Abstract
Purpose of Review
Sudden cardiac death (SCD) is a major public health burden accounting for 15–20% of global mortality. Contemporary guidelines for SCD prevention are centered around the presence of low left ventricular ejection fraction, although the majority of SCD accrues in those not meeting contemporary criteria for SCD prevention. The goal of this review is to elaborate on the contemporary landscape of SCD prediction tools and further highlight gaps and opportunities in SCD prediction and prevention.
Recent Findings
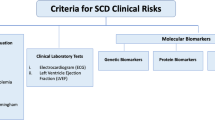
There have been considerable advancements in both non-invasive and invasive measures for SCD risk prediction including clinical morbidities, electrocardiographic measures, cardiac imaging (nuclear, magnetic resonance, computed tomography), serum biomarkers, genetics, and invasively assessed electrophysiological characteristics. Novel methodological approaches including application of machine learning, incorporation of competing risk, and use of computational modeling have underscored a future of personalized risk prediction.
Summary
SCD remains a vital public health challenge. Emerging methods highlight opportunities to improve SCD prediction in the majority of those at risk who do not meet contemporary criteria for SCD prevention therapies. Future efforts will need to focus on easily deployed, multi-parametric risk models that enrich for SCD risk and not for competing mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sudden cardiac death (SCD) is a major public health challenge, estimated to account for up to 20% of deaths worldwide [1]. Coronary heart disease is the most common underlying substrate for SCD which is often secondary to ventricular arrhythmias. For patients with symptomatic heart failure and depressed left ventricular ejection fraction (LVEF; < 30–35%), implantable cardioverter-defibrillator (ICD) therapy improves survival [2]. Importantly, up to 70% of the global burden of SCD occurs in patients with an LVEF greater than 35% [3] for whom there is no consensus strategy for SCD prediction or prevention. Furthermore, the survival benefit of ICD therapy even in those who qualify for ICD therapy—including, for example, patients with non-ischemic cardiomyopathy (NICM)—has more recently been called into question on the basis of randomized clinical trials [4] and observational evidence suggesting attenuating rates of SCD in the contemporary era of heart failure pharmacotherapy [5]. Taken together, there remains a critical unmet need to improve SCD risk prediction to tackle this ongoing public health burden.
Left Ventricular Function as Predictor—Limitations
Abnormal LVEF has been long recognized as a major risk factor for SCD, initially in patients with myocardial infarction [6] and subsequently in patients with NICM [7]. Low LVEF was a consistent inclusion criteria for seminal trials establishing the efficacy of ICD therapy [2] and is a cornerstone of contemporary guidelines for SCD primary prevention [8]. There are, however, limitations to the use of LVEF as a predictor of SCD and its role in identifying those who may benefit from ICD therapy. As our group and others have shown [9], there is a continuous, inverse relationship between LVEF and SCD risk suggesting that the contemporary paradigm dichotomizing LVEF at 30–35% for ICD candidacy underestimates risk across the range of LV function. Furthermore, a low LVEF is not only a predictor of SCD but also a predictor of competing, non-SCD mortality [9]. When considering the association of LVEF with competing risk mortality, reliance on LVEF to identify patients likely to benefit from SCD prevention therapies is less clear. These limitations help frame the unmet scientific needs in SCD risk prediction which include (1) identifying markers of SCD risk across the spectrum of LV function as well as (2) markers that are specific to SCD and not competing modes of death.
Clinical and Lifestyle Predictors of Sudden Death Risk
Coronary heart disease is the most common underlying substrate for SCD. Other clinical risk factors associated with a higher risk of SCD in the general population include diabetes mellitus [10, 11], hypertension [12], hyperlipidemia [13], obesity [14], atrial fibrillation [9, 15], and chronic kidney disease [16]. In addition to these clinical risk factors, a family history of SCD has also been associated with an increased in SCD risk in the general population [17], although the association is less clear in patients with established coronary heart disease [9]. In terms of lifestyle factors, smoking is a potent risk factor for SCD and smoking cessation is associated with a lower risk of SCD [18]. Population-based cohort studies have shown a general relationship between alcohol consumption and risk of SCD [19], though the association with SCD may be more complex, with some studies suggesting a U-shaped relationship [20]. Physical activity has generally been associated with a lower risk of SCD in the general population [21] though vigorous activity has been associated with SCD risk, particularly in men [22].
Non-invasive Electrocardiographic Markers of SCD Risk
Resting 12-Lead Electrocardiogram
There has been a long standing interest in the role of cross-sectional and continuous rhythm monitoring as a means to predict sudden cardiac death. The role of the resting 12 lead ECG as a tool for risk prediction has been appealing given its low-cost and widespread deployment in a range of clinical settings. As our group [23] and others have demonstrated [24], the ECG is able to capture domains of risk that are relevant to the pathophysiology of SCD. Salient ECG predictors associated with SCD risk in patients with and without established cardiovascular disease include markers of structural abnormalities (contiguous Q waves, left ventricular hypertrophy, left atrial enlargement) [25,26,27,28], autonomic risk (resting heart rate) [29, 30], abnormalities of electrical depolarization (QRS duration, Q wave fragmentation, bundle branch block) [31,32,33,34,35], and abnormalities of repolarization (JT prolongation, T-wave inversion) [36,37,38,39]. More complex ECG parameters derived from signal-averaged ECG, including identification of late ventricular potentials, have also been linked to SCD in both ischemic [40] and non-ischemic cardiomyopathy [41] though positive predictive accuracy in meta-analysis was poor (20%) [41]. Other more complex parameters including use of vectorcardiography to identify abnormal electrical dispersion (e.g., QRS-T angle) have been linked to SCD in observational studies [42, 43] though the practicality of these measures is uncertain given the complexity of measurement and variation in normative values noted across age and sex [44].
Dynamic Electrocardiographic Markers
In addition to cross-sectional assessment, there has also been interest in continuous electrical measures of autonomic function, ventricular ectopy, and dynamic repolarization abnormalities as markers of SCD risk. Perturbations of autonomic tone have been implicated in the risk of ventricular arrhythmias and electrical surrogates of autonomic dysfunction including heart rate variability (HRV), heart rate turbulence (HRT), and baroreflex sensitivity (BRS) have been a focus of risk prediction studies. Dynamic markers of electrical repolarization heterogeneity have also been linked to SCD risk. This has most commonly been quantified as microvolt T-wave alternans, which reflects beat-to-beat alternation of the T-wave amplitude [45].
