Abstract
Purpose of Review
Patients with localized renal cell carcinoma (RCC) are at risk of recurrence. The purpose of this review was to characterize the literature on recurrence rates and risk factors after diagnosis of localized RCC.
Recent Findings
Our search revealed that existing data examining the prevalence of recurrence rates predominantly originates from cohorts of patients diagnosed and treated in the 1980s to 1990s, and may therefore not be as useful for counseling for current patients today. Many nomograms including the Cindolo Recurrence Risk Formula, the University of California-Los Angeles (UCLA) Integrated Scoring System (UISS), the SSIGN score, the Kattan nomogram, and the Karakiewicz nomogram have shown value in identifying patients at higher risk for recurrence. Biomarkers and gene assays have shown promise in augmenting the predictive accuracy of some of the aforementioned predictive models, especially when multiple gene markers are used in combination. However, more work is needed in not only developing a model but also validating it in other settings prior to clinical use. Adjuvant therapy is a promising new treatment strategy for patients with high-risk disease. Importantly, too many surveillance strategies exist. This may stem from the lack of a consensus in the urological community in how to follow these patients, as well as the variable guideline recommendations.
Summary
In conclusion, contemporary recurrence rates are needed. Recurrence risk prediction models should be developed based on a series of more contemporary patients, and externally validated prior to routine clinical practice. Surveillance strategies following treatment of localized RCC need to be identified and standardized. Finally, there is a trend toward personalizing surveillance regimens to more appropriately screen patients at higher risk of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Renal cell carcinoma (RCC) is the 6th leading cause of cancer in men and the 10th cause of cancer in women in the USA. There will be 62,700 new cases of kidney and renal pelvic cancer including 14,240 deaths in the USA in 2016 [1]. The incidence of RCC has been rising by 2–3% globally per decade, though incidence and mortality rates have been noted to be stabilizing in the last few years in many countries in Europe [2]. Established risk factors for RCC include smoking, obesity, acquired renal cystic disease, and germline mutations [3]. Thought to be in part due to the increased use of cross-sectional imaging, there has been an increase in the diagnosis of localized RCC over the last few decades, with the prevalence of age-adjusted rates of localized RCC in the USA rising by +4.55% (95% confidence interval [CI] 4.34–4.76%, p < 0.001) between 1975 and 2009 (from 2.99 to 12.16 per 100,000 person-years) [4]. Additionally, the mortality rates for localized RCC between 1975 and 2009 continue to increase by 3.92%/year (95% CI 3.45–4.39, p < 0.001) [4].
Once localized RCC is diagnosed, a radical or partial nephrectomy (depending on the characteristics of the lesion) is the gold standard of treatment in patients who are surgical candidates [5]. Other options for localized lesions include active surveillance and ablative techniques. Contemporary population-based data suggest that approximately 69% of patients undergo surgery, and 31% are non-surgically managed [6]. Among non-surgically managed patients, ablation is offered to 30% of patients and the remaining are treated with observation/active surveillance [7]. Unfortunately, between 20 and 40% of patients who are treated for localized disease have been shown to have recurrence [8].
This review attempts to characterize contemporary data on recurrence after diagnosis and/or treatment for localized RCC by presenting rates of recurrence, risk factors for recurrence, models that were developed for the purpose of predicting recurrence, the integration of biomarkers in such models, and the intricacies of the various surveillance protocols in existing guidelines.
Prevalence/Rates of Recurrence
Recurrence-Free Survival Rates
There have been several large retrospective studies examining recurrence rates after surgery for RCC (Table 1). Of note, the majority of data (seven out of eight studies) included patients who underwent a nephrectomy in the 1980s–1990s. The sample sizes ranged between 559 and 2404 patients. All studies originated from institutional cohorts, with no population-based cohorts or hospital-based registries.
Overall, the 5-year recurrence-free survival (RFS) ranged from 41.9 to 97.8%. However, the cohorts varied greatly in the distribution of the stage of disease and the method of treatment (partial versus radical nephrectomy and laparoscopic versus open techniques). The most contemporary cohort of patients is comprised of 1541 patients from the Cleveland Clinic who underwent partial nephrectomies for cT1a and cT1b tumors between years 1999 and 2008 [9•]. Distant metastases were detected in 59 patients (4.9%) following nephrectomy. The 5-year RFS ranged between 97.1 and 97.8% for clinical T1a tumors, and 92.7 and 93.1% for clinical T1b tumors, although this study examined lower stage tumors relative to some of the other studies listed in Table 1. Though there have not been studies directly comparing recurrence rates in older versus more contemporary cohorts for localized RCC, the 5-year RFS appears to be over 90% in patients with T1 disease after surgical management.
Timing of Recurrence
The greatest risk of recurrence appears to be within 5 years following surgery, but varies based on disease characteristics. Specifically, Adamy et al. examined a series of 2368 patients undergoing radical and partial nephrectomy with a median follow-up time of 49 months to determine when recurrence occurred after treatment. Of 256 patients who recurred, 212 patients (83%) experienced disease progression less than 5 years after surgery, and 44 patients (17%) more than 5 years after surgery. Factors associated with early (<5 years) versus late (≥5 years) recurrences were symptoms at presentation, tumor size, and pathological T stage [12]. The risk of recurrence also depends on risk groups. For example, Lam et al. stratified patients according to the risk groups developed by the University of California-Los Angeles Integrated Staging System (UISS). In patients with low-, intermediate-, and high-risk disease, the median time to recurrence was 28.9 months (mean 26.5 ± standard deviation [SD]: 17.1), 17.8 months (mean 25.5 ± SD: 23.9), and 9.5 months (mean 21.9 ± SD: 26.2), respectively [16]. This shows that higher risk patients according to the UISS are more likely to recur sooner, and as such, warrant closer surveillance early on in their disease course.
