Abstract
Purpose
To provide an overview of recent studies on pathogenesis, diagnosis, and management of juvenile spondyloarthritis (JSpA).
Recent Findings
Recent studies show differences in gut microbiome in patients with JSpA in comparison to healthy controls. There is increased recognition of the impact of the innate immune system on disease pathology. Normative reference on MRI of sacroiliac (SI) joints in children is now available. However, there is significant variability in interpretation of MRI of SI joints in children and a need for standardization. NSAIDs, physical therapy, and Tumor Necrosis Factor Inhibitors (TNFi) remain the mainstay of management for patients with JIA who have polyarthritis, sacroiliitis, and/or enthesitis as per recent ACR guidelines. Newer therapeutic options beyond TNFi are needed to manage patients who fail TNFi.
Summary
This review highlights some of the recent advances in our knowledge of JSpA pathophysiology, diagnosis, and treatment. It also identifies areas in need of further research and standardization to improve our understanding and outcomes in JSpA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
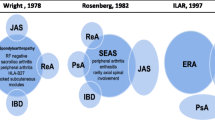
Juvenile Spondyloarthritis (JSpA) is the pediatric counterpart of adult spondyloarthritis (SpA). However, there is a huge gulf between the classification system of adult arthritis and juvenile arthritis [1]. The differences in nomenclature lead to confusion and hinders both research and clinical care. There is new push to consider juvenile arthritis on a continuum with adult arthritis [1]. This issue is most relevant in JSpA where it is well known that many children have continued disease activity into adulthood [2]. Patients who develop chronic arthritis before their 16th birthday are considered to have juvenile idiopathic arthritis (JIA). The current classification system is the one established by the International League of Associations for Rheumatology (ILAR) in 2004 where patients with JIA are separated into 7 subcategories [3]. Of these, the subcategories of enthesitis related arthritis, psoriatic arthritis, and undifferentiated arthritis are considered to fall under the umbrella of JSpA [3]. Further, patients who satisfy modified New York criteria for ankylosing spondylitis (AS) and undifferentiated arthritis by European Spondyloarthropathy Study Group (ESSG) or Amor criteria before age 16 are also considered to have JSpA [4,5,6]. While patients with JSpA have several similarities with adult spondyloarthritis in terms of presence of enthesitis and axial involvement, important distinctions exist. For example, children with JSpA can have sacroiliitis in the absence of inflammatory back pain and present with peripheral joint involvement [7, 8]. Very young children with psoriatic arthritis behave more like oligoarticular JIA than spondyloarthritis [9, 10]. There is wide variability in prevalence of JSpA ranging from 10–30% of juvenile idiopathic arthritis based on geographic area [11,12,13,14]. Patients with JSpA, particularly those with a prominent enthesitis component, tend to have worse quality of life, function, and pain [15, 16]. While tumor necrosis factor inhibitors (TNFi) have been established as standard of therapy, TNFi failure remains a huge challenge [17]. With limited availability of US Food and Drug Administration (FDA) approved medications, these patients are often left with limited treatment options [18].
We focus this review on advances made in understanding the pathogenesis of spondyloarthritis and how it applies to children in addition to advances in imaging modalities and treatment. For this systematic review, PubMed, Web of Science, and Scopus were searched for articles published in the English language between years 2015 and 2020 using the MeSH terms of “arthritis, ” “juvenile,” and “spondyloarthritis” (Fig. 1). Each abstract was screened by all authors, following which full articles were independently reviewed.
Advances in Pathogenesis
Association With Gut Microbiome
Subclinical gut inflammation is seen in patients with adult SpA and JSpA [19, 20]. One of the most significant and well-studied aspects of SpA pathogenesis is its association with gut inflammation and the gut microbiome. Studies evaluating the fecal microbiome of adult SpA patients have shown differences in certain gut microbiota, including Dialister, Ruminococcus gnavus, and Bacteroides fragilis associated with inflammatory bowel disease (IBD) and SpA [21, 22]. Analyses of gut microbiota have also identified specific bacterial strains that can produce increased levels of small chain fatty acids (SCFA), which possess antiinflammatory properties [23]. Comparison of gut microbiota in SpA and JSpA patients found that both had decreased levels of SCFA-producing Faecalibacterium prausnitzii strains compared to healthy controls. However, adult and pediatric patients did have different levels of other microbiota, such as B. fragilis, suggesting some microbiota may directly impact the inflammatory response while others affect the ontogeny of the immune system [24]. While these studies have identified different gut microbiota implicated in the development of SpA/JSpA, no one microbiota profile has been identified as pathognomonic for developing inflammatory arthritis. Recent studies looking at the microbiota of three different HLA-B27 arthritis rat models showed significant variation in the microbiota associated with developing inflammation in the different rat models. The variation in inflammation-associated microbiota in the three different rat models suggests that microbiota associated with inflammation may be dependent on the genetic background and/or environment in which it exists [25]. Other studies have looked at the direct immune response to gut microbiota. Pediatric enthesitis-related arthritis (ERA) patients were shown to produce increased levels of IgA antibodies to commensal oral microbiota, P. oralis, implicating these bacteria as possible antigen triggers for immune system activation [26]. Fecal microbiota transplantation has shown mixed results in clinical studies for IBD [27]. However, before such treatments become a feasible option for JSpA, further studies are needed to demonstrate safety in addition to identifying the optimal donors/microbiota and recipients.
Genetic Associations With JSpA
HLA-B27 is the most well-known and widely studied genetic associations with SpA but is only present in 30 to 50% of JSpA patients, suggesting there are multiple genes contributing to the pathogenesis of JSpA [26]. Several other genes and signaling pathways such as endoplasmic reticulum aminopeptidase-1 (ERAP1) and, IL-23 receptor gene (IL23R), have been identified as important in the pathogenesis of SpA and JSpA [28,29,30,31]. A 2018 study compared differentially expressed genes and signaling pathways in whole blood from 15 JSpA patients to age-matched healthy controls. Significant differences in gene expression were found in the genes regulating the mitogen-activated protein kinase (MAPK) pathway and C-X-C motif chemokine 5 (CXCL5) [32]. In relating these results to JSpA pathogenesis, MAPK signaling and CXCL5 are important in innate immune activation, suggesting constitutive activation of the innate immune system could be important in JSpA pathology [32]. These genetic associations with JSpA are supported by research describing innate cell activity in SpA/JSpA as described below.
