Abstract
The objective of osteoarthritis (OA) treatment is not only control of symptoms (i.e. reducing pain and improving function) but also to preserve joint structure and maintain quality of life. OA management remains challenging. Glucosamine and chondroitin are two compounds available for treatment of OA patients. Taken alone or in combination, they have a good safety profile and a variety of effects. In-vitro and in-vivo experiments have revealed that both compounds induced key intermediates in the OA pathophysiological process. Clinical trials, although providing conflicting and questionable results, report symptomatic and structure-modifying effects for both pharmaceutical-grade compounds. This review will discuss all these subjects and emphasize the importance of the quality of tested compounds for achieving high quality clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is one of the most debilitating arthritic diseases, associated with pain and impairment of joint function leading to patient disability. This common and multi-factorial disease, which evolves over decades, remains incurable. OA involves all joint tissues [58•, 73], and is associated with degeneration of articular cartilage and of the menisci, and sclerosis of subchondral bone accompanied by inflammation of the synovial membrane.
OA pathogenesis is complex, and management of OA is challenging. No specific therapy has yet been found to stop disease progression: management of OA mostly involves control of symptoms, i.e. reduction of pain and improvement of joint function, and relies on a combination of non-pharmacological and pharmacological approaches as recommended in recent clinical guidelines [34, 47, 93–96, 97••]. Although important, symptom control is not the only objective of OA treatment. An ideal treatment would preserve articular structures, improve patient quality of life [35], and have a good safety profile. It is of great importance to take into account side effects of OA therapy, as illustrated by the long-term risks associated with non-steroidal anti-inflammatory drugs [90].
Symptomatic slow-acting drugs (SYSADOAs), including chondroitin sulfate (CS) and glucosamine (GlcN) sulfate (S) or hydrochloride (HCl), are part of the symptomatic treatment of OA. Some of these compounds have also been revealed, on the basis of joint-space narrowing measured on plain radiographs, to have disease-modifying (DMOAD) potential. Use of these compounds, and the significance of their clinical efficacy, is debated: they are sold “over the counter” as dietary supplements in North America, whereas they are registered drugs in Europe.
CS and GlcN are recommended by European League Against Rheumatism (EULAR) and Osteoarthritis Research Society International (OARSI) guidelines for treatment of symptomatic knee and hip OA [93, 95, 96, 97••]. However, recent American College of Rheumatology (ACR) guidelines did not recommend these compounds [34] because data supporting their efficacy are equivocal, they are not approved by the Food and Drug Administration (FDA), and they are only available as dietary supplements. Both products have a variety of properties, revealed by in-vivo and in-vitro experiments, and clinical trials of their effects revealed many causes for concern. This review will provide an update on possible mechanisms of action of GlcN and CS, and will review and discuss clinical trial results. Finally, the potential benefits of treatment with a combination of these products will be investigated.
Glucosamine
In-vivo and in-vitro experiments, many of which have recently been reviewed [32•], have provided much evidence for possible mechanisms of action leading to structure-modifying effects of glucosamine. This section will update the reader on effects observed in vivo and in vitro on cartilage, subchondral bone, and synovial inflammation. It will also cover the effect of glucosamine on OA symptoms, and its structure-modifying potential observed in clinical trials.
In-vitro Effect
GlcN was first believed to affect cartilage by providing building blocks for synthesis of glycosaminoglycans (GAG) by the GLUT receptor, then by competing with glucose [30]. Studies reported that GlcN could have anti-catabolic and anti-inflammatory effects: when GlcN-HCl (100 μg mL−1) is applied to chondrocytes and synoviocytes it inhibits inflammatory mediators, prostaglandin (PG) E2, nitric oxide (NO), and matrix metalloproteinases (MMPs) [65]. This is the result of its effect on different cell-signaling intermediates: for example, it has been revealed to inhibit cyclooxygenase (COX)-2 and MMP-13 in human skin fibroblasts (10 mmol L−1) by blocking p38 [38]. These results support previously published data obtained from chondrosarcoma cell lines [57] and mouse macrophages (RAW 264.7) [71]. D-GlcN (2 mmol L−1) blocks activation of the signaling intermediates p38 and Akt, thus inhibiting COX-2 expression, PGE2 production and iNOS expression and synthesis (p38), and MMP-3 inhibition and proteoglycan synthesis (Akt) [57]. Inhibition by GlcN-HCl (2.5–10 mmol L−1) of COX-2 and iNOS in mouse macrophages was also found to occur via inhibition of p38 [71]. Finally, a cationic derivative of GlcN (10–50 μg mL−1) was proved to inhibit production of cytokines and MAPK, p38 and JNK in RAW 264.7 [60]. The latest study revealed that GlcN inhibited MMP-2 and MMP-9, and confirmed its effect on nuclear factor-kappa B (NF-κB) and on AP-1 [61]. It was also revealed that GlcN affected both NF-κB synthesis and its translocation to the nucleus. The inhibitory effect of GlcN on NF-κB was first observed in human OA chondrocytes with GlcN-S (10–1,000 μg mL−1) [54]. This effect was recently revealed to occur via an epigenetic mechanism [43]: GlcN prevents demethylation of specific CpG sites in the IL-1β promoter, consequently preventing expression of IL-1β.
Inhibition of MMPs could be caused by the increased GAG production observed in synovial cells and chondrocytes with GlcN-HCl (0.06–1 mmol L−1) [40]. Another study suggested that the protective effect of GlcN-HCl in rat cartilage was brought about via induction of anabolic mediators, including transforming growth factor (TGF)-β1 and connective tissue growth factor (CTGF) [2]. Kapoor et al. revealed that GlcN-S (1–2 mmol L−1) reduced PGE2 in human chondrocytes via inhibition of microsomal prostaglandin E synthase 1 (mPGES1) [49]. The same study revealed inhibition of COX-2 and increased levels of an anti-inflammatory transcription factor, peroxisome proliferator-activated receptor (PPAR)-λ.
Chiusaroli et al. revealed that low concentrations of GlcN-S (0.001–100 μmol L −1) inhibited IL-1β-stimulated IL-6, tumor necrosis factor (TNF)-α, MMP-3 and a disintegrin and metalloproteinase with thrombospondin motifs (ADAMTS)-5 in a chondrosarcoma cell line (SW1353), via inhibition of NF-κB and AP-1 [21•]. The same authors continued the investigation with an in-vivo experiment on the STR/ort mouse (which spontaneously develops OA), and reported that GlcN reduced all OA histology scores.
