Abstract
Chondroitin sulfate (CS) being a natural glycosaminoglycan is found in the cartilage and extracellular matrix. It shows clinical benefits in symptomatic osteoarthritis (OA) of the finger, knee, hip joints, low back, facial joints and other diseases due to its anti-inflammatory activity. It also helps in OA by providing resistance to compression, maintaining the structural integrity, homeostasis, slows breakdown and reduces pain in sore muscles. It is most often used in combination with glucosamine to treat OA. CS is a key role player in the regulation of cell development, cell adhesion, proliferation, and differentiation. Its commercial applications have been continuously explored in the engineering of biological tissues and its combination with other biopolymers to formulate scaffolds which promote and accelerate the regeneration of damaged structure. It is approved in the USA as a dietary supplement for OA, while it is used as a symptomatic slow-acting drug (SYSADOA) in Europe and some other countries. Any significant side effects or overdoses of CS have not been reported in clinical trials suggesting its long-term safety. This review highlights the potential of CS, either alone or in combination with other drugs, to attract the scientists engaged in OA treatment and management across the world.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
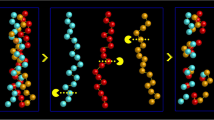
Chondroitin sulphate (CS) is a naturally occurring sulphated heteropolysaccharide. This sulfate is covalently attached to sugar composed of glucuronic acid (GlcA) and N-acetyl-galactosamine (GalNAc) as shown in Fig. 1. CS plays a significant role in biological processes as it is abundantly distributed in humans, other mammals and invertebrates [1]. CS is generally found in all mammalian connective tissues, especially in the cartilage, skin, blood vessels, ligaments, tendons [2], in axon terminals around neuronal cell bodies [3], brain and in the extracellular matrix (ECM) surrounding cells [4], where it constitutes an essential component of proteoglycans (PGs).
CS possesses negative charge which interacts readily with proteins in the extracellular matrix that helps in regulation of cellular activities [5]. CS is considered as the most widely used slow-acting drug for OA (SADOA) [6, 7], which was officially accepted by the WHO/ILAR Task Force in 1994. The main reasons for the use of the CS as SYSADOA therapeutic class are:
-
i.
The ability of CS to slow down the development of OA has been demonstrated in several clinical trials with significant positive effects [8, 9]. CS enables to decrease the dosage of others treatment such as NSAIDs and shows better gastrointestinal (GI) tolerability by limiting the significant risks of upper GI tract erosions, ulcers with bleeding and/or deleterious renal effects in elderly patients [10, 11].
-
ii.
On biochemical basis, the effect of CS in patients with OA is due to reactions involved in its anti-inflammatory activity, stimulation of the synthesis of proteoglycans and hyaluronic acid, and the decrease in catabolic activity of chondrocytes inhibiting the synthesis of proteolytic enzymes, nitric oxide, and other substances that contribute to damage cartilage matrix and cause death of articular chondrocytes [12].
-
iii.
CS in most of the cases shows a remnant effect for few months, a feature which is never observed with analgesics and NSAIDs, substances which need to be continuously administered in order to provide relief from pain and increased mobility in OA patients [13].
-
iv.
CS plays a role in forming new bones, cartilage and tendons, and maintains structural integrity of tissues as well as repair damage [14].
-
v.
From diagnostic point, antibody specific for a chondroitin sulphate epitope is useful in diagnosis and treatment of connective tissue diseases, such as arthritis and sarcomas [15].
-
vi.
CS provides specific biological functions in cell adhesion, morphogenesis, neural network formation, and cell division [1].
-
vii.
Chondroitin is also used in veterinary medicine [16].
Physicochemical and structural properties
CS is a mucopolysaccharide of high viscosity. Physically, it is a clear or slightly hazy or faintly yellow compound depending on its source. It is soluble in water (100 mg/ml), and has a molecular weight of 50,000 to 100,000 Da [17]. The low molecular weight form has a potentially superior absorption rate to that of high molecular weight CS [18]. Chemically, Chondroitin sulphate comprises a repeating disaccharide motif with sulphate groups, which is modified or catalyzed by sulfo-transferases, replacing one, or more, of the -OH groups on C4 and C6 of GalNAc and C2 and C3 of GlcA [19]. Various modifications can generate different isomers forms. Example: CS with four sulphates per disaccharide unit helps in production of anaphylactic mediators, including C3a and C5a as well as in activation of contact system. Monoclonal antibodies (mAb) were generated and characterized for recognition of sulphate motifs and epitopes in CS [20].
Sources
Commercially, CS is mainly derived from cow trachea, pig ear and nasal septa [21] but other sources include chicken keel [22], shark cartilage [23], and fish [24]. CS derived from fish (Ray and shark) is referred as a better source than that of mammalian because of its sulfation pattern and safety [25]. CS chain size varies among various sources e.g. tracheal CS is 20–25 kDa, while shark CS is 50–80 kDa [26]. The CS employed in scientific studies is mainly obtained from bovine, porcine, chicken, or marine cartilage. From these, bovine CS is most often used in vitro and in clinical trials [27]. The sources and structures of CS impact on its functions, quality, effectiveness, percentage yield (~50–100 %) and identity e.g. CS (porcine, purity 90.4 %), induces the activation of inflammatory and catabolic pathways, whereas CS (bovine, purity 96.2 % and 99.9 %) induce an anti-inflammatory and anabolic response [28]. This is illustrated in Fig. 2 [29].
Production
The industrial production of chondroitin sulphate (CS) uses animal tissue sources as raw materials. CS is extracted with long and complex procedures that start with the recovery of CS from the cartilaginous tissues and continue with numerous steps of purifications for the complete removal of all the contaminants. In general, the methods of CS isolation from cartilage [30–32] include various steps based on: (1) chemical hydrolysis of cartilage using high concentrations of NaOH, urea and guanidine HCl; (2) breakdown of proteoglycan core; (3) elimination of proteins by trichloroacetic acid and CS recovery; (4) purification of CS with gel filtration and/or ion-exchange and size-exclusion chromatography. Recently, a two-step enzymatic processing with alcalase and flavourzyme showed better yields of degradation with a significant reduction of time-processing [33]. Various types of other enzymes are also involved in biosynthesis of CS affecting its metabolism, involved in differentiation, cellular proliferation, development, regeneration and repair in the disease. Two different biotechnological approaches have been investigated for CS production. In the first case CS is obtained enzymatically by in vitro chain elongation using UDP-sugar precursors and biotechnologically produced synthase enzymes. UDP-glucose oxidized into UDP-glucuronic acid which promotes chondrogenesis and GAGs synthesis monosaccharides precursors help in boosting chondroitin-like capsular polysaccharide production [34, 35], a hetero-oligomer complex of CS synthase-1 (CSS1)/chondroitin synthase-1 and CS synthase-2 (CSS2)/chondroitin polymerizing factor with the strongest polymerizing activity participate in the extension and initiation of CS [1]. In the other case CS is produced by using a biotechnological-chemical strategy consisting of three main steps: fermentative production of a chondroitin-like polysaccharide by capsulated bacteria, purification from the fermentation broth and then site specific chain sulphation. From a production point of view, biotechnological approaches could be designed to obtain structural tailored cut molecules [36]. CS analysis has been reported by different techniques from various sources as listed below in Table 1.
