Abstract
Purpose of Review
Cardiac magnetic resonance imaging (CMR) use in the context of heart failure (HF) has increased over the last decade as it is able to provide detailed, quantitative information on function, morphology, and myocardial tissue composition. Furthermore, oxygenation-sensitive CMR (OS-CMR) has emerged as a CMR imaging method capable of monitoring changes of myocardial oxygenation without the use of exogenous contrast agents.
Recent Findings
The contributions of OS-CMR to the investigation of patients with HF includes not only a fully quantitative assessment of cardiac morphology, function, and tissue characteristics, but also high-resolution information on both endothelium-dependent and endothelium-independent vascular function as assessed through changes of myocardial oxygenation.
Summary
In patients with heart failure, OS-CMR can provide deep phenotyping on the status and important associated pathophysiology as a one-stop, needle-free diagnostic imaging test.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a complex clinical syndrome characterized by dyspnea or an exertional capacity limitation caused by impaired ventricular filling or emptying, or both [1]. Currently, an estimated 26 million people are diagnosed with heart failure (HF) worldwide [2]. It is a leading cause of hospitalization, and its prevalence is increasing. The increase in prevalence has been attributed to factors including an aging population, improvements in the long-term survival of patients with chronic HF, and a reduction in short-term mortality of other cardiovascular conditions known to cause HF [2, 3].
A recent joint consensus statement on the classification of HF has subcategorized HF based on functional and/or structural abnormalities resulting in either a reduction in overall systolic function (LVEF ≤40%, heart failure with reduced ejection fraction, HFrEF), preserved overall systolic function (LVEF ≥50%, heart failure with preserved ejection fraction, HFpEF), an intermediate functional classification (LVEF 40–49%, heart failure with mildly reduced ejection fraction, HFmrEF), or a classification for functional improvement (LVEF ≤40% at baseline and a ≥10 point improvement on second measurement with an LVEF ≥40%, heart failure with improved ejection fraction, HFimpEF) [4]. These HF phenotypes may display different clinical characteristics, comorbidities, outcomes, response to therapy, and prognoses [5,6,7]. There is a need for improved recognition of the specific causes of acute HF to establish an HF diagnosis, optimize therapy, and improve overall quality of life for HF patients [4, 8, 9].
Cardiac imaging is routinely used in the investigation of all HF phenotypes. Echocardiography is typically applied as the first-line imaging modality for HF. It is less expensive than other frequently used imaging modalities and widely available and can be used at the bedside. However, image quality and accuracy of quantitative results are inconsistent [4]. Importantly, echocardiography provides little information about the myocardial tissue [10] or coronary vascular function.
Cardiovascular magnetic resonance imaging (CMR) is the current gold standard for quantitative functional assessment of the heart. CMR is also able to provide detailed information on cardiac morphology and especially on the composition of myocardial tissue [11, 12]. This includes the identification of myocardial edema, fibrosis, or infiltration with amyloid, fat, or iron. Consequently, the use of CMR in patients with HF has significantly increased over the past decade to aid in diagnosis, risk stratification, therapeutic decision-making, and monitoring [13, 14]. CMR has been shown to more accurately classify HF patients into subgroups based on left ventricular ejection fraction (LVEF) when compared with echocardiography [15]. Additionally, studies have indicated that in patients with HFpEF, CMR often identifies new pathology in HFpEF patients and better establishes specific diagnoses than echocardiography [16, 17]. CMR is a versatile, comprehensive imaging diagnostic tool for the quantitative assessment of cardiac morphology, function, and tissue status in patients with HF [13].
Coronary vascular function plays an important role in HF, with a known role of endothelial dysfunction in HF patients with and without macrovascular ischemic heart disease [18, 19]. Coronary microvascular dysfunction (endothelial-dependent or endothelial-independent) is also associated with cardiovascular risk factors such as diabetes and hypertension and is considered an early marker of atherosclerosis [20]. Moreover, endothelial dysfunction has also been identified as a key part of the pathophysiology of HFrEF and HFpEF, associated with worse prognosis and increased rates of cardiovascular events [21, 22, 23••, 24]. Diagnostic techniques that can assess endothelium-dependent pathways may thus provide more meaningful clinical information for personalized therapeutic decision-making.
Over the past decade, oxygenation-sensitive CMR (OS-CMR) has emerged as a CMR imaging method capable of assessing endothelial dysfunction through monitoring changes of myocardial oxygenation without the use of exogenous contrast agents, based on the intrinsic magnetic properties of oxy- and deoxyhemoglobin [25, 26, 27•, 28,29,30]. The unique ability of OS-CMR to non-invasively monitor changes of myocardial oxygenation has been demonstrated in animal models, healthy volunteers, and in patients with macrovascular and microvascular disease states including coronary artery disease (CAD), ischemia with no obstructive coronary artery stenosis (INOCA), obstructive sleep apnea (OSA), hypertrophic cardiomyopathy (HCM), aortic stenosis, dilated cardiomyopathy (DCM), chronic heart failure, and post-transplantation [26, 27•, 31,32,33,34, 35••, 36].
We review OS-CMR and discuss its potential contributions to the investigation of patients with heart failure and introduce new imaging biomarkers to aid in the risk stratification and understanding of the underlying pathophysiology in heart failure patients.
The Blood Oxygen Level-Dependent (BOLD) Effect
The ability of magnetic resonance imaging (MRI) to harness the intrinsic magnetic differences of oxygenated vs deoxygenated hemoglobin in blood to visualize changes in oxygenation states was first demonstrated in 1990 [37]. Changes of the oxygenation state of hemoglobin in tissue result in changes of signal intensity in certain MRI images that are sensitive to the so-called blood oxygen level-dependent (BOLD) effect: Oxyhemoglobin has no unpaired electrons and no magnetic moment and does not significantly alter the peri-molecular magnetic field. Deoxyhemoglobin on the other hand has unpaired electrons with a destabilizing effect on surrounding protons, inducing its paramagnetic effect that results in an accelerated relaxation of surrounding protons. In MRI images that are “BOLD-sensitive” (typically T2*-weighted images), this effect leads to a decreased signal intensity of tissue with a higher concentration of deoxyhemoglobin [37]. Oxygenation-sensitive CMR (OS-CMR) can utilize the BOLD effect in clinical settings to monitor dynamic changes in deoxyhemoglobin concentrations as a marker for myocardial oxygenation. Such changes can be induced by vasoactive or other interventions that alter myocardial blood volume and blood flow or otherwise alter the balance between oxygen demand and supply [38,39,40,41,42,43].
