Abstract
Purpose of review
This article reviews the contemporary evidence for the use of intravascular ultrasound (IVUS) for peripheral arterial disease (PAD) endovascular interventions.
Recent findings
Earlier observational studies have shown that IVUS use for endovascular interventions is associated with improved patency rates and freedom from restenosis. Recently, a randomized trial demonstrated that IVUS was associated with a significantly larger mean vessel diameter than angiography, higher freedom from binary restenosis at 12 months. Recent large observational studies have suggested that IVUS is also associated with improved clinical outcomes. One study of 543,488 Medicare beneficiaries showed that IVUS use was associated with lower risk of major adverse limb events, including amputation and arterial thrombosis. Another Japanese analysis of 85,649 showed that the IVUS was associated with lower incidence of amputation at 12 months.
Summary
The benefit of IVUS use in coronary interventions is well established, but the translation of these benefits to endovascular interventions has lagged behind, with a growing body of evidence supporting its use, mainly observational studies. Randomized trials are emerging to better document the benefit of IVUS in endovascular interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Opinion statement
The evidence supporting IVUS use for endovascular interventions is mostly driven from retrospective observational studies. IVUS use for endovascular interventions is controversial given the availability of other less expensive imaging modalities—unlike coronaries—to assess lesion morphology and provide help with preprocedural planning. Future randomized trials establishing the role of IVUS for endovascular interventions are encouraged.
Introduction
Peripheral arterial disease (PAD) is the third leading cause of atherosclerotic morbidity, following coronary heart disease and stroke, with a prevalence of approximately 5% at age 40–44 and 12% at age 70–74 [1], and it has been estimated that 238 million people were living with PAD in 2015 [2].
The use of percutaneous endovascular approaches to treat PAD has increased over the years [3] with new advances in technology, wires, stents, balloons, and improved imaging modalities [4]. That led to an increased number of endovascular interventions, including balloon angioplasty, atherectomy, and stenting [5]. However, patency rates in the lower extremity are not durable [6, 7]. Digital subtraction angiography (DSA) remains the imaging modality during endovascular peripheral procedures. However, it has the limitation of providing a two-dimensional image of a three-dimensional luminal structure, and the images can be confounded by vessel tortuosity and complex luminal irregularities [4, 8].
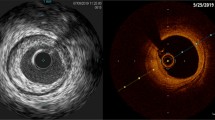
Intravascular ultrasound (IVUS) is an invasive vascular imaging modality that was first introduced in the early 1990s. It has been used as an adjunctive modality to angiography overcoming its two-dimensional imaging limitation. It acquires images perpendicular to the axis of imaging catheter. Once the IVUS catheter is at the desired location, imaging is performed by a slow pullback which can be performed manually or automatically with rates of pullback of 0.5 or 1.0 mm/s depending on the type of catheter.
IVUS can guide adequate lesion preparation by providing information regarding lesion severity, morphology, plaque burden, and vessel dimensions, which will help to ensure appropriate stent sizing. It can also provide information about adequate stent expansion and strut apposition as well as identifying complications such as dissections. Furthermore, IVUS provides potential benefits in reducing iodinated contrast and radiation exposure [9]. For these reasons, IVUS has been increasingly used in coronary interventions and has been associated with better clinical outcomes [10, 11]. The main objective of this review is to provide an update on the use of IVUS in endovascular interventions for PAD.
Clinical outcomes with IVUS-guided endovascular interventions for PAD
The data on clinical outcomes with IVUS-guided interventions for PAD are scarce and mostly driven from observational studies with limited prospective studies or clinical trials comparing the outcomes between IVUS-guided and angiography-guided endovascular interventions.
In a systematic review, Natesan et al. identified 29 studies comparing IVUS with angiography alone during endovascular interventions for PAD [12]. The majority were retrospective cohorts with a total number of 95,192 patients. Among29 studies, 18 evaluated the utility of IVUS for device sizing, placement, and optimization. Six studies examined the utility of IVUS in the evaluation of lesion characteristics, 3 studies evaluated IVUS utility in cases of arterial dissections, and 2 studies evaluated IVUS use in reentry of chronic total occlusions. IVUS-guided endovascular interventions were associated with accurate reference vessel diameter measurements, larger balloons and stents sizes, and better wound healing rates compared with angiography alone.
