Abstract
The predictive value of vascular biomarkers such as pulse wave velocity (PWV), central arterial pressure (CAP), and augmentation index (AIx), obtained through pulse wave analysis (PWA) in resting conditions, has been documented in a variety of patient groups and populations. This allowed to make appropriate recommendations in clinical practice guidelines of several scientific societies. Due to advances in technologies, largely operator-independent methods are currently available for estimating vascular biomarkers also in ambulatory conditions, over the 24 h. According to the acceptable accuracy and reproducibility of 24-h ambulatory PWA, it appears to be a promising tool for evaluating vascular biomarkers in daily life conditions. This approach may provide an opportunity to further improve the early cardiovascular screening in subjects at risk. However, concerning the clinical use of PWA over the 24 h in ambulatory conditions at the moment, there is no sufficient evidence to support its routine clinical use. In particular, long-term outcome studies are needed to show the predictive value of 24-h PWV, CAP, and AIx values, provided by these devices, over and beyond peripheral blood pressure, and to answer the many technical and clinical questions still open. To this regard, the VASOTENS Registry, an international observational prospective study recently started, will help providing answers on a large sample of hypertensive patients recruited worldwide.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arterial damage is mainly an effect of ageing and elevated blood pressure (BP), and can be non-invasively assessed through the measurement of arterial stiffness, central arterial pressure (CAP), and pulse wave reflections [1]. Pulse wave velocity (PWV), namely carotid-femoral PWV (cfPWV), is considered as the clinical “gold standard” measurement for determination of arterial stiffness, has the largest amount of epidemiological evidence for its predictive value for cardiovascular (CV) events, and requires moderate technical expertise [2–4]. Pulse wave analysis (PWA) allows to obtain information on CAP and wave reflections, thus on augmentation index (AIx). Pulse wave should be optimally obtained either at the central level, at the site of the ascending aorta or the carotid artery, or directly recorded or computed from a peripheral artery waveform using a transfer function analysis.
Introduction of applanation tonometry allowed arterial stiffness and central hemodynamics to be assessed non-invasively, and extended the more limited data that were obtained invasively with diagnostic cardiac catheterization [2, 4]. Tonometry is widely employed, though the recent introduction of techniques combining brachial cuff measurements and analysis of pulse waveform have made the assessment largely operator-independent and allowed to extend the evaluation of arterial functional state to ambulatory conditions [2, 4]. These new and less operator-dependent methods may provide an opportunity for the spread of arterial stiffness measurements and to further refine the CV risk stratification.
In the present review, we will briefly summarize the current status of the scientific evidence on the prognostic and clinical value of PWV, CAP, and AIx obtained through PWA. We will then specifically focus our attention on the presentation of the technologies currently used to determine the 24-h profile of arterial stiffness and wave reflections and on the evidence collected so far, supporting their use.
PWA Techniques
The most accurate assessment of vascular biomarkers such as PWV, CAP, and AIx is obtained invasively at the ascending aorta, using high fidelity pressure transducers, measuring pressure directly at the tip (or at two tips, in case of PWV measurement) of the catheter. However, such a technique is not feasible for daily use in the clinic or in the population. Therefore, non-invasive approaches which can be used to record a pulse waveform and then run a PWA are preferable. To this regard, various techniques are available (Table 1). The pulse waveform can be recorded non-invasively by applanation tonometry, pressure sensors, oscillometry, or cuff-based techniques applied to the brachial artery, multi-signal techniques, or a volume-clamped photoplethysmographic device on the finger [2, 4, 5]. The BP waveform can also be acceptably derived by ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI). The vascular parameters are then estimated by signal processing of the recorded waveform, based on mathematical transformation.
cfPWV through applanation tonometry is the most commonly used clinical parameter of arterial stiffness [2, 6]. PWV represents the speed at which the pressure waveform travels (wave propagation) along the aorta and large arteries, during each cardiac cycle. Pressure waveforms are obtained transcutaneously over the common carotid artery and the femoral artery, and the time delay between the feet of the two recorded waveforms is measured (foot-to-foot method). The distance covered by the waves is taken as the distance measured between the two recording sites multiplied by 0.8 [6]. PWV is calculated as the ratio between the distance (in meters) and the time delay (in seconds). Earlier techniques involved synchronization with the ECG signal and a sequential measurement of the carotid and femoral pulse wave, whereas modern techniques with simultaneous recording of the waves at two sites helped improve the accuracy of cfPWV determination by reducing the influence of its variability over time. In contrast to PWV, CAP and AIx are influenced not only by arterial stiffness but also by the intensity of wave reflections and may be considered as clinical surrogate endpoints, as further discussed in this paper. CAP and AIx can be estimated either from the common carotid or from a peripheral artery (radial, brachial or femoral) waveform. In case the waveform is taken at the carotid artery level, no mathematical processing is needed, but only calibration, since this artery is considered itself a central artery. In case of peripheral artery, the local waveform is recorded and then the aortic waveform is computed using a transfer function or proprietary algorithms or mathematical modeling [7].
CAP is the pressure measured at the level of the central large arteries preferably defined at the root of the aorta: its systolic component is lower than the corresponding brachial one because arterial stiffness and wave reflections increase moving away from the heart (amplification phenomenon) [8]. AIx represents the extra pressure caused by pressure wave reflection back from the periphery and thus it is the parameter showing the magnitude of wave reflection relative to primary pressure waves. It is usually defined as the ratio of the difference between the second (reflected wave) and first (initial wave) systolic peak and pulse pressure (PP), expressed as a percentage. It is influenced not only by arterial stiffness, but mostly by both intensity and timing of waves reflection upon their arrival at the heart, though it has been suggested that the reflected pressure is only a small contributor to overall pressure when the aortic reservoir (Frank’s Windkessel) is accounted for [9].
Figure 1 depicts how PWV, CAP, and AIx are identified and computed on the reconstructed central pulse waveform.
Method of computation or central hemodynamic and wave reflection indices through pulse wave analysis. a A peripheral waveform is recorded (e.g., from the brachial artery). b This waveform is analyzed by a mathematical algorithm based on a transfer function, with a certain amplitude and phase characteristics. c The central waveform is then reconstructed. From this waveform, central systolic (SBP) and diastolic blood pressure (DBP), and pulse pressure (PP) are derived. The systolic peak defines the central arterial systolic pressure (CASP). The augmentation index (AIx) is computed as the ratio between the augmentation pressure (AP, the difference between the reflected wave, P1, and the forward wave, P2) and PP, expressed as a percentage. d Pulse wave velocity (PWV) may be computed according to the foot-to-foot method for example of carotid-femoral PWV (cfPWV) by multiplying the carotid-femoral distance (ΔL) by 0.8 and dividing the result by the time interval (Δt) between the foot of the carotid and femoral waveform. e Alternatively, for ambulatory estimation, PWV may be derived by multiplying the surrogate length of the aorta (ΔL, jugulum-symphisis distance or superficial morphological distance corresponding to the projection of the aorta on the body surface) by 2 and by a constant (k) and by dividing the result by the reflected wave transit time (RWTT, the time interval between the forward and the reflected wave)
Predictive Value of Arterial Stiffness, CAP, and Wave Reflections for Cardiovascular Events
As previously mentioned, ageing and high BP are associated with large artery stiffening and damage. The close relationship between increased PWV, CAP, and AIx, and CV outcome and the predictive value of arterial stiffness, central pressure, and wave reflections have been shown in a variety of patient groups and populations.