A recent pharmacoproteomic study by Calamia et al. [12••] revealed that GlcN-S inhibited proteins involved in signal transduction pathways, redox and stress response, and protein synthesis and folding processes. GlcN may also increase levels of chaperone GRP78, suggesting another possible mechanism for GlcN’s anti-inflammatory effect.
In addition to cartilage and synovial membrane, it is now well recognized that subchondral bone has an important function in OA pathogenesis. GlcN (0.1–1 mmol L−1) induced osteoblast differentiation and blocked differentiation of osteoclasts in mouse cells (MC3T3-E1) [41], limiting the effect on bone resorption and enabling bone deposition. The effect that it produced on the osteoblastic differentiation of MG-63 cells was more than that associated with an anti-inflammatory action [51].
Animal Studies
In animal studies, GlcN had different protective effects. High doses of GlcN (300 mg kg−1) given to rats with adjuvant arthritis (AA) reduced both arthritic score and synovitis [39]. This effect was associated with reduction of PGE2 and NO concentrations in plasma. Different studies have illustrated the anabolic effect of GlcN. GlcN-HCl (100 mg daily) administered to rabbits after anterior cruciate ligament transection (ACLT) preserved cartilage [78]. The same effect was observed when GlcN-HCl (20 or 100 mg day−1) was administered to rabbits after chymopapain injection [66]. Cartilage preservation was believed to be caused by restoration of GAG content. Loss of GAG in cartilage, and bone erosion and osteophyte formation, were also inhibited by GlcN-HCl (20 mg kg−1 day−1) administered to collagen-induced-arthritis (CIA) mice [44]. Reduced soluble receptor activator of nuclear factor-kappa B ligand (RANKL) and interleukin (IL)-6, and increased IL-10, were believed to cause this protective effect. For rats, GlcN-HCl also reduced macroscopic changes induced by ACLT, and inhibited degradation and enhanced synthesis of type II collagen [64]. For guinea pigs spontaneously developing OA, GlcN-HCl (200 mg kg−1) reduced Mankin histology scores for OA via inhibition of MMP-3 mRNA [75]. For ACLT rabbits with early stage OA, GlcN-HCl (100 mg day−1) preserved joint structure, possibly by attenuating bone changes [87]. Finally, GlcN-S (250 mg kg−1 day−1) affected rat nociception, protected cartilage and reduced synovitis, via inhibition of mitogen-activated protein kinases (MAPK), p38, and JNK, and increasing extra-cellular Erk1/2 [89]. It is noted that most experimental data concern GlcN-HCl.
Clinical Efficacy
Whether GlcN should be regarded as a SYSADOA and whether it has a structure-modifying effect remain controversial. However, numerous published clinical trials document a symptomatic effect, i.e. reduced pain and improved joint function. There have been several meta-analyses (MAs) of data from these trials [8, 59, 70, 79, 82].
The DMOAD effect of GlcN was analyzed by two MAs [55•, 86]. On the basis of an effect size (ES) for joint pain of −0.17 (−0.28 to −0.05) and for joint space width (JSW) of −0.16 (−0.25 to 0.00), Wandel et al. reported no clinically meaningful effect [86]. However, this MA had several limitations [29] and several OA experts have questioned the validity of the conclusions. Disadvantages of this MA were addressed in part by the report from the British Medical Journal post-publication review meeting, which states that the study data did not directly support the strong negative conclusion (Groves T. Report from BMJ post publication review meeting. Available at: http://www.bmj.com/content/341/bmj.c4675.full%20./reply#bmj_el_247719; accessed July 21, 2013).
A second MA reported a small-to-moderate protective effect on the minimum JSN after three years. However, it included only two trials [55•]. The GAIT study, the largest randomized controlled trial (RCT), did not report any significant effect of GlcN-HCl for knee OA patients [24], and no effect of GlcN-S was observed for hip OA [72]. However, a recent trial suggested GlcN-S could prevent total knee replacement (TKR) [9].
When analyzing the symptomatic and structure-modifying effects of GlcN, it is important to consider the RCT analysis provided in OARSI’s recommendations. OARSI guidelines committee members analyzed 19 RCTs (16 of GlcN-S and three of GlcN-HCl) [97••]. They reported an ES for pain of 0.46 (0.23 to 0.69), which was reduced in size compared with the previous analysis (0.61 (0.28 to 0.95)) but still equivalent to a moderate effect on symptoms [96]. Data analysis continues to emphasize the difference between different preparations of glucosamine: the ES for pain of GlcN-S is 0.58 (0.30 to 0.87), whereas that of GlcN-HCl ES is −0.02 (−0.15 to 0.11). In addition, the ES for pain of GlcN-S tended to decrease when only high-quality clinical trials were included in analysis (0.29 (0.003 to 0.57)). This analysis also reported a reduction of joint space narrowing (JSN) ES for GlcN-S of 0.24 (0.04 to 0.43) for knee OA, but no effect on hip OA.
Chondroitin Sulfate
As for GlcN, understanding of the mechanisms of action of CS is incomplete. Several extensive reviews [26, 31, 85] have detailed the effectiveness of CS in vivo and in vitro. This section will summarize available information and discuss use of CS as a symptomatic and structure-modifying OA treatment. Just as there is controversy about which glucosamine formulation has the greatest effect, different authors favor different chondroitin formulas. Different CS formulations produce different effects in vitro. C4S from shark cartilage and C6S from porcine cartilage had different efficacy profiles for chondrocytes and synoviocytes [42], and in a pharmacoproteomic study [10•] on chondrocytes, reported by Tat et al. [76], different results were obtained with three different CS formulations. Hence, because CS is extracted and purified from animal sources, different properties and effects are observed [83, 84].
