Abstract
Purpose of Review
Electrical storm (ES) is a life-threatening medical emergency of repetitive episodes of sustained ventricular arrhythmias within a short period. Its occurrence is associated with poor short- and long-term survival, even in patients with implantable cardioverter defibrillators (ICD). Management of ES is challenging and mainly based on retrospective studies. This article reviews the existing literature on ES, presents the available data regarding its management, and proposes a new algorithm based on current evidence.
Recent Findings
Recent research could modify the management of ES supporting the role of non-selective β1 and β2 blockade and the early intervention with catheter ablation as well as strengthening the role of cardiac sympathetic denervation.
Summary
A multipronged approach should be considered for the management of ES including identification and correction of reversible causes, ICD reprogramming, drug therapy (beta-blockers—especially non-selective ones—and other anti-arrhythmic drugs) and non-pharmacologic therapies such as catheter ablation and techniques of neuroaxial modulation. Although current data suggest early aggressive management, further research is required to clarify the optimal order and combination of therapies for the prevention of future events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Electrical storm (ES) is most commonly defined as the occurrence of three or more repetitive episodes of sustained ventricular arrhythmias (VA) within a 24-h period. This extends to patients equipped with an implantable cardioverter defibrillator (ICD), in whom ES is best defined as 3 appropriate detections of VA in a 24-h period leading to ICD therapies [anti-tachycardia pacing (ATP) or shock] or eventually untreated but sustained ventricular tachycardia (VT) in a monitoring zone [1].
While ICD implantation reduces the rate of sudden arrhythmic death in patients with cardiomyopathies and inherited primary arrhythmia syndromes [2], the occurrence of ES is associated with poor short- and long-term prognosis even in ICD carriers. Approximately 4–7% of patients implanted for primary prevention and 10–58% of those implanted for secondary prevention will experience an episode of ES at some point after implant [3, 4].
Management of ES is challenging and mainly based on retrospective studies. This article reviews the existing literature on this topic, presents the available strategies, and provides a proposed algorithm based on current evidence (Fig. 1).
Initial Assessment and Care
The electrocardiographic differential diagnosis of wide-QRS regular tachycardias is often challenging [5]. Several algorithms based on QRS morphology exist to help in the diagnosis, which should also take into account the clinical context—namely the presence of underlying heart disease and the hemodynamic state. In case of hemodynamically unstable wide-QRS tachycardia, electrical cardioversion is the treatment of choice and should be performed immediately [2, 6]; on the other hand, if the patient is hemodynamically stable, either pharmacologic or electrical cardioversion can be appropriate.
Identification and, if possible, correction of factors predisposing to ventricular arrhythmogenesis are mandatory elements of clinical management [7]. Ischemia and hypoxia, electrolyte disturbances (such as hypokalemia, which is especially common in heart failure) [8], cardiac decompensation, and proarrhythmic drugs all modulate the electrophysiological properties of the myocardium. Even though these factors are related mainly to triggered arrhythmias, they may be involved in initiating and perpetuating ES [7, 9]. Up to 6% of patients with acute coronary syndromes present with VT, usually polymorphic, or ventricular fibrillation (VF) within the first 48 h after symptom onset [2].
ICD Programming
In ICD carriers, device interrogation to confirm that ICD therapies are appropriate should be performed first, as inappropriate shocks remain frequent despite fairly accurate discrimination criteria [10, 11]; up to 22% of the total amount of shocks were inappropriate in a retrospective analysis with a long follow-up period [11]. The most frequent cause of inappropriate ICD therapies was atrial fibrillation with fast ventricular response, but other supraventricular arrhythmias, oversensing of T waves (in some cases due to lead defect), and even sinus tachycardia may also be responsible.
However, the occurrence of both appropriate and inappropriate ICD therapies increases the risk for ES [12]. Myocardial injury as a direct effect of intracardiac defibrillation has been extensively investigated, and there is general agreement that unnecessary ICD discharges should be avoided [13, 14]. Reentrant VT can be terminated by overdrive, and there is no evidence that ATP has adverse cardiac effects.
In the ADVANCE III trial, programming a long detection interval (30 of 40 ventricular intervals) rather than a standard detection interval (18 of 24) effectively reduced total ICD therapies (ATP and shocks), as well as inappropriate shocks and hospitalizations. The incidence of syncope was low and did not significantly differ between the two programming options. Long detection was combined with ATP during charging, resulting in delayed arrhythmia detection without excessively delaying therapy (shock expected to be delivered within 17 to 21 s of arrhythmia detection), if still needed [15]. In the PainFREE Rx II Trial, ATP was demonstrated to be highly effective and equally safe compared with shocks, even for fast VTs of a cycle length between 240 and 320 ms. The use of ICDs capable of programming a fast VT detection zone defined within the VF zone is necessary in this case [16].