Myocardial oxygen balance is subject to a complex coupling between myocardial ventricular function, myocardial oxygen consumption, and coronary blood flow. Under conditions of an increased myocardial work, healthy coronary vasculature will meet the additional oxygen demand by upregulating coronary blood flow through vasodilation [44]. Vasodilation without an associated increase of myocardial oxygen demand however results in a decrease in deoxyhemoglobin concentration (static demand, increase of supply). This change will lead to a reduction of the BOLD effect in myocardial tissue and thereby to an increase in BOLD-sensitive MRI signal intensity [38]. Vasoactive interventions can therefore be used to induce a detectable change of myocardial oxygenation. Dynamic changes of BOLD-sensitive MRI signal intensity during OS-CMR image acquisition in combination of vasoactive interventions can therefore be used as a marker for coronary vascular function.
Vasoactive Interventions for Assessing Coronary Vascular Function
Vasoactive stress can be induced through several different mechanisms including pharmacologic vasodilation (increase of blood/oxygen supply, no significant change of oxygen demand) or physical stress (increase of blood/oxygen supply with associated increase of oxygen demand). CMR stress testing typically relies on pharmacologic vasodilators to induce a response from the myocardial vasculature. Endothelium-independent pharmacologic vasodilators such as adenosine act to uncouple myocardial blood flow from oxygen demand, inducing excess (above demand level) myocardial perfusion in healthy tissue. This intervention decreases deoxyhemoglobin concentration and results in an increased OS-CMR signal intensity [45]. Endothelium-dependent vasodilation through the use of respiratory maneuvers can be utilized to assess changes in myocardial oxygenation through the actions of carbon dioxide (CO2), a known vasodilator [46]. An inadequate response of the coronary vasculature to an increased demand results in a higher concentration of deoxyhemoglobin. OS-CMR has been used to assess each of these different mechanisms, each with their own strengths and limitations for overall feasibility and ability to add information in the clinical context of heart failure.
OS-CMR in Heart Failure
The diagnostic work-up of patients with suspected HF consists of an assessment of left ventricular systolic function and the determination of the presence or absence of ischemic disease [47].
Heart Failure: Ischemic vs Non-ischemic Cardiomyopathy
Coronary artery disease (CAD) accounts for approximately half of acute HF patients and half of HFrEF patients [48]. Given the therapeutic options of coronary revascularization and prevention treatment, the determination of the presence or absence of ischemic heart disease is critical to clinical decision-making in patients with HF. Coronary angiography is the current gold standard test to identify obstructive CAD, with fractional flow reserve (FFR) being a quantitative marker for the hemodynamic relevance of an observed coronary artery stenosis.
While first-pass perfusion stress CMR is currently not a first-line strategy for the investigation of patients with HF if non-ischemic etiology is suspected [1], its utility in suspected ischemic HF is however undisputable. Recent studies have demonstrated that stress CMR may not only be very accurate in identifying tissue subject to severe coronary artery stenoses, but also be part of the most cost-effective strategies to do that [49, 50]. Additionally, the clinical use of first-pass perfusion stress CMR has been associated with less coronary angiographies in patients with suspected CAD and in less revascularizations, even when compared to coronary angiography with FFR, all with similar clinical outcomes [51].
CMR first-pass perfusion is limited by the need for the intravenous application of gadolinium-based contrast agents and vasodilatory agents.
OS-CMR of coronary vascular function does not require contrast agents. In combination with adenosine, it can be used for assessing myocardial perfusion and oxygenation in a number of disease states [28]. In patients with CAD, adenosine OS-CMR could accurately detect regionally reduced myocardial perfusion and oxygenation in myocardial territories downstream of a significant coronary artery stenosis [52, 53]. Additionally, adenosine OS-CMR studies detected a regional myocardial perfusion and oxygenation dissociation in non-flow limiting CAD, indicating that perfusion deficits do not always indicate underlying oxygenation deficits [54,55,56].
A dissociation between myocardial perfusion and oxygenation may be an important pathophysiologic component in HF and therefore critical for our understanding of the pathophysiology of HF, with an impact on management strategies in both, ischemic and non-ischemic HF. This is particularly important in light of recent evidence that when comparing medical therapy to procedural intervention as a first-line treatment strategy, there were no significant changes in patient clinical outcomes [51, 57].
The endogenous contrast in OS-CMR that eliminates the need for gadolinium-based contrast agents represents a first important step in moving towards a needle-free CMR non-invasive stress test [52, 58]. An approach using vasodilatory agents however still requires an inconvenient and mildly risky administration of pharmacologic agents. Moreover, adenosine and analogues induce vasodilation through endothelium-independent mechanisms. A microvascular response to increased myocardial oxygen demand however may use endothelium-independent or endothelium-dependent mechanisms. However, endothelial-dependent dysfunction has significant prognostic value in HF and has been associated with an increased mortality risk in patients with HF [19, 59]. Endothelium-dependent interventions more accurately resemble physiological stress and may be more informative in terms of therapeutic consequences [60, 61].
Respiratory challenges, especially manipulations in blood carbon dioxide (CO2) and oxygen levels, were explored due to their ability to act as endothelial-dependent vasoactive mechanisms. Inhaled gas and breathing maneuvers have been investigated based on the underlying principle that alterations in arterial carbon dioxide, and to a lesser extent oxygen, result in endothelial-dependent vascular changes similar to those obtained with physiologic stress [62]. Carbon dioxide (CO2) is a significant modulator of vascular tone in the cerebral and coronary circulation, with hypercapnia resulting in vasodilation and hypocapnia resulting in vasoconstriction [46, 63].
OS-CMR studies have been performed by directly modulating the percentage of carbon dioxide in inhaled air through a face mask or nasal cannula, resulting in consistent and reproducible changes in signal intensity [64,65,66,67]. Recently, OS-CMR with intermittent carbon dioxide was successfully used to perform a rapid, whole heart, free-breathing acquisition in an animal model [68]. Induced hypercapnia however is associated with often intolerable side effects related to the urge to breathe and associated anxiety [69].
Respiratory maneuvers such as hyperventilation and breath-holding have also been evaluated in humans for their ability to modify oxygen and carbon dioxide concentrations without the need for inspired gas manipulations or additional equipment [40, 70, 71].
A combination of hyperventilation with a subsequent breath-hold as a standardized breathing maneuver has emerged as an effective mechanism of inducing vasoactive stress [25, 67, 72, 73]. The standardized breathing maneuver consists of a 60-s period of paced deep breathing (hyperventilation) at 30 breaths per minute, inducing coronary vasoconstriction, followed by a voluntary maximal breath-hold, inducing coronary vasodilation (Fig 1) [26].
Oxygenation-sensitive CMR (OS-CMR) scanning protocol with pharmacologic stress agent or using a standardized breathing maneuver. Hyperventilation leads to a coronary vasoconstrictive response through a decrease in arterial carbon dioxide, while the following breath-hold increases arterial carbon dioxide and induces coronary artery dilatation. Myocardial signal intensity changes in OS-CMR images are measured at the end of the hyperventilation (maximal vasoconstriction) to the end of the breath-hold (maximal vasodilatation).
