Abstract
Purpose of Review
Current clinical practice guidelines recommend regular hepatocellular carcinoma (HCC) surveillance with biannual ultrasound with or without serum alpha-fetoprotein uniformly applied to all patients with cirrhosis. However, clinical implementation of this one-size-fits-all strategy has been challenging as evidenced by very low application rate below 20% due to various reasons, including suboptimal performance of the surveillance modalities.
Recent Findings
Newly emerging imaging techniques such as abbreviated MRI (AMRI) and molecular HCC risk biomarkers have increasingly become available for clinical evaluation and implementation. These technologies may have a potential to reshape HCC surveillance by enabling tailored strategies. This would involve performing optimized surveillance tests according to individual HCC risk and allocating limited medical resources for HCC surveillance based on cost-effectiveness.
Summary
Tailored HCC surveillance could lead to achievement of precision HCC care and substantial improvement of the current dismal patient prognosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver cancer, mainly hepatocellular carcinoma (HCC), is the second leading cause of cancer death worldwide, and its prognosis is still dismal with a 5-year survival rate below 15% [1]. In the USA, the incidence of HCC has significantly increased over the past 30 years and it is currently the fastest rising cause of cancer-related deaths [2]. The incidence of HCC is expected to continue to climb in the next decades, due to the increase of subjects with non-alcoholic fatty liver disease (NAFLD) and the increase of HCV-induced HCC despite the development of highly efficacious direct-acting antivirals [3].
Given an identifiable at-risk population, such as those with chronic viral hepatitis and/or cirrhosis, HCC surveillance using biannual ultrasound has been shown, in cohort studies and their meta-analyses, to be associated with improved survival, improved tumor detection at earlier stage, and improved curative treatment rates [4••, 5]. These findings support the recommendation for biannual HCC surveillance with ultrasound with or without serum alpha-fetoprotein (AFP) in subjects at sufficient risk for HCC [6,7,8]. Although the strength of evidence supporting survival benefit of surveillance is not strong [9], it is ethically difficult to conduct randomized controlled studies with a “no surveillance arm” to determine the magnitude of benefit [10]. Model-based simulation studies have demonstrated that biannual ultrasound for all cirrhotic patients is cost-effective compared to no surveillance, although average survival extension was less than 6 months [11]. The major limitations include suboptimal performance of the currently available surveillance modalities and the one-size-fits-all strategy recommended in the practice guidelines [12, 13], which may be substantially improved by tailored approaches discussed in this review.
Limitation of HCC Surveillance Modalities
Ultrasound and AFP have been the main HCC surveillance modalities widely used in clinical practice despite their suboptimal performance. The sensitivity of ultrasound detecting early stage HCC tumor is only 63% in a meta-analysis of 13 studies [14], which somewhat exceeds suggested minimal sensitivity for a screening test to be cost-effective, 42%, assuming an access to surveillance of 34% [15]. However, the sensitivities hugely vary across institutions and could be as low as 32% for early stage HCC detection, highlighting considerable operator dependency of its performance [16]. Serum alpha-fetoprotein (AFP) level has been widely used for HCC surveillance and diagnosis, although its clinical utility as a surveillance modality has been a matter of debate [17]. The sensitivity of AFP to detect early stage HCC tumor is approximately 60%, but serum levels may rise in non-malignant conditions such as hepatic regeneration following an inflammation flare in patients with chronic hepatitis or cirrhosis [18].
Limitation of One-Size-Fits-All HCC Surveillance Strategy
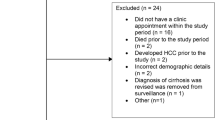
HCC risk is approximately defined according to etiologies and stages of chronic liver diseases. For instance, 5-year cumulative HCC risks in HCV cirrhosis, hemochromatosis, alcoholic cirrhosis, and biliary cirrhosis collected from epidemiological studies are 17–30, 21, 8–12, and 4%, respectively [19,20,21]. Based on the gross estimate for the underlying liver disease condition, a uniform regular HCC surveillance strategy, i.e., biannual assessment with ultrasound with or without AFP, is recommended when estimated overall HCC risk in the population exceeds a certain threshold of annual HCC incidence, e.g., 1.5% in cirrhotics and 0.2% in chronic hepatitis B in the American guideline [6]. However, this one-size-fits-all strategy is practically challenging to implement in clinical practice, even in developed countries, as evidenced by the extremely low utilization rate. Patients’ access to the surveillance program is a critical factor affecting its effectiveness [2]. A Markov model-based analysis revealed that the access rate should be at least 34% (with 42% effectiveness) for HCC surveillance to be associated with a survival benefit [15]. In a population-based cohort study of cirrhotic subjects over 65 years old in the USA, only 17% of the patients received regular HCC surveillance prior to HCC diagnosis [22]. A systematic review among American patients reported a pooled rate of 18.4% [23], confirming the low surveillance rate below 20%. A European study (22%) and a Japanese study (26% in non-viral cirrhosis) found similar numbers with some exceptions (57% in Japanese viral cirrhosis), suggesting that HCC surveillance is applied only in one fourth to half of cirrhosis patients globally [24, 25]. The poor application rate was not linked to patient adherence, as only 3% of patients with HCC in one study failed to complete surveillance despite orders [26]. Instead, provider-related factors, including failure to recognize liver disease or cirrhosis, failure to order surveillance, and time constraints, were identified as more influential factors [26, 27]. Hepatologists were more likely to order surveillance compared to non-specialists (odds ratio of 6.1), and patients with alcohol abuse were less likely to have surveillance (odds ratio 0.14) [26]. Population-based interventions, such as mailed outreach invitations, nearly doubled surveillance rates, although still less than half (approximately 45%) of the patients received surveillance [28•].