Pharmacokinetics considerations
Pharmacokinetic studies showed that CS can be absorbed orally but absorption depends upon molecular mass (10 % as high–molecular-weight and 90 % as low-molecular-weight compounds) and charge density, its bioavailability ranges from 15 % to 24 %. Intestinal absorption of low molecular weight CS is enhanced by conjugating it with α-linolenic acid as it opens the intercellular tight junctions rather than disrupting the overall integrity of the monolayer [42]. Absorbed labeled CS found in high content in synovial fluid and cartilage [43]. Orally ingested CS affects pain due to changes in the cellular activities in the gut lining or in the liver, not by dosing and higher circulating concentrations of CS [41]. CS’s onset of action is slower but efficacy is equivalent to non-steroidal anti-inflammatory agents (NSAIDs). The Cmax (peak plasma concentration) of CS cannot be calculated due to its rapid degradation to lower molecular weight compounds as well as the difficulty in differentiating it from endogenous molecules. In mammals, the major site of metabolism is liver where it is hydrolyzed into monosaccharides by lyase and bacteroides thetaiotaomicron, a gram-negative anaerobe found in human colons but not by cytochrome P450. Smaller amounts of di-, oligo-, and polysaccharides survive intact throughout the digestive process. Analysis shows that uptake of desulphated chondroitin occurred very sharply (peak level after, 15 min) followed by rapid clearance and return to baseline after 3 h [44]. For tracheal CS, peak plasma level reaches within 1–5 h while, in shark after 8.7 h. CS up to single dosage of 3000 mg shows first-order kinetics [45] which is not altered even by multiple doses of 800 mg in OA patients. CS in urine is of lower molecular weight, with lower sulfate content, and is attached to proteins smaller than found in tissues.
Toxicity
Clinical studies of commercial CS show that it is well tolerated with no side effects of over dosages, and without any drug-drug interactions. It has rare adverse reactions which suggests its long term safety [46]. Its safety is confirmed by The European League Against Rheumatism (EULAR) committee, by giving it 6 points on a level of toxicity scale from 0 to 100, proving it to be one of the safest drugs for osteoarthritis [18]. However, mild side effects such as nausea, stomach upset, diarrhea or constipation, indigestion, stomach pain, intraocular hypertension (when used in eye) and heart burn are reported in some literature. For instance, in chronic liver disease, sometimes hepatotoxicity is observed, which leads to hepatitis [47, 48]. As chondroitin supplements usually contain glucosamine, diabetics should take extreme caution when taking this supplement. There are no known interactions with foods, herbs and supplements. Some contraindications for CS usage include: (1) Pregnancy or breast-feeding condition, (2) Having asthma, (3) Allergic to shellfish, (4) Having prostate cancer or an increased risk for prostate cancer, (5) Taking blood thinning medications, because chondroitin is a natural anticoagulant [49, 50].
Dose and dosage forms
CS can be taken in the form of pill, tablet, capsule, powder, or liquid and also administered by injection. It is used in creams, eye drops, cosmetics and medical applications. It is also available as plain or in combination with various forms of glucosamine. CS can be taken irrespective of food intake. Dose for arthritis and osteoarthritis relief is about 1200 to 1600 mg per day divided in two or three doses, for a span of about two months or so depending upon individual needs. Single dose of 1200 mg is equivalent to 3 times a day (400 mg) dose [51].
Chondroitin sulphate and osteoarthritis
The main factor causing the inflammation of the OA is the activation of nuclear factor-κB (NF-κB). CS is able to diminish NF-κB activation and nuclear translocation in chondrocytes and synovial membrane [52].
Mechanism of inflammation in OA
Broadly two types of patterns are observed in OA inflammation: first is Danger/damaged associated molecular pattern (DAMPs) [53], and the other one is pathogen-associated molecular patterns (PAMPs) which includes bacteria, viruses and fungi. DAMPs stimulate immune system, via pattern recognition receptors (PRRs) to either combat infection or initiate repair process, by inducing innate immunity or host immune responses. PRRs are composed of several families of receptors including cell surface, endosomal and cytosolic receptors e.g. in vitro. Toll like receptors (TLRs). DAMPs include various types of pattern, which cause inflammation in OA are listed below:
-
(a)
Plasma protein damage associated molecular patterns: After joint injury and damage, vascular leak and exudation from site of tissue damage occurs [54] the proteomic survey of OA observed increased level of many plasma proteins e.g. in vitro. Fibrinogen [55] in the synovial fluid which helps in production of various inflammatory cytokines and growth factors including TNFα, IL-6,IL-1β and vascular endothelial growth factors (VEGF) that further propagates the intra-articular inflammatory responses and cartilage breakdown [54].
-
(b)
Intracellular alarmins: Intracellular proteins released from stressed, damaged or necrotic cells, sequestered within cell, can signal to immune system [56] e.g. High mobility group box1 protein (HMGB-1) [57] and S-100 family of proteins (S100 A8 & S100 A9 in synovium) [58, 59]. These proteins upregulate catabolic mediators including MMPs 1, 3, 9 & 13 as well as cytokines IL-6 and concomitant down-regulation of aggrecan and type-2 collagen [60].
-
(c)
Crystals of calcium, damage associated molecular patterns: In OA patients synovial fluids and tissues crystals like basic calcium phosphate (BCP) and calcium pyrophosphate dehydrate (CPPD) are observed. These crystals contribute in OA associated inflammation as CPPD induces chondrocyte production of nitric oxide with the help of TLRs [61] and IL-1β, IL-18 mediated by NLRP3 [62], by CPPD and BCP [63]. Uric acid level in synovial fluid contributes to inflammatory processes and cartilage degradation in OA [64].
-
(d)
Cellular mediators: Joint cells e.g. Fibroblast like syoviocytes (FLS) acts as intermediate mediators of local inflammation by producing TNFα, IL-1β, MMPs and Cartilage degradation and chondrocytes by upregulation of TLRs [65].
-
(i)
Complement in OA: In OA, synovium upregulation of complement effector genes and down regulation of complement inhibitors was also observed relative to normal controls [66].
-
(ii)
Mechanical stress induced immune activation: It directly induces production of inflammatory mediators from cartilage and synovium [67].
-
(iii)
Soluble inflammatory mediators in OA: In serum and synovial fluid, the increased level of cytokines includes IL-6, IL-8 [68] and IL-15(in early knee OA) [68] as well as prostaglandins, leukotrienes mediates inflammation. The enzyme cyclooxegenase-2 (COX-2) is upregulated in inflamed joint tissues leads to elevated production of prostaglandins such as PGE2 in the joint [69].
Following joint trauma or overuse, tissue damage results in the production of damage associated molecular patterns (DAMPs), including cartilage extracellular matrix (ECM) including fibronectin [70], hyaluronan [71], known & novel plasma DAMPs, and intracellular alarmins that signal through pattern recognition receptors on synovial macrophages, fibroblast-like synoviocytes (FLS) and chondrocytes to induce the local production of inflammatory mediator which further leads to chondrolysis and release of additional ECM breakdown products e.g. Tenascin C [72, 73] and hyaluronic acid [74]. Fibronectin fragments include the production of proinflammatory cytokines including Tumor necrosis factor (TNF α) and IL-1β as well as matrix metallo-proteinase MMP1 & MMP3 [75]. Inflammation-induced angiogenesis and increased vascular permeability result in the subsequent influx of plasma proteins, which is also capable of functioning as DAMPs. Acute and chronic production of inflammatory mediators promote further cartilage degradation either directly or indirectly through their induction of proteolytic enzymes, amplifying a vicious cycle of innate immune activation of osteoarthritis. Chondrocytes from OA cartilage display high levels of IL-1α and IL-1β and have elevated expression of the plasma membrane-bound IL-1 receptor I, while the decoy IL-1 receptor II is down-regulated in OA chondrocytes. Blood-borne neutrophils and monocytes migrate to the site by chemotaxis and pass through endothelial cells by extravasation, causes edema (swelling). Mast cells and macrophages by releasing histamine, leukotrienes, and prostaglandins by vasodilation increase vascular permeability. Neutrophils create a cytotoxic environment by a process called degranulation, releases toxic chemicals highly reactive oxygen and nitrogen species (ROS and RNS, respectively) [76] and various proteinases. These substances are destructive to both pathogens and hosts. Collective effects of all these lead to symptoms like heat, swelling, redness, pain and loss of function. CS glycosyltransferases gene expression lowered, which may reduce CS chain length and contribute to OA [77]. Figure 3 shows schematic representation of chronic inflammation as a mediator of OA [78].