This maneuver in combination with OS-CMR has demonstrated breathing-induced changes in myocardial oxygenation (BMORE) in a healthy population [43, 74]. BMORE OS-CMR can detect blunted myocardial oxygenation in myocardial territories subtended by an angiographically significant coronary artery stenosis in both animal models and patients with CAD [26, 27•]. Of note, BMORE OS-CMR may have a more significant effect on myocardial oxygenation changes than adenosine OS-CMR, with less side effects [45]. Used in conjunction with the endogenous contrast of OS-CMR, BMORE was shown to provide a safe, fast, non-invasive, and convenient method for assessing coronary vascular function, without the use of needles, exogenous contrast agents, radioactivity, or specialized additional equipment.
Heart Failure—Microvascular Dysfunction
Adenosine and OS-CMR have demonstrated to be feasible and accurately identify CAD through a regionally impaired myocardial perfusion and oxygenation response in areas of macrovascular disease.
OS-CMR has also been used to assess microvascular disease and dysfunction.
Ischemia With No Significant Coronary Artery Disease
Reports estimate that up to half of patients who undergo a coronary angiography have no obstructive CAD, a clinical scenario that is especially prevalent in women [75, 76•]. Studies have demonstrated that over 50% of patients with ischemia with no obstructive coronary artery disease (INOCA) have microvascular dysfunction (MVD) [77].
An improved understanding of the underlying pathophysiology of INOCA would help guide personalized treatment strategies in these patients with a known increased risk of cardiovascular events and the development of HFpEF [76•, 77].
Adenosine stress perfusion CMR demonstrated subendocardial myocardial perfusion deficits in patients with INOCA [78]. However, these findings have not been replicated in subsequent studies utilizing adenosine stress perfusion CMR and OS-CMR [79]. Recently, novel biomarkers derived from BMORE OS-CMR images demonstrated regional heterogeneity in the myocardial oxygenation of INOCA patients without globally reduced oxygenation or perfusion abnormalities [35••] (Fig 2).
The impact of the breathing maneuver induced changes in myocardial oxygenation reserve on the myocardium and associated heterogenous myocardial oxygenation changes as reflected by a change of signal intensity in OS-CMR images in the 3 spatial dimensions. Regional heterogeneity in myocardial oxygenation in women with INOCA compared with healthy volunteers. Schema demonstrating the determination of regional variability in signal intensity using radial, circumferential, and longitudinal differences. Radial differences were defined as the sum of the absolute differences between the endo- and epicardium in each of the myocardial segments. Circumferential differences were the sum of the absolute differences between myocardial segments within the endo- and epicardium. Longitudinal differences were the sum of the absolute differences within the endo- and epicardium for corresponding segments of each slice acquired. INOCA, ischemia with no obstructive coronary artery disease; OS-CMR, oxygenation-sensitive cardiac magnetic resonance imaging; SI, signal intensity; *P<0.05; **P <0.01 (figure modified from Elharram, Circulation, 2021)
Regional myocardial deficits are consistent with previous observations of a maladaptive physiologic response to exercise and heterogenous flow in MVD, suggested to be a result of a variable combination of increased vasoconstriction and impaired vasodilation [80, 81]. These findings suggest a potential role of endothelium-dependent microvascular dysfunction in this patient population [35••], consistent with previously published evidence for heterogeneity of microvascular function [80].
Non-ischemic Heart Failure
Once significant CAD is excluded, the accurate identification of the etiology and associated pathomechanisms with HF often remains a significant clinical challenge. CMR has demonstrated increased diagnostic accuracy when compared to echocardiography in a non-ischemic HF population [16, 17]. Beyond the more accurate information on function including strain however, the potential of OS-CMR to investigate myocardial oxygenation and therefore provide additional insights on the individual underlying pathophysiology has been demonstrated in patients with non-ischemic HF.
OS-CMR has been used to investigate a number of microvascular disease states characterized by microvascular dysfunction. OS-CMR demonstrated a globally reduced BMORE in patients with obstructive sleep apnea, especially when undergoing positive airway pressure therapy, and after heart transplantation even in the absence of cardiac allograft vasculopathy [34, 36]. Preliminary evidence from OS-CMR studies has demonstrated a reduced BMORE in HFrEF and with healthy aging [82, 83]. In a non-ischemic, dilated cardiomyopathy population, one study utilizing adenosine OS-CMR found a reduced myocardial perfusion response without a concomitant reduction in myocardial oxygenation, suggesting a dissociation between microvascular dysfunction and oxygenation [32]. Mahmod et al have demonstrated a reduced perfusion and oxygenation reserve in severe aortic stenosis without epicardial CAD, indicating coronary microvascular dysfunction [33]. The perfusion-oxygenation reduction seen in severe aortic stenosis with left ventricular hypertrophy is consistent with previous OS-CMR findings in a hypertensive left ventricular hypertrophy population [84]. In an overt hypertrophic cardiomyopathy (HCM) population, adenosine OS-CMR demonstrated an impaired myocardial perfusion/oxygenation. In HCM mutation carriers without overt left ventricular hypertrophy, a reduction in overall myocardial oxygenation was observed without a corresponding reduction in perfusion that was associated with a risk for arrhythmia [31, 85]. Impaired myocardial oxygenation and vasodilation was also observed in pulmonary hypertension with unobstructed epicardial coronary arteries likely reflecting microvascular dysfunction [86].
The impaired myocardial oxygenation response in these populations is consistent with our current understanding of a higher oxidative stress, reduced nitric oxide production, and endothelial dysfunction in these populations [34].
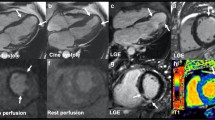
OS-CMR provides information on myocardial oxygenation and can obtain quantitative markers of myocardial ischemia and microvascular dysfunction across a number of disease states (Fig 3).
Oxygenation-sensitive CMR (OS-CMR) in a heart failure patient demonstrating a globally impaired myocardial oxygenation reserve, in a patient with coronary artery disease with a significant left anterior descending (LAD) lesion with a fractional flow reserve of 0.58 demonstrating regionally impaired myocardial oxygenation, and a healthy volunteer demonstrating a globally increased myocardial oxygenation response to a combined vasoactive breathing maneuver.
Table 1 provides an overview of studies on myocardial oxygenation in patients with heart failure.