Experimental HCC Surveillance Modalities
As alternatives to the current HCC surveillance modalities, several imaging techniques and molecular biomarkers have been proposed to potentially replace ultrasound and/or AFP (Table 1). Computed tomography (CT) and magnetic resonance imaging (MRI) have been widely used for HCC diagnosis and are less affected by the limitations of ultrasound, e.g., inter-operator variation, and likely yield better performance [13, 29]. However, these modalities have been deemed unsuitable as tools for surveillance due to the high costs and irradiation (for CT) [6]. Nevertheless, several studies assessed CT and MRI in an HCC surveillance setting (as opposed to a diagnostic setting). One study tested the diagnostic performance of a one-time screening by CT or MRI compared with ultrasound alone to detect HCC in 638 consecutive patients within 6 months before liver transplantation in a tertiary-care institution comparing to findings of pathology at the time of transplantation [30]. Lesion-based sensitivity for HCC tumors smaller than 2 cm was 21, 40, and 47% for ultrasound, CT, and MRI, respectively, suggesting that although all three surveillance modalities had relatively low sensitivities for small tumors, CT and MRI provided substantial improvements doubling the sensitivity of ultrasound [30]. In another study, randomizing 163 subjects with compensated cirrhosis to biannual ultrasound or yearly CT, overall sensitivity for HCC detection was 71 and 67% for ultrasound and CT, respectively, with a similar proportion of early stage HCC detected (56 versus 63%) [31]. Although performance was similar, cost was higher in the CT-based surveillance strategy ($17,000 versus $57,000 for ultrasound and CT, respectively) [31]. A recent prospective study performed three rounds of paired ultrasound and MRI in 407 cirrhotic subjects and found an overall sensitivity for HCC detection of 85% for MRI but only 27% for ultrasound, whereas sensitivity for early HCC was 86 and 26% for MRI and ultrasound, respectively [32•]. Although encouraging, the authors themselves highlighted that the cost-effectiveness of this approach has yet to be assessed. To circumvent the issue of higher cost, simplified protocols have been explored to identify modalities that could replace ultrasound in the context of surveillance.
Abbreviated contrast-enhanced MRI (AMRI) was retrospectively tested in 298 patients enrolled in a gadoxetic acid-enhanced MRI-based HCC surveillance program [33•]. Analysis of a simulated AMRI protocol from the complete image set yielded a mean per-patient sensitivity of 83% for HCC detection, with reduced cost compared to the standard. Another retrospective single-center study reported a per-patient sensitivity of 81% and per-lesion sensitivity of 78%, confirming the maintained sensitivity in the simplified protocol [34]. The estimated range of cost saving with AMRI was 31–49%. Although these findings need prospective validation, AMRI and similar strategies could be promising options for improved performance with acceptable costs for HCC surveillance.
In parallel, to overcome the limitations of AFP, i.e., low sensitivity and specificity, there have been long-standing efforts to identify and develop serum molecular biomarkers for HCC detection (Table 1). Reported performance of detection varies, and these tests need validation in the setting of HCC surveillance in comparison with AFP.
From One-Size-Fits-All to Tailored HCC Surveillance Strategy
Studies have indicated that HCC risk is not uniform across all patients with the same clinical condition, e.g., HCV cirrhosis, and therefore, the current one-size-fits-all approach likely results in over- or under-estimated HCC risk for each individual [2]. In addition, the magnitude of HCC risk is not yet completely understood in emerging populations, i.e., non-alcoholic fatty liver disease (NAFLD) without cirrhosis and chronic hepatitis C after viral cure especially by direct-acting antivirals [35,36,37,38,39]. More precise individual HCC risk determination will address the heterogeneous HCC risk among patients and enable optimal allocation of limited resources and capability of HCC surveillance to the subset of patients who have higher risk and may benefit more from regular surveillance. Tailored surveillance strategies after prior determination of cancer risk have been successfully implemented in other disease settings, such as colorectal cancer screening, where clinical and genetic risk factors drive screening modalities and frequency, and breast cancer screening, where risk prediction models are available to determine cancer risk based on a number of variables [40,41,42].