Chondroitin sulphate and its receptors
CS shows its therapeutic efficiency by the involvement of various receptors as it is widely distributed in the tissues as shown in Table 2.
Anti-inflammatory activity of CS in OA
CS directly and/or indirectly modulates anti-inflammatory effects. CS being a large molecule cannot penetrate chondrocytes so it is internalized as oligosaccharide or disaccharide by engaging membrane receptors [e.g. CD44, RHAMM and intercellular adhesion molecule 1 (ICAM1)]. By engaging CD44 and ICAM1, it may promote the release of IL-1 receptor associated kinase-M (IRAK-M), an inhibitor of IRAK, or the release of MKP-1, that will dephosphorylate MAPK. These effects will reduce the nuclear translocation of NF-κB and the inflammatory reaction. In addition, CS engages integrins and increases TGF-β1 expression that will foster the synthesis of high molecular weight hyaluronic acid (HMW-HA) and of collagen II. HMW-HA binds to CD44, TLR4 and ICAM1 and impedes the binding of ECM fragments or LPS. Finally, CS diminishes the proteolysis of kininogen to bradykinin (BK) and induces the desentization and internalization of B2R, thus blocks the signal transduction pathway [83]. It acts directly by decreasing the presence of several complement components (CFAB, C1S, CO3, and C1R) and indirectly by increasing proteins such as TNFα-induced protein (TSG6) thereby lowering the pro-matrix metalloproteinase activation (observed in MMP1 and MMP3 levels). It also brings a strong CS dependent increase of an angiogenesis inhibitor and thrombospondin-1 (TSP1) that demonstrates the anti-angiogenic action of CS (Fig. 4) [28].
Mechanism of anti-inflammatory activity of CS with specific inflammatory pathways in different types of cells of OA. [Cell surface glycoprotein cluster designation 44(CD44), Receptor for hyaluronan mediated motility (RHAMM), Intercellular adhesion molecule 1(ICAM1), Toll-like Receptor-4 (TLR4), Bradykinin receptor (B2R), Interleukin-1 receptor (IL-1R1), Mylenoid differentiation primary response gene88 (MyD88), Interleukin receptor associated kinase (IRAK), Inhibitor of IRAK(IRAK-M), TNF receptor associated factor-6(TRAF-6), Mitogen activated protein kinase (MAPK), MAPK-phosphatase 1(MKP-1), Response element, specific sequences of DNA (RE), Activator protein-1(AP-1),Transforming growth factor β (TGF-β), HA synthase-2(HAS2), Hyaluronidase (Hyal ), Aggrecanases(ADAMTS),cyclooxygenase2 (COX-2), Interleukin-1 (IL-1), Phospholipase A2 (LPA2), Matrix metalloproteinases (MMPs), Tumor necrosis factor α(TNF-α), Prostaglandin E2 (PGE2), Monosulfated disaccharides of CS, sulphated in position 4 (ΔDi-4S)]
CS’s structure-modifying role in OA
CS is a basic component of cartilage and synovial fluid, which stimulates the anabolic process of the cartilage metabolism by increasing type II collagen and proteoglycan synthesis. Loss of CS from the cartilage leads to osteochondral angiogenesis, which is a major cause of OA [84]. CS as SYSADOA, in the osteoarthritis (OA) repairs at 3 levels:
-
(a)
Articular cartilage : Mechanically articular cartilage is tightly packed and its highly negatively charged sulfate groups have the ability to bind water and cations (Na+) to form a resilient layer to generate electrostatic repulsion that provides much of the resistance of cartilage to compression leads to its elasticity. In its anti-inflammatory actions it reduces pro-inflammatory factors, proteases and improves the anabolic/catabolic balance of the extracellular cartilage matrix (ECM) [85], also reduces the cartilage volume loss [86], decreases the synovial histopathological lesions [87], pain reduction and declination of joint space [88], delay many inflammation-induced catabolic processes in the cartilage [89], reduces the matrix metalloproteases (MMP), key proteases that are specifically related to articular tissues, including MMP-3, MMP-9, MMP-13, and MT1-MMP or MMP-14 [90] CS can impact processes associated with cartilage degeneration; induces the production of proteoglycans by the expression vector for the glycosyltransferase β-1,3-glucuronosyltransferase-I (GlcAT-I) promotion [91], inhibiting elastase and cathepsin G activity [92], reducing gene expression for a range of proteolytic enzymes [93]. The uptake studies indicate that (99 m)Tc-CS accumulates in articular cartilage and prove its chondrotropic effects [94]. CS protects against hydrogen peroxide formation and superoxide anions [95]. It also prevents the atherosclerosis (AT) lesions in the treatment of OA [96].
-
(b)
Synovial membrane : CS inhibits some inflammatory markers of synovitis, including cell infiltration, fibrosis and proliferation of the synovial lining cells [74]. As CS is able to modulate the function of synovial fibroblasts as well as that of chondrocytes. Therefore, it is promising a multifunctional chondroprotective material for OA.
Subchondral bone
In the sub-chondral bone, resorption and bone formation, tightly regulated by a molecular triad composed of osteoprotegerin (OPG)/receptor activator of NF-κB (RANK)/RANK ligand (RANKL). The RANKL (localized on osteoblasts) and its receptor RANK (localized on osteoclasts), enhances osteoclastogenesis, whereas OPG (produced by osteoblasts) inhibits this osteoclastogenesis by binding to RANKL. The ratio of OPG to RANKL pay a key role in regulating bone metabolism: a high ratio promotes bone formation, while a low ratio favors bone resorption. CS or combination of CS and glucosamine controls over it and decreases the resorption activity [93].
Novel drug delivery systems of CS
Polysaccharide based novel drug delivery systems have emerged with great success [97–99]. Over the past few years, plethora of novel drug delivery systems based on CS came into existence either as a ligand or a drug. Various combinations of CS have been reported for the treatment of OA such as CS4 and CS6 [100, 101] with glucosamine [85], or glucosamine and antioxidant micronutrients [102], or hyaluronic acid [103], or derivatives of quercetin [104], or diet supplements such as glucosamine, antioxidants and green-lipped mussel [105], GLU,/CS with eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and green-lipped mussel extract [106], or avocado soybean un-saponifiable [107, 108], or diacerein, and glucosamine sulphate [109, 110], or lucosamine and hyaluronic acid [111], or Structum® group [112]. Table 3 summarizes reported CS based drug delivery systems.
Clinical studies, patent status, and regulatory aspects
To evaluate the benefit and harm of oral CS for treating OA compared with placebo or a comparator oral medication, various clinical studies have been carried out. The outcome of all such studies concluded that CS improves pain (Knee pain) and quality of life (by Lequesne’s index), slows down the narrowing of joint space (X-rays study), and has no significant adverse and withdrawal effects [128]. Some specific clinical trials evidenced that CS acts as SMOAD (structure-modifying drug in OA) or SYSADOA (Symptomatic slow-acting drugs for the treatment of OA) and supports above remarks. For instance: (a) Michel et al. (2005) reported joint space narrowing [8]; (b) Uebelhart et al. (2004) with the help of Lequesne’s AFI, VAS, and walking time parameters proved SMOAD effects of CS in knee with OA [129]; (c) Mazieres et al. (2001) also supported SYSADOA effects of CS (oral delivery) for the treatment of knee OA [130].