The performance of these dynamic measures as SCD risk predictors has been mixed and primarily studied in patients with established cardiovascular disease. For example, in patients with NICM, there was only modest association of these autonomic parameters (HRV, BRS, HRT) and SCD risk [41]. Comparatively, in the post-myocardial infarction period in patients with LVEF < 50%, impaired HRT and abnormal T-wave alternans were associated with an increased risk of SCD [46]. Likewise, the combination of abnormal LVEF and autonomic markers did improve the sensitivity of SCD prediction in ischemic cardiomyopathy although positive predictive accuracy in this population was poor (13%) [47]. Finally, ventricular ectopy by continuous rhythm assessment (generally defined as > 10 premature ventricular beats in an hour or the presence of non-sustained ventricular tachycardia) has been variably associated with an increased risk of SCD in the post-MI setting with some studies finding symmetric increases in both arrhythmic and non-arrhythmic mortality [48]. In non-ischemic cardiomyopathy, NSVT was associated with a twofold increase risk of SCD though the positive predictive accuracy of this finding was low (21%) [41].
Cardiac Imaging and Sudden Death Risk
With advances in cardiac imaging modalities including computed tomography (CT), magnetic resonance imaging (MRI) and nuclear cardiac imaging there has been substantial interest in their role in SCD prediction. Cardiac imaging provides the potential to elucidate substrate relevant to SCD risk (e.g., ventricular scar, lipomatous metaplasia), as well as dynamic triggers (e.g., abnormal autonomic innervation) of ventricular arrhythmias.
Cardiac MRI for SCD Prediction
Cardiac MRI is one of most robust imaging modalities linked to SCD risk. The most commonly evaluated parameter is the presence of late gadolinium enhancement (LGE), which is thought to reflect accumulation of collagen in the extracellular space and therefore serve as an imaging surrogate for fibrosis. Notably, LGE may also be present in the setting of non-fibrotic substrate including myocardial edema or infiltrative disease such as amyloid. LGE has been associated with an increased risk of SCD in patients with ischemic heart disease [49, 50] as well as patients with NICM [51,52,53]. In both substrates, both the presence of LGE (present or absent) as well as the extent of LGE (evaluated as a continuous function) have been linked to increased SCD risk. In addition to general assessment of LGE, other MRI features of myocardial scar such as scar heterogeneity (typified using various parameters including scar border zone [54], gray zone [55], and scar entropy [56]) or localization characteristics (e.g., ring-like pattern of fibrosis [57]) have also been associated with an increased risk of SCD. In addition to its prognostic use in ischemic and non-ischemic dilated cardiomyopathy, LGE on cardiac MRI has also been associated with increased SCD risk in other cardiac substrates including acute myocarditis [58, 59], sarcoidosis [60], hypertrophic cardiomyopathy [61], left ventricular non-compaction [62], and arrhythmogenic right ventricular cardiomyopathy [63]. Perhaps the most practical question related to LGE as a risk marker is the identification of a numeric threshold to guide clinical decision making such as ICD implantation. This threshold will likely vary in accordance with substrate. There has been limited work identifying such thresholds in hypertrophic cardiomyopathy where LGE ≥ 10% appears to be increment risk beyond traditional clinical risk markers [64, 65]. Such thresholds remain unknown in non-ischemic cardiomyopathy and for ischemic cardiomyopathy, it is possible that scar characteristics (e.g., gray zone, border zone, entropy) are more potent predictors of SCD risk than scar size to the extent that areas of trans-mural “core” scar are less likely to be arrhythmogenic.
Another intriguing imaging feature evident on MRI is the presence of lipomatous metaplasia (LM). LM is thought to be related to the infiltration of infarcted myocardium by adipose cells. Given the uniquely higher impedance of LM compared to fibrotic scar, the increased regional resistance and reduced current loss at sites of LM has been theorized to be associated with a higher risk of electrical re-entry and ventricular arrhythmia. In the recent INFINITY (Intra-Myocardial Fat Deposition and Ventricular Tachycardia in Cardiomyopathy) study enrolling patients with ischemic cardiomyopathy and ventricular arrhythmias, the majority of invasively mapped VT circuits corresponded to sites of LM [66•], suggesting this as a potential exciting avenue for future risk stratification.
Cardiac CT and Nuclear Imaging for SCD Prediction
Other imaging modalities linked to SCD risk stratification include cardiac CT and nuclear imaging, specifically single-photon emission computer tomography (SPECT) and positron emission tomography (PET). For cardiac CT, there is emerging evidence for its use to detect myocardial fibrosis via late enhanced multi-slice formatting [67]. This might of particular benefit in patients who are either not a candidate for cardiac MRI or for whom LGE assessment by MRI is obscured by imaging artifact related to indwelling cardiac devices. In addition, recent work has identified cardiac CT-derived channels (i.e., areas of wall thinning adjacent to relatively preserved thickness) as potent predictors of VT isthmuses during invasive electrophysiology study in patients with ischemic cardiomyopathy [68].
Finally, there has been long standing interest in the role of nuclear SPECT imaging to identify abnormal autonomic or sympathetic innervation as a risk marker for SCD. Several studies including the ADMIRE (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) [69] and PARAPET (Prediction of Arrhythmic Events with Positron Emission Tomography) [70] studies identified associations between abnormal SPECT imaging and SCD risk in both ischemic and non-ischemic cardiomyopathy. Other nuclear modalities such as PET are known to identify metabolically active tissue and have been shown to be potent predictors of ventricular arrhythmia risk in particular cardiac substrates such as cardiac sarcoidosis [71]. Given the expanding recognition of myocardial inflammation and PET abnormalities in non-ischemic cardiomyopathy [72] and genetic cardiomyopathy [73, 74], it will be of interest to see the role of PET as a risk marker in these expanded populations.
Emerging Markers of Risk—Circulating Biomarkers, Genetics, Computational Modeling, and Invasive Cellular Phenotyping
There are several emerging tools for SCD risk prediction including novel circulating biomarkers, genetic risk scores, computational modeling, and invasive phenotyping.
Circulating Biomarkers of SCD Risk
To the extent that circulating biomarkers exert physiological effects on the myocardium—either structurally or electrically—there has been interest in identifying signatures of SCD risk from the blood. Recent proteomics analysis of survivors of cardiac arrest identified 6 novel biomarkers—implicated in extracellular matrix formation, coagulation cascades, and platelet activation—associated with SCD [75]. Our group similarly identified three circulating microRNAs (miR-150, miR29a-3p, and miR-30a-5p)—implicated in apoptosis, fibrosis and inflammation—associated with a nearly fivefold gradient of SCD risk in patients with coronary disease and low normal LVEF compared to healthy controls [76]. Other biomarkers that have been linked to SCD include markers of inflammation including interleukin-6 and C-reactive protein) [77, 78], dietary markers (e.g., circulating long-chain n-3 fatty acids) [79], metabolic markers (e.g., cystatin C) [80], and neuro-hormonal markers (e.g., renin) [81]. These markers have been evaluated in a range of substrates from the general population without prevalent heart disease to those with established ischemic heart disease. The utility of serum markers for risk stratification may be hampered by their associations with non-SCD risk, as well as the generally low magnitude of risk elevation for any individual biomarker.
