Abstract
Purpose of Review
Local tumor staging is paramount in the evaluation and management of bladder cancer. While neoadjuvant chemotherapy (NAC) followed by radical cystectomy and urinary diversion remains the gold standard for management of muscle-invasive bladder cancer, bladder-sparing regimens involving systemic chemotherapy and pelvic radiotherapy remain a viable option for select patients. Moreover, pre-cystectomy identification of patients with a complete response to NAC may obviate the need for radical cystectomy, but accurate post-therapy staging can be difficult to achieve. Contemporary imaging techniques may provide additional benefit in local tumor staging beyond standard imaging and cystoscopic biopsy. Our purpose is to summarize the ability of different imaging modalities to accurately stage bladder cancer patients in the treatment-naïve and post-chemotherapy settings.
Recent Findings
Contemporary investigations have been studying multiparametric magnetic resonance imaging (mp-MRI) in the evaluation of bladder cancer. Its recent incorporation into bladder cancer staging is mainly being assessed in treatment-naïve patients; however, different sequences are being studied to assess their accuracy after the introduction of chemotherapy and possibly radiation. Multiple recent studies incorporating cystoscopy and biopsy are proving to be less accurate than originally predicted.
Summary
Imaging has generally had a very limited role in guiding therapy in localized bladder cancer, but with the incorporation of newer sequences and techniques, imaging is poised to become vital in decision-making strategies of this cancer. Reliable local tumor staging through improved imaging may help better select patients for bladder-sparing treatments while maintaining optimized oncologic outcomes and allow this paradigm to become more acceptable in the urologic oncology community.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bladder cancer is a common malignancy in the United States with over 81,190 new cases diagnosed in 2018 with an associated 17,240 deaths [1]. It also has a large societal cost by being the most expensive cancer to treat on a per patient basis [2]. The gold standard treatment for muscle-invasive bladder cancer (MIBC) remains radical cystectomy with perioperative chemotherapy, though this is a morbid procedure with a 90-day mortality rate of 1.6–8.1% and a complication rate approaching of 60% [3]. Multimodal therapy involving aggressive endoscopic resection followed by a combination of systemic chemotherapy and pelvic radiotherapy has allowed for bladder preservation with acceptable oncologic outcomes in select patients [4].
Neoadjuvant chemotherapy (NAC) was introduced through multiple prospective trials and was shown by the Advanced Bladder Cancer Meta-analysis Collaboration to improve overall survival by 5% compared to radical cystectomy alone [5]. Patients who were found to have no residual cancer in the cystectomy specimen have the best disease-specific survival. As NAC became more widespread and prevalent, there was a subset of patients who either refused cystectomy or were medically unfit to undergo surgery after receiving NAC. Among these patients who achieved a seemingly complete response after NAC (based on imaging and endoscopic evaluation), the outcomes were surprisingly reasonable, with a reported 5-year disease-specific survival rate of 90% and cystectomy free rates of 76% [6]. Findings such as these have spurred further investigation into how to better identify patients who were downstaged from MIBC to non-muscle invasive bladder cancer (NMIBC) and who could potentially benefit from bladder preservation.
The goal of this manuscript is to review the performance of current diagnostic modalities for local staging of MIBC in the treatment-naive setting and then, the post-neoadjuvant chemotherapy +/- radiation setting, with a focus on multiparametric magnetic resonance imaging (mp-MRI), cystoscopy, and novel developments with PET imaging.
Diagnostic Modalities in Treatment-Naive Patients
Cystoscopy has long been the standard to evaluate the bladder for urothelial carcinoma (UC) due to its high sensitivity for identifying papillary tumors of all sizes. However, given its invasive nature, radiographic methods have been studied to find an alternative to cystoscopy. Conventional ultrasound has been examined and shown to have a sensitivity of 72–87% for detecting tumors [7, 8]. Other modalities such as 3D and contrast-enhanced ultrasonography (CEUS) have been employed to help increase both the sensitivity of detecting lesions and accuracy in detecting other tumor characteristics, such as tumor grade and depth of invasion. Nicolau et al. have compared CEUS with conventional ultrasonography and showed an improvement in tumor detection (88.3% vs 72%) and the ability to detect more tumors per patient (66% vs 61%) [7]. Both modalities were poor in detecting very small lesions. Sensitivity for detecting lesions <5 mm in size was considerably worse than those >5 mm in size using CEUS (29% vs 95%), and this shortcoming has been replicated in similar studies. CEUS has also been added to color Doppler ultrasonography to differentiate between high-grade and low-grade tumors with improvements in sensitivity from 87.5% to 92% and specificity from 60% to 85.7% [9, 10]. 3D virtual sonography with multiplanar reconstruction has also been used as a method for detecting tumors. When comparing it to standard cystoscopy, 3D sonography showed a sensitivity of 96% and a specificity of 70.6% [11]. While the performance of these ultrasonographic techniques has demonstrated a promising performance, they have not been adopted in the standard diagnostic algorithm for this malignancy.