In-vitro Effect
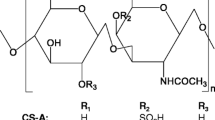
Recent in-vitro studies have investigated the mechanism of action of CS to explain its variety of properties. Its anti-inflammatory effects have been widely reviewed [26, 32•, 85]. In addition to an anabolic effect, CS has anti-inflammatory, anti-catabolic, anti-apoptotic, and anti-oxidant effects (Fig. 1) on articular tissue. Its anti-catabolic effects have been studied in human chondrocytes and synovial fibroblasts [42]. CS (1–10 μg mL−1) inhibited IL-1β-induced expression of ADAMTS-4 and ADAMTS-5 genes in both cell types, and increased levels of tissue inhibitor of metalloproteinase (TIMP)-1 and TIMP-3 in synoviocytes. CS also had an anabolic effect, characterized by increased type II collagen and proteoglycan synthesis in human articular chondrocytes [4, 88] and increased GAG, with concentrations in the range 1–1,000 μg mL−1, in bovine chondrocytes [56]. The anti-catabolic effect in chondrocytes occurred at doses in the range 1–1,000 μg mL−1, via inhibition of MMP-1, MMP-3, and MMP-13, and via ADAMTS-4 and ADAMTS-5 expression [56, 63, 74]. Another mechanism of action is induction of some cell signaling intermediates, including Akt and Erk1/2, and inhibition of some others, including p38 and JNK. In human synoviocytes, CS (100 μg mL−1) brought about activation of hyaluronic acid (HA) synthase and HA production [25]. The investigators interpreted their results as indicating that CS had an anti-inflammatory effect, and that it maintained viscosity within the joint. A joint-lubricating effect was also suggested in bovine cartilage explants [50]. Other signaling mediators are also affected by CS: p38 and Erk1/2 activation were inhibited by CS (25 μg mL−1) in human articular chondrocytes stimulated by lipopolysaccharide (LPS), reducing levels of MMP-13 [37].
Schematic representation of the cellular mechanisms of action of chondroitin sulfate (CS). ERK, extracellular signal-regulated kinases; JNK, c-Jun N-terminal kinases; IKK, IκB kinase; NFκB, nuclear factor kappa-light-chain-enhancer of activated B cell; ROS, reactive oxygen species; MMP, matrix metalloproteases; IL, interleukin; PGE2, prostaglandin E2; NO, nitric oxide
CS (0.5–1.0 mg mL−1) had anti-apoptotic effects on mouse chondrocytes stimulated with LPS [17], and CS (30–120 mg kg−1) inhibited caspase-3 and caspase-9 and NF-κB in mouse CIA [16].
Inhibition of NF-κB by CS could be an important mechanism for both its chondroprotective and its anti-inflammatory effect. CS inhibits both p38 and Erk1/2 activation, and inhibits NF-κB translocation in rabbit chondrocytes (CS, 200 μg mL−1) [46]. A potent anti-inflammatory effect of CS (25–50 μg mL−1) was observed in mouse chondrocytes. In this model, inhibition by CS of the signaling pathway involving MyD88, TRAF-6 and NF-κB activation [18] caused down-regulation of inflammatory cytokines and iNOS. This evidence supports the theory that CS has a function in cell survival and anti-inflammatory action [81], resulting in its chondroprotective effect.
Another potentially important aspect of the effect of CS on OA is its anti-oxidant effect. CS provided protection against hydrogen peroxide and superoxide anions, limited cell death by reducing DNA fragmentation and protein oxidation, reduced generation of free radicals, and acted as a scavenger. It reduced lipid peroxidation, and supported anti-oxidative defense by restoring endogenous anti-oxidants, including glutathione and superoxide dismutase (GSH and SOD) [14, 15]. Interestingly, CS had anti-angiogenic potential in an innovative model of culture of human OA synoviocytes [53]: CS (10–200 μg mL−1) reversed the inhibitory effect of IL-1 on the anti-angiogenic factors VEGI and TSP-1. This mechanism could explain the protective and anti-inflammatory effect of CS in the synovial membrane. Finally, CS (200 μg mL−1) preserved subchondral bone in human OA osteoblasts, reducing bone resorption while increasing osteoprotegerin (OPG) and reducing RANKL, then modulating the OPG/RANKL ratio to favor bone formation [77]. A recent study of primary calvaria mouse osteoblasts confirmed and detailed the CS mechanism of action [69•]: CS (100 μg mL−1) reduced PGE2 and MMP-3 and MMP-13 in an inflammatory context, and inhibited COX-2, mPGES1, and RANKL. Furthermore, the previously mentioned pharmacoproteomic study on articular chondrocytes [12••], revealed that CS blocked proteins involved in energy production (31 %) and metabolic pathways (15 %). An additional investigation of the chondrocyte secretome [11••] also provided evidence of potential anti-inflammatory, anti-angiogenic, and anti-catabolic properties of CS. CS inhibited several complement components (CFAB, C1S, CO3, and C1R) and increased TNF-α-induced protein (TSG6), which is responsible for reduction of pro-MMP activation.
Animal Studies
The effect of CS observed in animal models provided insight into the potential of CS for use as an anti-inflammatory agent able to preserve articular structures. It has been known for a long time that CS can reduce synovitis (1,000 mg kg−1) [67] and inhibit IL-6 (1,200 mg kg−1) [22] in mouse CIA. In addition, when administered as a food supplement (1.2 g kg−1 day−1) CS halted IL-1β effects in rat adjuvant arthritis (AA) [23], inhibited plasma TNF-α and myeloperoxidase, and limited destruction of articular structures in rat CIA [13]. More recently, CS (300–900 mg kg−1) reduced severity of arthritis and inhibited oxidative stress in rat AA [5]. The authors reported that the treatment reduced C-reactive protein (CRP), phagocytic activity and the intra-cellular oxidative burst of neutrophils. As also observed for GlcN-HCl, when tested on guinea pigs spontaneously developing OA, CS (200 mg kg−1) protected cartilage by inhibition of MMP-3 mRNA [75].
Clinical Efficacy
Clinical trials have evaluated the symptomatic potential and structure-modifying effect of CS. There is much evidence of the symptomatic efficacy of CS for knee OA [9], and a highly purified CS formulation (800 mg day−1) reduced symptoms of hand OA [27••]. A recent study [92] observed a similar efficacy of CS for symptoms (pain on VAS and LI for function) when administered as a single daily dose of 1,200 mg or three times a day at 400 mg. The authors concluded that CS was an effective and safe intervention. One of the few positive findings of the GAIT study was that CS significantly reduced joint swelling and effusion [24].