Two large meta-analyses of longitudinal studies clearly demonstrated that PWV is a robust and independent predictor of all-cause and CV mortality, fatal and non-fatal coronary events, and fatal strokes; thus, it can be considered as an intermediate or surrogate endpoint for CV events. A first meta-analysis by Vlachopoulos and coworkers [10] was based on 17 longitudinal studies that evaluated PWV and followed up 15,877 subjects for a mean of 7.7 years. In this study, the relative risks for total CV events, CV mortality, and all cause mortality, after adjustment for traditional risk factors, were 2.26 (95 % confidence interval, 1.89, 2.70), 2.02 (1.68, 2.42), and 1.90 (1.61, 2.24), respectively, for high vs. low aortic PWV subjects (Fig. 2). Interestingly, the risk of total CV events and CV mortality was significantly higher in high baseline risk groups compared with low-risk subjects. An individual participant meta-analysis of prospective data from 16 studies including 17,635 subjects has documented that a 1-SD increase in aortic PWV is associated with a 35 % age- and sex-adjusted increased risk of coronary heart disease, a 54 % risk of stroke, and a 30 % risk of CV disease [11]. There was no evidence that the increased risk associated with PWV was modified by sex, smoking status, population type, concomitant diabetes, hypertension, or renal function. However, PWV was more strongly related to the risk of CV events in younger participants (Fig. 3). Adding PWV to the risk model based on classic risk factors had only modest effect on the risk prediction of coronary events and strokes when the whole population was studied, but the risk prediction was strongly improved by 13 % when the subjects with intermediate risk were considered.
Relative risk (RR) and 95 % confidence interval (CI) of total cardiovascular (CV) events (a), CV mortality (b), and all-cause mortality (c) for a 1-SD increase in aortic pulse wave velocity (PWV) [redrawn with permission from 10]
Hazard ratio (and 95 % confidence interval, CI) for cardiovascular (CV) events for a 1-SD increase in aortic pulse wave velocity (PWV) in subgroups of subjects [redrawn with permission from 11]
A limited number of prospective studies explored the predictive value of CAP and AIx, either measured directly on carotid artery or estimated on the basis of applanation tonometry performed on radial artery coupled with PWA. A meta-analysis of such 11 original studies with a good quality was performed by Vlachopoulos and coworkers [12]. In 5648 subjects followed for an average of 45 months, the adjusted increase in the risk of total CV events for an increase of central systolic BP (SBP) of 10 mmHg, central PP of 10 mmHg, and central AIx of 10 % was 9, 14, and 32 %, respectively (Fig. 4). Five studies comparing the risk of clinical events with both central and brachial PP revealed that central PP is associated with a marginally but not significantly (p = 0.057) higher risk of clinical events (+32 %) than brachial PP (+19 %), whereas the risk estimates for central and peripheral SBP were similar (+14 vs. +20 %, p = 0.062).
Relative risk (RR) and 95 % confidence interval (CI) of total cardiovascular (CV) events for a 10-mmHg increase in central systolic blood pressure (SBP), a 10-mmHg increase in central pulse pressure (PP), and a 10 % increase in augmentation index (AIx) [redrawn with permission from 12]
Although several longitudinal studies and meta-analyses suggested that CAP, arterial stiffness, and wave reflection may be predictive of CV events, unequivocal proof has yet to be provided that their improvement or regression after intervention is predictive of the reduction in CV events, independently of brachial BP lowering. A study conducted in 150 patients with end-stage renal disease followed up for 51 months provided the first and only available evidence that PWV is an independent predictor of mortality. In this study, the absence of PWV decrease in response to BP reduction was a significant predictor of all-cause and CV mortality, demonstrating that at least in this population aortic stiffness is a good surrogate endpoint for CV prognosis and that its attenuation is predictive of the reduction in CV outcomes [13]. The impact of improving aortic stiffness on CV mortality, coronary events, and stroke remains to be established in other populations, particularly those with hypertension, which might be at lower but still high CV risk. Similarly, the CAFE study showed that CAP was lower than brachial BP in patients treated with the amlodipine plus perindopril combination than in those treated with atenolol plus bendroflumethiazide, despite similar reduction in brachial BP [14]. The former dual drug combination resulted superior in terms of prevention of CV morbidity and mortality, suggesting that the lower CAP achieved during treatment might be part of the explanation of this finding.
Recommendations of Current Guidelines on the Clinical Use of PWA-Derived Vascular Biomarkers
cfPWV is the clinical “gold standard” for estimating aortic stiffness [2–4]. As detailed in the previous section, the evidence that PWV, and particularly cfPWV, is an important independent predictor of CV disease is more consistent and stronger than for CAP and even more so for AIx.
According to current European Society of Cardiology (ESC)/European Society of Hypertension (ESH) guidelines [3, 4], a cfPWV >10 m/s may indicate asymptomatic organ damage. cfPWV is useful for stratification of total CV risk and should be considered for hypertensives, whereas can add predictive value to the usual risk estimate of diabetics (Table 2). A scientific statement from the American Heart Association (AHA) also recommends that arterial stiffness should be determined non-invasively by measurement of cfPWV (class of recommendation, I; level of evidence, A) and emphasizes that single-point estimates of PWV require evidence for their predictive value in longitudinal studies [15].
Although reference values for CAP have been recently published, at the moment in Europe or in America there is no specific practical recommendation on the use of CAP and AIx and more data are required before these vascular biomarkers can be recommended for routine use in hypertension in general [3, 4, 16]. ESC/ESH guidelines suggest that CAP and AIx might be helpful when assessing young patients with isolated systolic hypertension (Table 2).
Interestingly, only Taiwanese guidelines recommend the measurement of CAP obtained non-invasively with either tonometry-based or cuff-based techniques with a cutoff value of 130/90 mmHg when a diagnosis of hypertension is clinically suspected but cannot be established by current conventional BP criteria (class of recommendation, IIb; level of evidence, B). These recommendations and thresholds were based on two independent Taiwanese cohorts studies using an outcome-driven approach [17].
Finally, concerning the clinical use of 24-h ambulatory PWA at the moment, there is no sufficient evidence to support its routine clinical use. However, its usability confers a great potential for 24-h PWA techniques, once they are validated in prospective studies.
PWA over the 24 h: Available Technologies
Few techniques and devices are currently available for simultaneous monitoring of peripheral BP, CAP, and arterial stiffness in ambulatory conditions over the 24 h. Main characteristics of the various devices are summarized in Table 3. A description of the methodologies employed by each individual device to obtain vascular parameters is reported in the next sections.
Mobil-O-Graph PWA
This device obtains pulse waves with a conventional upper arm BP cuff. Following inflation to a diastolic brachial pressure level, the device acquires the pulse waveform over 10 s through a high fidelity pressor sensor [21]. The sensor is connected to a 12-bit A/D converter by means of an active analogue band pass filter. After digitalization, a three-stage signal processing is used to confirm signal quality. At the end of this process, an aortic pulse wave is generated by means of a generalized transfer function (ARCSolver) and this is used to compute vascular parameters. The ARCSolver method uses the late systolic peak and a transfer function-like method to convert brachial into central pressure. To estimate aortic PWV, this method utilizes parameters from PWA combined into a proprietary mathematical model, coupled with information on age and CAP [27].
BPLab
Another cuff-based device for 24-h PWA is the BPLab monitor. During a step-by-step deflation of an upper arm cuff, brachial pulse wave forms are obtained from oscillograms, digitalized and stored in the device memory. Thereafter, signal processing is performed using a special mathematical algorithm, which is based on a specially developed transfer function that utilizes a modification in a certain frequency range within the acquired pulse signal to derive the aortic pressure wave. The modulus and phase characteristics of the Vasotens transfer function have been published previously [31]. The algorithm used for estimating PWV is also proprietary and close to methods of wave separation and timing, where the difference in time between the first wave and the second wave (i.e., the reflected wave) correlates to the distance, according to the manufacturer’s instructions. CAP and AIx are derived from the analysis of the reconstructed central pulse wave.
