Abstract
Purpose of Review
Trichomonas vaginalis is the most prevalent sexually transmitted parasite in the USA; resistant infection is emerging. New drug therapies and dosing regimens of standard therapies are being studied to treat resistant infection.
Recent Findings
Diagnosis of trichomoniasis has become more sensitive, specific, and widely available with the advent of nucleic acid amplification tests (NAATs). Women with resistant trichomoniasis should be treated with high-dose regimens of metronidazole or tinidazole. Alternative treatment options have been described, and there has been some success particularly with high-dose tinidazole/intravaginal paromomycin cream combination, intravaginal boric acid, and intravaginal metronidazole/miconazole.
Summary
Resistant trichomoniasis is a growing public health concern with implications for long-term health consequences. More data are needed to further evaluate mechanisms by which resistance occurs as well as promising therapies for those affected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Affecting an estimated 3.7 million men and women, trichomoniasis is the most prevalent nonviral sexually transmitted infection (STI) in the USA [1]. It is more prevalent than chlamydia, gonorrhea, and syphilis combined [2]. Health disparities related to the epidemiology of the infection are prominent. Unlike most STIs, prevalence increases with age; an estimated 11% of infections occur among women over 40 years of age. Prevalence is also high among non-Hispanic black women, incarcerated individuals, women infected with HIV, STI clinic patients, and drug users [1]. Similar to bacterial vaginosis, trichomoniasis has been associated with long-term sequelae including pelvic inflammatory disease, which can impact future fertility, as well as contribute to poor pregnancy outcome and increased transmission of HIV [3]. Since the 1950s, the mainstay of therapy has been the nitroimidazoles, a drug class demonstrating high cure rates against T. vaginalis. However, persistent and recurrent infections are becoming a greater concern as the incidence of treatment failure due to resistant infection rises.
Clinical Presentation
T. vaginalis preferentially infects the urethra of men and women as well as the vagina and endocervix of women. It is unclear if the rectal or oral cavity can be a reservoir, as few studies have evaluated these sites [1]. Approximately 50 to 60% of infections in women are asymptomatic [4]. The most common symptom is vaginal discharge, which is usually frothy and yellowish-gray or green in color and often associated with a pH > 4.5. Other symptoms include dyspareunia, dysuria, lower abdominal pain, and vulvovaginal irritation [5]. Physical findings may include vulvovaginal erythema, discharge, and rarely, punctate hemorrhages of the vaginal mucosa or cervix, termed colpitis macularis or “strawberry cervix.” Common symptoms in men include urethral discharge, pruritis, dysuria, urinary frequency, and lower abdominal pain [6]. It can also cause epididymitis, prostatitis, and decreased sperm motility [2].
Screening
There are currently no guidelines for the optimal frequency of screening asymptomatic patients for T. vaginalis. The CDC recommends testing symptomatic women with vaginal discharge, as well as women who are at high risk for contracting an STI. Local or regional prevalence may be taken into account. Regarding HIV-infected women, screening is recommended at least annually due to high prevalence and increased risk of PID. There is also an increased risk of transmitting HIV with a concomitant trichomoniasis infection and potential for decreased viral load and shedding with treatment. Screening in pregnancy is at the discretion of the provider, as routine screening is currently not recommended [1].
Diagnosis
Trichomoniasis can most commonly be diagnosed using microscopic evaluation of vaginal secretions via saline microscopy. Microscopy can be performed at point of care for low cost, but the sensitivity of this method is poor, ranging between 51 and 65%. It detects motile organisms only when present in vaginal secretions in high concentrations. Furthermore, the sample must be evaluated immediately, within 30 min of obtaining it [1, 7]. Prior to the development of molecular testing, culture was considered the gold standard for diagnosis of T. vaginalis. Sensitivity for culture is around 75–96% with a specificity of up to 100% [1]. Traditionally, our impression has been that culture was a relatively underutilized testing modality because many providers did not have culture medium available when needed. A further limitation of culture is that sensitivity may be less than 40% in men [3]. Although a Pap smear can also detect T. vaginalis, its sensitivity is similar to saline microscopy; the positive predictive value may be as low as 61.7%, and false positives can occur up to 31% of the time [7,8,9].