A significant DMOAD effect of CS has been reported by RCTs. It was observed to produce a reduction of JSN [48], a significant difference in mean and minimum JSW [62], and a significant difference in joint space surface and mean JSW [80]. The MA by Hochberg et al. [36] and its update [33], including studies of two years’ duration, concluded that CS (800 mg kg−1) had a modest but significant effect on decline of minimum JSW. A second MA by Lee et al. concluded that both CS and GlcN could delay disease progression [55•]. A recent trial, not yet included in published MAs, reported a symptomatic effect of CS (800 mg day−1) combined with reduction of cartilage volume loss, bone marrow lesion, and synovitis for knee OA patients [91].
The analysis in the OARSI guidelines [97••] determined an ES of 0.75 (0.50–0.99) for pain and of 0.26 (0.16–0.36) for JSN, but mentioned that industry bias could exist and that results were heterogeneous. If all studies are considered, the ES for pain of CS (0.75 (0.50–1.01)) was higher than those reported for GS (0.58 (0.30–0.87)) and, interestingly, for NSAIDS (0.29 (0.22–0.39)). Therefore, some investigators suggest that the risk/benefit balance seems to be in favor of CS and that this should be considered when making therapeutic decisions in daily practice.
Glucosamine and Chondroitin Combination
GlcN and CS have also been tested for efficacy when administered in combination, to determine whether concomitant administration of GlcN and CS could provide additional benefit over either agent alone.
In-vitro Effect
Some evidence for combined effects of GlcN and CS comes from in-vitro experiments. A combination of 5 μg mL−1 GlcN-HCl and 20 μg mL−1 CS had complementary anti-catabolic and anti-inflammatory effects in bovine cartilage explants stimulated by IL-1β [19, 20]. The combination reversed the catabolic effect of IL-1β by inhibiting the proteolytic enzymes MMP-3, MMP-13, ADAMTS-4, and ADAMTS-5, and by increasing the expression of TIMP-1 and TIMP-3. This effect resulted in increased expression of GAG and increased type II collagen. Under the same experimental conditions the anti-inflammatory mediators mPGES1, COX-2, PGE2, and NO were inhibited by the GlcN–CS combination, rather than by CS alone.
Another study ([12••], previously mentioned) observed that not only could both compounds affect different pathways, but that they could also induce combined inhibition of superoxide dismutase (SOD)-2. This further supports the theory that, at least in combination, these two agents have an anti-oxidant effect.
The anti-resorptive effect observed with CS alone was confirmed for the combination of GlcN (200 μg mL−1) and CS (200 μg mL−1) in OA osteoblasts [77]. On the basis of this study, the combination might be more effective against bone resorption than either compound alone.
Animal Studies
In vivo, the combination of GlcN-S (1,000 mg kg−1) and CS (800 mg kg−1) was chondroprotective for rabbit OA generated through partial meniscectomy [52]. The combination of 1.5 g kg−1 day−1 GlcN-S + 1.2 g kg−1 day−1 CS, given via a food bar, was observed to have a better effect than CS alone on mouse CIA, inhibiting IL-1β and MMP-9. A combination of GlcN (750 mg) and CS (750 mg) administered intramuscularly) also had a positive effect on horses with OA, measured via a flexion test of the tarsocrural and metacarpophalangeal joints [3]. A significant symptomatic effect of the combination (1.8 g day−1 GlcN + 5.4 g day−1 CS) was also reported by an in-vivo investigation on global pain of horses [28].
Finally, a combination of GlcN-HCl (500 mg) and CS (400 mg) seemed to enable rabbits to remodel tendon [68]. It is important to consider the effect of potential OA treatment on soft periarticular tissues, because these also affect pathogenesis of OA.
Clinical Efficacy
Only very limited data are available regarding the effect of combined GlcN and CS on humans. When administered alone, neither GlcN-HCl nor CS had any clinical effect during the GAIT study. However, the combination (GlcN-HCl 500 mg + CS 400 mg; three times a day) brought about pain relief and function improvement for OA patients with moderate to severe knee pain [24]. The limitations of the GAIT trial are well known, and make it difficult to determine whether this result is clinically meaningful.
Discussion
Glucosamine and chondroitin sulfate have a variety of in-vitro anti-inflammatory and anti-catabolic effects, although these have been obtained by using higher concentrations than those reached in humans [6, 7, 31, 32•]. These effects have led to the generation of hypotheses regarding potential mechanisms by which GS and CS might bring about symptom control and structure modification for OA patients.
The actions of these products involve multiple signaling intermediates: for example, they bring about their anti-inflammatory and anti-catabolic effect via inhibition of P38, AKT, and NF-κB. CS and GS also stimulate synthesis of proteoglycans, via a “building block” process. Interestingly, these compounds act on the three main articular tissues involved in OA physiopathology, i.e. cartilage, subchondral bone, and synovial membrane. CS and GS may counteract the deleterious crosstalk between these tissues and break the vicious circle that perpetuates OA.
These in-vitro data contribute to explaining the symptomatic and structural effects of GS and CS. Some meta-analyses have supported these beneficial effects, and the compounds are now recommended by EULAR and OARSI, two international organizations for scientists and health care professionals focused on the prevention and treatment of OA. These organizations also emphasized the importance of using pharmaceutical grade products: quality control requirements for prescribed drugs and OTC dietary supplements are not the same. Interestingly, most of the positive results were obtained from sponsored studies, but these were also the ones using pharmaceutical-grade products. In addition, doses and formulations should be adjusted to achieve sufficient concentration of treatment in plasma [1]. A recent pharmacokinetic study of both compounds (GlcN-HCl 500 mg three times a day, CS 400 mg three times a day), alone or in combination, for knee OA patients reported the compounds had low circulating levels after oral administration [45•]. It could be worth testing an improved formulation.
Conclusions
GlcN and CS have promising in-vitro properties and effects. The extent to which formulation of the products affects efficacy in vitro remains the subject of debate. Although symptomatic effect is well documented, the structure-modifying effect suggested by animal and human clinical trials should be confirmed by additional studies to establish their clinical efficacy beyond doubt. In addition, it might be worth further investigating use of GlcN and CS in combination. Finally, standardization of the outcome measures of clinical trials would assist data interpretation and enable rigorous comparisons.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Aghazadeh-Habashi A, Jamali F. The glucosamine controversy; a pharmacokinetic issue. J Pharm Pharm Sci. 2011;14(2):264–73.
