Abstract
Early rectal cancer (cT1 and cT2) has been increasingly detected due to the wide application of colorectal cancer screening program. Total mesorectal excision (TME) is a gold standard for the treatment of this early stage disease. However, postoperative complications, unfavorable functional outcomes, and risk of permanent stoma following TME are not uncommon. In contrast, local excision (LE) is less invasive and more tolerable to frail patients and those with severe co-morbidities. Simultaneously, both functional and sexual outcomes following LE were not disturbed and the patient could avoid abdominoperineal resection. The drawback of LE is leaving perirectal lymph node yielding unknown actual pathological nodal staging—which partly leads to more recurrence comparing to TME. This article aimed to review the current evidence of TME and LE in early rectal cancer, to critically review the role and consequence of chemoradiation in LE, and to update ongoing trials on this subject.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly half of 100,000 rectal cancer cases were newly diagnosed each year partly due to the widespread introduction of population-based screening programs [1]. Management of rectal cancer patients is one of the most challenging problems in surgical practice. The principles of rectal cancer surgery include removal of tumor and node-baring area aiming to achieve long-term oncologic outcomes and, if possible, restoration of bowel function and avoidance of permanent stoma. Since total mesorectal excision (TME) results in excellent oncologic outcomes, this surgical technique is widely acceptable as a gold standard for the treatment of rectal cancer. TME allows accurate and complete pathological staging. It is regarded as a curative procedure for either early T stage or node-positive rectal cancer. This radical resection could be a low anterior resection (LAR) with coloanal anastomosis or an abdominoperineal resection (APR) with a permanent colostomy. However, TME has been associated with postoperative mortality rate of 2–3% and morbidity rate of 20–30% including anastomotic leakage [2]. Furthermore, TME may result in poor functional outcomes adversely affecting quality of life such as sexual and urinary dysfunction, infertility, unsatisfactory bowel function, and the possibility for a permanent stoma [3,4,5].
Comparing to TME, local excision (LE) of rectal cancer yields fewer postoperative complications, less blood loss, shorter hospital stay, and quicker recovery. However, while LE is less invasive, it might be associated with poorer oncologic outcomes due to failure to remove occult lymph node metastases in the mesorectum. As a result, appropriate selection of patients and tumors as well as an intense postoperative surveillance to detect any recurrence is crucial when LE is considered as a treatment option for rectal cancer. With the current advances in diagnosis and treatment modalities including endoscopic submucosal dissection, transanal endoscopic microsurgery, and (neo-)adjuvant chemoradiation, LE has now become a much more viable alternative to radical surgery in early rectal cancer.
Similar to TME, LE aims to optimize oncologic outcomes while minimizing postoperative morbidities [6]. However, there are some controversial issues regarding surgical treatments in early clinical stage I (cT1–cT2) rectal cancer—especially between TME and LE. This article aims to critically and comprehensively review the current status of surgical options in cT1–cT2 early rectal cancer.
Techniques of Local Excision and Criteria for Patient Selection in Early Rectal Cancer
For early rectal cancer (cT1–cT2N0M0), most surgeons recommend radical resection (i.e., TME). In recent years, the tendency of surgery in early rectal cancer has shifted toward less invasive procedures (i.e., LE) because it could avoid major complications and unfavorable bowel function following TME. Techniques of LE have been developed for many years including transanal excision (TAE), trans-sphincteric local excision or the York Mason procedure [7], and trans-sacral local excision or the Kraske procedure [8]. Technically, TAE is suitable for mobile tumor in distal rectum with a tumor diameter of less than 3 cm and occupying less than one third of bowel circumference [9]. For more proximal lesion, the tumor can be approached by trans-sacral or trans-sphincteric excisions. However, trans-sacral or trans-sphincteric excision had high complication rate and undesirable functional outcomes.
The advent of transanal endoscopic microsurgery (TEM) described by Gerhard Buess of Tubingen, Germany, in 1980 seems to resolve the limitation of TAE and reduce unfavorable complications of the trans-sacral or the trans-sphincteric excision [10]. This technique has had a slow clinical implementation because of its technically demanding nature and the cost of special instrumentation. Until 2009, a group from the minimally invasive surgery center of FL, USA, proposed a technique called trans-anal minimally invasive surgery (TAMIS). The procedure was started by using a single-port platform placed at the anal canal to maintain a seal for air insufflation into the rectum then performing TAE with a video camera and laparoscopic instruments [11]. TAMIS leads to a reconsideration using endoscopic excision in early rectal carcinoma as it is cheaper than TEM but anticipated similar results of TEM. Endoscopic visualization for trans-anal minimally invasive surgery (eTAMIS) has been reported in some literature with limited long-term follow-up [12].
