being made in determining the best treatment protocol for CSE. BNZ’s remain established as first-line treatment. Recent studies proved the utility of IM, nasal and buccal BNZ in cases where IV access is not obtainable, including in the pre-hospital setting. VPA is effective at treating CSE—at least as effective as phenytoin and better tolerated. LEV has increasing evidence supporting it as an effective treatment option, but further study is needed. Prospective, blinded, head to head trials are largely lacking; results of the pending ESETT trial will hopefully break this trend, at least for three commonly used agents (valproate, phenytoin, and levetiracetam). In cases of unexplained RSE of any type with no obvious cause after a couple of days, this qualifies as NORSE; evidence is emerging that immuno-modulatory treatment may be beneficial in these cases, especially when given early. Ketamine is probably effective in treating RCSE and may warrant earlier use; this requires further study. The ketogenic diet and surgery have roles in selected severe cases.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Trinka E et al. A definition and classification of status epilepticus—report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015;56(10):1515–23. Comprehensive review of seizure types and definitions by world experts.
DeLorenzo RJ et al. Persistent nonconvulsive status epilepticus after the control of convulsive status epilepticus. Epilepsia. 1998;39(8):833–40.
Treiman DM et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339(12):792–8.
DeLorenzo RJ et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond. Virginia Neurol. 1996;46(4):1029–35.
Hesdorffer DC et al. Incidence of status epilepticus in Rochester, Minnesota, 1965–1984. Neurology. 1998;50(3):735–41.
Logroscino G et al. Time trends in incidence, mortality, and case-fatality after first episode of status epilepticus. Epilepsia. 2001;42(8):1031–5.
Betjemann JP, Lowenstein DH. Status epilepticus in adults. Lancet Neurol. 2015;14(6):615–24.
Dham BS, Hunter K, Rincon F. The epidemiology of status epilepticus in the United States. Neurocrit Care. 2014;20(3):476–83.
Logroscino G et al. Short-term mortality after a first episode of status epilepticus. Epilepsia. 1997;38(12):1344–9.
Logroscino G et al. Mortality after a first episode of status epilepticus in the United States and Europe. Epilepsia. 2005;46 Suppl 11:46–8.
Rossetti AO, Lowenstein DH. Management of refractory status epilepticus in adults: still more questions than answers. Lancet Neurol. 2011;10(10):922–30.
Foreman B, Hirsch LJ. Epilepsy emergencies: diagnosis and management. Neurol Clin. 2012;30(1):11–41. vii.
Belcour D et al. Prevalence and risk factors of stress cardiomyopathy after convulsive status epilepticus in ICU patients. Crit Care Med. 2015;43(10):2164–70.
Kalviainen R. Intranasal therapies for acute seizures. Epilepsy Behav. 2015;49:303–6.
Manno EM et al. Cardiac pathology in status epilepticus. Ann Neurol. 2005;58(6):954–7.
Vooturi S et al. Prognosis and predictors of outcome of refractory generalized convulsive status epilepticus in adults treated in neurointensive care unit. Clin Neurol Neurosurg. 2014;126:7–10.
Kapur J, Macdonald RL. Rapid seizure-induced reduction of benzodiazepine and Zn2+ sensitivity of hippocampal dentate granule cell GABAA receptors. J Neurosci. 1997;17(19):7532–40.
Hillman J et al. Clinical significance of treatment delay in status epilepticus. Int J Emerg Med. 2013;6(1):6.
Alldredge BK et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345(9):631–7.
Brophy GM et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23. Provides the standard evidence based guidelines in managing SE, from the Neurocritical Care Society.
Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134(Pt 10):2802–18.
Silbergleit R et al. Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med. 2012;366(7):591–600. Provides class 1 evidence supporting treatment of SE with IM midazolam. Underscores the importance of rapid administration of anti-epileptic medications.
