Abstract
Sarcoidosis with cardiac involvement is underdiagnosed and can put patients at risk of morbidity including conduction defects, arrhythmias and heart failure, as well as sudden cardiac death. In addition, cardiac sarcoidosis may have no clinical manifestations or non-specific presentation and diagnosis may be difficult on clinical criteria. Investigation for cardiac sarcoidosis should be considered in those with extra-cardiac sarcoidosis and cardiac findings as well as those under the age of 60 years presenting with atrioventricular block without a clear cause. Advanced imaging modalities including cardiac magnetic resonance and positron emission tomography may help in both the diagnosis and assessment of response to treatment for cardiac sarcoidosis. This ultimately may help to minimize associated adverse outcomes from this enigmatic disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a multisystem inflammatory disease with characteristic non-caseating granulomas on histopathology [1]. The lungs and pulmonary lymph nodes are most commonly affected, but the heart and other tissues including skin, eyes, central nervous system, liver, spleen and skeleton can also be involved [2–7]. The aetiology of sarcoidosis is not well understood. It is most likely to be multifactorial with environmental triggers precipitating an immune response and granulomatous inflammation in susceptible individuals with a polygenic predisposition [3, 8, 9].
Sarcoidosis can occur at any age, with peak incidence at 20–39 years [10]. Although it affects all racial groups, a likely genetic component is reflected by the predominance of the disease in certain populations; incidence of sarcoidosis in white Americans approximates 10 per 100,000 per annum, compared to 35 per 100,000 in African Americans [10]. Scandinavians have the highest annual incidence rates with reports of 55–64 cases per 100,000, whereas rates of 10–20 per 100,000 are seen across Europe and ≤6 per 100,000 in Asia [11].
Cardiac Sarcoidosis
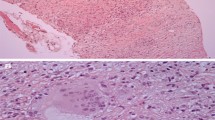
The heart is the third most commonly affected organ in sarcoidosis [2]. Johns and Michele reported that only up to 7 % of patients with systemic sarcoidosis had cardiac symptoms or clinical manifestations [12]. Autopsy series describe higher rates of myocardial involvement, ranging from 27 to 47 % [1, 4, 13]. Clinical imaging studies also describe prevalence rates between 19 and 55 % for asymptomatic cardiac sarcoidosis (CS) in patients with extra-cardiac sarcoidosis [14••, 15••, 16–18]. The typical pathology in CS is patchy oedematous and granulomatous infiltration of the myocardium. The active, inflammatory phase may subside or progress to fibrosis [1, 3].
Cardiac disease worsens prognosis and is an important cause of mortality in sarcoidosis patients, although pulmonary sarcoidosis has been reported as the most common cause of death from sarcoidosis in Caucasians [3, 4, 13]. Japanese studies have observed the highest rates of cardiac involvement and adverse outcome in their population. It has been reported that 67 % of patients with systemic sarcoidosis in Japan have CS, and up to 85 % of deaths are attributed to CS [13, 19–21]. One Japanese study has observed overall mortality rates in CS of 40 % at 5 years [20]. In our meta-analysis of CS patients treated with corticosteroids, 5-year mortality rates ranging between 0 and 25 % were observed [22••].
Clinical Aspects
CS is usually clinically silent and often is detected on screening of patients with systemic sarcoidosis. It may have variable clinical manifestations which depend on the stage, degree and location of disease. Presentations can range from conduction disturbances (most commonly), supraventricular and ventricular arrhythmias, left and/or right heart failure, pericardial effusion and sudden death [1, 6, 9, 23, 24••].
Electrical manifestations of CS are clinically significant [25••]. Nery et al., in a series of consecutive patients aged ≤60 years, showed that 34 % of those with unexplained atrioventricular block had previously undiagnosed CS, and were more likely to have adverse outcomes than those without CS [24••]. Kandolin et al. in a 72 patient Finish study have also shown CS is common in patients with unexplained AV block, occurring in 19 % of cases [26••]. Patients with CS may experience ventricular tachycardia (VT) and ventricular fibrillation (VF). Betensky and colleagues observed an incidence of 15 % per year on long-term follow up in those with biopsy-proven sarcoidosis and cardiac involvement confirmed by clinical criteria, and/or advanced imaging, and/or cardiac biopsy [27••].
Ventricular tachyarrhythmias and atrioventricular block account for 30–65 % of deaths in patients with CS [2]. Extent of left ventricular (LV) dysfunction, worse New York Heart Association functional class, LV dilation and history of VT have been shown to be predictors of mortality [20, 22••]. CS should be considered and ruled out in all patients diagnosed with extra-cardiac sarcoidosis and in all patients under the age of 60 with unexplained advanced atrioventricular block [24••, 25••].