Endoscopic submucosal dissection (ESD) is another advanced endoscopic technique which has recently become one of the treatment options for early colorectal cancer. This procedure was originally pioneered in Japan in 1999 [13]. Being a partial-thickness resection, ESD is only suitable for treating rectal cancer invading into the submucosa of less than 1000 μm or the so-called sm1 lesion [14, 15]. However, determining the depth of tumor invasion prior to performing ESD is currently challenging.
Practically, LE should be considered for curative intent only in T1N0 rectal cancer with low-risk histopathological features—which include the tumor with the following characteristics: (1) well to moderately differentiated, (2) absence of lympho-vascular invasion, (3) absence of perineural invasion, and (4) absence of mucinous components. For tumor with high-risk histopathological features, LE should not be performed as a curative procedure because of a significant risk of nodal metastasis (about 10–15%) [16]. Unfortunately, while current stringent criteria are followed for selecting patients with LE, high recurrence is still widely reported [4, 17, 18].
Outcomes of LE Versus TME in T1 Rectal Cancer
Data available regarding oncologic outcomes of LE emanates from case series with a limited number of studies comparing LE to radical resection. Due to the retrospective nature of these studies, selection bias of patient was unavoidable. For example, Willett and his colleagues reported a comparable 5-year recurrence-free survival and local control rate between TAE and APR only when T1 rectal cancer with favorable histology was selected [19]. On the other hand, different studies have demonstrated that TAE had a higher rate of local recurrence (7–18%) compared to TME (0–3%)—with an inferior 5-year overall survival [3,21,, 4, 20–22]. Recently, a report from the Memorial Sloan-Kettering Cancer Center has emphasized on the application of TAE for T1 low-risk rectal cancers. With a median follow-up of 5.6 years, there was a significant difference in 5-year disease-specific and overall survival between TAE and TME, favoring TME [23].
Since T1 lesion may carry a different risk of nodal metastasis, Kikuchi and his co-workers demonstrated that a deeper level of submucosal invasion was associated with a higher incidence of perirectal lymph node metastasis. The authors equally divided submucosal layer (between muscularis mucosae and muscular propria) into three parts: sm1, sm2, and sm3. For tumor slightly invading into the submucosa (sm1), lymph node metastasis was barely detected. For tumor invading the deepest one third of the submucosa (sm3), lymph node metastasis was approximately 25% [24]. However, it is impossible to determine the depth of submucosal invasion (sm level) in specimen resected by LE that does not include full thickness of rectal wall, e.g., ESD. As a result, Kitajima and his colleagues further analyzed the depth of submucosal invasion in microns from muscularis mucosae and found that T1 rectal tumor invading submucosa deeper than 1000 μm had a 5-fold increased risk of lymph node metastasis than those with lesser invasion [25].
Outcomes of LE Versus TME in T2 Rectal Cancer
LE in T2 rectal cancer carries a higher local recurrence than T1 lesions, ranging from 13 to 30%. For TME in T2 rectal cancer, rate of local recurrence was around 7%. A higher local recurrence rate of LE in T2 lesion is likely due to an increased risk of perirectal lymph node metastasis (28–38%) [26]. Local recurrence following LE in T2 lesion resulted in worse overall survival when compared to TME. This was confirmed by a US nationwide study in 2007 [27], which demonstrated an inferior overall survival of LE (68%) to radical surgery (77%). However, the 5-year disease-free survival was not different between LE and radical surgery (90 vs 92%). It is argued that patient’s factors such as advanced age and multiple co-morbidities rather than type of surgery determine overall survival [28]. To date, TME is recommended as a standard of care in T2 rectal cancers while LE is only reserved for T2 rectal cancer patients with advanced age or patients with a prohibitive risk to undergo major surgery.
