Abstract
Purpose
The optimal method for detecting CMV colitis in patients with inflammatory bowel disease (IBD) has not been established. We wanted to investigate which diagnostic test would be most accurate when defining CMV colitis rather by the further clinical course than by using another diagnostic modality.
Methods
All consecutive patients with moderately or severely active IBD who had been tested for CMV by PCR, histology, or antigenemia assay at the two campuses CBF and CCM of the Charité - Universitätsmedizin Berlin between September 2006 and September 2009 were included in this retrospective study. During that time, in patients with a positive CMV test, immunosuppressive treatment of any kind was immediately reduced and antiviral treatment was started. This allowed identifying patients who responded to antiviral treatment and those who only responded to later escalation of immunosuppressive therapy.
Results
One hundred and nine patients were identified, out of whom nine were considered to have clinically relevant CMV colitis. Sensitivity and specificity were 1 and 0.94 for CMV PCR and 0.5 and 1 for pp65 antigen immunofluorescence assay from peripheral blood, 0.67 and 0.98 for immunohistochemistry, and 0.17 and 0.98 for hematoxylin-eosin staining. When using absence of leukocytosis, splenomegaly, and steroid refractory disease as clinical parameters to test for CMV colitis, blood CMV PCR and immunohistochemistry were able to exclude CMV colitis in negative patients with a 75% likelihood of positive patients to have clinically relevant CMV colitis.
Conclusions
Blood-based CMV PCR together with simple clinical parameters can exclude clinically relevant CMV colitis at a high specificity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) and ulcerative colitis (UC) are inflammatory bowel diseases (IBD). Treatment with immunosuppressive drugs predisposes IBD patients to opportunistic infections, cytomegalovirus (CMV) infection being one of them. CMV colitis as a complication in patients with UC has been associated with active disease, immunosuppressive medication, steroid treatment, and especially steroid refractory disease progression [1, 2]. Depending on the definition of CMV colitis/disease and the diagnostic modality employed, the prevalence of CMV in severe or refractory colitis is estimated to be between 21 and 36% [3,4,5,6].
Currently, there is considerable uncertainty about the clinical relevance of CMV infection in IBD patients. Some studies were able to show a particularly bad prognosis for IBD patients tested positive for CMV [3, 4, 7]. In addition, antiviral treatment reduced the number of patients that needed colectomy for medical treatment failure [8, 9]. On the other hand, these results were not always reproducible as the disease course in other studies was independent from treatment with antiviral drugs [10, 11].
The lack of a gold standard for diagnosing CMV colitis in IBD patients is most likely the reason for this discrepancy. During treatment with immunosuppressive drugs, subclinical reactivation of CMV (“CMV infection” according to the terminology used by the European Crohn’s and Colitis organization (ECCO) as well as the American Society of Transplantation) occurs frequently and must be distinguished from CMV colitis [7, 11, 12]. The American Society of Transplantation defined definite gastrointestinal CMV disease in recipients of solid organ transplantation on the other hand as gastrointestinal disease plus detection of CMV in gastrointestinal tissue [12]. We cannot apply this definition to IBD patients since intestinal inflammation is a hallmark of IBD itself. According to the ECCO consensus, the optimal method for detecting clinically relevant CMV infection in patients with colitis has not been established [7]. Therefore, it is still unclear which subpopulation of IBD patients with CMV replication might benefit from antiviral treatment [8, 13, 14].
In this study, we aimed to determine if common diagnostic tests for CMV are able to detect those IBD patients that needed antiviral treatment by analyzing patients ex post in order to see if their disease responded to antiviral treatment instead of intensified immunosuppression. We wanted to calculate statistical measures of these tests. Finally, we propose a clinical algorithm for identifying IBD patients with CMV colitis in need of antiviral treatment.
Methods
Study population
This retrospective study was conducted at the Campus Benjamin Franklin and Campus Charité Mitte of the Charité - Universitätsmedizin Berlin. Patients with the International Classification of Diseases (ICD) 10 diagnoses K50 or K51 who had a diagnostic test for CMV between September 2006 and September 2009 were included.