BPro
This wristwatch-like device acquires the radial pressure waveform through automated radial tonometry (EVBP, EVidence-Based blood Pressure tonometry) at a frequency of 60 Hz [35, 36]. A single radial waveform is averaged from individual waveforms recorded consecutively for 10 s per block of waveforms. From the radial waveform, the software estimates CAP using an N-point moving average method, a mathematical low pass filter. This method is designed to accurately derive CAP and does not generate an aortic waveform. Although in one validation study AIx could be computed from radial waveform, this parameter and PWV are not provided by the device and are not available in the marketed model [38].
Arteriograph 24
The Arteriograph 24 is a device using a brachial cuff-based technique involving pressurization to 35–40 mmHg above SBP to occlude the brachial artery for a period of 2 min. The pulsatile waveform is recorded from the brachial artery through a high fidelity pressor sensor. The first systolic peak of the recorded waveform corresponds to the ejection of the left ventricle, whereas the second peak is assumed to be the reflection of the first pressure wave from the periphery. The difference in time between the first and the second (reflected wave) is related to the measured distance from the sternal notch to the pubic symphysis, resulting in PWV [43, 50]. The AIx corresponds to the pressure difference between the first and second wave in relation to the PP [43, 50]. The calculation of systolic CAP is based on the relationship between invasively measured SBP in the aorta and in the brachial artery, on the basis of the late systolic wave amplitude [50].
Diasys Integra II
This is an oscillometric BP monitor that measures Q wave to Korotkoff Delay (QKD), which is considered as a surrogate of arterial stiffness. The non-invasively acquired brachial BP is used for calibration and for estimation of CAP through a regression equation which also takes into account HR, height, and QKD [53, 54].
Oscar 2
The Oscar 2 device records the brachial waveform through an upper arm cuff which is inflated 10 mmHg below the individual’s diastolic BP (DBP). This threshold for inflation pressure allows to obtain an optimal volume pulse waveform free of distortion. The waveform is calibrated to SBP and DBP by oscillometric measurement of brachial BP. Proprietary digital signal processing and transfer function (based on the SphygmoCor technique), programmed into the device, and applied to the calibrated brachial waveform, allow to estimate the aortic pressure waveform [57, 58].
Somnotouch NIBP
The Somnotouch NIBP measures beat-to-beat BP through a finger photoplethysmograph, coupled to a three-lead ECG, both connected to a watch-like control unit placed at the wrist level and equipped with a screen displaying the beat-to-beat pulse waveform [59]. The principle of BP estimation is based on the beat-to-beat determination of the pulse transit time (PTT), calculated as the interval between R-wave on ECG and the arrival of the corresponding pulse wave (determined through finger photoplethysmography signal) at the peripheral site. SBP and DBP values are calculated on the basis of the relationship between BP levels and PTT, where the increase in BP increases arterial wall tension, thus increasing its stiffness. Consequently, pulse wave propagation velocity increases, leading to a reduction in PTT. Combining this model with a single initial BP measurement at the level of the brachial artery and used for calibrating the device allows to derive beat-to-beat BP values corresponding to changing PTT.
Accuracy and Reproducibility of PWA over the 24 h
In recent years, 24-h monitoring of central hemodynamics, arterial stiffness, and wave reflections in ambulatory conditions has become available and more and more popular. Several studies validated the arterial stiffness parameters provided by these devices or technologies with respect to accuracy vs. invasive or non-invasive standards (Table 3). In most studies, measurements of PWV, CAP, and AIx were in accordance with the reference standard.
However, all studies were performed in resting conditions and no systematic analysis of the validation studies has ever been performed, except for CAP [60–62]. The cuff-based method seems to be the most promising technique, given the fact that it is affordable, convenient, and easy-to-use, allowing a potential widespread use in clinical daily practice. However, its accuracy, reliability, and clinical value need to be further elucidated in validation and outcome studies. Interestingly, in a recently published systematic review of invasive validation studies of different devices, Papaioannou and coworkers [61] showed that oscillometric devices with autocalibration function can estimate central SBP with a very high degree of accuracy [test-reference difference and 95 % confidence interval: −0.77 (−3.27, 1.73) mmHg]. When other calibration methods are used, the best approach seems to be the use of brachial mean arterial pressure and DBP (C2 method) [estimated error −2.99 (−5.76, −0.22)], rather than the more traditional brachial SBP and DBP one (C1 method) [estimated error, −7.78 (−10.28, −5.28)].
Few studies also assessed reproducibility, though in most of the cases in resting conditions and between consecutive measurements taken in a time span of few minutes: the good reproducibility of measurements at rest may not necessarily and automatically apply to those taken in ambulatory conditions. Protogerou [63] evaluated the reproducibility or 24-h ambulatory CAP taken at least 1-week apart in 30 consecutive subjects. Variation coefficients of SBP and DBP indicated acceptable reproducibility of both 24-h CAP (2.6 and 3.2 %) and 24-h brachial BP (2.7 and 3.3 %). In 31 treated or untreated hypertensives having test-retest 24-h monitoring 1-week apart, PWV and AIx were highly reproducible, with average variation coefficients of 1.5 and 11.4 %, respectively, and intraclass correlation coefficients always >0.8 [64]. Posokhov [65] tested the reproducibility of a new interesting index, the Pulse Time Index of Norm (PTIN), defined as the percentage of a 24-h period during which the PWV does not exceed the 10 m/s threshold, in 85 subjects who repeated the ambulatory blood pressure monitoring (ABPM) after 2 or more days. The 24-h PTINs were similar during the first and second recording, either in normotensive subjects (86.5 vs. 87.3 %) or in hypertensive patients (57.5 vs. 57.4 %), with excellent intraclass correlation coefficients (0.98 for normotensives and 0.95 for hypertensives) indicating good repeatability of the measure.
Clinical Evidence
As previously discussed, the most popular methods for 24-h PWA are those based on brachial oscillometry. The availability of these non-invasive operator-independent methodologies has resulted in widespread reporting of vascular parameters in diverse patient groups and disease states. However, at the moment, there is a conspicuous lack of published evidence validating each technique in clinical conditions. In particular, no studies have yet evaluated the long-term predictive ability for CV events of vascular indices such as PWV, CAP, and AIx, measured over the 24 h by ABPM. Some incomplete evidence is available from cross-sectional studies. Most of such evidence is derived from studies based on two devices, the Mobil-O-Graph and the BPLab. Results of main clinical studies are summarized in Table 4. The most relevant among these studies are discussed in the next sections.
Clinical Studies Based on the Mobil-O-Graph Device
One of the first study performed in ambulatory conditions with the Mobil-O-Graph aimed at comparing the diurnal profiles in 50 hypertensives and 50 normotensives [66]. In the whole population, systolic CAP was significantly lower than peripheral SBP either during the day (124.1 ± 15.7 vs. 133.9 ± 16.3 mmHg) or during the night (114.4 ± 14.5 vs. 121.5 ± 15.2 mmHg). The nocturnal fall in systolic CAP was lower than the peripheral SBP fall in normotensive subjects as well as in hypertensive patients. Recently, an article within the framework of the GEnotipo, Fenotipo y Ambiente de la HiperTensión Arterial en UruguaY (GEFAHT-UY) study carried out in 167 individuals confirmed that the diurnal rhythm of CAP runs in parallel with that of peripheral BP, with smaller nocturnal fall for systolic CAP [67]. Additionally, the study showed that PWV decreases from day to night (0.7 m/s), whereas AIx increases (2.3 %).
In the SAFAR Study [68, 69], both 24-h central and brachial SBP measured by the Mobil-O-Graph device were superior to conventional office BP measurements in predicting BP-related cardiac damage (left ventricular hypertrophy and left ventricular diastolic dysfunction) in 230 subjects (75 % having arterial hypertension). In the same study, 24-h ambulatory central SBP was also more closely associated with left ventricular hypertrophy than 24-h ambulatory brachial SBP (r = 0.51 vs. r = 0.40). The same authors also [70] found that ambulatory PWV provides additional information to cfPWV regarding the association of arterial stiffness with the retinal vessel calibers.