Sites of Recurrence
RCC recurs primarily in the lung (52–64%) and bone (9–15%) [12, 13, 17]. Other sites of recurrence include pancreas (3–7%), liver (5–11%), distant lymph nodes (4–7%), local recurrences (3–9%), brain (7%), adrenal gland (10–11%), and other sites (3–33%). Each site has a different time to recurrence, and (as noted above), time to recurrence by site generally decreases by the pathologic stage of the patient. For example, in patients with pT1 disease versus pT2 disease, the median months to diagnosis of lung metastases is 53 months (range 30–67) versus 31 months (range 4–67), 35–42 months versus 24 months (range 3–115) for bone metastases, and 18 months versus 11 months, respectively, for brain metastases [18].
Recurrence After Partial Versus Radical Nephrectomy
The comparative effectiveness of partial versus radical nephrectomy has been predominantly focused on renal function preservation, and cancer-specific mortality [19,21,21]. With respect to recurrence, the consensus is that a partial nephrectomy is non-inferior to a radical nephrectomy [22, 23]. For example, Leibovich et al. examined 932 patients with 4 to 7 cm localized renal masses treated with partial or radical nephrectomy. The risk of developing metastases was not statistically significantly different between radical and partial nephrectomy when adjusting for adverse features (hazard ratio [HR]: 1.76, 95% confidence interval [CI] 0.64–4.83, p = 0.273) [23].
Recurrence After Minimally Invasive Versus Open Procedures
Minimally invasive techniques for both radical and partial nephrectomies are used with increasing frequency. Population-based data shows that patients diagnosed with RCC in 2009 are 2.6 times more likely than patients in 2004 to receive a laparoscopic RN than an open RN (CI 1.15 to 5.73, p = 0.02) [24]. Oncologic outcomes for open RN versus laparoscopic RN as well as open PN versus laparoscopic PN appear to be equivalent [9•, 25, 26]. Long-term oncologic outcomes are emerging for robotic PN as well with 5-year cancer-free survival rates of 97.8% for patients with localized renal cell carcinoma [27]. To date, no specific comparisons between minimally invasive versus open procedures have been made for RFS.
Recurrence After Ablation Versus Surgery
Ablation for small renal masses is recommended in some select patients. In general, patients receiving ablative therapies are older, with one or more baseline medical conditions, and considered non-surgical candidates. The American Urology Association (AUA) renal mass guideline presents comparisons of recurrence rates for ablative techniques (i.e., radiofrequency ablation and cryoablation) and surgery, and observed that RFS was lower for ablative versus surgical techniques. Specifically, they found that RFS ranged between 83.2 and 94.7% for various tumor ablation techniques at a median follow-up of 18.2 and 19.4 months (for cryoablation versus radiofrequency ablation, respectively) versus 97.1 and 99.7% in patients who underwent surgery (all p < 0.05) with median follow-ups ranging from 15.0 to 58.3 months varying by surgical approach [28]. Moreover, patients selected to undergo tumor ablation are considerably older and sicker at diagnosis compared to their surgically managed counterparts. A recent meta-analysis that included 107 studies compared the different treatment options for localized RCC. Outcomes included oncologic efficacy, renal functional outcomes, overall survival, and quality of life. This study corroborated the finding that RFS was worse for a single thermal ablation than partial nephrectomy (HR 0.37, 95% CI 0.15 to 0.89). However, the authors noted that when multiple ablations were done, the difference between surgery and ablation was no longer significantly different [29]. Given the absence of level one evidence, it remains difficult to truly compare the rate of disease progression between the two treatment modalities when considering the differences related to patient characteristics during treatment selection.
Progression on Active Surveillance
Active surveillance is an accepted management option for patients at high surgical risk [28]. Studies have shown low growth rates of tumors (0.25 cm/year, SD 0.49 cm/year) and low rates of progression to metastatic disease [30]. A meta-analysis comprised of 18 studies found that of patients on active surveillance, 45.4% (129 patients) underwent delayed intervention at a mean of 30.5 months (range 6.4–143 months, SD 21.8 months) primarily due to patient preference (57.2%) and tumor growth (35.7%) [31]. The same analysis identified 18 of 880 patients who progressed to metastatic disease. The mean time to metastasis was 40.2 months [31].
Prognostic Factors for Recurrence in Nonmetastatic RCC
Several risk factors have been studied for the purpose of identifying patients at high risk of recurrence. Other risk factors have not specifically been tested for predicting recurrence, but have shown to be highly associated with other oncological endpoints, such as cancer-specific mortality and overall survival.
Tumor Size
In patients with small renal masses (<4 cm), tumor size is not a reliable marker to distinguish between benign versus malignant or metastatic versus localized disease [11]. However, in patients with localized RCC who have undergone extirpative treatment, tumor size has been shown to be significantly associated with survival and recurrence, with local RFS decreasing significantly with each 1 cm increase in size of the tumor (p < 0.05) [10].
Presentation
Due to the increased utilization of imaging in the last decade, patients are increasingly presenting with incidentally found renal masses. Interestingly, patients who are symptomatic at presentation have been shown to have worse prognosis independent of the size of the tumor (HR 3.69, 95% CI 2.11–6.08, p < 0.001) [32]. It is worth observing that many of the risk models that were previously developed relied on symptoms at presentation as a risk factor. However, the population in which the models were developed on included between 52 and 60% of individuals who presented symptomatically [32,34,34], which is highly different from contemporary patients where symptomatic individuals may represent only 40% of the cohort [35].
