Abstract
Purpose of Review
The investigation of total neoadjuvant therapy has increased significantly in recent years, with a number of approaches being utilized in ongoing prospective studies, including (1) induction neoadjuvant chemotherapy (INCT), (2) consolidation neoadjuvant chemotherapy (CNCT), and (3) short-course radiation therapy (SC-RT) for locally advanced rectal cancer (LARC). Significant questions remain regarding the ideal sequence of a total neoadjuvant therapy (TNT) approach.
Recent Findings
Multiple prospective multi-institutional trials have evaluated the addition of multi-agent chemotherapy before or after neoadjuvant rectal cancer chemoradiation. In 2019, a multi-center randomized phase II trial from Germany, CAO/ARO/AIO-12, demonstrated better compliance and lower toxicities with CNCT in comparison to INCT. The OPRA study recently reported in ASCO 2020 improved organ preservation for CNCT, and similar 3-year disease-free survival (DFS) and distant metastasis-free survival (DMFS). RAPIDO reports higher rates of pathologic complete response (pCR) and lower rates of 3-year distant metastases (DM) for TNT compared to traditional treatment sequencing.
Summary
Recent literature on TNT for LARC highlights the potential of this approach to enhance compliance, increase distant control and survival rates, and reduce toxicities. Further research is important to tailor treatment approaches to patients with LARC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rectal cancer is one of the most common cancer diagnoses in the USA with an estimated 43,000 new cases in 2018 [1]. While the overall incidence of colorectal cancer has decreased [2], the incidence has increased in patients less than 50 years old [3], emphasizing the need for effective treatments that minimize long-term morbidity. For the past several decades, standard treatment for most stages II and III locally advanced rectal cancer (LARC) has consisted of a trimodality approach involving radiation, surgery, and chemotherapy. Until recently, the only standard sequence of the trimodality approach was preoperative radiation or chemoradiation followed by surgery, with consideration of adjuvant multi-agent chemotherapy. Recent advances in rectal cancer treatment have centered around optimizing the sequence of these treatments and selecting favorable risk patients for de-escalation via omission of a treatment modality. For patients with a high risk of recurrence, recent efforts have explored a total neoadjuvant therapy (TNT) approach, with delivery of radiation or chemoradiation in sequence with multi-agent chemotherapy in the preoperative setting. In this review, we will outline the rationale for preoperative radiation and chemotherapy, as well as evolving data regarding applications of the TNT approach. We will then turn our attention to the rates of complete clinical complete response (cCR) seen with TNT and how this approach may facilitate the use of non-operative management (NOM). Finally, we will highlight ongoing clinical trials that will further inform the optimal treatment paradigm for LARC.
Rationale for Preoperative Radiation
Preoperative radiation or chemoradiation was established as an important component of rectal cancer therapy after multiple randomized controlled trials demonstrated a significant reduction in the rate of local recurrence (LR) compared to surgery alone, even despite improvements in surgical technique to include total mesorectal excision (TME) [4,5,6,7,8]. When comparing preoperative to postoperative radiation, delivery of radiation upfront showed lower rates of LR with more favorable toxicity profiles [9,10,11,12]. Two predominant approaches to radiation were used in these trials: long-course chemoradiation (LC-CRT) consisting of 45–55.8 Gy in 25–31 fractions with concurrent 5-fluorouracil (5-FU) or capecitabine, or short-course radiation (SC-RT) consisting of 25 Gy in 5 fractions without concurrent chemotherapy. A number of randomized trials have compared LC-CRT and SC-RT, most notably TROG 01.04, which demonstrated no significant differences in disease control, survival, late toxicity, or quality of life (QoL) [13, 14], though the use of SC-RT has been less common in the USA [15].
Initial Exploration of Multi-Agent Chemotherapy Concurrent with Radiation
Approximately 25–30% of stages II–III rectal cancer patients develop distant metastases (DM) by 10 years, regardless of the receipt of preoperative radiation [4,5,6, 9, 12]. Such data has provided justification for exploration of multi-agent systemic therapy given in the preoperative setting. Earlier delivery of multi-agent chemotherapy may allow for more prompt treatment of occult metastatic disease and facilitate greater tumor downstaging prior to surgery. After the MOSAIC study demonstrated improved survival with the addition of oxaliplatin to adjuvant 5-FU (FOLFOX) for stage III colorectal cancer ( [16]), investigators questioned whether radiation with concurrent multi-agent chemotherapy would provide additional disease control due to earlier delivery of multi-agent chemotherapy and potential radiosensitization effects. Four of 5 randomized trials demonstrated no disease control or survival benefit, two of which found worse acute toxicity, with the use of multi-agent chemotherapy in combination with preoperative radiation [17,18,19,20,21,22]). Though these studies were negative, they led investigators to explore the efficacy of sequential radiation and multi-agent chemotherapy prior to surgery, an approach now known as TNT.