Ali AA, Lewis SM, Badgley HL, et al. Oral glucosamine increases expression of transforming growth factor beta1 (TGFbeta1) and connective tissue growth factor (CTGF) mRNA in rat cartilage and kidney: implications for human efficacy and toxicity. Arch Biochem Biophys. 2011;510(1):11–8. doi:10.1016/j.abb.2011.03.014.
Baccarin RYA, Machado TSL, Lopes-Moraes AP, et al. Urinary glycosaminoglycans in horse osteoarthritis. Effects of chondroitin sulfate and glucosamine. Res Vet Sci. 2012;93(1):88–96. doi:10.1016/j.rvsc.2011.08.009.
Bassleer CT, Combal JP, Bougaret S, Malaise M. Effects of chondroitin sulfate and interleukin-1 beta on human articular chondrocytes cultivated in clusters. Osteoarthr Cartil. 1998;6(3):196–204. doi:10.1053/joca.1998.0112.
Bauerova K, Ponist S, Kuncirova V, et al. Chondroitin sulfate effect on induced arthritis in rats. Osteoarthr Cartil. 2011;19(11):1373–9. doi:10.1016/j.joca.2011.08.006.
Biggee BA, Blinn CM, McAlindon TE, et al. Low levels of human serum glucosamine after ingestion of glucosamine sulphate relative to capability for peripheral effectiveness. Ann Rheum Dis. 2006;65(2):222–6. doi:10.1136/ard.2005.036368.
Block JA, Oegema TR, Sandy JD, Plaas A. The effects of oral glucosamine on joint health: is a change in research approach needed? Osteoarthr Cartil. 2010;18(1):5–11. doi:10.1016/j.joca.2009.07.005.
Bruyere O, Burlet N, Delmas PD, et al. Evaluation of symptomatic slow-acting drugs in osteoarthritis using the GRADE system. BMC Musculoskelet Disord. 2008;9:165. doi:10.1186/1471-2474-9-165.
Bruyere O, Pavelka K, Rovati LC, et al. Total joint replacement after glucosamine sulphate treatment in knee osteoarthritis: results of a mean 8-year observation of patients from two previous 3-year, randomised, placebo-controlled trials. Osteoarthr Cartil. 2008;16(2):254–60. doi:10.1016/j.joca.2007.06.011.
• Calamia V, Fernández-Puente P, Mateos J et al. Pharmacoproteomic Study of Three Different Chondroitin Sulfate Compounds on Intracellular and Extracellular Human Chondrocyte Proteomes. Molecular & Cellular Proteomics. 2012;11(6). doi:10.1074/mcp.M111.013417. Relevant confirmation of the different effects of different CS formulations using state-of-the-art technology
•• Calamia V, Lourido L, Fernandez-Puente P, et al. Secretome analysis of chondroitin sulfate-treated chondrocytes reveals anti-angiogenic, anti-inflammatory and anti-catabolic properties. Arthritis Res Ther. 2012;14(5):R202. doi:10.1186/ar4040. Up-to-date report of the different effects of CS.
•• Calamia V, Ruiz-Romero C, Rocha B, et al. Pharmacoproteomic study of the effects of chondroitin and glucosamine sulfate on human articular chondrocytes. Arthritis Res Ther. 2010;12(4):R138. doi:10.1186/ar3077. Interesting approach with the latest technology providing additional data about mechanism of action of both GlcN and CS.
Campo GM, Avenoso A, Campo S, et al. Efficacy of treatment with glycosaminoglycans on experimental collagen-induced arthritis in rats. Arthritis Res Ther. 2003;5(3):R122–31.
Campo GM, Avenoso A, Campo S, et al. Antioxidant activity of chondroitin sulfate. Adv Pharmacol. 2006;53:417–31. doi:10.1016/S1054-3589(05)53020-5.
Campo GM, Avenoso A, Campo S, et al. Chondroitin sulphate: antioxidant properties and beneficial effects. Mini Rev Med Chem. 2006;6(12):1311–20.
Campo GM, Avenoso A, Campo S, et al. Chondroitin-4-sulphate inhibits NF-kB translocation and caspase activation in collagen-induced arthritis in mice. Osteoarthr Cartil. 2008;16(12):1474–83. doi:10.1016/j.joca.2008.04.002.
Campo GM, Avenoso A, Campo S, et al. Glycosaminoglycans modulate inflammation and apoptosis in LPS-treated chondrocytes. J Cell Biochem. 2009;106(1):83–92. doi:10.1002/jcb.21981.
Campo GM, Avenoso A, Campo S, et al. Glycosaminoglycans reduced inflammatory response by modulating toll-like receptor-4 in LPS-stimulated chondrocytes. Arch Biochem Biophys. 2009;491(1–2):7–15. doi:10.1016/j.abb.2009.09.017.
Chan PS, Caron JP, Orth MW. Effect of glucosamine and chondroitin sulfate on regulation of gene expression of proteolytic enzymes and their inhibitors in interleukin-1-challenged bovine articular cartilage explants. Am J Vet Res. 2005;66(11):1870–6.
Chan PS, Caron JP, Orth MW. Effects of glucosamine and chondroitin sulfate on bovine cartilage explants under long-term culture conditions. Am J Vet Res. 2007;68(7):709–15. doi:10.2460/ajvr.68.7.709.
• Chiusaroli R, Piepoli T, Zanelli T et al. Experimental pharmacology of glucosamine sulfate. Int J Rheumatol. 2011;2011:939265. doi:10.1155/2011/939265. Relevant results obtained with low doses of GlcN
Cho SY, Sim JS, Jeong CS, et al. Effects of low molecular weight chondroitin sulfate on type II collagen-induced arthritis in DBA/1J mice. Biol Pharm Bull. 2004;27(1):47–51.
Chou MM, Vergnolle N, McDougall JJ, et al. Effects of chondroitin and glucosamine sulfate in a dietary bar formulation on inflammation, interleukin-1beta, matrix metalloprotease-9, and cartilage damage in arthritis. Exp Biol Med (Maywood). 2005;230(4):255–62.
Clegg D, Reda D, Harris C, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006;354:795–808.