In addition to enhancing risk of SCD, biomarkers may also identify competing mortality risk and therefore be useful identifying patients unlikely to benefit from SCD prevention. For example, in a recent analysis of a randomized trial of ICD therapy in non-ischemic cardiomyopathy [4], ICD survival benefit was only seen in patients with a low NT-proBNP (< 1177 pg/ml; 40% relative risk reduction in mortality), whereas no survival benefit was seen in those with an elevated NT-proBNP for whom competing mortality risk rendered ICD efficacy null [82].
Genetic Predictors of SCD Risk
In addition to circulating biomarkers, there has also been substantial efforts evaluating the role of cardiovascular genetics as a risk predictor for SCD [83]. Initial approaches leveraged our existing understanding of SCD pathophysiology with a focus on genetic variants associated with factors thought to be on the causal pathway to SCD, including for example coronary heart disease and longer QT interval. With respect to ECG parameters, given that genetic variation accounts for only a minority of variance in ECG parameters, this approach has not identified meaningful risk elevations in the general population [84]. Conversely, genetic variants associated with coronary heart disease have been associated with SCD in both the general population [85] and in patients with established ischemic heart disease [86]. Other approaches have sought to identify common genetic variants implicated in SCD pathophysiology including autonomic function, atherosclerosis, neuro-hormonal activation, and electrical conduction [83]. Taken together, these associations have not been replicated and, given their high prevalence in the population, are unlikely to yield specific risk increments for SCD prediction. Using an inverse approach, genetic studies have also identified rare variants in several commonly known genetic arrhythmic syndromes—including long QT, Brugada, and arrhythmogenic right ventricular cardiomyopathy (ARVC)—that are associated with SCD risk in the general population [87]. While the prevalence of these variants—by definition—is rare in the general population, they may serve as mediator of risk for a subset of the global burden of SCD. To this end, more contemporary work has included genome-wide association studies (GWAS) to identify novel variants associated with SCD risk. A consistent locus of risk has been 21q21 which was associated with an increased risk of VF in patients presenting with an MI [88]. Consistent with the potential importance of rare genetic variants in SCD risk, even more recent work identified 14 variants (including variants associated with familial hypercholesterolemia, long QT syndrome, and dilated cardiomyopathy) present in ~ 1% of the general population that were associated with an approximate threefold increase risk of cardiovascular death including arrhythmic mortality [89].
Computational Modeling for SCD Prediction
Another emerging approach for SCD prediction has been the integration of cardiac imaging with computational modeling. This approach employs three-dimensional models which simulate arrhythmias in silico by integrating cardiac MRI imaging (and associated scar characteristics) with biophysical models of electrical propagation [90]. This approach has demonstrated utility in predicting critical sites of ventricular tachycardia induction for patients with ischemic heart disease during invasive EP study [91] and remains a promising paradigm for personalizing risk assessment. How these models will perform in patients with non-ischemic or genetic heart disease—where scar distribution is more heterogeneous and biophysical assumptions of cellular transduction may be less certain—remains to be seen.
Invasive Phenotyping of SCD Risk
There has also been recent work applying machine learning approaches to invasively assessed monophasic ventricular action potentials as a means to predict SCD in patients with ischemic heart disease and abnormal LVEF [92]. In exploratory biophysical cell models, perturbations in the functionality of L-type calcium current or the sodium-calcium exchanger yielded action potential phenotypes associated with higher SCD risk. Though early, these studies highlight the potential to personalize SCD risk assessment via the integration of advanced computational approaches and invasively determined electrical properties of the ventricle.
Putting It Together and Gaps in Prediction—Risk Models for Sudden Death Prediction
Contemporary SCD Risk Models and Approaches
As highlighted, current gaps in SCD prediction include (1) identification of validated models in patients not currently qualifying for ICD therapy, (2) enriching for benefit in those who do qualify for ICD therapy, and (3) identifying risk markers that are specific to SCD and not competing risk mortality. In contemporary practice, there remains no validated models for SCD risk prediction in the general population. While the absolute risk of SCD in the general population is low (0.1–0.2%/year), the majority of global burden of SCD occurs in the general population. Desperately needed then are novel and creative approaches to enriching and capturing risk in this population, which could include leveraging multi-dimensional data sources such as the electronic heart record to dynamically screen patients for risk. These efforts could involve machine learning as well as advanced computational methods such as natural language processing to enhance our ability to identify risk. Models will need to be externally validated and, importantly, provide sufficient lead-time to deploy further screening and potential intervention to mitigate risk.
In patients with established heart disease but not meeting criteria for SCD prevention (e.g., ICD therapy), there have been a range of proposed models with variable degrees of validation and performance. The most robust example has been the integration of validated SCD risk estimates in hypertrophic cardiomyopathy [93] into contemporary ICD guidelines [94]. Salient features of this model include its ease of use (i.e., deployment of easily measurable clinical and imaging parameters), clear risk output (quantitative SCD risk estimates) over an actionable timeline (5 years), and validation in an independent cohort [93]. There are other recent examples of SCD risk calculators in other substrates with established heart disease including ARVC [95] and patients with established coronary heart disease [96, 97] though validation in the majority of these examples was internal. Another salient limitation of risk models is the often cross-sectional nature of their use in the context of a dynamic disease process. To that end, a recent analysis of an established SCD risk calculator in ARVC [98] showed that the ability of the risk calculator to predict 5 year ventricular arrhythmia risk worsened during follow-up, making the strong case to update risk inputs when evaluating patients clinically.
Application of machine learning to dynamically updated data sources provides an intriguing opportunity to actualize flexible risk prediction. There have been preliminary efforts in patients with established heart disease to apply this approach incorporating demographic, clinical, ECG, imaging, and genetic data [99••]. There are unique features of SCD prediction that challenge the application of machine learning methods, not the least of which is the inevitable rarity of the outcome, yielding an event to control imbalance that makes traditional measures of model performance inaccurate [99••]. This challenge and others, including external validation, interpretability, and ease of use, will be critical to overcome in future application of machine learning to SCD prediction.
In addition to ease of use and deployment of dynamic risk models, effective SCD risk prediction will entail identifying markers specific to SCD and not competing risk mortality. As our group [9] and others [100, 101] have demonstrated, patients at increased risk for SCD but also increased risk of competing mortality are unlikely to benefit from SCD prevention strategies such as ICD therapy. Tools such as the Seattle Proportional Risk Model, which estimates the proportional risk of SCD in patients with heart failure, have demonstrated external validity [102] and utility in identifying patients likely to benefit from ICD therapy [101, 103]. These tools have primarily been applied in patients currently qualifying for ICD therapy and their use in a broader context remains to be seen.