Nucleic acid amplification testing (NAAT) is now available for the detection of T. vaginalis with sensitivities higher than those of wet mount and culture. The APTIMA Trichomonas vaginalis assay (Hologic Gen-Probe; San Diego, CA) was FDA cleared in 2011 and can detect T. vaginalis RNA by transcription-mediated amplification from vaginal and endocervical swabs, thin prep samples, and urine [1, 8]. This assay has a clinical sensitivity of 95.2–100% and a specificity of 95.3–100%. Additionally, this assay can be used with urethral swabs or urine from men. The Cobas Amplicor CT/NG PCR assay (Roche, Indianapolis, Indiana) is FDA cleared for the detection of chlamydia and gonorrhea; however, it can be modified for T. vaginalis using vaginal and endocervical swabs, or urine. Sensitivities range from 88 to 97% and specificities from 98 to 99% [1, 10]. The Xpert TV test (Cepheid; Sunnyvale, CA) works by amplifying microbial DNA and provides results in 45 min. Sensitivity is 96–99% and specificity is 99%. Specimens can be obtained from both men and women [11, 12]. Lastly, the BD Max CT/GC/TV (MAX) assay is another NAAT for detection of chlamydia, gonorrhea, and trichomonas. T. vaginalis sensitivity was 96.1% for vaginal swabs, 93.4% for endocervical swabs, and 92.9% for female urine samples per a study by Van Der Pol et al. [13]. Specificity across all sample types was > 98.6%. Because T. vaginalis commonly occurs in conjunction with other STIs, testing for these three highly common infections simultaneously may potentially lead to better patient management [14].
Other options for testing for trichomoniasis include the OSOM Trichomonas Rapid Test (Sekisui Diagnostics; Framingham, MA), which detects antigens using immunochromatographic capillary flow dipstick technology [1]. Results of this test are ready within 10 min with a sensitivity of 82–95% and specificity of 97–100% [15]. Finally, recent studies have shown that the Affirm VP III (BD Diagnostic Systems, Sparks, MD), a commonly used nucleic acid probe-hybridization test for vaginal infections, has a lower than expected sensitivity of 46% [16]. Furthermore, the OSOM and Affirm VP III tests cannot be used to evaluate specimens from men [1].
Treatment
Standard of Care
Recommended medications for the treatment of trichomoniasis are metronidazole and tinidazole, which are both nitroimidazoles. A one-time 2-g dose of either drug orally has been considered standard therapy and has been recommended by the CDC [1, 15]. Metronidazole has been the mainstay of therapy since 1959. It is easily absorbed into the gastrointestinal tract with > 90% bioavailability. Peak plasma concentrations reach 40 mg/l after a single 2-g oral dose and 8 to 13 mg/l after 500 mg. The ability of metronidazole to exert its killing effect on T. vaginalis is concentration dependent under anaerobic conditions at a concentration ranging from 0.1 to > 8 mg/l. The drug is able to reach the necessary plasma concentration in most tissues including the uterus and fallopian tubes. Of interest, studies have suggested that it is not always detectable in vaginal secretions [3]. It is unclear whether insufficient drug concentrations in the vagina play a role in persistent infection and treatment failure.
Cure rates for a single dose of metronidazole is 90–95% and 86–100% for tinidazole [10]. An alternate regimen of metronidazole 500 mg twice daily for 7 days is recommended by the CDC as an alternative first-line regimen. Although single-dose therapy is convenient, especially for patients with compliance issues, evidence has shown that single-dose therapy may not always be sufficient for complete eradication and is more likely to be associated with side effects [2, 3]. Furthermore, a recent meta-analysis by Howe and Kissinger, which showed that treatment failure is 1.87 times more likely with a single-dose regimen of metronidazole as compared with a multidose, raises concerns about the effectiveness of a single 2-g dose of metronidazole [17••], and current evidence suggests that a single 2-g dose should no longer be used to routinely treat trichomoniasis. Metronidazole gel does not reach therapeutic levels in the vagina and is currently not recommended [15].