Shift Towards Sequential Neoadjuvant Chemotherapy and Radiation
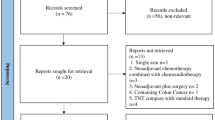
The investigation of TNT has increased significantly in recent years, with a number of approaches being utilized in ongoing prospective studies (Fig. 1). With the use of LC-CRT, multi-agent chemotherapy may be given upfront, i.e., induction neoadjuvant chemotherapy (INCT), or after chemoradiation, i.e., consolidation neoadjuvant chemotherapy (CNCT). With the use of SC-RT, surgery is preferred either in the days immediately after completion of radiation, or in a delayed fashion 4–8 weeks later to allow for tumor response [23, 24]. To date, in studies utilizing SC-RT as part of a TNT approach, multi-agent chemotherapy has been given after radiation. In terms of the multi-agent chemotherapy regimen, either FOLFOX or capecitabine with oxaliplatin (CAPOX) is appropriate, given that CAPOX has also been shown to be superior to 5-FU alone in patients with colon cancer [25]. Existing retrospective and prospective studies of TNT have used both chemotherapy regimens, and in the absence of comparative data in this setting, both are acceptable. Significant questions remain regarding the ideal sequence of a TNT approach, with general paradigms shown in Fig. 1.
Long-Course Chemoradiation Followed by Chemotherapy
Given that the adherence of administering adjuvant chemotherapy for patients with locally advanced rectal cancer is low (42.9% for postoperative chemotherapy vs. 82% for preoperative chemotherapy) [26], there have been attempts to deliver multi-agent chemotherapy following chemoradiation in the neoadjuvant setting. Several studies have evaluated a TNT strategy administrating multi-agent chemotherapy between chemoradiation and definitive surgery.
A recent prospective multi-institutional phase 2 trial, Timing of Rectal Cancer Response to Chemoradiation Consortium, by Garcia-Aguilar et al. assigned patients to receive chemoradiation (with concurrent 5-FU) followed by chemotherapy then surgery. Four treatment arms were included, with patients assigned to 0, 2, 4, or 6 cycles of modified FOLFOX6 chemotherapy between chemoradiation and surgery. In contrast to adjuvant chemotherapy trials, treatment compliance with neoadjuvant chemotherapy was good, approximately 77 to 82% [27, 28]. In 259 analyzable patient charts, the pathologic complete response (pCR) rate was higher in patients who received additional chemotherapy and longer intervals until surgery (18%, 25%, 30%, and 38% in groups one to four, respectively) [28]. No patients experienced disease progression during neoadjuvant chemotherapy. On a long-term follow-up paper, adding neoadjuvant mFOLFOX6 not only improved pCR but also improved disease-free survival (DFS) [29]. DFS was higher in patients who received additional chemotherapy (50%, 81%, 86%, 76% in groups one to four, respectively, p = 0.004). Overall survival was not significantly different.
A multi-center randomized phase II trial from Germany, CAO/ARO/AIO-12, looked to determine the optimal scheduling of preoperative chemoradiation and chemotherapy. Patients with stage II or III rectal cancer were assigned to group A (induction chemotherapy with 3 cycles of fluorouracil, leucovorin, and oxaliplatin followed by CRT) or to group B (CRT followed by consolidation chemotherapy). Of the 306 patients evaluated, group B had lower grade 3 or 4 toxicities (27% vs. 37%) and higher compliance (92% vs. 85%) [30]. pCR was achieved in 17% vs. 25% in group A vs. group B respectively, and thus, only group B fulfilled the predefined statistical hypothesis [30]. Results from this study demonstrate that CRT followed by consolidative chemotherapy had improved pCR, lower toxicities, and higher compliance. Long-term follow-up is required to determine whether pCR translates to better outcomes.
Induction Neoadjuvant Chemotherapy Followed by Chemoradiation
The potential advantages of upfront chemotherapy followed by chemoradiation for locally advanced cancer include earlier delivery of multi-agent chemotherapy, improved tolerance and delivery of induction compared with consolidation multi-agent chemotherapy, earlier delivery of chemotherapy, and increased facilitation of NOM. Several prospective studies have evaluated the use of induction chemotherapy followed by chemoradiation in patients with high-risk disease. A comprehensive list of relevant studies is provided in Table 1.