Beta-Blockers
Given the influences of the autonomic nervous system in cardiovascular properties involved in genesis and maintenance of VAs, it is no surprise that sympathetic blockade is a cornerstone in the management of ES [17, 18]. The anti-arrhythmic effects of beta-blockers are explained by adrenergic-receptor blockade on sympathetically mediated triggered mechanisms, slowing of the sinus rate, and possibly inhibition of excess calcium release by the ryanodine receptor [6].
In dogs, several beta-blocking drugs caused substantial (average 6-fold) increases in the VF threshold under both non-ischemic and ischemic conditions [19]. Despite the absence of placebo-controlled studies of beta-blockers in ICD carriers, current evidence supports their use. In the MADIT II study, high doses of beta-blockers (metoprolol, atenolol or carvedilol) reduced the risk for VT or VF in ICD-treated patients with ischemic cardiomyopathy (hazard ratio 0.48, p = 0.02) [20].
Sympathetic blockade by administration of beta-blockers and left stellate ganglion blockade (SGB) was superior to anti-arrhythmic drugs (AADs) in a study of forty-nine patients who experienced ES associated with a recent myocardial infarction [21]. A lower 1-week mortality (22% vs 82%, p < 0.0001) and a higher survival over a 1-year follow-up period (67% vs 5%, p < 0.0001) were observed in the group of sympathetic blockade.
Importantly, the use of non-selective beta-blockers (antagonizing both β1 and β2 receptors) may offer a superior antiarrhythmic effect. Chatzidou et al. recently reported that oral propranolol was superior to oral metoprolol in controlling ES in ICD patients receiving intravenous (IV) amiodarone. Incidence rate of VAs and ICD discharges was decreased by more than two times during the intensive care unit stay in patients receiving propranolol, compared to metoprolol [22••].
In the setting of cardiac arrest from VF or pulseless VT, current guidelines of resuscitation recommend epinephrine administration. Although prospective trials of AADs with beta-blocking properties, case series, and experimental animal studies suggest that beta-blockers during VF may increase rates of successful resuscitation and improve outcome, preliminary human studies are lacking [23]. Beta-blockers are also the medical treatment of choice for certain channelopathies (e.g., congenital long QT-syndrome type 1 and catecholaminergic polymorphic VT).
Antiarrhythmic Drugs
Amiodarone
Although originally classified as a class III AAD, amiodarone displays a wide spectrum of actions. Being a multichannel blocker (including sodium, calcium potassium channels, and beta-adrenoreceptors), it is the most effective treatment to reduce ICD discharges [24]. It is also often preferred in patients with structural heart disease, in whom class IC antiarrhythmics are relatively contraindicated.
Intravenous amiodarone use is associated with noticeable antiarrhythmic response in at least 40% of patients with recurrent sustained VAs refractory to other AADs [25]. It is relatively safe for short-term administration, and loading may still be effective even in patients already on chronic oral amiodarone therapy, shortening the time to optimal VA control [26].
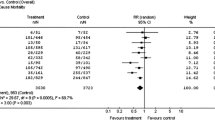
Long-term oral amiodarone can be used to prevent the recurrence of life-threatening VAs, but its usefulness should be weighed against potential drug toxicity. The OPTIC trial showed that in patients implanted with an ICD for the secondary prevention of life-threatening VAs, a combined drug regimen consisting of amiodarone and a beta-blocker significantly reduced the risk of shocks compared to beta-blocker alone (HR 0.27, 95% CI 0.14–0.52, P < .001) and sotalol (HR 0.43, 95% CI 0.22–0.85, P = .02) [27]. Despite this, the mortality rate was not significantly different between treatments. Pulmonary and thyroid toxicity as well as symptomatic bradycardia were more common among patients randomized to amiodarone and led to drug discontinuation in 18.2% of patients. In a meta-analysis of randomized control trials, Santangeli et al. found a significant reduction in appropriate ICD interventions with AADs (OR 0.66, 95% CI 0.44–0.97, P = .037). However, the significant reduction of recurrent VT episodes was not associated with a mortality benefit, with a potential for increased mortality with amiodarone [28••]. The SCD-HeFT trial demonstrated the substantial role of ICD in patients with heart failure with reduced ejection fraction; on the contrary, amiodarone was associated with a similar risk of death as placebo [29].