Innate Immunity and JSpA
Recent studies into the pathogenesis of SpA/JSpA support the significant impact of the innate immune system on disease pathology. Calprotectin is a S100 protein that functions as a damage-associated molecular pattern (DAMP) ligand for toll-like receptor (TLR) 4-mediated innate immune activation. In adult SpA patients with uveitis, calprotectin levels were significantly elevated compared to those with other autoimmune diseases, such as JIA, regardless of uveitis or arthritis activity. A similar elevation in calprotectin was seen in non-SpA HLA-B27+ uveitis patients, suggesting constitutive immune activation associated with HLA-B27 is important to disease pathology in HLA-B27-associated conditions, such as JSpA [33]. While calprotectin did not correlate with disease activity in SpA-associated uveitis, it was the most sensitive predictor of disease relapse in PsA patients when compared to other acute phase reactants, supporting the important role of innate immune activation in PsA [34].
Monocytes are subdivided into M1, classically activated/inflammatory, and M2, alternatively activated/antiinflammatory, subsets. M2 monocytes express a scavenger receptor CD163 as a soluble, surface, and/or intracellular protein [35]. Studies of innate immune activation in adult spondyloarthritis have shown a positive correlation between numbers of synovial CD163+ monocytes with swollen joint count and acute phase reactants [36]. Activation of CD163+ monocytes has also been associated with increased expression of interleukin (IL)-6, TNF-α, and IL-1ß in adult SpA. Studies on pediatric ERA showed soluble CD163+ expression in the sera and synovial fluid to be significantly increased compared to healthy controls, but this expression did not correlate with swollen joint count or acute phase reactants [37]. While it is unclear what role calprotectin and CD163 play in JSpA, the increased expression of these molecules supports the significant contribution of the innate immune system to the pathogenesis of JSpA.
Increased expression of IL-17/IL-23 has long been associated with SpA and JSpA [38]. HLA-B27 misfolding result in endoplasmic reticulum stress and activation of unfolded protein response that promote TLR-mediated IFN-β and IL-23 induction [39, 40]. Nucleotide binding oligomerization domain (NOD) mouse models treated with adenoviral vectors containing IL-23 develop psoriatic skin lesions, arthritis, and increased IL-17 and IL-23 expression. These symptoms improved with treatment with IL-17 inhibitory antibodies [41]. While IL-17/IL-23 cytokine expression is typically associated with CD4+ Th17 cells, mouse models and human studies have identified various other cell subsets, such as γδ T cells and innate-like cells (ILCs), as important contributors to IL-17 and IL-23 production [38]. Interestingly, γδ T cells and ILCs both express the Th17-associated transcription factor, retinoic acid receptor-related orphan receptor-gamma-t (RORγt). Inhibition of RORγt suppressed the IL-17 production from these cell subsets, highlighting these cells as potential targets for immune suppression in patients with SpA/JSpA [42, 43]. These studies suggest that the imbalance in the IL17/23 axis seen in JSpA may be due to multiple innate or innate-like immune cells. Figure 2 pictorially represents the pathogenesis of JSpA.
Advances in Imaging
For updates until year 2016, we direct the readers to a comprehensive review of imaging in JSpA in the journal by Weiss et al [44]. Recent developments between 2016 and 2020 are discussed here. Magnetic resonance imaging (MRI) is an important diagnostic tool in evaluating for axial disease in JSpA [45]. There is limited utility for plain radiographs of sacroiliac joints (SIJ) in detecting early changes of sacroiliitis, especially in children. A retrospective study of 60 subjects who underwent radiographs and MRI of SIJ within 6 months of each other demonstrated poor inter-rater reliability and high false positive and false negative rates for radiographs compared to MRI in detecting active sacroiliitis [46]. Interpretation of sacroiliitis on MRI in children is not without its challenges. Developmental changes of metaphyseal equivalent signal in the sacral apophyses can be confused for bone marrow edema around the SIJ. Knowledge of normal variability of MRI of SIJ in healthy children is necessary to distinguish between normative findings and pathology. The study by Chauvin et al describing MRI findings in 70 healthy children in 3 age groups—prepubertal (9–10 years), peripubertal (11–13 years), and approaching skeletal maturity (14–17 years) serve as a good reference for normative data on SIJ by MRI [47]. There is wide variability in interpretation of MRI of SIJ by radiologists as demonstrated in the study by Weiss et al where interpretation of SIJ MRI from 120 subjects were compared between local radiologists and central readers. Considering central reader interpretation as the gold standard, the study noted high sensitivity (93.5%) for detection of active inflammation by local radiologists but poor positive predictive value (PPV) (51.8%) indicating interpretation of developmental metaphyseal changes as active sacroiliitis. There was low sensitivity (45.7%) and positive predictive value (61.5%) for detecting chronic changes [48]. This underscores the need for standardization and training for interpretation of SIJ MRI studies. Efforts are underway to address these gaps. The outcome measures in rheumatology workgroup on juvenile arthritis MRI SIJ (OMERACT JAMRIS-SIJ) consisting of an international group of radiologists and rheumatologists have developed definitions for domains of inflammation (bone marrow edema, joint space inflammation, capsulitis, and enthesitis) and structural joint changes (sclerosis, erosion, fatty lesion and ankylosis) by consensus-driven methodology consisting of iterative surveys and focus groups [49]. This provides a framework for their ongoing work on development of a scoring system for MRI of SIJ. The Spondyloarthritis Research Consortium of Canada (SPARCC) scoring system is a validated tool for use in adults with axial spondyloarthritis [50, 51]. The scoring system was evaluated in 90 whole-body (WB) MRI examinations with dedicated views of the SIJ in 46 subjects who satisfied ESSG criteria for SpA and were younger than 16 years of age and/or ERA by ILAR criteria. It showed excellent intra- and inter-rater reliability and higher responsiveness to treatment related changes than most clinical outcome measures. Cross-sectional and longitudinal correlation between clinical indicators and MRI scoring was poor [52]. Use of real-time iterative calibration (RETIC) modules can improve the overall inter-rater reliability among readers for both sacroiliac joint inflammation (SIS) and structural scores (SSS) for SPARCC as demonstrated by Weiss et al. Further, all components except sclerosis can reliably measure change over time in children. The authors conclude by identifying need for a pediatric-based module to account for age-related difference in the appearance of SIJ [53]. WB MRI is emerging as a potential tool for evaluation of disease activity in JSpA. An OMERACT special interest group outline the challenges and opportunities and address consideration for development of a pediatric WB MRI scoring system for use in JIA [54].