Treatment with corticosteroids may improve outcomes in patients with active CS, with modest data to support its use [22••, 28]. There may be a role for steroid-sparing immunosuppression (e.g. methotrexate, azathioprine). However, no current therapies for cardiac sarcoidosis are validated by randomized control trials. There is an important role for pacemaker devices for those with advanced conduction abnormality, and prophylactic implantable cardiac defibrillator (ICD) devices can be lifesaving in those at risk of ventricular arrhythmia [25••, 29]. The 2014 Heart Rhythm Society (HRS) consensus statement offers comprehensive guidelines for prophylactic ICD implant, with recommendations ranging from class I to class IIb depending on clinical and imaging findings [25••]. For all these reasons, it is important to accurately diagnose CS early [5].
Diagnosis
Diagnosis of CS can be challenging, particularly in the early stages of disease. Myocardial biopsy, considered to be the gold standard when positive, is highly specific but is invasive and has poor sensitivity with a diagnostic yield as low as 19 % [2, 30]. This is because cardiac involvement is not homogeneous and lesions are usually in a patchy distribution. Lesions predominate in the basal and mid interventricular septum and are patchy elsewhere [5, 6, 16], whereas biopsy sampling tends to be acquired from along the right side of the septum [17]. Cardiac biopsy cannot effectively rule out disease. Newer techniques such as voltage guidance may increase the yield of endomyocardial biopsy [31].
Although positive biopsy is definitive, the poor sensitivity means that currently, the diagnosis of CS is most often made using clinical criteria. Until recently, the Japanese Ministry of Health and Welfare (JMHW) guidelines have been used as the best available standard and take into account invasive tissue diagnosis, and electrical, functional and structural abnormalities noted on electrocardiography, echocardiography, nuclear imaging or cardiac magnetic resonance (CMR) imaging [32]. However, some data have suggested that these criteria have low sensitivity [30] and may fail to detect early signs of cardiac involvement [33]. JMHW criteria presently do not give heavy weighting to modern advanced cardiac imaging modalities, with gadolinium-enhanced CMR added as a minor criterion in the 2006 revision and positron emission tomography (PET) not included in the current JMHW algorithm.
The recent collaborative consensus statement from the Heart Rhythm Society (HRS) and others does however recognize the role of advanced imaging with PET and CMR in the diagnostic workup for CS (Table 1) [25••]. The HRS expert consensus provides the current accepted criteria for the diagnosis of CS. Advanced cardiac imaging holds much promise in the identification and surveillance of CS. CMR and PET are the tests of choice in most centres that have access to them. Whilst they are not optimal modalities for diagnosis of CS, there are features on echocardiography and cardiac CT that may corroborate diagnosis. This review will address each of the imaging modalities for CS.
Echocardiography
Abnormalities on echocardiography have been described in up to 13–31 % of patients with systemic sarcoidosis and in 46 % of those with CS [6, 17, 34, 35]. There are no definite findings on echocardiogram that may confirm CS, but there are changes that may be consistent with the diagnosis. Additional tests are required to establish or exclude a diagnosis of CS. The most common echocardiographic abnormalities in patients with CS are septal wall thinning or thickening, systolic and diastolic dysfunction and wall motion abnormalities [34, 35]. Pericardial effusion and mitral regurgitation can rarely be present.
Echocardiography can determine LV cavity size, which has prognostic implications in that LV dilatation is strongly associated with increased mortality [20]. However, early, localized or limited disease often does not have changes that can be seen on echocardiogram. Recent studies suggest that speckle tracking strain echocardiography may have a role in assessment of CS, as patients with structural lesions have a drop in global longitudinal and circumferential strain parameters [36, 37]; however, more and larger studies are needed to determine its clinical role.
Nuclear Perfusion Imaging
Radionuclide studies have been commonly used to identify cardiac disease in patients with sarcoidosis. These include single photon emission CT (SPECT) myocardial perfusion imaging (MPI) with thallium-201(Tl-201) or technetium-99m (Tc-99m) and gallium-67 (Ga-67) scintigraphy [9]. Resting perfusion scans using Tl-201 or Tc-99m based MPI may show decreased tracer uptake in areas of damaged myocardium representing fibrotic or granulomatous tissue; this may correlate with heart block and tachyarrhythmia [8, 9, 38].
Sensitivity of Tl-201-based MPI in patients with clinical suspicion of CS has been reported at 45 and 58 % in small studies, whereas sensitivity for Tc-99-based MPI studies has been reported at 65 % [39, 40]. Abnormality on Tl-201 MPI in patients with systemic sarcoidosis who do not have cardiac symptoms has not been shown to have prognostic value [41]. ‘Reverse redistribution’ is a finding sometimes seen in patients with CS described on Tl-201 and Tc-99m-based MPI, where focal perfusion defects on rest imaging improve or disappear altogether on stress imaging, which is opposite to the pattern seen in ischaemia caused by coronary artery stenosis [42, 43]. This has been hypothesized to be due to focal reversible vasoconstriction in arterioles adjacent to sarcoid granulomas [44].