Due to safety concerns, chronic amiodarone treatment should be ideally reserved as a bridge to more definitive treatment options such as catheter ablation, while periodic evaluation for drug toxicity is mandatory [6]. Importantly, chronic amiodarone therapy has also been associated with an increase in the defibrillation threshold and thus, ICD testing should be considered [30].
Other Antiarrhythmic Drugs
In the case of amiodarone failure, other drugs may be considered. Procainamide blocks fast sodium channels (class Ia antiarrhythmic agent). Its negative inotropic actions raised concerns about the use in patients with depressed systolic function, as procainamide can cause hypotension [31]. Moreover, prolongation of the width of the QRS complex by more than 50% necessitates discontinuation of the drug. On the other hand, administration of procainamide for acute VT termination is supported by recent evidence. In the PROCAMIO study, IV procainamide was compared to IV amiodarone for the acute therapy of tolerated wide-QRS tachycardia, presumably VT [32]. Procainamide was more effective at terminating tachycardia and was associated with fewer major adverse events, such as severe hypotension requiring electrical cardioversion. Importantly, these findings equally applied to patients with structural heart disease. Current guidelines recommend IV procainamide and amiodarone as drugs of choice for the treatment of hemodynamically stable VT in patients with structural heart disease [2, 6]. However, evidence for prevention of recurrent VAs, as in the setting of ES, is limited.
Intravenous lidocaine is only moderately effective in patients presenting with monomorphic scar-related VT. However, its administration may be useful during acute ischemia complicated by VAs as the altered membrane potential and pH reduction increase the drug-binding rate [2, 6, 7].
Sotalol has been demonstrated to reduce ICD shocks but has not been shown to be superior to amiodarone or beta-blockers for preventing VAs [27, 33, 34]. Moreover, administration of d-sotalol, the isomer that acts on potassium channels, has been associated with increased mortality in patients with left ventricular dysfunction, which was presumed to be due primarily to arrhythmias [35].
Several combinations of AADs have also been investigated. In the VANISH trial, mexiletine had limited efficacy in the treatment of recurrent VT despite high-dose amiodarone therapy [36]. The combination of low-dose sotalol and a class Ia agent has also been shown to greatly prolong refractoriness [37] but has not been tested in randomized controlled trials. When combining AADs, even greater consideration should be given to the risk of proarrhythmic effects. Moreover, increase of defibrillation threshold and prolongation of VT cycle length may have an impact on ICD shock efficacy and arrhythmia detection, respectively [38].
Sedation
Anesthetic agents as propofol have been associated with suppression of VAs. Abolishing sympathetically mediated tone may explain this action, as sympathetic activation has been implicated in the genesis of ES [39]. Sedation is also important to reduce distress in patients with ES and multiple ICD shocks.
Catheter Ablation
Electrical storm that remains refractory to AADs presents a major clinical challenge. Current guidelines recommend the use of catheter ablation in the case of recurrent VAs despite optimal antiarrhythmic therapy [2, 6]. Moreover, ICD-unresponsive sudden cardiac death still occurs frequently in ICD recipients, indicating the importance of strategies to reduce arrhythmic burden [40, 41].
The majority of sustained monomorphic VTs arise from a ventricular scar, most commonly caused by a previous myocardial infarction. The usual mechanism of post-infarct VTs is reentry, facilitated by areas of unidirectional block due to slow and inhomogeneous conduction through surviving myocytes within the scar. This region of slow conduction is usually an anatomically or functionally circumscribed narrow isthmus that often becomes a main target for ablation [42].
Ablation for VT has been proved effective and safe, its use for post-infarct VT having increased steadily over the past decade [43, 44]. In a meta-analysis of 39 publications that included 471 patients with ES, 72% of all VAs were successfully ablated. Procedure-related mortality was relatively low (0.6%), and only 6% of patients presented with a recurrent ES [45]. Limitations surround unmappable VT morphologies where non-inducibility and non-tolerability frequently cause problems related to efficacy and safety, respectively. Additionally, multiple reentry circuits can be present in a single patient [42]. However, “scar homogenization” substrate ablation approach has also been shown to be effective [46]. Moreover, intra-aortic balloon pump and percutaneous mechanical circulatory support devices facilitate mapping and ablation of non-tolerated VAs and are increasingly utilized in selected occasions [43].
Catheter ablation has been demonstrated to improve outcome compared to medical therapy alone. In the VANISH trial, there was a significantly lower rate of the composite primary outcome of death, ES, or appropriate ICD shock among patients who underwent ablation compared to escalation in AAD therapy (59.1% vs 68.5%, p = 0.004) [47]. In a meta-analysis by Santangeli et al., both amiodarone and ablation reduced the risk of recurrent VT compared to control medical therapy, with no significant difference between the two treatments [28••]. However, amiodarone appeared to increase the risk of death. Of note, the above-mentioned studies failed to show a mortality benefit with ablation.