David-Raoudi M, Deschrevel B, Leclercq S, et al. Chondroitin sulfate increases hyaluronan production by human synoviocytes through differential regulation of hyaluronan synthases: Role of p38 and Akt. Arthritis Rheum. 2009;60(3):760–70. doi:10.1002/art.24302.
du Souich P, Garcia AG, Verges J, Montell E. Immunomodulatory and anti-inflammatory effects of chondroitin sulphate. J Cell Mol Med. 2009;13(8A):1451–63. doi:10.1111/j.1582-4934.2009.00826.x.
•• Gabay C, Medinger-Sadowski C, Gascon D, et al. Symptomatic effects of chondroitin 4 and chondroitin 6 sulfate on hand osteoarthritis: A randomized, double-blind, placebo-controlled clinical trial at a single center. Arthritis Rheum. 2011;63(11):3383–91. doi:10.1002/art.30574. One of the latest clinical trials of CS, documenting the effect of using a highly purified formulation.
Gupta RC, Canerdy TD, Skaggs P, et al. Therapeutic efficacy of undenatured type-II collagen (UC-II) in comparison to glucosamine and chondroitin in arthritic horses. J Vet Pharmacol Ther. 2009;32(6):577–84. doi:10.1111/j.1365-2885.2009.01079.x.
Henrotin YE. Interpretation of metaanalyses: pitfalls should be more widely recognized. J Rheumatol. 2012;39(6):1107–9. doi:10.3899/jrheum.111420.
Henrotin Y, Chevalier X, Herrero-Beaumont G, et al. Physiological effects of oral glucosamine on joint health: current status and consensus on future research priorities. BMC Res Notes. 2013;6:115. doi:10.1186/1756-0500-6-115.
Henrotin Y, Mathy M, Sanchez C, Lambert C. Chondroitin sulfate in the treatment of osteoarthritis: from in vitro studies to clinical recommendations. Ther Adv Musculoskelet Dis. 2010;2(6):335–48. doi:10.1177/1759720X10383076.
• Henrotin Y, Mobasheri A, Marty M. Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis? Arthritis Res Ther. 2012;14(1):201. doi:10.1186/ar3657. Interesting and comprehensive points of view about the different aspects of GlcN in OA.
Hochberg M. Structure-modifying effects of chondroitin sulfate in knee osteoarthritis: an updated meta-analysis of randomized placebo-controlled trials of 2-year duration. Osteoarthr Cartil. 2010;18 Suppl 1:S28–31.
Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465–74.
Hochberg M, Chevalier X, Henrotin Y, et al. Symptom and structure modification in osteoarthritis with pharmaceutical-grade chondroitin sulfate: what's the evidence? Curr Med Res Opin. 2013;29(3):259–67. doi:10.1185/03007995.2012.753430.
Hochberg MC, Zhan M, Langenberg P. The rate of decline of joint space width in patients with osteoarthritis of the knee: a systematic review and meta-analysis of randomized placebo-controlled trials of chondroitin sulfate. Curr Med Res Opin. 2008. doi:10.1185/03007990802434932.
Holzmann J, Brandl N, Zemann A, et al. Assorted effects of TGFbeta and chondroitinsulfate on p38 and ERK1/2 activation levels in human articular chondrocytes stimulated with LPS. Osteoarthr Cartil. 2006;14(6):519–25.
Hong H, Park YK, Choi MS, et al. Differential down-regulation of COX-2 and MMP-13 in human skin fibroblasts by glucosamine-hydrochloride. J Dermatol Sci. 2009;56(1):43–50. doi:10.1016/j.jdermsci.2009.06.017.
Hua J, Suguro S, Hirano S, et al. Preventive actions of a high dose of glucosamine on adjuvant arthritis in rats. Inflamm Res. 2005;54(3):127–32. doi:10.1007/s00011-004-1333-6.
Igarashi M, Kaga I, Takamori Y, et al. Effects of glucosamine derivatives and uronic acids on the production of glycosaminoglycans by human synovial cells and chondrocytes. Int J Mol Med. 2011;27(6):821–7. doi:10.3892/ijmm.2011.662.
Igarashi M, Sakamoto K, Nagaoka I. Effect of glucosamine, a therapeutic agent for osteoarthritis, on osteoblastic cell differentiation. Int J Mol Med. 2011;28(3):373–9. doi:10.3892/ijmm.2011.686.
Imada K, Oka H, Kawasaki D, et al. Anti-arthritic action mechanisms of natural chondroitin sulfate in human articular chondrocytes and synovial fibroblasts. Biol Pharm Bull. 2010;33(3):410–4.
Imagawa K, de Andres MC, Hashimoto K, et al. The epigenetic effect of glucosamine and a nuclear factor-kappa B (NF-kB) inhibitor on primary human chondrocytes–implications for osteoarthritis. Biochem Biophys Res Commun. 2011;405(3):362–7. doi:10.1016/j.bbrc.2011.01.007.
Ivanovska N, Dimitrova P. Bone resorption and remodeling in murine collagenase-induced osteoarthritis after administration of glucosamine. Arthritis Res Ther. 2011;13(2):R44. doi:10.1186/ar3283.
• Jackson CG, Plaas AH, Sandy JD, et al. The human pharmacokinetics of oral ingestion of glucosamine and chondroitin sulfate taken separately or in combination. Osteoarthr Cartil. 2010;18(3):297–302. doi:10.1016/j.joca.2009.10.013. Important information regarding the pharmacokinetics of both compounds.
Jomphe C, Gabriac M, Hale TM, et al. Chondroitin sulfate inhibits the nuclear translocation of nuclear factor-kappaB in interleukin-1beta-stimulated chondrocytes. Basic Clin Pharmacol Toxicol. 2008;102(1):59–65. doi:10.1111/j.1742-7843.2007.00158.x.
Jordan KM, Arden NK, Doherty M, et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62(12):1145–55.
Kahan A, Uebelhart D, De Vathaire F, et al. Long-term effects of chondroitins 4 and 6 sulfate on knee osteoarthritis: The study on osteoarthritis progression prevention, a two-year, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2009;60(2):524–33.
Kapoor M, Mineau F, Fahmi H, et al. Glucosamine sulfate reduces prostaglandin E(2) production in osteoarthritic chondrocytes through inhibition of microsomal PGE synthase-1. J Rheumatol. 2012;39(3):635–44. doi:10.3899/jrheum.110621.