Computed tomography (CT) is commonly employed for the evaluation of the upper urinary tract in patients with hematuria, and it is not uncommon for a sizeable bladder tumor to be identified using this modality. However, the poor performance of CT in identifying small and/or sessile bladder tumors has not permitted CT to replace cystoscopy in the hematuria workup. With the use multidetector CT (MDCT), bladder lesions have been identified more readily. In their study, Wang et al. detected all but 1 of 44 bladder tumors, while other studies have shown high specificities of 94% to 99% and sensitivities of 85% to 87% with MDCT [12,13,14]. The use of virtual endoscopy by CT and magnetic resonance imaging (MRI) has also been used in other hollow organ structures to obtain an endoluminal image, plausibly allowing for better tumor detection. A meta-analysis was performed comparing conventional ultrasound and virtual cystoscopy with both MRI and CT. Assessment of 26 studies showed that the sensitivity for CT cystoscopy, MR virtual cystoscopy, and US was 94%, 91%, and 78%, respectively, when compared to conventional cystoscopy with or without histopathologic confirmation [15].
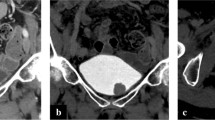
Though CT has shown promise in detecting bladder tumors, mp-MRI has been more extensively studied due to its better soft tissue imaging properties. Mp-MRI is able to not only identify some bladder tumors but can predict the depth of tumor invasion. Recently, the Vesical Imaging-Reporting and Data System (VI-RADS) was developed in order to help standardize reporting of bladder tumors and allow for better comparison of results between patients [16••]. VI-RADS incorporates T2-weighted (T2W), diffusion-weighted imaging (DWI), and dynamic contrast-enhancing (DCE) sequences to assess the bladder. T2W is predominantly used to identify the low-intensity muscularis propria line, which can help determine muscle invasion.
DCE MRI enables in vivo assessment of blood flow and permeability in tumor tissue using paramagnetic contrast agents. These contrast agents are taken up more readily by tumor relative to surrounding tissue due to abnormal vasculature allowing for greater permeability. This allows for the generation of signal and concentration-time curves that can be analyzed relative to surrounding tissue [17]. DCE, unlike other single-phase acquisitions also has the ability to discriminate the early enhancing mucosa from muscularis propria, which physiologically does not enhance early. In the DCE sequence, early tumoral enhancement with concomitant enhancement of the muscularis or perivesical fat is concerning for advanced disease [16••].
DWI is the final sequence used to assess the bladder, and it is constructed by quantifying the diffusion of water molecules in tissues without any contrast agents, tracers, or exposure to radiation. In this measure, malignant lesions exhibit high signal intensity as a result of their higher cellularity, tissue disorganization, and decreased extracellular space, all of which restrict water diffusion. The extent of the diffusion of water molecules can be quantitatively expressed as apparent diffusion coefficient (ADC) values. Lesions with high cellularity restrict diffusion would have corresponding low signal on ADC and high signal on DWI [18]. Tumors are hyperintense on DWI; muscularis propria is intermediate, while tumor stalk and mucosa present with low intensity on DWI. These three sequences are used to calculate a final five-point VI-RADS score.
