ABSTRACT
BACKGROUND
Although surveillance for hepatocellular carcinoma (HCC) is recommended in high-risk patients, several studies have suggested it is being underutilized in clinical practice. The aim of our study was to quantify utilization rates for HCC surveillance among patients with cirrhosis and summarize patterns of association between utilization rates and patient socio-demographic characteristics.
DATA SOURCES
We performed a systematic literature review using the Medline database from January 1990 through March 2011 and a manual search of national meeting abstracts from 2008–2010.
METHODS
Two investigators independently extracted data on patient populations, study methods, and results using standardized forms. A pooled surveillance rate with 95% confidence intervals was calculated. Pre-specified subgroup analysis was performed to find correlates of surveillance utilization.
RESULTS
We identified nine studies that met inclusion criteria. The pooled surveillance rate was 18.4% (95%CI 17.8%–19.0%). Surveillance rates were significantly higher among patients followed in subspecialty gastroenterology clinics compared to those followed in primary care clinics (51.7% vs. 16.9%, p < 0.001). Non-Caucasians and patients of low socioeconomic status had lower surveillance rates than their counterparts.
CONCLUSIONS
Utilization rates for HCC surveillance are low, although they are significantly higher among patients followed in subspecialty clinics. Current studies fail to determine why HCC surveillance is not being performed. Future efforts should focus on identifying appropriate intervention targets to increase surveillance rates and reduce socio-demographic disparities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide and has an increasing incidence in the United States.1 Age-adjusted incidence rates of HCC have tripled over the last 30 years, rising from 1.6 to 4.9 per 100,000.2 Cirrhosis of any etiology increases the risk for HCC, with the most common etiologies in the United States being hepatitis C virus (HCV), alcoholic cirrhosis, and non-alcoholic steatohepatitis (NASH).1 Patients with non-cirrhotic hepatitis B are also at high risk.3 Surveillance is defined as regular screening of these high-risk populations for development of HCC. The American Association for the Study of Liver Diseases (AASLD) currently recommends ultrasound with or without alpha fetoprotein (AFP) at 6–12 month intervals.3 Patients with early HCC can achieve 5-year survival rates near 70% with resection and liver transplantation,4 whereas patients with advanced HCC have a median survival below one year.5 Although surveillance can be highly efficacious for detecting early HCC,6 its effectiveness in clinical practice may be impacted by low utilization rates among at-risk patients.7–15
HCC disproportionately affects disadvantaged populations, with the highest age-specific rates occurring among minorities. HCC rates are two times higher in Asian Americans than African Americans, whose rates are two times higher than those in Caucasians.1 Elderly, African Americans and patients of low socioeconomic status (SES) also have poor survival rates.16 The reasons for differences in survival are likely multi-factorial, involving a combination of medical, financial, and social factors. Several studies have reported lower rates of curative therapies being offered, whereas others have postulated biologic differences in tumor behavior.16,17–19 The potential role of differences in surveillance utilization rates has been well documented for other cancer screening modalities, such as mammography and colonoscopy,20–23 but not for HCC surveillance. The purpose of our study was to 1) quantify utilization rates for HCC surveillance among patients with cirrhosis in the United States and 2) to summarize patterns of association between utilization rates and patient socio-demographic characteristics.
METHODS
Literature Search
We conducted a computer-assisted search with the Ovid interface to Medline to identify relevant published articles. We searched the Medline database from January 1, 1990 through March 1, 2011 with the following keyword combinations: [screen$ OR surveillance OR detect$ OR diagnosis] AND [hepatocellular ca$ OR liver ca$]. Given our focus on current utilization of surveillance within the United States, our search was limited to human studies published in English after 1990. Manual searches of references from relevant articles were performed to identify studies that were missed by our computer-assisted search. Additional manual searches of Digestive Diseases Week (DDW), American Association for the Study of Liver Diseases (AASLD), European Association for the Study of the Liver (EASL), American College of Gastroenterology (ACG), and American Society of Clinical Oncology (ASCO) meeting abstracts from 2008–2010 were performed. Finally, consultation with expert hepatologists was performed to identify additional references or unpublished data.