Ga-67 scintigraphy displays ‘hot spots’ in areas of active inflammation and has the advantage of being able to diagnose both pulmonary and systemic sarcoidosis, as well as assess disease activity and effect of treatment [45, 46]. Ga-67 scanning has high specificity (reported at nearly 100 %); however, its image resolution is low and has much lower sensitivity (reports ranging from 18 to 50 %) than other radionuclide tests [40, 42, 47, 48]. Whilst Ga-67 scintigraphy is excellent in detection of inflammation, it may not identify areas of fibrosis and may miss quiescent disease.
FDG PET is more accurate in detecting myocardial abnormalities than Tc-99m MPI and Ga-67 SPECT in sarcoidosis patients [48–50]. In centres where PET or CMR are available, these newer imaging techniques have mostly replaced other radionuclide imaging.
Computed Tomography
Cardiac computed tomography (CT) angiography can be helpful to exclude coronary artery disease in patients being assessed for cardiac sarcoid. Additionally, there are case reports that describe findings on cardiac CT in patients with CS. Late contrast-enhanced cardiac CT images have been reported to demonstrate similar location and extent of enhancement to those of CMR [51, 52]. Generally, fibrosis if large enough can also be seen as areas of hypo-enhancement in the myocardium on rest CT perfusion imaging; however, this is not specific to scar from sarcoidosis.
Furthermore, if retrospective ECG-gated cardiac CT examination is performed, relevant findings may also be detected such as wall motion abnormalities, decreased LV ejection fraction (LVEF) and/or morphological abnormalities (aneurysms, myocardial thinning or thickening), all of which may help to support the diagnosis of CS, but at the expense of increasing radiation dose.
Screening for characteristic pulmonary parenchymal abnormalities and enlarged mediastinal and hilar lymph nodes in an extended field of view reconstruction should be performed when Sarcoidosis is suspected. It should be noted that the recent consensus statement from HRS recommends high resolution CT of the thorax be performed in patients <60 years old with unexplained advanced AV block [25••].
Cardiac Magnetic Resonance Imaging
Role and Diagnostic Performance
Cardiac magnetic resonance with late gadolinium enhancement (LGE-CMR) is emerging as a preferred advanced imaging modality to evaluate CS [16, 53]. CMR is an accurate non-invasive test that offers both structural and functional information. It has high sensitivity (87.5–100 %), but lower specificity (38.5–78 %) for detecting CS [5, 6]. Smedema et al. reported “positive and negative predictive values of 55 and 100 % respectively, with overall accuracy of 83 %” [6]. Thus, to enable early diagnosis if CS is suspected, recent guidelines recommend advanced imaging with high sensitivity, such as CMR or PET, be performed [25••].
CMR represents an important tool for the early diagnosis and treatment of CS [6]. Due to the high spatial resolution of the LGE techniques, CMR is able to detect even small areas of myocardial damage which may not have yet caused structural or electrical abnormality, and may not be detected by other imaging methods [15••]. Such areas of myocardial damage are clinically relevant as they may be potential substrate for arrhythmias and sudden cardiac death, and they can also be targeted if endomyocardial biopsy is required, to increase its diagnostic yield.
Imaging Techniques and Findings
CMR findings depend on the stage of disease. CMR is able to detect the acute inflammatory and chronic phases of CS [54]. These two phases may frequently overlap. During the acute phase, areas of focal wall thickening associated with wall motion abnormalities on steady state free precession (SSFP) CINE sequences may be seen. T2 weighted imaging (T2WI) may show foci of increased signal intensity, indicative of edema and active granulomatous infiltration [55•, 56]. Crouser et al. have also reported that T2 mapping techniques allow quantitative measurement of free water in the myocardium [57], which in the context of CS is presumed to represent granulomatous inflammation [58]. Importantly, recent reports suggest that high myocardial T2 values could represent early stages of disease that may be reversible with appropriate treatment [55•].
Despite useful information provided by T2WI techniques, LGE-CMR has attracted most of the attention of the scientific community in recent years. Gadolinium, an extracellular contrast agent, is depicted as areas of myocardial enhancement (Fig. 1c). It is retained in areas of myocardial damage such as fibrosis and necrosis [59]. LGE may be seen in up to 19–35 % of patients with extra-cardiac sarcoidosis in whom a clinical diagnosis of CS has not been established [6, 14••, 15••, 17, 55•, 60]. Although there is no pathognomonic finding, frequently seen patterns in CS include patchy mid-myocardial, linear sub-epicardial or transmural enhancement.