Allan et al. [13] performed a single-center randomized trial of 150 patients undergoing femoropopliteal endovascular intervention and demonstrated that IVUS was associated with a significantly larger mean vessel diameter than angiography (5.60 mm vs. 5.10 mm; p < 0.001), higher freedom from binary restenosis at 12 months (72.4% vs. 55.4%; p = 0.008), and lower binary restenosis for cases treated with drug-coated balloons (9.1% vs. 37.5%; p = 0.001). There was a high grade (82%) of disagreement between IVUS and angiographic findings, with a change in treatment strategies with IVUS in 79% of cases.
In a recent analysis by Divakaran et al. [14], among 543,488 Medicare beneficiaries (i.e., aged > 65 years) between 2016 and 2019 treated for endovascular interventions, IVUS use has marginally increased. IVUS was associated with a lower risk of major adverse limb events, including amputation and arterial thrombosis (adjusted hazard ratio, 0.73; 95% confidence interval (CI) 0.70–0.75; p < 0.0001). A recent Japanese analysis of 85,649 patients showed that IVUS was associated with a significantly lower incidence of amputation at 12 months (6.9% in the IVUS group versus 9.3% in the non-IVUS group; hazard ratio, 0.80 [95% CI, 0.72–0.89]). IVUS was also associated with a lower incidence of bypass surgery and stent grafting, but a higher incidence of reintervention and readmission. Iida et al. in a cohort study of 965 patients with PAD undergoing femoropopliteal artery stenting showed that IVUS was associated with higher 5-year primary patency rate (65% ± 6% vs. 35% ± 6%, p < 0.001), better freedom from any adverse limb event rate (p < 0.001), and better event-free survival rate (p < 0.001) [15]. Similar results were demonstrated by Kumakura et al. [16] who showed a 5-, 10-, and 15-year patency of 89, 83, and 75%, respectively, among 455 patients undergoing IVUS-guided primary stenting for iliac artery disease. Miki et al. [17] in a retrospective analysis of 274 patients showed that IVUS-guided stenting was associated with a primary patency rate of 82.5% (95% CI 78.1 to 86.9%) at 12 months and 73.2% (95% CI 67.9 to 78.5%) at 24 months. Other observational studies reported on the clinical outcomes of IVUS-guided peripheral endovascular procedures [16,17,18,19,20].
Tsujimura et al. investigated the effect of IVUS on clinical outcomes after aortoiliac stenting in patients with PAD, with a total of 803 patients (IVUS, 545; no IVUS, 258). In 138 matched pairs, they found no significant difference in the 12-month restenosis rate between the 2 groups (10.2% (95% CI 6.9 to 14.9%) vs. 10.3% (95% CI 5.4 to 18.6%), p = 0.99) [21]. These findings were similar to another study with1,091 patients undergoing drug-eluting stent implantation for femoropopliteal lesions There was no significant difference in the rate of 1-year restenosis the 2 groups (11.5% (95% CI 9.1–14.0%) vs. 15.5% (95% CI 10.9–20.1%); p = 0.22), with a significantly higher incidence of aneurysmal degeneration in the IVUS group [22].
Tables 1 and 2 summarize the characteristics and outcomes of the main studies evaluating IVUS in the endovascular management of PAD.
IVUS for evaluation of lesion characteristics and severity
The proper evaluation of plaque morphology and accurate vessel sizing is a major component for peripheral endovascular procedures. IVUS provides detailed information not only about the vessel lumen but also about plaque morphology and composition, with a high degree of accurate measurements of the vessel diameter. Several studies showed that IVUS is superior than angiography in terms of accurate vessel measurements [29,30,31,32,33]. In a study by Yin et al., IVUS detected calcium in 44/47 (93.6%) lesions, while angiography detected calcium in only 26/47 (55.3%) [34].
Iida et al. in a prospective multicenter study including 1725 patients undergoing femoropopliteal interventions for symptomatic PAD showed that IVUS-assessed RVD (reference vessel diameter) was significantly larger than angiography-assessed RVD (6.0 ± 1.0 mm vs. 5.0 ± 1.0 mm; p < 0.001), with a mean difference of 0.98 mm (95% CI 0.94–1.03 mm). About half of the study cohort had ΔRVD ≥ 1 mm. IVUS measurements were more likely to be different by angiography in cases with small vessels, chronic total occlusion (CTO), bilateral calcification, and history of stent implantation [35]. A retrospective study of 165 patients showed that drug-coated balloon (DCB) sizing according to IVUS-measured external elastic membrane (EEM) size, but not of angio-lumen size or IVUS-lumen size, was associated with a reduced risk of restenosis after femoropopliteal interventions [23].