Couple of patents has been acquired on CS based applications in OA as described under this section (Table 4).
CS is prescribed or used as an over-the-counter (OTC) drug in 22 countries and it is regulated as SYSADOA in Europe. United States Pharmacopoeia (USP) testing standards also exist for the identification and quantification of chondroitin. In the USA, it is referred to as a dietary supplement so there are no mandatory standards for formulations while in Europe it is approved as a drug or reference product and demands efficiency and safety approval at clinical outsets [128].
Conclusion and future perspectives
This review article enlightens about CS with its various parameters including structure, sequence and size have impact on function, understanding how CS is taken up and exerts an influence on biological processes. It is an important structural component in connective tissues and cartilage, (GAGs), which are primarily located on the surface of cells or in the extracellular matrix. CS is able to block the signal transduction pathways activated by the fragments of the extracellular matrix which diminish the nuclear translocation of proinflammatory transcription factors in chondrocytes and synovial membrane. This explains the benefits of CS in osteoarthritis. However, there are unanswered questions for the scientists viz.
-
What is relevance of CS’s level in chondrocytes to cause OA in humans?
-
Is CS better active as a ligand or a drug?
-
Does blocking signal transduction in inflammatory process of chondrocytes the only approach to target OA?
So far, a list of documents based on CS in osteoarthritis has been reported but the research arena in the field of OA treatment is still unsatisfactory because of lack of reliable and quantifiable biomarkers that can be utilized as a prognostic tool for OA because they are not specific to disease stage, cartilage or the affected joints [134]. Therefore, it is the need of time to improve OA outcomes in clinical trials.
References
Ogawa H., Hatano S., Sugiura N., Nagai N., Sato T., Shimizu K., Kimata K., Narimatsu H., Watanabe H.: Chondroitin sulfate synthase-2 is necessary for chain extension of chondroitin sulfate but not critical for skeletal development. PLoS One. 7(8), e43806 (2012)
Zhang G., Ezura Y., Chervoneva I., Robinson P.S., Beason D.P., Carine E.T., Soslowsky L.J., Iozzo R.V., Birk D.E.: Decorin regulates assembly of collagen fibrils and acquisition of biomechanical properties during tendon development. J. Cell. Biochem. 98(6), 1436–1449 (2006)
Atoji Y., Yamamoto Y., Suzuki Y.: The presence of chondroitin sulfate A and C within axon terminals in the Superior olivary nuclei of the adult dog. Neurosci. Lett. 189(1), 39–42 (1995)
Raspanti M., Congiu T., Guizzardi S.: Structural aspects of the extracellular matrix of the tendon: an atomic force and scanning electron microscopy study. Arch. Histol. Cytol. 65(1), 37–43 (2002)
Silbert J.E., Sugumaran G.: Biosynthesis of chondroitin/dermatan sulfate. IUBMB life. 54(4), 177–186 (2002)
Kubový P., Mensikova L., Kůrková E., Lopot F., Hojka V., Jelen K.: Influence of SYSADOA group chemicals on progression of human knee joint osteoarthritis: new objective evaluation method-measuring of rheological properties in vivo. Neuro endocrinology letters. 33(6), 651–659 (2011)
Schneider H., Maheu E., Cucherat M.: Symptom-modifying effect of chondroitin sulfate in knee osteoarthritis: a meta-analysis of randomized placebo-controlled trials performed with Structum®. The open rheumatology journal. 6, 183 (2012)
Michel B.A., Stucki G., Frey D., De Vathaire F., Vignon E., Bruehlmann P., Uebelhart D.: Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Arthritis Rheum. 52(3), 779–786 (2005). doi:10.1002/art.20867
Volpi N.: Analytical aspects of pharmaceutical grade chondroitin sulfates. J. Pharm. Sci. 96(12), 3168–3180 (2007)
Rubio-Terrés C.: An economic evaluation of chondroitin sulfate and non-steroidal anti-inflammatory drugs for the treatment of osteoarthritis. Data from the VECTRA study. Reumatología Clínica. English Edition 6(4), 187–195 (2010)
Aubry-Rozier B.: [Role of slow-acting anti-arthritic agents in osteoarthritis (chondroitin sulfate, glucosamine, hyaluronic acid)]. Revue medicale suisse. 8(332), 571–572 (2012)574, 576
Monfort J., Pelletier J.-P., Garcia-Giralt N., Martel-Pelletier J.: Biochemical basis of the effect of chondroitin sulphate on osteoarthritis articular tissues. Ann. Rheum. Dis. 67(6), 735–740 (2008)
Uebelhart D.: Clinical review of chondroitin sulfate in osteoarthritis. Osteoarthritis and cartilage/OARS, Osteoarthritis Research Society. 16(Suppl 3), S19–S21 (2008). doi:10.1016/j.joca.2008.06.006
Schiraldi C., Cimini D., De Rosa M.: Production of chondroitin sulfate and chondroitin. Appl. Microbiol. Biotechnol. 87(4), 1209–1220 (2010)
Caterson B., Mahmoodian F., Sorrell J.M., Hardingham T., Bayliss M., Carney S., Ratcliffe A., Muir H.: Modulation of native chondroitin sulphate structure in tissue development and in disease. J. Cell Sci. 97(3), 411–417 (1990)
Oryan, A., Moshiri, A., Meimandi-Parizi, A.-H.: Short and long terms healing of the experimentally transverse sectioned tendon in rabbits. BMC Sports Science, Medicine and Rehabilitation 4(1), 14 (2012).