HCC risk prediction has been attempted to identify a subset of patients at higher risk of HCC development using risk scores based on clinical variables such as older age, male sex, viral etiology of liver disease, Child-Pugh B/C cirrhosis, diabetes, and obesity, although their risk-predictive performance is limited especially in the sizable population of patients with earlier stage liver diseases in whom there is an unmet need for clinical prognostic factors (Table 2) [43]. Nevertheless, these studies clearly demonstrate feasibility to risk-stratify patients with chronic liver disease according to future HCC risk.
To supplement/complement these imperfect clinical scores, molecular biomarkers have been actively explored in parallel with the advent of high-throughput molecular profiling technologies (Table 2) [43]. Several germline single nucleotide polymorphisms (SNPs) have been reported as indicators of elevated HCC risk. The EGF 61*G allele was associated with HCC risk in a prospective cohort of patients with HCV-related advanced fibrosis (39% cirrhotic), and a prediction model including the EGF G/G genotype stratified subjects into three risk groups with increasing 6-year HCC incidence [44, 45]. A SNP in MPO encoding an antioxidant enzyme was associated with HCC risk in a prospective cohort of HCV cirrhotics [46]. A transcriptomic signature in the diseased liver, now available as a laboratory developed test (LDT), has been validated as a pan-etiology HCC risk predictor in patients with chronic hepatitis B/C, alcohol abuse, or non-alcoholic steatohepatitis (NASH) [47, 48•, 49, 50].
Prior to its diagnosis, HCC tumor is assumed to undergo a subclinical growth phase with a tumor volume doubling time estimated at approximately 3–6 months, based on which the surveillance interval could be optimized [51, 52]. Given that high-risk patients are at risk of increased multicentric tumor occurrence, altering HCC surveillance interval according to estimated HCC risk may be a rational strategy. To date, uniformly longer or shorter surveillance interval has been clinically evaluated irrespective of individual HCC risk. An Italian study found that reducing surveillance to once a year led to a decrease in the detection of very early HCC and increased the number of advanced tumors detected, suggesting that this was a suboptimal strategy at least in the setting of Child-Pugh class A or B cirrhosis patients enrolled in the study [53]. Shortening surveillance interval to 3 months was tested in a randomized controlled trial, enrolling 1278 French patients with mostly alcohol- or HCV-related liver diseases [54]. Although an increased incidence of lesions smaller than 10 mm was identified in the 3-month surveillance group, this did not lead to an increase in HCC incidence or in prevalence of tumors smaller than 30-mm diameter leading the authors to conclude that 3-monthly ultrasound surveillance detects more small focal lesions than biannual ultrasound, but does not improve detection of small HCC tumors at 5-year cumulative incidence of 10–12% in this study population [54]. It is still an unanswered question whether personalizing surveillance interval according to individual HCC risk leads to improved early HCC tumor detection and prognostic benefit for the patients.
With the new candidate surveillance modalities and tools for individual HCC risk assessment, one may consider tailored HCC surveillance choosing an optimal surveillance modality based on each patient’s HCC risk status. However, it is challenging to ethically justify and logistically carry out prospective clinical trials assessing new HCC surveillance strategies. One viable alternative is to quantitatively evaluate tailored surveillance strategies in Markov model-based simulation studies, similar to the evidence-based underlying current clinical recommendations, based on the generally adopted criteria of cost-effectiveness, i.e., increased survival by 3 months or more and incremental cost-effectiveness ratio (ICER) below $50,000/quality adjusted life year gained [6, 55, 56]. Indeed, a comprehensive survey of theoretically possible combinations of tailored HCC surveillance following clinical and molecular HCC risk assessment and patient stratification has revealed superior cost-effectiveness of personalized surveillance strategies compared to the current standard of care, biannual ultrasound uniformly applied to all patients with cirrhosis [57]. Although this result needs to be clinically verified, testing of such strategies is now technically feasible given the clinical availability of the new surveillance modalities and molecular risk assessment assays.
Conclusion
Clinical implementation of HCC surveillance programs recommended in current practice guidelines, i.e., uniform biannual ultrasound HCC surveillance in all patients with cirrhosis, is practically infeasible due to multiple reasons and results in inefficient and wasteful distribution of limited medical resources for surveillance. It is now a prime time to consider tailored surveillance strategies with the rapid development of clinically available new imaging techniques and molecular assays, guided by the measure of net cost-effectiveness, which will eventually lead to achievement of precision clinical care for patients with chronic liver disease and substantial improvement of the still dismal HCC prognosis.
Abbreviations
- AFP:
-
α-Fetoprotein
- ALD:
-
Alcoholic liver disease
- CT:
-
Computed tomography
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- MRI:
-
Magnetic resonance imaging
- NAFLD:
-
Non-alcoholic fatty liver disease
- SNP:
-
Single nucleotide polymorphism
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi:10.3322/caac.21262.
Singal AG, El-Serag HB. Hepatocellular carcinoma from epidemiology to prevention: translating knowledge into practice. Clin Gastroenterol Hepatol. 2015;13(12):2140–51. doi:10.1016/j.cgh.2015.08.014.