Study Selection
One investigator (A.S.) reviewed all publication titles of citations identified by the search strategy. Potentially relevant studies were retrieved, and selection criteria were applied. The articles were independently checked for inclusion (A.S. and A.Y.) and disagreements were resolved through consensus with a third reviewer (J.T.).
Inclusion criteria included: (i) cohort studies that described receipt of HCC surveillance in patients with cirrhosis, ii) studies from the United States after 1990 so as to be representative of current delivery of care, and (iii) available data regarding socio-demographic information for patients who did and did not receive surveillance. We excluded: i) clinical trials with a surveillance protocol and/or extra nursing support as they do not evaluate delivery of care in a real-world clinical setting and ii) survey studies because of high rates of over-reporting by physicians. Additional exclusion criteria included non-English language, non-human data, and lack of original data. If publications used the same patient cohort, data from the most recent manuscript were included.
Data Extraction
Two reviewers (A.S. and A.Y.) independently extracted required information from eligible studies using standardized forms. A third investigator (J.T.) was available to resolve any discrepancies. Data were collected on age, gender, race/ethnicity, and SES (insurance status and income) for those who received surveillance and those who failed to receive care. We collected data regarding the population of interest (patients with cirrhosis vs. patients with HCC), surveillance definition (ultrasound vs. ultrasound +/− AFP), and surveillance interval (6–12 months vs. less frequently). Finally, data were collected on study design, geographic location and date of the study, and number of patients in each study. Authors were contacted as necessary for missing information.
Clinical End Point and Statistical Analysis
Our primary study outcome was HCC surveillance rates among patients with cirrhosis. Surveillance rates were defined as the proportion of patients who underwent evaluation with imaging or AFP at any specified interval prior to HCC diagnosis. The proportion of patients who received surveillance was derived for each study, and 95% confidence intervals were calculated using the adjusted Wald method. A weighed pooled estimate of surveillance rates was computed by multiplying the surveillance rate point estimate for each study by the proportion of individuals with cirrhosis in that study relative to the number of individuals in all included studies. Subset analyses were planned for the following predefined subsets of studies: 1) the at-risk population, 2) the definition of surveillance, including surveillance interval,24 and 3) the clinical setting, including receipt of subspecialty care.8 All data analysis was performed using Stata 11 (StataCorp, College Station, TX).
RESULTS
Literature Search
The computer-assisted search yielded 9,289 potentially relevant articles. After initial review, 157 titles were potentially appropriate, and these abstracts were reviewed. Nineteen publications underwent full-text review, and thirteen were excluded. Six studies were excluded because they described the efficacy of surveillance (and not effectiveness), three described HCC treatments, two described HCC epidemiology, and two articles did not provide socio-demographic predictors for surveillance. The remaining six studies met all inclusion criteria (Fig. 1). Searches of annual meeting abstracts yielded two relevant abstracts; sufficient data for inclusion were obtained for both abstracts after contacting the authors. Finally, recursive literature searches identified one additional article that met inclusion criteria, producing a total of nine studies for inclusion in this meta-analysis7–15 (Table 1).
Surveillance Utilization
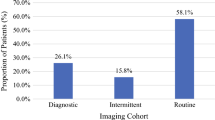
Among all nine included studies, 3,183 of 17,286 (18.4%, 95%CI: 17.8–19.0%) patients received surveillance according to the definition established by each study (Table 2, Fig. 2). Surveillance rates among the studies ranged from 11% to 64%. We examined whether the following differences in study design explained the range in surveillance rates: 1) study population, 2) definition of surveillance, and 3) clinical setting of each study.
Study Population
Four studies retrospectively assessed whether patients with HCC had surveillance prior to their diagnosis8–11 and five studies retrospectively assessed surveillance among patients with a known diagnosis of cirrhosis.7,12–15 The surveillance rates between the two groups were not statistically different, 18.7% (95%CI 17.2–20.3%) and 18.4% (95%CI 17.8–19.0%), respectively.