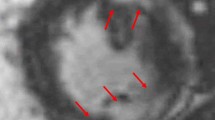
54-year-old female presented with ventricular tachycardia and complete heart block requiring emergent temporary pacing, with subsequent implant of ICD for secondary prevention. Endomyocardial biopsy demonstrated non caseating granuloma, confirming the diagnosis of CS. CMR and PET imaging performed at time of diagnosis are shown below. a PET study with focal intense uptake of FDG tracer (black and white panels) in the basal and inferior septum and inferior wall, with partially corresponding areas of reduced perfusion on rubidium-82 PET images seen in the basal septum and inferior wall (upper panels). These metabolically active areas on PET represent active inflammation due to CS, and in this case, parallel enhancement on CMR. Note RV uptake is present. b Whole body PET image, depicting multifocal hypermetabolic lesions in the heart, as well as extra-cardiac active inflammation from sarcoidosis in the pulmonary, mediastinal and hilar lymph nodes. Uptake in the kidneys, urinary bladder and gut are physiological. c Late gadolinium enhancement magnitude inversion recovery image in the short axis oblique plane of the same patient shows typical linear enhancement in the septum and subepicardial anterior wall (short arrows), as well as almost transmural enhancement in the inferior wall (long arrow). Note the enhancement in the right ventricular side of the septum (black arrow), a characteristic finding in cardiac sarcoid
In CS, LGE is usually in a non-vascular distribution. However, sub-endocardial enhancement in a coronary distribution similar to myocardial infarction has been observed. This pattern can be difficult to differentiate from myocardial infarction caused by ischemic heart disease [14••, 16, 56, 61]. Enhancement in CS has a preference to involve the basal and mid interventricular septum and to a lesser extent lateral LV wall [5, 6, 8, 16]. Interestingly, enhancement in the RV side of the interventricular septum has been reported as a common pattern present in up to 67 % of CS patients [16]. Typically, transmural enhancement may be associated with myocardial thinning and regional wall motion abnormalities in the chronic phase of the disease [14••, 33, 56].
As noted above for CT imaging, SSFP CINE sequences are able to accurately depict other findings suggestive of CS including morphological abnormalities (aneurysms, myocardial thickening or thinning), wall motion abnormalities as well as LV systolic dysfunction.
As CS is often associated with arrhythmias and cardiomyopathy, in some cases, an important differential to consider is arrhythmogenic right ventricular cardiomyopathy (ARVC). CMR can be very useful to differentiate these two entities. Steckman et al., in a study of 61 patients, observed that those with CS versus ARVC were more likely to have CMR findings of LGE (73 vs 19 %), isolated LV involvement (53 vs 0 %), septal involvement (43 vs 0 %) and mediastinal lymphadenopathy (68 vs 0 %), whereas those with ARVC where more likely to have isolated right ventricular involvement (76 vs 20 %), lower right ventricular (RV) ejection fraction, and larger LV and RV systolic and diastolic volumes [62••]. All patients with ARVC had RV CMR findings [62••].
Prognosis and Monitoring Response to Therapy
LGE-CMR is able to detect small scars that may be the substrate of arrhythmias and SCD [6]. There is increasing evidence that the presence of LGE is a robust independent predictor of death and adverse events in patients with suspected CS [6, 14••, 16], with one recent study suggesting the contrary [33]. Thus, the presence of myocardial enhancement is emerging as an important tool for risk stratification. Greulich and colleagues reported hazard ratio (HR) of 31.6 for ‘death, aborted SCD, and appropriate ICD discharge’ and HR of 33.9 for VT [14••]. Similarly, Patel et al., demonstrated that patients with LGE “had a 9-fold higher rate of major adverse cardiac events (MACE) and 11.5-fold higher rate of cardiac death compared to patients without LGE” (MACE, 17.2 % versus 1.9 % per year; cardiac death, 11.5 % versus 1.0 % per year) [16].
In addition, in at least one study of patients with systemic sarcoidosis without myocardial enhancement, no SCD or VT was observed, even in the presence of dilated LV and severely impaired systolic function. This suggests that LGE on CMR may confer prognostic data beyond that provided by ventricular function alone [14••]. LGE-CMR has also been shown to be useful in assessing response to steroid therapy, as enhancement may improve after treatment and correlate with clinical course [8, 63–65].
Advantages and Limitations
CMR has the advantage of wider availability than PET, lack of radiation exposure for patients, and high sensitivity and specificity for the detection of CS. It has high spatial resolution that can enable identification of small areas of scar. Different techniques are available to help differentiate active and fibrotic phases of CS.