Outcomes of Other LE Techniques in T1 and T2 Rectal Cancer
TAE is the most common LE technique. It has been performed by colorectal surgeons for more than three decades. Recent LE techniques include TEM, TAMIS, and ESD. TEM and TAMIS bare the same principles and comparable technique. Because of the superior visualization and delicate instrumentations, TEM and TAMIS can reach more proximal lesion than TAE and the former could yield more complete en bloc resection of the tumor. Despite the fact that TEM had a lower rate of R1 resection than TAE (2 vs 16%) [29], achieving R0 resection by TEM did not prevent local recurrence [30]. Reportedly, local recurrence after TEM in low-risk T1 rectal cancer could be as high as 17% [30]. There was also no significant difference in 5-year recurrence of early rectal cancer treated by either TAE or TEM [29]. This could be the result of the incomplete removal of potential nodal metastasis in some forms of LE [18].
A limited number of trials have reported outcomes between TEM and TME—with some conflicting results. For example, a small prospective study comparing outcomes of 50 T1 rectal cancer patients undergoing either TEM or radical surgery demonstrated that 5-year local recurrence after TEM was 4.1% but none in TME group. However, with a median follow-up of 3.5 years, 5-year overall survival was comparable between the two techniques [31]. In contrast, with a larger sample size, the TME Dutch trial showed a higher local recurrence in TEM group [32]. Hence, TEM should be performed with caution in the treatment of early rectal cancer. Criteria for patient selection as of conventional TAE must be exercised.
Salvage Surgery After Local Excision
In general, LE has a significant higher rate of local recurrence than TME in high-risk T1 and T2 rectal cancers. Therefore, LE is not standard of care in such cases—instead, TME is the potentially curative operation of choice in these circumstances. Tumor recurrence after LE may occur in the rectal wall, mesorectum, or regional lymph nodes. If recurrent or residual disease is detected early, salvage surgery may be performed with a curative intention. However, several studies reported that significant disease progression, including distant metastasis, was evident prior to the detection of local recurrence.
Friel and his colleagues reported that, within intensive surveillance, 93% of patients with local recurrence presented with stage III disease and curative R0 resection was achieved in only 79% of the patients [33]. Another study from the Memorial Sloan-Kettering Cancer Center showed that 94% of patients with local recurrence after LE could undergo curative resections, but most of them required extensive pelvic operation. In spite of an aggressive salvage operation, disease-free survival was quite low [34]. Timing of salvage surgery after LE is extremely crucial as described by Baron and his team. Their study retrospectively compared the results between immediate salvage surgery after LE with unfavorable histology and salvage surgery performed when local recurrence was clinically detected. The authors demonstrated that 5-year disease-free survival was significantly higher in patients undergoing immediate salvage surgery (94%) comparing to those in the delayed salvage surgery (56%) [35]. The oncologic advantage of immediate salvage surgery was highlighted by Hahnloser and his colleagues. They showed that the oncologic outcome of immediate salvage surgery after LE was comparable to an initial radical surgery in early rectal cancer [36]. Hence, immediate salvage radical surgery is recommended for patients with high-risk T1 and T2 lesions who have a higher chance of local recurrence. If such high-risk patients especially with T2 lesions refuse immediate salvage surgery, they have to be informed that they carry a significant risk of local recurrence even with intensive and close surveillance program. Extensive salvage operations and decreased survival are inevitable when local recurrence occurred. Delay in diagnosis until symptoms occur makes salvage surgery substantially less feasible [37].
Adjuvant Chemoradiation After Local Excision
Adjuvant chemoradiation may have a role in reducing local recurrence after LE especially in patients with high-risk T1 or T2 rectal cancer. A retrospective study comparing LE alone to LE followed by radiation in early rectal cancer found no difference in 5-year local recurrence and disease-free survival between the two groups. But, in high-risk T1 and T2 rectal cancer, local recurrence in those with postoperative radiation therapy was significantly lower than those without (37 vs 85%)—with a modestly better disease-free survival in the adjuvant setting [38].
A phase II prospective multicenter trial conducted by the Radiation Therapy Oncology Group (RTOG) evaluating adjuvant chemoradiation after LE has been reported. This study divided patients into three groups: (1) low-risk T1 lesions with negative margin managed by clinical surveillance, (2) high-risk T1 or more than T2 lesions managed by postoperative standard dose of chemoradiation, and (3) patients similar to the second group but with positive margin managed by a higher dose of chemoradiation. With median follow-up of approximately 6 years, local recurrence was around 12% in all groups. The risk of recurrence depended on resection margin and T stage (4% in T1, 16% in T2, and 23% in T3). The 5-year free of pelvic relapse was 86% in the latter two groups with chemoradiation. The recurrence rate especially in T2 and T3 tumors in this study was comparable to patients treated with radical surgery. These findings supported the beneficial effects of adjuvant chemoradiation therapy in high-risk early rectal cancer patient who underwent LE [39].