Harris RJ, Thomas B, Griffiths J, Costella A, Chapman R, Ramsay M, et al. Increased uptake and new therapies are needed to avert rising hepatitis C-related end stage liver disease in England: modelling the predicted impact of treatment under different scenarios. J Hepatol. 2014;61(3):530–7. doi:10.1016/j.jhep.2014.05.008.
•• Singal AG, Pillai A, Tiro J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 2014;11(4):e1001624. doi:10.1371/journal.pmed.1001624. A systematic review clarifying the benefit of HCC surveillance.
Mittal S, Kanwal F, Ying J, Chung R, Sada YH, Temple S, et al. Effectiveness of surveillance for hepatocellular carcinoma in clinical practice: a United States cohort. J Hepatol. 2016;65(6):1148–54. doi:10.1016/j.jhep.2016.07.025.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–2. doi:10.1002/hep.24199.
EASL-EORTC. Clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908–43. doi:10.1016/j.jhep.2011.12.001.
Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, et al. Asian Pacific association for the study of the liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4(2):439–74. doi:10.1007/s12072-010-9165-7.
Kansagara D, Papak J, Pasha AS, O’Neil M, Freeman M, Relevo R, et al. Screening for hepatocellular carcinoma in chronic liver disease: a systematic review. Ann Intern Med. 2014;161(4):261–9. doi:10.7326/M14-0558.
Poustchi H, Farrell GC, Strasser SI, Lee AU, McCaughan GW, George J. Feasibility of conducting a randomized control trial for liver cancer screening: is a randomized controlled trial for liver cancer screening feasible or still needed? Hepatology. 2011;54(6):1998–2004.
Andersson KL, Salomon JA, Goldie SJ, Chung RT. Cost effectiveness of alternative surveillance strategies for hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2008;6(12):1418–24. doi:10.1016/j.cgh.2008.08.005.
Singal AG, Nehra M, Adams-Huet B, Yopp AC, Tiro JA, Marrero JA, et al. Detection of hepatocellular carcinoma at advanced stages among patients in the HALT-C trial: where did surveillance fail? Am J Gastroenterol. 2013;108(3):425–32. doi:10.1038/ajg.2012.449.
Del Poggio P, Olmi S, Ciccarese F, Di Marco M, Rapaccini GL, Benvegnu L, et al. Factors that affect efficacy of ultrasound surveillance for early stage hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2014;12(11):1927–33. doi:10.1016/j.cgh.2014.02.025. e2.
Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MA, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30(1):37–47. doi:10.1111/j.1365-2036.2009.04014.x.
Mourad A, Deuffic-Burban S, Ganne-Carrie N, Renaut-Vantroys T, Rosa I, Bouvier AM, et al. Hepatocellular carcinoma screening in patients with compensated hepatitis C virus (HCV)-related cirrhosis aware of their HCV status improves survival: a modeling approach. Hepatology. 2014;59(4):1471–81. doi:10.1002/hep.26944.
Singal AG, Conjeevaram HS, Volk ML, Fu S, Fontana RJ, Askari F, et al. Effectiveness of hepatocellular carcinoma surveillance in patients with cirrhosis. Cancer Epidemiol Biomarkers Prev. 2012;21(5):793–9. doi:10.1158/1055-9965.EPI-11-1005.
Song PP, Xia JF, Inagaki Y, Hasegawa K, Sakamoto Y, Kokudo N, et al. Controversies regarding and perspectives on clinical utility of biomarkers in hepatocellular carcinoma. World J Gastroenterol. 2016;22(1):262–74. doi:10.3748/wjg.v22.i1.262.
Gupta S, Bent S, Kohlwes J. Test characteristics of α-fetoprotein for detecting hepatocellular carcinoma in patients with hepatitis C: a systematic review and critical analysis. Ann Intern Med. 2003;139(1):46–50.
Mancebo A, González–Diéguez ML, Cadahía V, Varela M, Pérez R, Navascués CA, et al. Annual incidence of hepatocellular carcinoma among patients with alcoholic cirrhosis and identification of risk groups. Clin Gastroenterol Hepatol. 2013;11(1):95–101. doi:10.1016/j.cgh.2012.09.007.
Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127(5 Suppl 1):S35–50.
El-Serag HB, Kanwal F. Epidemiology of hepatocellular carcinoma in the United States: where are we? where do we go? Hepatology. 2014;60(5):1767–75. doi:10.1002/hep.27222.
Davila JA, Morgan RO, Richardson PA, Du XL, McGlynn KA, El-Serag HB. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology. 2010;52(1):132–41. doi:10.1002/hep.23615.
Singal AG, Yopp A, Skinner CS, Packer M, Lee WM, Tiro JA. Utilization of hepatocellular carcinoma surveillance among American patients: a systematic review. J Gen Intern Med. 2012;27(7):861–7.
Edenvik P, Davidsdottir L, Oksanen A, Isaksson B, Hultcrantz R, Stål P. Application of hepatocellular carcinoma surveillance in a European setting. What can we learn from clinical practice? Liver Int. 2015;35(7):1862–71.