IVUS for device sizing, placement, and optimization
Five observational studies with a total number of 1,133 patients compared IVUS use versus angiography alone during percutaneous transluminal angioplasty (PTA) and stenting [15, 27, 28, 36, 37]. Long-term patency rates ranged from 57 to 100% with IVUS use vs. 64 to 83.4% without IVUS use. Four studies reported that IVUS identified more under-deployed stents and provided improved vessel sizing information compared to angiography [28, 37,38,39].
Hitchner et al. in their observational study of 59 patients undergoing superficial femoral artery interventions showed that IVUS was able to detect residual stenosis and 80% of patients underwent additional treatment after identification of significant residual stenosis by IVUS [40]. IVUS provides optimal measurements, identify under-deployed stents, and detect residual stenosis.
IVUS for below-the-knee (BTK) interventions
IVUS use in below-the-knee (BTK) interventions was studied in few observational studiess. A recent consensus document on the appropriate use of IVUS in various phases of peripheral arterial and venous interventions in which thirty international vascular experts anonymously completed a survey showed that IVUS was rated appropriate especially in all interventional phases for the tibial arteries [41].
In a single-center retrospective analysis of 155 CLI patients [24], IVUS was associated with larger balloon size (p < 0.001). Wound healing was significantly earlier, whereas limb salvage and overall survival were not significantly different. Another observational study by Fujihara et al. [25] of 33 propensity score-matched pairs of patients who underwent successful balloon angioplasty treated with IVUS-guided versus angiography-guided procedures, demonstrating a significantly larger maximal balloon size in the IVUS group (2.45 ± 0.4 mm vs. 2.23 ± 0.4 mm; p < 0.001). There was no significant difference in limb salvage rates, complication rate, or technical success (p > 0.99, p = 0.16, and p = 0.56, respectively). In a small observational study of 20 patients, Kuku et al. [32] compared mean reference vessel diameter (RVD) between IVUS and angiography during BTK interventions and found that IVUS use was associated with larger mean RVD (3.27 ± 0.68 mm vs. 2.81 ± 1.19 mm; p = 0.15). They also found a greater correlation between IVUS measurements and the nominal balloon diameters (IVUS: balloon, R2 = 0.45 vs. QVA: balloon, R2 = 0.34). Interestingly, there was a greater degree of acute gain (defined by the difference between pre- and post-intervention minimal lumen diameters) in cases where the treatment balloon size correlates with IVUS-measured reference size. These findings of larger mean vessel diameter were also shown in a study by Shammas et al. [33].
The main findings of the aforementioned studies of larger balloons being used with IVUS measurements, leading to favorable wound healing rates, shed the light on the importance of proper measurements of BTK vessel beds. Assessing the true lumen diameter would help with optimal balloon sizing and stenting, which will probably shorten the healing period and lower the likelihood of re-intervention.
IVUS for diagnosis of arterial dissections
Dissections are common complications with endovascular interventions. Dissections can be classified by angiography based on the NHLBI classification [42] or by IVUS based on the iDissection classification [43]. Some pathologic studies have shown that deeper dissections into the media and adventitia correlate with patency loss [44]. Angiography under appreciates the presence, extent, and depth of dissections and often can be misleading. Multiple studies have confirmed the superiority of IVUS in detecting dissections [26, 37, 45,46,47], which can correlate with clinical outcomes and improved patency rates. In a prospective study by Shammas et al. [26] of 15 patients undergoing treatment of femoropopliteal de novo or non-stent restenosis using atherectomy, forty-six dissections were identified on IVUS post atherectomy vs. 8 dissections on angiogram (p < 0.01) (ratio, 5.75 to 1). For post adjunctive angioplasty, IVUS identified 39 dissections vs. 11 by angiogram. There are similar findings to another study [46], in which IVUS detected 49 dissections post adjunctive angioplasty vs. 6 on angiogram. In BTK interventions, IVUS detected more dissections than seen on angiography (34 on IVUS vs. 9 dissection on angiography) [33]. Interestingly, IVUS can also be a useful tool to undercover extraluminal diseases, as in the case report of an adventitial cystic disease that was misdiagnosed as PAD in which IVUS was a useful tool to reach proper diagnosis [48].