Definition of Surveillance among Included Studies
There were a variety of definitions for surveillance among the nine studies, including differences in surveillance tests and surveillance intervals. Six of the studies determined surveillance rates via manual chart review,9–11,13–15 whereas three studies used administrative data.7,8,12 Only four studies assessed surveillance utilization every 6–12 months,10,13–15 consistent with AASLD guidelines, whereas five studies used a less stringent definition of surveillance, such as less frequent intervals.7–9,11,12 Furthermore, patients who received AFP alone accounted for over one-third of screened patients in four of the latter five studies.7–9,11 Current guidelines strongly discourage using AFP alone as a surveillance tool if imaging studies are available. We found a significantly higher rate of surveillance in the four studies that used more stringent surveillance regimens compared to the studies with a less stringent regimen, (51.7% vs. 16.9%, p < 0.001).
Clinical Setting and Subspecialty Care
There were four studies in which most patients received subspecialty care by gastroenterologists/hepatologists, including three studies from academic centers and one study from a community gastroenterology clinic.10,13–15 There were five studies in which most patients received care through their primary care physicians, including two VA hospital studies and three multi-center database studies.7–9,11,12 We found a pooled surveillance rate of 51.7% (95%CI: 48.2–55.3%) in studies where patients received subspecialty care, compared to a pooled surveillance rate of 16.9% (95%CI 16.3–17.5%) in studies where most patients were followed by primary care physicians (p < 0.001). Furthermore, subspecialty care was found to be a significant predictor of surveillance in two of the multi-center database studies.8,12
Correlates of HCC Surveillance
Patient and clinic factors associated with higher utilization rates for HCC surveillance are listed in Table 3.
Age
Extremes of age have been demonstrated to be a negative predictor of HCC surveillance, with lower surveillance rates observed in patients older than 65 years and those younger than 50 years. Davila et al. demonstrated that patients younger than 50 years old were less likely to have surveillance compared to patients aged 50–65 years old (OR 0.79, 95%CI 0.64-0.99).7 Similarly patients over the age of 65 years have significantly lower rates of surveillance than their younger counterparts (p = 0.01).9
Gender
There is conflicting data regarding the impact of gender on HCC surveillance utilization. Routine surveillance was performed more often in females in the SEER-Medicare (21.5% vs. 14.9%, p = 0.006)8 and North Carolina Medicaid databases (OR 1.18, 95%CI 1.02–1.37),12 but the contrary was true in the study by Singal and colleagues (66.4% vs. 43.9%, p = 0.03).14 Other studies that evaluated the impact of gender found no difference in surveillance rates between males and females.7,10,13,15
Race
Several studies demonstrated disparities in HCC surveillance utilization according to race. Two studies from the VA demonstrated significantly higher rates among Caucasian patients than non-Caucasians, but neither study distinguished between non-Caucasian races.9,11 In the national VA database, African Americans were significantly less likely to receive surveillance than Caucasians (OR 0.60, 95%CI 0.45–0.81) and other non-Caucasians had a trend toward lower surveillance rates (OR 0.73, 95%CI 0.49–1.08).7 In the SEER-Medicare database, the highest surveillance rates were found among Asian patients (28.1%) and the lowest rates among Black patients (12.2%), with intermediate rates in Caucasian (14.9%) and Hispanic (16.8%) patients (p < 0.001).8
Socioeconomic Status
The impact of SES on HCC surveillance utilization has only been evaluated in three studies. Several studies evaluated patients with insurance12,13 or easy access to health care7,9,11 and therefore were unable to determine the impact of SES on surveillance utilization. Davila and colleagues demonstrated that income level was a strong predictor of surveillance utilization using the SEER-Medicare database.8 Patients who lived in zip codes with higher median income and/or education levels had significantly higher surveillance utilization. In the study by Singal and colleagues, patient education and employment status had a trend toward predicting surveillance rates, although neither reached statistical significance.14
DISCUSSION
Although HCC surveillance is recommended by the AASLD and is considered to be standard-of-care by many physicians, our meta-analysis highlights its underutilization in clinical practice. Low utilization rates were first reported by Leykum and colleagues11 and have been replicated in several studies, including three analyses from multi-center databases.7,8,12 Our systematic review is the first to critically summarize these studies and document the socio-demographic disparities in HCC surveillance programs. Most studies found surveillance rates below 30%, although rates of 60-80% were reported in single-center studies from tertiary care and/or community practices. There were also significant socio-demographic disparities with the lowest surveillance rates in non-Caucasians and patients of low SES.