The accuracy of the VI-RADS system has been assessed by various groups showing that the area under the receiver operating curves were 0.90 to 0.94 in treatment-naive patients [19,20,21]. The VI-RADS scoring system has subsequently been validated for likelihood of detrusor muscle invasion. In a study by Wang et al., bladder tumors in 340 patients without prior treatment were retrospectively categorized according to the 5-point scoring system and compared with post-cystectomy pathology [20]. Both the VI-RADS score and its components were associated with muscle-invasive disease (p < 0.001). The area under the receiver operating characteristic curve for VI-RADS for muscle invasion was 0.94, and the sensitivity and specificity of a VI-RADS score of 3 or greater were 87.1% and 96.5%, respectively. The VI-RADS system has also shown excellent intraobserver variability rates with intraclass correlation coefficients of 0.85–0.92 in most studies, though one study showed a lower coefficient of 0.73 between two radiologists with significantly different sensitivities and specificities in detecting tumors [19,20,21].
Performance of Diagnostic Modalities After Systemic Therapy
In most bladder-sparing protocols, patients with MIBC who achieve a CR to initial treatment with maximal trans-urethral resection of bladder tumor (TURBT) and induction chemoradiotherapy are potential candidates for bladder preservation, whereas patients with residual cancer are recommended to undergo salvage radical cystectomy. Therefore, accurate evaluation of therapeutic response is paramount for optimal patient selection, with imaging techniques playing a critical role.
In MIBC patients who have elected for NAC and radical cystectomy, those who are found to have no residual tumor in the bladder specimen tend to have the best long-term oncologic outcomes. This fact has led some investigators to question whether cystectomy is necessary in those patients who achieve a complete response (CR). Mazza et al. examined the outcomes of patients with MIBC who elected for close surveillance following a clinical CR after platinum-based NAC. CR was defined as absent tumor on post-chemotherapy cystoscopy and bladder biopsy, negative urine cytology, and normal cross-sectional imaging. In their series of 148 patients, the 5-year disease-specific, cystectomy-free, and recurrence-free survival rates were 90%, 76%, and 64%, respectively. Furthermore, salvage radical cystectomy prevented cancer-specific death in the majority of patients who subsequently relapsed. This data provides evidence that bladder preservation after achieving CR with neoadjuvant chemotherapy can result in acceptable oncologic outcomes. Careful patient selection will be paramount in achieving successful outcomes with such an approach, and it is unclear whether current endoscopic and diagnostic imaging techniques will be able to accurately differentiate patients with a true CR versus those with subclinical disease who may be destined to recur and/or progress.
Conventional MRI
In the post-TURBT and chemoradiotherapy (CRT) setting, conventional MRI seems to be more limited in its diagnostic performance compared to mp-MRI. For instance, in a study by Nishimura et al., 27 patients who underwent total or partial cystectomy for invasive bladder tumors underwent pre-cystectomy MRI [22]. Eight cases had received NAC (group A), ten cases had received CRT (group B), and nine cases had received preoperative staging biopsy alone (group C). Pathologic stage was assessed by histologic examination of the entire bladder wall from the surgical specimen. Tumor stage assessed by MRI was consistent with final pathology in 16 out of 27 cases (59.3%), with the MRI over-staging and under-staging the primary tumor stage in seven and four cases, respectively. Five of the seven over-staging cases were predicted to be pT2a or pT2b by MRI but were not found to have any residual tumor on final pathology.
On the other hand, all four instances of under-staging would not change clinical course as they were all changed from cT2b to pT3a. The accuracy of staging was 75%, 30%, and 77.8% in groups A, B, and C, respectively. The authors posited that CRT induces local fibrotic changes and inflammatory infiltrations that may manifest as bladder wall thickening and alter interpretation of images, thereby making precise staging with conventional MRI particularly difficult.
Additionally, after combined therapy with maximal TURBT and chemotherapy, bladder cancer bulk volume may regress yet remain persistent as a flat lesion [18]. Therefore, anatomic assessment of therapeutic response based on RECIST criteria on T2-weighted imaging may not accurately discern remnant cancerous tissue from secondary inflammatory changes.