Hirata A, Hirata T, Takahashi Y, Nakayama T. Surveillance rates for hepatocellular carcinoma among patients with cirrhosis, chronic hepatitis B, and chronic hepatitis C based on Japanese claims database. Hepatology Research. 2016
Singal AG, Yopp AC, Gupta S, Skinner CS, Halm EA, Okolo E, et al. Failure rates in the hepatocellular carcinoma surveillance process. Cancer Prev Res. 2012;5(9):1124–30. doi:10.1158/1940-6207.CAPR-12-0046.
Dalton-Fitzgerald E, Tiro J, Kandunoori P, Halm EA, Yopp A, Singal AG, et al. Practice patterns and attitudes of primary care providers and barriers to surveillance of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:791–8. e1.
• Singal AG, Tiro JA, Marrero JA, McCallister K, Mejias C, Adamson B et al. Mailed outreach program increases ultrasound screening of patients with cirrhosis for hepatocellular carcinoma. Gastroenterology. 2016. A practical outreach program showing a doubling of HCC screening rates with a simple intervention
Simmons O, Fetzer D, Yokoo T, Marrero J, Yopp A, Kono Y, et al. Predictors of adequate ultrasound quality for hepatocellular carcinoma surveillance in patients with cirrhosis. Aliment Pharmacol Ther. 2017;45(1):169–77.
Yu NC, Chaudhari V, Raman SS, Lassman C, Tong MJ, Busuttil RW, et al. CT and MRI improve detection of hepatocellular carcinoma, compared with ultrasound alone, in patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9(2):161–7. doi:10.1016/j.cgh.2010.09.017.
Pocha C, Dieperink E, McMaken K, Knott A, Thuras P, Ho S. Surveillance for hepatocellular cancer with ultrasonography vs. computed tomography—a randomised study. Aliment Pharmacol Ther. 2013;38(3):303–12.
• Kim SY, An J, Lim Y-S, Han S, Lee J-Y, Byun JH et al. MRI with liver-specific contrast for surveillance of patients with cirrhosis at high risk of hepatocellular carcinoma. JAMA Oncology. 2016. A prospective study comparing ultrasound to MRI-based HCC surveillance
• Marks RM, Ryan A, Heba ER, Tang A, Wolfson TJ, Gamst AC et al. Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid-enhanced MRI for hepatocellular carcinoma surveillance. American Journal of Roentgenology. 2015;204(3):527–35. Proof of principle of effectiveness of an abbreviated MRI protocol for HCC surveillance
Besa C, Lewis S, Pandharipande PV, Chhatwal J, Kamath A, Cooper N et al. Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdominal Radiology. 2016:1–12
Goossens N, Hoshida Y. Is hepatocellular cancer the same disease in alcoholic and non-alcoholic fatty liver diseases? Gastroenterology. 2016. doi:10.1053/j.gastro.2016.01.006.
Reig M, Mariño Z, Perelló C, Iñarrairaegui M, Ribeiro A, Lens S, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol. 2016;65(4):719–26.
Conti F, Buonfiglioli F, Scuteri A, Crespi C, Bolondi L, Caraceni P, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol. 2016;65(4):727–33.
El‐Serag HB, Kanwal F, Richardson P, Kramer J. Risk of hepatocellular carcinoma after sustained virologic response in veterans with HCV‐infection. Hepatology. 2016
Baumert TF, Jühling F, Atsushi O, Hoshida Y. Hepatitis C-related hepatocellular carcinoma in the era of new generation antivirals. BMC Med. 2017 (in press).
Levin B, Lieberman DA, McFarland B, Smith RA, Brooks D, Andrews KS, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi‐Society Task Force on Colorectal Cancer, and the American College of Radiology*†. CA Cancer J Clin. 2008;58(3):130–60.
Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K. Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Ann Intern Med. 2008;148(5):337–47.
Parmigiani G, Chen S, Iversen ES, Friebel TM, Finkelstein DM, Anton-Culver H, et al. Validity of models for predicting BRCA1 and BRCA2 mutations. Ann Intern Med. 2007;147(7):441–50.
Goossens N, Nakagawa S, Hoshida Y. Molecular prognostic prediction in liver cirrhosis. World J Gastroenterol. 2015;21(36):10262–73. doi:10.3748/wjg.v21.i36.10262.
Tanabe KK, Lemoine A, Finkelstein DM, Kawasaki H, Fujii T, Chung RT, et al. Epidermal growth factor gene functional polymorphism and the risk of hepatocellular carcinoma in patients with cirrhosis. JAMA. 2008;299(1):53–60. doi:10.1001/jama.2007.65.
Abu Dayyeh BK, Yang M, Fuchs BC, Karl DL, Yamada S, Sninsky JJ, et al. A functional polymorphism in the epidermal growth factor gene is associated with risk for hepatocellular carcinoma. Gastroenterology. 2011;141(1):141–9. doi:10.1053/j.gastro.2011.03.045.