Surveillance rates in HCC are substantially lower than those currently seen for other cancers. In fact, surveillance rates for colon, breast, and cervical cancer are currently greater than 60% for most of the United States.25 This difference in surveillance rates is likely due to a combination of issues, including under-recognition of at-risk individuals with cirrhosis and poor education of primary care physicians regarding the importance of HCC surveillance.
HCC surveillance is a complex process, with multiple steps that are prone to failure.26 Providers must accurately identify high-risk patients, they must refer these patients for surveillance, the healthcare system must schedule the tests, and patients must comply with surveillance recommendations.27 This challenge is even more relevant in primary care settings, where providers face increasing time constraints and might be less knowledgeable about HCC guidelines. Current studies fail to provide an in-depth analysis to clarify which factors mediate or moderate underutilization of HCC surveillance. Future research should investigate correlates of these breakdowns to identify appropriate intervention targets.
Under-recognition of patients with cirrhosis may be an important factor in the low surveillance rates for HCC. Many patients with well-compensated cirrhosis are asymptomatic, but they remain at high risk for developing HCC and warrant surveillance. This was suggested in the SEER-Medicare study, as HCC surveillance rates were substantially higher in patients with recognized cirrhosis than the remainder of the cohort (29% vs. 17%).8 Similarly, Stravitz and colleagues reported that 21.9% of patients were not recognized as having cirrhosis prior to their HCC diagnosis.28 It is possible that some patients with unrecognized cirrhosis could be identified using non-invasive fibrosis markers, which would permit earlier application of appropriate surveillance. Unfortunately, this intervention would likely be insufficient in isolation given that surveillance rates among patients with known cirrhosis are still disappointingly low, suggesting the need for concurrent issues to be addressed.
Patients who received subspecialty care from gastroenterologists/hepatologists had significantly higher surveillance rates than patients followed by primary care physicians (52% vs. 17%, p < 0.001). Four studies evaluating patients followed in subspecialty clinics reported the highest utilization of surveillance, with all having rates of 60–80%.10,13–15 Three studies were conducted in tertiary-care academic centers, but this finding was also replicated in a community-based gastroenterology practice. Subspecialty care was also a strong predictor of surveillance utilization in the North Carolina Medicaid health claims and SEER-Medicare databases.8,12 Although socioeconomic status and access to care could be potential confounding factors in this relationship, the association between subspecialty care and surveillance utilization persisted on multivariate analysis after adjusting for patient-level and system-level factors.8 These results suggest that differences in surveillance rates are likely related to variation in provider knowledge and attitudes, rather than patient-level factors such as socioeconomic status or system-level factors related to the academic center.
Currently, primary care physicians follow most patients with cirrhosis nationally, with only 20–40% of cirrhotic patients being followed by gastroenterologists or hepatologists.8 Unfortunately, referring every patient with cirrhosis to a subspecialist is not a viable option, particularly given limited availability of subspecialty care in some areas. Accordingly, educating primary care physicians how to recognize patients with cirrhosis and about the importance of HCC surveillance is one crucial step to improve surveillance rates. Per current AASLD guidelines,3 primary care education should reinforce that AFP is an effective screening tool only if used in conjunction with imaging studies. Further studies are necessary to characterize the effect of provider factors on surveillance utilization and develop intervention strategies to increase HCC surveillance rates through primary care clinics.