TNM Classification
TNM Classification has been externally validated as a tool to accurately stratify the cancer-specific survival of patients with clear cell RCC. Although no formal assessment has been made with regard to how well the TNM classification can differentiate patients at high- versus low-risk of recurrence, patients with more advanced tumor or nodal stages are more likely to experience worse oncological outcomes.
ECOG Performance Status
Eastern Cooperative Oncology Group (ECOG) performance status is one of two components in the UISS model to predict survival [36]; though to the best of our knowledge, ECOG performance status has not been evaluated for prediction of disease recurrence.
Microvascular Invasion
Microvascular invasion (MVI) has been shown to be an independent predictor of disease recurrence in several instances. In a study by Dall’Oglio et al., within a cohort of 230 patients, the 5-year disease-free survival was 87.1% (95% CI 79–95%) for patients without MVI versus 27.2% (95% CI 14.9–50.3%, p < 0.001) in patients with MVI [37]. A recent meta-analysis comprised of 33 studies found that MVI was significantly associated with higher risks of cancer-specific mortality (HR 1.96, 95% CI 1.50–2.56, p < 0.001), recurrence (HR 2.75; 95% CI 1.97–3.823, p < 0.001), and developing distant metastases (HR 1.62; 95% CI 1.10–2.40, p < 0.001), but failed to be statistically significantly associated with all-cause mortality (HR 1.37, 95% CI 0.98–1.92, p = 0.112) [38].
Sarcomatoid Features
Sarcomatoid features can be present in all subtypes of RCC. Patients with sarcomatoid differentiation often present at a more advanced stage [39]. According to de Peralta-Venturina et al., in a stage-matched comparison of patients with and without sarcomatoid differentiation, patients with sarcomatoid features had a poorer prognosis. Specifically, the 5- and 10-year overall survival rates were 22 and 13% in patients with sarcomatoid differentiation versus 79 and 76% in patients without sarcomatoid differentiation for the same time points, respectively (p < 0.001) [39]. No studies have assessed the effect of sarcomatoid differentiation on the risk of recurrence.
Collecting System Invasion
Collecting system invasion has also been evaluated as a predictor of recurrence and disease progression [40,42,42]. A recent meta-analysis by Chen et al. pooled 17 studies and found that the RFS (HR 2.27, 95% CI 1.54–3.34, p < 0.001) and overall mortality (HR 1.45, 95% CI 1.26–1.66, p < 0.001) in patients with collecting system invasion were significantly higher than patients without collecting system invasion [43]. The increased risks in recurrence and mortality were most notable in patients with localized RCC.
Necrosis
Tumor necrosis has been shown to be associated with adverse prognostic factors [57] and to independently predict both cancer-specific survival [58] and progression to metastatic RCC [59]. Lam et al. found in a retrospective review of 311 patients with localized RCC that recurrence was higher in patients with tumor necrosis (HR 4.12, 95% CI 1.48–11.5, p = 0.0068) [57].
Thrombocytosis
An initial study on the role of pre-operative thrombocytosis (platelet count >400,000) included 180 patients with localized RCC. The authors found lower cancer-specific-free survival in patients with thrombocytosis than those without: median of 45.2 months (95% CI 29.5–60.8) versus 76.6 months (95% CI 70.9–82.2, respectively) (p = 0.002) [60]. More recently, a meta-analysis by Gu et al. examined 25 pooled studies and 11,458 patients for prediction of recurrence in patients with RCC and stratified their analyses according to disease stage. In patients with localized disease, the risk of recurrence was significantly higher in patients with thrombocytosis than those without (HR 6.68, CI 3.35–13.34, p < 0.001) [61].
Elevated C-Reactive Protein
C-reactive protein (CRP) levels have been shown to be associated with tumor progression and pro-inflammatory cytokine production. In a cohort of patients of all stages of RCC, CRP was independently associated with cancer-specific mortality [47]. It was also shown to increase the discrimination of the UISS score in predicting disease-specific mortality by +2.5% at 2 years (from 85.3 to 87.8%, p < 0.001) and +3.8% at 5 years (80.2 to 84.0%, p < 0.001) [47]. A recent meta-analysis among 24 pooled studies by Hu et al. examined CRP by stage and found that in patients with localized RCC, elevated CRP was associated with poorer cancer-specific survival (HR 3.49, 95% CI 2.93–4.05, p < 0.0001) and worse progression-free survival (HR 3.29, 95% CI 2.91–3.67, p < 0.0001) [62].
Surgical Margins
In patients treated with partial nephrectomies, the effect of positive surgical margins holds an unclear prognostic significance. In the literature, the rates of positive surgical margins vary between 1.7 and 7.8% [63, 64]. Kang et al. examined 1831 patients with pT1 clear cell RCC treated with partial nephrectomy. The positive margin rate was 1.7%. The authors did not find any difference in the rates of recurrence based on margin status (2.1% in patients with a negative margin versus 3.2% in patients with a positive margin, p = 0.492) [63]. However, given the low event rate, the study may have been underpowered. Shah et al. recently studied 1240 patients undergoing partial nephrectomies for localized RCC with up to stage pT3a [64]. Positive margin rates were 7.8% and the rate of recurrence was 5.6% after a median follow-up time of 33 months. The authors found that a positive surgical margin was associated with an increased risk of relapse in high-risk disease defined as pT2–T3 disease and Fuhrman grade III–IV (HR 7.48, 95% CI 2.75–20.34, p < 0.001) but not in low-risk disease (HR 0.62, 95% CI 0.08–4.75, p = 0.647) [64]. Consequently, the data may be indicative that patients with high-risk disease and positive margins should be closely monitored for recurrence.