The optimal timing of ablation in patients at risk of ventricular arrhythmias is unknown. Although catheter ablation was usually performed as a treatment of last resort, early intervention is supported by current evidence. In the SMASH-VT randomized study, prophylactic substrate-based catheter ablation reduced the incidence of ICD therapy in patients with a history of myocardial infarction who received ICDs for the secondary prevention of sudden death compared to patients who were assigned to defibrillator implantation alone (12% vs. 33%) [48]. In the VTACH trial, prophylactic VT ablation before ICD implantation prolonged time to recurrence of VT from 5.9 to 18.6 months in patients with stable VT, previous myocardial infarction, and reduced ejection fraction [49].
Scar-related VTs can also occur in other structural diseases, such as dilated cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy (ARVC), sarcoidosis, Chagas’ disease, or after surgical ventricular incisions (for example after repair of tetralogy of Fallot). The distribution of abnormal substrate in non-ischemic cardiomyopathy presents a higher likelihood of epicardial and intramural involvement and long-term outcome after catheter ablation depends on the underlying cause [50]. Catheter ablation can also be performed for polymorphic VTs in patients without structural heart disease [2, 51].
Denervation and Surgical Treatment
Neuroaxial modulation plays a critical role in the therapeutic management of ES, particularly in cases of long QT syndrome and catecholaminergic ventricular tachyarrhythmias. Nevertheless, limited data support the use of cardiac sympathetic denervation (CSD) as an option in a wider range of ES cases, refractory to medication, and/or ablation treatments [52, 53]. Vaseghi et al. demonstrated in a retrospective study of 121 patients with refractory VAs and structural heart disease that left or bilateral CSD treatment resulted in a 1-year freedom from sustained VT and ICD shock of 58.2% and 50.4%, respectively. Moreover, out of 120 patients on AAD treatment prior to CSD, 39 (32%) were eligible to discontinue oral AADs at follow-up [54•].
Thoracic epidural anesthesia (TEA) has also been proposed to help relieve ES. Bradfield et al. displayed its efficacy in a multi-center study of 11 patients with ES. Five patients responded completely and 1 responded partially, while a sedation response was associated with a probable clinical favorable response to TEA [55]. Bourke et al. showed similar favorable clinical results when left CSD and/or TEA where included in the therapeutic management of patients with VT, refractory to medical treatment and ablation [56].
Stellate ganglion blockade has been suggested as another feasible approach in cases of refractory ES, when performed by experienced operators. A recent review and meta-analysis by Fudim et al. demonstrated the clinical efficacy of unilateral and bilateral SGB in patients with a high VA burden: SGB resulted in a significant decrease in VT episodes and the need for defibrillation. Moreover, SGB correlated with a reduction in VAs regardless of cause for contractile dysfunction, ventricular arrhythmia, and cardiomyopathy [57].
Renal denervation (RDN) could also hold promise in selected cases, but data is extremely limited. Remo et al. recently reported favorable clinical results while performing RDN in 4 patients (2 ischemic, 2 non-ischemic) with cardiomyopathy and frequent VT episodes refractory to all other therapeutic interventions (medication, ablation, cardiac resynchronization). A reduction in VT episodes was recorded from 11 ± 4.2 (5.0–14.0) over the month before RDN, to 0.3 ± 0.1 (0.2–0.4) in the month following treatment [58].
Not Scar-Related Polymorphic VT/Electrical Storm
In contrast to substrate-related monomorphic VTs, polymorphic VTs are most often attributable to myocardial ischemia, inherited primary arrhythmia syndromes, and acquired long QT syndrome. Electrical storm in patients with Brugada or early repolarization syndrome can be managed acutely with IV isoproterenol and oral quinidine [59]. In patients with repeated ICD shocks, oral quinidine and cilostazol are the treatment of choice. Class Ia and Ic AADs are contraindicated because of their effects of unmasking J wave syndromes and inducing arrhythmogenesis due to their Na+ channel blockade. In selected patients with drug-refractory ES presenting with polymorphic VTs, catheter ablation targeting premature ventricular beat triggers can be attempted [2, 51].
Intravenous magnesium administration is the initial approach for polymorphic VT due to a long QT interval [2, 6]. In the case of bradycardia, isoproterenol therapy or temporary pacing eliminates bursts of VAs associated with pause-dependent triggered activity by reducing the duration of the action potential. Exclusion of acquired causes is also mandatory in the context of polymorphic VT and a long QT interval. Beta-blockers are recommended in all patients with long QT syndrome, while left CSD should be considered in patients with multiple ICD shocks, as previously was discussed [2].