Cardiac devices, such as defibrillators or pacemakers, are often required in patients with CS, but are, in general, contraindications to CMR. This limits the role of CMR in surveillance for disease progression and effects of treatment. CMR-conditional devices are now available (presently selected pacemakers and implantable loop recorders (ILR) have received CMR-conditional labelling in North America, but no ICD system is approved as CMR-conditional). However, with the CMR conditional devices, image quality may be suboptimal due to artefact. The risks of proceeding with CMR in patients with devices should be carefully balanced with the potential benefit of CMR imaging and assessed on a case-by-case basis. CMR also may miss early inflammation. Whilst T2 imaging may help, it is still associated with technical challenges for the time being.
Positron Emission Tomography
Role and Diagnostic Performance
18-Fluorodeoxyglucose (FDG) positron emission tomography (PET) can also be useful to aid in the diagnosis and follow up of CS. Uptake on FDG-PET suggests active inflammatory process, and steroid treatment has been shown to decrease its size and intensity. The strength of FDG-PET is high sensitivity to detect active CS [5, 50, 66••]. A number of small studies have confirmed its diagnostic accuracy, reporting sensitivity of 81–100 % for detection of CS, with four studies noting a sensitivity of 100 % [5, 48, 50, 67, 68••, 69]. Although studies have reported specificities of 82–91 % [49, 50, 67, 68••], recent reports have observed lower specificity, as low as 39 % [5, 70••]. An explanation for the lower specificity seen in the latter studies may be the ability of PET to detect subclinical CS when compared to JMHW criteria.
We have previously conducted a meta-analysis of seven studies, including the Ontario registry, which included a total of 164 patients, most diagnosed with systemic sarcoidosis, and approximately half with cardiac sarcoidosis [66••]. Pooled data for FDG PET yielded “89 % sensitivity and 78 % specificity, with 4.1 positive likelihood ratio and 0.19 negative likelihood ratio”, and overall diagnostic odds ratio was 25.6 [66••]. Our meta-analysis confirms the high diagnostic accuracy of FDG PET to assist in diagnosing CS when compared to JMHW guidelines.
Imaging Techniques and Findings
FDG PET uptake assesses active inflammation, which is characterized by increased glucose metabolism, particularly by activated macrophages. Additionally, rubidium-82 (Rb-82) and N-13-ammonia can be used to assess for perfusion defects (PD), which can be caused by fibrous replacement secondary to chronic granulomatous disease [9]. Patterns suggestive of active CS are mainly focal areas of FDG uptake, and focal on top of diffuse uptake [71•]. In patients with CS, FDG uptake is frequently seen in the lungs, lymph nodes and other organs affected by this systemic disease; however, very occasionally, CS can be isolated without systemic sarcoidosis [31].
Normal cardiac uptake of FDG can vary depending on fasting state. Thus, PET scanning protocols aim to suppress physiological uptake of FDG by the myocardium and enable switch to free fatty acid (FFA) metabolism. Methods to suppress normal myocardial glucose uptake include high-fat/low-carbohydrate diet, overnight fast and administration of unfractionated heparin (stimulates lipoprotein lipase which hydrolyzes triglycerides to FFA and glycerol) [71•, 72–75]. Recent advances include attempts at quantification of total volume and intensity of FDG uptake in patients with CS to improve consistency of readings and clinical correlation and prognostication [68••, 76•].
Prognosis and Monitoring Response to Therapy
Recent data supports the use of PET for risk stratification in CS and its ability to predict events [68••, 70••]. McArdle et al. demonstrated a correlation between FDG uptake and clinical presentation; patients with CS presenting with VT had significantly higher FDG uptake compared to those with advanced atrioventricular block or if clinically silent [68••]. In addition, maximal FDG uptake was localized to the basal septum in the majority of patients presenting with advanced atrioventricular block [68••].
Most recent findings confirming the prognostic ability of PET have come from Blankstein and colleagues who investigated 118 patients who underwent FDG PET as part of a workup for CS. In this study, 60 % had abnormal PET studies and VT and death were observed in 26 % [70••]. Cardiac PET predicted adverse events, and the presence of both a perfusion defect and abnormal FDG was associated with a hazard ratio of 3.9 [70••]. Their data suggest PET offers prognostic value superior to JMHW clinical criteria, presence of extra-cardiac sarcoidosis and LVEF. Blankstein et al. also noted the importance of RV uptake of FDG, which held a worse prognosis [70••]. Likewise, Manabe et al. demonstrated that when RV uptake was present, patients were more likely to have positive JMHW criteria than when RV uptake was absent, and this difference was more striking than having LV uptake or not [77•].
FDG PET may also have a role to monitor treatment effect and progress in those with CS requiring treatment with corticosteroids. Following treatment with corticosteroids, perfusion defects associated with CS tend to remain unchanged, whereas degree of FDG uptake reduces or resolves with good response to treatment [48]. Osborne and colleagues have also recently shown that reduction in intensity and extent of myocardial inflammation on FDG PET is associated with improved LVEF and that follow-up PET scanning may help guide therapy [78••]. Although the current available data is promising, large prospective studies are required to better define the clinical role of FDG PET and determine its value for predicting outcome.