During that time, diagnosis and therapy of CMV colitis in IBD patients followed a very structured approach: All patients presenting with moderately severe to severe symptoms or with a steroid refractory course of ulcerative colitis or colitis Crohn were tested for CMV with at least one peripheral blood test as well as histology where feasible. This blood test was mostly CMV PCR in plasma. Some patients were also tested for antigenemia. Histology always included hematoxylin and eosin staining (H&E) as well as immunohistochemistry in most patients. In all patients who had at least one “owls’s eye cell” in H&E staining, had at least one positive cell in immunohistochemistry, had at least 2 positive cells/200,000 in the antigenemia assay, or more than 750 IU of CMV DNA/ml plasma in the polymerase chain reaction (PCR), glucocorticoids were immediately reduced (≤ 20 mg prednisolone) and patients were started on antiviral medication (ganciclovir 5 mg/kg body weight bid). After 3 to 5 days, treatment response was evaluated. Patients responding to therapy or in remission continued to receive antiviral treatment. Otherwise, antiviral medication was discontinued and immunosuppressive therapy was escalated. After that time, we changed our standard protocol, acknowledging that CMV colitis and active IBD could be present concurrently.
Inclusion criteria for this study were (1) diagnosis of IBD with colonic involvement (UC, colitis Crohn or unclassified IBD) at least 3 months prior to CMV testing; (2) CMV testing with at least one of the following methods: CMV PCR in patient plasma or in intestinal biopsies, pp65-antigenaemia testing in patients’ blood, immunohistochemistry or H&E staining in intestinal biopsies; (3) patients presented with an either moderately severe to severe flare or a steroid refractory disease. Severity of colitis was defined by applying a pragmatic definition that differed slightly from the definitions by ECCO. We included patients with a partial Mayo score (PMS) of at least 6 for UC and unclassified colitis or a Harvey-Bradshaw Index (HBI) of more than 10 for CD. Steroid refractory was defined as a lack of response (i.e., a drop of at least 3 or 4 in the PMS or the HBI, respectively) after 5 days of treatment or a lack of remission (PMS of less than 3 or HBI of less than 7) after 14 days of steroid treatment at a dose of at least 0.75 mg prednisolone/kg body weight or 60 mg/day.
Patients with CMV testing at first diagnosis or in other hospitals as well as patients with concomitant severe immunosuppressive disease (e.g., human immunodeficiency virus infection, malignancy) were excluded from the study. Furthermore, we had to exclude cases with lack of follow-up.
We used the term “antimetabolites” for thiopurines and methotrexate and “immunosuppressant” or “immunosuppressive drugs” for all drugs with immunosuppressive properties including glucocorticoids, antimetabolites, calcineurin inhibitors, and TNF antibodies. Migration inhibitors or IL-23 blockers were not used in our study population.
Gold standard
Within the evaluated period, all patients received treatment in accordance with the German and European clinical practice guidelines [21, 22]. The optimal method for detecting clinically relevant CMV infection in patients with colitis has not been established [15]. Since no diagnostic method as of now has been shown to have at least close to 100% sensitivity and specificity, no true gold standard exists for CMV colitis in IBD patients. According to the ECCO consensus on opportunistic infections in IBD, “immunomodulator therapy is often associated with subclinical reactivation of latent CMV infection. This reactivation is usually asymptomatic, or characterised by a mild, self-limited course. Serious tissue damage is very rare. It is appropriate to draw a distinction between CMV infection (detectable by serology or viral DNA), and CMV disease (such as colitis, causing end-organ damage)” [7]. In the absence of a gold standard for the diagnosis of a clinically relevant CMV colitis, we used the clinical course in order to differentiate clinically relevant CMV colitis from merely subclinical reactivation. Two independent gastroenterologists assessed each patient according to the following criteria: response to antiviral treatment, response to immunosuppressive medication, and further clinical course after discharge. During that time in our department, we adhered to a strict treatment protocol, which mandated immediate reduction of immunosuppressive drugs and initiation of an antiviral drug as soon as CMV was detected by histology, PCR, or antigenemia assay. Immunosuppressive treatment was only escalated if the patient did not respond to antiviral treatment after 3 to 5 days. Since antiviral treatment was not combined with an increase in immunosuppressive treatment, we were able to assess the response to each treatment modality separately. Patients, who responded to antiviral treatment, were defined to have CMV colitis (CMV disease). We therefore labeled all patients, who did not respond to antiviral treatment but rather to the increased anti-inflammatory treatment, applied thereafter as “subclinical reactivation.” The latter patients, together with all patients in whom no CMV was detected, constituted the control group.