Bobula T., Buffa R., Procházková P., Vágnerová H., Moravcová V., Šuláková R., Židek O., Velebný V.: One-pot synthesis of α, β-unsaturated polyaldehyde of chondroitin sulfate. Carbohydr. Polym. 136, 1002–1009 (2016)
Adebowale A.O., Cox D.S., Liang Z., Eddington N.D.: Analysis of glucosamine and chondroitin sulfate content in marketed products and the Caco-2 permeability of chondroitin sulfate raw materials. J Am Nutraceutical Assoc. 3(1), 37–44 (2000)
Kinoshita-Toyoda A., Yamada S., Haslam S.M., Khoo K.H., Sugiura M., Morris H.R., Dell A., Sugahara K.: Structural determination of five novel tetrasaccharides containing 3-O-sulfated D-glucuronic acid and two rare oligosaccharides containing a beta-D-glucose branch isolated from squid cartilage chondroitin sulfate E. Biochemistry. 43(34), 11063–11074 (2004). doi:10.1021/bi049622d
Caterson B.: Fell-Muir Lecture: chondroitin sulphate glycosaminoglycans: fun for some and confusion for others. Int. J. Exp. Pathol. 93(1), 1–10 (2012)
Nakano T., Ikawa N., Ozimek L.: An economical method to extract chondroitin sulphate-peptide from bovine nasal cartilage. Can. Agric. Eng. 42(4), 205–208 (2000)
Luo X., Fosmire G., Leach R.: Chicken keel cartilage as a source of chondroitin sulfate. Poult. Sci. 81(7), 1086–1089 (2002)
Nandini C.D., Itoh N., Sugahara K.: Novel 70-kDa chondroitin sulfate/dermatan sulfate hybrid chains with a unique heterogenous sulfation pattern from shark skin, which exhibit neuritogenic activity and binding activities for growth factors and neurotrophic factors. J. Biol. Chem. 280(6), 4058–4069 (2005)
Lignot B., Lahogue V., Bourseau P.: Enzymatic extraction of chondroitin sulfate from skate cartilage and concentration-desalting by ultrafiltration. J. Biotechnol. 103(3), 281–284 (2003)
Vázquez J.A., Rodríguez-Amado I., Montemayor M.I., Fraguas J., González M.D.P., Murado M.A.: Chondroitin sulfate, hyaluronic acid and chitin/chitosan production using marine waste sources: Characteristics, applications and eco-friendly processes: A review. Marine drugs. 11(3), 747–774 (2013)
Lauder R.M.: Chondroitin sulphate: a complex molecule with potential impacts on a wide range of biological systems. Complementary therapies in medicine. 17(1), 56–62 (2009)
Tat S.K., Pelletier J.-P., Mineau F., Duval N., Martel-Pelletier J.: Variable effects of 3 different chondroitin sulfate compounds on human osteoarthritic cartilage/chondrocytes: relevance of purity and production process. J. Rheumatol. 37(3), 656–664 (2010)
Calamia V., Lourido L., Fernández-Puente P., Mateos J., Rocha B., Montell E., Vergés J., Ruiz-Romero C., Blanco F.J.: Secretome analysis of chondroitin sulfate-treated chondrocytes reveals anti-angiogenic, anti-inflammatory and anti-catabolic properties. Arthritis research & therapy. 14(5), R202 (2012)
Guerrini M., Beccati D., Shriver Z., Naggi A., Viswanathan K., Bisio A., Capila I., Lansing J.C., Guglieri S., Fraser B.: Oversulfated chondroitin sulfate is a contaminant in heparin associated with adverse clinical events. Nat. Biotechnol. 26(6), 669–675 (2008)
Bollet A.J., Nance J.L.: Biochemical findings in normal and osteoarthritic articular cartilage. II. Chondroitin sulfate concentration and chain length, water, and ash content. Journal of Clinical Investigation. 45(7), 1170 (1966)
Hascall V.C., Calabro A., Midura R.J., Yanagishita M.: Isolation and characterization of proteoglycans. Methods Enzymol. 230, 390–417 (1993)
Rodén L., Baker J.R., Cifonelli J.A., Mathews M.B.: [7] isolation and characterization of connective tissue polysaccharides. Methods Enzymol. 28, 73–140 (1972)
Kim S.B., Ji C.I., Woo J.W., Do J.R., Cho S.M., Lee Y.B., Kang S.N., Park J.H.: Simplified purification of chondroitin sulphate from scapular cartilage of shortfin mako shark (Isurus oxyrinchus). International Journal of Food Science & Technology. 47(1), 91–99 (2012)
Bedini E., De Castro C., De Rosa M., Di Nola A., Restaino O.F., Schiraldi C., Parrilli M.: Semi-Synthesis of Unusual chondroitin sulfate polysaccharides containing GlcA (3-O-sulfate) or GlcA (2, 3-di-O-sulfate) Units. Chemistry-A European Journal. 18(7), 2123–2130 (2012)
Restaino O.F., di Lauro I., Cimini D., Carlino E., De Rosa M., Schiraldi C.: Monosaccharide precursors for boosting chondroitin-like capsular polysaccharide production. Appl. Microbiol. Biotechnol. 97(4), 1699–1709 (2013)
Pomin V.H.: Chondroitin sulfate: Structure, uses and health implications. Nova Science Publishers, Incorporated, Hauppauge (2013)
Liu X., Sun C., Zang H., Wang W., Guo R., Wang F.: Capillary electrophoresis for simultaneous analysis of heparin, chondroitin sulfate and hyaluronic acid and its application in preparations and synovial fluid. J. Chromatogr. Sci. 50(5), 373–379 (2012)
Bielik A.M., Zaia J.: Extraction of chondroitin/dermatan sulfate glycosaminoglycans from connective tissue for mass spectrometric analysis. Methods in molecular biology (Clifton, N.J.). 600, 215–225 (2010). doi:10.1007/978-1-60761-454-8_15
David J., Roman M., Zhou J., Hildreth J.: Determination of chondroitin sulfate content in raw materials and dietary supplements by high-performance liquid chromatography with ultraviolet detection after enzymatic hydrolysis: Single-laboratory validation. J. AOAC Int. 90(3), 659 (2007)
Solakyildirim K., Zhang Z., Linhardt R.J.: Ultraperformance liquid chromatography with electrospray ionization ion trap mass spectrometry for chondroitin disaccharide analysis. Anal. Biochem. 397(1), 24–28 (2010)
Jackson C.G., Plaas A.H., Sandy J.D., Hua C., Kim-Rolands S., Barnhill J.G., Harris C.L., Clegg D.O.: The human pharmacokinetics of oral ingestion of glucosamine and chondroitin sulfate taken separately or in combination. Osteoarthr. Cartil. 18(3), 297–302 (2010)
Xiao Y., Li P., Cheng Y., Zhang X., Sheng J., Wang D., Li J., Zhang Q., Zhong C., Cao R.: Enhancing the intestinal absorption of low molecular weight chondroitin sulfate by conjugation with α-linolenic acid and the transport mechanism of the conjugates. Int. J. Pharm. 465(1), 143–158 (2014)
Ronca G., Conte A.: Metabolic fate of partially depolymerized shark chondroitin sulfate in man. Int. J. Clin. Pharmacol. Res. 13, 27–34 (1992)
Volpi N.: Oral absorption and bioavailability of ichthyic origin chondroitin sulfate in healthy male volunteers. Osteoarthr. Cartil. 11(6), 433–441 (2003)
Du J., White N., Eddington N.D.: The bioavailability and pharmacokinetics of glucosamine hydrochloride and chondroitin sulfate after oral and intravenous single dose administration in the horse. Biopharm. Drug Dispos. 25(3), 109–116 (2004)
Hathcock J.N., Shao A.: Risk assessment for glucosamine and chondroitin sulfate. Regul. Toxicol. Pharmacol. 47(1), 78–83 (2007)
Cerda C., Bruguera M., Parés A.: Hepatotoxicity associated with glucosamine and chondroitin sulfate in patients with chronic liver disease. World journal of gastroenterology: WJG. 19(32), 5381 (2013)