DCE MRI
Functional MRI with DCE and DWI sequences has recently shown promise as a valuable tool in the post-CRT setting. Schrier et al. first discussed MRI to predict chemotherapy response for locally advanced bladder cancer [23]. In this prospective study, 36 patients with regionally metastatic or unresectable bladder transitional cell carcinoma underwent mp-MRI before and after two, four, and six cycles of chemotherapy. After two cycles of chemotherapy, the accuracy, sensitivity, and specificity in distinguishing responders from nonresponders with conventional MRI were 69%, 81%, and 50%, respectively. However, the DCE sequence showed an accuracy, sensitivity, and specificity of 92%, 91%, and 93%, respectively. The considerable improvement in accuracy and specificity distinguished DCE MRI in this patient population. Responders to chemotherapy based on DCE MRI also were shown to have better median disease-specific survival than nonresponders (42 months vs. 12 months, p < 0.0001).
In a study by Donaldson et al., 21 patients with localized bladder cancer underwent DCE MRI before and following NAC [24]. Regions of interest were defined as areas suspicious for residual tumor on T2W, and various parameters within these regions were measured including relative signal intensity and plasma perfusion. The bladder was subsequently examined histologically after cystectomy for evidence of residual tumor or treatment effect including hemorrhagic inflammation. Twenty-four abnormal sites were identified, of which 10 were residual tumor and 14 were deemed treatment effect. Median relative signal intensity and plasma perfusion were significantly higher in areas of residual tumor compared to those with treatment effect (median relative signal intensity = 2.9 vs. 1.7, p < 0.001; plasma perfusion = 20.7 vs. 9.1 ml/100 ml/min, p = 0.03). The sensitivity and specificity for differentiating residual tumor from treatment effects were 70% and 100% for median relative signal intensity, 60% and 86% for plasma perfusion, and 75% and 100% when combined. This once again reiterates the strength of DCE as a modality to effectively discriminate between treatment effect and residual tumor after chemotherapy.
In a study by Chakiba et al., 12 patients with localized bladder cancer were prospectively evaluated by DCE MRI before and after two courses of cisplatin-based NAC [25]. Size and thickness of tumors were measured as well as relative enhancement at the arterial and venous phases. Histological examination after NAC by either cystectomy or radical TUR prior to CRT showed CR for 6 out of 12 patients. After NAC, relative enhancement at the venous phase was significantly different between patients who were found to have a CR and patients without a CR (p = 0.04) with a cutoff value of 40%. For this cutoff value, sensitivity, specificity, and accuracy were 83.33%. This study only assessed if changes in MRI were predictive of downgrading to pT0. Though this study was hampered by a small sample size, these results suggest that DCE MRI may be a useful tool in the neoadjuvant chemotherapy setting to improve selection for either surgery or bladder-sparing approaches.
DWI
Yoshida et al. studied the role of DWI in predicting sensitivity of MIBC to CRT [26]. They examined 23 patients with MIBC who underwent induction CRT consisting of radiotherapy to the pelvis (40 Gy) with two cycles of cisplatin (20 mg/day for 5 days) followed by partial or radical cystectomy. All patients underwent DWI before initiation of chemoradiation, and associations with ADC values with chemoradiation sensitivity were analyzed. Thirteen patients (57%) achieved pathologic CR to CRT. These CRT-sensitive MIBCs showed significantly lower ADC values than CRT-resistant MIBCs (p = 0.0003). Multivariate analysis identified ADC value as the only significant and independent predictor of CRT sensitivity. With a cutoff ADC value at 0.74 × 10(-3) mm (2)/s, sensitivity, specificity, and accuracy in predicting CRT sensitivity was 92%, 90%, and 91%, respectively. Therefore, this study demonstrated DWI’s potential as an imaging biomarker for predicting response to bladder-sparing CRT in patients with MIBC.
Furthermore, this group also investigated the capability of the different aspects of mp-MRI in assessing the therapeutic response in 21 patients of the prior patient cohort [27]. The MRI results were compared with final pathology of surgical specimen. The sensitivity/specificity/accuracy of T2W, DCE, and DWI in predicting pathologic response was 43%/45%/44%, 57%/18%/33%, and 57%/92%/80%, respectively. Despite comparable sensitivity, DWI was significantly higher in specificity and accuracy to T2W (P = 0.03 and 0.02, respectively) and DCE MRI (p = 0.002 for both). This was the first study to show superiority of DWI sequences over T2W and DCE for assessing therapeutic response to induction CRT against MIBC with high specificity. It is important to note the inferior performance of DCE MRI in the CRT setting as compared to the NAC setting, which suggests that DCE may have a limited role in predicting response after CRT.