OS-CMR and Myocardial Strain
While LVEF has been widely used for subclassifying HF phenotypes, it is not a sensitive marker of more subtle changes in myocardial function. Therefore, measuring myocardial deformation, or strain, using imaging has received more and more attention as a useful approach for detecting subclinical changes in myocardial function with better risk stratification than LVEF [4, 87, 88]. Strain imaging can evaluate strain in the three distinct layers of myocardial muscle fibers, i.e., endo-, mid-, and epicardium [89]. Strain is reported as deformation in three different directions, radial (concentric wall thickening), longitudinal (shortening of the ventricular long axis), and circumferential (tangential/rotational deformation) [89]. Longitudinal strain can be used to predict LVEF change and HF phenotype as persistent HFrEF or HFimpEF [90] and appears to be a more accurate predictor of decompensation and mortality in both acute and chronic heart failure patients than LVEF [91,92,93]. Global longitudinal strain has therefore been found to add incremental value and have greater prognostic value than LVEF [92]. These findings have led some authors to suggest the standard use of strain parameters in all HF patients to assess both systolic and diastolic dysfunction [4, 94, 95].
Strain imaging has traditionally been assessed by speckle tracking echocardiography.
CMR strain techniques such as fast strain-encoded CMR (fSENC), feature tracking (FT), or tissue tracking (TT) have emerged as convenient and readily available techniques that can accurately and reproducibly obtain strain parameters [96,97,98]. CMR FT-derived longitudinal strain recently demonstrated good correlation to echocardiography in the setting of acute myocardial infarction [99]. Combined CMR fSENC with standardized breathing maneuvers can yield a high diagnostic accuracy (95% sensitivity) for the detection of patients with suspected CAD, with significantly shorter acquisition times than established methods [100••].
In contrast to fSENC, CMR FT/TT does not need additional images as it can measure strain in routine cine images as used for ventricular volumes [101, 102]. Stress longitudinal strain from CMR FT with vasodilator stress was an incremental and independent predictor of adverse cardiac events in patients with known or suspected CAD [103]. In the context of HF, CMR reveals a transmural strain gradient from endocardium (highest strain) to epicardium (lowest strain values) that is blunted in patients with HF and lower ejection fraction (HFmEF and HFrEF) [101]. CMR FT has been suggested as having potential to be the new gold standard for assessment of systolic function [104]. Additionally, abnormal longitudinal strain has been found to be a useful prognostic marker in patients with HFpEF and in patients with dilated cardiomyopathy, incremental to LVEF [57, 105•, 106]. The observed longitudinal strain impairment reflects LV stiffness and impaired relaxation, causes for the observed “diastolic dysfunction” in HFpEF [94, 105•, 107]. However, although diastolic dysfunction plays a fundamental role in the pathophysiology of HFpEF, worsening of diastolic dysfunction is associated with other cardiometabolic comorbidities and even physiological aging [108]. Therefore, strain parameters should be used in a proper clinical context and in conjunction with other imaging parameters.
In recent studies, myocardial oxygenation as measured by OS-CMR and MORE parameters correlated with echocardiography-derived LV strain parameters in patients with aortic stenosis. These impairments were shown to be reversible with improved myocardial perfusion, oxygenation, and strain parameters 8 months post aortic valve replacement [33]. In a CAD population, post-stenotic hyperoxia-induced myocardial oxygenation deficits were found to be accompanied by reduced diastolic strain [109]. As OS-CMR is mostly performed using slightly modified regular cine sequences, one set of images yields data on both myocardial oxygenation and myocardial strain. Importantly, this can be done in a dynamic setting. Preliminary evidence utilizing OS-CMR images to derive strain response to stress demonstrated the ability of the technique to assess myocardial strain in young adults born pre-term before and after exercise intervention [110].
Strain CMR imaging studies have highlighted the ability of OS-CMR to obtain dynamic information on myocardial oxygenation and function providing both functional and vascular information in one acquisition. OS-CMR markers in combination with CMR strain parameters to investigate HF on an individual basis may then allow for a more robust, personalized imaging evaluation.
Limitations of OS-CMR
The limitations of both CMR and OS-CMR include a lack of access to scan time, cost, inability to image patients with specific contraindications such as claustrophobia, issues between subspecialties, and a lack of local expertise [111]. OS-CMR with breathing maneuvers may however help alleviate some of these issues, as it does not require contrast agents, specialized equipment, or the presence of a trained physician at the scanner. Local expertise will be necessary only in training patients in deep, paced breathing. However, the need for specific strategies and software algorithms and to analyze the dynamic changes related to tissue oxygenation and strain evaluation remain a significant limitation of OS-CMR. CMR software is costly and can be a barrier to widespread implementation where manual annotation and analysis is time-consuming and can introduce human error.
Conclusion
In patients with heart failure (HF), CMR offers a wide range of quantitative markers that provide important diagnostic and prognostic information. The addition of oxygenation-sensitive CMR (OS-CMR) will further improve clinical decision-making by novel insights into the role of coronary vascular function in this context. This includes the differentiation of ischemic from non-ischemic etiology of HF (by identifying regional abnormalities of coronary vascular function, but also by providing information on the regional integrity and homogeneity of vascular function). Importantly, the use of breathing maneuvers in combination with OS-CMR allows for assessing endothelium-dependent function.
OS-CMR has already been applied in multiple studies of patients with various cardiac diseases associated with HF, such as cardiomyopathies, valvular heart disease, arterial hypertension, and patients with microvascular dysfunction in the absence of coronary artery stenosis.
Comprehensive CMR scans can therefore be used to quantitatively study markers of cardiac morphology, volumes, gross function, strain, myocardial tissue composition, and vascular function, all as part of a safe, needle-free scan. The multiparametric approach that uses oxygenation-sensitive cine imaging for function and vascular function allows for short, cost-efficient scan protocols.
Future OS-CMR studies should focus on validation in larger populations and comparative analyses of its clinical utility in various etiologies. Furthermore, the use of deep learning techniques will allow for identifying novel biomarkers for an improved personalized risk stratification and management strategies in patients with heart failure.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Murphy SP, Ibrahim NE, Januzzi JL Jr. Heart failure with reduced ejection fraction: a review. JAMA. 2020;324(5):488–504.
Ferreira JP, Kraus S, Mitchell S, Perel P, Piñeiro D, Chioncel O, et al. World Heart Federation roadmap for heart failure. Glob Heart. 2019;14(3):197–214.
Braunwald E. Heart failure. JACC Heart Fail. 2013;1(1):1–20.
Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021 1;
Lopatin Y. Heart failure with mid-range ejection fraction and how to treat it. Card Fail Rev. 2018;4(1):9–13.
Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo-Leiro MG, Harjola V-P, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2017;19(12):1574–85.
Rastogi A, Novak E, Platts AE, Mann DL. Epidemiology, pathophysiology and clinical outcomes for heart failure patients with a mid-range ejection fraction. Eur J Heart Fail. 2017;19(12):1597–605.
Cowie MR, Anker SD, Cleland JGF, Felker GM, Filippatos G, Jaarsma T, et al. Improving care for patients with acute heart failure: before, during and after hospitalization. ESC Heart Fail. 2014;1(2):110–45.
Čerlinskaitė K, Javanainen T, Cinotti R, Mebazaa A. Acute heart failure management. Korean Circ J. 2018;48(6):463–80.