Update on Treatment of Juvenile Spondyloarthritis
Principles of Management
Clinical trials in treatment efficacy require many patients followed over an extended period. Given the relatively low prevalence of JSpA, such clinical trials are logistically difficult to execute. Therefore, clinical trials in adult SpA treatment are often used by pediatric rheumatology providers for treatment guidance [55]. However, this often leaves children with JSpA with limited treatment options due to reluctance by insurance companies to approve off-label indications. Further, there are very few clinical trials on JSpA in particular and many of the clinical trials include subjects having several subcategories of JIA of which, ERA or juvenile psoriatic arthritis (jPsA) may be a very small fraction. Given similarities in pathogenesis and clinical manifestations to adult spondyloarthritis, there is greater impetus to study medications approved in adult SpA in children with ERA with an ultimate goal for obtaining FDA approval for pediatric indications [56].
Pharmacologic Management
In 2019 the American College of Rheumatology and Arthritis Foundation published guidelines for the initial and subsequent treatment of juvenile idiopathic arthritis (JIA) with nonsystemic polyarthritis, sacroiliitis, and/or enthesitis that were developed using systematic review, Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology, and group consensus [57]. As characteristic features of JSpA include enthesitis and axial involvement (sacroiliitis), those recommendations are summarized in Table 1.
While there is low evidence for the strong recommendation to treat with NSAIDs, it is consistent with the most recent recommendations for active AS and nonradiographic axial spondyloarthritis (nr-axSpA) [58].
For patients with predominant enthesitis, TNFi or bridging therapy with short course of steroids are conditionally recommended over conventional disease-modifying antirheumatic drugs (csDMARDS) such as methotrexate or sulfasalazine although the level of evidence for this recommendation is very low to low. In our practice, in children with JSpA presenting with predominantly peripheral arthritis, a trial of csDMARDS is considered a reasonable option.
TNFi have been established as the first line biologic in AS and nr-axSpA by multiple randomized controlled trials and by the recent ACR guidelines [58]. Similarly, in the current ACR guidelines for children, TNFi are recommended over other csDMARDS in the setting of active sacroiliitis or enthesitis despite NSAIDs.
In a phase III study of 46 children with ERA, there was significant improvement in active joint count and secondary measures of disease activity in those treated with adalimumab compared to placebo, and these improvements were sustained through 52 weeks [59].
CLIPPER study found etanercept to be effective through 96 weeks of therapy in children with extended oligoarticular JIA (n=60), ERA (n=38), and juvenile psoriatic arthritis (jPsA) (n=29) with increasing ACR 30/50/70/90/100 responses over time [60]. There was stable efficacy through 6 years of etanercept in the patients who continued into CLIPPER2, which included lower percentages of ERA and jPsA compared to extended oligoarticular JIA [61]. A UK study also looked at response to etanercept in the first year, finding improvements in Juvenile Arthritis Disease Activity Score (JADAS)-71 in all ILAR subtypes except persistent oligoarticular JIA [62]. In this cohort, odds of achieving ACR Pedi 90 after 1 year of etanercept included age younger than 9, shorter disease duration, lower childhood health assessment questionnaire (CHAQ), and not requiring concurrent steroids.
Golimumab is a fully human TNFi that has been used in adults with SpA. A study of subcutaneous golimumab in children with active polyarticular juvenile idiopathic arthritis (polyJIA), which included some subjects with jPsA, failed to reach its endpoint with similar flare rates and remission rates at week 48 compared to placebo, though there was clinical improvement in those treated with golimumab [63]. However, the GO-VIVA Study (NCT02277444) assessed pharmacokinetics, safety and efficacy of IV golimumab in children with polyJIA and jPsA. In this case there were improvements in JIA ACR 30/50/70/90 at 28 weeks on IV golimumab and methotrexate that were sustained through 52 weeks [64]. Based on this data, IV golimumab was recently approved by FDA for children ages 2 and older with polyJIA and jPsA.
Children with ERA who were treated with TNFi in the first year after diagnosis had statistically significant improvements in active joint count, patient reported pain, and disease activity compared to those treated with csDMARDS in a retrospective comparative effectiveness study [65]. Favalli et al found lower rates of discontinuation of first TNFi due to inefficacy in children with nonsystemic-onset JIA compared to adults (HR 0.719 [95% CI 0.548-0.943], p=0.017); both ERA and jPsA patients were included in this study [66]. Immunogenicity of biologic agents remains a concern, particularly in regard to infliximab and adalimumab. Skrabl-Baumgartner et al determined patients with JIA and antidrug antibodies had lower rates of clinical response to adalimumab than those without and were less likely to have received concomitant methotrexate [67].