Diagnostic methods
Polymerase chain reaction
The real-time PCR for the detection of CMV-DNA targets the US17 gene. Primers and probes were described elsewhere [16]. The nucleic acid was extracted from EDTA plasma using the QIAamp DNA Mini Kit (Qiagen, Germany) according to the manufacturer’s instructions. To assess an increased sensitivity (95% detection limit is 330 IU/ml), all reactions were controlled for presence of inhibiting factors by the use of an internal co-amplified DNA. Quantitative results were given in international units per milliliter.
Antigenemia
The antigenemia assay (CMV pp65 antigenemia immunofluorescence assay (IFA), CINA kit, Argene, France) detects the CMV lower-matrix protein pp65 (UL83) by immunofluorescence staining of infected polymorphonuclear leukocytes. Quantitative results are expressed as the number of CMV-infected polymorphonuclear leukocytes per number of 200,000 cells; pp65 IFA was considered positive with 2 positive/200,000 cells.
Histology
After fixing the biopsies in buffered formalin and embedding them in paraffin, serial sections (2–3 μm) were stained with H&E for histological examination. For immunohistochemistry, 4-μm-thick sections were deparaffinized and subjected to a heat-induced epitope retrieval step before incubation with the anti-CMV antibody (clones CCH2 and DDG9, Dako, Hamburg, Germany; dilution 1:20). Antibody clone CCH2 reacts with an early nuclear protein identical with the non-structural DNA-binding protein p52 and clone DDG9 reacts with an intermediate early nuclear protein. For detection, the alkaline phosphatase-anti-alkaline phosphatase complex (APAAP) method was used. Conventional histology and immunohistochemistry were considered positive, when one positive cell was present. For quantification of immunohistochemistry, the number of inclusions in each biopsy fragment was counted as described in Jones et al. [8].
Calculation of diagnostic parameters and statistics
Measures of diagnostic accuracy (sensitivity, specificity, positive and negative predictive values as well as likelihood ratios) were calculated using standard formulas. 95% confidence intervals for sensitivity and specificity as well as positive and negative predictive values were calculated with the efficient-score method (corrected for continuity) by using VassarStats Clinical Research Calculators (http://vassarstats.net/). Since some of the 95% confidence intervals for likelihood ratios were 0 or infinite, those were calculated using a bootstrapping approach in R 3.5.1 using the bootLR package BayesianLR.test( ) function [17, 18].
Statistical analysis was performed with IBM SPSS Statistics Version 24. Statistical significance was determined with Fisher’s exact test for dichotomous and the Student t test for continuous variables. Probability values p ≤ 0.05 were considered statistically significant.
Construction of a clinical algorithm
For construction of the clinical algorithm, it was postulated that a 75% likelihood of CMV colitis would be sufficient for initiating antiviral treatment. Due to a lack of reliable data, a “test-treatment” threshold could not be calculated. The threshold was therefore reached by consensus in the study group. The percentage of CMV disease patients being positive for a combination of different clinical parameters was calculated for all permutations of predictors with an odds ratio larger than 10. The combination of predictors with the highest percentage of patients with clinically relevant CMV colitis was then used to assess post-test likelihood for different cutoff values for CMV PCR. We restricted possible cutoff values to full or 0.5 log10 levels as the variation of test values between different laboratories can be up to 0.5 log10 IU/ml [19].
Results
Population characteristics
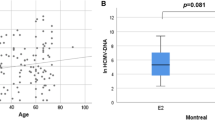
One hundred and nine out of the 314 patients reviewed met the study criteria (Fig. 1). Demographics and clinical characteristics of the population are shown in Table 1. The prevalence of patients with UC was higher than that with CD. Age as well as duration of the disease was typical for a tertiary care center. About two thirds of the population received immunosuppressive therapy.
Sixteen of the included patients tested positive for CMV in one of the tests employed. Nine (8% of all patients) were classified as having “clinically relevant CMV colitis” (CMV disease); the remaining seven (7% of all patients) were classified as “subclinical reactivation” based on the criteria described in the “Methods” section. These patients, together with the 93 patients that tested negative for CMV, constituted the reference group. The 1-year colectomy rate among the patients with CMV colitis was 38% versus 17% among the patients with subclinical reactivation.
