Abstract
Purpose of Review
Cytomegalovirus (CMV) colitis is a relatively common end-organ infectious complication in immunocompromised hosts which negatively affects clinical outcomes. This paper presents the contemporary approaches to the diagnosis and management of CMV colitis and discusses some of the controversies of this condition, focusing on methods of diagnosis.
Recent Findings
While certain risk factors for CMV colitis are well recognized, the clinical as well as endoscopic features of this condition are nonspecific. Rapid diagnosis and management are usually needed, especially in critically ill patients, which necessitate invasive diagnostic procedures. Hematoxylin and eosin staining of colonic mucosal tissue may show the typical viral inclusions associated with CMV colitis that are highly specific for this condition. However, the staining has low sensitivity compared to immunohistochemistry, which is considered the gold standard for diagnosis of CMV colitis. Tissue polymerase chain reaction (PCR) is highly sensitive for diagnosis, but is controversial for many reasons, detailed in this paper.
Summary
A high index of suspicion is needed, and once diagnosis is made, treatment should be highly considered to improve the outcome of these severely ill patients. Noninvasive diagnostic tests will be available in the future and will hopefully improve the diagnosis and care of patients with CMV colitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cytomegalovirus (CMV), a member of the herpesviridae family, is a common viral infection in the general population. The seroprevalence of CMV varies between 40 and 100% and is influenced by age and geographic distribution [1]. CMV usually causes self-limited disease in the healthy population but may result in severe systemic disease in immunocompromised patients. CMV colitis occurs most commonly in immunocompromised hosts and is believed to negatively affect the clinical outcome of those patients [2].
The objective of this paper is to present contemporary approaches to the diagnosis and management of CMV colitis.
Epidemiology of CMV Colitis
CMV end-organ infection, including colitis, is a relatively common infectious complication among immunodeficient patients. In liver transplant recipients, the cumulative incidence of post-transplantation CMV end-organ disease (pneumonia, colitis, hepatitis, retinitis, and gastritis) at 10 years was 4.9% [3]. In allogeneic hematopoietic stem cell transplantation patients, the incidence of CMV end-organ disease was 15–25% [4].
One of the most common settings of CMV colitis, other than the classical immunodeficiency conditions, is inflammatory bowel disease (IBD). The prevalence of CMV disease in IBD ranges from 1.5 to 4.5% [5, 6]. Among IBD patients, CMV is found more commonly in ulcerative colitis (UC) than in Crohn’s disease. A prevalence as high as 40% was found within UC patients, with the highest prevalence during episodes of acute severe colitis [7•, 8, 9].
CMV colitis is rarely encountered in immunocompetent hosts. In a meta-analysis, Galiatsatos et al. [10] showed that 36% of critically ill immunocompetent patients in intensive care unit (ICU) had CMV end-organ disease. The mean age of immunocompetent patients with CMV disease was stated to range between 64 and 75 years and most patients had underlying comorbidities, such as chronic kidney disease, diabetes, or cardiomyopathy [11, 12]. The in-hospital mortality of patients with CMV colitis, probably affected by these comorbidities, was 71.4% despite treatment [11].
Risk Factors
Immunodeficiency is the principal risk factor for CMV colitis. CMV colitis has been described in patients infected with human immunodeficiency virus (HIV), in patients who underwent solid organ transplants, or in patients with malignancy. Among pediatric acute lymphoblastic leukemia patients, CMV disease, including colitis, was associated with periods of prolonged lymphopenia [13]. Lymphopenia was also a risk factor for CMV invasive infection in solid organ transplants [14].
In IBD, risk factors that were associated with CMV colitis were older age [8], shorter IBD disease duration [15], and in acute severe colitis, a higher endoscopic score [9] and pancolitis [16]. Immunosuppression also has a significant role in IBD. High doses of systemic corticosteroids were found to be an independent risk factor for CMV-associated colitis in patients with active UC [9, 16]. Other studies also confirmed previous findings regarding the association of other immunomodulators (i.e., thiopurines and methotrexate) but not anti-TNF agents with CMV disease in patients with IBD [17, 18].
Several risk factors for CMV colitis were recognized in the immunocompetent population. Ko et al. [19] reported certain conditions, including renal, neurologic, and rheumatologic diseases, ICU admission and exposure to antibiotics, antacids, steroids, or blood transfusions, to be associated with CMV colitis. Among these, steroid use and blood transfusion were identified as independent risk factors for CMV colitis. In addition, higher mortality rate was shown in patients over 55 years of age with comorbidities such as diabetes or chronic kidney disease. Among immunocompetent infants, although breastfeeding is not contraindicated, it has been suggested that breastmilk may play a role in acquiring CMV infection including colitis [20, 21].