Tinidazole has a mechanism similar to metronidazole but has a longer half-life and can achieve greater serum levels. Because it is about ten times more expensive than metronidazole, most providers use it as second-line therapy for most cases of trichomoniasis [1]. Oral tinidazole has > 90% bioavailability when taken orally and a 2-g dose can produce peak plasma concentrations between 40 and 58 mg/l, far greater than that of metronidazole. In vitro data demonstrate that 60% of T. vaginalis isolates had a lower minimum lethal concentration (MLC) for tinidazole compared with that for metronidazole, further enhancing clinical efficacy [3, 18].
Partner Treatment
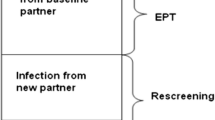
Because the infection can be readily passed between sex partners, both partners should receive the same treatment. One study showed 72% of male sex partners of women with trichomoniasis were also infected and 77% of them were asymptomatic [3]. Oftentimes, providers advise patients that their partner should be tested and treated. However, sensitive tests for men are not readily available. Providers may consider presumptively treating partners by expedited partner therapy (EPT) and providing prescriptions or medications to the patient for their partner [2]. Optimal timing for a test of cure has not been established for NAAT and testing too soon could detect remnants of nucleic acid from nonviable organisms that have been treated. Per the CDC, the patient can be re-tested as early as 2 weeks following treatment; however, the studies supporting this do not consider sexual exposure or treatment failure. A study by Craig-Kuhn et al. demonstrated that the optimal timing for NAAT re-testing following completion of treatment without sexual re-exposure is 3 weeks for patients who received multidose metronidazole and 4 weeks for those who received single dose. This time frame allows for clearance of the trichomonal nucleic acid and avoids unnecessary re-treatment [19]. A test of cure for all sexually active women should be performed within 3 months, even if the patient is asymptomatic, to ensure that she is cured and to allow for the evaluation of possible re-infection [8, 15].
Alternative Treatments for Nonresistant T. vaginalis
Other nitromidazoles such as fexinidazole, secnidazole, and ornidazole are used as antiparasitic agents in other countries, but, with the exception of secnidazole, which is newly available for treatment of bacterial vaginosis, have not been approved in the USA and have not yet been studied for treatment of resistant infection [1]. Mentha crispa is a peppermint herbal medication with a similar efficacy as secnidazole in a small randomized trial performed in Brazil [20]. Other topically applied agents, including intravaginal povidone-iodine, clotrimazole, acetic acid, furazolidone, gentian violet, nonoxynol-9, and potassium permanganate, have not been shown to be effective and are not currently recommended by the CDC [15]. There are no reports of these drugs being studied for use in resistant infection [3].
Pathogenesis of Resistant Infection
Resistant trichomoniasis is primarily a clinical diagnosis, where a woman presents with an ongoing infection after taking appropriate treatment. As such, resistant trichomoniasis must be distinguished from reinfection and medication noncompliance. Reinfection may be acquired from a new partner or because the current partner was untreated or inadequately treated, possibly reinfected from another partner. Treatment failure can range from 7 to 10%, but the prevalence of resistant infection is estimated to be about 2–5% [2, 3].
Metronidazole resistance has been clinically defined as failure to cure infection after two courses of treatment [5, 21]. Insufficient absorption of metronidazole or inadequate transport of the drug to the site of infection may play an occasional role in treatment failure [22], but metronidazole resistance of the organism itself seems to be related to alterations in the chemical reaction required for the drug to take effect. Resistance can occur under both aerobic and anaerobic conditions by way of different mechanisms [3]. Nitroimidazoles are prodrugs requiring reductive activation of the nitro group in order to become active. The release of toxic-free radicals such as hydrogen peroxide and nitro radicals allows for metronidazole’s trichomonacidal activity [23•]. Decreased oxygen scavenging in the cell leads to higher intracellular oxygen concentration allowing for resistance to occur. Furthermore, expression of flavin reductase 1, an enzyme playing a role in the reduction of the nitro group, has been found to be downregulated in metronidazole-resistant T. vaginalis. Correlations have also been found between metronidazole resistance and mutations in the genes for nitroreductase enzymes, which are also essential in this reaction [24].