IVUS for chronic total occlusion interventions
Chronic total occlusions (CTOs) are encountered in around 40–50% of patients undergoing endovascular interventions [49]. Long occlusion with heavy calcification can be technically challenging; thus, failure to cross such lesions can be as high as 30% [49] and is associated with a higher risk of complications [50]. Percutaneous subintimal recanalization is the most common endovascular revascularization technique for CTO of the iliac arteries. The primary reason for failure of this technique is failure to reenter the true lumen [51,52,53]. Some studies evaluated the use of IVUS for true lumen reentry during subintimal angioplasty and showed very promising results with technical success rates of almost 100%. The real-time imaging of IVUS allows the operator to create a subintimal tract and direct the needle deployment. IVUS also confirms vessel patency at the point of the needle due to its color flow capabilities. The controlled reentry offered by IVUS catheters reduces the risk of complications, such as dissections or perforations caused by wire or catheter misplacements [52, 54,55,56,57,58]. Kawasaki et al. [55] compared true lumen reentry with and without IVUS and showed that technical success was higher in the IVUS group (97% vs. 81%).
IVUS and contrast exposure
It was proposed that with IVUS guidance contrast injection could be reduced or completely avoided. Kawasaki et al. [55] evaluated IVUS use in reentry and demonstrated that the total volume of contrast material was less with IVUS than without IVUS guidance (104 ± 56 mL vs. 201 ± 100 mL (p < 0.01). Essa et al. [30] also showed that IVUS was associated with a lower overall mean contrast utilization compared to computed tomography angiography (CTA) (29 vs. 100 cc; p < 0.001). The lower contrast media used with IVUS guidance decreases the risk of complications as contrast-induced acute kidney injury and can be very important especially for patients suffering from diabetes, chronic renal disease, or contrast allergies.
IVUS and cost
The incorporation of IVUS catheters in endovascular interventions adds additional cost to the overall procedure with an increase that ranges from $1,080 to $1,333 [28, 59]. Schiele et al. [59] reported that acute procedural costs can be 18% higher with IVUS compared to non-IVUS use. Interestingly, they reported a higher number of revascularization procedures in the control group (31 in the control group vs. 20 in the IVUS group), then analyzed the cumulative medical costs at 18 months which was slightly higher in the IVUS group (4535 ± 2020 Euros vs. 4679 ± 1471 Euros in the IVUS group). The higher acute costs in the group with IVUS guidance were partially offset by the lower number of re-interventions. This observation sheds the light to that; the use of IVUS can be cost effective when properly used.
Barriers to IVUS use
Many operators and researchers are opposed to the use of IVUS for peripheral endovascular interventions. There is paucity of data driven from randomized controlled trials demonstrating the long-term clinical outcomes of IVUS use as almost all studies are retrospective observational, so there is a risk for unmeasured confounding. Most of the studies did not account for the operator’s experience. IVUS being a morphologic assessment tool that cannot provide information about the hemodynamic significance of stenosis is a concern [60]. The use of larger balloons and stents based upon IVUS outer vessel diameter measurements may cause complications as dissections as reported by Tsujimura et al. [21] with a significantly higher frequency of aneurysmal degeneration at 1 year in the IVUS group than in the non-IVUS group (19.8% (95% CI 16.3–23.4%) vs. 7.1% (95% CI 3.3–11.0%); p < 0.001). Similar results by Iida et al. [61] showed that IVUS was associated with a high rate of superficial femoral artery degeneration with a 1-year occurrence of aneurysmal degeneration of 16.8% (95% CI 13.9–19.6%). Unlike coronaries, there are other modalities to assess lesion characteristics regarding reference vessel size and plaque composition non-invasively as preprocedural duplex ultrasound or computed tomographic angiography which can reduce the total procedure time without additional cost to the procedure.
Conclusion
IVUS was shown in multiple observational studies to provide better vessel diameter measurements and ensure optimal stent sizing and proper deployment with some studies reporting better long-term patency rates, which was confirmed by a recent randomized trial. Accordingly, some data indicate that there has been a marginal increase in IVUS use for PAD. In addition, large observational studies suggest that IVUS is associated with lower risk of major adverse limb events, including amputation. Future randomized trials to further establish the role of IVUS during endovascular interventions are encouraged.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fowkes FGR, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. The Lancet. 2013;382:1329–40.
Song P, Fang Z, Wang H, Cai Y, Rahimi K, Zhu Y, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob Health. 2020;8:e721–9.
Eb D, K I, Db R. Virtual histology and color flow intravascular ultrasound in peripheral interventions. Seminars in vascular surgery [Internet]. Semin Vasc Surg; 2006 [cited 2023 Mar 20];19. Available from: https://pubmed.ncbi.nlm.nih.gov/16996418/
Duran C, Bismuth J. Advanced imaging in limb salvage. Methodist DeBakey Cardiovascular Journal. Methodist DeBakey Heart & Vascular Center; 2012;8:28.