Advantages and Limitations
FDG PET has the advantage of the ability to well define the active inflammatory phase of CS disease, identify both cardiac and extra-cardiac sarcoidosis involvement (Fig. 1a, b), and follow patients for response to treatment, even if cardiac devices are present. Whilst more sensitive than CMR, it is less specific [5, 59]. Limitations of FDG PET include radiation exposure, albeit small, inadequate suppression of physiological FDG uptake in normal myocardium can render quality of the study suboptimal, and its low resolution may limit ability to detect small areas of myocardial damage. FDG-PET’s lower specificity means there may be difficulty in differentiating CS from other inflammatory diseases.
Future Developments
Given that CMR and PET have unique strengths and weaknesses in assessing different aspects of CS, hybrid imaging may have a role in the future. There are case reports describing PET-CMR to diagnose CS [79, 80]. In preliminary data in an abstract report, Wicks and colleagues have also undertaken a feasibility study of 51 patients to assess accuracy of hybrid PET-CMR for CS diagnosis [81]. They found that in isolation sensitivity of PET and CMR at detecting probable cardiac sarcoidosis was 65 and 60 % respectively; with hybrid imaging sensitivity improved to 89 % [81]. Hybrid imaging thus may enable more accurate and earlier diagnoses in this complex disease characterized by both active and chronic phases, as well as facilitate more effective monitoring of response to therapy.
Conclusions and Diagnostic Approach
Early diagnosis of CS is important because it can be associated with cardiomyopathy, atrioventricular block, ventricular arrhythmias and sudden cardiac death. Investigation for CS should be undertaken for in patients with extra-cardiac sarcoidosis and cardiac symptoms, ECG or echocardiography abnormalities (Fig. 2). Guidelines also suggest screening for CS in younger patients (≤60 years) with unexplained advanced heart block (Fig. 2) [25••]. Initial assessment should include history, examination, 12-lead ECG and echocardiogram [25••]. Echocardiography is universally available, without risk to the patient, and provides useful information about cardiac structure and function, and assesses for possible differential diagnoses.
Diagnostic Algorithm. a Suggested algorithm for the investigation of patients with biopsy-proven extracardiac sarcoidosis. Asterisk (*) indicates palpitations were defined as “prominent patient complaint lasting >2 weeks.” Double asterisk (**) indicates abnormal ECG defined as complete left or right bundle branch block and/or presence of unexplained pathological Q waves in two or more leads and/or sustained 2 or 3° AV block and/or sustained or non-sustained VT. Triple asterisk (***) indicates abnormal echocardiogram defined as RWMA and/or wall aneurysm and/or basal septum thinning and/or LVEF <40 %. b Suggested algorithm for the investigation of patients with unexplained Mobitz II or third-degree AV block who are younger than 60 years. Asterisk (*) indicates voltage-guided or advanced imaging-guided endomyocardial biopsy (reproduced with permission from the author and journal: Birnie DH, Sauer WH, Bogun F et al. HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Heart rhythm: the official journal of the Heart Rhythm Society 2014;11:1305–23) [25••]
If initial screen suggests possible CS, PET and CMR are powerful imaging tools that are preferred to other imaging modalities as they offer the best correlation with the disease [25••]. They can aid in the diagnosis of CS, and also monitor disease activity and response to treatment. CMR has the advantage of wider availability than PET, absence of radiation and is able to better detect small areas of scar and subclinical disease. PET is more sensitive and better for assessing acute inflammatory phase of the disease. It also has the advantage of being able to assess the response to anti-inflammatory therapy even in those with cardiac devices. If neither CMR nor PET is available, then investigation with Tl-201 or Tc-99m-based MPI and Ga-67 scintigraphy would be appropriate.
Surveillance imaging can assist in monitoring sarcoidosis activity, progression and response to therapy. There are no guidelines with regard to the timing of follow-up scans or how to adjust therapy after scanning. However, a reasonable approach may be repeat imaging 3–6 months after initiation of anti-inflammatory therapy. Collaborative multicentre studies are required to answer much about this condition. This includes identifying those at risk for cardiac events, the role of ICDs, steroids and other immunosuppressive therapies, the duration of treatments and the role of advanced cardiac imaging in monitoring response to treatment.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation. 1978;58:1204–11.
Roberts WC, McAllister Jr HA, Ferrans VJ. Sarcoidosis of the heart. A clinicopathologic study of 35 necropsy patients (group 1) and review of 78 previously described necropsy patients (group 11). Am J Med. 1977;63:86–108.
Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357:2153–65.
Perry A, Vuitch F. Causes of death in patients with sarcoidosis. A morphologic study of 38 autopsies with clinicopathologic correlations. Arch Pathol Lab Med. 1995;119:167–72.