Different hypertension types have been found to be associated with different levels of ambulatory arterial stiffness and wave reflections. In 78 South African adults, those with sustained hypertension (26 % of the total sample) or masked hypertension (42 %) showed 24-h PWV (6.6 ± 0.2 and 6.8 ± 0.2 m/s) and AIx values (27.9 ± 6.0 and 26.5 ± 6.0 %) significantly higher than normotensive individuals (PWV, 5.5 ± 0.1 m/s; AIx, 23.6 ± 6.0 %) [71]. Several studies have assessed the relationship between vascular biomarkers measured in ambulatory conditions and biochemical markers of inflammation. Elsurer [72] found that in 339 hypertensive patients with chronic kidney disease (CKD), serum uric acid was significantly correlated with both 24-h PWV (r = 0.22) and AIx (r = -0.19). However, serum uric acid was independently associated with AIx only (r = −0.16 after adjustment), while this was not the case for PWV (r = −0.02 after adjustment). The same group of authors [73] demonstrated an independent and significant relationship between gamma-glutamyltransferase, a proinflammatory marker involved in the pathogenesis of CV diseases, and 24-h PWV (r = 0.14) and day-time AIx (r = 0.14), in 320 hypertensive patients. Increased serum levels of magnesium, which are often associated with elevated BP, endothelial dysfunction, insulin resistance, vascular calcification, inflammation, and atherosclerosis, were significantly and inversely correlated to 24-h AIx (r = −0.25), but not with PWV [74].
Hanssen and coworkers [75] investigated the 24-h effect of different levels of exercise in 21 young healthy male individuals, in a randomized cross-over study. Ambulatory AIx significantly declined after high-intensity interval training, but not after moderate continuous training.
A few cross-sectional studies evaluated the impact of different systemic diseases on ambulatory arterial stiffness. In two different studies, Korkmaz and coworkers documented an increased 24-h PWV in 102 patients with inflammatory bowel disease as compared to 74 matched controls, and in 58 patients with celiac disease as compared to 58 age-matched controls [76, 77]. Authors postulated that the inflammatory status associated with these two conditions may have contributed to the increased arterial stiffening, independently from CV risk factors. Hillebrand [78] observed significantly lower central SBP values during night sleep in 27 Marfan patients as compared to a similar number of healthy controls (108.0 ± 11.7 vs. 116.0 ± 14.6 mmHg). Such differences were accompanied by differences in forward and backward wave amplitudes during the night, indicating a disease effect on waves reflection. Maloberti [79] studied 19 children with Williams-Beuren syndrome, a genetic disorder involving elastin gene and adversely affecting arterial function. Sick children showed significantly higher heart rate and AIx values at night than age-matched controls (24.6 ± 13.5 vs. 16.5 ± 8.9 %), suggesting an abnormal sympathetic CV control and an increase in small arteries resistance. Yilmaz [80] examined 96 patients with Behcet’s disease, a multisystemic vasculitis involving veins and arteries of various sizes, and 60 age- and sex-matched control subjects. Non-dipping status was more common in patients than in controls (66 vs. 10 %). The percentage of patients with high AIx was also larger than that of controls (34 vs. 12 %), this suggesting that non-dipping status and arterial stiffness may exacerbate the harmful CV effects of the other.
Finally, two longitudinal studies investigated the variation of indices of wave reflections and arterial stiffness during intra- and interdialytic intervals in ESRD patients undergoing hemodialysis [81, 82]. During a 48-h monitoring, Karpetas and coworkers showed a gradual and statistically significant interdialytic increase in ambulatory CAP (from day 1, 119.2 ± 16.9 mmHg to day 2, 121.7 ± 15.1 mmHg) and AIx (from 24.7 ± 9.7 to 28.8 ± 9.8 %), whereas PWV was only slightly elevated (9.31 ± 2.2 vs. 9.39 ± 2.3 m/s) in 153 patients. Another study of the same group evaluated vascular indices with a 72-h monitoring, during the third interdialytic day compared with the second interdialytic day, showing a statistically significant increase in all indices (PWV, from 9.4 ± 2.3 to 9.6 ± 2.3 m/s; CAP, from 118.5 ± 17.1 to 123.6 ± 17.0 mmHg; AIx, from 28.8 ± 9.9 to 30.5 ± 9.9 %) and suggesting a potentially increased CV risk in these patients during interdialytic days in hemodialysis [82].
Clinical Studies Based on the BPLab Device
Few cross-sectional studies conducted in large samples of healthy subjects and hypertensive patients allowed to collect substantial, although initial, clinical evidence on the usefulness of non-invasive 24-h arterial stiffness and central hemodynamics assessment with BPLab for the assessment of the arterial function impairment in daily life conditions. Kuznetsova [83] provided age- and gender-specific reference diagnostic values for 24-h PWV, CAP, and AIx in 467 normotensive volunteers. These authors found a significant nocturnal fall of PWV and CAP in all age groups, in both sexes, and lower values of PWV in women than in men. In a recent publication, we reported on significantly higher 24-h average PWV, CAP, and AIx in 661 hypertensive (119.3 mmHg, 10.3 m/s, and 24.7 %) than in 142 normotensive controls (105.6 mmHg, 10.0 m/s, 11.0 %) [84]. We also observed a typical circadian rhythm, with CAP and PWV values lower during night sleep and AIx lower during waking hours. More recently, in the subgroup of 661 hypertensive patients, we documented a strong relationship of 24-h BP variability with CAP and arterial stiffness, which is largely independent from the average 24-h BP level [85]. Twenty-four-hour PWV was also found to be positively and significantly correlated with LVMI in 137 hypertensive patients (r = 0.32), the correlation being superior to that observed for the average 24-h SBP (r = 0.14) [86]. In the same study, the authors found a good correlation (r = −0.72) between PTIN and LVMI, indicating that PTIN may represent an interesting marker of end organ damage in hypertension. The PTIN was also employed to assess the effect of renal transplantation on arterial stiffness in 41 patients with ESRD enrolled in a longitudinal study [87]. A week after the transplantation, a decrease in the average PTIN was observed in the whole population (from 56.3 ± 18.4 to 27.6 ± 11.1 %), whereas after 20 weeks the PTIN increased again returning to pre-transplant levels (52.0 ± 23.6).
Finally, in a study including 27 patients with a combination of hypertension and chronic obstructive pulmonary disease (COPD), larger ambulatory peripheral BP and CAP were observed compared to 31 patients with isolated essential hypertension and 13 normotensive controls [88]. Interestingly, patients with hypertension and COPD displayed more often a non-dipping status (44 % based on brachial BP and 55 % based on CAP) compared to hypertension free from COPD (5 and 13 %, respectively).
Clinical Studies Based on the BPro Device
The BPro is able to provide CAP measurements during the 24 h. In a cross-sectional observational study, 24-h systolic CAP was higher in 629 diabetics than in 86 controls, and progressively and significantly increased with diabetic complications, being 114 ± 17 mmHg in healthy subjects, 115 ± 13 mmHg in patients with short diabetes duration (<10 years), 121 ± 13 mmHg in normoalbuminuric patients not receiving antihypertensive treatment, 119 ± 16 mmHg in patients with microalbuminuria, and 121 ± 13 mmHg in patients with macroalbuminuria [89]. Ambulatory CAP was more strongly associated to complications than peripheral 24-h SBP: the odds ratio per 1 SD increase in 24-h CAP were 3.19 (95 % confidence interval, 1.68, 6.05; p < 0.001) for CV disease, 4.41 (2.03, 9.57; p < 0.001) for retinopathy, and 3.25 (1.65, 6.41; p < 0.05) for autonomic dysfunction.