Another prospective multicenter trial from the Cancer and Leukemia Group B (CALGB) revealed treatment outcomes between 59 patients with T1 lesions treated by LE alone and 51 patients with T2 lesions treated by LE plus postoperative chemoradiation. With a median follow-up of 7 years, recurrence rate was 7% for T1 and 14% for T2. The 10-year overall survival and disease-free survival were 84 and 75% for T1, 66 and 64% for T2 [40]. The authors concluded that LE alone for T1 was associated with low recurrence and good long-term survival while T2 lesions treated by LE and adjuvant therapy had higher recurrence rate.
Although a randomized controlled trial examining the advantage of adjuvant therapy after LE is lacking, there was a tendency of lower recurrence and better disease-free survival in those receiving adjuvant chemoradiation. To date, a multicenter randomized trial named TESAR trial is ongoing conducted to compare outcomes between TME and postoperative chemoradiation in high-risk T1 or T2 rectal cancer treated by LE with endoluminal excision technique (TEM, TAMIS, ESD) [41].
Local Excision After Neoadjuvant Chemoradiation
This is a relatively new area in oncology because some patients with rectal cancer (typically T2 or T3) who received neoadjuvant chemoradiation undergo LE due to their poor status for radical surgery or refuse of major operation. Many retrospective reviews with small number of patients and short-term follow-up revealed promising results from this approach. A comparative study between 26 rectal cancer patients with neoadjuvant chemoradiation followed by LE and 405 patients with the same chemoradiation regimen followed by TME found that LE group had a 5-year local recurrence rate of 6% and an overall survival rate of 86% comparing to 8 and 81%, respectively, in TME group [42]. However, there was a selection bias because a tendency toward less advanced disease and a better response to chemoradiation were seen in LE group. Lezoche and co-workers reported 100 patients with T2 or T3 rectal cancers treated with radiation or chemoradiation followed by TEM [43]. The 5-year local recurrence and overall survival rates were 5 and 72%, respectively. The same authors also conducted a prospective randomized trial comparing TEM to laparoscopic TME in 70 T2N0 rectal cancer patients having neoadjuvant chemoradiation. Interestingly, pathologic complete response was high (35%) in both groups. With a median follow-up of 84 months, local recurrence rate was 5.7% in TEM group and 2.8% in laparoscopic TME group [44•]. The local recurrence rates in this study were significantly lower than the expected rate of lymph node metastasis in patients with T2 tumors. This result is probably due to the effect of neoadjuvant treatment in perirectal lymph node metastasis in these patients.
Recently, the American College of Surgeons Oncology Group (ACOSOG) reported the ACOSOG Z6041 trial which was a phase II trial determining 3-year disease-free survival rate of cT2cN0 rectal cancer patients staged by endorectal ultrasonography or endorectal coil MRI and underwent neoadjuvant chemoradiation followed by LE. Chemoradiation regimen comprised capecitabine and oxaliplatin with a total radiation dose of 50.4–54 Gy. With a median follow-up of 56 months, there was a 3-year disease-free survival rate of 88.2% in an intention-to-treat basis. The authors emphasized that chemoradiation followed by LE for T2N0 rectal cancer resulted in a very high complete pathologic response (49%) and negative resection margin (99%). Although the observed 3-year disease-free survival in this study was slightly lower than previously reported, the authors suggested that neoadjuvant chemoradiation followed by LE might be considered as an organ-preserving alternative in carefully selected T2N0 rectal cancer patients who refuse or are not candidates for TME [45••]. Since the ACOSOG Z6041 trial was an open-label, non-randomized, phase II trial with a small sample size of 79 patients with highly selective T2N0 low rectal cancer (tumor <4 cm in diameter involving <40% of rectal circumference), a prospective randomized phase III trial comparing oncological and functional outcomes between neoadjuvant chemoradiation followed by LE versus radical surgery for T2N0 rectal cancer with longer follow up is definitely warranted. Moreover, the drawbacks of preoperative chemoradiation have to be discussed with patients because its toxic effects were quite high as demonstrated in this study (29% gastrointestinal and 15% hematological adverse events).