When comparing the two groups, several clinical findings stand out (Table 2). While 89% of all patients with CMV colitis were classified as steroid refractory, only 3% from the control group were refractory to steroids. Regarding clinical characteristics, splenomegaly was more frequent in CMV colitis patients. CMV colitis patients presented more often fever, weight loss, and elevated CRP compared with the control group while leukocytosis was not observed in patients with CMV colitis. Anemia was present in more than 50% of the patients in both groups. Prior to CMV testing, the CMV colitis patients had been treated more often with steroids. In particular, patients with ≥ 40 mg of prednisolone per day were overrepresented. Moreover, significantly more CMV colitis patients had been treated with immunosuppressants compared to the control group.
CMV PCR was on average 78,299 IU/ml in the population with CMV colitis and 3863 IU/ml in the patients with subclinical reactivation, whereas immunohistochemistry showed on average 12.8 inclusions in the patients with CMV colitis and 1.5 in the group with subclinical reactivation.
Accuracy of diagnostic tests
We calculated sensitivity and specificity, positive and negative predictive values, and likelihood ratio (Table 3) for CMV PCR and pp65-antigenaemia testing from blood samples as well as H&E staining and immunohistochemistry from tissue samples. Since CMV PCR from intestinal biopsies and CMV-antibody titers had not been determined regularly, we could not calculate measures of diagnostic accuracy for these methods.
CMV PCR in patient plasma had the highest sensitivity with 100%, with a very high specificity of 94%. All analyzed assay methods appeared specific for CMV, but their sensitivity varied distinctly. As would be expected, the sensitivity of CMV detection in H&E stained histology was low. The sensitivity of immunohistochemistry was markedly higher (71%) with wide margins of error since immunohistochemistry was only performed in the 39% of patients where the endoscopist or pathologist requested it due to heightened suspicion.
Clinical algorithm
Next, we aimed to determine under which circumstances IBD patients should be treated with antiviral substances. On one hand, antiviral medication, namely ganciclovir and foscarnet, can have detrimental side effects and reducing immunosuppressive therapy might worsen IBD symptoms. On the other hand, untreated CMV colitis had been shown to result in colectomy in a significant number of patients. We postulated that a 75% likelihood of CMV colitis would be sufficient for initiating antiviral treatment. We wanted to construct a diagnostic algorithm with easy application in clinical practice. We therefore decided to not use different weighting of parameters but rather apply an equal weight of 1 to each predictor. When combining the clinical parameters, steroid refractory course, splenomegaly, and absence of leukocytosis, the likelihood of CMV colitis was 14.8%. We then calculated likelihood ratios for different cutoff values for the CMV PCR (Table 4). By using a cutoff of 1000 IU/ml plasma for CMV PCR, corresponding to a positive likelihood ratio of 17.2 in our population, a positive CMV PCR would result in a post-test probability of 75%. With the negative likelihood ratio being 0, this effectively rules out CMV colitis in all patients with either no clinical finding or a negative CMV PCR. Only 3% of all patients in our population would have been misclassified as positive. When we added positive immunohistochemistry defined as more than 5 signals per biopsy (high-grade positive, as suggested before) to our model, this did not change the results of our model [8]. Peripheral blood diagnostics have been claimed to have a too low sensitivity and several studies have already shown the diagnostic value of quantifying immunohistochemistry [8, 20,21,22]. Based on these findings, we suggest a clinical algorithm using clinical parameters together with two highly specific tests (Fig. 2).
Discussion
In this retrospective study, we determined the value of different diagnostic methods and clinical signs as well as laboratory findings for CMV infection in IBD. One hundred and nine patients could be included in our study, of whom 16 patients (15%) tested positive for CMV, yet only nine were classified as clinically relevant CMV colitis according to the prior defined criteria. This corresponds with a rate of 8.3% clinically relevant CMV colitis cases in our population. All other patients were considered to have merely a flare of their IBD disease with or without subclinical reactivation of CMV. Our retrospective approach allowed us to consider response to antiviral therapy as an indicator of patients in whom a positive test result did actually indicate clinically relevant CMV colitis.
The two groups studied had different characteristics: CMV colitis patients showed higher incidence of fever, splenomegaly, and severe weight loss, as well as higher CRP levels. We did not see lymphadenopathy, which has been previously described as typical for CMV colitis, in any of our patients. The IBD flare patients had significantly more leukocytosis.
We compared four different CMV tests regarding their diagnostic accuracy. In our study, the CMV PCR with a sensitivity of 100% and 94% specificity yielded the best results. The test proved to be valid and given its high negative predictive value, a negative CMV-PCR test excluded the diagnosis of CMV colitis in our IBD patients. Because of the low prevalence of CMV colitis, the positive predictive value was only 64%.