Misra UK, Kalita J, Maurya PK. Levetiracetam versus lorazepam in status epilepticus: a randomized, open labeled pilot study. J Neurol. 2012;259(4):645–8. A prospective, randomized study pitting lorazepam versus levetiracetam as first line treatment of SE. Authors found levetiracetam to be similiarly effective as lorazepam. This study needs to be replicated.
Gillies D et al. Benzodiazepines alone or in combination with antipsychotic drugs for acute psychosis. Cochrane Database Syst Rev. 2005;4:CD003079.
Ameer B, Greenblatt DJ. Lorazepam: a review of its clinical pharmacological properties and therapeutic uses. Drugs. 1981;21(3):162–200.
Leppik IE et al. Double-blind study of lorazepam and diazepam in status epilepticus. JAMA. 1983;249(11):1452–4.
Verrotti A et al. The adverse event profile of levetiracetam: a meta-analysis on children and adults. Seizure. 2015;31:49–55.
Brigo F et al. A common reference-based indirect comparison meta-analysis of buccal versus intranasal midazolam for early status epilepticus. CNS Drugs. 2015;29(9):741–57.
Shafer A. Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens. Crit Care Med. 1998;26(5):947–56.
Zhou Y et al. Midazolam and propofol used alone or sequentially for long-term sedation in critically ill, mechanically ventilated patients: a prospective, randomized study. Crit Care. 2014;18(3):R122.
Spina SP, Ensom MH. Clinical pharmacokinetic monitoring of midazolam in critically ill patients. Pharmacotherapy. 2007;27(3):389–98.
Devlin JW, Mallow-Corbett S, Riker RR. Adverse drug events associated with the use of analgesics, sedatives, and antipsychotics in the intensive care unit. Crit Care Med. 2010;38(6 Suppl):S231–43.
De Winter S et al. Impact of temperature exposure on stability of drugs in a real-world out-of-hospital setting. Ann Emerg Med. 2013;62(4):380–7. e1.
Welch RD et al. Intramuscular midazolam versus intravenous lorazepam for the prehospital treatment of status epilepticus in the pediatric population. Epilepsia. 2015;56(2):254–62.
Arya R et al. Efficacy of nonvenous medications for acute convulsive seizures: a network meta-analysis. Neurology. 2015;85(21):1859–68. Interesting analysis of available non-venous treatment modalities for acute convulsive seizures. Adds to the building evidence supporting the use of intranasal or buccal midazolam in this setting.
Brigo F et al. Nonintravenous midazolam versus intravenous or rectal diazepam for the treatment of early status epilepticus: a systematic review with meta-analysis. Epilepsy Behav. 2015;49:325–36.
Inokuchi R et al. Comparison of intranasal and intravenous diazepam on status epilepticus in stroke patients: a retrospective cohort study. Medicine (Baltimore). 2015;94(7):e555.
Gibbons RJ et al. American College of Cardiology/American Heart Association clinical practice guidelines: part I: where do they come from? Circulation. 2003;107(23):2979–86.
Misra UK, Kalita J, Patel R. Sodium valproate vs phenytoin in status epilepticus: a pilot study. Neurology. 2006;67(2):340–2.
Agarwal P et al. Randomized study of intravenous valproate and phenytoin in status epilepticus. Seizure. 2007;16(6):527–32.
Chakravarthi S et al. Levetiracetam versus phenytoin in management of status epilepticus. J Clin Neurosci. 2015;22(6):959–63.
Malamiri RA et al. Efficacy and safety of intravenous sodium valproate versus phenobarbital in controlling convulsive status epilepticus and acute prolonged convulsive seizures in children: a randomised trial. Eur J Paediatr Neurol. 2012;16(5):536–41.
Mundlamuri RC et al. Management of generalised convulsive status epilepticus (SE): a prospective randomised controlled study of combined treatment with intravenous lorazepam with either phenytoin, sodium valproate or levetiracetam—pilot study. Epilepsy Res. 2015;114:52–8.