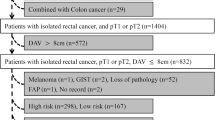
The European multicenter prospective study, known as the CARTS study, investigated cT1–cT3N0 rectal cancer patients treated with long-course radiation and concurrent capecitabine. Six weeks after completion of neoadjuvant therapy, the patients were re-evaluated and classified into good clinical responder (cT0 to cT2 or scar) and no clinical responder (more than cT2). No clinical responders underwent TME 8–10 weeks after chemoradiation then follow-up whereas good responders underwent TEM 8–10 weeks after chemoradiation then further managements based on pathological results (ypT2 or more after TEM underwent salvage TME and ypT0/ypT1 after TEM would be followed up). The enrolled patients included 10 cT1N0, 29 cT2N0, and 16 cT3N0. Chemoradiation-related complications of at least grade 3 occurred in 23 of 55 patients, with two deaths from toxicity, and two patients did not have TEM or major surgery. Among 47 patients who had TEM, ypT0-1 disease was found in 30 patients, ypT0 N1 in one patient, ypT2 in 15 patients, and ypT3 in one patient. Local recurrence developed in three of the nine patients with ypT2 tumors who declined further surgery. Postoperative complications grades I–IIIb occurred in 13 of 47 patients after TEM and in 5 of 12 after salvage surgery. After a median follow-up of 17 months, four local recurrences had developed in overall, three ypT2 patients after TEM who refused further TME, and one out of nine ypT1 patients after TEM. None of the 21 patients with ypT0 lesions after TEM developed a local recurrence. The authors concluded that TEM after chemoradiation enabled organ preservation in one-half of rectal cancer patients [46•]. However, either toxicities or mortality caused by chemoradiation as well as the higher rate of complications in surgery after chemoradiation should be a concern and discussed with patients who opt for this alternative treatment.
An ongoing phase II multicenter randomized controlled trial called the transanal endoscopic microsurgery and radiotherapy in early rectal cancer (TREC) trial has been reported [47]. This trial will be conducted to compare between TME and short-course radiation therapy followed by TEM 8–10 weeks later in early rectal cancer. In the meantime, a phase III trial protocol that combined the phase II protocols, the TREC and CARTS trials called STAR-TREC trial, has been proposed [48]. The authors will enroll early rectal cancer patients who will be randomized to one of three groups in a 1:1:1 basis: (1) TME only, (2) short-course radiation therapy followed by watch and wait or TEM or TME, and (3) long-course radiation with concurrent capecitabine followed by watch and wait or TEM or TME.
Conclusion
Accurate clinical staging is the key for success and guidance of appropriate management in early (cT1/cT2) rectal cancer. To date, endorectal ultrasonography and high-resolution rectal MRI are the investigations of choice to define accurate preoperative clinical staging. For cT1N0M0 rectal cancer, local excision may be performed with a full thickness excision. There is a tendency to gain more acceptable margin if TEM was applied comparing to conventional TAE technique particularly in more proximal rectal lesion.
If the excised specimen has low-risk features (such as pT1sm1 or carcinoma invading submucosa less than 1000 μm), intensive and close surveillance after LE is appropriated. If the excised specimen has high-risk features (such as poorly differentiated, positive lymphatic or vascular invasions, threatened or positive resected margin, pT1sm2 or sm3, carcinoma invading submucosa more than 1000 μm, and pT2 or more), immediate salvage TME should be performed. Otherwise, postoperative chemoradiation should be initiated in patients who refuse or are not a good candidate for TME.
In patients with cT2N0M0 rectal cancer, TME should always be offered. If patients are too frail for radical surgery or deny major operation, neoadjuvant chemoradiation followed by LE might be an alternative. Patients must be advised for potential toxicities and mortality of chemoradiation along with higher complication rate of LE after chemoradiation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stamos MJ, Murrell Z. Management of early rectal T1 and T2 cancers. Clin Cancer Res. 2007; 13: 6885s-9s.
Endreseth BH, Myrvold HE, Romundstad P, et al. Transanal excision vs. major surgery for T1 rectal cancer. Dis Colon Rectum. 2005;48:1380–8.
Madbouly KM, Remzi FH, Erkek BA, et al. Recurrence after transanal excision of T1 rectal cancer: should we be concerned? Dis Colon Rectum. 2005;48:711–9.
Bentrem DJ, Okabe S, Wong WD, et al. T1 adenocarcinoma of the rectum: transanal excision or radical surgery? Ann Surg. 2005;242:472–7.