Fernandez-Martos et al. reported in a phase II randomized trial of 108 patients from Spain with poor-risk rectal cancer based on MRI received either 4 cycles of induction capecitabine and oxaliplatin (CAPOX), chemoradiation and then surgery or concurrent chemoradiation followed by surgery and adjuvant CAPOX. Compliance with completing chemotherapy was higher in the induction arm in comparison to the adjuvant chemotherapy arm (94% vs. 57%) [31]. Additionally, grade 3 or above toxicity was significantly lower for the induction arm (19% vs. 54%) [31]. In terms of outcomes, there was similar overall 5-year overall survival for the induction vs. adjuvant chemotherapy arm (75% vs. 78%), 5-year cumulative incidence of LR (2% vs. 5%; p = 0.61), and 5-year DM (21% vs. 23%; p = 0.79) [31, 32]. The conclusion was that given better treatment tolerance, upfront systemic therapy is a promising option without compromising outcomes. However, the study may have been underpowered to detect a difference in outcomes.
A UK group running the EXPERT trial also evaluated the role of induction chemotherapy [33, 34]. EXPERT enrolled 105 patients treated with 4 cycles of CAPOX followed by chemoradiation (54 Gy with capecitabine) then surgery followed by four additional cycles of CAPOX. The 3-year progression-free survival and overall survival rates were 68% and 83% respectively [33].
The largest series reported of the TNT approach was a single-institution, retrospective, cohort study including patients with locally advanced rectal cancer treated with chemoradiation (CRT), 5-FU and oxaliplatin–based chemotherapy, and surgery at Memorial Sloan Kettering Cancer Center (MSKCC) between 2009 and 2015 [35•]. The two following cohorts were compared: [1] patients who were treated with neoadjuvant CRT, surgery, and planned adjuvant chemotherapy (n = 320), and [2] patients who were treated with TNT consisting of induction chemotherapy followed by CRT or CRT followed by consolidation chemotherapy and subsequently surgery (n = 308). The complete response rate, including both pCR and cCR at 12 months post-treatment, was better in the TNT cohort compared to the group with planned adjuvant chemotherapy (37% vs. 22%) [35•]. Additionally, patients in the TNT group received a greater percentage of planned 5-FU and oxaliplatin. There was no difference in distant metastatic-free survival (DMFS) despite a higher number of cT4 and cN+ tumors in the TNT group. The authors concluded that TNT is a viable treatment strategy for rectal cancer and is associated with higher rates of pCR and cCR as well as nodal downstaging.
Additionally, there is interest at testing new therapies using pCR as a marker. NRG Oncology GI002 is currently ongoing and is entitled “A phase II clinical trial platform of sensitization utilizing total neoadjuvant therapy in rectal cancer.” This trial is examining the outcomes of induction FOLFOX for 4 cycles followed by chemoradiation with the addition of novel radiosensitizers to the neoadjuvant therapy. Histologic response will be measured by neoadjuvant rectal cancer (NAR) score, which is based on tumor downstaging and pathologic nodal stage validated in NASBP R-04 [28].
Short-Course Radiation Followed by Chemotherapy
SC-RT as a component of TNT is an attractive approach for several reasons. As mentioned above, a period of delay between completion of SC-RT and surgery may allow for tumor downstaging [23]. Perhaps this “downtime” could instead be used to provide multi-agent chemotherapy and enhance disease control, assuming there is an adequate time between therapies to prevent overlap of toxicities. Furthermore, compared to TNT with LC-CRT, the use of SC-RT could reduce the time between the start of preoperative treatment and radical surgery. Compared to INCT regimens, TNT with SC-RT minimizes the time to starting multi-agent chemotherapy while also providing early local therapy and is more convenient for patients given the shorter duration of daily radiotherapy. Relevant studies are listed in Table 1.
In a single-arm phase II trial at Washington University, 69 patients with cT3-4 cN0-2 rectal cancer received a near TNT (nTNT) regimen consisting of SC-RT followed by 4 cycles of FOLFOX and a subsequent 4–9-week delay prior to TME, with or without up to 8 cycles of adjuvant FOLFOX [36, 37]. Compared to a stage-matched cohort of patients who underwent preoperative LC-CRT and adjuvant FOLFOX, patients receiving the nTNT regimen demonstrated improvements in pathologic downstaging of the primary tumor (75% vs. 41%, p < 0.001), 3-year DFS (85% vs. 68%, p = 0.032), and 3-year DMFS (88% vs. 70%, p = 0.028), with no significant difference in 3-year actuarial local control (92% vs. 96%, p = 0.36). Additional patients from a Stanford University cohort were added to the comparison group to minimize bias, and TNT remained associated with a lower risk of recurrence. Similar local control between groups may suggest that the improvement in DMFS and DFS is due to an earlier delivery of multi-agent chemotherapy. There were expectedly more preoperative grades 3–4 acute hematologic toxicities in the nTNT cohort (22% vs. 0%), but these findings are comparable to toxicity profiles during adjuvant chemotherapy, and patient-reported QoL was stable from pre-treatment to 1 year after surgery [38]. Furthermore, 28% of patients in the nTNT cohort had a pCR compared to 16% in the matched cohort (p = 0.21). While not significantly different, the rate of pCR in the nTNT group was high relative to historical controls, especially considering the high-risk disease characteristics prevalent in this cohort (75% cN1-2, 76% with one or more adverse features including tumor < 5 cm from the anal verge, fixed, circumferential, or near-obstructing). A subset analysis showed that patients with low-risk disease characteristics as defined by the ongoing PROSPECT trial (≥ 5 cm from the anal verge, circumferential margin clear by ≥ 3 mm, and cT ≤ cT3), had an impressive pCR rate of 39% (15 of 38 patients).