Risk Models for Prediction of Recurrence in Patients with Localized RCC
Several developed prognostic risk models have included many of the aforementioned individual risk factors for prediction of outcomes in patients with RCC. However, only two models were formally developed for the purpose of predicting recurrence: the Cindolo Recurrence Risk Formula, which uses pre-operative tumor size and presence or absence of symptoms [32]; and the Kattan nomogram, which examines histologic type, tumor size, TNM classification, and presence or absence of symptoms [15, 34]. Other models were developed for the purpose of evaluating other oncological endpoints. For example, the UISS score which in the nonmetastatic setting includes ECOG performance status and Fuhrman grade was developed to assess overall survival [65]; the SSIGN nomogram which includes tumor stage, size, grade, and presence of necrosis was developed for prediction of cancer-specific survival [58]; and the Karakiewicz nomogram which includes TNM stage, tumor size, Fuhrman grade, histologic subtype, local symptoms, age, and sex was modeled to predict cancer-specific mortality [66]. In 2005, Cindolo et al. used data from six European centers to compare the discriminative accuracy of some of the above nomograms and found that the Kattan and UISS nomogram performed the best. In terms of RFS, the c-indices were as follows: Kattan 0.807 (95% CI 0.777–0.835), UISS 0.782 (95% CI 0.752–0.812), Cindolo 0.672 (95% CI: 0.640–0.704) [14]. Recently, the SSIGN nomogram was applied to a more contemporary cohort who had undergone partial and radical nephrectomies and demonstrated good discrimination for prediction of recurrence (c-index 0.84 and 0.82 for RN and PN cohorts, respectively) [67].
Biomarkers
Biomarkers are a potentially powerful tool that can provide additional predictive accuracy in identifying which patients are at highest risk for the recurrence of RCC. The predominant issues with the studies on biomarkers include the paucity of direct comparison and external validation, as well as the absence of comparisons with existing risk models that incorporate patient and disease characteristics. Table 2 is a compilation of several prominent biomarkers and their effects on c-indices when available. While a full review of all potential biomarkers is beyond the scope of the current review, included below is a sampling of more promising and/or recently identified biomarkers. Articles that more specifically examine biomarkers include Ngo et al. [68], Nogueira et al. [69], Crispen et al. [70], and Lam et al. [71].
IMP3
Insulin-like growth factor 2 mRNA-binding protein 3 has been shown to be associated with tumor aggressiveness. IMP3 binds to, localizes, and stabilizes mRNA during embryogenesis. More recently, enhanced IMP3 activity was found to activate the NF-κB pathway [72], which is an established transcription factor involved in cell proliferation, development, and tumorigenesis. IMP3 is an externally validated marker. In Hoffman et al., among 629 patients with localized RCC, patients with IMP3 positivity were nearly five times more likely to progress to distant metastasis than IMP3-negative patients (HR 4.71; 95% CI 3.44–6.43 [p < .001]) [44].
MET Variant rs11762213
c-Met is a receptor tyrosine kinase encoded by the MET proto-oncogene. Higher c-Met expression is associated with high-grade and high-stage tumors and is a poor prognostic factor [73]. rs11762213 is a small nucleotide polymorphism that maps to an enhancer region of MET, potentially altering regulation of MET. Hakimi et al. showed that the Met variant rs11762213 is an independent risk factor for decreased cancer-specific survival and RFS, then validated the biomarker. When used in combination with the SSIGN score, the MET variant increased the c-index slightly from 0.845 to 0.866 for prediction of death from the disease and from 0.719 to 0.738 for prediction of recurrence [45]. (See Table 2)
MicroRNAs
MicroRNAs are small noncoding nucleotide RNAs that regulate gene regulation at the post-transcriptional level though RNA interference. If a microRNA (miRNA) increases expression of an oncogene or decreases expression of a tumor suppressor gene, the tumor may be more aggressive [74]. miRNAs have been shown to have prognostic significance in colon, lung, breast, and ovarian cancer. Slaby et al. found an association between miRNA expression files and RCC recurrence. In the study, the authors examined 77 patients with clear cell RCC and obtained global miRNA expression files. They were able to identify a miRNA signature that was associated with relapse and in a validation phase identified three miRNAs (miR-145 (p = 0.05), miR-126 (p = 0.015), and miR-127-3p (p = 0.014)) that were significantly associated with decreased RFS [74].
Since then, multiple studies have identified and characterized miRNAs that appear to have a role in RCC tumorigenesis. A systematic review that examined the prognostic value of miRNAs identified two miRNAs that on a meta-analysis significantly affected overall survival, cancer-specific survival, and disease-free survival [75]. Aberrant miR-21 expression negatively affects overall survival (HR 2.29, 95% CI 1.28–4.08), cancer-specific survival (HR 4.16, 95% CI 2.49–6.95), and disease-free survival (HR 2.15, 95% CI 1.16–3.98) [75]. Conversely, miR-126 aberrant expression has a protective effect with respect to overall survival (HR 0.35, 95% CI 0.15–0.85), cancer-specific survival (HR 0.45 95% CI 0.30–0.69), and disease-free survival (HR 0.30, 95% CI 0.18–0.50) [75]. A prominent limitation of the miRNA studies is that there are many different signatures and miRNAs that have been associated with either worse or better prognosis, but very few overlap between the studies.