The BPro was also used in two longitudinal studies evaluating the effect of treatment on 24-h arterial hemodynamics and stiffness. The Ambulatory Central Aortic Pressure (AmCAP) study described a significant CAP lowering effect on both day-time (8.1 mmHg) and night-time (7.5 mmHg) with a 12-week treatment based on either aliskiren 300 mg or telmisartan 80 mg once-daily [90]. CAP also showed a typical diurnal pattern, with lower pressures at night.
However, both before and under treatment, nocturnal systolic CAP values (129.6 ± 15.1 and 122.1 ± 16.6 mmHg) were relatively lower than brachial SBP ones (136.5 ± 15.8 and 129.0 ± 17.2 mmHg), and night-time dip significantly larger when assessed by brachial BP (baseline, brachial 8.2 ± 4.4 % vs. aortic 6.9 ± 4.3 %; end of treatment, brachial 8.2 ± 4.9 % vs. aortic 6.9 ± 4.7 %). In an open prospective cohort study enrolling 44 hypertensive Asians, 12 weeks of treatment with valsartan were associated with good reduction in both office brachial SBP and 24-h systolic CAP (14.9 ± 10.7 and 15.3 ± 10.9 mmHg, respectively) [91].
Clinical Studies for Other Devices
In spite of the numerous validation studies performed at rest and the availability of prospective data, there is only one study featuring Arteriograph 24 [92]. The study enrolled 48 gout patients, of which 40.1 % had CKD, and 32 age-matched control subject. The 24-h CAP was significantly higher in gout patients compared to healthy controls. Moreover, when the gout patients with and without CKD were compared, the gout patients with CKD had significantly higher CAP and AIx than the gout patients without CKD.
As far as other previously mentioned devices are regarded, no clinical studies are available for devices based on the SphygmoCor technique (Oscar 2), for the Somnotouch device and for the Diasys Integra II. Indeed for the Diasys device, there are a number of cross-sectional and longitudinal studies, though they are based on the QKD, a surrogate of arterial stiffness for which there is no current clinical indication or recommendation by guidelines [93]. Such studies showed an independent prognostic value of this index in the hypertensive patients, whenever measured before or after the administration of antihypertensive treatment.
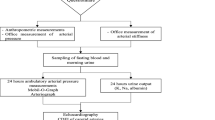
Outcome-Based Evidence for 24-h PWA: the VASOTENS Registry
An attempt to provide supporting evidence for the inclusion of 24-h PWA in routine hypertensive management will be made by the VASOTENS (Vascular health ASssesment Of The hypertENSive) Registry [94]. In this international, multicenter, observational, non-randomized, prospective study, approximately 2000 subjects referred to 20 hypertension clinics worldwide for routine diagnostic evaluation and follow-up of hypertension of any severity or stage will be recruited. Each subject will be submitted every 6 to 12 months to an ABPM performed with a BPLab monitor, which allows simultaneous assessment of brachial BP, PWV, CAP, and AIx (see above for details on the PWA technique employed by the device). On each visit, clinical data, including information on CV outcomes, will also be collected. A web-based telemedicine platform (Fig. 5) will be used in order to standardize and centralize data collection, data validation by experts and counseling to remote centers, as well as setup and maintenance of the Registry, and prompt data analysis. Subjects will be followed up for a minimum of 2 years. At the end of this period, the impact of 24-h PWA on target organ damage and CV prognosis will be evaluated and the use of the PWA electronic health (e-health) solution provided in the study will be validated for the screening of early vascular damage and the management of the hypertensive patient.
Workflow of the THOLOMEUS web-based telemedicine system used in the VASOTENS Registry. ABPM, ambulatory blood pressure monitoring; AIx, augmentation index; BP, blood pressure; CAP, central aortic pressure; e-CRF, electronic case report form; HR, heart rate; PWA, pulse wave analysis; PWV, pulse wave velocity; SaaS, software as a service; SSL, secure sockets layer [redrawn with permission from 94]
Current Advantages and Limitations of PWA Assessment over the 24 h
Advantages
Although, as detailed above, there is still limited evidence on the clinical usefulness of 24-h PWA and no recommendation on its use has yet been issued by clinical guidelines, the technique has many potential advantages for improving the management of the hypertensive patients (Table 5). All the available methods, and in particular those cuff-based, are easy to use and their accuracy is largely operator-independent. Ambulatory 24-h PWA extends the evaluation of central hemodynamics and wave reflections to daily life conditions, allowing repeated measurements to be obtained in different situations, particularly during day activities and night sleep. They make also possible to study the effect of antihypertensive treatment on the vascular function and its persistence in dynamic conditions.
The technologies are definitely more affordable and cheaper than those used in the laboratory, a feature that combined with their usability may favor the extension of their use to a broader spectrum of patients with early vascular damage, such as hypertensive patients, diabetics, and subjects at high CV risk in general.
Limitations
Although the simplicity of the technologies currently available makes evaluation of central hemodynamics and arterial stiffness feasible in daily life ambulatory conditions, further research is required before such techniques can be introduced in the routine clinical practice. Current issues are summarized in Table 5 and discussed in details in the next paragraphs.
A first issue regards the accuracy of the various techniques. Validation studies against the gold standard tonometric SphygmoCor device or intra-arterial measurements have documented strong correlation and acceptable accuracy for most of the tested non-invasive devices, although the accuracy of the estimation is device- or technique-dependent [60–62]. Regrettably, with the exception of the ARTERY guidelines for the process of validating devices measuring cfPWV [95], at the moment there are no standardized protocols for device clinical validation. Although the validation against invasive aortic BP may represent the gold standard, such an approach has the limitation of applying only to specific populations, because for ethical and practical reasons the validation can be performed exclusively in patients undergoing elective cardiac catheterization for diagnostic purposes. In addition, we do not know whether the results of a validation study performed in a very controlled and standardized condition of a laboratory setting still holds true for and apply to ambulatory conditions. As a matter of fact, PWA analysis is highly dependent on the quality of the tracing, which may be heavily altered during ambulatory measurements, limiting the accuracy of the assessment. The different daily activities may also influence the morphology of the pulse waveform and consequently the accuracy of the algorithm used to reconstruct the central pulse wave.
Second, the different methods used to analyze the derived brachial pulse waveforms are strongly device-dependent. Thus, data and results collected in the various studies should not be considered interchangeable, both in terms of accuracy and predictive value: a clinical result that is demonstrated with one device cannot be universalized for all of them. For instance, arm cuff-based techniques rely on brachial pulse waveforms recorded from an upper arm cuff by oscillometry, while tonometric techniques are based on pulse waves recorded at the radial artery level. The aortic pulse waveform is then reconstructed through PWA. The most obvious drawback of this approach is that it measures only local brachial or radial arterial wall characteristics, which may be different from the properties exhibited by other arteries, in particular by large arteries, such the carotid or the aorta.
Third, since we do not know which is the most accurate method for 24-h PWA, we need long-term follow-up studies to show the prognostic values of the parameters provided by the different devices. We already know that 24-h BP is prognostically superior to office BP [96]. However, we need to demonstrate whether ambulatory CAP, PWV, and AIx have any superiority over corresponding office measurements. The longitudinal studies should separately assess the impact of day-time and night-time measures of arterial stiffness and wave reflection, since preliminary evidence exists, for instance, that the circadian profiles of central and brachial pressure may be different, and thus changes in CAP occurring during night sleep may not have the same importance as those occurring for brachial BP.
Another issue regards the reference values and thresholds for clinical implementation of these parameters. We already have cutoffs for cfPWV and CAP used for measurements taken at rest [16, 97–99], but such references are lacking in ambulatory conditions. We know that office brachial BP and 24-h brachial BP differ and different normalcy values are currently applied in clinical practice [96]. This could hold true also for 24-h CAP, PWV, and AIx.