Glucocorticoids as a short course bridging therapy are conditionally recommended in the recent ACR guidelines. Intraarticular injection of corticosteroids into the SI joints is conditionally recommended as an adjunct therapy. Chamlati et al assessed the feasibility and efficacy of image guided intraarticular corticosteroid injections of the sacroiliac joints in 50 children, predominantly JIA, with sacroiliitis based on clinical symptoms and MRI findings [68]. Majority of patients (66%) had clinical improvement 3 months after injection; however, within 2 years 47% required escalation in therapy, most commonly (13/15) to biologic therapy. Corticosteroid injection was associated with a decrease in SPARCC score in 93% of patients but this improvement did not correlate with long-term medical management as many remained on the same treatment or had escalation of therapy.
Pathogenesis of Juvenile Spondyloarthritis. Intestinal dysbiosis and environmental stress leads to the release of pathogen associated molecular pattern molecules (PAMPs), which in turn activate innate immune cells, such as macrophages (m0), γδT cells, neutrophils, and innate-lymphoid cells (ILCs). Activation of these cells is signaled by the expression of proteins such as calprotectin and soluble CD163 (sCD163). Innate immune activation under these unique environmental and genetic conditions is thought to preferentially activate the Th1 and Th17 T-cell subsets, leading to the development of arthritis, enthesitis, psoriatic skin lesions, and uveitis associated with JSpA. While other molecular and cellular mechanisms likely contribute to the development of JSpA, these are several key factors elucidated by research over the past several years. Abbreviations: HLA-B27: Human leukocyte antigen B27; NLRP3: Nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain containing 3; ERAP 1/2: Endoplasmic reticulum aminopeptidase ½; CXCR4: C-X-C chemokine receptor type 4; CXCL5: C-X-C motif chemokine 5; MAPK: Mitogen-activated protein kinase; BNIP3L: B-cell lymphoma 2 interacting protein 3 like; DUSP5: Dual specificity protein phosphatase 5; TP53: Tumor protein p53
Emerging Pharmacologic Treatments
As previously mentioned, IL-17 expression and imbalance in the IL-17/IL-23 axis have been implicated in the pathogenesis of SpA. Therefore, IL-17 inhibition has been evaluated as a possible therapeutic option for SpA [69,70,71,72]. While adult SpA and JSpA are unique medical conditions, the similarities in TNF, and IL-17/IL-23 involvement in disease pathogenesis would suggest that both conditions would respond to biologic DMARD to these cytokines in a similar manner [37, 56]. However, IL-17 has been known to exacerbate Crohn’s disease in adults and should be avoided in patients with IBD associated arthritis [73].
Ustekinumab is a human monoclonal antibody that targets IL-12 and IL-23. It is approved for adults with PsA, plaque psoriasis in patients aged 6 years or greater, and adults with moderately to severely active Crohn disease or ulcerative colitis [74]. However, trials on IL-23 inhibition have failed to meet key endpoints in axial SpA (NCT02438787, NCT02407223, [75]). There are currently no clinical trials registered for ustekinumab in juvenile idiopathic arthritis, including juvenile spondyloarthritis, though improvements in enthesitis and dactylitis in patients with adult PsA suggests this treatment may be utilized in juvenile spondyloarthritis. Case studies of ustekinumab in 5 children with enthesitis related arthritis noted improvement in active enthesitis and arthritis [76].
Tofacitinib is a Janus Kinase (JAK) inhibitor that is FDA approved for use in polyJIA. A Phase I multicenter study assessed pharmacokinetics, efficacy, and short-term safety of tofacitinib in children with polyJIA [77]. A Phase III (NCT02592434) study of tofacitinib in JIA (polyJIA, jPsA, and ERA) found lower flare rate with tofacitinib compared to placebo and longer time to disease flare [78]. An ongoing study (NCT01500551) is investigating the safety, tolerability, and efficacy in JIA, including subjects aged 2–18 years with polyJIA (n=172), jPsA (n=19), and ERA (n=21). Interval analysis revealed that while no patients achieved JIA ACR clinical remission, there were sustained improvements in disease activity and physical function through 18 months [79].
Nonpharmacologic Management
Biomechanical stress has been known to play a role in causing enthesitis in animal models [80]. In children, there may be additional impact for a developing skeleton and entheseal complex. Physical activity, such as a structured exercise program, is routinely recommended in children with JIA. Benefits of such exercise program include preserving/improving joint range of motion, improving strength, promoting cardiovascular fitness, and decreasing pain [81]. While there are no specific studies of JSpA and structured exercise programs, they often make up the population in JIA studies. The LEAP study demonstrated improvement in fatigue with a 6-month home exercise program, though adherence to the program was low [82]. A pilot randomized control program is investigating yoga and aerobic dance for pain management in adolescent females with any ILAR subtype of JIA [83]. Despite very low evidence, physical therapy is recommended in children and adolescents with enthesitis or sacroiliitis who have or are risk for functional limitations [57].
Outcome Measures and Monitoring of Disease Activity
Core domain sets for studies in JIA are a framework to assess efficacy of medications in randomized controlled trials and longitudinal observational studies. The JIA core domain set was updated by an international group of clinicians, researchers, and patient/parent partners in 2018 as the prior set from 1997 was developed without input from patient/parent partners. They identified mandatory domains of pain, joint inflammatory signs, activity limitation/physical function, patient’s perception of disease activity (overall well-being), and adverse events to be included in all studies [84]. The Juvenile Spondyloarthritis Disease Activity Index (JSpADA) remains the only disease activity score specifically for JSpA and includes measures specific for this condition such as active enthesitis count, clinical sacroiliitis, uveitis, and back mobility [85]. This measure was recently prospectively validated in a cohort of Indian children with ERA and found the measure performed well even after eliminating back mobility from the set of items [86].
Conclusions
Deeper understanding of pathophysiology of JSpA and immune pathways are paving the way for newer therapeutic options beyond TNFi. There is urgent need to translate these into clinical trials in patients with JSpA for medications currently approved for adult SpA beyond TNFi biologics. Improvement in understanding and interpretation of MRI of SIJ through standardization exercises have a potential to improve diagnostic accuracy.
References
Nigrovic PA, Colbert RA, Holers VM, Ozen S, Ruperto N, Thompson SD, et al. Biological classification of childhood arthritis: roadmap to a molecular nomenclature. Nature reviews Rheumatology. 2021.