Nahon P, Sutton A, Rufat P, Charnaux N, Mansouri A, Moreau R, et al. A variant in myeloperoxidase promoter hastens the emergence of hepatocellular carcinoma in patients with HCV-related cirrhosis. J Hepatol. 2012;56(2):426–32. doi:10.1016/j.jhep.2011.08.010.
Hoshida Y, Villanueva A, Sangiovanni A, Sole M, Hur C, Andersson KL, et al. Prognostic gene expression signature for patients with hepatitis C-related early-stage cirrhosis. Gastroenterology. 2013;144(5):1024–30. doi:10.1053/j.gastro.2013.01.021.
• King LY, Canasto-Chibuque C, Johnson KB, Yip S, Chen X, Kojima K, et al. A genomic and clinical prognostic index for hepatitis C-related early-stage cirrhosis that predicts clinical deterioration. Gut. 2014. doi:10.1136/gutjnl-2014-307862. Molecular risk stratification of patients with early stage cirrhosis using a gene expression molecular score.
Hoshida Y, Villanueva A, Kobayashi M, Peix J, Chiang DY, Camargo A, et al. Gene expression in fixed tissues and outcome in hepatocellular carcinoma. N Engl J Med. 2008;359(19):1995–2004. doi:10.1056/NEJMoa0804525.
Nakagawa S, Wei L, Song W, Higashi T, Ghoshal S, Kim RS et al. Molecular liver cancer prevention in cirrhosis by organ transcriptome analysis and lysophosphatidic acid pathway inhibition. Cancer Cell. 2016, in press.
Furlan A, Marin D, Agnello F, Di Martino M, Di Marco V, Lagalla R, et al. Hepatocellular carcinoma presenting at contrast-enhanced multi-detector-row computed tomography or gadolinium-enhanced magnetic resonance Imaging as a small (≤2 cm), indeterminate nodule: growth rate and optimal interval time for imaging follow-up. J Comput Assist Tomogr. 2012;36(1):20–5.
Taouli B, Goh JS, Lu Y, Qayyum A, Yeh BM, Merriman RB, et al. Growth rate of hepatocellular carcinoma: evaluation with serial computed tomography or magnetic resonance imaging. J Comput Assist Tomogr. 2005;29(4):425–9.
Santi V, Trevisani F, Gramenzi A, Grignaschi A, Mirici-Cappa F, Del Poggio P, et al. Semiannual surveillance is superior to annual surveillance for the detection of early hepatocellular carcinoma and patient survival. J Hepatol. 2010;53(2):291–7.
Trinchet JC, Chaffaut C, Bourcier V, Degos F, Henrion J, Fontaine H, et al. Ultrasonographic surveillance of hepatocellular carcinoma in cirrhosis: a randomized trial comparing 3- and 6-month periodicities. Hepatology. 2011;54(6):1987–97. doi:10.1002/hep.24545.
Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis. Am J Med. 1996;101(4):422–34.
Lin OS, Keeffe EB, Sanders GD, Owens DK. Cost-effectiveness of screening for hepatocellular carcinoma in patients with cirrhosis due to chronic hepatitis C. Aliment Pharmacol Ther. 2004;19(11):1159–72. doi:10.1111/j.1365-2036.2004.01963.x.
Goossens N, Singal AG, King LY, Andersson KL, Fuchs BC, Besa C et al., editors. Cost-effectiveness of a risk-stratified hepatocellular carcinoma surveillance strategy in patients with cirrhosis. HEPATOLOGY; 2016: WILEY-BLACKWELL 111 RIVER ST, HOBOKEN 07030–5774, NJ USA
Yoshihiroshimauchi M, Ryokokuromatsu RO, Yukiotateishi S, ONO N, Yutani S, Hiroakinagamatsu S, et al. A simultaneous monitoring of Lens culinaris agglutinin a-reactive a-fetoprotein and des-γ-carboxy prothrombin as an early diagnosis of hepatocellular carcinoma in the follow-up of cirrhotic patients. Oncol Rep. 2000;7:249–56.
Volk ML, Hernandez JC, Su GL, Lok AS, Marrero JA. Risk factors for hepatocellular carcinoma may impair the performance of biomarkers: a comparison of AFP, DCP, and AFP-L3. Cancer Biomark. 2007;3(2):79–87.
Sterling RK, Jeffers L, Gordon F, Sherman M, Venook AP, Reddy KR, et al. Clinical utility of AFP-L3% measurement in North American patients with HCV-related cirrhosis. Am J Gastroenterol. 2007;102(10):2196–205.
Lok AS, Sterling RK, Everhart JE, Wright EC, Hoefs JC, Di Bisceglie AM, et al. Des-γ-carboxy prothrombin and α-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology. 2010;138(2):493–502.
Wang M, Long RE, Comunale MA, Junaidi O, Marrero J, Di Bisceglie AM, et al. Novel fucosylated biomarkers for the early detection of hepatocellular carcinoma. Cancer Epidemiol Biomark Prev. 2009;18(6):1914–21.