Perspectives and Conclusions
According to the evidence collected so far, 24-h PWA appears to be a potentially promising tool for evaluating vascular function, structure, and damage in daily life conditions and promoting early screening in subjects at risk. However, at present, there is limited evidence on the usefulness of such an approach in the clinical practice and much has still to be done to prove its actual benefit for hypertension management. In particular, the accuracy and quality of the evidence collected so far seems to be strongly device-dependent and results could not be considered interchangeable between devices.
Long-term follow-up (outcome) studies, such as the VASOTENS Registry, are needed to show the predictive value of the parameters provided by the various devices and to answer the many technical and clinical questions still open.
References
Palatini P, Casiglia E, Gąsowski J, Głuszek J, Jankowski P, Narkiewicz K, et al. Arterial stiffness, central hemodynamics, and cardiovascular risk in hypertension. Vasc Health Risk Manag. 2011;7:725–39.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífková R, Cosentino F, et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation: Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241:507–32.
McEniery CM, Cockcroft JR, Roman MJ, Franklin SS, Wilkinson IB. Central blood pressure: current evidence and clinical importance. Eur Heart J. 2014;35:1719–25.
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens. 2012;30:445–8.
Stergiou GS, Parati G, Vlachopoulos C, Achimastos A, Andreadis E, Asmar R, et al. Methodology and technology for peripheral and central blood pressure and blood pressure variability measurement: current status and future directions—position statement of the European Society of Hypertension Working Group on blood pressure monitoring and cardiovascular variability. J Hypertens. 2016;34:1665–77.
Nichols W, O’Rourke M, Vlachopoulos C. McDonald’s blood flow in arteries, Sixth Edition: Theoretical, Experimental and Clinical Principles. Boca Raton: CRC Press, 2011.
Tyberg JV, Davies JE, Wang Z, Whitelaw WA, Flewitt JA, Shrive NG, et al. Wave intensity analysis and the development of the reservoir-wave approach. Med Biol Eng Comput. 2009;47:221–32.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–27.
Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63:636–46.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31:1865–71.
Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation. 2001;103:987–92.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113:1213–25.
Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American Heart Association. Hypertension. 2015;66:698–722.
Herbert A, Cruickshank JK, Laurent S, Boutouyrie P, Reference Values for Arterial Measurements Collaboration. Establishing reference values for central blood pressure and its amplification in a general healthy population and according to cardiovascular risk factors. Eur Heart J. 2014;35:3122–33.
Chiang CE, Wang TD, Ueng KC, Lin TH, Yeh HI, Chen CY, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1–47.
Jones CR, Taylor K, Chowienczyk P, Poston L, Shennan AH. A validation of the Mobil O Graph (version 12) ambulatory blood pressure monitor. Blood Press Monit. 2000;5:233–8.
Wei W, Tölle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Press Monit. 2010;15:225–8.
Franssen PM, Imholz BP. Evaluation of the Mobil-O-Graph new generation ABPM device using the ESH criteria. Blood Press Monit. 2010;15:229–31.
Wassertheurer S, Kropf J, Weber T, van der Giet M, Baulmann J, Ammer M, et al. A new oscillometric method for pulse wave analysis: comparison with a common tonometric method. J Hum Hypertens. 2010;24:498–504.
Weber T, Wassertheurer S, Rammer M, Maurer E, Hametner B, Mayer CC, et al. Validation of a brachial cuff-based method for estimating central systolic blood pressure. Hypertension. 2011;58:825–32.
Weiss W, Gohlisch C, Harsch-Gladisch C, Tölle M, Zidek W, van der Giet M. Oscillometric estimation of central blood pressure: validation of the Mobil-O-Graph in comparison with the SphygmoCor device. Blood Press Monit. 2012;17:128–31.
Luzardo L, Lujambio I, Sottolano M, da Rosa A, Thijs L, Noboa O, et al. 24-h ambulatory recording of aortic pulse wave velocity and central systolic augmentation: a feasibility study. Hypertens Res. 2012;35:980–7.
Sarafidis PA, Georgianos PI, Karpetas A, Bikos A, Korelidou L, Tersi M, et al. Evaluation of a novel brachial cuff-based oscillometric method for estimating central systolic pressure in hemodialysis patients. Am J Nephrol. 2014;40:242–50.
Feistritzer HJ, Reinstadler SJ, Klug G, Kremser C, Seidner B, Esterhammer R, et al. Comparison of an oscillometric method with cardiac magnetic resonance for the analysis of aortic pulse wave velocity. PLoS One. 2015;10:e0116862.
Hametner B, Wassertheurer S, Kropf J, Mayer C, Eber B, Weber T. Oscillometric estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurements. Blood Press Monit. 2013;18:173–6.
Koudryavtcev SA, Lazarev VM. Validation of the BPLab(®) 24-hour blood pressure monitoring system according to the European standard BS EN 1060-4:2004 and British Hypertension Society protocol. Med Devices (Auckl). 2011;4:193–6.
Ledyaev MY, Stepanova OV, Ledyaeva AM. Validation of the BPLab(®) 24-hour blood pressure monitoring system in a pediatric population according to the 1993 British Hypertension Society protocol. Med Devices (Auckl). 2015;8:115–8.
Dorogova IV, Panina ES. Comparison of the BPLab(®) sphygmomanometer for ambulatory blood pressure monitoring with mercury sphygmomanometry in pregnant women: validation study according to the British Hypertension Society protocol. Vasc Health Risk Manag. 2015;11:245–9.
Rogoza AN, Kuznetsov AA. Central aortic blood pressure and augmentation index: comparison between Vasotens and SphygmoCor technology. Res Rep Clin Cardiol. 2012;3:27–33.
Kotovskaya YV, Kobalava ZD, Orlov AV. Validation of the integration of technology that measures additional “vascular” indices into an ambulatory blood pressure monitoring system. Med Devices (Auckl). 2014;7:91–7.
Butlin M, Alqahtani A, Qasem A, Turner M, Avolio AP. 6A.07: Aortic systolic pressure values but not indices derived from waveform features are consistent between brachial cuff-based devices used for estimation of central aortic pressure. J Hypertens. 2015;33(Suppl1):e74–5.
Nair D, Tan SY, Gan HW, Lim SF, Tan J, Zhu M, et al. The use of ambulatory tonometric radial arterial wave capture to measure ambulatory blood pressure: the validation of a novel wrist-bound device in adults. J Hum Hypertens. 2008;22:220–2.
Williams B, Lacy PS, Yan P, Hwee CN, Liang C, Ting CM. Development and validation of a novel method to derive central aortic systolic pressure from the radial pressure waveform using an n-point moving average method. J Am Coll Cardiol. 2011;57:951–61.
Ott C, Haetinger S, Schneider MP, Pauschinger M, Schmieder RE. Comparison of two noninvasive devices for measurement of central systolic blood pressure with invasive measurement during cardiac catheterization. J Clin Hypertens (Greenwich). 2012;14:575–9.
Theilade S, Hansen TW, Joergensen C, Lajer M, Rossing P. Tonometric devices for central aortic systolic pressure measurements in patients with type 1 diabetes: comparison of the BPro and SphygmoCor devices. Blood Press Monit. 2013;18:156–60.
Garcia-Ortiz L, Recio-Rodríguez JI, Canales-Reina JJ, Cabrejas-Sánchez A, Gomez-Arranz A, Magdalena-Belio JF, et al. Comparison of two measuring instruments, B-pro and SphygmoCor system as reference, to evaluate central systolic blood pressure and radial augmentation index. Hypertens Res. 2012;35:617–23.
Németh Z, Móczár K, Deák G. Evaluation of the Tensioday ambulatory blood pressure monitor according to the protocols of the British Hypertension Society and the Association for the Advancement of Medical Instrumentation. Blood Press Monit. 2002;7:191–7.
Magometschnigg D. Blood pressure and arterial stiffness. A comparison of two devices for measuring augmentationindex and pulse wave velocity. Wien Med Wochenschr. 2005;155:404–10.