Clinical Features
Symptoms of CMV colitis are nonspecific. It has been commonly described as incorporating mild-to-severe symptoms of colitis, such as diarrhea, rectal bleeding, fever, abdominal pain, weight loss, and up to colonic perforation [12, 19]. Ko et al. [19] reported hematochezia and diarrhea to be the two most frequently observed symptoms. Patients with CMV colitis had lower WBC counts, hemoglobin, and albumin levels compared to controls [19], as well as thrombocytopenia [22]. In a case series comprised of 23 cases of invasive CMV enterocolitis among young immunocompetent children [20], patients have been shown to have marked leukocytosis and thrombocytosis. Clinical symptoms tended to show watery or bloody diarrhea, with a mean 13-day-symptom duration.
In IBD, the symptoms of CMV colitis tend to mimic IBD exacerbation and include abdominal pain, anorexia, malaise, nausea, vomiting, diarrhea, and bleeding [5]. Colonic perforation, although uncommon (about 1% of cases), is a potentially fatal complication in these patients.
In a meta-analysis [15], Zhang et al. found that CMV-positive patients (by PCR or IHC) presented with significantly higher susceptibility to severe colitis, pancolitis, and colectomy. Prolonged hospitalization [8] and the presence of fever [7•] were also associated with CMV colitis in IBD.
The patients with CMV colitis do not present, however, with the classical symptoms of CMV viremia (such as pharyngitis, lymphadenopathy, and splenomegaly). CMV is a potential cause of steroid resistance in IBD, with a resistance rate as high as 70% in CMV-positive IBD patients compared to a rate of 35% in CMV-negative IBD patients [23]. Among the pediatric UC population, Cohen et al. showed higher prevalence of CMV-positivity in patients who required colectomy within 12 months of hospitalization for acute severe colitis [24•].
Whether CMV colitis is associated with higher risk of mortality is not clear [25, 26]. Zhang et al. [25] reported that the odds of in-hospital mortality for an IBD patient with CMV disease or infection was seven times higher compared with an IBD patient without CMV, while Grossberg et al. [26] showed only a trend toward higher in-hospital mortality among hospitalized patients with ulcerative colitis complicated by CMV. Nevertheless, this association, if exists, does not imply causality, i.e., CMV could only be a marker of more severe or refractory UC and not the trigger.
Endoscopic Findings
Generally, endoscopic findings of CMV colitis are nonspecific. The only significant independent endoscopic findings of CMV colitis are ulcerations with a well-defined, punched-out appearance [16, 27]. The prevalence of mucosal ulcerations is high, 70–80% and over [19, 28]. Irregular ulceration and a cobblestone-like appearance are also associated with CMV colitis [29]. Histologically, the number of CMV inclusion bodies was reportedly significantly higher in patients with punched-out lesions [29]. Infrequently, CMV colitis manifests as toxic megacolon with pseudomembrane formation or ischemic colitis [30, 31]. Two recent case reports also showed CMV colitis to be misdiagnosed as a rectal malignancy, described as an inflammatory tumor-like mass, in an immunocompetent patient [31, 32]. Therefore, diagnosis requires histological evaluation of biopsy tissue, preferably taken from the base and edge of the ulcers [33]. It is important to note, however, that since CMV colitis may only be seen in the right colon, diagnosis may not be possible with an incomplete colonoscopy. In gastrointestinal graft-versus-host-disease (GVHD), an ulcer in the cecum, especially in the ileocecal valve, was reported as a specific endoscopic finding of CMV colitis [28].
Diagnosis
Blood serology for CMV has no diagnostic value for CMV colitis since the seroprevalence of CMV within the adult population is high (at least 40% seropositive) [34]. In a localized infection, the tissue may contain higher CMV viral concentration than found within the blood. Blood serology could have potential benefits, such as identifying patients who are at risk of acquiring a new CMV infection (seronegative) or reactivation (seropositive) [3]. However, serology cannot replace invasive endoscopic procedures for pathological confirmation of CMV colitis.