In the first phase III trial investigating TNT with SC-RT, the Polish II trial randomized 541 patients to SC-RT followed by 3 cycles of FOLFOX or 5-FU alone (TNT arm) versus LC-CRT with concurrent FOLFOX (rather than standard continuous infusion 5-FU or capecitabine) or bolus 5-FU alone (control arm) [39]. The study did not meet its primary endpoint of R0 resections, and there was no difference in pCR, LR, DM, or 3-year DFS, but there was a significant improvement in 3-year overall survival (OS, 73% vs. 65%, p = 0.046). The reason for these findings is unclear. The lack of improvement in DM and DFS rates may be due to the regimen of multi-agent chemotherapy (FOLFOX4 rather than the standard mFOLFOX6), the use of single-agent chemotherapy in about one-third of patients, or the number of cycles (3 compared to 4–6 in other studies). Besides the use of single-agent chemotherapy in about one-third of patients, the low pCR rates (16% vs. 12%, p = 0.17) may have also been impacted by the shorter interval between completion of radiation and surgery (11 weeks compared to 17 weeks in the Washington University study and 25 weeks in the Dutch M1 trial).
Though the results of the Polish II trial are difficult to interpret, there are two ongoing multi-institutional phase III randomized controlled trials investigating the use of TNT with SC-RT. In the Chinese STELLAR trial, an expected 552 patients will be randomized to TNT with SC-RT followed by CAPOX or LC-CRT with adjuvant CAPOX (Jin Ann Oncol 2018). In a planned interim analysis of the first 100 patients, the pCR rate was substantially higher in the TNT arm (26% vs. 5%, p = 0.011), despite evenly balanced high-risk disease characteristics.
Early results of the anticipated RAPIDO trial were recently reported with encouraging findings. In this study, carried out in the USA and Europe, 920 patients were randomized to receive TNT with SC-RT followed by 6 cycles of CAPOX or standard LC-CRT with an optional 8 cycles of adjuvant CAPOX [40•]. This study strictly included high-risk disease characterized by at least one of cT4 (30–32%), cN2 (65–66%), enlarged lateral lymph nodes (14–15%), positive MRF (60–62%), or positive EMVI (28–32%). Patients who received TNT had a higher rate of pCR (28% vs. 14%, OR 2.40, p < 0.001) and lower rates of 3-year disease-related treatment failure (DrTF, 24% vs. 30%, HR 0.76, p = 0.02) and DM (20% vs. 27%, HR 0.69, p = 0.004) with similar locoregional recurrence (LRR, 9% vs. 6%, HR 1.45, p = 0.10). There was no difference in outcomes when controlling for receipt of adjuvant chemotherapy in the control arm, and there were no differences in patient-reported health or quality outcomes. This study thus provided randomized prospective data to show improved disease control with TNT. The 3-year DFS of 76% in the TNT arm is similar to historical data that would suggest an average 3-year DFS of about 75% in a heterogeneous population receiving trimodality therapy. However, bearing in mind the high-risk features of the present cohort, these results are more impressive still.
Non-operative Management
As discussed above, a subset of patients receiving neoadjuvant therapy are found to have a pCR, typically 10–20% after preoperative radiation alone [9, 10, 18, 41] and up to 25% after neoadjuvant multi-agent chemotherapy alone [42, 43], with associated improvements in long-term outcomes [44]. By delivering both treatments prior to surgery in a TNT approach, the rate of complete responses would be expected to increase, as demonstrated in several randomized trials [45]; Jin Ann Oncol 2018; [40•], with pCR rates up to about 40% [45]. Perhaps some of these patients, if found to have a cCR to preoperative therapy, could be managed without surgery, an approach referred to as NOM or watch-and-wait (WW).