The Future of SCD Risk Prediction
Looking ahead, how should we frame our needs and aspirations in SCD risk prediction? For the general population, where baseline absolute risk is low (0.1–0.2%/year), the clinical utility of a single marker—even one, for example, that doubles the risk of SCD—is not likely to be useful. Therefore, meaningful enrichment of SCD risk will require integration of multiple parameters and use of data sources germane to the general population, such as the electronic health record. Given that the vast majority of those in the general population will not experience SCD, risk models in this population are likely to primarily be used as an initial screen to justify further non-invasive (e.g., imaging), minimally invasive (blood markers, genetics), or invasive (e.g., electrophysiology study) testing.
For patients at intermediate risk including, for example, patients with ischemic heart disease and abnormal LV function not meeting criteria for ICD therapy, there are several potential risk parameters highlighted here that could be used. Needed, however, are robust studies evaluating the integration of these measures (e.g., imaging, biomarkers, genetics) in an externally validated sample of patients. Several of these markers may be associated with both SCD and competing mortality risk, thus blunting the efficacy of SCD prevention tools [9]. Therefore, future work needs to specifically evaluate the association of SCD risk models with both arrhythmic and non-SCD mortality. The ongoing PROFID project (Personalized Risk Prediction and Prevention of Sudden Cardiac Death After Myocardial Infarction) is aimed at understanding the role of personalized multi-parameter risk prediction in identifying ICD benefit in those with ischemic heart disease across a range of LV function [104]. Recent work highlighting the role of imaging (MRI, CT), invasive electrophysiological phenotyping, and machine learning to predict SCD underscore an exciting future of personalized risk prediction and mitigation. It is worth noting that the majority of this work has been centered in patients with ischemic heart disease, underscoring the ongoing gap in knowledge and uncertainty in their utility in other cardiovascular disease substrates.
Finally, for patients meeting contemporary guideline criteria for ICD implantation, there is well-established recognition that the majority of patients receiving an ICD for the primary prevention of SCD will not use their device over the course of their lifetime. Increased penetrance of validated models integrating absolute and proportional risk (e.g., the Seattle Proportional Risk Model) will be important, as will use of imaging (e.g., absence of LGE on cardiac MRI) or biomarkers (e.g., elevated NT-proBNP) to identify those unlikely to benefit.
Conclusion
Sudden cardiac death remains a critical public health burden and is responsible for hundreds of thousands of deaths around the world each year. Promising studies have identified a range of non-invasive and invasive tools to guide SCD risk prediction and prevention. To maximize the public health impact of ongoing efforts, future work will need to focus on identifying SCD prediction strategies in a broader population than contemporary guidelines reliant on LV ejection fraction.
References
Langer C, Lutz M, Eden M, Lüdde M, Hohnhorst M, Gierloff C, et al. Hypertrophic cardiomyopathy in cardiac CT: a validation study on the detection of intramyocardial fibrosis in consecutive patients. Int J Cardiovasc Imaging. 2014;30(3):659–67. https://doi.org/10.1007/s10554-013-0358-8.
Takigawa M, Duchateau J, Sacher F, Martin R, Vlachos K, Kitamura T, et al. Are wall thickness channels defined by computed tomography predictive of isthmuses of postinfarction ventricular tachycardia? Heart Rhythm. 2019;16(11):1661–8. https://doi.org/10.1016/j.hrthm.2019.06.012.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55(20):2212–21. https://doi.org/10.1016/j.jacc.2010.01.014.
Fallavollita JA, Heavey BM, Luisi AJ Jr, Michalek SM, Baldwa S, Mashtare TL Jr, et al. Regional myocardial sympathetic denervation predicts the risk of sudden cardiac arrest in ischemic cardiomyopathy. J Am Coll Cardiol. 2014;63(2):141–9. https://doi.org/10.1016/j.jacc.2013.07.096.
Blankstein R, Osborne M, Naya M, Waller A, Kim CK, Murthy VL, et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol. 2014;63(4):329–36. https://doi.org/10.1016/j.jacc.2013.09.022.
Tung R, Bauer B, Schelbert H, Lynch JP 3rd, Auerbach M, Gupta P, et al. Incidence of abnormal positron emission tomography in patients with unexplained cardiomyopathy and ventricular arrhythmias: the potential role of occult inflammation in arrhythmogenesis. Heart Rhythm. 2015;12(12):2488–98. https://doi.org/10.1016/j.hrthm.2015.08.014.
Lal M, Chen C, Newsome B, Masha L, Camacho SA, Masri A, et al. Genetic cardiomyopathy masquerading as cardiac sarcoidosis. J Am Coll Cardiol. 2023;81(1):100–2. https://doi.org/10.1016/j.jacc.2022.10.021.
Li A, Tung R, Shivkumar K, Bradfield JS. Brugada syndrome-malignant phenotype associated with acute cardiac inflammation? HeartRhythm Case Rep. 2017;3(8):384–8. https://doi.org/10.1016/j.hrcr.2017.04.011.
Norby FL, Nakamura K, Fu Q, Venkatraman V, Sundararaman N, Mastali M, et al. A panel of blood biomarkers unique to sudden cardiac arrest. Heart Rhythm. 2022. https://doi.org/10.1016/j.hrthm.2022.12.014.
Silverman MG, Yeri A, Moorthy MV, Camacho Garcia F, Chatterjee NA, Glinge CSA, et al. Circulating miRNAs and risk of sudden death in patients with coronary heart disease. JACC Clin Electrophysiol. 2020;6(1):70–9. https://doi.org/10.1016/j.jacep.2019.08.011.
Empana JP, Jouven X, Canouï-Poitrine F, Luc G, Tafflet M, Haas B, et al. C-reactive protein, interleukin 6, fibrinogen and risk of sudden death in European middle-aged men: the PRIME study. Arterioscler Thromb Vasc Biol. 2010;30(10):2047–52. https://doi.org/10.1161/atvbaha.110.208785.
Albert CM, Ma J, Rifai N, Stampfer MJ, Ridker PM. Prospective study of C-reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. Circulation. 2002;105(22):2595–9. https://doi.org/10.1161/01.cir.0000017493.03108.1c.
Albert CM, Campos H, Stampfer MJ, Ridker PM, Manson JE, Willett WC, et al. Blood levels of long-chain n-3 fatty acids and the risk of sudden death. N Engl J Med. 2002;346(15):1113–8. https://doi.org/10.1056/NEJMoa012918.
Deo R, Sotoodehnia N, Katz R, Sarnak MJ, Fried LF, Chonchol M, et al. Cystatin C and sudden cardiac death risk in the elderly. Circ Cardiovasc Qual Outcomes. 2010;3(2):159–64. https://doi.org/10.1161/circoutcomes.109.875369.