Yasiry Z, Shorvon SD. The relative effectiveness of five antiepileptic drugs in treatment of benzodiazepine-resistant convulsive status epilepticus: a meta-analysis of published studies. Seizure. 2014;23(3):167–74. Interesting meta-analysis with strict inclusion criteria. Authors concluded that phenytoin should not be considered before valproic acid, levetiracetam and phenobarbital in the treatment of RSE.
Rogawski MA, Loscher W. The neurobiology of antiepileptic drugs. Nat Rev Neurosci. 2004;5(7):553–64.
Perucca P, Gilliam FG. Adverse effects of antiepileptic drugs. Lancet Neurol. 2012;11(9):792–802.
Frend V, Chetty M. Dosing and therapeutic monitoring of phenytoin in young adults after neurotrauma: are current practices relevant? Clin Neuropharmacol. 2007;30(6):362–9.
Cook AM et al. Practice variations in the management of status epilepticus. Neurocrit Care. 2012;17(1):24–30.
Kay HY et al. M-current preservation contributes to anticonvulsant effects of valproic acid. J Clin Invest. 2015;125(10):3904–14.
Alvarez V et al. Second-line status epilepticus treatment: comparison of phenytoin, valproate, and levetiracetam. Epilepsia. 2011;52(7):1292–6.
Limdi NA et al. Efficacy of rapid IV administration of valproic acid for status epilepticus. Neurology. 2005;64(2):353–5.
Nanau RM, Neuman MG. Adverse drug reactions induced by valproic acid. Clin Biochem. 2013;46(15):1323–38.
Knudsen JF, Sokol GH, Flowers CM. Adjunctive topiramate enhances the risk of hypothermia associated with valproic acid therapy. J Clin Pharm Ther. 2008;33(5):513–9.
Hernandez-Diaz S et al. Comparative safety of antiepileptic drugs during pregnancy. Neurology. 2012;78(21):1692–9.
Brigo F et al. IV Valproate in generalized convulsive status epilepticus: a systematic review. Eur J Neurol. 2012;19(9):1180–91.
Rogawski MA. Diverse mechanisms of antiepileptic drugs in the development pipeline. Epilepsy Res. 2006;69(3):273–94.
Garcia-Perez E et al. Levetiracetam accelerates the onset of supply rate depression in synaptic vesicle trafficking. Epilepsia. 2015;56(4):535–45.
Patsalos PN. Pharmacokinetic profile of levetiracetam: toward ideal characteristics. Pharmacol Ther. 2000;85(2):77–85.
Atmaca MM et al. Intravenous levetiracetam treatment in status epilepticus: a prospective study. Epilepsy Res. 2015;114:13–22.
Loscher W, Rogawski MA. How theories evolved concerning the mechanism of action of barbiturates. Epilepsia. 2012;53 Suppl 8:12–25.
Bledsoe KA, Kramer AH. Propylene glycol toxicity complicating use of barbiturate coma. Neurocrit Care. 2008;9(1):122–4.
Brigo F et al. A common reference-based indirect comparison meta-analysis of intravenous valproate versus intravenous phenobarbitone for convulsive status epilepticus. Epileptic Disord. 2013;15(3):314–23.
Rogawski MA et al. Current understanding of the mechanism of action of the antiepileptic drug lacosamide. Epilepsy Res. 2015;110:189–205.
Cross SA, Curran MP. Lacosamide: in partial-onset seizures. Drugs. 2009;69(4):449–59.
Kropeit D et al. Lacosamide cardiac safety: a thorough QT/QTc trial in healthy volunteers. Acta Neurol Scand. 2015;132(5):346–54.
Hofler J, Trinka E. Lacosamide as a new treatment option in status epilepticus. Epilepsia. 2013;54(3):393–404.