Carbonic Anhydrase IX
Carbonic Anhydrase IX is a protein mediated by the hypoxia inducible factor (HIF) complex and has been shown to play a role in tumorigenesis [76]. A recent meta-analysis in patients with all stages of RCC attempts to clarify the prognostic value of CAIX. They found that low CAIX expression is associated with worse disease-free survival (HR 1.89, 95% CI 1.20–2.98, p = 0.006), overall survival (HR 2.03, 95% CI 1.28–3.21, p = 0.002), and progression-free survival rates (HR 2.62, 95% CI 1.14–6.05, p = 0.02) [77]. Unfortunately, CAIX as an adjunct to existing risk models to augment its prognostic value has not yet been studied.
Composite Biomarkers
Several studies have examined multiple gene assays to predict recurrence. Rini et al. developed a 16-gene assay that was shown in a multivariable analysis to be a significant predictor of recurrence [46]. Moreover, the addition of the recurrence score as calculated by the gene assay to the Leibovich score significantly improved the c-index from 0.74 to 0.81. The BioScore is another composite model that includes several established biomarkers including B7-H1, Survivin, and Ki-67 [48]. With the addition of the BioScore, the UISS discrimination significantly improved from 0.774 to 0.819, but only slightly improved for the SSIGN score nomogram from 0.821 to 0.837.
The Role of Metastatectomy and Local Treatment After Recurrence
Historically, given the poor response of advanced RCC to cytokine therapy, metastatectomy and local treatment have been explored as treatment options in recurrent or metastatic disease. This was initially well-described in a cohort of 278 patients with solitary recurrence where 51% of patients underwent a curative metastatectomy. The 5-year overall survival rate was 44% in patients who underwent curative metastatectomy compared to 14 and 11% in patients after noncurative metastatectomy and nonsurgical treatment, respectively [78]. Alt et al. further explored the role for metastatectomy in patients with multiple sites of recurrence and again found that patients with a complete metastatectomy had an improved median cancer-specific survival compared to those who did not have a complete resection (4.8 years versus 1.3 years; p < 0.001) [79].
Complete metastatectomy has been shown to be superior to incomplete metastatectomy or no local treatment in a systematic review with a longer median survival or cancer-specific survival was reported (14.8 months, range 13.3 to 21.0) [80]. However, all studies included contained a significant risk of treatment selection bias and additional confounding.
The Role for Adjuvant/Neoadjuvant Therapy for RCC
In the neoadjuvant setting, there has been some examination of neoadjuvant therapy to decrease tumor volume prior to surgery. A study by Zhang et al. gave 18 patients neoadjuvant sorafenib and noted a decrease in inferior vena cava thrombi tumor grade and a decrease in tumor size, enabling the surgery to proceed [81]. However, other studies examining patients in the metastatic setting have shown increased surgical complications in patients who receive pre-operative targeted therapy. For example, Jonasch et al. found that patients who had received pre-operative bevacizumab had delayed wound healing (20.9 versus 2%, p < 0.001) [82]. Harshman et al. studied 14 patients who had received a tyrosine kinase inhibitor (TKI) (sunitinib or sorafenib) pre-operatively compared to a cohort of 73 control patients [83]. Patients who had received TKI in the perioperative setting underwent pre-operative angioembolization if renal artery access was difficult and were noted to have worse adhesions making the surgery more challenging.
In the adjuvant setting, a seminal randomized, double-blind, phase III trial was recently completed and published assessing the efficacy of sunitinib versus placebo in patients with locoregional renal cell carcinoma at high-risk of tumor recurrence after nephrectomy. High-risk patients were identified via the UISS risk stratification and resulted in 615 eligible patients. Cancer-specific mortality-free survival rates were significantly improved for the sunitinib group compared to placebo (6.8 versus 5.6 years, HR 0.76, 95% CI 0.59–0.98, p = 0.03) [84••]. The use of adjuvant sunitinib in patients with high-risk disease is a promising new treatment strategy.
Surveillance for RCC
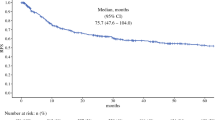
The American Urological Association (AUA), National Comprehensive Cancer Network (NCCN), and European Association of Urology (EAU) have set forth guidelines for the surveillance of RCC after localized treatment [5, 85, 86]. These guidelines are comprised of abdominal imaging, chest imaging, and laboratory testing. The guidelines stratify patients by risk-group, defined according to differing definitions (AUA and EAU with high, intermediate, and low risk, and NCCN with high and low risk). The AUA and NCCN guidelines also vary in their screening algorithm depending on whether the patient had a partial or radical nephrectomy. With the exception of the high- and intermediate-risk patients in the EAU guidelines, the recommendations are to image patients for up to 5 years (depending on treatment and risk), after which imaging is at the discretion of the urologist (Fig. 1).
A recent study by Sohn et al. used the SEER database and identified 7603 patients with localized RCC who underwent localized treatment. They examined practice patterns of surveillance and the correlation of increased surveillance with survival [87]. They noted poor adherence to the AUA screening guidelines where over 30% of patients did not receive a recommended abdominal imaging and over 40% of patients not receiving chest imaging in the 15 months after treatment. More important, there was no survival benefit in patients with more frequent imaging when stratified by pathologic stage [87].
In 2014, Stewart et al. evaluated the ability of guidelines to capture recurrences [88]. In a cohort who underwent surgery between years 1970 and 2008, 29.8% experienced a recurrence after a median follow-up of 9.0 years. The 2014 NCCN guidelines and AUA recommendations captured 68.2 and 66.9% of the recurrences, respectively. The authors found that up to 14–21 years of surveillance was necessary depending on risk and type of surgery to capture 95% of recurrences, though this would also result in higher costs. Lobo et al. used a simulation model to examine the percentage of recurrences captured as well as radiation exposure and the cost of surveillance by guideline (AUA, Canadian Urological Association, EAU, and NCCN) [89]. All guidelines were noted to capture 92% of high-risk recurrences within 5 years after treatment with large variability in radiation exposure (46.88 mSv in CAU guidelines compared to 231.61 mSv in NCCN/AUA guidelines for the high-risk group) and cost ($903 in CAU to $3904 NCCN/AUA) [89].