Rajzer MW, Wojciechowska W, Klocek M, Palka I, Brzozowska-Kiszka M, Kawecka- Jaszcz K. Comparison of aortic pulse wave velocity measured by three techniques: Complior, SphygmoCor and Arteriograph. J Hypertens. 2008;26:2001–7.
Baulmann J, Schillings U, Rickert S, Uen S, Düsing R, Illyes M, et al. A new oscillometric method for assessment of arterial stiffness: comparison with tonometric and piezo-electronic methods. J Hypertens. 2008;26:523–8.
Jatoi NA, Mahmud A, Bennett K, Feely J. Assessment of arterial stiffness in hypertension: comparison of oscillometric (Arteriograph), piezoelectronic (Complior) and tonometric (SphygmoCor) techniques. J Hypertens. 2009;27:2186–91.
Gunjaca G, Jeroncic A, Budimir D, Mudnic I, Kolcic I, Polasek O, et al. A complex pattern of agreement between oscillometric and tonometric measurement of arterial stiffness in a population-based sample. J Hypertens. 2012;30:1444–52.
van Dijk SC, Enneman AW, Swart KM, van Schoor NM, Uitterlinden AG, Smulders YM, et al. Oscillometry and applanation tonometry measurements in older individuals with elevated levels of arterial stiffness. Blood Press Monit. 2013;18:332–8.
Ring M, Eriksson MJ, Zierath JR, Caidahl K. Arterial stiffness estimation in healthy subjects: a validation of oscillometric (Arteriograph) and tonometric (SphygmoCor) techniques. Hypertens Res. 2014;37:999–1007.
Ikonomidis I, Ntai K, Kadoglou NP, Papadakis I, Kornelakis M, Tritakis V, et al. The evaluation of pulse wave velocity using Arteriograph and Complior apparatus across multiple cohorts of cardiovascular-related diseases. Int J Cardiol. 2013;168:4890–2.
Mihalcea DJ, Florescu M, Suran BM, Enescu OA, Mincu RI, Magda S, et al. Comparison of pulse wave velocity assessed by three different techniques: Arteriograph, Complior, and Echo-tracking. Heart Vessel. 2016;31:568–77.
Nemcsik J, Egresits J, El Hadj Othmane T, Fekete BC, Fodor E, Szabó T, et al. Validation of arteriograph—a new oscillometric device to measure arterial stiffness in patients on maintenance hemodialysis. Kidney Blood Press Res. 2009;32:223–9.
Horváth IG, Németh A, Lenkey Z, Alessandri N, Tufano F, Kis P, et al. Invasive validation of a new oscillometric device (Arteriograph) for measuring augmentation index, central blood pressure and aortic pulse wave velocity. J Hypertens. 2010;28:2068–75.
Rossen NB, Laugesen E, Peters CD, Ebbehøj E, Knudsen ST, Poulsen PL, et al. Invasive validation of arteriograph estimates of central blood pressure in patients with type 2 diabetes. Am J Hypertens. 2014;27:674–9.
O’Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ. 2001;322:531–6.
Cremer A, Codjo L, Butlin M, Papaioannou G, Yeim S, Jan E, et al. Determination of central blood pressure by a noninvasive method (brachial blood pressure and QKD interval): a noninvasive validation. J Hypertens. 2013;31:1847–52.
Cremer A, Butlin M, Codjo L, Coulon P, Ranouil X, Joret C, et al. Determination of central blood pressure by a noninvasive method (brachial BP and QKD interval). J Hypertens. 2012;30:1533–9.
Goodwin J, Bilous M, Winship S, Finn P, Jones SC. Validation of the Oscar 2 oscillometric 24-h ambulatory blood pressure monitor according to the British Hypertension Society protocol. Blood Press Monit. 2007;12:113–7.
Jones SC, Bilous M, Winship S, Finn P, Goodwin J. Validation of the OSCAR 2 oscillometric 24-hour ambulatory blood pressure monitor according to the International Protocol for the validation of blood pressure measuring devices. Blood Press Monit. 2004;9:219–23.
Butlin M, Qasem A, Avolio AP. Estimation of central aortic pressure waveform features derived from the brachial cuff volume displacement waveform. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:2591–4.
Hwang MH, Yoo JK, Kim HK, Hwang CL, Mackay K, Hemstreet O, et al. Validity and reliability of aortic pulse wave velocity and augmentation index determined by the new cuff-based SphygmoCor Xcel. J Hum Hypertens. 2014;28:475–81.
Bilo G, Zorzi C, Ochoa Munera JE, Torlasco C, Giuli V, Parati G. Validation of the Somnotouch-NIBP noninvasive continuous blood pressure monitor according to the European Society of Hypertension International Protocol revision 2010. Blood Press Monit. 2015;20:291–4.
Narayan O, Casan J, Szarski M, Dart AM, Meredith IT, Cameron JD. Estimation of central aortic blood pressure: a systematic meta-analysis of available techniques. J Hypertens. 2014;32:1727–40.
Papaioannou TG, Karageorgopoulou TD, Sergentanis TN, Protogerou AD, Psaltopoulou T, Sharman JE, et al. Accuracy of commercial devices and methods for noninvasive estimation of aortic systolic blood pressure a systematic review and meta-analysis of invasive validation studies. J Hypertens. 2016;34:1237–48.
Cheng HM, Lang D, Tufanaru C, Pearson A. Measurement accuracy of non-invasively obtained central blood pressure by applanation tonometry: a systematic review and meta-analysis. Int J Cardiol. 2013;167:1867–76.
Protogerou AD, Argyris A, Nasothimiou E, Vrachatis D, Papaioannou TG, Tzamouranis D, et al. Feasibility and reproducibility of noninvasive 24-h ambulatory aortic blood pressure monitoring with a brachial cuff-based oscillometric device. Am J Hypertens. 2012;25:876–82.
Papaioannou TG, Argyris A, Protogerou AD, Vrachatis D, Nasothimiou EG, Sfikakis PP, et al. Non-invasive 24 hour ambulatory monitoring of aortic wave reflection and arterial stiffness by a novel oscillometric device: the first feasibility and reproducibility study. Int J Cardiol. 2013;169:57–61.
Posokhov IN, Konradi AO, Shlyakhto EV, Mamontov OV, Orlov AV, Rogoza AN. Day- to-day repeatability of the Pulse Time Index of Norm. Med Devices (Auckl). 2014;7:29–33.
Jankowski P, Bednarek A, Olszanecka A, Windak A, Kawecka-Jaszcz K, Czarnecka D. Twenty-four-hour profile of central blood pressure and central-to-peripheral systolic pressure amplification. Am J Hypertens. 2013;26:27–33.
Boggia J, Luzardo L, Lujambio I, Sottolano M, Robaina S, Thijs L, et al. The diurnal profile of central hemodynamics in a general Uruguayan population. Am J Hypertens. 2016;29:737–46.
Protogerou AD, Argyris AA, Papaioannou TG, Kollias GE, Konstantonis GD, Nasothimiou E, et al. Left-ventricular hypertrophy is associated better with 24-h aortic pressure than 24-h brachial pressure in hypertensive patients: the SAFAR study. J Hypertens. 2014;32:1805–14.
Zhang Y, Kollias G, Argyris AA, Papaioannou TG, Tountas C, Konstantonis GD, et al. Association of left ventricular diastolic dysfunction with 24-h aortic ambulatory blood pressure: the SAFAR study. J Hum Hypertens. 2015;29:442–8.
Aissopou EK, Argyris AA, Nasothimiou EG, Konstantonis GD, Tampakis K, Tentolouris N, et al. Ambulatory aortic stiffness is associated with narrow retinal arteriolar caliber in hypertensives: the SAFAR study. Am J Hypertens. 2016;29:626–33.