Kellinghaus C, Berning S, Stogbauer F. Intravenous lacosamide or phenytoin for treatment of refractory status epilepticus. Acta Neurol Scand. 2014;129(5):294–9.
Miro J et al. Efficacy of intravenous lacosamide as an add-on treatment in refractory status epilepticus: a multicentric prospective study. Seizure. 2013;22(1):77–9.
Husain A. The TRENdS trial: Intravenous lacosamide versus fosphenytoin for the treatment of frequent nonconvulsive seizures in critically ill patients. Late breaking abstract American Epilepsy Society 2015, 2015.
Moseley BD, Degiorgio CM. Refractory status epilepticus treated with trigeminal nerve stimulation. Epilepsy Res. 2014;108(3):600–3.
Rossetti AO. Which anesthetic should be used in the treatment of refractory status epilepticus? Epilepsia. 2007;48 Suppl 8:52–5.
Fernandez A et al. High-dose midazolam infusion for refractory status epilepticus. Neurology. 2014;82(4):359–65. Provides evidence supporting high dose midazolam in treating RSE. Showed better outcomes in the high dose midazolam group, and shed light on the safety profile at such high doses.
Marik PE. Propofol: therapeutic indications and side-effects. Curr Pharm Des. 2004;10(29):3639–49.
Matta JA et al. General anesthetics activate a nociceptive ion channel to enhance pain and inflammation. Proc Natl Acad Sci U S A. 2008;105(25):8784–9.
Robinson BJ et al. Mechanisms whereby propofol mediates peripheral vasodilation in humans. Sympathoinhibition or direct vascular relaxation? Anesthesiology. 1997;86(1):64–72.
Bayrlee A et al. Treatment of super-refractory status epilepticus. Curr Neurol Neurosci Rep. 2015;15(10):66.
Yan J, Jiang H. Dual effects of ketamine: neurotoxicity versus neuroprotection in anesthesia for the developing brain. J Neurosurg Anesthesiol. 2014;26(2):155–60.
Gaspard N et al. Intravenous ketamine for the treatment of refractory status epilepticus: a retrospective multicenter study. Epilepsia. 2013;54(8):1498–503. Although retrospective, this large multicenter study found ketamine to be relatively safe and somewhat effective for treating RSE.
Ilvento L et al. Ketamine in refractory convulsive status epilepticus in children avoids endotracheal intubation. Epilepsy Behav. 2015;49:343–6.
Zeiler FA et al. Lidocaine for status epilepticus in adults. Seizure. 2015;31:41–8.
Achar S, Kundu S. Principles of office anesthesia: part I. Infiltrative anesthesia. Am Fam Physician. 2002;66(1):91–4.
Peixoto RD, Hawley P. Intravenous lidocaine for cancer pain without electrocardiographic monitoring: a retrospective review. J Palliat Med. 2015;18(4):373–7.
Forrence E, Covinsky JO, Mullen C. A seizure induced by concurrent lidocaine-tocainide therapy—is it just a case of additive toxicity? Drug Intell Clin Pharm. 1986;20(1):56–9.
Gaspard N et al. New-onset refractory status epilepticus: etiology, clinical features, and outcome. Neurology. 2015;85(18):1604–13. Reviews the clinical features of NORSE and highlights its diverse etiologies, especially autoimmune.
Khawaja AM et al. New-onset refractory status epilepticus (NORSE)—the potential role for immunotherapy. Epilepsy Behav. 2015;47:17–23.
Lopinto-Khoury C, Sperling MR. Autoimmune status epilepticus. Curr Treat Options Neurol. 2013;15(5):545–56.
Broomall E et al. Pediatric super-refractory status epilepticus treated with allopregnanolone. Ann Neurol. 2014;76(6):911–5.
Hottinger A et al. Topiramate as an adjunctive treatment in patients with refractory status epilepticus: an observational cohort study. CNS Drugs. 2012;26(9):761–72.