Sado DM, Hasleton JM, Herrey AS, Moon JC. CMR in Heart Failure [Internet]. Vol. 2011, Cardiology Research and Practice. Hindawi; 2011 [cited 2021 Feb 8]. p. e739157. Available from: https://www.hindawi.com/journals/crp/2011/739157/
Le Ven F, Bibeau K, De Larochellière É, Tizón-Marcos H, Deneault-Bissonnette S, Pibarot P, et al. Cardiac morphology and function reference values derived from a large subset of healthy young Caucasian adults by magnetic resonance imaging. Eur Heart J Cardiovasc Imaging. 2016;17(9):981–90.
Karamitsos TD. Arvanitaki Alexandra, Karvounis Haralambos, Neubauer Stefan, Ferreira Vanessa M. Myocardial tissue characterization and fibrosis by imaging. JACC Cardiovasc Imaging. 2020;13(5):1221–34.
Barison A, Aimo A, Todiere G, Grigoratos C, Aquaro GD, Emdin M. Cardiovascular magnetic resonance for the diagnosis and management of heart failure with preserved ejection fraction. Heart Fail Rev [Internet]. 2020 22 [cited 2021 Feb 8]; Available from. https://doi.org/10.1007/s10741-020-09998-w.
Mitropoulou P, Georgiopoulos G, Figliozzi S, Klettas D, Nicoli F, Masci PG. Multi-modality imaging in dilated cardiomyopathy: with a focus on the role of cardiac magnetic resonance. Front Cardiovasc Med [Internet]. 2020 [cited 2021 Feb 19];7. Available from. https://doi.org/10.3389/fcvm.2020.00097/full.
Simpson R, Bromage D, Dancy L, McDiarmid A, Monaghan M, McDonagh T, et al. 6 Comparing echocardiography and cardiac magnetic resonance measures of ejection fraction: implications for HFMRF research. Heart. 2018;104(Suppl 5):A3.
Paterson D. Ian, Wells George, Erthal Fernanda, Mielniczuk Lisa, O’Meara Eileen, White James, et al. Outsmart hf Circulation. 2020;141(10):818–27.
Kanagala P, Cheng ASH, Singh A, McAdam J, Marsh A-M, Arnold JR, et al. Diagnostic and prognostic utility of cardiovascular magnetic resonance imaging in heart failure with preserved ejection fraction – implications for clinical trials. J Cardiovasc Magn Reson. 2018;20(1):4.
Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72(21):2625–41.
Katz SD, Katarzyna H, Ingrid H, Kujtim B, Clarito D, Alhakam H, et al. Vascular endothelial dysfunction and mortality risk in patients with chronic heart failure. Circulation. 2005;111(3):310–4.
Giannotti G, Landmesser U. Endothelial dysfunction as an early sign of atherosclerosis. Herz. 2007;32(7):568–72.
Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan R-S, et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J. 2018;39(37):3439–50.
Dryer K, Gajjar M, Narang N, Lee M, Paul J, Shah AP, et al. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am J Physiol-Heart Circ Physiol. 2018;314(5):H1033–42.
Zuchi C, Tritto I, Carluccio E, Mattei C, Cattadori G, Ambrosio G. Role of endothelial dysfunction in heart failure. Heart Fail Rev. 2020;25(1):21–30. This paper reviews the role of endothelial dysfunction, notably alteraed endothelium dependent vasodilatation mechanisms, in the pathophysiology of heart failure and its association with worse prognosis and higher rates of cardiovascular events.
Franssen C, Chen S, Unger A, Korkmaz HI, De Keulenaer GW, Tschöpe C, et al. Myocardial microvascular inflammatory endothelial activation in heart failure with preserved ejection fraction. JACC Heart Fail. 2016;4(4):312–24.
Guensch DP, Fischer K, Flewitt JA, Friedrich MG. Impact of intermittent apnea on myocardial tissue oxygenation--a study using oxygenation-sensitive cardiovascular magnetic resonance. PLoS One. 2013;8(1):e53282.
Fischer K, Guensch DP, Shie N, Lebel J, Friedrich MG. Breathing maneuvers as a vasoactive stimulus for detecting inducible myocardial ischemia - an experimental cardiovascular magnetic resonance study. PLoS One. 2016;11(10):e0164524.
Fischer K, Yamaji K, Luescher S, Ueki Y, Jung B, von Tengg-Kobligk H, et al. Feasibility of cardiovascular magnetic resonance to detect oxygenation deficits in patients with multi-vessel coronary artery disease triggered by breathing maneuvers. J Cardiovasc Magn Reson. 2018;20(1):31. This study demonstrated the feasibility of oxygenation-sensitive CMR with standardized vasoactive breathing maneuvers to identify regional myocardial oxygenation abnormalities in patients with coronary artery disease.
Friedrich MG, Karamitsos TD. Oxygenation-sensitive cardiovascular magnetic resonance. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2013;15:43.
Vöhringer M, Flewitt JA, Green JD, Dharmakumar R, Wang J, Tyberg JV, et al. Oxygenation-sensitive CMR for assessing vasodilator-induced changes of myocardial oxygenation. J Cardiovasc Magn Reson. 2010;12(1):20.
Raman KS, Nucifora G, Selvanayagam JB. Novel cardiovascular magnetic resonance oxygenation approaches in understanding pathophysiology of cardiac diseases. Clin Exp Pharmacol Physiol. 2018;45(5):475–80.
Karamitsos TD, Dass S, Suttie J, Sever E, Birks J, Holloway CJ, et al. Blunted myocardial oxygenation response during vasodilator stress in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2013;61(11):1169–76.
Sairia D, Holloway CJ, Cochlin LE, Rider OJ, Masliza M, Matthew R, et al. No evidence of myocardial oxygen deprivation in nonischemic heart failure. Circ Heart Fail. 2015;8(6):1088–93.
Mahmod M, Francis JM, Pal N, Lewis A, Dass S, De Silva R, et al. Myocardial perfusion and oxygenation are impaired during stress in severe aortic stenosis and correlate with impaired energetics and subclinical left ventricular dysfunction. J Cardiovasc Magn Reson. 2014;16(1):29.
Roubille F, Fischer K, Guensch DP, Tardif J-C, Friedrich MG. Impact of hyperventilation and apnea on myocardial oxygenation in patients with obstructive sleep apnea – an oxygenation-sensitive CMR study. J Cardiol. 2017;69(2):489–94.
Elharram M, Hillier E, Hawkins S, Mikami Y, Heydari B, Merchant N, et al. Regional heterogeneity in the coronary vascular response in women with chest pain and nonobstructive coronary artery disease. Circulation. 2021;143(7):764–6. Novel biomarkers derived from oxygenation-sensitive CMR images with breathing maneuvers as a vasoactive stress identified regional heterogeneity in the mypcardial oxygenation reserve of women with ischemia and no obstructive coronary artery stenosis, which may highlight underlying vascular dysfunction in this poorly understood patient population.