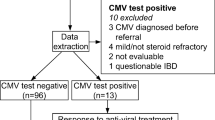
Hematoxylin and eosin (H&E) staining has the ability to show the typical viral inclusions commonly associated with CMV colitis (“owl eye appearance” inclusions, Fig. 1). If present, this histological appearance is highly specific for CMV. However, the H&E method has been shown to have a lower sensitivity compared to immunohistochemistry (IHC) and tissue polymerase chain reaction (PCR) [8, 36]. “Atypical inclusions” are described as smaller infected cells with basophilic inclusions that are up to twice the size of their non-infected neighbors and do not have the classic halo appearance, especially within patients that have concomitant IBD (Fig. 1) [33, 37]. Therefore, it has been stated that if GI biopsy from transplant patients contains gland apoptosis, even without viral inclusions, CMV IHC should be performed [38]. An alternative explanation for low sensitivity of H&E staining could be due to the rarity of finding these inclusion bodies within the relatively small amount of tissue biopsied [36].
a Hematoxylin eosin–stained slide at a high power showing cytomegalic cells containing basophilic intranuclear inclusion bodies (asterisk) and cells with a thickened nuclear membrane and smaller granular intracytoplasmic inclusions (number sign). b Immunohistochemical staining cytomegalovirus (CMV) at a high power highlighting CMV-infected endothelial cells. (From Baniak N. et al. Arch Pathol Lab Med [35]; used with permission)
The gold standard for detection of CMV in GI mucosal biopsies is CMV-specific IHC, labeling CMV antigen in infected cells [27, 33, 39]. IHC should be performed in any clinical suspicion or consistent findings in the H&E staining. The inclusions in IHC tend to be nuclear, occasionally cytoplasmic, mainly within endothelial cells. Zidar et al. [33] showed that no positive cells in IHC had been found within tissues not infected with CMV. This study showed the density of positive cells determined by IHC to correlate with the number of viral copies determined by PCR, as opposed to an earlier study that found IHC only variably agrees with viral load levels [27]. However, IHC seems to be particularly useful for isolated infected cells, and so should be considered when there is only mild active inflammation [37].
Whereas quantitative plasma PCR implies for diagnosis of systemic infection, PCR in the colonic tissue has been shown to be more sensitive than IHC, and guidelines of the European Crohn’s and Colitis organization (ECCO) recommend diagnosing CMV colitis in IBD patients using PCR in GI biopsy tissue [40]. This method is fast, objective, and highly standardized [12]. However, using PCR for diagnosis of CMV colitis is controversial [33]. One source of controversy is related to the difference between fresh and formalin-fixed, paraffin-embedded tissue (FFPE) when performing PCR. Fresh tissue is often hard to obtain in clinical practice. Mills shows that CMV PCR on FFPE GI biopsies complements IHC [27], and therefore can be used instead of fresh tissue. Another aspect to consider is that CMV remains latent within leukocytes after a primary infection, meaning, a positive result does not necessarily indicate an active infection due to very high sensitivity. McCoy et al. [34] showed that PCR increased sensitivity to detect CMV in observed prior histologically negative biopsies from patients with subsequent positive CMV colitis. Hence, the use of PCR has been suggested when IHC is negative and there is a strong clinical suspicion of CMV infection [27]. However, there is still a need to define a cut-off for PCR within GI biopsies [12]. A mucosal viral load greater than 103 copies/105 cells was associated with refractoriness to treatment [41], whereas a viral load of 250 copies/mg of tissue was shown to be a predictor of steroid-resistant disease [42].
Furthermore, there is a need to develop noninvasive molecular tests for diagnosis of CMV colitis. PCR for CMV in stool may become the noninvasive diagnostic test of choice [1]. Either way, high index of suspicion is needed for diagnosis of CMV colitis in immunocompromised as well as immunocompetent patients.
Management
The drug of choice for CMV colitis in adults is oral or intravenous ganciclovir (5 mg/kg twice daily) [43, 44]. ECCO guidelines suggest that after 3–5 days of intravenous ganciclovir, a transition can be made to oral valganciclovir (900 mg/twice daily) for the remainder of the 2–3-week course [40]. Within pediatric patients, it is recommended to use 14–21 days of parenteral ganciclovir, as an early switch to oral treatment could promote CMV reactivation [13]. Foscarnet may be used as an alternative when the patient has gained resistance or intolerance [44]. Combination of antiviral therapy with granulocyte and monocyte adsorptive apheresis (GMAA) within renal transplant recipients decreased the therapeutic duration of CMV infection without any adverse effects [45].