Treatment of Resistant Infection
In general, treatment of resistant trichomoniasis infections is primarily empirical, and the initial plan as recommended in CDC guidelines is to give higher doses of nitroimidazoles. Patients with suspected resistance should initially be treated with a higher dose of metronidazole of 500 mg twice daily for 7 days [8, 21]. If this treatment fails, high-dose metronidazole or tinidazole should be used (2 g orally for 7 days) [15]. If this latter regimen does not work, tinidazole should be considered the primary nitroimidazole to be used. Tinidazole resistance occurs in only an estimated 1% of cases of vaginal trichomoniasis [21]. Furthermore, tinidazole seems to be more active against isolates that have demonstrated resistance. For subsequent failures, even higher doses of oral tinidazole can be used (2 to 3 g orally for 14 days), in combination with intravaginal tinidazole 500 mg twice daily [15].
CDC guidelines also discuss the option of in vitro susceptibility testing of resistant isolates [1, 15]. A study by Bosserman and colleagues examined isolates undergoing susceptibility testing from women who had failed at least 2 courses of standard therapy for trichomonas. In vitro, 115 of 175 isolates demonstrated metronidazole resistance. Resistance to tinidazole was similar or lower. Out of the women who received an alternative recommended nitroimidazole treatment based on susceptibility testing, 82% were cured compared with 53% of women who received a lower dose than recommended. Thus, susceptibility testing may be beneficial for management of women with persistent infection [22]. Several in vitro studies have looked at the level of metronidazole resistance; however, more data is needed to determine if there is any relationship to clinical response to treatment [25,26,27]. Although susceptibility testing may help guide treatment, it is important to remember that metronidazole resistance is ultimately a clinical diagnosis. Susceptibility testing for tinidazole is encouraged but it is not mandatory and the benefits are unclear.
Beyond the nitroimidazoles, compounded vaginal paromomycin is an approach to treatment which has been used with the greatest success in resistant infections. Paromomycin is an aminoglycoside which destroys ribosomal RNA. It is not absorbed by the GI tract and must be used vaginally. Used as solo therapy, paromomycin cream may have a relatively high failure rate. Of further concern, it can cause acute vulvar ulcers, which are self-limited but can be very painful [18]. To mitigate the possibility of ulcers, we routinely recommend that patients apply petrolatum liberally to the vulva and vestibule to protect the area, and that they stop use of the cream immediately if they begin to notice any vulvar or vaginal pain while using it. Management of resistant trichomoniasis was reviewed by Miller and Nyirjesy in 2011, and at the time, the best treatment options for which there was the most published experience were high-dose oral and vaginal tinidazole or high-dose oral tinidazole with paromomycin cream [6]. Table 1 summarizes data about what we consider the best options for treating patients with highly resistant infections.
Since our earlier review, case reports have shown that high-level nitroimidazole-resistant trichomoniasis can be treated successfully with a combination of high-dose oral tinidazole (1 g three times a day) and intravaginal paromomycin cream (6.25%, 5 g vaginally nightly) for 14 days. Two cases of patients with infections resistant to high-dose metronidazole and tindazole were cured with a combination of high-dose oral tinidazole and vaginal paromomycin cream [35]. In a more recent case, we described a patient with a resistant infection who initially, mistakenly, took high-dose oral tinidazole, followed by a course of vaginal paromomycin cream, but was not cured [36••]. She subsequently took the same two medications, but this time in combination, and was successfully cured. This case illustrates the possibility that paromomycin and tinidazole, which have completely different mechanisms of action, may have either an additive or possibly even a synergistic effect. To our knowledge, there has not been a single treatment failure with this combination.
Since our last review, a new option for treating trichomoniasis, boric acid, has been described. Boric acid is an inorganic acid that has long been used for the treatment of vulvovaginal candidiasis, especially for non-Albicans candida, as well as more recently an adjunct to treatment for women with recurrent bacterial vaginosis. The usual dose for these vaginal infections is 600-mg capsule administered vaginally every night for a variable amount of time. In vitro studies have suggested activity against T. vaginalis by inhibiting its growth across a range of vaginal pHs. Activity appears dose dependent; case reports have demonstrated T. vaginalis clearance, particularly in women who have failed metronidazole therapy and in those with a metronidazole allergy. A review of cases reports by Thorley [37••] demonstrated clearance of T. vaginalis using boric acid in a variety of intravaginal dosing regimens, ranging from 600 mg every other night up to 600 mg twice daily over the course of 1 to 5 months. In general, across all uses, vaginal boric acid is well tolerated, inexpensive, and widely available. Thus, the possibility that vaginal boric acid may be a useful option for a clinical scenario where the options are limited and, in the case of tinidazole, expensive, is encouraging. However, it should be emphasized that experience with boric acid for trichomoniasis remains very limited.