Marrero JA, Romano PR, Nikolaeva O, Steel L, Mehta A, Fimmel CJ, et al. GP73, a resident Golgi glycoprotein, is a novel serum marker for hepatocellular carcinoma. J Hepatol. 2005;43(6):1007–12.
Tian L, Wang Y, Xu D, Gui J, Jia X, Tong H, et al. Serological AFP/Golgi protein 73 could be a new diagnostic parameter of hepatic diseases. Int J Cancer. 2011;129(8):1923–31.
Shang S, Plymoth A, Ge S, Feng Z, Rosen HR, Sangrajrang S, et al. Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology. 2012;55(2):483–90. doi:10.1002/hep.24703.
Duarte-Salles T, Misra S, Stepien M, Plymoth A, Muller D, Overvad K, et al. Circulating osteopontin and prediction of hepatocellular carcinoma development in a large European population. Cancer Prev Res (Phila). 2016;9(9):758–65. doi:10.1158/1940-6207.CAPR-15-0434.
Hippo Y, Watanabe K, Watanabe A, Midorikawa Y, Yamamoto S, Ihara S, et al. Identification of soluble NH2-terminal fragment of glypican-3 as a serological marker for early-stage hepatocellular carcinoma. Cancer Res. 2004;64(7):2418–23.
Beneduce L, Castaldi F, Marino M, Quarta S, Ruvoletto M, Benvegnu L, et al. Squamous cell carcinoma antigen-immunoglobulin M complexes as novel biomarkers for hepatocellular carcinoma. Cancer. 2005;103(12):2558–65. doi:10.1002/cncr.21106.
Shen Q, Fan J, Yang XR, Tan Y, Zhao W, Xu Y, et al. Serum DKK1 as a protein biomarker for the diagnosis of hepatocellular carcinoma: a large-scale, multicentre study. Lancet Oncol. 2012;13(8):817–26. doi:10.1016/S1470-2045(12)70233-4.
Z-q Z, Meng H, Wang N, Liang LN, Liu LN, Lu SM, et al. Serum microRNA 143 and microRNA 215 as potential biomarkers for the diagnosis of chronic hepatitis and hepatocellular carcinoma. Diagn Pathol. 2014;9(1):1.
Lin X-J, Chong Y, Guo Z-W, Xie C, Yang X-J, Zhang Q, et al. A serum microRNA classifier for early detection of hepatocellular carcinoma: a multicentre, retrospective, longitudinal biomarker identification study with a nested case-control study. Lancet Oncol. 2015;16(7):804–15.
Liu XE, Desmyter L, Gao CF, Laroy W, Dewaele S, Vanhooren V, et al. N-glycomic changes in hepatocellular carcinoma patients with liver cirrhosis induced by hepatitis B virus. Hepatology. 2007;46(5):1426–35. doi:10.1002/hep.21855.
Biselli M, Conti F, Gramenzi A, Frigerio M, Cucchetti A, Fatti G, et al. A new approach to the use of α-fetoprotein as surveillance test for hepatocellular carcinoma in patients with cirrhosis. Br J Cancer. 2015;112(1):69–76.
El-Serag HB, Kanwal F, Davila JA, Kramer J, Richardson P, 5. A new laboratory-based algorithm to predict development of hepatocellular carcinoma in patients with hepatitis C and cirrhosis. Gastroenterology. 2014;146:1249–55. doi:10.1053/j.gastro.2014.01.045. e1.
Hung Y-C, Lin C-L, Liu C-J, Hung H, Lin S-M, Lee S-D, et al. Development of risk scoring system for stratifying population for hepatocellular-carcinoma screening. Hepatology. 2015;61:1934–44. doi:10.1002/hep.27610.
Flemming JA, Yang JD, Vittinghoff E, Kim WR, Terrault NA. Risk prediction of hepatocellular carcinoma in patients with cirrhosis: the ADRESS-HCC risk model. Cancer. 2014;120(22):3485–93. doi:10.1002/cncr.28832.
Velázquez RF, Rodríguez M, Navascués CA, Linares A, Pérez R, Sotorríos NG, et al. Prospective analysis of risk factors for hepatocellular carcinoma in patients with liver cirrhosis. Hepatology. 2003;37(3):520–7. doi:10.1053/jhep.2003.50093.
Singal AG, Mukherjee A, Joseph Elmunzer B, Higgins PDR, Lok AS, Zhu J, et al. Machine learning algorithms outperform conventional regression models in predicting development of hepatocellular carcinoma. Am J Gastroenterol. 2013;108(11):1723–30. doi:10.1038/ajg.2013.332.
Yuen M-F, Tanaka Y, Fong DY-T, Fung J, Wong DK-H, Yuen JC-H, et al. Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. J Hepatol. 2009;50:80–8. doi:10.1016/j.jhep.2008.07.023.
Wong VW-S, Chan SL, Mo F, Chan T-C, Loong HH-F, Wong GL-H, et al. Clinical scoring system to predict hepatocellular carcinoma in chronic hepatitis B carriers. J Clin Oncol. 2010;28(10):1660–5. doi:10.1200/jco.2009.26.2675.