Ware LJ, Rennie KL, Gafane LF, Nell TM, Thompson JE, Van Rooyen JM, et al. Masked hypertension in low-income South African adults. J Clin Hypertens (Greenwich). 2016;18:396–404.
Elsurer R, Afsar B. Serum uric acid and arterial stiffness in hypertensive chronic kidney disease patients: sex-specific variations. Blood Press Monit. 2014;19:271–9.
Elsurer R, Afsar B. Morning blood pressure surge is associated with serum gamma-glutamyltransferase activity in essential hypertensive patients. J Hum Hypertens. 2015;29:331–6.
Afsar B, Elsurer R. The relationship between magnesium and ambulatory blood pressure, augmentation index, pulse wave velocity, total peripheral resistance, and cardiac output in essential hypertensive patients. J Am Soc Hypertens. 2014;8:28–35.
Hanssen H, Nussbaumer M, Moor C, Cordes M, Schindler C, Schmidt-Trucksäss A. Acute effects of interval versus continuous endurance training on pulse wave reflection in healthy young men. Atherosclerosis. 2015;238:399–406.
Korkmaz H, Sahin F, Ipekci SH, Temel T, Kebapcilar L. Increased pulse wave velocity and relationship with inflammation, insulin, and insulin resistance in inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2014;26:725–32.
Korkmaz H, Sozen M, Kebapcilar L. Increased arterial stiffness and its relationship with inflammation, insulin, and insulin resistance in celiac disease. Eur J Gastroenterol Hepatol. 2015;27:1193–9.
Hillebrand M, Nouri G, Hametner B, Parragh S, Köster J, Mortensen K, et al. Ambulatory (24 h) blood pressure and arterial stiffness measurement in Marfan syndrome patients: a case control feasibility and pilot study. BMC Cardiovasc Disord. 2016;16:81.
Maloberti A, Cesana F, Hametner B, Dozio D, Villa P, Hulpke-Wette M, et al. Increased nocturnal heart rate and wave reflection are early markers of cardiovascular disease in Williams-Beuren syndrome children. J Hypertens. 2015;33:804–9.
Yilmaz S, Celik G, Esmen SE. Assessment of arterial stiffness in patients with inactive and active Behçet’s disease. Scand J Rheumatol. 2014;43:63–9.
Karpetas A, Sarafidis PA, Georgianos PI, Protogerou A, Vakianis P, Koutroumpas G, et al. Ambulatory recording of wave reflections and arterial stiffness during intra- and interdialytic periods in patients treated with dialysis. Clin J Am Soc Nephrol. 2015;10:630–8.
Koutroumbas G, Georgianos PI, Sarafidis PA, Protogerou A, Karpetas A, Vakianis P, et al. Ambulatory aortic blood pressure, wave reflections and pulse wave velocity are elevated during the third in comparison to the second interdialytic day of the long interval in chronic haemodialysis patients. Nephrol Dial Transplant. 2015;30:2046–53.
Kuznetsova TY, Korneva VA, Bryantseva EN, Barkan VS, Orlov AV, Posokhov IN, et al. The 24-hour pulse wave velocity, aortic augmentation index, and central blood pressure in normotensive volunteers. Vasc Health Risk Manag. 2014;10:247–51.
Omboni S, Posokhov IN, Rogoza AN. Evaluation of 24-hour arterial stiffness indices and central hemodynamics in healthy normotensive subjects versus treated or untreated hypertensive patients: a feasibility study. Int J Hypertens. 2015;2015:601812.
Omboni S, Posokhov IN, Rogoza AN. 3D.05: relationship between 24-hour blood pressure variability and 24-hour aortic pressure and stiffness in hypertensive patients. J Hypertens. 2015;33(Suppl1):e41–2.
Posokhov IN, Kulikova NN, Starchenkova IV, Grigoricheva EA, Evdokimov VV, Orlov AV, et al. The “Pulse Time Index of Norm” highly correlates with the leftventricular mass index in patients with arterial hypertension. Vasc Health Risk Manag. 2014;10:139–44.
Minyukhina IE, Lipatov KS, Posokhov IN. Analysis of 24-hour pulse wave velocity in patients with renal transplantation. Int J Nephrol Renov Dis. 2013;6:125–9.
Aksenova TA, Gorbunov VV, Parkhomenko IV. 24-hour monitoring central aortic pressure in patients with hypertensive disease and concomitant chronic obstructive pulmonary disease. Klin Med (Mosk). 2013;91:43–7.
Theilade S, Lajer M, Hansen TW, Joergensen C, Persson F, Andrésdottir G, et al. 24-hour central aortic systolic pressure and 24-hour central pulse pressure are related to diabetic complications in type 1 diabetes—a cross-sectional study. Cardiovasc Diabetol. 2013;12:122.
Williams B, Lacy PS, Baschiera F, Brunel P, Düsing R. Novel description of the 24-hour circadian rhythms of brachial versus central aortic blood pressure and the impact of blood pressure treatment in a randomized controlled clinical trial: the Ambulatory Central Aortic Pressure (AmCAP) Study. Hypertension. 2013;61:1168–76.
Teong HH, Chin AM, Sule AA, Tay JC. Effect of angiotensin receptor blockade on central aortic systolic blood pressure in hypertensive Asians measured using radial tonometry: an open prospective cohort study. Singap Med J. 2016;57:384–9.
Celik G, Yilmaz S, Kebapcilar L, Gundogdu A. Central arterial characteristics of gout patients with chronic kidney diseases. Int J Rheum Dis. 2015. doi:10.1111/1756-185X.12689.
Gosse P, Cremer A, Papaioannou G, Yeim S. Arterial stiffness from monitoring of timing of Korotkoff sounds predicts the occurrence of cardiovascular events independently of left ventricular mass in hypertensive patients. Hypertension. 2013;62:161–7.
Omboni S, Posokhov IN, Parati G, Avolio A, Rogoza AN, Kotovskaya YV, et al. Vascular Health Assessment of The Hypertensive Patients (VASOTENS) Registry: study protocol of an international, web-based telemonitoring registry for ambulatory blood pressure and arterial stiffness. JMIR Res Prot. 2016;5:e137.
Wilkinson IB, McEniery CM, Schillaci G, Boutouyrie P, Segers P, Donald A, et al. ARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: part 1, arterial pulse wave velocity. Artery Res. 2010;4:34–40.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–66.
Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J. 2010;31:2338–50.
Engelen L, Bossuyt J, Ferreira I, van Bortel LM, Reesink KD, Segers P, et al. Reference values for local arterial stiffness. Part A: carotid artery. J Hypertens. 2015;33:1981–96.
Bossuyt J, Engelen L, Ferreira I, Stehouwer CD, Boutouyrie P, Laurent S, et al. Reference values for local arterial stiffness. Part B: femoral artery. J Hypertens. 2015;33:1997–2009.
Acknowledgments
We thank the manufacturers of the devices described in the paper for providing all the relevant updated information needed for completing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
SO is scientific consultant of Biotechmed Ltd., provider of the telemedicine services used in the VASOTENS Registry. ADP’s research group has received non-restricted educational grant and research equipment from I.E.M. GmbH, a manufacturer of 24-h pulse wave analysis devices.
The other authors declare no conflicts of interest regarding the publication of this paper.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Source of Funding
The authors received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors for the preparation of the manuscript.
Additional information
This article is part of the Topical Collection on Blood Pressure Monitoring and Management
Rights and permissions
About this article
Cite this article
Omboni, S., Posokhov, I.N., Kotovskaya, Y.V. et al. Twenty-Four-Hour Ambulatory Pulse Wave Analysis in Hypertension Management: Current Evidence and Perspectives. Curr Hypertens Rep 18, 72 (2016). https://doi.org/10.1007/s11906-016-0681-2
Published:
DOI: https://doi.org/10.1007/s11906-016-0681-2