Finally, Byun and colleagues reported 8 cases of trichomoniasis, all of which had failed to respond to various nitromidazole dosing regimens, which were treated with 1% zinc sulfate douches with or without oral tinidazole for 14–28 days [5]. All of the patients were described as clinically improved with negative saline microscopy, but the absence of negative cultures or NAATs after treatment greatly limits the ability to draw conclusions from this experience. On a separate note, Chacon and colleagues have shown that chlorinated metronidazole, an analog of metronidazole, which produced higher rates of free radicals increasing the efficacy of the drug, may be more effective against T. vaginalis in vitro, but clinical experience with this formulation of metronidazole is lacking [23•].
Treatment of Resistant Infection in Partners
To our knowledge, there are very limited data that address how to treat metronidazole-resistant T. vaginalis strains in men. In case series of the partners of women with resistant strains, metronidazole 500 mg twice daily for 7 days, used in three partners, was the most commonly used treatment [28,29,30]. When we have treated women with resistant trichomoniasis, if they are still with their current male partners, we recommend that they take tinidazole 1 g daily for 7 days. To date, none of our patients have returned with a newly acquired T. vaginalis infection, but our experience should be considered anecdotal at best.
Metronidazole Hypersensitivity Reactions
There have been instances of adverse reactions to metronidazole including urticaria, pruritis, erythema, anaphylaxis, angioedema, and gastrointestinal distress. Reactions do not always recur with repeated doses. Tinidazole is closely related to metronidazole and data on cross-reactivity is highly limited, though similar adverse reactions have been documented [3, 8]. Thus, metronidazole desensitization should be performed. Oral and intravenous incremental dosing protocols for increasing doses of metronidazole being given over the course of a day have been used to desensitize patients successfully [38]. A study by Helms et al. demonstrated that out of 15 women who received metronidazole desensitization by a published IV or oral regimen, 100% were cured of infection. One woman who received the oral regimen developed a pruritic rash which resolved with steroids and another woman who received the IV regimen developed mild urticaria and pruritis, managed with antihistamines. Of the women with suspected metronidazole allergy who were treated with alternative regimens instead of undergoing desensitization, only about 42% were cured [38]. For patients unable to undergo metronidazole desensitization, it may be reasonable to try tinidazole desensitization. It may also be reasonable to try an alternative regimen such as paromomycin cream, paromomycin cream in combination with high-dose tinidazole, or boric acid. However, there is no data on how well these alternative regimens work in this patient population.
Conclusions
T. vaginalis is a highly prevalent sexually transmitted infection worldwide and the true incidence is likely underestimated due to the fact that it is nonreportable. Fortunately, the proportion of resistant infection is low but for those affected by it, the burden can be physically and emotionally substantial. The drugs available to treat T. vaginalis are highly limited as well as the data supporting alternative regimens for persistent infection. Future studies are needed to further examine the mechanisms by which resistance develops and new treatment regimens that can overcome it. The long-term health consequences associated with persistent infection must also be investigated.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Meites E, Gaydos CA, Hobbs MM, Kissinger P, Nyirjesy P, Schwebke JR, et al. A review of evidence-based care of symptomatic trichomoniasis and asymptomatic Trichomonas vaginalis infections. Clin Infect Dis. 2015;61(Suppl 8):S837–48. https://doi.org/10.1093/cid/civ738.
Kissinger P. Trichomonas vaginalis: a review of epidemiologic, clinical and treatment issues. BMC Infect Dis. 2015;15:307. https://doi.org/10.1186/s12879-015-1055-0.
Seña AC, Bachmann LH, Hobbs MM, et al. Persistent and recurrent Trichomonas vaginalis infections: epidemiology, treatment and management considerations. Expert Rev Anti Infect Ther. 2014;12(6):637–685. https://doi.org/10.1586/14787210.2014.887440.
Allsworth JE, Ratner JA, Peipert JF. Trichomoniasis and other sexually transmitted infections: results from the 2001e2004 National Health and Nutrition Examination Surveys. Sex Transm Dis. 2009;36:738e44.