In an attempt to maximize diagnosis of recurrences and minimize the cost of unnecessary testing, the Stewart et al. group modeled the risk of non-RCC death (based on CCI, patient age) with risk of recurrence (based on tumor stage and location of probable relapse) [90•]. This attempts to offer a personalized approach to surveillance duration, holding surveillance when the risk of non-RCC death exceeds the risk of recurrence. The model is not yet externally or prospectively validated and does not specify frequency or modality for screening. However, it is an attractive consideration in order to optimize the efficacy of a surveillance regimen, without exacerbating the costs. Surveillance regimens need continued scrutiny to achieve appropriate and cost-effective screening based on patient and tumor characteristics.
Conclusion
Localized RCC is undergoing a stage migration with patients being diagnosed earlier. Most cohorts in the literature are from the 1980s–1990s. There are few contemporary cohorts, but those that are present do show a decreased recurrence rate, possibly secondary to earlier diagnosis. There are many clinical prognostic factors that predict recurrence including TNM staging, presence of LVI, sarcomatoid differentiation, collecting system invasion, necrosis, and presence of symptoms, CRP. Numerous other biomarkers and composites of biomarkers have been examined though few are externally validated and few have been shown to add to the prognostic efficacy of the existing nomograms. Promising biomarkers include IMP-3, CRP, c-Met, and many of the composite assays.
The frontier of treatment for recurrent and metastatic RCC is rapidly expanding. Potential upcoming treatment changes in patients with localized RCC include possible neoadjuvant versus adjuvant-targeted therapy for patients with high-risk advanced disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30.
Karim-Kos HE et al. Recent trends of cancer in Europe: a combined approach of incidence, survival and mortality for 17 cancer sites since the 1990s. Eur J Cancer. 2008;44(10):1345–89.
Ljungberg B et al. The epidemiology of renal cell carcinoma. Eur Urol. 2011;60(4):615–21.
Gandaglia G et al. Contemporary incidence and mortality rates of kidney cancer in the United States. Can Urol Assoc J. 2014;8(7-8):247–52.
Motzer RJ et al. Kidney Cancer, Version 3.2015. J Natl Compr Canc Netw. 2015;13(2):151-–159.
Sun M et al. Management of localized kidney cancer: calculating cancer-specific mortality and competing risks of death for surgery and nonsurgical management. Eur Urol. 2014;65(1):235–41.
Larcher A et al. Population-based assessment of cancer-specific mortality after local tumour ablation or observation for kidney cancer: a competing risks analysis. BJU Int. 2016;118(4):541–6.
Janzen NK et al. Surveillance after radical or partial nephrectomy for localized renal cell carcinoma and management of recurrent disease. Urol Clin N Am. 2003;30(4):843–52.
• Lane BR, Campbell SC, Gill IS. 10-year oncologic outcomes after laparoscopic and open partial nephrectomy. J Uro. 2013;190(1):44–9. One of the most contemporary large studies that analyzes recurrence outcomes.
Crispen PL et al. Outcomes following partial nephrectomy by tumor size. J Urol. 2008;180(5):1912–7.
Klatte T et al. Tumor size does not predict risk of metastatic disease or prognosis of small renal cell carcinomas. J Urol. 2008;179(5):1719–26.
Adamy A et al. Clinical characteristics and outcomes of patients with recurrence 5 years after nephrectomy for localized renal cell carcinoma. J Urol. 2011;185(2):433–8.
Eggener SE et al. Renal cell carcinoma recurrence after nephrectomy for localized disease: predicting survival from time of recurrence. J Clin Oncol. 2006;24(19):3101–6.
Cindolo L et al. Comparison of predictive accuracy of four prognostic models for nonmetastatic renal cell carcinoma after nephrectomy: a multicenter European study. Cancer. 2005;104(7):1362–71.
Sorbellini M et al. A postoperative prognostic nomogram predicting recurrence for patients with conventional clear cell renal cell carcinoma. J Urol. 2005;173(1):48–51.
Lam JS et al. Postoperative surveillance protocol for patients with localized and locally advanced renal cell carcinoma based on a validated prognostic nomogram and risk group stratification system. J Urol. 2005;174(2):466–72. discussion 472; quiz 801.
Hafez K, Novick A, Campbell SC. Patterns of Tumor Recurrence and Guidelines for Followup after Nephron Sparing Surgery for Sporadic Renal Cell Carcinoma. J Urol. 1997;157:2067–70.
Levy D et al. Stage specific guidelines for surveillance after radical nephrectomy for local renal cell carcinoma. J Urol. 1998;159:1163–7.
Forbes CM, et al. Disease progression and kidney function after partial vs. radical nephrectomy for T1 renal cancer Urol Oncol, 2016.
Huang W et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol. 2006;7:735–40.
Fergany A, Hafez K, Novick A. Long-term results of nephron sparing surgery for localized renal cell carcinoma: 10-year followup. J Urol. 2000;163:442–5.
Becker F et al. Excellent long-term cancer control with elective nephron-sparing surgery for selected renal cell carcinomas measuring more than 4 cm. Eur Urol. 2006;49(6):1058–63. discussion 1063-4.
Leibovich BC et al. Nephron sparing surgery for appropriately selected renal cell carcinoma between 4 and 7 cm results in outcome similar to radical nephrectomy. J Urol. 2004;171(3):1066–70.