Immunohistochemistry and pp65-antigen testing were both highly specific but had a high false negative rate. In the case of the pp65 antigen, this might be partially explained by the low numbers of pp65 testing in our study population. The diagnostic accuracy of conventional H&E is very low due to its low sensitivity.
The most striking difference between this study and other studies that evaluated blood-based tests for CMV in IBD patients is the lower prevalence of patients which were finally deemed to have clinically relevant CMV colitis as compared to earlier studies [13, 23,24,25]. The prevalence of course is dependent on the population. Some of these studies included primarily patients with steroid refractory disease. In that population, clinically relevant CMV colitis has a higher prevalence [26, 27]. Other studies considered every patient with a positive signal in tissue CMV PCR as having CMV colitis [24, 28]. Low levels of CMV DNA in colonic biopsy though have been shown to be a poor marker for clinically relevant CMV colitis [29, 30].
CMV PCR in general can be unspecific. Also, detection of CMV in peripheral blood has been claimed to lack sensitivity, because it does not necessarily detect replication in the colon [13]. Yet due to the low prevalence of CMV colitis, the specificity of 95% in our study translates to a very high positive predictive value. In line, previous data from kidney and liver transplant as well as HIV patients had shown that sensitivity of blood-based CMV PCR is also very high [31, 32]. Also, there is a high correlation between immunohistochemistry and blood-based PCR in patients with IBD [20].
A recent systematic review performed a meta-analysis of blood-based tests to detect CMV colitis [13]. In that meta-analysis, the authors found sensitivity and specificity of blood-based PCR to be 60.0% and 100%. The low sensitivity might be explained by the fact that many of the included studies again used detection of any CMV DNA by PCR in the tissue as their gold standard. This can lead to a high number of false-positive patients due to a low specificity in the employed gold standard [29, 30].
Recently, a different model for selecting patients with a high likelihood of CMV colitis on the basis of clinical parameters had been published [33]. The authors used refractory disease, antimetabolite exposure, and age in their predictive model. Similarly, in our population, a steroid refractory was able to discriminate patients with clinically relevant CMV colitis from patients without CMV disease. In our population, age on the other hand did not turn out to be a statistically significant predictor.
Most studies did not discriminate in their CMV-positive cases between clinically relevant CMV disease and subclinical CMV reactivation. The differentiation between these two entities in daily practice is often difficult but essential, since different treatment strategies are required [1, 9].
By analyzing response to antiviral therapy, our analysis allowed for distinction between CMV colitis versus asymptomatic reactivation. We therefore suggest that this is the first study that applied a valid gold standard in order to calculate sensitivity and specificity.
This study was a retrospective study; hence, notes of the treating physicians were used to classify disease severity. We tried to compensate for this deficiency by using standardized scores. Due to a lack of follow-up, we had to exclude two patients. Also, not all clinical signs or laboratory values were documented in every patient. Nevertheless, all relevant analyses were performed on > 90% of the total study population. Due to the completeness of data combined with the robustness of the sensitivity analysis, a relevant systematic error can be excluded.
A pre-test screening of patients regarding their clinical presentation, and here in particular the steroid refractory course and absence of leukocytosis, as well as splenomegaly, could help to lower the number of false positives.
Based on our study population, a clinical algorithm can be established that ensures antiviral treatment in almost all patients with clinically relevant CMV colitis without exposing too many patients to a treatment with high potential of side effects (see Fig. 2). All patients presenting at least a moderately severe flare with a steroid refractory course, splenomegaly, or absence of leukocytosis and showing either more than 1000 IU/ml plasma in a CMV PCR or more than four signals in CMV immunohistochemistry per biopsy should receive antiviral treatment. This approach should not miss any cases of CMV colitis while overtreating only a very small number of patients.
Our data indicate that IBD patients with colitis and systemic signs of inflammation, steroid-refractory disease, fever, splenomegaly, or a lack of leukocytosis have a high pre-test probability for CMV colitis. In these patients, CMV testing seems essential. Therefore, not every available test has the same validity. As previously shown for other diseases, in our study in plasma of IBD patients, CMV PCR had the highest sensitivity and specificity of all analyzed methods. We found a strong correlation between the amount of CMV DNA in the plasma and the diagnosis CMV colitis. Nevertheless, a few CMV colitis patients had low systemic CMV replication. In patients without CMV colitis, CMV PCR is usually below a threshold of 1000 IU/ml. Therefore, a patient with active colitis, characteristic clinical symptoms, and a clear positive finding in either of these diagnostic tests should be treated with antiviral medication.