Tomaschitz A, Pilz S, Ritz E, Morganti A, Grammer T, Amrein K, et al. Associations of plasma renin with 10-year cardiovascular mortality, sudden cardiac death, and death due to heart failure. Eur Heart J. 2011;32(21):2642–9. https://doi.org/10.1093/eurheartj/ehr150.
Butt JH, Yafasova A, Elming MB, Dixen U, Nielsen JC, Haarbo J, et al. NT-proBNP and ICD in nonischemic systolic heart failure: extended follow-up of the DANISH trial. JACC Heart failure. 2022;10(3):161–71. https://doi.org/10.1016/j.jchf.2022.01.003.
Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125(4):620–37. https://doi.org/10.1161/circulationaha.111.023838.
Noseworthy PA, Havulinna AS, Porthan K, Lahtinen AM, Jula A, Karhunen PJ, et al. Common genetic variants, QT interval, and sudden cardiac death in a Finnish population-based study. Circ Cardiovasc Genet. 2011;4(3):305–11. https://doi.org/10.1161/circgenetics.110.959049.
Schunkert H, König IR, Kathiresan S, Reilly MP, Assimes TL, Holm H, et al. Large-scale association analysis identifies 13 new susceptibility loci for coronary artery disease. Nat Genet. 2011;43(4):333–8. https://doi.org/10.1038/ng.784.
Sandhu RK, Dron JS, Liu Y, Moorthy MV, Chatterjee NA, Ellinor PT, et al. Polygenic risk score predicts sudden death in patients with coronary disease and preserved systolic function. J Am Coll Cardiol. 2022;80(9):873–83. https://doi.org/10.1016/j.jacc.2022.05.049.
Albert CM, Nam EG, Rimm EB, Jin HW, Hajjar RJ, Hunter DJ, et al. Cardiac sodium channel gene variants and sudden cardiac death in women. Circulation. 2008;117(1):16–23. https://doi.org/10.1161/circulationaha.107.736330.
Bezzina CR, Pazoki R, Bardai A, Marsman RF, de Jong J, Blom MT, et al. Genome-wide association study identifies a susceptibility locus at 21q21 for ventricular fibrillation in acute myocardial infarction. Nat Genet. 2010;42(8):688–91. https://doi.org/10.1038/ng.623.
Khera AV, Mason-Suares H, Brockman D, Wang M, VanDenburgh MJ, Senol-Cosar O, et al. Rare genetic variants associated with sudden cardiac death in adults. J Am Coll Cardiol. 2019;74(21):2623–34. https://doi.org/10.1016/j.jacc.2019.08.1060.
Trayanova NA, Pashakhanloo F, Wu KC, Halperin HR. Imaging-based simulations for predicting sudden death and guiding ventricular tachycardia ablation. Circ Arrhythm Electrophysiol. 2017;10(7). https://doi.org/10.1161/circep.117.004743.
Arevalo HJ, Vadakkumpadan F, Guallar E, Jebb A, Malamas P, Wu KC, et al. Arrhythmia risk stratification of patients after myocardial infarction using personalized heart models. Nat Commun. 2016;7:11437. https://doi.org/10.1038/ncomms11437.
Rogers AJ, Selvalingam A, Alhusseini MI, Krummen DE, Corrado C, Abuzaid F, et al. Machine learned cellular phenotypes in cardiomyopathy predict sudden death. Circ Res. 2021;128(2):172–84. https://doi.org/10.1161/circresaha.120.317345.
O’Mahony C, Jichi F, Pavlou M, Monserrat L, Anastasakis A, Rapezzi C, et al. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur Heart J. 2014;35(30):2010–20. https://doi.org/10.1093/eurheartj/eht439.
Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022;43(40):3997–4126. https://doi.org/10.1093/eurheartj/ehac262.
Cadrin-Tourigny J, Bosman LP, Nozza A, Wang W, Tadros R, Bhonsale A, et al. A new prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy. Eur Heart J. 2022;43(32):e1–9. https://doi.org/10.1093/eurheartj/ehac180.
Chatterjee NA, Tikkanen JT, Panicker GK, Narula D, Lee DC, Kentta T, et al. Simple electrocardiographic measures improve sudden arrhythmic death prediction in coronary disease. Eur Heart J. 2020. https://doi.org/10.1093/eurheartj/ehaa177.
Chugh SS, Reinier K, Uy-Evanado A, Chugh HS, Elashoff D, Young C, et al. Prediction of sudden cardiac death manifesting with documented ventricular fibrillation or pulseless ventricular tachycardia. JACC Clin Electrophysiol. 2022;8(4):411–23. https://doi.org/10.1016/j.jacep.2022.02.004.
Carrick RT, Te Riele A, Gasperetti A, Bosman L, Muller SA, Pendleton C, et al. Longitudinal prediction of ventricular arrhythmic risk in patients with arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2022;15(11):e011207. https://doi.org/10.1161/circep.122.011207.
•• Barker J, Li X, Khavandi S, Koeckerling D, Mavilakandy A, Pepper C, et al. Machine learning in sudden cardiac death risk prediction: a systematic review. Europace: European pacing, arrhythmias, and cardiac electrophysiology: Journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2022;24(11):1777–87. https://doi.org/10.1093/europace/euac135. Findings from the study summarize the contemporary landscape of machine learning application and limitation for the prediction of sudden cardiac death.
Levy WC, Hellkamp AS, Mark DB, Poole JE, Shadman R, Dardas TF, et al. Improving the use of primary prevention implantable cardioverter-defibrillators therapy with validated patient-centric risk estimates. JACC Clin Electrophysiol. 2018;4(8):1089–102. https://doi.org/10.1016/j.jacep.2018.04.015.
Levy WC, Li Y, Reed SD, Zile MR, Shadman R, Dardas T, et al. Does the implantable cardioverter-defibrillator benefit vary with the estimated proportional risk of sudden death in heart failure patients? JACC Clin Electrophysiol. 2017;3(3):291–8. https://doi.org/10.1016/j.jacep.2016.09.006.
Fukuoka R, Kohno T, Kohsaka S, Shiraishi Y, Sawano M, Abe T, et al. Prediction of sudden cardiac death in Japanese heart failure patients: international validation of the Seattle Proportional Risk Model. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2020;22(4):588–97. https://doi.org/10.1093/europace/euaa002.
Bilchick KC, Wang Y, Cheng A, Curtis JP, Dharmarajan K, Stukenborg GJ, et al. Seattle heart failure and proportional risk models predict benefit from implantable cardioverter-defibrillators. J Am Coll Cardiol. 2017;69(21):2606–18. https://doi.org/10.1016/j.jacc.2017.03.568.
Dagres N, Peek N, Leclercq C, Hindricks G. The PROFID project. Eur Heart J. 2020;41(39):3781–2. https://doi.org/10.1093/eurheartj/ehaa645.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116(12):1887–906. https://doi.org/10.1161/circresaha.116.304521.