Iannino N, Fischer K, Friedrich M, Hafyane T, Mongeon F-P, White M. Myocardial vascular function assessed by dynamic oxygenation-sensitive cardiac magnetic resonance imaging long-term following cardiac transplantation. Transpl Int. 2021; 16 [cited 2021 Feb 19];Online First. Available from: https://journals.lww.com/transplantjournal/Abstract/9000/Myocardial_Vascular_Function_Assessed_by_Dynamic.95567.aspx.
Ogawa S, Lee TM, Kay AR, Tank DW. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci U S A. 1990;87(24):9868–72.
Ogawa S, Tank DW, Menon R, Ellermann JM, Kim SG, Merkle H, et al. Intrinsic signal changes accompanying sensory stimulation: functional brain mapping with magnetic resonance imaging. Proc Natl Acad Sci U S A. 1992;89(13):5951–5.
Ogawa S, Lee TM, Nayak AS, Glynn P. Oxygenation-sensitive contrast in magnetic resonance image of rodent brain at high magnetic fields. Magn Reson Med. 1990;14(1):68–78.
Rostrup E, Knudsen GM, Law I, Holm S, Larsson HBW, Paulson OB. The relationship between cerebral blood flow and volume in humans. NeuroImage. 2005;24(1):1–11.
Bauer WR, Nadler W, Bock M, Schad LR, Wacker C, Hartlep A, et al. Theory of the BOLD effect in the capillary region: an analytical approach for the determination of T*2 in the capillary network of myocardium. Magn Reson Med. 1999;41(1):51–62.
Wacker CM, Bock M, Hartlep AW, Beck G, van Kaick G, Ertl G, et al. Changes in myocardial oxygenation and perfusion under pharmacological stress with dipyridamole: assessment using T*2 and T1 measurements. Magn Reson Med. 1999;41(4):686–95.
Guensch DP, Fischer K, Flewitt JA, Yu J, Lukic R, Friedrich JA, et al. Breathing manoeuvre-dependent changes in myocardial oxygenation in healthy humans. Eur Heart J Cardiovasc Imaging. 2014;15(4):409–14.
Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev. 2008 Jul;88(3):1009–86.
Fischer K, Guensch DP, Friedrich MG. Response of myocardial oxygenation to breathing manoeuvres and adenosine infusion. Eur Heart J Cardiovasc Imaging. 2015;16(4):395–401.
Moreton FC, Dani KA, Goutcher C, O’Hare K, Muir KW. Respiratory challenge MRI: Practical aspects. NeuroImage Clin. 2016;11:667–77.
Udelson JE. Cardiac magnetic resonance imaging for long-term prognosis in heart failure. Circ Cardiovasc Imaging. 2018;11(9):e008264.
Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Crespo Leiro M, Drozdz J, et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail. 2013;15(7):808–17.
Pilz G, Patel PA, Fell U, Ladapo JA, Rizzo JA, Fang H, et al. Adenosine-stress cardiac magnetic resonance imaging in suspected coronary artery disease: a net cost analysis and reimbursement implications. Int J Card Imaging. 2011;27(1):113–21.
Kwong RY. Ge Yin, Steel Kevin, Bingham Scott, Abdullah Shuaib, Fujikura Kana, et al. Cardiac magnetic resonance stress perfusion imaging for evaluation of patients with chest pain. J Am Coll Cardiol. 2019;74(14):1741–55.
Nagel E, Greenwood JP, McCann GP, Bettencourt N, Shah AM, Hussain ST, et al. Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med. 2019;380(25):2418–28.
Manka R, Paetsch I, Schnackenburg B, Gebker R, Fleck E, Jahnke C. BOLD cardiovascular magnetic resonance at 3.0 tesla in myocardial ischemia. J Cardiovasc Magn Reson. 2010;12(1):54.
Walcher T, Manzke R, Hombach V, Rottbauer W, Wöhrle J, Bernhardt P. Myocardial perfusion reserve assessed by T2-prepared steady-state free precession blood oxygen level-dependent magnetic resonance imaging in comparison to fractional flow reserve. Circ Cardiovasc Imaging. 2012;5(5):580–6.
Karamitsos TD, Leccisotti L, Arnold JR, Recio-Mayoral A, Bhamra-Ariza P, Howells RK, et al. Relationship between regional myocardial oxygenation and perfusion in patients with coronary artery disease: insights from cardiovascular magnetic resonance and positron emission tomography. Circ Cardiovasc Imaging. 2010;3(1):32–40.
Arnold JR, Karamitsos TD, Bhamra-Ariza P, Francis JM, Searle N, Robson MD, et al. Myocardial oxygenation in coronary artery disease: insights from blood oxygen level-dependent magnetic resonance imaging at 3 tesla. J Am Coll Cardiol. 2012;59(22):1954–64.
Luu JM, Friedrich MG, Harker J, Dwyer N, Guensch D, Mikami Y, et al. Relationship of vasodilator-induced changes in myocardial oxygenation with the severity of coronary artery stenosis: a study using oxygenation-sensitive cardiovascular magnetic resonance. Eur Heart J Cardiovasc Imaging. 2014;15(12):1358–67.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395–407.
Bernhardt P, Manzke R, Bornstedt A, Gradinger R, Spiess J, Walcher D, et al. Blood oxygen level-dependent magnetic resonance imaging using T2-prepared steady-state free-precession imaging in comparison to contrast-enhanced myocardial perfusion imaging. Int J Cardiol. 2011;147(3):416–9.
Shantsila E, Wrigley BJ, Blann AD, Gill PS, Lip GYH. A contemporary view on endothelial function in heart failure. Eur J Heart Fail. 2012;14(8):873–81.
Hasdai D, Cannan CR, Mathew V, Holmes DR, Lerman A. Evaluation of patients with minimally obstructive coronary artery disease and angina. Int J Cardiol. 1996;53(3):203–8.
Coronary vasomotion in response to sympathetic stimulation in humans: importance of the functional integrity of the endothelium. J Am Coll Cardiol. 1989 Nov 1;14(5):1181–90.
Kety SS, Schmidt CF. The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Invest. 1948;27(4):484–92.
Coverdale NS, Gati JS, Opalevych O, Perrotta A, Shoemaker JK. Cerebral blood flow velocity underestimates cerebral blood flow during modest hypercapnia and hypocapnia. J Appl Physiol Bethesda Md 1985. 2014;117(10):1090–6.
Tancredi FB, Lajoie I, Hoge RD. A simple breathing circuit allowing precise control of inspiratory gases for experimental respiratory manipulations. BMC Res Notes. 2014;7:235.