Wong GLH, Chan HLY, Wong CKY, Leung C, Chan CY, Ho PPL, et al. Liver stiffness-based optimization of hepatocellular carcinoma risk score in patients with chronic hepatitis B. J Hepatol. 2014;60(2):339–45. doi:10.1016/j.jhep.2013.09.029.
Yang HI, Yuen MF, Chan HLY, Han KH, Chen PJ, Kim DY, et al. Risk estimation for hepatocellular carcinoma in chronic hepatitis B (REACH-B): development and validation of a predictive score. Lancet Oncol. 2011;12(6):568–74. doi:10.1016/S1470-2045(11)70077-8.
Ikeda M, Fujiyama S, Tanaka M, Sata M, Ide T, Yatsuhashi H, et al. Risk factors for development of hepatocellular carcinoma in patients with chronic hepatitis C after sustained response to interferon. J Gastroenterol. 2005;40(2):148–56. doi:10.1007/s00535-004-1519-2.
Chang KC, Hung CH, Lu SN, Wang JH, Lee CM, Chen CH, et al. A novel predictive score for hepatocellular carcinoma development in patients with chronic hepatitis C after sustained response to pegylated interferon and ribavirin combination therapy. J Antimicrob Chemother. 2012;67(11):2766–72. doi:10.1093/jac/dks269.
Chang KC, Wu YY, Hung CH, Lu SN, Lee CM, Chiu KW, et al. Clinical-guide risk prediction of hepatocellular carcinoma development in chronic hepatitis C patients after interferon-based therapy. Br J Cancer. 2013;109(9):2481–8. doi:10.1038/bjc.2013.564.
Lok AS, Seeff LB, Morgan TR, di Bisceglie AM, Sterling RK, Curto TM, et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease. Gastroenterology. 2009;136(1):138–48. doi:10.1053/j.gastro.2008.09.014.
Lee MH, Lu SN, Yuan Y, Yang HI, Jen CL, You SL, et al. Development and validation of a clinical scoring system for predicting risk of HCC in asymptomatic individuals seropositive for anti-HCV antibodies. PLoS One. 2014;9(5), e94760. doi:10.1371/journal.pone.0094760.
Shin SH, Kim SU, Park JY, Kim Do Y, Ahn SH, Han KH, et al. Liver stiffness-based model for prediction of hepatocellular carcinoma in chronic hepatitis B virus infection: comparison with histological fibrosis. Liver Int. 2015;35(3):1054–62. doi:10.1111/liv.12621.
Suh B, Park S, Shin DW, Yun JM, Yang H-K, Yu SJ, et al. High liver fibrosis index FIB-4 is highly predictive of hepatocellular carcinoma in chronic hepatitis B carriers. Hepatology. 2015;61(4):1261–8. doi:10.1002/hep.27654.
Kim JH, Sohn BH, Lee HS, Kim SB, Yoo JE, Park YY, et al. Genomic predictors for recurrence patterns of hepatocellular carcinoma: model derivation and validation. PLoS Med. 2014;11(12), e1001770. doi:10.1371/journal.pmed.1001770.
Ji J, Eggert T, Budhu A, Forgues M, Takai A, Dang H, et al. Hepatic stellate cell and monocyte interaction contributes to poor prognosis in hepatocellular carcinoma. Hepatology. 2015. doi:10.1002/hep.27822.
Guyot E, Sutton A, Rufat P, Laguillier C, Mansouri A, Moreau R, et al. PNPLA3 rs738409, hepatocellular carcinoma occurrence and risk model prediction in patients with cirrhosis. J Hepatol. 2013;58(2):312–8. doi:10.1016/j.jhep.2012.09.036.
Nahon P, Sutton A, Rufat P, Ziol M, Thabut G, Schischmanoff PO, et al. Liver iron, HFE gene mutations, and hepatocellular carcinoma occurrence in patients with cirrhosis. Gastroenterology. 2008;134(1):102–10. doi:10.1053/j.gastro.2007.10.038.
Acknowledgements
This work was supported by the FLAGS foundation, the Nuovo-Soldati Cancer Research Foundation, and a research fellowship by the Geneva University Hospital to NG and NIH/NIDDK R01 DK099558, Irma T. Hirschl Trust, Dr. Harold and Golden Lamport Research Award, European Union ERC-2014-AdG-671231-HEPCIR, and US Department of Defense W81XWH-16-1-0363 to YH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nicolas Goossens, C. Billie Bian, and Yujin Hoshida each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hepatic Cancer
Rights and permissions
About this article
Cite this article
Goossens, N., Bian, C.B. & Hoshida, Y. Tailored Algorithms for Hepatocellular Carcinoma Surveillance: Is One-Size-Fits-All Strategy Outdated?. Curr Hepatology Rep 16, 64–71 (2017). https://doi.org/10.1007/s11901-017-0336-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-017-0336-z