Cystoscopy
Cystoscopy has been evaluated as one method for assessing response to NAC with somewhat mixed results. In 2015, Mansour et al. reported on a series of 101 patients who received NAC prior to radical cystectomy [28]. All patients underwent initial TURBT during which photographs were taken and saved in their database. Outpatient flexible cystoscopy was then performed after two cycles of NAC to evaluate response. Patients were divided into two groups: 60 were responders (those with decreased tumor volume or no evidence of tumor), while 41 were nonresponders (those who had no change in tumor volume or tumor volume progression). All patients underwent subsequent radical cystectomy and pelvic lymphadenectomy.
Pathologic tumor downstaging was observed in 41 of 60 patients (69.5%) in the cystoscopic responders and 11 of 41 patients (26.4%) in the cystoscopic nonresponders. In the responders, 22 patients (36.5%) were downstaged to pT0, which is consistent with prior reports. An additional 16 patients (26.5%) were downstaged to NMIBC (pTis/T1). Conversely, in the nonresponders, only one patient (2.5%) was downstaged to pT0, and an additional one patient was downstaged to non-muscle invasive disease (pT1). Multivariate analysis showed that cystoscopy findings were independent predictors of both extravesical disease (>pT2) and pathologic downstaging.
This study suggests that in-office, flexible cystoscopy may be useful in evaluating response to NAC. Specifically, it can be utilized to predict which patients have residual muscle-invasive disease and are not acceptable candidates for bladder-sparing procedures. It does not seem to be as accurate in differentiating between pT0 versus pTa/T1/CIS. Differentiating between pT0 and NMIBC may not be of considerable clinical importance as large retrospective study by Zargar et al. of 1500 patients undergoing NAC and RC showed no difference in overall survival in patients who were pT0 at RC compared to those who had residual NMIBC [29].
In contrast to the Mansour study, Meyer et al. reported on a series of approximately 300 patients who underwent cystoscopy after NAC and prior to radical cystectomy [30]. Biopsy or TURBT was performed on 118 of these patients that had visible lesions. In their cohort, 57 of those 118 patients had no evidence of disease on biopsy or TUR, but only 26 out of 57 (46%) were confirmed to have pT0 disease at cystectomy. Out of the 118 patients, 101 were determined to have T0 or NMIBC based on cystoscopy and biopsy, 61 patients (60%) were confirmed to have non-muscle invasive disease on final pathology. Sensitivity and specificity of post-NAC biopsy was reported at 65.2% and 89.7%, respectively. If imaging was added to the evaluation, sensitivity increased to 98.3% and specificity decreased to 19.2%, though which imaging modality used was not reported. On multivariate analysis, they found that lack of tumor progression from non-muscle invasive disease at initial diagnosis, ypT0 pathology and tumor >2 cm in size, were predictive of accurate biopsy. They concluded that cystoscopy and biopsy may not be accurate in determining response to NAC and suggested that one should exercise caution if planning to deviate from standard of care based on cystoscopy findings alone.
Recently, researchers at Fox Chase Cancer Center reported on the interim results of a prospective study which incorporates a standardized bladder map and biopsies at time of radical cystectomy to evaluate the concordance of cystoscopy and biopsy with final RC pathology [31•]. They included any patient undergoing RC, and while patients did not have to receive NAC or have MIBC to be included in the study, 57% received NAC and 63% had MIBC. At time of interim analysis, 24 of 49 patients (49%) were found to have negative biopsies. However, pT0 in the bladder specimen after radical cystectomy was found in only 11 patients (22%). Ten of the 24 patients (42%) with no detectable disease on biopsy were found to be pT0 on the final cystectomy pathology, and 17 of these patients (71%) were shown to be either pT0 or to harbor NMIBC on the final specimen. This data translates to a 29% false negative rate for cystoscopy and biopsy for detecting ≥pT2.