Winklhofer S, Pazahr S, Manka R, Alkadhi H, Boss A, Stolzmann P. Quantitative blood oxygenation level-dependent (BOLD) response of the left ventricular myocardium to hyperoxic respiratory challenge at 1.5 and 3.0 T. NMR Biomed. 2014;27(7):795–801.
Yang H-J, Yumul R, Tang R, Cokic I, Klein M, Kali A, et al. Assessment of myocardial reactivity to controlled hypercapnia with free-breathing T2-prepared cardiac blood oxygen level-dependent MR imaging. Radiology. 2014;272(2):397–406.
Stalder AF, Schmidt M, Greiser A, Speier P, Guehring J, Friedrich MG, et al. Robust cardiac BOLD MRI using an fMRI-like approach with repeated stress paradigms. Magn Reson Med. 2015;73(2):577–85.
Yang H-J, Oksuz I, Dey D, Sykes J, Klein M, Butler J, et al. Accurate needle-free assessment of myocardial oxygenation for ischemic heart disease in canines using magnetic resonance imaging. Sci Transl Med [Internet]. 2019; 29 [cited 2021 Jan 31];11(494). Available from: https://stm.sciencemag.org/content/11/494/eaat4407.
Patel S, Miao JH, Yetiskul E, Anokhin A, Majmundar SH. Physiology, carbon dioxide retention. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 [cited 2021 Feb 25]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK482456/
Raichle ME, Plum F. Hyperventilation and cerebral blood flow. Stroke. 1972;3(5):566–75.
Vogt KM, Ibinson JW, Schmalbrock P, Small RH. Comparison between end-tidal CO2 and respiration volume per time for detecting BOLD signal fluctuations during paced hyperventilation. Magn Reson Imaging. 2011;29(9):1186–94.
Wendland MF, Saeed M, Lauerma K, Crespigny AD, Moseley ME, Higgins CB. Endogenous susceptibility contrast in myocardium during apnea measured using gradient recalled echo planar imaging. Magn Reson Med. 1993;29(2):273–6.
Guensch DP, Fischer K, Flewitt JA, Friedrich MG. Myocardial oxygenation is maintained during hypoxia when combined with apnea – a cardiovascular MR study. Physiol Rep [Internet]. 2013;1(5) Oct [cited 2021 Jan 31] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3841034/.
Teixeira T, Nadeshalingam G, Fischer K, Marcotte F, Friedrich MG. Breathing maneuvers as a coronary vasodilator for myocardial perfusion imaging. J Magn Reson Imaging. 2016;44(4):947–55.
Farrehi PM, Bernstein SJ, Rasak M, Dabbous SA, Stomel RJ, Eagle KA, et al. Frequency of negative coronary arteriographic findings in patients with chest pain is related to community practice patterns. Am J Manag Care. 2002;8(7):643–8.
Gulati M, Cooper-DeHoff RM, McClure C, Johnson BD, Shaw LJ, Handberg EM, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease. Arch Intern Med. 2009;169(9):843–50. This paper from the Women’s Ischemia Syndrome Evaluation (WISE) cohort found that women with signs and symptoms that are suggestive of ischemia but with no obstructive coronary artery disease on angiography have a higher risk of cardiovascular events when compared to asymptomatic women.
Kothawade K, Bairey Merz CN. Microvascular coronary dysfunction in women: pathophysiology, diagnosis, and management. Curr Probl Cardiol. 2011;36(8):291–318.
Panting JR, Gatehouse PD, Yang G-Z, Grothues F, Firmin DN, Collins P, et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med. 2002;346(25):1948–53.
Karamitsos TD, Arnold JR, Pegg TJ, Francis JM, Birks J, Jerosch-Herold M, et al. Patients with syndrome X have normal transmural myocardial perfusion and oxygenation: a 3-T cardiovascular magnetic resonance imaging study. Circ Cardiovasc Imaging. 2012;5(2):194–200.
Lanza GA. Cardiac syndrome X: a critical overview and future perspectives. Heart. 2007;93(2):159–66.
Haseeb R, Matthew R, Matthew L, Bhavik M, Hannah MC, Howard E, et al. Coronary microvascular dysfunction is associated with myocardial ischemia and abnormal coronary perfusion during exercise. Circulation. 2019;140(22):1805–16.
Hillier E, Hawkins S, Friedrich M. Healthy aging reduces the myocardial oxygenation reserve as assessed with oxygenation sensitive CMR. Can J Cardiol. 2019;35(10):S81.
Hillier E, Hafyane T, Friedrich MG. 285Myocardial and cerebral oxygenation deficits in heart failure patients - a multi-parametric study. Eur Heart J - Cardiovasc Imaging [Internet]. 2019 Jun 1 [cited 2021 Feb 19];20(jez114.003). Available from. https://doi.org/10.1093/ehjci/jez114.003.
Beache GM, Herzka DA, Boxerman JL, Post WS, Gupta SN, Faranesh AZ, et al. Attenuated myocardial vasodilator response in patients with hypertensive hypertrophy revealed by oxygenation-dependent magnetic resonance imaging. Circulation. 2001;104(11):1214–7.
Betty R, Kenneth C, Rina A, Masliza M, Moritz H, Sanjay S, et al. Abstract 10875: Impaired stress myocardial oxygenation and not perfusion reserve is associated with arrhythmic risk in hypertrophic cardiomyopathy: insights from a novel oxygen sensitive cardiac magnetic resonance approach. Circulation. 2019;140(Suppl_1):A10875.
K SR, R S, M S, A W, Rj W, R A, et al. Left ventricular ischemia in pre-capillary pulmonary hypertension: a cardiovascular magnetic resonance study. Cardiovasc Diagn Ther. 2020;10(5):1280–92.
Smiseth OA, Torp H, Opdahl A, Haugaa KH, Urheim S. Myocardial strain imaging: how useful is it in clinical decision making? Eur Heart J. 2016;37(15):1196–207.
Amzulescu MS, De Craene M, Langet H, Pasquet A, Vancraeynest D, Pouleur AC, et al. Myocardial strain imaging: review of general principles, validation, and sources of discrepancies. Eur Heart J Cardiovasc Imaging. 2019;20(6):605–19.
Gerald B, Hoffman Julien IE, Aman M, Saleh S, Cecil C. Cardiac mechanics revisited. Circulation. 2008;118(24):2571–87.
Joo PJ, Alexandre M, In-Chang H, Jun-Bean P, Jae-Hyeong P, Goo-Yeong C. Phenotyping heart failure according to the longitudinal ejection fraction change: myocardial strain, predictors, and outcomes. J Am Heart Assoc. 2020;9(12):e015009.
Kaufman DP, Kandle PF, Murray I, Dhamoon AS. Physiology, oxyhemoglobin dissociation curve. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2020 Aug 3]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK499818/
Ashish K, Faisaluddin M, Bandyopadhyay D, Hajra A, Herzog E. Prognostic value of global longitudinal strain in heart failure subjects: a recent prototype. Int J Cardiol Heart Vasc. 2018;22:48–9.