Byun JM, Jeong DH, Kim YN, et al. Experience of successful treatment of patients with metronidazole-resistant Trichomonas vaginalis with zinc sulfate: a case series. Taiwan J Obstet Gynecol. 2015;54(5):617–20. https://doi.org/10.1016/j.tjog.2015.08.018.
Miller MR, Nyirjesy P. Refractory trichomoniasis in HIV-positive and HIV-negative subjects. Curr Infect Dis Rep. 2011;13(6):595–603. https://doi.org/10.1007/s11908-011-0213-9.
Lobo T, Feijo G, Carvalho S, Costa P, Chagas C, Xavier J, et al. A comparative evaluation of the Papanicolaou test for the diagnosis of trichomoniasis. Sex Transm Dis. 2003;30(9):694–9. https://doi.org/10.1097/01.OLQ.0000079525.04451.05.
Nyirjesy, P. Trichomoniasis and the 2015 CDC STD treatment guidelines: new insights, new urgency. OBG Manag 2016:S4–S6.
Lossick JG. The diagnosis of vaginal trichomoniasis. JAMA. 1988;259(8):1230. https://doi.org/10.1001/jama.1988.03720080064030.
Van Der Pol B, Kraft CS, Williams JA. Use of an adaptation of a commercially available PCR assay aimed at diagnosis of chlamydia and gonorrhea to detect Trichomonas vaginalis in urogenital specimens. J Clin Microbiol. 2006;44:366–73.
Hillier SL, Danby C The end of the wet mount. OBG Manag 2016: S2–S4.
Schwebke JR, Gaydoes CA, Davis T, et al. Clinical evaluation of the Cepheid Xpert TV assay for detection of Trichomonas vaginalis with prospectively collected specimens from men and women. J Clin Microbiol. 2018;56(2):e01091–17. https://doi.org/10.1128/JCM.01091-17.
Van Der Pol B, Williams JA, Fuller D, et al. Combined testing for chlamydia, gonorrhea, and trichomonas by use of the BD Max CT/GC/TV assay with genitourinary specimen types. J Clin Microbiol. 2017;55(1):155–64.
Kawa D, Kostiha B, Yu JH, et al. Elevating the standard of care for STIs: the BD Max CT/GC/TV assay. 2017.
Workowski KA, Bolan GA. Centers for Disease Control and Prevention. Sex Transm Dis Guidel. 2015;64(RR-03):1–137.
Cartwright CP, Lembke BD, Ramachandran K, Body BA, Nye MB, Rivers CA, et al. Comparison of nucleic-acid amplification assays with BD affirm VPIII for the diagnosis of vaginitis/vaginosis in symptomatic women. J Clin Microbiol. 2013;51(11):3694–9. https://doi.org/10.1128/JCM.01537-13.
•• Howe K, Kissinger PJ. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44(1):29–34. https://doi.org/10.1097/OLQ.0000000000000537 Study shows single dose has a higher failure rate than multidose regimen.
Crowell AL, Sanders-Lewis KA, Secor WE. In vitro metronidazole and tinidazole activities against metronidazole-resistant strains of Trichomonas vaginalis. Antimicrob Agents Chemother. 2003;47:1407–9.
Craig-Kuhn MC, Granade C, Muzny C, et al. Optimal timing for Trichomonas vaginalis test of cure using nucleic acid amplification testing. Sex Transm Dis. 2019;46:312–6.
Moraes ME, Cunha GH, Bezerra MM, et al. Efficacy of the Mentha crispa in the treatment of women with Trichomonas vaginalis infection. Arch Gynecol Obstet. 2012;286:125–30.
Ghosh AP, Aycock C, Schwebke JR. In vitro study of the susceptibility of clinical isolates of Trichomonas vaginalis to metronidazole and secnidazole. Antimicrob Agents Chemother. 2018;62(4):e02329–17.
Bosserman EA, Helms DJ, Mosure DJ, Secor WE, Workowski KA. Utility of antimicrobial susceptibility testing in Trichomonas vaginalis- infected women with clinical treatment failure. Sex Transm Dis. 2011;38(10):983–7.