Results of this prospective study shed light on some of the serious limitations of cystoscopy and biopsy on determining which patients truly have NMIBC. It is important to note that this study incorporated systemic bladder mapping with biopsies of any suspicious areas and also 2 biopsies of random areas in the bladder. Despite the generous biopsy sampling, there was still a considerable false negative rate. Combining information from all of these studies demonstrates that cystoscopy +/- biopsy may be useful in determining obvious nonresponders to CRT or NAC, which would preclude further bladder-sparing measures. However, accurate local tumor staging via cystoscopy +/- biopsy alone may not be accurate enough to predict a pathologic CR.
CT and PET
The role of CT in the evaluation of response to NAC for MIBC has also been evaluated, specifically its utility in predicting pathologic and oncologic outcomes. Fukui et al. reported on a series of 59 patients at their institution who underwent RC for MIBC following NAC [32]. They defined radiologic response rate (RRR) as (Pre-NAC tumor diameter–post-NAC tumor diameter)/(pre-NAC tumor diameter). RRR equal to 1 indicated CR and ≥ 30% was defined as partial response. They found that although there was no statistical difference in RRR between patients with and without viable tumor at RC, there was a significant difference between two different groups: (1) those who were found to have ≤pTa/Tis versus ≥pT1 and (2) those with ≤pT1 versus those with ≥pT2 at RC. These results were also found to translate to statistically significant increases in recurrence-free, disease-specific, and overall survival.
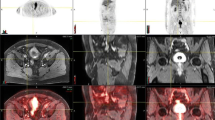
Given that hemorrhagic inflammation and necrosis after NAC can mimic residual tumor on CT and MRI, 18F-fluorodeoxyglucose with positron emission tomography (FDG/PET) with CT has been studied to further enhance radiologic evaluation of NAC response in MIBC. Soubra et al. performed a retrospective review of 37 patients who underwent FDG/PET scan at diagnosis of MIBC and again after completion of NAC and RC [33]. The authors specifically evaluated maximum standardized uptake value (SUVmax) on the pre-NAC and post-NAC FDG/PET scans, and the percentage change between the two values was used to assess response to chemotherapy. CR was defined as a reduction of 100% of SUVmax, and a chemosensitive tumor was defined as greater than 75% reduction in SUVmax but less than 100% reduction. In determining a pathologic CR, FDG/PET had a sensitivity of 75% and specificity of 90%. In order to assess FDG/PET’s ability to identify downstaging of tumors from MIBC to NMIBC, the authors assessed if detecting a chemosensitive response was predictive of this downstaging. If a mass was found to be a “chemosensitive tumor” per FDG/PET, it had a sensitivity of 83% and specificity of 94% to detecting downstaging to NMIBC. Notably, though, one patient had a complete response on FDG/PET but was found to have a small focus of pT2 disease on final pathology. Importantly, the authors note that a history of any intravesical chemotherapy may falsely elevate FDG activity on subsequent scan. This was not applicable in their study, as none of their patients received intravesical chemotherapy because they were all suspected to have muscle-invasive disease prior to, or at the time of, initial TURBT, but would be important to remember when applying the results of this study more broadly. This is a small study, and currently, any suggestion of complete response on FDG/PET should likely be verified by other methods prior to making any prognostic determinations or treatment decisions; however this is an area that merits future research.
Conclusion
Current diagnostic techniques are relatively accurate in local tumor staging prior to systemic chemotherapy +/- radiation and may eventually replace histologic staging from the TURBT specimen. As chemotherapeutics become more intertwined in the care of the MIBC patient, our understanding of which patients benefit from radical cystectomy and which ones can be spared from it continues to grow. Integrating various imaging modalities may allow practitioners to better select which patients can undergo bladder-sparing regimens and avoid the morbidity of radical cystectomy and urinary diversion. Further work needs to be done to understand which specific diagnostic modality should be utilized and what factors are prognostic for better outcomes, which will ultimately help to select the optimal treatment for each individual patient.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
Yeung C, Dinh T, Lee J. The health economics of bladder cancer: an updated review of the published literature. Pharmacoeconomics. 2014;32(11):1093–104.
Waingankar N, Mallin K, Smaldone M, Egleston BL, Higgins A, Winchester DP, et al. Assessing the relative influence of hospital and surgeon volume on short-term mortality after radical cystectomy. BJU Int. 2017;120(2):239–45.