von Felden J., Montani M., Kessebohm K., Stickel F.: Drug-induced acute liver injury mimicking autoimmune hepatitis after intake of dietary supplements containing glucosamine and chondroitin sulfate. Int. J. Clin. Pharmacol. Ther. 51(3), 219–223 (2013)
Felson D.T., Lawrence R.C., Hochberg M.C., McAlindon T., Dieppe P.A., Minor M.A., Blair S.N., Berman B.M., Fries J.F., Weinberger M.: Osteoarthritis: new insights. Part 2: treatment approaches. Annals of internal medicine. 133(9), 726–737 (2000)
Gerlie, C., Koda, R.T., Lien, E.J.: Glucosamine and chondroitin sulfates in the treatment of osteoarthritis: a survey. In: Progress in drug research. pp. 81–103. Springer, (2000)
Zegels B., Crozes P., Uebelhart D., Bruyère O., Reginster J.-Y.: Equivalence of a single dose (1200 mg) compared to a three-time a day dose (400 mg) of chondroitin 4&6 sulfate in patients with knee osteoarthritis. Results of a randomized double blind placebo controlled study. Osteoarthritis and Cartilage. 21(1), 22–27 (2013)
Uwe S.: Anti-inflammatory interventions of NF-κB signaling: potential applications and risks. Biochem. Pharmacol. 75(8), 1567–1579 (2008)
Foell D., Wittkowski H., Roth J.: Mechanisms of disease: a 'DAMP' view of inflammatory arthritis. Nature clinical practice. Rheumatology. 3(7), 382–390 (2007). doi:10.1038/ncprheum0531
Jomphe C., Gabriac M., Hale T.M., Heroux L., Trudeau L.E., Deblois D., Montell E., Verges J., du Souich P.: Chondroitin sulfate inhibits the nuclear translocation of nuclear factor-kappaB in interleukin-1beta-stimulated chondrocytes. Basic & clinical pharmacology & toxicology. 102(1), 59–65 (2008). doi:10.1111/j.1742-7843.2007.00158.x
Smiley S.T., King J.A., Hancock W.W.: Fibrinogen stimulates macrophage chemokine secretion through toll-like receptor 4. Journal of immunology (Baltimore, Md.: 1950). 167(5), 2887–2894 (2001)
Stahel P.F., Smith W.R., Moore E.E.: Role of biological modifiers regulating the immune response after trauma. Injury. 38(12), 1409–1422 (2007). doi:10.1016/j.injury.2007.09.023
Liu-Bryan R., Terkeltaub R.: Chondrocyte innate immune myeloid differentiation factor 88-dependent signaling drives procatabolic effects of the endogenous toll-like receptor 2/toll-like receptor 4 ligands low molecular weight hyaluronan and high mobility group box chromosomal protein 1 in mice. Arthritis Rheum. 62(7), 2004–2012 (2010). doi:10.1002/art.27475
van Lent P.L., Blom A.B., Schelbergen R.F., Sloetjes A., Lafeber F.P., Lems W.F., Cats H., Vogl T., Roth J., van den Berg W.B.: Active involvement of alarmins S100 A8 and S100 A9 in the regulation of synovial activation and joint destruction during mouse and human osteoarthritis. Arthritis Rheum. 64(5), 1466–1476 (2012). doi:10.1002/art.34315
Schelbergen R.F., Blom A.B., van den Bosch M.H., Sloetjes A., Abdollahi-Roodsaz S., Schreurs B.W., Mort J.S., Vogl T., Roth J., van den Berg W.B., van Lent P.L.: Alarmins S100 A8 and S100 A9 elicit a catabolic effect in human osteoarthritic chondrocytes that is dependent on toll-like receptor 4. Arthritis Rheum. 64(5), 1477–1487 (2012). doi:10.1002/art.33495
Sohn D.H., Sokolove J., Sharpe O., Erhart J.C., Chandra P.E., Lahey L.J., Lindstrom T.M., Hwang I., Boyer K.A., Andriacchi T.P., Robinson W.H.: Plasma proteins present in osteoarthritic synovial fluid can stimulate cytokine production via toll-like receptor 4. Arthritis research & therapy. 14(1), R7 (2012). doi:10.1186/ar3555
Liu-Bryan R., Pritzker K., Firestein G.S., Terkeltaub R.: TLR2 signaling in chondrocytes drives calcium pyrophosphate dihydrate and monosodium urate crystal-induced nitric oxide generation. Journal of immunology (Baltimore, Md.: 1950). 174(8), 5016–5023 (2005)
Martinon F., Petrilli V., Mayor A., Tardivel A., Tschopp J.: Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 440(7081), 237–241 (2006). doi:10.1038/nature04516
Pazar B., Ea H.K., Narayan S., Kolly L., Bagnoud N., Chobaz V., Roger T., Liote F., So A., Busso N.: Basic calcium phosphate crystals induce monocyte/macrophage IL-1beta secretion through the NLRP3 inflammasome in vitro. Journal of immunology (Baltimore, Md.: 1950). 186(4), 2495–2502 (2011). doi:10.4049/jimmunol.1001284
Denoble A.E., Huffman K.M., Stabler T.V., Kelly S.J., Hershfield M.S., McDaniel G.E., Coleman R.E., Kraus V.B.: Uric acid is a danger signal of increasing risk for osteoarthritis through inflammasome activation. Proc. Natl. Acad. Sci. U. S. A. 108(5), 2088–2093 (2011). doi:10.1073/pnas.1012743108
Steenvoorden M.M., Bank R.A., Ronday H.K., Toes R.E., Huizinga T.W., DeGroot J.: Fibroblast-like synoviocyte-chondrocyte interaction in cartilage degradation. Clin. Exp. Rheumatol. 25(2), 239–245 (2007)
Wang Q., Rozelle A.L., Lepus C.M., Scanzello C.R., Song J.J., Larsen D.M., Crish J.F., Bebek G., Ritter S.Y., Lindstrom T.M., Hwang I., Wong H.H., Punzi L., Encarnacion A., Shamloo M., Goodman S.B., Wyss-Coray T., Goldring S.R., Banda N.K., Thurman J.M., Gobezie R., Crow M.K., Holers V.M., Lee D.M., Robinson W.H.: Identification of a central role for complement in osteoarthritis. Nat. Med. 17(12), 1674–1679 (2011). doi:10.1038/nm.2543
Loeser R.F.: Molecular mechanisms of cartilage destruction: mechanics, inflammatory mediators, and aging collide. Arthritis Rheum. 54(5), 1357–1360 (2006). doi:10.1002/art.21813
Kaneko S., Satoh T., Chiba J., Ju C., Inoue K., Kagawa J.: Interleukin-6 and interleukin-8 levels in serum and synovial fluid of patients with osteoarthritis. Cytokines, cellular & molecular therapy. 6(2), 71–79 (2000)
Martel-Pelletier J., Pelletier J.P., Fahmi H.: Cyclooxygenase-2 and prostaglandins in articular tissues. Semin. Arthritis Rheum. 33(3), 155–167 (2003)
Okamura Y., Watari M., Jerud E.S., Young D.W., Ishizaka S.T., Rose J., Chow J.C., Strauss 3rd J.F.: The extra domain A of fibronectin activates toll-like receptor 4. J. Biol. Chem. 276(13), 10229–10233 (2001). doi:10.1074/jbc.M100099200
Termeer C., Benedix F., Sleeman J., Fieber C., Voith U., Ahrens T., Miyake K., Freudenberg M., Galanos C., Simon J.C.: Oligosaccharides of hyaluronan activate dendritic cells via toll-like receptor 4. The Journal of experimental medicine. 195(1), 99–111 (2002)
Midwood K., Sacre S., Piccinini A.M., Inglis J., Trebaul A., Chan E., Drexler S., Sofat N., Kashiwagi M., Orend G., Brennan F., Foxwell B.: Tenascin-C is an endogenous activator of toll-like receptor 4 that is essential for maintaining inflammation in arthritic joint disease. Nat. Med. 15(7), 774–780 (2009). doi:10.1038/nm.1987
Nakoshi Y., Hasegawa M., Akeda K., Iino T., Sudo A., Yoshida T., Uchida A.: Distribution and role of tenascin-C in human osteoarthritic cartilage. J. Orthop. Sci. 15(5), 666–673 (2010)
Monfort J., Nacher M., Montell E., Vila J., Verges J., Benito P.: Chondroitin sulfate and hyaluronic acid (500-730 kda) inhibit stromelysin-1 synthesis in human osteoarthritic chondrocytes. Drugs Exp. Clin. Res. 31(2), 71–76 (2004)