Whether medical treatment is necessary for immunocompetent patients is debatable. Antiviral medications have considerable side effects, such as myelosuppression, central nervous system disorders, hepatotoxicity, and nephrotoxicity [30]. However, untreated CMV disease is associated with higher morbidity and mortality. It has been suggested that an immunocompetent patient should only be given antiviral treatment if it is a male over 55 years old or if the patient has comorbidities that affect the immune system, such as diabetes or chronic renal insufficiency [43]. Still, many reports have described a rapid clinical improvement after starting therapy [7•, 20, 30]. Therefore, a common practice is to treat immunocompetent patients who have severe CMV colitis, at least until further studies can be done [30].
Conclusions
CMV is a common infection in the general population, and a relatively common end-organ infectious complication in immunocompromised patients. In UC patients, it is associated with severe colitis in both children and adults and often leads to deterioration in their clinical outcome. A high index of suspicion is needed, and once diagnosis is made, treatment should be highly considered to improve the outcome of these severely ill patients. Noninvasive diagnostic tests will be available in the near future and will hopefully improve the care of patients with CMV colitis.
Abbreviations
- CMV:
-
Cytomegalovirus
- IBD :
-
inflammatory bowel disease
- UC:
-
ulcerative colitis
- ICU :
-
intensive care unit
- HIV:
-
human immunodeficiency virus
- GVHD:
-
graft-versus-host-disease
- H&E:
-
hematoxylin and eosin
- IHC:
-
immunohistochemistry
- PCR:
-
polymerase chain reaction
- FFPE:
-
formalin-fixed, paraffin-embedded tissue
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Goodman AL, Murray CD, Watkins J, Griffiths PD, Webster DP. CMV in the gut: a critical review of CMV detection in the immunocompetent host with colitis. Eur J Clin Microbiol Infect Dis. 2015;34(1):13–8.
Yerushalmy-Feler A, Kern-Isaacs S, Cohen S. CMV infection in pediatric IBD. Curr Gastroenterol Rep. 2018;20(4):13.
Liu PY, Cheng SB, Lin CC, Lin CH, Chang SN, Cheng CY, et al. Cytomegalovirus disease after liver transplantation: a nationwide population-based study. Transplant Proc. 2014;46(3):832–4.
Bhutani D, Dyson G, Manasa R, Deol A, Ratanatharathorn V, Ayash L, et al. Incidence, risk factors, and outcome of cytomegalovirus viremia and gastroenteritis in patients with gastrointestinal graft-versus-host disease. Biol Blood Marrow Transplant. 2015;21(1):159–64.
Bontà J, Zeitz J, Frei P, Biedermann L, Sulz MC, Vavricka SR, et al. Cytomegalovirus disease in inflammatory bowel disease: epidemiology and disease characteristics in a large single-centre experience. Eur J Gastroenterol Hepatol. 2016;28:1329–34.
do Carmo AM, Santos FM, Ortiz-Agostinho CL, Nishitokukado I, Frota CS, Gomes FU, et al. Cytomegalovirus infection in inflammatory bowel disease is not associated with worsening of intestinal inflammatory activity. PLoS One. 2014;9(11):e111574.
• Levin A, Yaari S, Stoff R, Caplan O, Wolf DG, Israeli E. Diagnosis of Cytomegalovirus infection during exacerbation of ulcerative colitis. Digestion. 2017;96(3):142–8. This study provides a clinical model to detect the presence of CMV infection in patients hospitalized with UC exacerbation.
Gauss A, Rosenstiel S, Schnitzler P, Hinz U, Rehlen T, Kadmon M, et al. Intestinal cytomegalovirus infection in patients hospitalized for exacerbation of inflammatory bowel disease: a 10-year tertiary referral center experience. Eur J Gastroenterol Hepatol. 2015;27(6):712–20.
Lee HS, Park SH, Kim SH, Kim J, Choi J, Lee HJ, et al. Risk Factors and clinical outcomes associated with Cytomegalovirus colitis in patients with acute severe ulcerative colitis. Inflamm Bowel Dis. 2016;22(4):912–8.
Galiatsatos P, Shrier I, Lamoureux E, Szilagy A. Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts. Dig Dis Sci. 2005;50:609–16.
Siciliano RF, Castelli JB, Randi BA, Vieira RD, Strabelli TMV. Cytomegalovirus colitis in immunocompetent critically ill patients. Int J Infect Dis. 2014;20:71–3.
Bernard S, Germi R, Lupo J, Laverrière MH, Masse V, Morand P, et al. Symptomatic cytomegalovirus gastrointestinal infection with positive quantitative real-time PCR findings in apparently immunocompetent patients: a case series. Clin Microbiol Infect. 2015;21(12):1121.e1-e7.