Banegas MP et al. Toward greater adoption of minimally invasive and nephron-sparing surgical techniques for renal cell cancer in the United States. Urol Oncol. 2016;34(10):433 e9–433 e17.
Berger A et al. Laparoscopic radical nephrectomy for renal cell carcinoma: oncological outcomes at 10 years or more. J Urol. 2009;182(5):2172–6.
MacLennan S et al. Systematic review of oncological outcomes following surgical management of localised renal cancer. Eur Urol. 2012;61(5):972–93.
Andrade HS et al. Five-year oncologic outcomes after transperitoneal robotic partial nephrectomy for renal cell carcinoma. Eur Urol. 2016;69(6):1149–54.
Campbell SC et al. Guideline for management of the clinical T1 renal mass. J Urol. 2009;182(4):1271–9.
Pierorazio PM, et al. Management of Renal Masses and Localized Renal Cancer: Systematic Review and Meta-Analysis. J Urol. 2016.
Mason RJ et al. Growth kinetics of renal masses: analysis of a prospective cohort of patients undergoing active surveillance. Eur Urol. 2011;59(5):863–7.
Smaldone MC et al. Small renal masses progressing to metastases under active surveillance: a systematic review and pooled analysis. Cancer. 2012;118(4):997–1006.
Cindolo L et al. A preoperative clinical prognostic model for non-metastatic renal cell carcinoma. BJU Int. 2003;92:901–5.
Yaycioglu O et al. Prognostic assessment of nonmetastatic renal cell carcinoma: a clinically based model. Urology. 2001;58(2):141–5.
Kattan M et al. A postoperative predictive nomogram for renal cell carcinoma. J Urol. 2001;166:63–7.
Lindblad P. Epidemiology of renal cell carcinoma. Scand J Surg. 2004;93(2):88–96.
Zisman A et al. Mathematical model to predict individual survival for patients with renal cell carcinoma. J Clin Oncol. 2002;20(5):1368–74.
Dall’Oglio MF et al. Microvascular tumour invasion in renal cell carcinoma: the most important prognostic factor. BJU Int. 2007;100(3):552–5.
Huang H et al. Microvascular invasion as a prognostic indicator in renal cell carcinoma: a systematic review and meta-analysis. Int J Clin Exp Med. 2015;8(7):10779–92.
Peralta-Venturina MD et al. Sarcomatoid differentiation in renal cell carcinoma: a study of 101 cases. Am J Surg Pathol. 2001;25(3):275–84.
Terrone C et al. Prognostic value of the involvement of the urinary collecting system in renal cell carcinoma. Eur Urol. 2004;46(4):472–6.
Palapattu GS et al. Collecting system invasion in renal cell carcinoma: impact on prognosis and future staging strategies. J Urol. 2003;170(3):768–72. discussion 772.
Uzzo R et al. Renal cell carcinoma invading the urinary collecting system: implications for staging. J Urol. 2002;167:2392–6.
Chen L et al. Prognostic role of urinary collecting system invasion in renal cell carcinoma: a systematic review and meta-analysis. Sci Rep. 2016;6:21325.
Hoffmann NE et al. External validation of IMP3 expression as an independent prognostic marker for metastatic progression and death for patients with clear cell renal cell carcinoma. Cancer. 2008;112(7):1471–9.
Hakimi AA et al. Validation and genomic interrogation of the MET variant rs11762213 as a predictor of adverse outcomes in clear cell renal cell carcinoma. Cancer. 2016;122(3):402–10.
Rini B et al. A 16-gene assay to predict recurrence after surgery in localised renal cell carcinoma: development and validation studies. Lancet Oncol. 2015;16:676–85.
Karakiewicz PI et al. C-reactive protein is an informative predictor of renal cell carcinoma-specific mortality: a European study of 313 patients. Cancer. 2007;110(6):1241–7.
Parker AS et al. Development and evaluation of BioScore: a biomarker panel to enhance prognostic algorithms for clear cell renal cell carcinoma. Cancer. 2009;115(10):2092–103.
Klatte T et al. Molecular signatures of localized clear cell renal cell carcinoma to predict disease-free survival after nephrectomy. Cancer Epidemiol Biomarkers Prev. 2009;18(3):894–900.
Joseph RW et al. Loss of BAP1 protein expression is an independent marker of poor prognosis in patients with low-risk clear cell renal cell carcinoma. Cancer. 2014;120(7):1059–67.
Joseph RW et al. Clear cell renal cell carcinoma subtypes identified by BAP1 and PBRM1 Expression. J Urol. 2016;195(1):180–7.
Fan Y et al. Prognostic significance of hypoxia-inducible factor expression in renal cell carcinoma: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2015;94(38), e1646.
Klatte T et al. The chemokine receptor CXCR3 is an independent prognostic factor in patients with localized clear cell renal cell carcinoma. J Urol. 2008;179(1):61–6.
Zigeuner R et al. Value of p53 as a prognostic marker in histologic subtypes of renal cell carcinoma: a systematic analysis of primary and metastatic tumor tissue. Urology. 2004;63(4):651–5.
Hofmockel G et al. Expression of p53 and bcl-2 in primary locally confined renal cell carcinomas: no evidence for prognostic significance. Anticancer Res. 1996;16(6B):3807–11.
Ljungberg B et al. p53 expression in correlation to clinical outcomes in patients with renal cell carcinoma. Scand J Urol Nephrol. 2001;35(1):15–20
Lam JS et al. Clinicopathologic and molecular correlations of necrosis in the primary tumor of patients with renal cell carcinoma. Cancer. 2005;103(12):2517–25.
Frank I et al. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score. J Urol. 2002;168(6):2395–400.
Leibovich BC et al. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer. 2003;97(7):1663–71.