Racial and socioeconomic disparities have been well described in the survival of patients with HCC.16 Although prior studies have suggested difference in tumor biology and/or delivery of treatment, our meta-analysis is the first to highlight the importance of socio-demographic disparities. Patients who are elderly, non-Caucasian, and of low SES suffer from significantly lower HCC surveillance rates than their counterparts. While current studies suggest an association between socio-demographic factors and HCC surveillance practices, none have explored why surveillance is not being performed in these subgroups. The roles of patient attitudes, co-morbid conditions, and barriers to accessing care have not been clearly evaluated. For example, elderly patients and patients of low SES may have lower surveillance rates due to difficulty accessing medical care or a higher rate of co-morbid conditions that would limit the benefit of surveillance. Similarly, race and SES are often highly correlated so independent causal effects can be difficult to identify. It is important to note that current studies were all performed in highly uniform populations, with the majority of patients being male, Caucasian, and insured so confirmatory studies in racially and socioeconomically diverse patient populations are necessary.
The primary limitation of our meta-analysis was our inability to identify specific reasons for underutilization of HCC surveillance. Current studies did not distinguish cases in which physicians failed to order surveillance from cases in which surveillance was not appropriate (e.g., patients with significant co-morbidities or those with Child C cirrhosis who were not transplant candidates) or cases in which patients were non-adherent after surveillance was recommended. Studies evaluating the reasons behind surveillance under-utilization are necessary to identify intervention targets that can increase surveillance rates. Furthermore, all studies to date have evaluated homogeneous populations, and studies in racially and socioeconomically diverse populations are necessary. Finally, many studies use operational definitions for surveillance that are not consistent with AASLD guidelines. Only six studies assessed utilization every 12 months, and none reported surveillance with six-month intervals. Additionally, over one-third of patients in several studies had surveillance with AFP alone, which is contrary to current guidelines. The recent change in AASLD guidelines to six-month surveillance intervals suggests it is important for future studies to use stringent definitions of surveillance when assessing utilization. This variability in definitions used for surveillance makes it difficult to compare surveillance rates across studies. Clear consistent definitions and measures are necessary to better interpret and quantify HCC surveillance rates.24
In summary, HCC surveillance is underutilized nationally with most studies reporting rates below 30% and a pooled surveillance rate of 18.4%. Subspecialty care appears to be the strongest predictor of higher surveillance rates, with several studies demonstrating utilization rates of 60-80% in patients followed by gastroenterologists/hepatologists. There are also significant socio-demographic disparities with the lowest surveillance rates in non-Caucasians and patients of low SES. Further studies are needed to explore reasons for the underutilization of surveillance, particularly in these disadvantaged subgroups. These studies will be the first crucial step in identifying appropriate intervention targets to increase HCC surveillance rates and reduce socio-demographic disparities.
REFERENCES
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132(7):2557–2576.
Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;27(9):1485–1491.
Bruix J, Sherman M. Management of Hepatocellular Carcinoma: An Update. Hepatology. 2011;53(3):1020–1022.
Singal AG, Marrero JA. Recent advances in the treatment of hepatocellular carcinoma. Curr Opin Gastroenterol. 2010;26(3):189–195.
Llovet JM, Bustamante J, Castells A, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29(1):62–67.
Singal A, Volk ML, Waljee A, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30(1):37–47.
Davila JA, Henderson L, Kramer JR, et al. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154(2):85–93.
Davila JA, Morgan RO, Richardson PA, et al. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology. 2010;52(1):132–141.
Davila JA, Weston A, Smalley W, El-Serag HB. Utilization of screening for hepatocellular carcinoma in the United States. J Clin Gastroenterol. 2007;41(8):777–782.
Jou JH, Chen PH, Jazwinski A, et al. Rates of surveillance and management of hepatocellular carcinoma in patients evaluated at a liver transplant center. Dig Dis Sci. 2010;55(12):3591–3596.