Efstathiou JA, Spiegel DY, Shipley WU, Heney NM, Kaufman DS, Niemierko A, et al. Long-term outcomes of selective bladder preservation by combined-modality therapy for invasive bladder cancer: the MGH experience. Eur Urol. 2012;61(4):705–11.
Advanced Bladder Cancer Meta-analysis C. Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur Urol. 2005;48(2):202–5 discussion 205-206.
Mazza P, Moran GW, Li G, Robins DJ, Matulay JT, Herr HW, et al. Conservative management following complete clinical response to neoadjuvant chemotherapy of muscle invasive bladder cancer: contemporary outcomes of a multi-institutional cohort study. J Urol. 2018;200(5):1005–13.
Nicolau C, Bunesch L, Peri L, Salvador R, Corral JM, Mallofre C, et al. Accuracy of contrast-enhanced ultrasound in the detection of bladder cancer. Br J Radiol. 2011;84(1008):1091–9.
Stamatiou K, Papadoliopoulos I, Dahanis S, Zafiropoulos G, Polizois K. The accuracy of ultrasonography in the diagnosis of superficial bladder tumors in patients presenting with hematuria. Ann Saudi Med. 2009;29(2):134–7.
Drudi FM, Di Leo N, Malpassini F, Antonini F, Corongiu E, Iori F. CEUS in the differentiation between low and high-grade bladder carcinoma. J Ultrasound. 2012;15(4):247–51.
Li Q, Tang J, He E, Li Y, Zhou Y, Wang B. Differentiation between high- and low-grade urothelial carcinomas using contrast enhanced ultrasound. Oncotarget. 2017;8(41):70883–9.
Kocakoc E, Kiris A, Orhan I, Poyraz AK, Artas H, Firdolas F. Detection of bladder tumors with 3-dimensional sonography and virtual sonographic cystoscopy. J Ultrasound Med. 2008;27(1):45–53.
Wang LJ, Wong YC, Ng KF, Chuang CK, Lee SY, Wan YL. Tumor characteristics of urothelial carcinoma on multidetector computerized tomography urography. J Urol. 2010;183(6):2154–60.
Martingano P, Stacul F, Cavallaro M, Casagrande F, Cernic S, Belgrano M, et al. 64-Slice CT urography: 30 months of clinical experience. Radiol Med. 2010;115(6):920–35.
Helenius M, Brekkan E, Dahlman P, Lonnemark M, Magnusson A. Bladder cancer detection in patients with gross haematuria: computed tomography urography with enhancement-triggered scan versus flexible cystoscopy. Scand J Urol. 2015;49(5):377–81.
Qu X, Huang X, Wu L, Huang G, Ping X, Yan W. Comparison of virtual cystoscopy and ultrasonography for bladder cancer detection: a meta-analysis. Eur J Radiol. 2011;80(2):188–97.
•• Panebianco V, Narumi Y, Altun E, et al. Multiparametric magnetic resonance imaging for bladder cancer: development of VI-RADS (vesical imaging-reporting and data system). Eur Urol. 2018;74(3):294–306 This is the original article which discusses the creation and details of the VI-RADS system. It outlines each section of the scoring system and illustrates them with examples.
Rabie E, Faeghi F, Izadpanahi MH, Dayani MA. Role of dynamic contrast-enhanced magnetic resonance imaging in staging of bladder cancer. J Clin Diagn Res. 2016;10(4):TC01–5.
Yoshida S, Koga F, Kobayashi S, Tanaka H, Satoh S, Fujii Y, et al. Diffusion-weighted magnetic resonance imaging in management of bladder cancer, particularly with multimodal bladder-sparing strategy. World J Radiol. 2014;6(6):344–54.
Ueno Y, Takeuchi M, Tamada T, Sofue K, Takahashi S, Kamishima Y, et al. Diagnostic accuracy and interobserver agreement for the vesical imaging-reporting and data system for muscle-invasive bladder cancer: a multireader validation study. Eur Urol. 2019;76:54–6.
Wang H, Luo C, Zhang F, et al. Multiparametric MRI for bladder cancer: validation of VI-RADS for the detection of detrusor muscle invasion. Radiology. 2019;291(3):668–74.
Barchetti G, Simone G, Ceravolo I, Salvo V, Campa R, del Giudice F, et al. Multiparametric MRI of the bladder: inter-observer agreement and accuracy with the vesical imaging-reporting and data system (VI-RADS) at a single reference center. Eur Radiol. 2019;29:5498–506.