Jain R, Trehan A, Mishra B, Singh R, Saud B, Bansal D. Cytomegalovirus disease in children with acute lymphoblastic leukemia. Pediatr Hematol Oncol. 2016;33(4):239–47.
Nierenberg NE, Poutsiaka DD, Chow JK, Cooper J, Price LL, Freeman RB, et al. Pretransplant lymphopenia is a novel prognostic factor in CMV and non-CMV invasive infection after liver transplantation. Liver Transpl. 2014;20(12):1497–507.
Zhang WX, Ma CY, Zhang JG, He F, Liu QM, Cheng A, et al. Effects of cytomegalovirus infection on the prognosis of inflammatory bowel disease patients. Exp Ther Med. 2016;12(5):3287–93.
Hirayama Y, Ando T, Hirooka Y, Watanabe O, Miyahara R, Nakamura M, et al. Characteristic endoscopic findings and risk factors for cytomegalovirus-associated colitis in patients with active ulcerative colitis. World J Gastrointest Endosc. 2016;8(6):301–9.
McCurdy JD, Jones A, Enders FT, Killian JM, Loftus EV, Smyrk TC, et al. A model for identifying cytomegalovirus in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2015;13(1):131–7.
Shukla T, Singh S, Tandon P, McCurdy JD. Corticosteroids and thiopurines, but not tumor necrosis factor antagonists, are associated with cytomegalovirus reactivation in inflammatory bowel disease: a systematic review and meta-analysis. J Clin Gastroenterol. 2017;51(5):394–401.
Ko JH, Peck KR, Lee WJ, Lee JY, Cho SY, Ha YE, et al. Clinical presentation and risk factors for Cytomegalovirus colitis in immunocompetent adult patients. Clin Infect Dis. 2015;60(6):e20–6.
Sue PK, Salazar-Austin NM, McDonald OG, Rishi A, Cornish TC, Arav-Boger R. Cytomegalovirus enterocolitis in immunocompetent young children: a report of two cases and review of the literature. Pediatr Infect Dis J. 2016;35(5):573–6.
Novakova V, Hamprecht K, Müller AM, Arellano-Galindo J, Ehlen M, Horneff G. Severe postnatal CMV colitis with an extensive colonic stenosis in a 2-month-old male immunocompetent term infant infected via breast milk. J Clin Virol. 2014;59(4):259–63.
Durand CM, Marr KA, Arnold CA, Tang L, Durand DJ, Avery RK, et al. Detection of cytomegalovirus DNA in plasma as an adjunct diagnostic for gastrointestinal tract disease in kidney and liver transplant recipients. Clin Infect Dis. 2013;57(11):1550–9.
Wu XW, Wu L, Ji HZ, Wang FY. Relationship between cytomegalovirus infection and steroid resistance in inflammatory bowel disease: a meta-analysis. Dig Dis Sci. 2015;60(11):3203–8.
• Cohen S, Martinez-Vinson C, Aloi M, et al. Cytomegalovirus infection in pediatric severe ulcerative colitis-a multicenter study from the Pediatric Inflammatory Bowel Disease Porto Group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. Pediatr Infect Dis J. 2018;37(3):197–201. This article is the largest cohort of children with UC and CMV.
Zhang C, Krishna SG, Hinton A, Arsenescu R, Levine EJ, Conwell DL. Cytomegalovirus-related hospitalization is associated with adverse outcomes and increased health-care resource utilization in inflammatory bowel disease. Clin Transl Gastroenterol. 2016;7(3):e150.
Grossberg LB, Ezaz G, Grunwald D, Cohen J, Falchuk KR, Feuerstein JD. A national survey of the prevalence and impact of cytomegalovirus infection among hospitalized patients with ulcerative colitis. J Clin Gastroenterol. 2018 Mar;52(3):241–5.
Mills AM, Guo FP, Copland AP, Pai RK, Pinsky BA. A comparison of CMV detection in gastrointestinal mucosal biopsies using immunohistochemistry and PCR performed on formalin-fixed, paraffin-embedded tissue. Am J Surg Pathol. 2013;37(7):995–1000.
Matsuda K, Ono S, Ishikawa M, Miyamoto S, Abiko S, Tsuda M, et al. Cecum ulcer is a reliable endoscopic finding in cytomegalovirus colitis concomitant with graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2018;97(5):877–83.