Blumberg D, Paty PB, Guillem JG, et al. All patients with small intramural rectal cancers are at risk for lymph node metastasis. Dis Colon Rectum. 1999;42:881–5.
Stitzenberg KB, Sanoff HK, Penn DC, et al. Practice patterns and long-term survival for early-stage rectal cancer. J Clin Oncol. 2013;31:4276–82.
Mason AY. Transsphincteric approach to rectal lesions. Surg Annu. 1977;9:171–94.
Kraske P, Perry EG, Hinrichs B. A new translation of professor Dr P. Kraske’s Zur Exstirpation Hochsitzender Mastdarmkrebse. 1885. Aust N Z J Surg. 1989;59:421–4.
Engstrom PF, Arnoletti JP, Benson 3rd AB, et al. NCCN Clinical Practice Guidelines in Oncology: rectal cancer. J Natl Compr Canc Netw. 2009;7:838–81.
Buess G, Theiss R, Hutterer F, et al. Transanal endoscopic surgery of the rectum—testing a new method in animal experiments. Leber Magen Darm. 1983;13:73–7.
Atallah S, Albert M, Larach S. Transanal minimally invasive surgery: a giant leap forward. Surg Endosc. 2010;24:2200–5.
McLemore E, Coker A, Jacobsen G, et al. eTAMIS: endoscopic visualization for transanal minimally invasive surgery. Surg Endosc. 2013;27:1842–5.
Gotoda T, Kondo H, Ono H, et al. A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: report of two cases. Gastrointest Endosc. 1999;50:560–3.
Kudo S, Kashida H, Nakajima T, Tamura S, Nakajo K. Endoscopic diagnosis and treatment of early colorectal cancer. World J Surg. 1997;21:694–701.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003; 58 (6, Suppl): S3-S43.
Nascimbeni R, Burgart LJ, Nivatvong S, Larson DR. Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum. 2002;45:200–6.
Wirsing K, Lorenzo-Rivero S, Luchtefeld M, et al. Local excision of stratified T1 rectal cancer. Am J Surg. 2006;191:410–2.
Lohsiriwat V, Anubhonganant W, Prapasrivorakul S, et al. Outcomes of local excision for early rectal cancer: a 6-year experience from the largest university hospital in Thailand. Asian Pac J Cancer Prev. 2013;14:5141–4.
Willett CG, Compton CC, Shellito PC, Efird JT. Selection factors for local excision or abdominoperineal resection of early stage rectal cancer. Cancer. 1994;73:2716–20.
Garcia-Aguilar J, Mellgren A, Sirivongs P, et al. Local excision of rectal cancer without adjuvant therapy: a word of caution. Ann Surg. 2000;231:345–51.
Mellgren A, Sirivongs P, Rothenberger DA, et al. Is local excision adequate therapy for early rectal cancer? Dis Colon Rectum. 2000;43:1064–71.
Nascimbeni R, Nivatvongs S, Larson DR, et al. Long-term survival after local excision for T1 carcinoma of the rectum. Dis Colon Rectum. 2004;47:1773–9.
Nash GM, Weiser MR, Guillem JG, et al. Long-term survival after transanal excision of T1 rectal cancer. Dis Colon Rectum. 2009;52:577–82.
Kikuchi R, Takano M, Takagi K, et al. Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis Colon Rectum. 1995;38:1286–95.
Kitajima K, Fujimori T, Fujii S, et al. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol. 2004;39:534–43.
Gopaul D, Belliveau P, Vuong T, et al. Outcome of local excision of rectal carcinoma. Dis Colon Rectum. 2004;47:1780–8.
You YN, Baxter NN, Stewart A, et al. Is the increasing rate of local excision for stage I rectal cancer in the United States justified?: a nationwide cohort study from the National Cancer Database. Ann Surg. 2007;245:726–33.
Chang GJ, Skibber JM, Feig BW, Rodriguez-Bigas M. Are we undertreating rectal cancer in the elderly? An Epidemiologic Study Ann Surg. 2007;246:215–21.
Christoforidis D, Cho HM, Dixon MR, et al. Transanal endoscopic microsurgery versus conventional transanal excision for patients with early rectal cancer. Ann Surg. 2009;249:776–82.
Doornebosch PG, Ferenschild FT, de Wilt JH, et al. Treatment of recurrence after transanal endoscopic microsurgery (TEM) for T1 rectal cancer. Dis Colon Rectum. 2010;53:1234–9.