In order to be readily applicable in clinical practice, this approach of course needs to be validated in a separate cohort prospectively.
References
Pillet S, Pozzetto B, Roblin X (2016) Cytomegalovirus and ulcerative colitis: place of antiviral therapy. World J Gastroenterol 22:2030–2045. https://doi.org/10.3748/wjg.v22.i6.2030
Siegmund B (2017) Cytomegalovirus infection associated with inflammatory bowel disease. Lancet Gastroenterol Hepatol 2:369–376. https://doi.org/10.1016/S2468-1253(16)30159-5
Cottone M, Pietrosi G, Martorana G, Casa A, Pecoraro G, Oliva L, Orlando A, Rosselli M, Rizzo A, Pagliaro L (2001) Prevalence of cytomegalovirus infection in severe refractory ulcerative and Crohn’s colitis. Am J Gastroenterol 96:773–775. https://doi.org/10.1111/j.1572-0241.2001.03620.x
Domènech E, Vega R, Ojanguren I, Hernández Á, Garcia-Planella E, Bernal I, Rosinach M, Boix J, Cabré E, Gassull MA (2008) Cytomegalovirus infection in ulcerative colitis: a prospective, comparative study on prevalence and diagnostic strategy. Inflamm Bowel Dis 14:1373–1379. https://doi.org/10.1002/ibd.20498
Maher MM, Nassar MI (2009) Acute cytomegalovirus infection is a risk factor in refractory and complicated inflammatory bowel disease. Dig Dis Sci 54:2456–2462. https://doi.org/10.1007/s10620-008-0639-6
Criscuoli V, Casà A, Orlando A, Pecoraro G, Oliva L, Traina M, Rizzo A, Cottone M (2004) Severe acute colitis associated with CMV: a prevalence study. Dig Liver Dis 36:818–820. https://doi.org/10.1016/j.dld.2004.05.013
Rahier JF, Magro F, Abreu C, Armuzzi A, Ben-Horin S, Chowers Y, Cottone M, de Ridder L, Doherty G, Ehehalt R, Esteve M, Katsanos K, Lees CW, Macmahon E, Moreels T, Reinisch W, Tilg H, Tremblay L, Veereman-Wauters G, Viget N, Yazdanpanah Y, Eliakim R, Colombel JF, European Crohn's and Colitis Organisation (ECCO) (2014) Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis 8:443–468. https://doi.org/10.1016/j.crohns.2013.12.013
Jones A, McCurdy JD, Loftus EV et al (2015) Effects of antiviral therapy for patients with inflammatory bowel disease and a positive intestinal biopsy for cytomegalovirus. Clin Gastroenterol Hepatol 13:949–955. https://doi.org/10.1016/j.cgh.2014.09.042
Shukla T, Singh S, Loftus EV et al (2015) Antiviral therapy in steroid-refractory ulcerative colitis with cytomegalovirus: systematic review and meta-analysis. Inflamm Bowel Dis 21:2718–2725. https://doi.org/10.1097/MIB.0000000000000489
Delvincourt M, Lopez A, Pillet S, Bourrier A, Seksik P, Cosnes J, Carrat F, Gozlan J, Beaugerie L, Roblin X, Peyrin-Biroulet L, Sokol H (2014) The impact of cytomegalovirus reactivation and its treatment on the course of inflammatory bowel disease. Aliment Pharmacol Ther 39:712–720. https://doi.org/10.1111/apt.12650
Matsuoka K, Iwao Y, Mori T, Sakuraba A, Yajima T, Hisamatsu T, Okamoto S, Morohoshi Y, Izumiya M, Ichikawa H, Sato T, Inoue N, Ogata H, Hibi T (2007) Cytomegalovirus is frequently reactivated and disappears without antiviral agents in ulcerative colitis patients. Am J Gastroenterol 102:331–337. https://doi.org/10.1111/j.1572-0241.2006.00989.x
Humar A, Michaels M, on behalf of the AST ID Working Group on Infectious Disease Monitoring (2006) American Society of Transplantation recommendations for screening, monitoring and reporting of infectious complications in immunosuppression trials in recipients of organ transplantation. Am J Transplant 6:262–274. https://doi.org/10.1111/j.1600-6143.2005.01207.x
Tandon P, James P, Cordeiro E, Mallick R, Shukla T, McCurdy JD (2017) Diagnostic accuracy of blood-based tests and histopathology for cytomegalovirus reactivation in inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 23:551–560. https://doi.org/10.1097/MIB.0000000000001073