Anantha-Narayanan M, Doshi RP, Patel K, Sheikh AB, Llanos-Chea F, Abbott JD, et al. Contemporary trends in hospital admissions and outcomes in patients with critical limb ischemia. Circulation: Cardiovascular Quality and Outcomes. American Heart Association; 2021;14:e007539.
Md D, Gm A, Mr J, T O, Rr S, Hb S, et al. Durable clinical effectiveness with paclitaxel-eluting stents in the femoropopliteal artery: 5-year results of the Zilver PTX randomized trial. Circulation [Internet]. Circulation; 2016 [cited 2023 Mar 20];133. Available from: https://pubmed.ncbi.nlm.nih.gov/26969758/
K R, Mr J, Cj W, K R-S, C M-H, Dc M, et al. Trial of a paclitaxel-coated balloon for femoropopliteal artery disease. The New England journal of medicine [Internet]. N Engl J Med; 2015 [cited 2023 Mar 20];373. Available from: https://pubmed.ncbi.nlm.nih.gov/26106946/
Vs K, Ml P, Pd B, Sp N, Mj E, Dg C, et al. Angiography underestimates peripheral atherosclerosis: lumenography revisited. Journal of endovascular therapy : an official journal of the International Society of Endovascular Specialists [Internet]. J Endovasc Ther; 2008 [cited 2023 Mar 20];15. Available from: https://pubmed.ncbi.nlm.nih.gov/18254670/
Mariani J, Guedes C, Soares P, Zalc S, Campos CM, Lopes AC, et al. Intravascular ultrasound guidance to minimize the use of iodine contrast in percutaneous coronary intervention: the MOZART (Minimizing cOntrast utiliZation With IVUS Guidance in coRonary angioplasTy) randomized controlled trial. JACC Cardiovasc Interv. 2014;7:1287–93.
Räber L, Mintz GS, Koskinas KC, Johnson TW, Holm NR, Onuma Y, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. EuroIntervention. 2018;14:656–77.
Jang J-S, Song Y-J, Kang W, Jin H-Y, Seo J-S, Yang T-H, et al. Intravascular ultrasound-guided implantation of drug-eluting stents to improve outcome: a meta-analysis. JACC Cardiovasc Interv. 2014;7:233–43.
•• Natesan S, Mosarla RC, Parikh SA, Rosenfield K, Suomi J, Chalyan D, et al. Intravascular ultrasound in peripheral venous and arterial interventions: a contemporary systematic review and grading of the quality of evidence. Vascular Medicine [Internet]. SAGE PublicationsSage UK: London, England; 2022 [cited 2023 Mar 24]; Available from: https://journals.sagepub.com/doi/epub/10.1177/1358863X221092817. The latest systematic review evaluating 29 studies of IVUS use in peripheral arterial disease.
•• Allan RB, Puckridge PJ, Spark JI, Delaney CL. The impact of intravascular ultrasound on femoropopliteal artery endovascular interventions: A randomized controlled trial. JACC: Cardiovascular Interventions. 2022;15:536–46. The first randomized trial evaluating the role of IVUS in femoropopliteal interventions and demonstrated that IVUS was associated with higher freedom from binary restenosis at 12 months than angiography alone (72.4% vs. 55.4%; p = 0.008).
• Divakaran S, Parikh SA, Hawkins BM, Chen S, Song Y, Banerjee S, et al. Temporal trends, practice variation, and associated outcomes with IVUS use during peripheral arterial intervention. JACC: Cardiovascular Interventions. American College of Cardiology Foundation; 2022;15:2080–90. The largest peripheral intervention study with data from 543,488 Medicare beneficiaries undergoing endovascular intervention between 2016 and 2019 and reported an increase in the use of IVUS since 2016 and also showed that IVUS was associated with a lower risk of major adverse limb events, including amputation and arterial thrombosis (adjusted hazard ratio, 0.73; 95% confidence interval (CI) 0.70–0.75; p = 0.0001) as compared with no IVUS.
Iida O, Takahara M, Soga Y, Suzuki K, Hirano K, Kawasaki D, et al. Efficacy of intravascular ultrasound in femoropopliteal stenting for peripheral artery disease with TASC II class A to C lesions. J Endovasc Ther. 2014;21:485–92.