Outcomes of this approach were first reported by Habr-Gama et al. [46]. In this retrospective cohort study, 71 patients achieved a cCR after chemoradiation alone and underwent NOM with a 5-year OS and DFS of 100% and 92%, respectively, with 2 patients (2.8%) developing local regrowth and 3 patients (4.2%) with DM at a mean follow-up of 57 months. More recently, a meta-analysis of 23 studies including 867 patients who underwent NOM after a cCR found a pooled 2-year local regrowth rate of 15.7% (95% CI, 11.8–20.1%), with 95.4% of patients undergoing salvage therapy [47]. In 5 studies that compared 128 NOM patients to 189 patients with a pCR, there were no differences in non-regrowth recurrence (i.e., intrapelvic nodal recurrence or distant recurrence), cancer-specific mortality, or OS. DFS was improved in the pCR group (HR 0.47, 95% CI 0.28–0.78), but by definition, this measurement included patients in the NOM group who experienced local regrowth but underwent successful salvage surgery. Thus, a large portion of patients (~ 84% in this analysis) avoided surgery altogether with no detriment to extra-luminal disease control or survival. A more recent multi-center registry study of 880 patients undergoing NOM after cCR (50% previously unpublished data) found a 2-year cumulative incidence of local regrowth of 25.2% (95% CI, 22.2–28.5%) and incidence of DM of 8% at a median follow-up of 3.3 years [48].
Most comparative studies to date have analyzed outcomes of patients with a cCR who undergo NOM versus patients with a pCR identified after resection. However, a tumor with a pCR may be biologically different from one with a cCR, and these differences may impact disease control outcomes. A more ideal comparison would be patients with a cCR who undergo NOM versus surgery. In fact, this meta-analysis included 3 studies that compared patients who underwent NOM after a cCR (n = 71) to patients who underwent surgery after a cCR (n = 128), and found no differences in non-regrowth recurrence, cancer-specific mortality, DFS, or OS. Of note, these data from these 3 studies, and the majority of the existing NOM literature in general, come from retrospective cohort studies.
The Organ Preservation in Rectal Adenocarcinoma (OPRA) study is an ongoing phase II trial that randomizes patients to TNT with CNCT versus INCT followed by NOM if a cCR or near-cCR is achieved, thereby addressing two areas of inquiry: comparison of TNT regimens and obtaining prospective NOM outcomes [49]. Interim results were recently reported on the first 307 patients enrolled with the same 3-year DFS (77% vs. 78%) and DMFS (83% vs. 81%), but there was an improved organ preservation in the CNCT group (58% vs. 43%, p = .01) [50•]. While this study will provide useful information on optimizing the likelihood of achieving a cCR and outcomes with NOM, further investigation is needed to determine the optimal timing and criteria of response assessment, as well as surveillance protocols and QoL.
Limitations and Future Directions
One of the main reasons for the introduction of TNT is the goal to maintain optimal outcomes for patients while minimizing the long-term effects of treatment on the morbidity of treatment on patients with rectal cancer. Although trimodality therapy improves outcomes, there is a significant long-term toxicity. There are decrements in sexual and bowel function, primarily from surgery and radiation [51]. Long-term neurotoxicity is associated with oxaliplatin-based chemotherapy [52]. Further studies are needed to continue to investigate omitting portions of standard therapy in select individuals to prevent overtreatment and associated toxicities, and focus on long-term disease-related outcomes to validate the use of neoadjuvant strategies as evidence-based alternatives to the current standard of care.
As mentioned in the previous sections, ASCO 2020 provided exciting early results with (1) RAPIDO reporting high compliance of systemic therapy and better disease-related treatment outcomes with the experimental arm of SC-RT followed by 6 cycles of CAPOX [40•], (2) OPRA demonstrating improved organ preservation in the CRCT arm. Additionally, briefly discussed prior, future studies, including GI002, will be looking at determining biomarkers for optimal selection for treatment intensification and de-intensification for patients with locally advanced rectal cancer.
In the vein of de-escalating therapy, it will be interesting to see the results of the PROSPECT trial (NCT01515787), a multi-center phase II/III study comparing chemotherapy alone or chemoradiation in treatment patients with locally advanced rectal cancer undergoing surgery. The PROSPECT trial may discuss the role of de-escalating radiation treatment for select patients.
On the horizons is the TRIGGER trial (NCT02704520) which aims to determine whether patients can be offered MRI-directed patient management according to radiological response to CRT (mrTRG). Patients who have a good response according to MRI to treatment with CRT will defer surgery until the cancer stops reducing in size or avoid surgery altogether if the cancer cannot be detected on assessments by repeat scans.