Homandberg G.A., Hui F.: Association of proteoglycan degradation with catabolic cytokine and stromelysin release from cartilage cultured with fibronectin fragments. Arch. Biochem. Biophys. 334(2), 325–331 (1996). doi:10.1006/abbi.1996.0461
Vuolteenaho K., Koskinen A., Kukkonen M., Nieminen R., Päivärinta U., Moilanen T., Moilanen E.: Leptin enhances synthesis of proinflammatory mediators in human osteoarthritic cartilage—mediator role of NO in Leptin-Induced P G E. Mediat. Inflamm. 2009, 345838 (2009)
Ishimaru D., Sugiura N., Akiyama H., Watanabe H., Matsumoto K.: Alterations in the chondroitin sulfate chain in human osteoarthritic cartilage of the knee. Osteoarthr. Cartil. 22(2), 250–258 (2014)
Sokolove J., Lepus C.M.: Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Therapeutic advances in musculoskeletal disease. 5(2), 77–94 (2013)
Gupta G.S., Gupta A., Gupta R.K.: Animal lectins: form. Function and Clinical Applications, Form, Function and Clinical Applications. Springer, Vienna (2012)
Harris E.N., Weigel P.H.: The ligand-binding profile of HARE: hyaluronan and chondroitin sulfates A, C, and D bind to overlapping sites distinct from the sites for heparin, acetylated low-density lipoprotein, dermatan sulfate, and CS-E. Glycobiology. 18(8), 638–648 (2008). doi:10.1093/glycob/cwn045
Weigel P.H., Yik J.H.: Glycans as endocytosis signals: the cases of the asialoglycoprotein and hyaluronan/chondroitin sulfate receptors. Biochimica et Biophysica Acta (BBA)-General Subjects. 1572(2), 341–363 (2002)
Dickendesher T.L., Baldwin K.T., Mironova Y.A., Koriyama Y., Raiker S.J., Askew K.L., Wood A., Geoffroy C.G., Zheng B., Liepmann C.D.: NgR1 and NgR3 are receptors for chondroitin sulfate proteoglycans. Nat. Neurosci. 15(5), 703–712 (2012)
du Souich P.: Absorption, distribution and mechanism of action of SYSADOAS. Pharmacol. Ther. 142(3), 362–374 (2014)
Bara J.J., Johnson W.E.B., Caterson B., Roberts S.: Articular cartilage glycosaminoglycans inhibit the adhesion of endothelial cells. Connect. Tissue Res. 53(3), 220–228 (2012)
Martel-Pelletier J., Roubille C., Abram F., Hochberg M.C., Dorais M., Delorme P., Raynauld J.-P., Pelletier J.-P.: First-line analysis of the effects of treatment on progression of structural changes in knee osteoarthritis over 24 months: data from the osteoarthritis initiative progression cohort. Ann. Rheum. Dis. 74, 547–556 (2015)
Wildi L.M., Raynauld J.-P., Martel-Pelletier J., Beaulieu A., Bessette L., Morin F., Abram F., Dorais M., Pelletier J.-P.: Chondroitin sulphate reduces both cartilage volume loss and bone marrow lesions in knee osteoarthritis patients starting as early as 6 months after initiation of therapy: a randomised, double-blind, placebo-controlled pilot study using MRI. Ann. Rheum. Dis. 70(6), 982–989 (2011)
Largo R., Roman-Blas J., Moreno-Rubio J., Sánchez-Pernaute O., Martínez-Calatrava M., Castañeda S., Herrero-Beaumont G.: Chondroitin sulfate improves synovitis in rabbits with chronic antigen-induced arthritis. Osteoarthr. Cartil. 18, S17–S23 (2010)
Hochberg M.: Structure-modifying effects of chondroitin sulfate in knee osteoarthritis: an updated meta-analysis of randomized placebo-controlled trials of 2-year duration. Osteoarthr. Cartil. 18, S28–S31 (2010)
Hochberg M., Chevalier X., Henrotin Y., Hunter D., Uebelhart D.: Symptom and structure modification in osteoarthritis with pharmaceutical-grade chondroitin sulfate: what's the evidence? Current Medical Research & Opinion. 29(3), 259–267 (2013)
Imada K., Oka H., Kawasaki D., Miura N., Sato T., Ito A.: Anti-arthritic action mechanisms of natural chondroitin sulfate in human articular chondrocytes and synovial fibroblasts. Biol. Pharm. Bull. 33(3), 410–414 (2010)
Ouzzine M., Venkatesan N., Fournel-Gigleux S.: Proteoglycans and cartilage repair. in: proteoglycans, pp. 339–355. Springer, N. Y. (2012)
Campbell E.J., Owen C.A.: The sulfate groups of chondroitin sulfate-and heparan sulfate-containing proteoglycans in neutrophil plasma membranes are novel binding sites for human leukocyte elastase and cathepsin G. J. Biol. Chem. 282(19), 14645–14654 (2007)
Tat S.K., Pelletier J.-P., Vergés J., Lajeunesse D., Montell E., Fahmi H., Lavigne M., Martel-Pelletier J.: Chondroitin and glucosamine sulfate in combination decrease the pro-resorptive properties of human osteoarthritis subchondral bone osteoblasts: a basic science study. Arthritis Res. Ther. 9(6), R117 (2007)
Sobal G., Dorotka R., Menzel J., Sinzinger H.: Uptake studies with chondrotropic 99mTc-chondroitin sulfate in articular cartilage. Implications for imaging osteoarthritis in the knee. Nucl Med Biol. 40(8), 1013–1017 (2013). doi:10.1016/j.nucmedbio.2013.07.007
Campo G.M., Avenoso A., Campo S., Ferlazzo A., Altavilla D., Micali C., Calatroni A.: Aromatic trap analysis of free radicals production in experimental collagen-induced arthritis in the rat: protective effect of glycosaminoglycans treatment. Free Radic. Res. 37(3), 257–268 (2003)
Martínez-Calatrava M., Largo R., Herrero-Beaumont G.: Improvement of experimental accelerated atherosclerosis by chondroitin sulphate. Osteoarthr. Cartil. 18, S12–S16 (2010)
Jain A., Gulbake A., Shilpi S., Jain A., Hurkat P., Jain S.K.: A new horizon in modifications of chitosan: syntheses and applications. Crit. Rev. Ther. Drug Carrier Syst. 30(2), 91–181 (2013)
Subudhi M., Jain A., Jain A., Hurkat P., Shilpi S., Gulbake A., Jain S.: Eudragit S100 Coated Citrus Pectin nanoparticles for Colon targeting of 5-Fluorouracil. Materials. 8(3), 832–849 (2015)
Jain A., Jain S.K.: Environmentally Responsive Chitosan-based Nanocarriers (CBNs). Handbook of Polymers for Pharmaceutical Technologies, Biodegradable Polymers. 3, 105 (2015)
Bauerova K., Ponist S., Kuncirova V., Mihalova D., Paulovicova E., Volpi N.: Chondroitin sulfate effect on induced arthritis in rats. Osteoarthr. Cartil. 19(11), 1373–1379 (2011)
Gabay C., Medinger-Sadowski C., Gascon D., Kolo F., Finckh A.: Symptomatic effects of chondroitin 4 and chondroitin 6 sulfate on hand osteoarthritis: A randomized, double-blind, placebo-controlled clinical trial at a single center. Arthritis & Rheumatism. 63(11), 3383–3391 (2011)
Nakasone Y., Watabe K., Watanabe K., Tomonaga A., Nagaoka I., Yamamoto T., Yamaguchi H.: Effect of a glucosamine-based combination supplement containing chondroitin sulfate and antioxidant micronutrients in subjects with symptomatic knee osteoarthritis: A pilot study. Exp Ther Med. 2(5), 893–899 (2011). doi:10.3892/etm.2011.298
Chen L., Ling P., Jin Y., Zhang T.: Hyaluronic acid in combination with chondroitin sulfate and hyaluronic acid improved the degeneration of synovium and cartilage equally in rabbits with osteoarthritis. Drug discoveries & therapeutics. 5(4), 190–194 (2011)