Kumakura H, Kanai H, Araki Y, Hojo Y, Iwasaki T, Ichikawa S. 15-year patency and life expectancy after primary stenting guided by intravascular ultrasound for iliac artery lesions in peripheral arterial disease. JACC Cardiovasc Interv. 2015;8:1893–901.
Miki K, Fujii K, Tanaka T, Yanaka K, Yoshihara N, Nishimura M, et al. Impact of IVUS-derived vessel size on midterm outcomes after stent implantation in femoropopliteal lesions. J Endovasc Ther. 2020;27:77–85.
Krishnan P, Tarricone A, K-Raman P, Majeed F, Kapur V, Gujja K, et al. Intravascular ultrasound guided directional atherectomy versus directional atherectomy guided by angiography for the treatment of femoropopliteal in-stent restenosis. Ther Adv Cardiovasc Dis. 2018;12:17–22.
Fujihara M, Kozuki A, Tsubakimoto Y, Takahara M, Shintani Y, Fukunaga M, et al. Lumen gain after endovascular therapy in calcified superficial femoral artery occlusive disease assessed by intravascular ultrasound (CODE study). J Endovasc Ther. 2019;26:322–30.
Araki M, Hirano K, Nakano M, Ito Y, Ishimori H, Yamawaki M, et al. Two-year outcome of the self-expandable stent for chronic total occlusion of the iliac artery. Cardiovasc Interv Ther. 2014;29:40–6.
Tsujimura T, Takahara M, Iida O, Yamauchi Y, Shintani Y, Sugano T, et al. Intravascular ultrasound imaging during aortoiliac stenting: no impact on outcomes at 1 year. J Endovasc Ther. 2021;28:139–45.
Tsujimura T, Iida O, Takahara M, Soga Y, Yamaoka T, Fujihara M, et al. Clinical impact of intravascular ultrasound-guided fluoropolymer-based drug-eluting stent implantation for femoropopliteal lesions. JACC Cardiovasc Interv. 2022;15:1569–78.
Kurata N, Iida O, Takahara M, Asai M, Masuda M, Okamoto S, et al. Clinical impact of the size of drug-coated balloon therapy on restenosis rate in femoropopliteal lesions. J Endovasc Ther. 2022;15266028221081082.
Soga Y, Takahara M, Ito N, Katsuki T, Imada K, Hiramori S, et al. Clinical impact of intravascular ultrasound-guided balloon angioplasty in patients with chronic limb threatening ischemia for isolated infrapopliteal lesion. Catheter Cardiovasc Interv. 2021;97:E376–84.
Fujihara M, Yazu Y, Takahara M. Intravascular ultrasound-guided interventions for below-the-knee disease in patients with chronic limb-threatening ischemia. J Endovasc Ther. 2020;27:565–74.
Shammas NW, Torey JT, Shammas WJ, Jones-Miller S, Shammas GA. Intravascular ultrasound assessment and correlation with angiographic findings demonstrating femoropopliteal arterial dissections post atherectomy: results from the iDissection study. J Invasive Cardiol. 2018;30:240–4.
Baker AC, Humphries MD, Noll RE, Salhan N, Armstrong EJ, Williams TK, et al. Technical and early outcomes using ultrasound-guided reentry for chronic total occlusions. Ann Vasc Surg. 2015;29:55–62.
Buckley CJ, Arko FR, Lee S, Mettauer M, Little D, Atkins M, et al. Intravascular ultrasound scanning improves long-term patency of iliac lesions treated with balloon angioplasty and primary stenting. J Vasc Surg. 2002;35:316–23.
Arthurs ZM, Bishop PD, Feiten LE, Eagleton MJ, Clair DG, Kashyap VS. Evaluation of peripheral atherosclerosis: a comparative analysis of angiography and intravascular ultrasound imaging. J Vasc Surg. 2010;51:933–8; discussion 939.
E E, N M, P B, Q C, B G, G R, et al. Vascular Assessment for transcatheter aortic valve replacement: intravascular ultrasound compared with computed tomography. The Journal of invasive cardiology [Internet]. J Invasive Cardiol; 2016 [cited 2023 Mar 27];28. Available from: https://pubmed.ncbi.nlm.nih.gov/27922808/
Pliagas G, Saab F, Stavroulakis K, Bisdas T, Finton S, Heaney C, et al. Intravascular ultrasound imaging versus digital subtraction angiography in patients with peripheral vascular disease. J Invasive Cardiol. 2020;32:99–103.