Conclusion
There continues to be an increased interest in pursuing more tailored approaches to patients with LARC. The recent increase of literature on TNT for LARC highlights the potential of this approach to reduce toxicities, enhance compliance, increase distant control, and improve survival rates. Ongoing phase 2 and phase 3 trials should provide long-term, disease-related outcomes compared with the current standard treatment approaches using adjuvant systemic therapy. Additional trials are looking at the potential of augmentation of therapy with concurrent radiosensitizers, and there is potential for optimization of TNT with eligibility for organ preservation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Siegel RL, Jakubowski CD, Fedewa SA, Davis A, Azad NS. Colorectal cancer in the young: epidemiology, prevention, management. Am Soc Clin Oncol Educ Book. 2020;40:1–14.
Cheng L, Eng C, Nieman LZ, Kapadia AS, Du XL. Trends in colorectal cancer incidence by anatomic site and disease stage in the United States from 1976 to 2005. Am J Clin Oncol. 2011;34(6):573–80.
Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015;150(1):17–22.
Folkesson J, Birgisson H, Pahlman L, Cedermark B, Glimelius B, Gunnarsson U. Swedish Rectal Cancer Trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol. 2005;23(24):5644–50.
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011;12(6):575–82.
Abraha I, Aristei C, Palumbo I, Lupattelli M, Trastulli S, Cirocchi R, et al. Preoperative radiotherapy and curative surgery for the management of localised rectal carcinoma. Cochrane Database Syst Rev. 2018;10:CD002102.
Camma C, Giunta M, Fiorica F, Pagliaro L, Craxi A, Cottone M. Preoperative radiotherapy for resectable rectal cancer: a meta-analysis. JAMA. 2000;284(8):1008–15.
Rahbari NN, Elbers H, Askoxylakis V, Motschall E, Bork U, Buchler MW, et al. Neoadjuvant radiotherapy for rectal cancer: meta-analysis of randomized controlled trials. Ann Surg Oncol. 2013;20(13):4169–82.
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012;30(16):1926–33.
Roh MS, Colangelo LH, O’Connell MJ, Yothers G, Deutsch M, Allegra CJ, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol. 2009;27(31):5124–30.
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009;373(9666):811–20.
Song JH, Jeong JU, Lee JH, Kim SH, Cho HM, Um JW, et al. Preoperative chemoradiotherapy versus postoperative chemoradiotherapy for stage II-III resectable rectal cancer: a meta-analysis of randomized controlled trials. Radiat Oncol J. 2017;35(3):198–207.
Ngan SY, Burmeister B, Fisher RJ, Solomon M, Goldstein D, Joseph D, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol. 2012;30(31):3827–33.
McLachlan SA, Fisher RJ, Zalcberg J, Solomon M, Burmeister B, Goldstein D, et al. The impact on health-related quality of life in the first 12 months: a randomised comparison of preoperative short-course radiation versus long-course chemoradiation for T3 rectal cancer (Trans-Tasman Radiation Oncology Group Trial 01.04). Eur J Cancer. 2016;55:15–26.
Sineshaw HM, Jemal A, Thomas CR Jr, Mitin T. Changes in treatment patterns for patients with locally advanced rectal cancer in the United States over the past decade: an analysis from the National Cancer Data Base. Cancer. 2016;122(13):1996–2003.
Andre T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009;27(19):3109–16.
Aschele C, Cionini L, Lonardi S, Pinto C, Cordio S, Rosati G, et al. Primary tumor response to preoperative chemoradiation with or without oxaliplatin in locally advanced rectal cancer: pathologic results of the STAR-01 randomized phase III trial. J Clin Oncol. 2011;29(20):2773–80.
Gerard JP, Azria D, Gourgou-Bourgade S, Martel-Lafay I, Hennequin C, Etienne PL, et al. Clinical outcome of the ACCORD 12/0405 PRODIGE 2 randomized trial in rectal cancer. J Clin Oncol. 2012;30(36):4558–65.
Aschele C, Lonardi S, Cionini L, Pinto C, Cordio SS, Rosati G, et al. Final results of STAR-01: a randomized phase III trial comparing preoperative chemoradiation with or without oxaliplatin in locally advanced rectal cancer. J Clin Oncol. 2016;34(15_suppl):3521.
Azria D, Doyen J, Jarlier M, Martel-Lafay I, Hennequin C, Etienne P, et al. Late toxicities and clinical outcome at 5 years of the ACCORD 12/0405-PRODIGE 02 trial comparing two neoadjuvant chemoradiotherapy regimens for intermediate-risk rectal cancer. Ann Oncol. 2017;28(10):2436–42.