Kanzaki N., Saito K., Maeda A., Kitagawa Y., Kiso Y., Watanabe K., Tomonaga A., Nagaoka I., Yamaguchi H.: Effect of a dietary supplement containing glucosamine hydrochloride, chondroitin sulfate and quercetin glycosides on symptomatic knee osteoarthritis: a randomized, double-blind, placebo-controlled study. J. Sci. Food Agric. 92(4), 862–869 (2012)
Perea S.: Nutritional management of osteoarthritis. Compendium (Yardley, PA). 34(5), E4 (2012)
Lascelles B., DePuy V., Thomson A., Hansen B., Marcellin-Little D., Biourge V., Bauer J.: Evaluation of a therapeutic diet for feline degenerative joint disease. J. Vet. Intern. Med. 24(3), 487–495 (2010)
DiNubile N.A.: A potential role for Avocado-and Soybean-Based Nutritional supplements in the management of Osteoarthritis. Physician and Sportsmedicine. 38(2), 71–81 (2010)
Pavelka K., Coste P., Géher P., Krejci G.: Efficacy and safety of piascledine 300 versus chondroitin sulfate in a 6 months treatment plus 2 months observation in patients with osteoarthritis of the knee. Clin. Rheumatol. 29(6), 659–670 (2010)
Richette P.: Management of osteoarthritis: oral therapies. Rev Prat. 62(5), 654–660 (2012)
Sofat N., Beith I., Anilkumar P.G., Mitchell P.: Recent clinical evidence for the treatment of osteoarthritis: What we have learned. Reviews on recent clinical trials. 6(2), 114–126 (2011)
Diehl P., Gerdesmeyer L., Schauwecker J., Kreuz P., Gollwitzer H., Tischer T.: Conservative therapy of osteoarthritis. Der Orthopade. 42(2), 125–139 (2013)
Railhac J., Zaim M., Saurel A., Vial J., Fournie B.: Effect of 12 months treatment with chondroitin sulfate on cartilage volume in knee osteoarthritis patients: a randomized, double-blind, placebo-controlled pilot study using MRI. Clin. Rheumatol. 31(9), 1347–1357 (2012)
Guilherme M.R., Reis A.V., Alves B.R., Kunita M.H., Rubira A.F., Tambourgi E.B.: Smart hollow microspheres of chondroitin sulfate conjugates and magnetite nanoparticles for magnetic vector. J. Colloid Interface Sci. 352(1), 107–113 (2010)
Wang S.-C., Chen B.-H., Wang L.-F., Chen J.-S.: Characterization of chondroitin sulfate and its interpenetrating polymer network hydrogels for sustained-drug release. Int. J. Pharm. 329(1), 103–109 (2007)
Strehin I., Nahas Z., Arora K., Nguyen T., Elisseeff J.: A versatile pH sensitive chondroitin sulfate–PEG tissue adhesive and hydrogel. Biomaterials. 31(10), 2788–2797 (2010)
Oprea A.-M., Profire L., Lupusoru C.E., Ghiciuc C.M., Ciolacu D., Vasile C.: Synthesis and characterization of some cellulose/chondroitin sulphate hydrogels and their evaluation as carriers for drug delivery. Carbohydr. Polym. 87(1), 721–729 (2012)
Li W., Li X., Su H., Zhao S., Li Y., Hu J.: Facile synthesis of chondroitin sulfate-stabilized gold nanoparticles. Mater. Chem. Phys. 125(3), 518–521 (2011)
Jiang T., Petersen R.R., Call G., Ofek G., Gao J., Yao J.Q.: Development of chondroitin sulfate encapsulated PLGA microsphere delivery systems with controllable multiple burst releases for treating osteoarthritis. Journal of biomedical materials research. Part B, Applied biomaterials. 97(2), 355–363 (2011). doi:10.1002/jbm.b.31822
Craciunescu O., Moldovan L., Moisei M., Trif M.: Liposomal formulation of chondroitin sulfate enhances its antioxidant and anti-inflammatory potential in L929 fibroblast cell line. Journal of liposome research. 23(2), 145–153 (2013)
Bagari R., Bansal D., Gulbake A., Jain A., Soni V., Jain S.K.: Chondroitin sulfate functionalized liposomes for solid tumor targeting. J. Drug Target. 19(4), 251–257 (2011)
Onishi H., Yoshida R., Matsuyama M.: Chondroitin sulfate-glycyl-prednisolone conjugate as arthritis targeting system: localization and drug release in inflammatory joints. Biol. Pharm. Bull. 37(10), 1641–1649 (2014)
Avachat A., Kotwal V.: Design and evaluation of matrix-based controlled release tablets of diclofenac sodium and chondroitin sulphate. AAPS PharmSciTech. 8(4), 51–56 (2007)
Huang S.-J., Sun S.-L., Feng T.-H., Sung K.-H., Lui W.-L., Wang L.-F.: Folate-mediated chondroitin sulfate-Pluronic® 127 nanogels as a drug carrier. Eur. J. Pharm. Sci. 38(1), 64–73 (2009)
Lin Y.-J., Liu Y.-S., Yeh H.-H., Cheng T.-L., Wang L.-F.: Self-assembled poly (ε-caprolactone)-g-chondroitin sulfate copolymers as an intracellular doxorubicin delivery carrier against lung cancer cells. Int. J. Nanomedicine. 7, 4169 (2012)
Bishnoi M., Jain A., Hurkat P., Jain S.K.: Aceclofenac-loaded chondroitin sulfate conjugated SLNs for effective management of osteoarthritis. J. Drug Target. 22(9), 805–812 (2014)
Lee E.S., Park K.-H., Kang D., Park I.S., Min H.Y., Lee D.H., Kim S., Kim J.H., Na K.: Protein complexed with chondroitin sulfate in poly (lactide- co-glycolide) microspheres. Biomaterials. 28(17), 2754–2762 (2007)
Santo V.E., Duarte A.R.C., Gomes M.E., Mano J.F., Reis R.L.: Hybrid 3D structure of poly (d, l-lactic acid) loaded with chitosan/chondroitin sulfate nanoparticles to be used as carriers for biomacromolecules in tissue engineering. J. Supercrit. Fluids. 54(3), 320–327 (2010)
Singh, J.A., Noorbaloochi, S., MacDonald, R., Maxwell, L.J.: Chondroitin for osteoarthritis. Cochrane Database Syst. Rev. (2015). doi:10.1002/14651858.CD005614.pub2
Uebelhart D., Malaise M., Marcolongo R., DeVathaire F., Piperno M., Mailleux E., Fioravanti A., Matoso L., Vignon E.: Intermittent treatment of knee osteoarthritis with oral chondroitin sulfate: a one-year, randomized, double-blind, multicenter study versus placebo. Osteoarthr. Cartil. 12(4), 269–276 (2004)
Mazieres B., Combe B., Phan Van A., Tondut J., Grynfeltt M.: Chondroitin sulfate in osteoarthritis of the knee: a prospective, double blind, placebo controlled multicenter clinical study. J. Rheumatol. 28(1), 173–181 (2001)
Sorgente N.: Nakamura. R.M: Methods for treating arthritis using collagen type II, glucosamine chondroitin sulfate, and compositions. US 6162787 A (2000)
Nimni M.E.: Method for alleviating arthritis in mammals. US 6372794 B1 (2002)
Derrieu G.: Pougnas. J.L: Chondroitin sulphate and chitosan compositions for treating rheumatic disorders. US 6599888 B1 (2003)
Miyasaka M., Kawashima H.: Persulfated oligosaccharide acting on selectins and chemokine. US 20060211651 A1 (2006)
Aspberg A., Heinegaerd D., Johnson A., Kvist A.: Use of chondroitin sulphate e (cs-e) for the treatment diseases or conditions related to collagen fibril formation. In. Google Patents (2005)
Acknowledgments
Authors namely AJ and PH are thankful to Council of Scientific and Industrial Research (New Delhi) for providing Senior Research Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest including all financial and non-financial nature.
Author’s contribution
All authors contributed equally for the content and writing of this manuscript. They read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Bishnoi, M., Jain, A., Hurkat, P. et al. Chondroitin sulphate: a focus on osteoarthritis. Glycoconj J 33, 693–705 (2016). https://doi.org/10.1007/s10719-016-9665-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10719-016-9665-3