Kuku KO, Garcia-Garcia HM, Finizio M, Melaku GD, Wilson VA, Beyene SS, et al. Comparison of angiographic and intravascular ultrasound vessel measurements in infra-popliteal endovascular interventions: the below-the-knee calibration study. Cardiovasc Revasc Med. 2022;35:35–41.
Shammas NW, Shammas WJ, Jones-Miller S, Torey JT, Armstrong EJ, Radaideh Q, et al. Optimal vessel sizing and understanding dissections in infrapopliteal interventions: data from the iDissection below the knee study. J Endovasc Ther. 2020;27:575–80.
D Y, A M, Tm S, Jj R, V R, Mt F, et al. Intravascular ultrasound validation of contemporary angiographic scores evaluating the severity of calcification in peripheral arteries. Journal of endovascular therapy : an official journal of the International Society of Endovascular Specialists [Internet]. J Endovasc Ther; 2017 [cited 2023 Mar 27];24. Available from: https://pubmed.ncbi.nlm.nih.gov/28504047/
Iida O, Takahara M, Soga Y, Fujihara M, Kawasaki D, Hirano K, et al. Vessel diameter evaluated by intravascular ultrasound versus angiography. J Endovasc Ther. 2022;29:343–9.
Tielbeek AV, Vroegindeweij D, Buth J, Schol FP, Mali WP. Comparison of intravascular ultrasonography and intraarterial digital subtraction angiography after directional atherectomy of short lesions in femoropopliteal arteries. J Vasc Surg. 1996;23:436–45.
Colli R, Di Stasi C, Modugno P, Orlando G, Cavallaro A. Intravascular ultrasound in the endovascular management of atherosclerotic peripheral occlusive disease. Chir Ital. 2004;56:229–38.
Navarro F, Sullivan TM, Bacharach JM. Intravascular ultrasound assessment of iliac stent procedures. J Endovasc Ther. 2000;7:315–9.
Arko F, McCollough R, Manning L, Buckley C. Use of intravascular ultrasound in the endovascular management of atherosclerotic aortoiliac occlusive disease. Am J Surg. 1996;172:546–9; discussion 549–550.
Hitchner E, Zayed M, Varu V, Lee G, Aalami O, Zhou W. A prospective evaluation of using IVUS during percutaneous superficial femoral artery interventions. Ann Vasc Surg. 2015;29:28–33.
Secemsky EA, Mosarla RC, Rosenfield K, Kohi M, Lichtenberg M, Meissner M, et al. Appropriate use of intravascular ultrasound during arterial and venous lower extremity interventions. JACC Cardiovasc Interv. 2022;15:1558–68.
Rogers JH, Lasala JM. Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invasive Cardiol. 2004;16:493–9.
Shammas NW, Torey JT, Shammas WJ. Dissections in peripheral vascular interventions: a proposed classification using intravascular ultrasound. J Invasive Cardiol. 2018;30:145–6.
Tarricone A, Ali Z, Rajamanickam A, Gujja K, Kapur V, Purushothaman K-R, et al. Histopathological evidence of adventitial or medial injury is a strong predictor of restenosis during directional atherectomy for peripheral artery disease. J Endovasc Ther. 2015;22:712–5.
Tielbeek AV, Vroegindeweij D, Gussenhoven EJ, Buth J, Landman GH. Evaluation of directional atherectomy studied by intravascular ultrasound in femoropopliteal artery stenosis. Cardiovasc Intervent Radiol. 1997;20:413–9.
Nw S, Wj S, S J-M, Q R, Ga S. Femoropopliteal arterial dissections post flex vessel prep and adjunctive angioplasty: results of the flex iDissection study. The Journal of invasive cardiology [Internet]. J Invasive Cardiol; 2019 [cited 2023 Mar 27];31. Available from: https://pubmed.ncbi.nlm.nih.gov/31034434/
Pasterkamp G, Spijkerboer AM, Mali WP, Borst C. Residual stenosis determined by intravascular ultrasound and duplex ultrasound after balloon angioplasty of the superficial femoral artery. Ultrasound Med Biol. 1996;22:801–6.
Miyauchi E, Okui H, Yuasa T, Oketani N, Ohishi M. Adventitial cystic disease in the popliteal artery diagnosed by intravascular ultrasound imaging. Cureus. 15:e34362.
Banerjee S, Shishehbor MH, Mustapha JA, Armstrong EJ, Ansari M, Rundback JH, et al. A percutaneous crossing algorithm for femoropopliteal and tibial artery chronic total occlusions (PCTO algorithm). J Invasive Cardiol. 2019;31:111–9.