Schmoll H-J, Haustermans K, Price TJ, Nordlinger B, Hofheinz R, Daisne J-F, et al. Preoperative chemoradiotherapy and postoperative chemotherapy with capecitabine +/- oxaliplatin in locally advanced rectal cancer: final results of PETACC-6. J Clin Oncol. 2018;36(15_suppl):3500.
Rodel C, Graeven U, Fietkau R, Hohenberger W, Hothorn T, Arnold D, et al. Oxaliplatin added to fluorouracil-based preoperative chemoradiotherapy and postoperative chemotherapy of locally advanced rectal cancer (the German CAO/ARO/AIO-04 study): final results of the multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2015;16(8):979–89.
Pettersson D, Lorinc E, Holm T, Iversen H, Cedermark B, Glimelius B, et al. Tumour regression in the randomized Stockholm III Trial of radiotherapy regimens for rectal cancer. Br J Surg. 2015;102(8):972–8 discussion 8.
Erlandsson J, Holm T, Pettersson D, Berglund A, Cedermark B, Radu C, et al. Optimal fractionation of preoperative radiotherapy and timing to surgery for rectal cancer (Stockholm III): a multicentre, randomised, non-blinded, phase 3, non-inferiority trial. Lancet Oncol. 2017;18(3):336–46.
Haller DG, Tabernero J, Maroun J, de Braud F, Price T, Van Cutsem E, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol. 2011;29(11):1465–71.
Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355(11):1114–23.
Garcia-Aguilar J, Smith DD, Avila K, Bergsland EK, Chu P, Krieg RM, et al. Optimal timing of surgery after chemoradiation for advanced rectal cancer: preliminary results of a multicenter, nonrandomized phase II prospective trial. Ann Surg. 2011;254(1):97–102.
George TJ Jr, Allegra CJ, Yothers G. Neoadjuvant rectal (NAR) score: a new surrogate endpoint in rectal cancer clinical trials. Curr Colorectal Cancer Rep. 2015;11(5):275–80.
Marco MR, Zhou L, Patil S, Marcet JE, Varma MG, Oommen S, et al. Consolidation mFOLFOX6 chemotherapy after chemoradiotherapy improves survival in patients with locally advanced rectal cancer: final results of a multicenter phase II trial. Dis Colon Rectum. 2018;61(10):1146–55.
Fokas E, Allgauer M, Polat B, Klautke G, Grabenbauer GG, Fietkau R, et al. Randomized phase II trial of chemoradiotherapy plus induction or consolidation chemotherapy as total neoadjuvant therapy for locally advanced rectal cancer: CAO/ARO/AIO-12. J Clin Oncol. 2019;37(34):3212–22.
Fernandez-Martos C, Pericay C, Aparicio J, Salud A, Safont M, Massuti B, et al. Phase II, randomized study of concomitant chemoradiotherapy followed by surgery and adjuvant capecitabine plus oxaliplatin (CAPOX) compared with induction CAPOX followed by concomitant chemoradiotherapy and surgery in magnetic resonance imaging-defined, locally advanced rectal cancer: Grupo Cancer de Recto 3 Study. J Clin Oncol. 2010;28(5):859–65.
Fernandez-Martos C, Garcia-Albeniz X, Pericay C, Maurel J, Aparicio J, Montagut C, et al. Chemoradiation, surgery and adjuvant chemotherapy versus induction chemotherapy followed by chemoradiation and surgery: long-term results of the Spanish GCR-3 phase II randomized trial†. Ann Oncol. 2015;26(8):1722–8.
Chua YJ, Barbachano Y, Cunningham D, Oates JR, Brown G, Wotherspoon A, et al. Neoadjuvant capecitabine and oxaliplatin before chemoradiotherapy and total mesorectal excision in MRI-defined poor-risk rectal cancer: a phase 2 trial. Lancet Oncol. 2010;11(3):241–8.
Dewdney A, Cunningham D, Tabernero J, Capdevila J, Glimelius B, Cervantes A, et al. Multicenter randomized phase II clinical trial comparing neoadjuvant oxaliplatin, capecitabine, and preoperative radiotherapy with or without cetuximab followed by total mesorectal excision in patients with high-risk rectal cancer (EXPERT-C). J Clin Oncol. 2012;30(14):1620–7.
• Cercek A, Roxburgh CSD, Strombom P, Smith JJ, Temple LKF, Nash GM, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. The largest retrospective review demonstrating improved tolerability and response rates for TNT compared to traditional treatment sequencing.
Myerson RJ, Tan B, Hunt S, Olsen J, Birnbaum E, Fleshman J, et al. Five fractions of radiation therapy followed by 4 cycles of FOLFOX chemotherapy as preoperative treatment for rectal cancer. Int J Radiat Oncol Biol Phys. 2014;88(4):829–36.