Weiß A, Minden K, Listing J, Foeldvari I, Sieper J, Rudwaleit M. Course of patients with juvenile spondyloarthritis during 4 years of observation, juvenile part of GESPIC. RMD open. 2017;3(1):e000366.
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. The Journal of rheumatology. 2004;31(2):390–2.
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis and rheumatism. 1984;27(4):361–8.
Dougados M, van der Linden S, Juhlin R, Huitfeldt B, Amor B, Calin A, et al. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis and rheumatism. 1991;34(10):1218–27.
Amor B, Dougados M, Mijiyawa M. Criteria of the classification of spondylarthropathies. Rev Rhum Mal Osteoartic. 1990;57(2):85–9.
Stoll ML, Bhore R, Dempsey-Robertson M, Punaro M. Spondyloarthritis in a pediatric population: risk factors for sacroiliitis. The Journal of rheumatology. 2010;37(11):2402–8.
Burgos-Vargas R, Pacheco-Tena C, Vázquez-Mellado J. A short-term follow-up of enthesitis and arthritis in the active phase of juvenile onset spondyloarthropathies. Clinical and experimental rheumatology. 2002;20(5):727–31.
Stoll ML, Punaro M. Psoriatic juvenile idiopathic arthritis: a tale of two subgroups. Current opinion in rheumatology. 2011;23(5):437–43.
Ravelli A, Consolaro A, Schiappapietra B, Martini A. The conundrum of juvenile psoriatic arthritis. Clinical and experimental rheumatology. 2015;33(5 Suppl 93):S40–3.
Nordal E, Zak M, Aalto K, Berntson L, Fasth A, Herlin T, et al. Ongoing disease activity and changing categories in a long-term nordic cohort study of juvenile idiopathic arthritis. Arthritis and rheumatism. 2011;63(9):2809–18.
Modesto C, Antón J, Rodriguez B, Bou R, Arnal C, Ros J, et al. Incidence and prevalence of juvenile idiopathic arthritis in Catalonia (Spain). Scandinavian journal of rheumatology. 2010;39(6):472–9.
Oen K, Duffy CM, Tse SM, Ramsey S, Ellsworth J, Chédeville G, et al. Early outcomes and improvement of patients with juvenile idiopathic arthritis enrolled in a Canadian multicenter inception cohort. Arthritis care & research. 2010;62(4):527–36.
Kunjir V, Venugopalan A, Chopra A. Profile of Indian patients with juvenile onset chronic inflammatory joint disease using the ILAR classification criteria for JIA: a community-based cohort study. The Journal of rheumatology. 2010;37(8):1756–62.
Weiss PF, Beukelman T, Schanberg LE, Kimura Y, Colbert RA. Enthesitis-related arthritis is associated with higher pain intensity and poorer health status in comparison with other categories of juvenile idiopathic arthritis: the Childhood Arthritis and Rheumatology Research Alliance Registry. The Journal of rheumatology. 2012;39(12):2341–51.
Taxter AJ, Wileyto EP, Behrens EM, Weiss PF. Patient-reported Outcomes across Categories of Juvenile Idiopathic Arthritis. The Journal of rheumatology. 2015;42(10):1914–21.
Donnithorne KJ, Cron RQ, Beukelman T. Attainment of inactive disease status following initiation of TNF-α inhibitor therapy for juvenile idiopathic arthritis: enthesitis-related arthritis predicts persistent active disease. The Journal of rheumatology. 2011;38(12):2675–81.
Brunner HI, Schanberg LE, Kimura Y, Dennos A, Co DO, Colbert RA, et al. New Medications Are Needed for Children With Juvenile Idiopathic Arthritis. Arthritis & Rheumatology (Hoboken, NJ). 2020;72(11):1945–51.
Rizzo A, Guggino G, Ferrante A, Ciccia F. Role of subclinical gut inflammation in the pathogenesis of spondyloarthritis. Frontiers in medicine. 2018;5:63.
Stoll ML, Punaro M, Patel AS. Fecal calprotectin in children with the enthesitis-related arthritis subtype of juvenile idiopathic arthritis. The Journal of rheumatology. 2011;38(10):2274–5.
Cardoneanu A, Mihai C, Rezus E, Burlui A, Popa I, Cijevschi PC. Gut microbiota changes in inflammatory bowel diseases and ankylosing spondilytis. J Gastrointestin Liver Dis. 2021.
Tito RY, Cypers H, Joossens M, Varkas G, Van Praet L, Glorieus E, et al. Brief Report: Dialister as a Microbial Marker of Disease Activity in Spondyloarthritis. Arthritis & rheumatology (Hoboken, NJ). 2017;69(1):114–21.
Campos-Perez W, Martinez-Lopez E. Effects of short chain fatty acids on metabolic and inflammatory processes in human health. Biochim Biophys Acta Mol Cell Biol Lipids. 2021;158900.
Stoll ML, Weiss PF, Weiss JE, Nigrovic PA, Edelheit BS, Bridges SL Jr, et al. Age and fecal microbial strain-specific differences in patients with spondyloarthritis. Arthritis research & therapy. 2018;20(1):14.
Gill T, Asquith M, Brooks SR, Rosenbaum JT, Colbert RA. Effects of HLA-B27 on Gut Microbiota in Experimental Spondyloarthritis Implicate an Ecological Model of Dysbiosis. Arthritis Rheumatol. 2018;70(4):555–65.
Stoll ML, Duck LW, Chang MH, Colbert RA, Nigrovic PA, Thompson SD, et al. Identification of Prevotella Oralis as a possible target antigen in children with Enthesitis related arthritis. Clin Immunol. 2020;216:108463.
Lai CY, Sung J, Cheng F, Tang W, Wong SH, Chan PKS, et al. Systematic review with meta-analysis: review of donor features, procedures and outcomes in 168 clinical studies of faecal microbiota transplantation. Aliment Pharmacol Ther. 2019;49(4):354–63.