Kopylov U, Papamichael K, Katsanos K, Waterman M, Bar-Gil Shitrit A, Boysen T, Portela F, Peixoto A, Szilagyi A, Silva M, Maconi G, Har-Noy O, Bossuyt P, Mantzaris G, Barreiro de Acosta M, Chaparro M, Christodoulou DK, Eliakim R, Rahier JF, Magro F, Drobne D, Ferrante M, Sonnenberg E, Siegmund B, Muls V, Thurm T, Yanai H, Dotan I, Raine T, Levin A, Israeli E, Ghalim F, Carbonnel F, Vermeire S, Ben-Horin S, Roblin X (2017) Impact of infliximab and cyclosporine on the risk of colectomy in hospitalized patients with ulcerative colitis complicated by cytomegalovirus—a multicenter retrospective study. Inflamm Bowel Dis 23:1605–1613. https://doi.org/10.1097/MIB.0000000000001160
Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, Burisch J, Gecse KB, Hart AL, Hindryckx P, Langner C, Limdi JK, Pellino G, Zagórowicz E, Raine T, Harbord M, Rieder F, for the European Crohn’s and Colitis Organisation [ECCO] (2017) Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis 11:649–670. https://doi.org/10.1093/ecco-jcc/jjx008
Storch GA, Buller RS, Bailey TC, Ettinger NA, Langlois T, Gaudreault-Keener M, Welby PL (1994) Comparison of PCR and pp65 antigenemia assay with quantitative shell vial culture for detection of cytomegalovirus in blood leukocytes from solid-organ transplant recipients. J Clin Microbiol 32:997–1003
R Core Team (2018) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org/
Marill KA, Chang Y, Wong KF, Friedman AB (2017) Estimating negative likelihood ratio confidence when test sensitivity is 100%: a bootstrapping approach. Stat Methods Med Res 26:1936–1948. https://doi.org/10.1177/0962280215592907
Rychert J, Danziger-Isakov L, Yen-Lieberman B, Storch G, Buller R, Sweet SC, Mehta AK, Cheeseman JA, Heeger P, Rosenberg ES, Fishman JA (2014) Multicenter comparison of laboratory performance in cytomegalovirus and Epstein-Barr virus viral load testing using international standards. Clin Transpl 28:1416–1423. https://doi.org/10.1111/ctr.12473
Zagórowicz E, Bugajski M, Wieszczy P, Pietrzak A, Magdziak A, Mróz A (2016) Cytomegalovirus infection in ulcerative colitis is related to severe inflammation and a high count of cytomegalovirus-positive cells in biopsy is a risk factor for colectomy. J Crohns Colitis 10:1205–1211. https://doi.org/10.1093/ecco-jcc/jjw071
Nguyen M, Bradford K, Zhang X, Shih DQ (2011) Cytomegalovirus reactivation in ulcerative colitis patients. Ulcers 2011:1–7. https://doi.org/10.1155/2011/282507
Kuwabara A, Okamoto H, Suda T, Ajioka Y, Hatakeyama K (2007) Clinicopathologic characteristics of clinically relevant cytomegalovirus infection in inflammatory bowel disease. J Gastroenterol 42:823–829. https://doi.org/10.1007/s00535-007-2103-3
Lawlor G, Moss AC (2010) Cytomegalovirus in inflammatory bowel disease: pathogen or innocent bystander? Inflamm Bowel Dis 16:1620–1627. https://doi.org/10.1002/ibd.21275
Gauss A, Rosenstiel S, Schnitzler P, Hinz U, Rehlen T, Kadmon M, Ehehalt R, Stremmel W, Zawierucha A (2015) Intestinal cytomegalovirus infection in patients hospitalized for exacerbation of inflammatory bowel disease: a 10-year tertiary referral center experience. Eur J Gastroenterol Hepatol 27:712–720. https://doi.org/10.1097/MEG.0000000000000361
Kandiel A, Lashner B (2006) Cytomegalovirus colitis complicating inflammatory bowel disease. Am J Gastroenterol 101:2857–2865. https://doi.org/10.1111/j.1572-0241.2006.00869.x