Tung R, Zimetbaum P, Josephson ME. A critical appraisal of implantable cardioverter-defibrillator therapy for the prevention of sudden cardiac death. J Am Coll Cardiol. 2008;52(14):1111–21. https://doi.org/10.1016/j.jacc.2008.05.058.
Stecker EC, Vickers C, Waltz J, Socoteanu C, John BT, Mariani R, et al. Population-based analysis of sudden cardiac death with and without left ventricular systolic dysfunction: two-year findings from the Oregon Sudden Unexpected Death Study. J Am Coll Cardiol. 2006;47(6):1161–6. https://doi.org/10.1016/j.jacc.2005.11.045.
Kober L, Thune JJ, Nielsen JC, Haarbo J, Videbaek L, Korup E, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375(13):1221–30. https://doi.org/10.1056/NEJMoa1608029.
Shen L, Jhund PS, Petrie MC, Claggett BL, Barlera S, Cleland JGF, et al. Declining risk of sudden death in heart failure. N Engl J Med. 2017;377(1):41–51. https://doi.org/10.1056/NEJMoa1609758.
Risk stratification and survival after myocardial infarction. N Engl J Med. 1983;309(6):331–6. https://doi.org/10.1056/nejm198308113090602.
Carson PA, O’Connor CM, Miller AB, Anderson S, Belkin R, Neuberg GW, et al. Circadian rhythm and sudden death in heart failure: results from Prospective Randomized Amlodipine Survival Trial. J Am Coll Cardiol. 2000;36(2):541–6. https://doi.org/10.1016/s0735-1097(00)00728-2.
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2018;15(10):e190–252. https://doi.org/10.1016/j.hrthm.2017.10.035.
Chatterjee NA, Moorthy MV, Pester J, Schaecter A, Panicker GK, Narula D, et al. Sudden death in patients with coronary heart disease without severe systolic dysfunction. JAMA Cardiol. 2018;3(7):591–600. https://doi.org/10.1001/jamacardio.2018.1049.
Venkateswaran RV, Moorthy MV, Chatterjee NA, Pester J, Kadish AH, Lee DC, et al. Diabetes and risk of sudden death in coronary artery disease patients without severe systolic dysfunction. JACC Clin Electrophysiol. 2021;7(12):1604–14. https://doi.org/10.1016/j.jacep.2021.05.014.
Junttila MJ, Barthel P, Myerburg RJ, Makikallio TH, Bauer A, Ulm K, et al. Sudden cardiac death after myocardial infarction in patients with type 2 diabetes. Heart Rhythm. 2010;7(10):1396–403. https://doi.org/10.1016/j.hrthm.2010.07.031.
Koene RJ, Norby FL, Maheshwari A, Rooney MR, Soliman EZ, Alonso A, et al. Predictors of sudden cardiac death in atrial fibrillation: The Atherosclerosis Risk in Communities (ARIC) study. PLoS One. 2017;12(11):e0187659. https://doi.org/10.1371/journal.pone.0187659.
Albert CM, Chae CU, Grodstein F, Rose LM, Rexrode KM, Ruskin JN, et al. Prospective study of sudden cardiac death among women in the United States. Circulation. 2003;107(16):2096–101. https://doi.org/10.1161/01.Cir.0000065223.21530.11.
Yao Y, Xue J, Li B. Obesity and sudden cardiac death: Prevalence, pathogenesis, prevention and intervention. Front Cell Dev Biol. 2022;10:1044923. https://doi.org/10.3389/fcell.2022.1044923.
Chen LY, Sotoodehnia N, Bůžková P, Lopez FL, Yee LM, Heckbert SR, et al. Atrial fibrillation and the risk of sudden cardiac death: the atherosclerosis risk in communities study and cardiovascular health study. JAMA Intern Med. 2013;173(1):29–35. https://doi.org/10.1001/2013.jamainternmed.744.
van der Burgh AC, Stricker BH, Rizopoulos D, Ikram MA, Hoorn EJ, Chaker L. Kidney function and the risk of sudden cardiac death in the general population. Clin Kidney J. 2022;15(8):1524–33. https://doi.org/10.1093/ckj/sfac049.
Jouven X, Desnos M, Guerot C, Ducimetiere P. Predicting sudden death in the population: the Paris Prospective Study I. Circulation. 1999;99(15):1978–83.
Sandhu RK, Jimenez MC, Chiuve SE, Fitzgerald KC, Kenfield SA, Tedrow UB, et al. Smoking, smoking cessation, and risk of sudden cardiac death in women. Circ Arrhythm Electrophysiol. 2012;5(6):1091–7. https://doi.org/10.1161/circep.112.975219.
Tu SJ, Gallagher C, Elliott AD, Linz D, Pitman BM, Hendriks JML, et al. Alcohol consumption and risk of ventricular arrhythmias and sudden cardiac death: an observational study of 408,712 individuals. Heart Rhythm. 2022;19(2):177–84. https://doi.org/10.1016/j.hrthm.2021.09.040.
Albert CM, Manson JE, Cook NR, Ajani UA, Gaziano JM, Hennekens CH. Moderate alcohol consumption and the risk of sudden cardiac death among US male physicians. Circulation. 1999;100(9):944–50. https://doi.org/10.1161/01.cir.100.9.944.
Whang W, Manson JE, Hu FB, Chae CU, Rexrode KM, Willett WC, et al. Physical exertion, exercise, and sudden cardiac death in women. JAMA. 2006;295(12):1399–403. https://doi.org/10.1001/jama.295.12.1399.
Albert CM, Mittleman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343(19):1355–61. https://doi.org/10.1056/nejm200011093431902.
Chatterjee NA, Tikkanen JT, Panicker GK, Narula D, Lee DC, Kentta T, et al. Simple electrocardiographic measures improve sudden arrhythmic death prediction in coronary disease. Eur Heart J. 2020;41(21):1988–99. https://doi.org/10.1093/eurheartj/ehaa177.
Deyell MW, Krahn AD, Goldberger JJ. Sudden cardiac death risk stratification. Circ Res. 2015;116(12):1907–18. https://doi.org/10.1161/circresaha.116.304493.
Loring Z, Zareba W, McNitt S, Strauss DG, Wagner GS, Daubert JP. ECG quantification of myocardial scar and risk stratification in MADIT-II. Annals of noninvasive electrocardiology: the official Journal of the International Society for Holter and Noninvasive Electrocardiology, Inc. 2013;18(5):427–35. https://doi.org/10.1111/anec.12065.
Magnani JW, Gorodeski EZ, Johnson VM, Sullivan LM, Hamburg NM, Benjamin EJ, et al. P wave duration is associated with cardiovascular and all-cause mortality outcomes: the National Health and Nutrition Examination Survey. Heart Rhythm. 2011;8(1):93–100. https://doi.org/10.1016/j.hrthm.2010.09.020.