Leykum LK, El-Serag HB, Cornell J, Papadopoulos KP. Screening for hepatocellular carcinoma among veterans with hepatitis C on disease stage, treatment received, and survival. Clin Gastroenterol Hepatol. 2007;5(4):508–512.
Palmer L, Kappelman M, Porter C, Sandler R. Screening for Hepatocellular Carcinoma in a Medicaid Cirrhotic Population: Opportunities for Improvement. Gastroenterology. 2010;138(5(S1)):S-796.
Patwardhan V, Paul S, Corey K, et al. Hepatocellular Carcinoma Screening Rates in Cirrhotic Patients Differ by Specialty Practice. Hepatology. 2010;52(4(S1)):1249A.
Singal A, Volk M, Rakoski M, et al. Patient Involvement is Correlated with Higher HCC Surveillance in Patients with Cirrhosis. J Clin Gastroenterol. 2011;45(8):727–732.
Wong CR, Garcia RT, Trinh HN, et al. Adherence to screening for hepatocellular carcinoma among patients with cirrhosis or chronic hepatitis B in a community setting. Dig Dis Sci. 2009;54(12):2712–2721.
Artinyan A, Mailey B, Sanchez-Luege N, et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010;116(5):1367–1377.
Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma: tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc. 2006;98(12):1934–1939.
Davila JA, El-Serag HB. Racial differences in survival of hepatocellular carcinoma in the United States: a population-based study. Clin Gastroenterol Hepatol. 2006;4(1):104–110. quiz 104–105.
Siegel AB, McBride RB, El-Serag HB, et al. Racial disparities in utilization of liver transplantation for hepatocellular carcinoma in the United States, 1998–2002. Am J Gastroenterol. 2008;103(1):120–127.
Du XL, Fang S, Vernon SW, et al. Racial disparities and socioeconomic status in association with survival in a large population-based cohort of elderly patients with colon cancer. Cancer. 2007;110(3):660–669.
Du XL, Meyer TE, Franzini L. Meta-analysis of racial disparities in survival in association with socioeconomic status among men and women with colon cancer. Cancer. 2007;109(11):2161–2170.
Lloyd SC, Harvey NR, Hebert JR, et al. Racial disparities in colon cancer. Primary care endoscopy as a tool to increase screening rates among minority patients. Cancer. 2007;109(2 Suppl):378–385.
Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt). 2008;17(9):1477–1498.
Vernon SW, Briss PA, Tiro JA, Warnecke RB. Some methodologic lessons learned from cancer screening research. Cancer. 2004;101(5 Suppl):1131–1145.
National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, MD 2010.
Taplin SH, Rodgers AB. Toward improving the quality of cancer care: addressing the interfaces of primary and oncology-related subspecialty care. J Natl Cancer Inst Monogr. 2010;2010(40):3–10.
Zapka JG, Taplin SH, Solberg LI, Manos MM. A framework for improving the quality of cancer care: the case of breast and cervical cancer screening. Cancer Epidemiol Biomarkers Prev. 2003;12(1):4–13.
Stravitz RT, Heuman DM, Chand N, et al. Surveillance for hepatocellular carcinoma in patients with cirrhosis improves outcome. Am J Med. 2008;121(2):119–126.
Acknowledgements
All of the listed authors have made substantial contributions to the conception and design of the study, acquisition of data and/or analysis and interpretation of the data, drafting of the manuscript, and final approval of the version to be submitted.
Financial Disclosures
This project was supported in part by grant KL2 RR024983-04 and NIH CTSA grant UL1 RR024982 and the American College of Gastroenterology Junior Faculty Development Award
Conflicts of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singal, A.G., Yopp, A., S. Skinner, C. et al. Utilization of Hepatocellular Carcinoma Surveillance Among American Patients: A Systematic Review. J GEN INTERN MED 27, 861–867 (2012). https://doi.org/10.1007/s11606-011-1952-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1952-x