Asadi-Pooya AA et al. Treatment of refractory generalized convulsive status epilepticus with enteral topiramate in resource limited settings. Seizure. 2015;24:114–7.
Rohracher A et al. Perampanel in patients with refractory and super-refractory status epilepticus in a neurological intensive care unit. Epilepsy Behav. 2015;49:354–8.
Redecker J et al. Efficacy of perampanel in refractory nonconvulsive status epilepticus and simple partial status epilepticus. Epilepsy Behav. 2015;45:176–9.
Rantsch K et al. Treatment and course of different subtypes of status epilepticus. Epilepsy Res. 2013;107(1–2):156–62.
Alvarez V et al. Practice variability and efficacy of clonazepam, lorazepam, and midazolam in status epilepticus: a multicenter comparison. Epilepsia. 2015;56(8):1275–85.
Shangguan Y, Liao H, Wang X. Clonazepam in the treatment of status epilepticus. Expert Rev Neurother. 2015;15(7):733–40.
Zeiler FA et al. Magnesium sulfate for non-eclamptic status epilepticus. Seizure. 2015;32:100–8.
Zeiler FA et al. Modern inhalational anesthetics for refractory status epilepticus. Can J Neurol Sci. 2015;42(2):106–15.
Sivakumar S et al. Clobazam: an effective add-on therapy in refractory status epilepticus. Epilepsia. 2015;56(6):e83–9.
Shekh-Ahmad T et al. The potential of sec-butylpropylacetamide (SPD) and valnoctamide and their individual stereoisomers in status epilepticus. Epilepsy Behav. 2015;49:298–302.
Spampanato J, Dudek FE. Valnoctamide enhances phasic inhibition: a potential target mechanism for the treatment of benzodiazepine-refractory status epilepticus. Epilepsia. 2014;55(9):e94–8.
Zeiler FA et al. Therapeutic hypothermia for refractory status epilepticus. Can J Neurol Sci. 2015;42(4):221–9.
Zeiler FA et al. VNS for refractory status epilepticus. Epilepsy Res. 2015;112:100–13.
Lhatoo SD, Alexopoulos AV. The surgical treatment of status epilepticus. Epilepsia. 2007;48 Suppl 8:61–5.
Alexopoulos A et al. Resective surgery to treat refractory status epilepticus in children with focal epileptogenesis. Neurology. 2005;64(3):567–70.
Bhatia S et al. Surgical treatment of refractory status epilepticus in children: clinical article. J Neurosurg Pediatr. 2013;12(4):360–6.
Caraballo RH et al. Ketogenic diet in pediatric patients with refractory focal status epilepticus. Epilepsy Res. 2014;108(10):1912–6.
Thakur KT et al. Ketogenic diet for adults in super-refractory status epilepticus. Neurology. 2014;82(8):665–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Eric H. Grover and Yara Nazzal declare that they have no conflict of interest.
Lawrence J. Hirsch has received research support from UCB, Upsher-Smith, Lundbeck, Eisai, Sunovion, and Acorda. Dr. Hirsch also has received consultation fees from Upsher-Smith, Marinus, Monteris, and Sunovion as well as speaking honoraria from Neuropace.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Epilepsy
Rights and permissions
About this article
Cite this article
Grover, E.H., Nazzal, Y. & Hirsch, L.J. Treatment of Convulsive Status Epilepticus. Curr Treat Options Neurol 18, 11 (2016). https://doi.org/10.1007/s11940-016-0394-5
Published:
DOI: https://doi.org/10.1007/s11940-016-0394-5
Keywords
- Convulsive status epilepticus
- Anti-epileptic drugs
- Benzodiazepines
- First-line treatment
- Second-line treatment
- Operational definition of status epilepticus
- Mechanistic definition of generalized CSE
- Lorazepam
- Midazolam
- Valproate
- Phenytoin
- Levetiracetam
- Lacosamide
- Refractory status epilepticus
- New onset-refractory status epilepticus