Narayanan K, Reinier K, Teodorescu C, Uy-Evanado A, Chugh H, Gunson K, et al. Electrocardiographic versus echocardiographic left ventricular hypertrophy and sudden cardiac arrest in the community. Heart Rhythm. 2014;11(6):1040–6. https://doi.org/10.1016/j.hrthm.2014.03.023.
Strauss DG, Selvester RH, Lima JA, Arheden H, Miller JM, Gerstenblith G, et al. ECG quantification of myocardial scar in cardiomyopathy patients with or without conduction defects: correlation with cardiac magnetic resonance and arrhythmogenesis. Circ Arrhythm Electrophysiol. 2008;1(5):327–36. https://doi.org/10.1161/circep.108.798660.
Soliman EZ, Elsalam MA, Li Y. The relationship between high resting heart rate and ventricular arrhythmogenesis in patients referred to ambulatory 24 h electrocardiographic recording. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2010;12(2):261–5. https://doi.org/10.1093/europace/eup344.
Teodorescu C, Reinier K, Uy-Evanado A, Gunson K, Jui J, Chugh SS. Resting heart rate and risk of sudden cardiac death in the general population: influence of left ventricular systolic dysfunction and heart rate-modulating drugs. Heart Rhythm. 2013;10(8):1153–8. https://doi.org/10.1016/j.hrthm.2013.05.009.
Aro AL, Anttonen O, Tikkanen JT, Junttila MJ, Kerola T, Rissanen HA, et al. Intraventricular conduction delay in a standard 12-lead electrocardiogram as a predictor of mortality in the general population. Circ Arrhythm Electrophysiol. 2011;4(5):704–10. https://doi.org/10.1161/circep.111.963561.
Desai AD, Yaw TS, Yamazaki T, Kaykha A, Chun S, Froelicher VF. Prognostic significance of quantitative QRS duration. Am J Med. 2006;119(7):600–6. https://doi.org/10.1016/j.amjmed.2005.08.028.
Rosengarten JA, Scott PA, Morgan JM. Fragmented QRS for the prediction of sudden cardiac death: a meta-analysis. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2015;17(6):969–77. https://doi.org/10.1093/europace/euu279.
Torigoe K, Tamura A, Kawano Y, Shinozaki K, Kotoku M, Kadota J. The number of leads with fragmented QRS is independently associated with cardiac death or hospitalization for heart failure in patients with prior myocardial infarction. J Cardiol. 2012;59(1):36–41. https://doi.org/10.1016/j.jjcc.2011.09.003.
Zimetbaum PJ, Buxton AE, Batsford W, Fisher JD, Hafley GE, Lee KL, et al. Electrocardiographic predictors of arrhythmic death and total mortality in the multicenter unsustained tachycardia trial. Circulation. 2004;110(7):766–9. https://doi.org/10.1161/01.cir.0000139311.32278.32.
Crow RS, Hannan PJ, Folsom AR. Prognostic significance of corrected QT and corrected JT interval for incident coronary heart disease in a general population sample stratified by presence or absence of wide QRS complex: the ARIC Study with 13 years of follow-up. Circulation. 2003;108(16):1985–9. https://doi.org/10.1161/01.cir.0000095027.28753.9d.
Porthan K, Viitasalo M, Toivonen L, Havulinna AS, Jula A, Tikkanen JT, et al. Predictive value of electrocardiographic T-wave morphology parameters and T-wave peak to T-wave end interval for sudden cardiac death in the general population. Circ Arrhythm Electrophysiol. 2013;6(4):690–6. https://doi.org/10.1161/circep.113.000356.
Soliman EZ, Shah AJ, Boerkircher A, Li Y, Rautaharju PM. Inter-relationship between electrocardiographic left ventricular hypertrophy and QT prolongation as predictors of increased risk of mortality in the general population. Circ Arrhythm Electrophysiol. 2014;7(3):400–6. https://doi.org/10.1161/circep.113.001396.
Teodorescu C, Reinier K, Uy-Evanado A, Navarro J, Mariani R, Gunson K, et al. Prolonged QRS duration on the resting ECG is associated with sudden death risk in coronary disease, independent of prolonged ventricular repolarization. Heart Rhythm. 2011;8(10):1562–7. https://doi.org/10.1016/j.hrthm.2011.06.011.
Savard P, Rouleau JL, Ferguson J, Poitras N, Morel P, Davies RF, et al. Risk stratification after myocardial infarction using signal-averaged electrocardiographic criteria adjusted for sex, age, and myocardial infarction location. Circulation. 1997;96(1):202–13. https://doi.org/10.1161/01.cir.96.1.202.
Goldberger JJ, Subacius H, Patel T, Cunnane R, Kadish AH. Sudden cardiac death risk stratification in patients with nonischemic dilated cardiomyopathy. J Am Coll Cardiol. 2014;63(18):1879–89. https://doi.org/10.1016/j.jacc.2013.12.021.
Yamazaki T, Froelicher VF, Myers J, Chun S, Wang P. Spatial QRS-T angle predicts cardiac death in a clinical population. Heart Rhythm. 2005;2(1):73–8. https://doi.org/10.1016/j.hrthm.2004.10.040.
Kors JA, Kardys I, van der Meer IM, van Herpen G, Hofman A, van der Kuip DA, et al. Spatial QRS-T angle as a risk indicator of cardiac death in an elderly population. J Electrocardiol. 2003;36(Suppl):113–4. https://doi.org/10.1016/j.jelectrocard.2003.09.033.
Giovanardi P, Vernia C, Tincani E, Giberti C, Silipo F, Fabbo A. Combined effects of age and comorbidities on electrocardiographic parameters in a large non-selected population. J Clin Med. 2022;11(13). https://doi.org/10.3390/jcm11133737.
You T, Luo C, Zhang K, Zhang H. Electrophysiological Mechanisms Underlying T-Wave Alternans and their role in arrhythmogenesis. Front Physiol. 2021;12:614946. https://doi.org/10.3389/fphys.2021.614946.
Exner DV, Kavanagh KM, Slawnych MP, Mitchell LB, Ramadan D, Aggarwal SG, et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol. 2007;50(24):2275–84. https://doi.org/10.1016/j.jacc.2007.08.042.
Bauer A, Barthel P, Schneider R, Ulm K, Müller A, Joeinig A, et al. Improved Stratification of Autonomic Regulation for risk prediction in post-infarction patients with preserved left ventricular function (ISAR-Risk). Eur Heart J. 2009;30(5):576–83. https://doi.org/10.1093/eurheartj/ehn540.