Ghantous N, Heshin-Bekenstein M, Dequattro K, Lakovsky Y, Hendel AM, Rappoport N, et al. Do geography and ethnicity play a role in juvenile Spondyloarthritis? A multi-center binational retrospective study. Pediatr Rheumatol Online J. 2021;19(1):4.
Evans DM, Spencer CC, Pointon JJ, Su Z, Harvey D, Kochan G, et al. Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility. Nature genetics. 2011;43(8):761–7.
Cargill M, Schrodi SJ, Chang M, Garcia VE, Brandon R, Callis KP, et al. A large-scale genetic association study confirms IL12B and leads to the identification of IL23R as psoriasis-risk genes. American journal of human genetics. 2007;80(2):273–90.
Hinks A, Martin P, Flynn E, Eyre S, Packham J, Barton A, et al. Subtype specific genetic associations for juvenile idiopathic arthritis: ERAP1 with the enthesitis related arthritis subtype and IL23R with juvenile psoriatic arthritis. Arthritis research & therapy. 2011;13(1):R12.
Wang Z, Han Y, Zhang Z, Jia C, Zhao Q, Song W, et al. Identification of genes and signaling pathways associated with the pathogenesis of juvenile spondyloarthritis. Mol Med Rep. 2018;18(2):1263–70.
Kasper M, Walscheid K, Laffer B, Bauer D, Busch M, Loser K, et al. Phenotype of Innate Immune Cells in Uveitis Associated with Axial Spondyloarthritis- and Juvenile Idiopathic Arthritis-associated Uveitis. Ocul Immunol Inflamm. 2020:1–10.
Inciarte-Mundo J, Ramirez J, Hernandez MV, Ruiz-Esquide V, Cuervo A, Cabrera-Villalba SR, et al. Calprotectin strongly and independently predicts relapse in rheumatoid arthritis and polyarticular psoriatic arthritis patients treated with tumor necrosis factor inhibitors: a 1-year prospective cohort study. Arthritis Res Ther. 2018;20(1):275.
Etzerodt A, Moestrup SK. CD163 and inflammation: biological, diagnostic, and therapeutic aspects. Antioxid Redox Signal. 2013;18(17):2352–63.
Baeten D, Demetter P, Cuvelier CA, Kruithof E, Van Damme N, De Vos M, et al. Macrophages expressing the scavenger receptor CD163: a link between immune alterations of the gut and synovial inflammation in spondyloarthropathy. J Pathol. 2002;196(3):343–50.
Bhattacharya S, Misra R, Aggarwal A. Patients with enthesitis related arthritis show similar monocyte function pattern as seen in adult axial spondyloarthropathy. Pediatr Rheumatol Online J. 2020;18(1):6.
Reinhardt A, Prinz I. Whodunit? The Contribution of Interleukin (IL)-17/IL-22-Producing gammadelta T Cells, alphabeta T Cells, and Innate Lymphoid Cells to the Pathogenesis of Spondyloarthritis. Front Immunol. 2018;9:885.
Colbert RA, Tran TM, Layh-Schmitt G. HLA-B27 misfolding and ankylosing spondylitis. Mol Immunol. 2014;57(1):44–51.
DeLay ML, Turner MJ, Klenk EI, Smith JA, Sowders DP, Colbert RA. HLA-B27 misfolding and the unfolded protein response augment interleukin-23 production and are associated with Th17 activation in transgenic rats. Arthritis and rheumatism. 2009;60(9):2633–43.
Flores RR, Carbo L, Kim E, Van Meter M, De Padilla CML, Zhao J, et al. Adenoviral gene transfer of a single-chain IL-23 induces psoriatic arthritis-like symptoms in NOD mice. FASEB J. 2019;33(8):9505–15.
Venken K, Jacques P, Mortier C, Labadia ME, Decruy T, Coudenys J, et al. RORgammat inhibition selectively targets IL-17 producing iNKT and gammadelta-T cells enriched in Spondyloarthritis patients. Nat Commun. 2019;10(1):9.
Chen S, Paveley R, Kraal L, Sritharan L, Stevens E, Dedi N, et al. Selective targeting of PI3Kdelta suppresses human IL-17-producing T cells and innate-like lymphocytes and may be therapeutic for IL-17-mediated diseases. J Autoimmun. 2020;111:102435.
Weiss PF, Chauvin NA, Roth J. Imaging in Juvenile Spondyloarthritis. Current rheumatology reports. 2016;18(12):75.
Jaremko JL, Liu L, Winn NJ, Ellsworth JE, Lambert RG. Diagnostic utility of magnetic resonance imaging and radiography in juvenile spondyloarthritis: evaluation of the sacroiliac joints in controls and affected subjects. The Journal of rheumatology. 2014;41(5):963–70.
Weiss PF, Xiao R, Brandon TG, Biko DM, Maksymowych WP, Lambert RG, et al. Radiographs in screening for sacroiliitis in children: what is the value? Arthritis research & therapy. 2018;20(1):141.
Chauvin NA, Xiao R, Brandon TG, Biko DM, Francavilla M, Khrichenko D, et al. MRI of the Sacroiliac Joint in Healthy Children. AJR Am J Roentgenol. 2019:1–7.
Weiss PF, Brandon TG, Bohnsack J. Heshin-Bekenstein M. Jaremko JL, et al. Variability in magnetic resonance imaging interpretation of the pediatric sacroiliac joint. Arthritis care & research: Francavilla ML; 2020.
Otobo TM, Conaghan PG, Maksymowych WP, van der Heijde D, Weiss P, Sudol-Szopinska I, et al. Preliminary Definitions for Sacroiliac Joint Pathologies in the OMERACT Juvenile Idiopathic Arthritis Magnetic Resonance Imaging Score (OMERACT JAMRIS-SIJ). The Journal of rheumatology. 2019;46(9):1192–7.
Maksymowych WP, Inman RD, Salonen D, Dhillon SS, Williams M, Stone M, et al. Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. Arthritis and rheumatism. 2005;53(5):703–9.