Buggey J, Alenezi F, Yoon HJ, Phelan M, DeVore AD, Khouri MG, et al. Left ventricular global longitudinal strain in patients with heart failure with preserved ejection fraction: outcomes following an acute heart failure hospitalization. ESC Heart Fail. 2017;4(4):432–9.
Park JJ, Park J-B, Park J-H, Cho G-Y. Global longitudinal strain to predict mortality in patients with acute heart failure. J Am Coll Cardiol. 2018;71(18):1947–57.
Tony S, Rodel L, Marwick Thomas H. Prediction of all-cause mortality from global longitudinal speckle strain. Circ Cardiovasc Imaging. 2009;2(5):356–64.
Pedrizzetti G, Claus P, Kilner PJ, Nagel E. Principles of cardiovascular magnetic resonance feature tracking and echocardiographic speckle tracking for informed clinical use. J Cardiovasc Magn Reson. 2016;18(1):51.
Mangion K, Burke NMM, McComb C, Carrick D, Woodward R, Berry C. Feature-tracking myocardial strain in healthy adults- a magnetic resonance study at 3.0 tesla. Sci Rep. 2019;9(1):3239.
Pryds K, Larsen AH, Hansen MS, Grøndal AYK, Tougaard RS, Hansson NH, et al. Myocardial strain assessed by feature tracking cardiac magnetic resonance in patients with a variety of cardiovascular diseases – a comparison with echocardiography. Sci Rep. 2019;9(1):11296.
Valente F, Gutierrez L, Rodríguez-Eyras L, Fernandez R, Montano M, Sao-Aviles A, et al. Cardiac magnetic resonance longitudinal strain analysis in acute ST-segment elevation myocardial infarction: a comparison with speckle-tracking echocardiography. IJC Heart Vasc. 2020;29:100560.
Kajzar I, Ochs M, Salatzki J, Ochs A, Riffel J, Osman N, et al. Hyperventilation-breath-hold maneuver to detect ischemia by strain-encoded CMR: a pilot study to evaluate a needle-free stress protocol. Eur Heart J - Cardiovasc Imaging [Internet]. 2021;22:jeaa356.294). Available from. https://doi.org/10.1093/ehjci/jeaa356.294. This study demonstrated that fast strain encoded CMR in conjunction with standardized vasoactive breathing maneuvers is a fast, pharmacologic agent and contrast-free approach with a high diagnostic accuracy for the detection of significant coronary artery stenosis.
Tanacli R, Hashemi D, Lapinskas T, Edelmann F, Gebker R, Pedrizzetti G, et al. Range variability in CMR feature tracking multilayer strain across different stages of heart failure. Sci Rep. 2019;9(1):16478.
Kempny A, Fernández-Jiménez R, Orwat S, Schuler P, Bunck AC, Maintz D, et al. Quantification of biventricular myocardial function using cardiac magnetic resonance feature tracking, endocardial border delineation and echocardiographic speckle tracking in patients with repaired tetralogy of Fallot and healthy controls. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2012;14:32.
Romano S, Romer B, Evans K, Trybula M, Shenoy C, Kwong RY, et al. Prognostic implications of blunted feature-tracking global longitudinal strain during vasodilator cardiovascular magnetic resonance stress imaging. JACC Cardiovasc Imaging. 2020;13(1 Pt 1):58–65.
Kammerlander AA. Feature tracking by cardiovascular magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13(4):948–50.
Ito H, Ishida M, Makino W, Goto Y, Ichikawa Y, Kitagawa K, et al. Cardiovascular magnetic resonance feature tracking for characterization of patients with heart failure with preserved ejection fraction: correlation of global longitudinal strain with invasive diastolic functional indices. J Cardiovasc Magn Reson. 2020;22(1):42. This study demonstrated that CMR feature tracking is a reliable, noninvasive method that can identify impaired global longitudinal strain and diastolic dysfunction in heart failure patients with preserved ejection fraction that can independently predict altered left ventricular relaxation.
Simone R, Judd RM, Kim RJ, Kim HW, Igor K, Heitner JF, et al. Feature-tracking global longitudinal strain predicts death in a multicenter population of patients with ischemic and nonischemic dilated cardiomyopathy incremental to ejection fraction and late gadolinium enhancement. JACC Cardiovasc Imaging. 2018;11(10):1419–29.
DeVore AD, McNulty S, Alenezi F, Ersboll M, Vader JM, Oh JK, et al. Impaired left ventricular global longitudinal strain in patients with heart failure with preserved ejection fraction: insights from the RELAX trial. Eur J Heart Fail. 2017;19(7):893–900.
Masaru O, Reddy Yogesh NV, Borlaug Barry A. Diastolic dysfunction and heart failure with preserved ejection fraction. JACC Cardiovasc Imaging. 2020;13(1_Part_2):245–57.
Guensch DP, Kady F, Kyohei Y, Silvia L, Yasushi U, Bernd J, et al. Effect of hyperoxia on myocardial oxygenation and function in patients with stable multivessel coronary artery disease. J Am Heart Assoc. 2020;9(5):e014739.
Hillier E, Hawkins S, Friedrich MG, Nuyt AM. 334The assessment of functional cardiovascular health after exercise intervention in young adults born preterm. Eur Heart J - Cardiovasc Imaging [Internet]. 2019;20:jez122.003). Available from. https://doi.org/10.1093/ehjci/jez122.003.
ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012 | European Heart Journal | Oxford Academic [Internet]. [cited 2021 Feb 19]. Available from: https://academic.oup.com/eurheartj/article/33/14/1787/526884
Author information
Authors and Affiliations
Contributions
EH and MGF contributed to the idea, design, and editing of the manuscript. EH performed the literature search and drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
MGF is a shareholder and consultant of Circle Cardiovascular Imaging Inc. Dr Friedrich is listed as a holder of United States Patent No. 14/419,877: Inducing and measuring myocardial oxygenation changes as a marker for heart disease; United States Patent No. 15/483,712: Measuring oxygenation changes in tissue as a marker for vascular function; United States Patent No 10,653,394: Measuring oxygenation changes in tissue as a marker for vascular function - continuation; and Canadian Patent CA2020/051776: Method and apparatus for determining biomarkers of vascular function utilizing bold CMR images. EH is listed as a holder of Canadian Patent CA2020/051776: Method and apparatus for determining biomarkers of vascular function utilizing bold CMR images. The other authors report no conflicts.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging in Heart Failure
Supplementary Information
ESM 1
(PDF 153 kb)
Rights and permissions
About this article
Cite this article
Hillier, E., Friedrich, M.G. The Potential of Oxygenation-Sensitive CMR in Heart Failure. Curr Heart Fail Rep 18, 304–314 (2021). https://doi.org/10.1007/s11897-021-00525-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-021-00525-y