Gogus C et al. Significance of thrombocytosis for determining prognosis in patients with localized renal cell carcinoma. Urology. 2004;63(3):447–50.
Gu L et al. The association of platelet count with clinicopathological significance and prognosis in renal cell carcinoma: a systematic review and meta-analysis. PLoS One. 2015;10(5), e0125538.
Hu Q et al. The prognostic value of C-reactive protein in renal cell carcinoma: a systematic review and meta-analysis. Urol Oncol. 2014;32(1):50. e1-8.
Kang HW et al. Surgical margin does not influence recurrence rate in pT1 clear cell renal cell carcinoma after partial nephrectomy: a multicenter study. J Surg Oncol. 2016;114(1):70–4.
Shah PH et al. Positive surgical margins increase risk of recurrence after partial nephrectomy for high risk renal tumors. J Urol. 2016;196(2):327–34.
Zisman A et al. Improved prognostication of renal cell carcinoma using an integrated staging system. J Clin Oncol. 2001;19(6):1649–57.
Karakiewicz PI et al. Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol. 2007;25(11):1316–22.
Parker, W.P., et al., Application of the Stage, Size, Grade, and Necrosis (SSIGN) Score for Clear Cell Renal Cell Carcinoma in Contemporary Patients. Eur Urol, 2016.
Ngo TC, Wood CG, Karam JA. Biomarkers of renal cell carcinoma. Urol Oncol. 2014;32(3):243–51.
Nogueira M, Kim HL. Molecular markers for predicting prognosis of renal cell carcinoma. Urol Oncol. 2008;26(2):113–24.
Crispen PL et al. Predicting disease progression after nephrectomy for localized renal cell carcinoma: the utility of prognostic models and molecular biomarkers. Cancer. 2008;113(3):450–60.
Lam JS et al. Prognostic factors and selection for clinical studies of patients with kidney cancer. Crit Rev Oncol Hematol. 2008;65(3):235–62.
Pei X et al. Enhanced IMP3 expression activates NF-small ka, CyrillicB pathway and promotes renal cell carcinoma progression. PLoS One. 2015;10(4), e0124338.
Gibney GT et al. c-Met is a prognostic marker and potential therapeutic target in clear cell renal cell carcinoma. Ann Oncol. 2013;24(2):343–9.
Slaby O et al. Identification of MicroRNAs associated with early relapse after nephrectomy in renal cell carcinoma patients. Genes Chromosomes Cancer. 2012;51(7):707–16.
Gu L et al. MicroRNAs as prognostic molecular signatures in renal cell carcinoma: a systematic review and meta-analysis. Oncotarget. 2015;6(32):32545–60.
Thiry A et al. Targeting tumor-associated carbonic anhydrase IX in cancer therapy. Trends Pharmacol Sci. 2006;27(11):566–73.
Zhao Z et al. Prognostic value of carbonic anhydrase IX immunohistochemical expression in renal cell carcinoma: a meta-analysis of the literature. PLoS One. 2014;9(11), e114096.
Kavolius JP et al. Resection of metastatic renal cell carcinoma. J Clin Oncol. 1998;16(6):2261–6.
Alt AL et al. Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer. 2011;117(13):2873–82.
Dabestani S et al. Local treatments for metastases of renal cell carcinoma: a systematic review. Lancet Oncol. 2014;15:e549–61.
Zhang Y et al. Sorafenib neoadjuvant therapy in the treatment of high risk renal cell carcinoma. PLoS One. 2015;10(2), e0115896.
Jonasch E et al. Phase II presurgical feasibility study of bevacizumab in untreated patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(25):4076–81.
Harshman LC et al. Surgical outcomes and complications associated with presurgical tyrosine kinase inhibition for advanced renal cell carcinoma (RCC). Urol Oncol. 2013;31(3):379–85.
•• Ravaud, A., et al., Adjuvant Sunitinib in High-Risk Renal-Cell Carcinoma after Nephrectomy. N Engl J Med, 2016. This article highlights a potential promising new treatment strategy for patients with patients at high risk of renal cell recurrence.
Donat SM et al. Follow-up for clinically localized renal neoplasms: AUA guideline. J Urol. 2013;190(2):407–16.
Ljungberg B et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol. 2015;67(5):913–24.
Sohn, W., et al., An Empiric Evaluation of the Effect of Variation in Intensity of Follow-Up for Surgically Treated Renal Neoplasms on Cancer Specific Survival. J Urol, 2016.
Stewart SB et al. Evaluation of the National Comprehensive Cancer Network and American Urological Association renal cell carcinoma surveillance guidelines. J Clin Oncol. 2014;32(36):4059–65.
Lobo JM et al. Comparison of Renal Cell Carcinoma Surveillance Guidelines: competing trade-offs. J Urol. 2016;195(6):1664–70.
• Stewart-Merrill SB et al. Oncologic surveillance after surgical resection for renal cell carcinoma: a novel risk-based approach. J Clin Oncol. 2015;33(35):p. 4151–7. This article presents an individualized risk-based approach to surveillance that may improve both detection of recurrence and increase cost-effectiveness of screening.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jacqueline M. Speed, Quoc-Dien Trinh, Toni K. Choueiri, and Maxine Sun each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Kidney Diseases
Rights and permissions
About this article
Cite this article
Speed, J.M., Trinh, QD., Choueiri, T.K. et al. Recurrence in Localized Renal Cell Carcinoma: a Systematic Review of Contemporary Data. Curr Urol Rep 18, 15 (2017). https://doi.org/10.1007/s11934-017-0661-3
Published:
DOI: https://doi.org/10.1007/s11934-017-0661-3