Ohira H, Tsujino I, Ishimaru S, et al. Myocardial imaging with 18F-fluoro-2-deoxyglucose positron emission tomography and magnetic resonance imaging in sarcoidosis. Eur J Nucl Med Mol Imaging. 2008;35:933–41.
Smedema JP, Snoep G, van Kroonenburgh MP, et al. Evaluation of the accuracy of gadolinium-enhanced cardiovascular magnetic resonance in the diagnosis of cardiac sarcoidosis. J Am Coll Cardiol. 2005;45:1683–90.
Longcope WT, Freiman DG. A study of sarcoidosis; based on a combined investigation of 160 cases including 30 autopsies from The Johns Hopkins Hospital and Massachusetts General Hospital. Medicine. 1952;31:1–132.
Kim JS, Judson MA, Donnino R, et al. Cardiac sarcoidosis. Am Heart J. 2009;157:9–21.
Youssef G, Beanlands RS, Birnie DH, Nery PB. Cardiac sarcoidosis: applications of imaging in diagnosis and directing treatment. Heart. 2011;97:2078–87.
Rybicki BA, Major M, Popovich Jr J, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145:234–41.
Bresnitz EA, Strom BL. Epidemiology of sarcoidosis. Epidemiol Rev. 1983;5:124–56.
Johns CJ, Michele TM. The clinical management of sarcoidosis. A 50-year experience at the Johns Hopkins Hospital. Medicine. 1999;78:65–111.
Iwai K, Sekiguti M, Hosoda Y, et al. Racial difference in cardiac sarcoidosis incidence observed at autopsy. Sarcoidosis. 1994;11:26–31.
Greulich S, Deluigi CC, Gloekler S, et al. CMR imaging predicts death and other adverse events in suspected cardiac sarcoidosis. J Am Coll Cardiol Img. 2013;6:501–11. Study of 155 consecutive patients with systemic sarcoid, finding that LGE was of prognositc value and the strongest predictor of adverse of adverse events and death.
Patel AR, Klein MR, Chandra S, et al. Myocardial damage in patients with sarcoidosis and preserved left ventricular systolic function: an observational study. Eur J Heart Fail. 2011;13:1231–7. Prospective study using CMR-LGE in 81 consecutive patients with biopsy-proven extracardiac sarcoidosis, finding that CMR-LGE was more sensitive than clinical criteria and predictive of outcomes.
Patel MR, Cawley PJ, Heitner JF, et al. Detection of myocardial damage in patients with sarcoidosis. Circulation. 2009;120:1969–77.
Mehta D, Lubitz SA, Frankel Z, et al. Cardiac involvement in patients with sarcoidosis: diagnostic and prognostic value of outpatient testing. Chest. 2008;133:1426–35.
Vignaux O, Dhote R, Duboc D, et al. Detection of myocardial involvement in patients with sarcoidosis applying T2-weighted, contrast-enhanced, and cine magnetic resonance imaging: initial results of a prospective study. J Comput Assist Tomogr. 2002;26:762–7.
Matsui Y, Iwai K, Tachibana T, et al. Clinicopathological study of fatal myocardial sarcoidosis. Ann N Y Acad Sci. 1976;278:455–69.
Yazaki Y, Isobe M, Hiroe M, et al. Prognostic determinants of long-term survival in Japanese patients with cardiac sarcoidosis treated with prednisone. Am J Cardiol. 2001;88:1006–10.
Sekiguchi M, Numao Y, Imai M, Furuie T, Mikami R. Clinical and histopathological profile of sarcoidosis of the heart and acute idiopathic myocarditis. Concepts through a study employing endomyocardial biopsy. I. Sarcoidosis. Jpn Circ J. 1980;44:249–63.
Sadek MM, Yung D, Birnie DH, Beanlands RS, Nery PB. Corticosteroid therapy for cardiac sarcoidosis: a systematic review. Can J Cardiol. 2013;29:1034–41. Systematic review that identified 10 publications reporting outcomes after corticosteroid therapy, with the best data related to atrioventricular conduction recovery, and use of corticosteroids in CS appeared to be beneficial.
Sharma OP, Maheshwari A, Thaker K. Myocardial sarcoidosis. Chest. 1993;103:253–8.
Nery PB, Beanlands RS, Nair GM et al. Atrioventricular Block as the Initial Manifestation of Cardiac Sarcoidosis in Middle-Aged Adults. J Cardiovasc Electrophysiol. 2014;25(8):875–81. Prospective study of 32 consecutive patients aged <60 years presenting with unexplained atrioventricular block, finding 34 % had had previously undiagnosed CS.