Flecainide should be considered in addition to beta-blockers in patients with catecholaminergic polymorphic VT who experience recurrent polymorphic or bidirectional VT [2]. Left CSD may also be considered.
Conclusion
Electrical storm is a life-threatening medical emergency with poor prognosis. Management requires a multipronged approach including identification and correction of reversible triggers, device programming, drug therapy (beta-blockers—especially non-selective ones—and other AADs) and non-pharmacologic therapies such as catheter ablation and neuroaxial modulation. Whether amore interventional approach should be taken simultaneously to pharmacological treatment or only in drug-refractory cases is not well-clarified. Although current data suggest early aggressive management, further research is warranted to establish the role of the available strategies for prevention of future events.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Israel CW, Barold SS. Electrical storm in patients with an implanted defibrillator: a matter of definition. Ann Noninvasive Electrocardiol. 2007 Oct;12(4):375–82. https://doi.org/10.1111/j.1542-474X.2007.00187.x.
Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36(41):2793–867. https://doi.org/10.1093/eurheartj/ehv316.
Guerra F, Palmisano P, Dell'Era G, Ziacchi M, Ammendola E, Pongetti G, et al. Cardiac resynchronization therapy and electrical storm: results of the OBSERVational registry on long-term outcome of ICD patients (OBSERVO-ICD). Europace. 2018;20(6):979–85. https://doi.org/10.1093/europace/eux166.
Nedios S, Darma A, Stevanello C, Richter S, Doering M, Rolf S, et al. Electrical storm in patients with implantable cardioverter-defibrillator in the era of catheter ablation: implications for better rhythm control. Heart Rhythm. 2015;12(12):2419–25. https://doi.org/10.1016/j.hrthm.2015.07.034.
Katritsis DG, Boriani G, Cosio FG, Hindricks G, Jaïs P, Josephson ME, et al. European Heart Rhythm Association (EHRA) consensus document on the management of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and SociedadLatinoamericana de EstimulaciónCardiaca y Electrofisiologia (SOLAECE). Europace. 2017;19(3):465–511. https://doi.org/10.1093/europace/euw301.
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients with Ventricular Arrhythmias and the prevention of sudden cardiac death: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am CollCardiol. 2018;72(14):1677–749. https://doi.org/10.1016/j.jacc.2017.10.053.
Muser D, Santangeli P, Liang JJ. Management of ventricular tachycardia storm in patients with structural heart disease. World J Cardiol. 2017;9(6):521–30. https://doi.org/10.4330/wjc.v9.i6.521.
Skogestad J, Aronsen JM. Hypokalemia-induced arrhythmias and heart failure: new insights and implications for therapy. Front Physiol. 2018;9:1500. https://doi.org/10.3389/fphys.2018.01500.
Saliba WI, Natale A. Ventricular tachycardia syndromes. Med Clin N Am. 2001;85:267–304. https://doi.org/10.1016/S0025-7125(05)70316-3.
van Rees JB, Borleffs CJ, de Bie MK, Stijnen T, van Erven L, Bax JJ, et al. Inappropriate implantable cardioverter-defibrillator shocks: incidence, predictors, and impact on mortality. J Am CollCardiol. 2011;57(5):556–62. https://doi.org/10.1016/j.jacc.2010.06.059.
Hofer D, Steffel J, Hürlimann D, Haegeli L, Lüscher TF, Duru F, et al. Long-term incidence of inappropriate shocks in patients with implantable cardioverter defibrillators in clinical practice-an underestimated complication? J Interv Card Electrophysiol. 2017;50(3):219–26. https://doi.org/10.1007/s10840-017-0297-8.
Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359(10):1009–17. https://doi.org/10.1056/NEJMoa071098.
Brewster J, Sexton T, Dhaliwal G, Charnigo R, Morales G, Parrott K, et al. Acute effects of implantable cardioverter-defibrillator shocks on biomarkers of myocardial injury, apoptosis, heart failure, and systemic inflammation. Pacing ClinElectrophysiol. 2017;40(4):344–52. https://doi.org/10.1111/pace.13037.
Semmler V, Biermann J, Haller B, Jilek C, Sarafoff N, Lennerz C, et al. ICD shock, not ventricular fibrillation, causes elevation of high sensitive troponin T after defibrillation threshold testing--the prospective, randomized, MulticentreTropShock-Trial. PLoS One. 2015;10(7):e0131570. https://doi.org/10.1371/journal.pone.0131570.