• Chacon MO, Fonseca THS, Oliveira MA, et al. Chlorinated metronidazole as a promising alternative for treating trichomoniasis. Parasitol Res. 2018;117(5):1333–40 In vitro study demonstrating that altering the nitro group of metronidazole may make the drug more efficacious for treating resistant strains of T. vaginalis .
Leitsch D. Recent advances in the trichomonas vaginalis field. F1000Res. 2016;5:F1000 Faculty Rev-162. https://doi.org/10.12688/f1000research.7594.1.
Ertabaklar H, Yaman KS, Malatyali E, et al. Investigation of in vitro metronidazole resistance in the clinical isolates of Trichomonas vaginalis. Mikrobiyol Bul. 2016;50(4):552–8.
Abdel-Magied AA, El-Kholya EI, Abou El-Khair SM, et al. The genetic diversity of metronidazole susceptibility in Trichomonas vaginalis clinical isolates in an Egyptian population. Parasitol Res. 2017;116(11):3125–30. https://doi.org/10.1007/s00436-017-5627-3.
Matini M, Maghsood AH, Mohebali M, Rabiee S, Fallah M, Rezaie S, et al. In vitro susceptibility of Iranian isolates of Trichomonas vaginalis to metronidazole. Iran J Parasitol. 2016;11(1):46–51.
Waters LJ, Dave SS, Deayton JR, French PD. Recalcitrant Trichomonas vaginalis infection – a case series. Int J STD AIDS. 2005;16:505–9.
Sobel JD, Nyirjesy P, Brown W. Tinidazole therapy for metronidazole-resistant vaginal trichomoniasis. Clin Infect Dis. 2001;33:1341–6.
Hager DW. Treatment of metronidazole-resistant trichomonas vaginalis with tinidazole: case reports of three patients. Sex Transm Dis. 2004;31:343–5.
Tayal SC, Ochogwu SA, Bunce H. Paromomycin treatment of recalcitrant Trichomonas vaginalis. Int J STD AIDS. 2010;21:217–8.
Nyirjesy P. Paromomycin for nitroimidazole-resistant trichomonosis. Lancet. 1995;346:1110.
Coelho DD. Metronidazole resistant trichomoniasis successfully treated with paromomycin. Genitourin Med. 1997;73:397–8.
Poppe WAJ. Nitroimidazole-resistant vaginal trichomoniasis treated with paromomycin. Eur J Obstet Gynecol. 2001;96:119–20.
Nyirjesy P, Gilbert J, Mulcahy LJ. Resistant trichomoniasis: successful treatment with combination therapy. Sex Transm Dis. 2011;38(10):962–3. https://doi.org/10.1097/OLQ.0b013e31822037e4.
•• Henien M, Nyirjesy P, Smith K. Metronidazole-resistant trichomoniasis: beneficial pharmacodynamic relationship with high-dose oral tinidazole and vaginal paromomycin combination therapy. Sex Transm Dis. 2019;46(1):e1–2. https://doi.org/10.1097/OLQ.0000000000000903 Combination therapy with high-dose tinidazole and paromomycin shows promising results.
•• Thorley N, Ross J. Intravaginal boric acid: is it an alternative therapeutic option for vaginal trichomoniasis? Sex Transm Infect. 2018;94:574–7. https://doi.org/10.1136/sextrans-2017-053343 Boric acid may be a good alternative therapeutic option for resistant infection.
Helms DJ, Mosure DJ, Secor WE, et al. Management of Trichomonas vaginalis in women with suspected metronidazole hypersensitivity. Am J Obstet Gynecol. 2008;198:370–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Alessio has no conflicts of interest to disclose.
Dr. Nyirjesy has received grants from Mycovia Pharmaceuticals; Curatek Pharmaceuticals; Scynexis, Inc.; and Hologic. He also serves as a consultant for Mycovia Pharmaceuticals; Lupin Pharmaceuticals; Hologic; Scynexis, Inc.; Daré Bioscience; Inc.; and BD.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Female Genital Tract Infections
Rights and permissions
About this article
Cite this article
Alessio, C., Nyirjesy, P. Management of Resistant Trichomoniasis. Curr Infect Dis Rep 21, 31 (2019). https://doi.org/10.1007/s11908-019-0687-4
Published:
DOI: https://doi.org/10.1007/s11908-019-0687-4