Nishimura K, Fujiyama C, Nakashima K, Satoh Y, Tokuda Y, Uozumi J. The effects of neoadjuvant chemotherapy and chemo-radiation therapy on MRI staging in invasive bladder cancer: comparative study based on the pathological examination of whole layer bladder wall. Int Urol Nephrol. 2009;41(4):869–75.
Schrier BP, Peters M, Barentsz JO, Witjes JA. Evaluation of chemotherapy with magnetic resonance imaging in patients with regionally metastatic or unresectable bladder cancer. Eur Urol. 2006;49(4):698–703.
Donaldson SB, Bonington SC, Kershaw LE, Cowan R, Lyons J, Elliott T, et al. Dynamic contrast-enhanced MRI in patients with muscle-invasive transitional cell carcinoma of the bladder can distinguish between residual tumour and post-chemotherapy effect. Eur J Radiol. 2013;82(12):2161–8.
Chakiba C, Cornelis F, Descat E, Gross-Goupil M, Sargos P, Roubaud G, et al. Dynamic contrast enhanced MRI-derived parameters are potential biomarkers of therapeutic response in bladder carcinoma. Eur J Radiol. 2015;84(6):1023–8.
Yoshida S, Koga F, Kobayashi S, et al. Role of diffusion-weighted magnetic resonance imaging in predicting sensitivity to chemoradiotherapy in muscle-invasive bladder cancer. Int J Radiat Oncol Biol Phys. 2012;83(1):e21–7.
Yoshida S, Koga F, Kawakami S, Ishii C, Tanaka H, Numao N, et al. Initial experience of diffusion-weighted magnetic resonance imaging to assess therapeutic response to induction chemoradiotherapy against muscle-invasive bladder cancer. Urology. 2010;75(2):387–91.
Mansour AM, Soloway MS, Eldefrawy A, Singal R, Joshi S, Manoharan M. Prognostic significance of cystoscopy findings following neoadjuvant chemotherapy for muscle-invasive bladder cancer. Can J Urol. 2015;22(2):7690–7.
Zargar H, Zargar-Shoshtari K, Lotan Y, Shah JB, van Rhijn B, Daneshmand S, et al. Final pathological stage after neoadjuvant chemotherapy and radical cystectomy for bladder cancer-does pT0 predict better survival than pTa/Tis/T1? J Urol. 2016;195(4 Pt 1):886–93.
Meyer A, Brant A, Nichols P, Kates M, Reese A, Hahn N, et al. Inaccuracy of clinical staging after neoadjuvant chemotherapy for muscle invasive bladder cancer. J Urol. 2018;199.
• Asghar A, Parker D, McGowan T, et al. Prospective evaluation of cystoscopy and bladder mapping reveals nearly a 30% miss rate for pT2 pathology. J Urol. 2019;201(Supplement 4):e1194 These two recently presented abstracts give us much better information about the limitations of cystoscopy and biopsy in determining the response to neoadjuvent chemotherapy.
Fukui T, Matsui Y, Umeoka S, Inoue T, Kamba T, Togashi K, et al. Predictive value of radiological response rate for pathological response to neoadjuvant chemotherapy and post-cystectomy survival of bladder urothelial cancer. Jpn J Clin Oncol. 2016;46:560–7.
Soubra A, Gencturk M, Froelich J, Balaji P, Gupta S, Jha G, et al. FDG-PET/CT for assessing the response to neoadjuvant chemotherapy in bladder cancer patients. Clin Genitourin Cancer. 2018;16(5):360–4.
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Cancer Institute, NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sandeep Gurram, Akhil Muthigi, Jillian Egan, and Lambros Stamatakis each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on New Imaging Techniques
Rights and permissions
About this article
Cite this article
Gurram, S., Muthigi, A., Egan, J. et al. Imaging in Localized Bladder Cancer: Can Current Diagnostic Modalities Provide Accurate Local Tumor Staging?. Curr Urol Rep 20, 82 (2019). https://doi.org/10.1007/s11934-019-0948-7
Published:
DOI: https://doi.org/10.1007/s11934-019-0948-7