Gasparini M, Proclemer A, Klersy C, Kloppe A, Lunati M, Ferrer JB, et al. Effect of long-detection interval vs standard-detection interval for implantable cardioverter-defibrillators on antitachycardia pacing and shock delivery: the ADVANCE III randomized clinical trial. JAMA. 2013;309(18):1903–11. https://doi.org/10.1001/jama.2013.4598.
Wathen MS, De Groot PJ, Sweeney MO, Stark AJ, Otterness MF, Adkisson WO, et al. Prospective randomized multicenter trial of empirical antitachycardia pacing versus shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter defibrillators: PainFREE Rx II Trial Results. Circulation. 2004;104:796–801. https://doi.org/10.1161/01.CIR.0000145610.64014.E4.
Vaseghi M, Shivkumar K. The role of the autonomic nervous system in sudden cardiac death. ProgCardiovasc Dis. 2008;50(6):404–19. https://doi.org/10.1016/j.pcad.2008.01.003.
Zipes DP, Barber MJ, Takahashi N, Gilmour RF. Influence of the autonomic nervous system on the genesis of cardiac arrhythmias. Pacing ClinElectrophysiol. 1983;6:1210–20.
Anderson JL, Rodier HE, Green LS. Comparative effects of beta-adrenergic blocking drugs on experimental ventricular fibrillation threshold. Am J Cardiol. 1983;51(7):1196–202. https://doi.org/10.1016/0002-9149(83)90368-5.
Brodine WN, Tung RT, Lee JK, Hockstad ES, Moss AJ, Zareba W, et al. Effects of beta-blockers on implantable cardioverter defibrillator therapy and survival in the patients with ischemic cardiomyopathy (from the Multicenter Automatic Defibrillator Implantation Trial-II). Am J Cardiol. 2005;96(5):691–5. https://doi.org/10.1016/j.amjcard.2005.04.046.
Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm: sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation. 2000;102(7):742–7.
•• Chatzidou S, Kontogiannis C, Tsilimigras DI, Georgiopoulos G, Kosmopoulos M, Papadopoulou E, et al. Propranolol versus metoprolol for treatment of electrical storm in patients with implantable cardioverter-defibrillator. J Am CollCardiol. 2018;71(17):1897–906. https://doi.org/10.1016/j.jacc.2018.02.056 Findings from this study suggest that non-selective β1 and β2 blockade is superior to β1 blockade in the management of electrical storm.
Bourque D, Daoust R, Huard V, Charneux M. Beta-blockers for the treatment of cardiac arrest from ventricular fibrillation? Resuscitation. 2007;75(3):434–44. https://doi.org/10.1016/j.resuscitation.2007.05.013.
Ferreira-González I, Dos-Subirá L, Guyatt GH. Adjunctive antiarrhythmic drug therapy in patients with implantable cardioverter defibrillators: a systematic review. Eur Heart J. 2007;28(4):469–77. https://doi.org/10.1093/eurheartj/ehl478.
Levine JH, Massumi A, Scheinman MM, Winkle RA, Platia EV, Chilson DA, et al. Intravenous amiodarone for recurrent sustained hypotensive ventricular tachyarrhythmias. Intravenous Amiodarone Multicenter Trial Group. J Am CollCardiol. 1996;27(1):67–75. https://doi.org/10.1016/0735-1097(95)00427-0.
Kerin NZ, Blevins RD, Frumin H, Faitel K, Rubenfire M. Intravenous and oral loading versus oral loading alone with amiodarone for chronic refractory ventricular arrhythmias. Am J Cardiol. 1985;55(1):89–91. https://doi.org/10.1016/0002-9149(85)90305-4.
Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES, et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC Study: a randomized trial. JAMA. 2006;295(2):165–71. https://doi.org/10.1001/jama.295.2.165.
•• Santangeli P, Muser D, Maeda S, Filtz A, Zado ES, Frankel DS, et al. Comparative effectiveness of antiarrhythmic drugs and catheter ablation for the prevention of recurrent ventricular tachycardia in patients with implantable cardioverter-defibrillators: a systematic review and meta-analysis of randomized controlled trials. Heart Rhythm. 2016;13:1552–9. https://doi.org/10.1016/j.hrthm.2016.03.004 Findings from this systematic review and meta-analysis demonstrate the role of both antiarrhythmic drugs and catheter ablation for the reduction of ICD shocks. Notably, the lack of a mortality benefit highlights the need for further research.
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352(3):225–37. https://doi.org/10.1056/NEJMoa043399.
Jung W, Manz M, Pizzulli L, Pfeiffer D, Lüderitz B. Effects of chronic amiodarone therapy on defibrillation threshold. Am J Cardiol. 1992;70(11):1023–7. https://doi.org/10.1016/0002-9149(92)90354-2.