Yang H, Zhou W, Lv H, Wu D, Feng Y, Shu H, et al. The association between CMV viremia or endoscopic features and histopathological characteristics of CMV colitis in patients with underlying ulcerative colitis. Inflamm Bowel Dis. 2017;23(5):814–21.
Hasegawa T, Aomatsu K, Nakamura M, Aomatsu N, Aomatsu K. Cytomegalovirus colitis followed by ischemic colitis in a non-immunocompromised adult: a case report. World J Gastroenterol. 2015;21(12):3750–4.
Jacob S, Zayyani NR. Cytomegalovirus colitis masquerading as rectal malignancy in an immunocompetent patient. Indian J Pathol Microbiol. 2015;58(1):80–2.
Chidlovskii E, Deroux A, Bernard S, Couturier P. Cytomegalovirus colitis mimicking rectal carcinoma in an immunocompetent elderly woman. BMJ Case Rep. 2016. https://doi.org/10.1136/bcr-2016-214694
Zidar N, Ferkolj I, Tepeš K, Štabuc B, Kojc N, Uršič T, et al. Diagnosing cytomegalovirus in patients with inflammatory bowel disease—by immunohistochemistry or polymerase chain reaction? Virchows Arch. 2015;466(5):533–9.
McCoy MH, Post K, Sen JD, Chang HY, Zhao Z, Fan R, et al. qPCR increases sensitivity to detect cytomegalovirus in formalin-fixed, paraffin-embedded tissue of gastrointestinal biopsies. Hum Pathol. 2014;45(1):48–53.
Baniak N, Kanthan R. Cytomegalovirus colitis: an uncommon mimicker of common Colitides. Arch Pathol Lab Med. 2016;140(8):854–8.
Tandon P, James P, Cordeiro E, Mallick R, Shukla T, McCurdy JD. Diagnostic accuracy of blood-based tests and histopathology for cytomegalovirus reactivation in inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis. 2017;23(4):551–60.
Yan Z, Wang L, Dennis J, Doern C, Baker J, Park JY. Clinical significance of isolated Cytomegalovirus-infected gastrointestinal cells. Int J Surg Pathol. 2014;22(6):492–8.
Wong NACS. Gastrointestinal pathology in transplant patients. Histopathology. 2015;66(4):467–79.
Juric-Sekhar G, Upton MP, Swanson PE, Westerhoff M. Cytomegalovirus (CMV) in gastrointestinal mucosal biopsies: should a pathologist perform CMV immunohistochemistry if the clinician requests it? Hum Pathol. 2017;60:11–5.
Rahier JF, Magro F, Abreu C, Armuzzi A, Ben-Horin S, Chowers Y, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohn's Colitis. 2014;8(6):443–68.
Ciccocioppo R, Racca F, Paolucci S, Campanini G, Pozzi L, Betti E, et al. Human cytomegalovirus and Epstein-Barr virus infection in inflammatory bowel disease: need for mucosal viral load measurement. World J Gastroenterol. 2015;21(6):1915–26.
Roblin X, Pillet S, Oussalah A, Berthelot P, Del Tedesco E, Phelip JM, et al. Cytomegalovirus load in inflamed intestinal tissue is predictive of resistance to immunosuppressive therapy in ulcerative colitis. Am J Gastroenterol. 2011;106(11):2001–8.
Fyock C, Gaitanis M, Gao J, Resnick M, Shah S. Gastrointestinal CMV in an elderly, immunocompetent patient. R I Med J. 2014;97(6):53–6.
Jones A, McCurdy JD, Loftus EV, Bruining DH, Enders FT, Killian JM, et al. Effects of antiviral therapy for patients with inflammatory bowel disease and a positive intestinal biopsy for Cytomegalovirus. Clin Gastroenterol Hepatol. 2015;13(5):949–55.
Naganuma T, Takemoto Y, Iwai T, Kuwabara N, Uchida J, Nakatani T, et al. Effects of granulocyte and monocyte adsorptive apheresis in renal transplantation recipients with concomitant Cytomegalovirus infection. Transplant Proc. 2016;48(3):929–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by anyof the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Intra-Abdominal Infections, Hepatitis and Gastroenteritis
Rights and permissions
About this article
Cite this article
Yerushalmy-Feler, A., Padlipsky, J. & Cohen, S. Diagnosis and Management of CMV Colitis. Curr Infect Dis Rep 21, 5 (2019). https://doi.org/10.1007/s11908-019-0664-y
Published:
DOI: https://doi.org/10.1007/s11908-019-0664-y