A K, H J-S, H L, H X, H K, A P, et al. Comparative assessment of patient outcomes with intraluminal or subintimal crossing of infrainguinal peripheral artery chronic total occlusions. Vascular medicine (London, England) [Internet]. Vasc Med; 2018 [cited 2023 Mar 27];23. Available from: https://pubmed.ncbi.nlm.nih.gov/29105577/
Lipsitz EC, Ohki T, Veith FJ, Suggs WD, Wain RA, Cynamon J, et al. Does subintimal angioplasty have a role in the treatment of severe lower extremity ischemia? J Vasc Surg. 2003;37:386–91.
Saket RR, Razavi MK, Padidar A, Kee ST, Sze DY, Dake MD. Novel intravascular ultrasound-guided method to create transintimal arterial communications: initial experience in peripheral occlusive disease and aortic dissection. J Endovasc Ther. 2004;11:274–80.
London NJ, Srinivasan R, Naylor AR, Hartshorne T, Ratliff DA, Bell PR, et al. Subintimal angioplasty of femoropopliteal artery occlusions: the long-term results. Eur J Vasc Surg. 1994;8:148–55.
Vn K, Jl E, Pk H, Je R. Intravascular ultrasound-guided true lumen reentry device for recanalization of unilateral chronic total occlusion of iliac arteries: technique and follow-up. Annals of vascular surgery [Internet]. Ann Vasc Surg; 2010 [cited 2023 Mar 27];24. Available from: https://pubmed.ncbi.nlm.nih.gov/20363107/
Kawasaki D, Tsujino T, Fujii K, Masutani M, Ohyanagi M, Masuyama T. Novel use of ultrasound guidance for recanalization of iliac, femoral, and popliteal arteries. Catheter Cardiovasc Interv. 2008;71:727–33.
Saketkhoo RR, Razavi MK, Padidar A, Kee ST, Sze DY, Dake MD. Percutaneous bypass: subintimal recanalization of peripheral occlusive disease with IVUS guided luminal re-entry. Tech Vasc Interv Radiol. 2004;7:23–7.
Jacobs DL, Motaganahalli RL, Cox DE, Wittgen CM, Peterson GJ. True lumen re-entry devices facilitate subintimal angioplasty and stenting of total chronic occlusions: initial report. J Vasc Surg. 2006;43:1291–6.
Ac B, Md H, Re N, N S, Ej A, Tk W, et al. Technical and early outcomes using ultrasound-guided reentry for chronic total occlusions. Annals of vascular surgery [Internet]. Ann Vasc Surg; 2015 [cited 2023 Mar 27];29. Available from: https://pubmed.ncbi.nlm.nih.gov/25449989/
Schiele F, Meneveau N, Seronde M-F, Caulfield F, Pisa B, Arveux P, et al. Medical costs of intravascular ultrasound optimization of stent deployment. Results of the multicenter randomized “REStenosis after Intravascular ultrasound STenting” (RESIST) study. Int J Cardiovasc Intervent. 2000;3:207–13.
Bk K, X H, J K, J Z, J J, Jy H, et al. Fractional flow reserve or intravascular ultrasonography to guide PCI. The New England journal of medicine [Internet]. N Engl J Med; 2022 [cited 2023 Apr 1];387. Available from: https://pubmed.ncbi.nlm.nih.gov/36053504/
Iida O, Takahara M, Soga Y, Yamaoka T, Fujihara M, Kawasaki D, et al. 1-year outcomes of fluoropolymer-based drug-eluting stent in femoropopliteal practice: predictors of restenosis and aneurysmal degeneration. JACC: Cardiovascular Interventions. 2022;15:630–8.
Setogawa N, Ohbe H, Matsui H, Yasunaga H. Amputation after endovascular therapy with and without intravascular ultrasound guidance: a nationwide propensity score–matched study. Circulation: Cardiovascular Interventions. American Heart Association; 2023;16:e012451.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mohamed Khedr declares that he has no conflict of interest. Michael Megaly declares that he has no conflict of interest. Islam Y. Elgendy declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khedr, M., Megaly, M. & Elgendy, I.Y. Intravascular Ultrasound in Endovascular Interventions for Peripheral Artery Disease. Curr Treat Options Cardio Med 25, 347–358 (2023). https://doi.org/10.1007/s11936-023-00997-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11936-023-00997-2