Winde G, Nottberg H, Keller R, Schmid KW, Bünte H. Surgical cure for early rectal carcinomas (T1). Transanal endoscopic microsurgery vs. anterior resection. Dis Colon Rectum. 1996;39:969–76.
De Graaf EJ, Doornebosch PG, Tollenaar RA, et al. Transanal endoscopic microsurgery versus total mesorectal excision of T1 rectal adenocarcinomas with curative intention. Eur J Surg Oncol. 2009;35:1280–5.
Friel CM, Cromwell JW, Marra C, et al. Salvage radical surgery after failed local excision for early rectal cancer. Dis Colon Rectum. 2002;45:875–9.
Weiser MR, Landmann RG, Wong WD, et al. Surgical salvage of recurrent rectal cancer after transanal excision. Dis Colon Rectum. 2005;48:1169–75.
Baron PL, Enker WE, Zakowski MF, et al. Immediate vs. salvage resection after local treatment for early rectal cancer. Dis Colon Rectum. 1995;38:177–81.
Hahnloser D, Wolff BG, Larson DW, et al. Immediate radical resection after local excision of rectal cancer: an oncologic compromise? Dis Colon Rectum. 2005;48:429–37.
de Anda E, Lee SH, Finne CO, et al. Endorectal ultrasound in the follow-up of rectal cancer patients treated by local excision or radical surgery. Dis Colon Rectum. 2004;47:818–24.
Chakravarti A, Compton CC, Shellito PC, et al. Long-term follow-up of patients with rectal cancer managed by local excision with and without adjuvant irradiation. Ann Surg. 1999;230:49–54.
Russell AH, Harris J, Rosenberg PJ, et al. Anal sphincter conservation for patients with adenocarcinoma of the distal rectum: long-term results of radiation therapy oncology group protocol 89-02. Int J Radiat Oncol Biol Phys. 2000;46:313–22.
Greenberg JA, Shibata D, Herndon JE, et al. Local excision of distal rectal cancer: an update of cancer and leukemia group B 8984. Dis Colon Rectum. 2008;51:1185–91.
Borstlap WA, Tanis PJ, Koedam TW, et al. A multi-centred randomised trial of radical surgery versus adjuvant chemoradiotherapy after local excision for early rectal cancer. BMC Cancer. 2016;16:513.
Bonnen M, Crane C, Vauthey JN, et al. Long-term results using local excision after preoperative chemoradiation among selected T3 rectal cancer patients. Int J Radiat Oncol Biol Phys. 2004;60:1098–105.
Lezoche E, Guerrieri M, Paganini AM, et al. Long-term results in patients with T2-3 N0 distal rectal cancer undergoing radiotherapy before transanal endoscopic microsurgery. Br J Surg. 2005;92:1546–52.
• Lezoche G, Baldarelli M, Guerrieri M, et al. A prospective randomized study with a 5-year minimum follow-up evaluation of transanal endoscopic microsurgery versus laparoscopic total mesorectal excision after neoadjuvant therapy. Surg Endosc. 2008;22:352–8. A prospective RCT evaluating long-term outcomes between TEM vs. laparoscopic TME in rectal cancer patients after receiving chemoradiation.
•• Garcia-Aguilar J, Renfro LA, Chow OS, et al. Organ preservation for clinical T2N0 distal rectal cancer using neoadjuvant chemoradiotherapy and local excision (ACOSOG Z6041): results of an open-label, single-arm, multi-institutional, phase 2 trial. Lancet Oncol. 2015;16:1537–46. A phase II prospective trial evaluating the outcomes after LE in T2N0 rectal cancer patients.
• Verseveld M, de Graaf EJ, Verhoef C, et al. Chemoradiation therapy for rectal cancer in the distal rectum followed by organ-sparing transanal endoscopic microsurgery (CARTS study). Br J Surg. 2015;102:853–60. A European multicenter prospective study determining outcomes of TEM after long course chemoradiation.
TREC study (2016) http://www.isrctn.com/ISRCTN14422743. (Accessed 10 November 2016)
STAR-TREC study (2016) http://www.isrctn.com/ISRCTN14240288. (Accessed 10 November 2016)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Surgery and Surgical Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
Riansuwan, W., Lohsiriwat, V. Local Excision Versus Total Mesorectal Excision for Clinical Stage I (cT1–cT2) Rectal Cancer. Curr Colorectal Cancer Rep 13, 54–60 (2017). https://doi.org/10.1007/s11888-017-0350-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-017-0350-0