Gorgels AP, van den Dool A, Hofs A, Mulleneers R, Smeets JL, Vos MA, et al. Comparison of procainamide and lidocaine in terminating sustained monomorphic ventricular tachycardia. Am J Cardiol. 1996;78:43–6. https://doi.org/10.1016/S0002-9149(96)00224-X.
Ortiz M, Martín A, Arribas F, Coll-Vinent B, Del Arco C, Peinado R, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J. 2017;38(17):1329–35. https://doi.org/10.1093/eurheartj/ehw230.
Pacifico A, Hohnloser SH, Williams JH, Tao B, Saksena S, Henry PD, et al. Prevention of implantable-defibrillator shocks by treatment with sotalol. N Engl J Med. 1999;340(24):1855–62. https://doi.org/10.1056/NEJM199906173402402.
Kettering K, Mewis C, Dörnberger V, Vonthein R, Bosch RF, Kühlkamp V. Efficacy of metoprolol and sotalol in the prevention of recurrences of sustained ventricular tachyarrhythmias in patients with an implantable cardioverter defibrillator. Pacing ClinElectrophysiol. 2002;25(11):1571–6. https://doi.org/10.1046/j.1460-9592.2002.01571.x.
Waldo AL, Camm AJ, de Ruyter H, Friedman PL, DJ MN, Pauls JF, et al. Effect of d-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction. The SWORD Investigators. Survival with Oral d-Sotalol. Lancet. 1996;348:7–12. https://doi.org/10.1016/S0140-6736(96)02149-6.
Deyell MW, Steinberg C, Doucette S, Parkash R, Nault I, Gray C, et al. Mexiletine or catheter ablation after amiodarone failure in the VANISH trial. J Cardiovasc Electrophysiol. 2018;29(4):603–8. https://doi.org/10.1111/jce.13431.
Lee SD, Newman D, Ham M, Dorian P. Electrophysiologic mechanisms of antiarrhythmic efficacy of a sotalol and class Ia drug combination: elimination of reverse use dependence. J Am Coll Cardiol. 1997;29(1):100–5. https://doi.org/10.1016/S0735-1097(96)00423-8.
Van Herendael H, Pinter A, Ahmad K, Korley V, Mangat I, Dorian P. Role of antiarrhythmic drugs in patients with implantable cardioverter defibrillators. Europace. 2010;12(5):618–25. https://doi.org/10.1093/europace/euq073.
Burjorjee JE, Milne B. Propofol for electrical storm; a case report of cardioversion and suppression of ventricular tachycardia by propofol. Can J Anaesth. 2002;49(9):973–7. https://doi.org/10.1007/BF03016886.
Anderson KP. Sudden cardiac death unresponsive to implantable defibrillator therapy: an urgent target for clinicians, industry and government. J Interv Card Electrophysiol. 2005;14:71–8.
Mitchell LB, Pineda EA, Titus JL, Bartosch PM, Benditt DG. Sudden death in patients with implantable cardioverter defibrillators: the importance of post-shock electromechanical dissociation. J Am Coll Cardiol. 2002;39:1323–8. https://doi.org/10.1016/S0735-1097(02)01784-9.
Huang S, Miller J. Catheter ablation of cardiac arrhythmias. Elsevier Editions, 3rd Edition.
Palaniswamy C, Kolte D, Harikrishnan P, Khera S, Aronow WS, Mujib M, et al. Catheter ablation of postinfarction ventricular tachycardia: ten-year trends in utilization, in-hospital complications, and in-hospital mortality in the United States. Heart Rhythm. 2014;11(11):2056–63. https://doi.org/10.1016/j.hrthm.2014.07.012.
Spartalis M, Spartalis E, Tzatzaki E, Tsilimigras DI, Moris D, Kontogiannis C, et al. Novel approaches for the treatment of ventricular tachycardia. World J Cardiol. 2018;10(7):52–9. https://doi.org/10.4330/wjc.v10.i7.52.
Nayyar S, Ganesan AN, Brooks AG, Sullivan T, Roberts-Thomson KC, Sanders P. Venturing into ventricular arrhythmia storm: a systematic review and meta-analysis. Eur Heart J. 2013;34(8):560–71. https://doi.org/10.1093/eurheartj/ehs453.
Di Biase L, Santangeli P, Burkhardt DJ, Bai R, Mohanty P, Carbucicchio C, et al. Endoepicardial homogenization of the scar versus limited substrate ablation for the treatment of electrical storms in patients with ischemic cardiomyopathy. J Am Coll Cardiol. 2012;60:132–41. https://doi.org/10.1016/j.jacc.2012.03.044.
Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin JF, et al. Ventricular tachycardia ablation versus escalation of antiarrhythmic drugs. N Engl J Med. 2016;375:111–21. https://doi.org/10.1056/NEJMoa1513614.
Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M, Jongnarangsin K, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007;357(26):2657–65. https://doi.org/10.1056/NEJMoa065457.
Kuck KH, Schaumann A, Eckardt L, Willems S, Ventura R, Delacrétaz E, et al. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicenter randomised controlled trial. Lancet. 2010;375(9708):31–40. https://doi.org/10.1016/S0140-6736(09)61755-4.
Liang JJ, Muser D, Santangeli P. Ventricular tachycardia ablation clinical trials. Card Electrophysiol Clin. 2017;9(1):153–65. https://doi.org/10.1016/j.ccep.2016.10.012.
Haegeli LM, Della Bella P, Brunckhorst CB. Management of a patient with electrical storm, role of epicardial catheter ablation. Circulation. 2016;133(7):672–6. https://doi.org/10.1161/CIRCULATIONAHA.115.016336.
Ajijola OA, Lellouche N, Bourke T, Tung R, Ahn S, Mahajan A, et al. Bilateral cardiac sympathetic denervation for the management of electrical storm. J Am Coll Cardiol. 2012;59(1):91–2. https://doi.org/10.1016/j.jacc.2011.09.043.
Vaseghi M, Gima J, Kanaan C, Ajijola OA, Marmureanu A, Mahajan A, et al. Cardiac sympathetic denervation in patients with refractory ventricular arrhythmias or electrical storm: intermediate and long-term follow-up. Heart Rhythm. 2014;11(3):360–6. https://doi.org/10.1016/j.hrthm.2013.11.028.
• Vaseghi M, Barwad P, MalavassiCorrales FJ, Tandri H, Mathuria N, Shah R, et al. Cardiac sympathetic denervation for refractory ventricular arrhythmias. J Am Coll Cardiol. 2017;69(25):3070–80. https://doi.org/10.1016/j.jacc.2017.04 The largest series of patients with refractory ventricular arrhythmias undergoing cardiac sympathetic denervation highlights the adjunctive role of this approach in patients with electrical storm.
Do DH, Bradfield J, Ajijola OA, Vaseghi M, Le J, Rahman S, et al. Thoracic epidural anesthesia can be effective for the short-term management of ventricular tachycardia storm. J Am Heart Assoc. 20176(11). pii: e007080. doi: https://doi.org/10.1161/JAHA.117.007080.
Bourke T, Vaseghi M, Michowitz Y, Sankhla V, Shah M, Swapna N, et al. Neuraxial modulation for refractory ventricular arrhythmias: value of thoracic epidural anesthesia and surgical left cardiac sympathetic denervation. Circulation. 2010;121(21):2255–62. https://doi.org/10.1161/CIRCULATIONAHA.109.929703.
Fudim M, Boortz-Marx R, Ganesh A, Waldron NH, Qadri YJ, Patel CB, et al. Stellate ganglion blockade for the treatment of refractory ventricular arrhythmias: a systematic review and meta-analysis. Cardiovasc Electrophysiol. 2017;28(12):1460–7. https://doi.org/10.1111/jce.13324.
Remo BF, Preminger M, Bradfield J, Mittal S, Boyle N, Gupta A, et al. Safety and efficacy of renal denervation as a novel treatment of ventricular tachycardia storm in patients with cardiomyopathy. Heart Rhythm. 2014;11(4):541–6. https://doi.org/10.1016/j.hrthm.2013.12.038.
Antzelevitch C, Yan GX, Ackerman MJ, Borggrefe M, Corrado D, Guo J, et al. J-wave syndromes expert consensus conference report: emerging concepts and gaps in knowledge. J Arrhythm. 2016;32(5):315–39. https://doi.org/10.1016/j.joa.2016.07.002.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Christos Kontogiannis, Konstantinos Tampakis, Georgios Georgiopoulos, Stefano Bartoletti, Christos Papageorgiou, Hector Anninos, Alkistis Kapelouzou, Michael Spartalis, Ioannis Paraskevaidis, and Sofia Chatzidou declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Kontogiannis, C., Tampakis, K., Georgiopoulos, G. et al. Electrical Storm: Current Evidence, Clinical Implications, and Future Perspectives. Curr Cardiol Rep 21, 96 (2019). https://doi.org/10.1007/s11886-019-1190-0
Published:
DOI: https://doi.org/10.1007/s11886-019-1190-0