Mäkikallio TH, Barthel P, Schneider R, Bauer A, Tapanainen JM, Tulppo MP, et al. Prediction of sudden cardiac death after acute myocardial infarction: role of Holter monitoring in the modern treatment era. Eur Heart J. 2005;26(8):762–9. https://doi.org/10.1093/eurheartj/ehi188.
Alexandre J, Saloux E, Dugué AE, Lebon A, Lemaitre A, Roule V, et al. Scar extent evaluated by late gadolinium enhancement CMR: a powerful predictor of long term appropriate ICD therapy in patients with coronary artery disease. J Cardiovasc Magn Reson: Offic J Soc Cardiovasc Magn Reson. 2013;15(1):12. https://doi.org/10.1186/1532-429x-15-12.
Scott PA, Morgan JM, Carroll N, Murday DC, Roberts PR, Peebles CR, et al. The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators. Circ Arrhythm Electrophysiol. 2011;4(3):324–30. https://doi.org/10.1161/circep.110.959544.
Assomull RG, Prasad SK, Lyne J, Smith G, Burman ED, Khan M, et al. Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol. 2006;48(10):1977–85. https://doi.org/10.1016/j.jacc.2006.07.049.
Masci PG, Doulaptsis C, Bertella E, Del Torto A, Symons R, Pontone G, et al. Incremental prognostic value of myocardial fibrosis in patients with non-ischemic cardiomyopathy without congestive heart failure. Circ Heart Fail. 2014;7(3):448–56. https://doi.org/10.1161/circheartfailure.113.000996.
Piers SR, Everaerts K, van der Geest RJ, Hazebroek MR, Siebelink HM, Pison LA, et al. Myocardial scar predicts monomorphic ventricular tachycardia but not polymorphic ventricular tachycardia or ventricular fibrillation in nonischemic dilated cardiomyopathy. Heart Rhythm. 2015;12(10):2106–14. https://doi.org/10.1016/j.hrthm.2015.05.026.
Jablonowski R, Chaudhry U, van der Pals J, Engblom H, Arheden H, Heiberg E, et al. Cardiovascular magnetic resonance to predict appropriate implantable cardioverter defibrillator therapy in ischemic and nonischemic cardiomyopathy patients using late gadolinium enhancement border zone: comparison of four analysis methods. Circ Cardiovasc Imaging. 2017;10(9). https://doi.org/10.1161/circimaging.116.006105.
Zeidan-Shwiri T, Yang Y, Lashevsky I, Kadmon E, Kagal D, Dick A, et al. Magnetic resonance estimates of the extent and heterogeneity of scar tissue in ICD patients with ischemic cardiomyopathy predict ventricular arrhythmia. Heart Rhythm. 2015;12(4):802–8. https://doi.org/10.1016/j.hrthm.2015.01.007.
Androulakis AFA, Zeppenfeld K, Paiman EHM, Piers SRD, Wijnmaalen AP, Siebelink HJ, et al. Entropy as a novel measure of myocardial tissue heterogeneity for prediction of ventricular arrhythmias and mortality in post-infarct patients. JACC Clin Electrophysiol. 2019;5(4):480–9. https://doi.org/10.1016/j.jacep.2018.12.005.
Muser D, Nucifora G, Muser D, Nucifora G, Pieroni M, Castro SA, et al. Prognostic value of nonischemic ringlike left ventricular scar in patients with apparently idiopathic nonsustained ventricular arrhythmias. Circulation. 2021;143(14):1359–73. https://doi.org/10.1161/circulationaha.120.047640.
Gräni C, Eichhorn C, Bière L, Murthy VL, Agarwal V, Kaneko K, et al. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J Am Coll Cardiol. 2017;70(16):1964–76. https://doi.org/10.1016/j.jacc.2017.08.050.
Aquaro GD, Perfetti M, Camastra G, Monti L, Dellegrottaglie S, Moro C, et al. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY study. J Am Coll Cardiol. 2017;70(16):1977–87. https://doi.org/10.1016/j.jacc.2017.08.044.
Hulten E, Agarwal V, Cahill M, Cole G, Vita T, Parrish S, et al. Presence of late gadolinium enhancement by cardiac magnetic resonance among patients with suspected cardiac sarcoidosis is associated with adverse cardiovascular prognosis: a systematic review and meta-analysis. Circ Cardiovasc Imaging. 2016;9(9):e005001. https://doi.org/10.1161/circimaging.116.005001.
Briasoulis A, Mallikethi-Reddy S, Palla M, Alesh I, Afonso L. Myocardial fibrosis on cardiac magnetic resonance and cardiac outcomes in hypertrophic cardiomyopathy: a meta-analysis. Heart (British Cardiac Society). 2015;101(17):1406–11. https://doi.org/10.1136/heartjnl-2015-307682.
Ashrith G, Gupta D, Hanmer J, Weiss RM. Cardiovascular magnetic resonance characterization of left ventricular non-compaction provides independent prognostic information in patients with incident heart failure or suspected cardiomyopathy. J Cardiovasc Magn Reson: Offic J Soc Cardiovasc Magn Reson. 2014;16(1):64. https://doi.org/10.1186/s12968-014-0064-2.
Jain A, Tandri H, Calkins H, Bluemke DA. Role of cardiovascular magnetic resonance imaging in arrhythmogenic right ventricular dysplasia. J Cardiovasc Magn Reson: Offic J Soc Cardiovasc Magn Reson. 2008;10(1):32. https://doi.org/10.1186/1532-429x-10-32.
Mentias A, Raeisi-Giglou P, Smedira NG, Feng K, Sato K, Wazni O, et al. Late gadolinium enhancement in patients with hypertrophic cardiomyopathy and preserved systolic function. J Am Coll Cardiol. 2018;72(8):857–70. https://doi.org/10.1016/j.jacc.2018.05.060.
Todiere G, Nugara C, Gentile G, Negri F, Bianco F, Falletta C, et al. Prognostic role of late gadolinium enhancement in patients with hypertrophic cardiomyopathy and low-to-intermediate sudden cardiac death risk score. Am J Cardiol. 2019;124(8):1286–92. https://doi.org/10.1016/j.amjcard.2019.07.023.
• Xu L, Khoshknab M, Berger RD, Chrispin J, Dixit S, Santangeli P, et al. Lipomatous metaplasia enables ventricular tachycardia by reducing current loss within the protected corridor. JACC Clin Electrophysiol. 2022;8(10):1274–85. https://doi.org/10.1016/j.jacep.2022.07.005. The findings of the study demonstrate the novel role of cardiac imaging and lipomatous metaplasia in the pathogenesis of ventricular arrhythmias.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no competing interests.
Human and Animal Rights and Informed Consent.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chatterjee, N.A. Prediction of Sudden Cardiac Death: Looking Beyond Ejection Fraction. Curr Cardiol Rep 25, 525–534 (2023). https://doi.org/10.1007/s11886-023-01871-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01871-0