Yoshino T, Nakase H, Ueno S, Uza N, Inoue S, Mikami S, Matsuura M, Ohmori K, Sakurai T, Nagayama S, Hasegawa S, Sakai Y, Chiba T (2007) Usefulness of quantitative real-time PCR assay for early detection of cytomegalovirus infection in patients with ulcerative colitis refractory to immunosuppressive therapies. Inflamm Bowel Dis 13:1516–1521. https://doi.org/10.1002/ibd.20253
Yang H, Zhou W, Lv H, Wu D, Feng Y, Shu H, Jin M, Hu L, Wang Q, Wu D, Chen J, Qian J (2017) The association between CMV viremia or endoscopic features and histopathological characteristics of CMV colitis in patients with underlying ulcerative colitis. Inflamm Bowel Dis 23:814–821. https://doi.org/10.1097/MIB.0000000000001095
Kim JW, Boo S-J, Ye BD, Kim CL, Yang SK, Kim J, Kim SA, Park SH, Park SK, Yang DH, Jung KW, Kim KJ, Byeon JS, Myung SJ, Kim JH (2014) Clinical utility of cytomegalovirus antigenemia assay and blood cytomegalovirus DNA PCR for cytomegaloviral colitis patients with moderate to severe ulcerative colitis. J Crohns Colitis 8:693–701. https://doi.org/10.1016/j.crohns.2013.12.014
Roblin X, Pillet S, Oussalah A, Berthelot P, del Tedesco E, Phelip JM, Chambonnière ML, Garraud O, Peyrin-Biroulet L, Pozzetto B (2011) Cytomegalovirus load in inflamed intestinal tissue is predictive of resistance to immunosuppressive therapy in ulcerative colitis. Am J Gastroenterol 106:2001–2008. https://doi.org/10.1038/ajg.2011.202
Ciccocioppo R, Racca F, Paolucci S, Campanini G, Pozzi L, Betti E, Riboni R, Vanoli A, Baldanti F, Corazza GR (2015) Human cytomegalovirus and Epstein-Barr virus infection in inflammatory bowel disease: need for mucosal viral load measurement. World J Gastroenterol 21:1915–1926. https://doi.org/10.3748/wjg.v21.i6.1915
Durand CM, Marr KA, Arnold CA, Tang L, Durand DJ, Avery RK, Valsamakis A, Neofytos D (2013) Detection of cytomegalovirus DNA in plasma as an adjunct diagnostic for gastrointestinal tract disease in kidney and liver transplant recipients. Clin Infect Dis 57:1550–1559. https://doi.org/10.1093/cid/cit521
Beaugerie L, Cywiner-Golenzer C, Monfort L, Girard PM, Carbonnel F, Ngô Y, Cosnes J, Rozenbaum W, Nicolas JC, Châtelet FP, Gendre JP (1997) Definition and diagnosis of cytomegalovirus colitis in patients infected by human immunodeficiency virus. J Acquir Immune Defic Syndr Hum Retrovirol 14:423–429
McCurdy JD, Jones A, Enders FT et al (2015) A model for identifying cytomegalovirus in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 13:131–137. https://doi.org/10.1016/j.cgh.2014.05.026
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
BS received a research grant from Pfizer; served as consultant for Falk, Janssen, MSD, Abbvie, Celgene, Lilly, Takeda, Pfizer, and Hospira; and received lecture fees from Abbvie, Falk, Ferring, Janssen, MSD, Merck, and Takeda; all money went to the Charité - Universitätsmedizin Berlin, Germany. JCP served as a consultant for MSD, Pfizer, Takeda, and Biogen and received lecture fees from Vifor, Falk, Janssen, Abbvie, Pfizer, MSD, and Takeda. The other authors declare that they have no conflict of interest.
Informed consent
For this study, formal consent was not required.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee (approval number EA4/092/09) and with the 1964 Helsinki declaration and its later amendments.
Rights and permissions
About this article
Cite this article
Kredel, L.I., Mundt, P., van Riesen, L. et al. Accuracy of diagnostic tests and a new algorithm for diagnosing cytomegalovirus colitis in inflammatory bowel diseases: a diagnostic study. Int J Colorectal Dis 34, 229–237 (2019). https://doi.org/10.1007/s00384-018-3170-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3170-z