Katta J, Jin Z, Ingham E, Fisher J. Chondroitin sulphate: an effective joint lubricant? Osteoarthr Cartil. 2009;17(8):1001–8. doi:10.1016/j.joca.2009.02.010.
Kim MM, Mendis E, Rajapakse N, Kim S-K. Glucosamine sulfate promotes osteoblastic differentiation of MG-63 cells via anti-inflammatory effect. Bioorg Med Chem Lett. 2007;17(7):1938–42. doi:10.1016/j.bmcl.2007.01.030.
Kobayashi T, Notoya K, Nakamura A, Akimoto K. Fursultiamine, a vitamin B1 derivative, enhances chondroprotective effects of glucosamine hydrochloride and chondroitin sulfate in rabbit experimental osteoarthritis. Inflamm Res. 2005;54(6):249–55. doi:10.1007/s00011-005-1351-z.
Lambert C, Mathy-Hartert M, Dubuc JE, et al. Characterization of synovial angiogenesis in osteoarthritis patients and its modulation by chondroitin sulfate. Arthritis Res Ther. 2012;14(2):R58. doi:10.1186/ar3771.
Largo R, Alvarez-Soria MA, Diez-Ortego I, et al. Glucosamine inhibits IL-1beta-induced NFkappaB activation in human osteoarthritic chondrocytes. Osteoarthr Cartil. 2003;11(4):290–8.
• Lee YH, Woo JH, Choi SJ, et al. Effect of glucosamine or chondroitin sulfate on the osteoarthritis progression: a meta-analysis. Rheumatol Int. 2010;30(3):357–63. doi:10.1007/s00296-009-0969-5. One of the latest meta-analyses.
Legendre F, Bauge C, Roche R, et al. Chondroitin sulfate modulation of matrix and inflammatory gene expression in IL-1beta-stimulated chondrocytes—study in hypoxic alginate bead cultures. Osteoarthr Cartil. 2008;16(1):105–14. doi:10.1016/j.joca.2007.05.020.
Lin YC, Liang YC, Sheu MT, et al. Chondroprotective effects of glucosamine involving the p38 MAPK and Akt signaling pathways. Rheumatol Int. 2008;28(10):1009–16. doi:10.1007/s00296-008-0561-4.
• Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697–707. doi:10.1002/art.34453. Latest statement of OA as a disease involving all the tissues of the joint.
McAlindon TE, LaValley MP, Gulin JP, Felson DT. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283(11):1469–75.
Mendis E, Kim M-M, Rajapakse N, Kim S-K. Suppression of cytokine production in lipopolysaccharide-stimulated mouse macrophages by novel cationic glucosamine derivative involves down-regulation of NF-[kappa]B and MAPK expressions. Bioorg Med Chem. 2008;16(18):8390–6. doi:10.1016/j.bmc.2008.08.037.
Mendis E, Kim MM, Rajapakse N, Kim SK. The inhibitory mechanism of a novel cationic glucosamine derivative against MMP-2 and MMP-9 expressions. Bioorg Med Chem Lett. 2009;19(10):2755–9. doi:10.1016/j.bmcl.2009.03.126.
Michel BA, Stucki G, Frey D, et al. Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Arthritis Rheum. 2005;52(3):779–86. doi:10.1002/art.20867.
Monfort J, Nacher M, Montell E, et al. Chondroitin sulfate and hyaluronic acid (500–730 kda) inhibit stromelysin-1 synthesis in human osteoarthritic chondrocytes. Drugs Exp Clin Res. 2005;31(2):71–6.
Naito K, Watari T, Furuhata A, et al. Evaluation of the effect of glucosamine on an experimental rat osteoarthritis model. Life Sci. 2010;86(13–14):538–43. doi:10.1016/j.lfs.2010.02.015.
Nakamura H, Shibakawa A, Tanaka M, et al. Effects of glucosamine hydrochloride on the production of prostaglandin E2, nitric oxide and metalloproteases by chondrocytes and synoviocytes in osteoarthritis. Clin Exp Rheumatol. 2004;22(3):293–9.
Oegema Jr TR, Deloria LB, Sandy JD, Hart DA. Effect of oral glucosamine on cartilage and meniscus in normal and chymopapain-injected knees of young rabbits. Arthritis Rheum. 2002;46(9):2495–503. doi:10.1002/art.10499.
Omata T, Itokazu Y, Inoue N, Segawa Y. Effects of chondroitin sulfate-C on articular cartilage destruction in murine collagen-induced arthritis. Arzneimittelforschung. 2000;50(2):148–53. doi:10.1055/s-0031-1300180.
Oryan A, Moshiri A, Meimandiparizi A-H. Effects of sodium-hyaluronate and glucosamine-chondroitin sulfate on remodeling stage of tenotomized superficial digital flexor tendon in rabbits: a clinical, histopathological, ultrastructural, and biomechanical study. Connect Tissue Res. 2011;52(4):329–39. doi:10.3109/03008207.2010.531332.
• Pecchi E, Priam S, Mladenovic Z, et al. A potential role of chondroitin sulfate on bone in osteoarthritis: inhibition of prostaglandin E2 and matrix metalloproteinases synthesis in interleukin-1β-stimulated osteoblasts. Osteoarthr Cartil. 2012;20(2):127–35. doi:10.1016/j.joca.2011.12.002. Recent data regarding the effect of CS on subchondral bone.
Poolsup N, Suthisisang C, Channark P, Kittikulsuth W. Glucosamine long-term treatment and the progression of knee osteoarthritis: systematic review of randomized controlled trials. Ann Pharmacother. 2005;39(6):1080–7. doi:10.1345/aph.1E576.
Rafi MM, Yadav PN, Rossi AO. Glucosamine inhibits LPS-induced COX-2 and iNOS expression in mouse macrophage cells (RAW 264.7) by inhibition of p38-MAP kinase and transcription factor NF-kappaB. Mol Nutr Food Res. 2007;51(5):587–93.
Rozendaal RM, Koes BW, van Osch GJ, et al. Effect of glucosamine sulfate on hip osteoarthritis: a randomized trial. Ann Intern Med. 2008;148(4):268–77.
Samuels J, Krasnokutsky S, Abramson SB. Osteoarthritis: a tale of three tissues. Bull NYU Hosp Jt Dis. 2008;66(3):244–50.