Maksymowych WP, Wichuk S, Chiowchanwisawakit P, Lambert RG, Pedersen SJ. Development and preliminary validation of the spondyloarthritis research consortium of Canada magnetic resonance imaging sacroiliac joint structural score. The Journal of rheumatology. 2015;42(1):79–86.
Panwar J, Tse SML, Lim L, Tolend MA, Radhakrishnan S, Salman M, et al. Spondyloarthritis Research Consortium of Canada Scoring System for Sacroiliitis in Juvenile Spondyloarthritis/Enthesitis-related Arthritis: A Reliability, Validity, and Responsiveness Study. The Journal of rheumatology. 2019;46(6):636–44.
Weiss PF, Maksymowych WP, Xiao R, Biko DM, Francavilla ML, Lambert RG, et al. Spondyloarthritis Research Consortium of Canada sacroiliac joint inflammation and structural scores: change score reliability and recalibration utility in children. Arthritis research & therapy. 2020;22(1):58.
Panwar J, Patel H, Tolend M, Akikusa J, Herregods N, Highmore K, et al. Toward Developing a Semiquantitative Whole Body-MRI Scoring for Juvenile Idiopathic Arthritis: Critical Appraisal of the State of the Art, Challenges, and Opportunities. Academic radiology. 2021;28(2):271–86.
Bridges JM, Stoll ML. Treatment of Juvenile Spondyloarthritis: Where We Stand. Paediatr Drugs. 2020;22(6):603–15.
Weiss PF, Fuhlbrigge RC, von Scheven E, Lovell DJ, Colbert RA, Brunner HI. Children with enthesitis-related arthritis could benefit from treatments targeted for adults with spondyloarthritis. Arthritis care & research. 2020.
Ringold S, Angeles-Han ST, Beukelman T, Lovell D, Cuello CA, Becker ML, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non-Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis & rheumatology (Hoboken, NJ). 2019;71(6):846–63.
Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis & rheumatology (Hoboken, NJ). 2019;71(10):1599-613.
Burgos-Vargas R, Tse SM, Horneff G, Pangan AL, Kalabic J, Goss S, et al. A Randomized, Double-Blind, Placebo-Controlled Multicenter Study of Adalimumab in Pediatric Patients With Enthesitis-Related Arthritis. Arthritis care & research. 2015;67(11):1503–12.
Constantin T, Foeldvari I, Vojinovic J, Horneff G, Burgos-Vargas R, Nikishina I, et al. Two-year Efficacy and Safety of Etanercept in Pediatric Patients with Extended Oligoarthritis, Enthesitis-related Arthritis, or Psoriatic Arthritis. The Journal of rheumatology. 2016;43(4):816–24.
Foeldvari I, Constantin T, Vojinović J, Horneff G, Chasnyk V, Dehoorne J, et al. Etanercept treatment for extended oligoarticular juvenile idiopathic arthritis, enthesitis-related arthritis, or psoriatic arthritis: 6-year efficacy and safety data from an open-label trial. Arthritis research & therapy. 2019;21(1):125.
Kearsley-Fleet L, Davies R, Lunt M, Southwood TR, Hyrich KL. Factors associated with improvement in disease activity following initiation of etanercept in children and young people with Juvenile Idiopathic Arthritis: results from the British Society for Paediatric and Adolescent Rheumatology Etanercept Cohort Study. Rheumatology (Oxford, England). 2016;55(5):840–7.
Brunner HI, Ruperto N, Tzaribachev N, Horneff G, Chasnyk VG, Panaviene V, et al. Subcutaneous golimumab for children with active polyarticular-course juvenile idiopathic arthritis: results of a multicentre, double-blind, randomised-withdrawal trial. Annals of the rheumatic diseases. 2018;77(1):21–9.
Ruperto N, Brunner HI, Pacheco-Tena C, Louw I, Vega-Cornejo G, Spindler AJ, et al. Open-Label Phase 3 Study of Intravenous Golimumab in Patients With Polyarticular Juvenile Idiopathic Arthritis. Rheumatology (Oxford, England). 2021.
Weiss PF, Xiao R, Brandon TG, Pagnini I, Wright TB, Beukelman T, et al. Comparative Effectiveness of Tumor Necrosis Factor Agents and Disease-modifying Antirheumatic Therapy in Children with Enthesitis-related Arthritis: The First Year after Diagnosis. The Journal of rheumatology. 2018;45(1):107–14.
Favalli EG, Pontikaki I, Becciolini A, Biggioggero M, Ughi N, Romano M, et al. Real-life 10-year retention rate of first-line anti-TNF drugs for inflammatory arthritides in adult- and juvenile-onset populations: similarities and differences. Clinical rheumatology. 2017;36(8):1747–55.
Skrabl-Baumgartner A, Erwa W, Muntean W, Jahnel J. Anti-adalimumab antibodies in juvenile idiopathic arthritis: frequent association with loss of response. Scandinavian journal of rheumatology. 2015;44(5):359–62.
Chamlati R, Connolly B, Laxer R, Stimec J, Panwar J, Tse S, et al. Image guided sacroiliac joint corticosteroid injections in children: an 18-year single-center retrospective study. Pediatric rheumatology online journal. 2020;18(1):52.
van der Heijde D, Cheng-Chung Wei J, Dougados M, Mease P, Deodhar A, Maksymowych WP, et al. Ixekizumab, an interleukin-17A antagonist in the treatment of ankylosing spondylitis or radiographic axial spondyloarthritis in patients previously untreated with biological disease-modifying anti-rheumatic drugs (COAST-V): 16 week results of a phase 3 randomised, double-blind, active-controlled and placebo-controlled trial. Lancet. 2018;392(10163):2441–51.
Deodhar A, Poddubnyy D, Pacheco-Tena C, Salvarani C, Lespessailles E, Rahman P, et al. Efficacy and Safety of Ixekizumab in the Treatment of Radiographic Axial Spondyloarthritis: Sixteen-Week Results From a Phase III Randomized, Double-Blind, Placebo-Controlled Trial in Patients With Prior Inadequate Response to or Intolerance of Tumor Necrosis Factor Inhibitors. Arthritis Rheumatol. 2019;71(4):599–611.