Markovina S, Youssef F, Roy A, Aggarwal S, Khwaja S, DeWees T, et al. Improved metastasis- and disease-free survival with preoperative sequential short-course radiation therapy and FOLFOX chemotherapy for rectal cancer compared with neoadjuvant long-course chemoradiotherapy: results of a matched pair analysis. Int J Radiat Oncol Biol Phys. 2017;99(2):417–26.
Khwaja SS, Roy A, Markovina S, Dewees TA, Hunt S, Tan B, et al. Quality of life outcomes from a phase 2 trial of short-course radiation therapy followed by FOLFOX chemotherapy as preoperative treatment for rectal cancer. Int J Radiat Oncol Biol Phys. 2016;95(5):1429–38.
Bujko K, Wyrwicz L, Rutkowski A, Malinowska M, Pietrzak L, Krynski J, et al. Long-course oxaliplatin-based preoperative chemoradiation versus 5 x 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: results of a randomized phase III study. Ann Oncol. 2016;27(5):834–42.
• Hospers G, Bahadoer RR, Dijkstra EA, Etten BV, Marijnen C, Putter H, et al. Short-course radiotherapy followed by chemotherapy before TME in locally advanced rectal cancer: the randomized RAPIDO trial. J Clin Oncol. 2020;38(15_suppl):4006. An important randomized trial demonstrating improved disease-related treatment failure for TNT using a short-course approach compared to traditional long-course chemoradiation with adjuvant chemotherapy.
O’Connell MJ, Colangelo LH, Beart RW, Petrelli NJ, Allegra CJ, Sharif S, et al. Capecitabine and oxaliplatin in the preoperative multimodality treatment of rectal cancer: surgical end points from National Surgical Adjuvant Breast and Bowel Project trial R-04. J Clin Oncol. 2014;32(18):1927–34.
Schrag D, Weiser MR, Goodman KA, Gonen M, Hollywood E, Cercek A, et al. Neoadjuvant chemotherapy without routine use of radiation therapy for patients with locally advanced rectal cancer: a pilot trial. J Clin Oncol. 2014;32(6):513–8.
Jalil O, Claydon L, Arulampalam T. Review of neoadjuvant chemotherapy alone in locally advanced rectal cancer. J Gastrointest Cancer. 2015;46(3):219–36.
Maas M, Nelemans PJ, Valentini V, Das P, Rodel C, Kuo LJ, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010;11(9):835–44.
Garcia-Aguilar J, Chow OS, Smith DD, Marcet JE, Cataldo PA, Varma MG, et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol. 2015;16(8):957–66.
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U Jr, Silva e Sousa AH Jr, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg. 2004;240(4):711–7 discussion 7-8.
Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2(7):501–13.
van der Valk MJM, Hilling DE, Bastiaannet E, Meershoek-Klein Kranenbarg E, Beets GL, Figueiredo NL, et al. Long-term outcomes of clinical complete responders after neoadjuvant treatment for rectal cancer in the International Watch & Wait Database (IWWD): an international multicentre registry study. Lancet. 2018;391(10139):2537–45.
Smith JJ, Chow OS, Gollub MJ, Nash GM, Temple LK, Weiser MR, et al. Organ Preservation in Rectal Adenocarcinoma: a phase II randomized controlled trial evaluating 3-year disease-free survival in patients with locally advanced rectal cancer treated with chemoradiation plus induction or consolidation chemotherapy, and total mesorectal excision or nonoperative management. BMC Cancer. 2015;15:767.
• Garcia-Aguilar J, Patil S, Kim JK, Yuval JB, Thompson H, Verheij F, et al. Preliminary results of the organ preservation of rectal adenocarcinoma (OPRA) trial. J Clin Oncol. 2020;38(15_suppl):4008. Initial report of the OPRA trial which evaluated INCT and CNCT approaches for NOM, with improved cCR for CNCT.
Hendren SK, O’Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, et al. Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg. 2005;242(2):212–23.
Park SB, Lin CS, Krishnan AV, Goldstein D, Friedlander ML, Kiernan MC. Long-term neuropathy after oxaliplatin treatment: challenging the dictum of reversibility. Oncologist. 2011;16(5):708–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Radiation Therapy and Radiation Therapy Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
Shiao, J.C., Fakhoury, K.R. & Olsen, J. Total Neoadjuvant Therapy for Rectal Cancer: Current Status and Future Directions. Curr Colorectal Cancer Rep 16, 125–134 (2020). https://doi.org/10.1007/s11888-020-00461-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-020-00461-4