Tahiri K, Korwin-Zmijowska C, Richette P, et al. Natural chondroitin sulphates increase aggregation of proteoglycan complexes and decrease ADAMTS-5 expression in interleukin 1 beta-treated chondrocytes. Ann Rheum Dis. 2008;67(5):696–702. doi:10.1136/ard.2007.078600.
Taniguchi S, Ryu J, Seki M, et al. Long-term oral administration of glucosamine or chondroitin sulfate reduces destruction of cartilage and up-regulation of MMP-3 mRNA in a model of spontaneous osteoarthritis in Hartley guinea pigs. J Orthop Res. 2012;30(5):673–8. doi:10.1002/jor.22003.
Tat SK, Pelletier JP, Mineau F, et al. Variable effects of 3 different chondroitin sulfate compounds on human osteoarthritic cartilage/chondrocytes: relevance of purity and production process. J Rheumatol. 2010;37(3):656–64. doi:10.3899/jrheum.090696.
Tat SK, Pelletier JP, Vergés J, et al. Chondroitin and glucosamine sulfate in combination decrease the pro-resorptive properties of human osteoarthritis subchondral bone osteoblasts. Arthritis Res Ther. 2007;9:R117.
Tiraloche G, Girard C, Chouinard L, et al. Effect of oral glucosamine on cartilage degradation in a rabbit model of osteoarthritis. Arthritis Rheum. 2005;52(4):1118–28. doi:10.1002/art.20951.
Towheed TE, Maxwell L, Anastassiades TP et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2006(3):(online).
Uebelhart D, Malaise M, Marcolongo R, et al. Intermittent treatment of knee osteoarthritis with oral chondroitin sulfate: a one-year, randomized, double-blind, multicenter study versus placebo. Osteoarthr Cartil. 2004;12(4):269–76. doi:10.1016/j.joca.2004.01.004.
Vallieres M, du Souich P. Modulation of inflammation by chondroitin sulfate. Osteoarthr Cartil. 2010;18 Suppl 1:S1–6. doi:10.1016/j.joca.2010.02.017.
Vlad SC, LaValley MP, McAlindon TE, Felson DT. Glucosamine for pain in osteoarthritis: why do trial results differ? Arthritis Rheum. 2007;56(7):2267–77. doi:10.1002/art.22728.
Volpi N. Analytical aspects of pharmaceutical grade chondroitin sulfates. J Pharm Sci. 2007;96(12):3168–80. doi:10.1002/jps.20997.
Volpi N. Quality of different chondroitin sulfate preparations in relation to their therapeutic activity. J Pharm Pharmacol. 2009;61(10):1271–80. doi:10.1211/jpp/61.10.0002.
Volpi N. Anti-inflammatory activity of chondroitin sulphate: new functions from an old natural macromolecule. Inflammopharmacology. 2011;19(6):299–306. doi:10.1007/s10787-011-0098-0.
Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341:c4675.
Wang SX, Laverty S, Dumitriu M, et al. The effects of glucosamine hydrochloride on subchondral bone changes in an animal model of osteoarthritis. Arthritis Rheum. 2007;56(5):1537–48. doi:10.1002/art.22574.
Wang L, Wang J, Almqvist KF, et al. Influence of polysulphated polysaccharides and hydrocortisone on the extracellular matrix metabolism of human articular chondrocytes in vitro. Clin Exp Rheumatol. 2002;20(5):669–76.
Wen ZH, Tang CC, Chang YC, et al. Glucosamine sulfate reduces experimental osteoarthritis and nociception in rats: association with changes of mitogen-activated protein kinase in chondrocytes. Osteoarthr Cartil. 2010;18(9):1192–202. doi:10.1016/j.joca.2010.05.012.
Wieland HA, Michaelis M, Kirschbaum BJ, Rudolphi KA. Osteoarthritis—an untreatable disease? Nat Rev Drug Discov. 2005;4(4):331–44. doi:10.1038/nrd1693.
Wildi LM, Raynauld JP, Martel-Pelletier J, et al. Chondroitin sulphate reduces both cartilage volume loss and bone marrow lesions in knee osteoarthritis patients starting as early as 6 months after initiation of therapy: a randomised, double-blind, placebo-controlled pilot study using MRI. Ann Rheum Dis. 2011;70(6):982–9. doi:10.1136/ard.2010.140848.
Zegels B, Crozes P, Uebelhart D, et al. Equivalence of a single dose (1200 mg) compared with a three-time a day dose (400 mg) of chondroitin 4 and 6 sulfate in patients with knee osteoarthritis. Results of a randomized double blind placebo controlled study. Osteoarthr Cartil. 2013;21(1):22–7. doi:10.1016/j.joca.2012.09.017.
Zhang W, Doherty M, Arden N, et al. EULAR evidence based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2005;64(5):669–81. doi:10.1136/ard.2004.028886.
Zhang W, Doherty M, Leeb BF, et al. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2007;66(3):377–88. doi:10.1136/ard.2006.062091.
Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part I: Critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthr Cartil. 2007;15(9):981–1000.
Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008;16(2):137–62.
•• Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: Part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr Cartil. 2010;18(4):476–99. doi:10.1016/j.joca.2010.01.013. Update of effect size (ES) for both compounds, and comprehensive analysis.
Acknowledgments
The authors thank Dr Christelle Boileau for her assistance in preparing this manuscript.
Compliance with ethics guidelines
ᇵ
Conflict of interest
Yves Henrotin has served as a consultant for Tilman; has received grant support from Biolberica, Royal Canin, and Nestle; has received honoraria from IBSA, Artialis, and Synolyne; has held stock/stock options in Artialis and Synolyne; has received speaker fees from IBS and Biolberica; and has had travel/accommodation expenses covered/reimbursed by IBSA, Expanscience, and Biolberica.
Cécile Lambert has received grant support from Biolberica.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Complementary and Alternative Medicine
Rights and permissions
About this article
Cite this article
Henrotin, Y., Lambert, C. Chondroitin and Glucosamine in the Management of Osteoarthritis: An Update. Curr Rheumatol Rep 15, 361 (2013). https://doi.org/10.1007/s11926-013-0361-z
Published:
DOI: https://doi.org/10.1007/s11926-013-0361-z