Dougados M, Wei JC, Landewe R, Sieper J, Baraliakos X, Van den Bosch F, et al. Efficacy and safety of ixekizumab through 52 weeks in two phase 3, randomised, controlled clinical trials in patients with active radiographic axial spondyloarthritis (COAST-V and COAST-W). Ann Rheum Dis. 2020;79(2):176–85.
Pavelka K, Kivitz A, Dokoupilova E, Blanco R, Maradiaga M, Tahir H, et al. Efficacy, safety, and tolerability of secukinumab in patients with active ankylosing spondylitis: a randomized, double-blind phase 3 study, MEASURE 3. Arthritis Res Ther. 2017;19(1):285.
Hueber W, Sands BE, Lewitzky S, Vandemeulebroecke M, Reinisch W, Higgins PD, et al. Secukinumab, a human anti-IL-17A monoclonal antibody, for moderate to severe Crohn's disease: unexpected results of a randomised, double-blind placebo-controlled trial. Gut. 2012;61(12):1693–700.
McInnes IB, Chakravarty SD, Apaolaza I, Kafka S, Hsia EC, You Y, et al. Efficacy of ustekinumab in biologic-naïve patients with psoriatic arthritis by prior treatment exposure and disease duration: data from PSUMMIT 1 and PSUMMIT 2. RMD open. 2019;5(2):e000990.
Baeten D, Østergaard M, Wei JC, Sieper J, Järvinen P, Tam LS, et al. Risankizumab, an IL-23 inhibitor, for ankylosing spondylitis: results of a randomised, double-blind, placebo-controlled, proof-of-concept, dose-finding phase 2 study. Annals of the rheumatic diseases. 2018;77(9):1295–302.
Mannion ML, McAllister L, Cron RQ, Stoll ML. Ustekinumab as a Therapeutic Option for Children With Refractory Enthesitis-Related Arthritis. Journal of clinical rheumatology: practical reports on rheumatic & musculoskeletal diseases. 2016;22(5):282–4.
Ruperto N, Brunner HI, Zuber Z, Tzaribachev N, Kingsbury DJ, Foeldvari I, et al. Pharmacokinetic and safety profile of tofacitinib in children with polyarticular course juvenile idiopathic arthritis: results of a phase 1, open-label, multicenter study. Pediatric rheumatology online journal. 2017;15(1):86.
Brunner H SO, Ting T, Abud Mendoza C, Spindler A, Vyzhga Y, Marzan K, Keltsev V, Tirosh I, Imundo L, Jerath R, Kingsbury D, Sozeri B, Vora S, Prahalad S, Zholobova E, Butbul Aviel Y, Chasnyk V, Lerman M, Nanda K, Schmeling H, Tory H, Uziel Y, V. Tofacitinib for the Treatment of Polyarticular Course Juvenile Idiopathic Arthritis: Results of a Phase 3 Randomized, Double-blind, Placebo-controlled Withdrawal Study. American College of Rheumatology Arthritis Rheumatol; 2019.
Brunner H AJ, Al-Abadi E, Bohnsack J, Boteanu A, Chedeville G, Cuttica R, De La Pena W, Jung L, Kasapcopur O, Kobusinska K, Schulert G, Neiva C, Rivas-Chacon R, Cruz Rizo Rodriguez J, Vazquez-Del Mercado M, Wagner-Weiner L, Weiss J, Wouters C, Suehiro R, Posner H, Wouters A, Kanik K, Luo Z, Martini A, Lovell D, Ruperto N. Tofacitinib for the Treatment of Patients with Juvenile Idiopathic Arthritis: An Interim Analysis of Data up to 5.5 Years from an Open-label, Long-term Extension Study. American College of Rheumatology Arthritis Rheumatol; 2020.
Van Mechelen M, Lories R. Spondyloarthritis on the Move: Biomechanical Benefits or Harm. Current rheumatology reports. 2020;22(8):35.
Powell AP, English J. Exercise for Athletes With Inflammatory Arthritis. Curr Sports Med Rep. 2018;17(9):302–7.
Houghton KM, Macdonald HM, McKay HA, Guzman J, Duffy C, Tucker L. Feasibility and safety of a 6-month exercise program to increase bone and muscle strength in children with juvenile idiopathic arthritis. Pediatric rheumatology online journal. 2018;16(1):67.
Toupin April K, Stinson J, Cavallo S, Proulx L, Wells GA, Duffy CM, et al. Yoga and Aerobic Dance for Pain Management in Juvenile Idiopathic Arthritis: Protocol for a Pilot Randomized Controlled Trial. JMIR Res Protoc. 2020;9(7):e12823.
Morgan EM, Munro JE, Horonjeff J, Horgan B, Shea B, Feldman BM, et al. Establishing an Updated Core Domain Set for Studies in Juvenile Idiopathic Arthritis: A Report from the OMERACT 2018 JIA Workshop. The Journal of rheumatology. 2019;46(8):1006–13.
Weiss PF, Colbert RA, Xiao R, Feudtner C, Beukelman T, DeWitt EM, et al. Development and retrospective validation of the juvenile spondyloarthritis disease activity index. Arthritis care & research. 2014;66(12):1775–82.
Zanwar A, Phatak S, Aggarwal A. Prospective validation of the Juvenile Spondyloarthritis Disease Activity Index in children with enthesitis-related arthritis. Rheumatology (Oxford, England). 2018;57(12):2167–71.
Acknowledgements
This research was supported [in part] by the Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spondyloarthritis
Rights and permissions
About this article
Cite this article
Srinivasalu, H., Treemarcki, E.B. & Redmond, C. Advances in Juvenile Spondyloarthritis. Curr Rheumatol Rep 23, 70 (2021). https://doi.org/10.1007/s11926-021-01036-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11926-021-01036-4