Birnie DH, Sauer WH, Bogun F, et al. HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Heart Rhythm Off J Heart Rhythm Soc. 2014;11:1305–23. Recent collaborative consensus statement from the Heart Rhythm Society and others. It recognizes the role of advanced imaging with PET and MRI in the diagnostic algorithm for CS and provides the most up to date recommendations regarding diagnosis and management of CS.
Kandolin R, Lehtonen J, Kupari M. Cardiac sarcoidosis and giant cell myocarditis as causes of atrioventricular block in young and middle-aged adults. Circ Arrhythm Electrophysiol. 2011;4:303–9. Finish series of 72 patients showing CS is common in patients with unexplained AV block, occurring in 19 % of cases.
Betensky BP, Tschabrunn CM, Zado ES, et al. Long-term follow-up of patients with cardiac sarcoidosis and implantable cardioverter-defibrillators. Heart Rhythm Off J Heart Rhythm Soc. 2012;9:884–91. Study with long term follow up of 45 patients with CS observing an incidence of 15 % per year of ventricular tachycardia and ventricular fibrillation.
Lorell B, Alderman EL, Mason JW. Cardiac sarcoidosis. Diagnosis with endomyocardial biopsy and treatment with corticosteroids. Am J Cardiol. 1978;42:143–6.
Epstein AE, Dimarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary. Heart Rhythm Off J Heart Rhythm Soc. 2008;5:934–55.
Uemura A, Morimoto S, Hiramitsu S, Kato Y, Ito T, Hishida H. Histologic diagnostic rate of cardiac sarcoidosis: evaluation of endomyocardial biopsies. Am Heart J. 1999;138:299–302.
Nery PB, Keren A, Healey J, Leug E, Beanlands RS, Birnie DH. Isolated cardiac sarcoidosis: establishing the diagnosis with electroanatomic mapping-guided endomyocardial biopsy. Can J Cardiol. 2013;29(8):1015 e1–3.
Tsuda T. [Diagnostic standards for sarcoidosis]. Nihon Naika Gakkai zasshi. J Jpn Soc Intern Med. 2006;95:1025–9.
Nagai T, Kohsaka S, Okuda S, Anzai T, Asano K, Fukuda K. Incidence and prognostic significance of myocardial late gadolinium-enhancement in sarcoidosis patients without cardiac manifestation. Chest. 2014;146(4):1064–72
Burstow DJ, Tajik AJ, Bailey KR, DeRemee RA, Taliercio CP. Two-dimensional echocardiographic findings in systemic sarcoidosis. Am J Cardiol. 1989;63:478–82.
Lewin RF, Mor R, Spitzer S, Arditti A, Hellman C, Agmon J. Echocardiographic evaluation of patients with systemic sarcoidosis. Am Heart J. 1985;110:116–22.
Kul S, Ozcelik HK, Uyarel H, et al. Diagnostic value of strain echocardiography, galectin-3, and tenascin-C levels for the identification of patients with pulmonary and cardiac sarcoidosis. Lung. 2014;192:533–42.
Shah BN, De Villa M, Khattar RS, Senior R. Imaging cardiac sarcoidosis: the incremental benefit of speckle tracking echocardiography. Echocardiography. 2013;30:E213–4.
Bulkley BH, Rouleau JR, Whitaker JQ, Strauss HW, Pitt B. The use of 201thallium for myocardial perfusion imaging in sarcoid heart disease. Chest. 1977;72:27–32.
Le Guludec D, Menad F, Faraggi M, Weinmann P, Battesti JP, Valeyre D. Myocardial sarcoidosis. Clinical value of technetium-99m sestamibi tomoscintigraphy. Chest. 1994;106:1675–82.
Kaminaga T, Takeshita T, Yamauchi T, Kawamura H, Yasuda M. The role of iodine-123-labeled 15-(p-iodophenyl)-3R, S-methylpentadecanoic acid scintigraphy in the detection of local myocardial involvement of sarcoidosis. Int J Cardiol. 2004;94:99–103.
Kinney EL, Caldwell JW. Do thallium myocardial perfusion scan abnormalities predict survival in sarcoid patients without cardiac symptoms? Angiology. 1990;41:573–6.
Fields CL, Ossorio MA, Roy TM, Denny DM, Varga DW. Thallium-201 scintigraphy in the diagnosis and management of myocardial sarcoidosis. South Med J. 1990;83:339–42.
Haywood LJ, Sharma OP, Siegel ME, et al. Detection of myocardial sarcoidosis by thallium 201 imaging. J Natl Med Assoc. 1982;74:959–64.
Hirose Y, Ishida Y, Hayashida K, et al. Myocardial involvement in patients with sarcoidosis. An analysis of 75 patients. Clin Nucl Med. 1994;19:522–6.
Okayama K, Kurata C, Tawarahara K, Wakabayashi Y, Chida K, Sato A. Diagnostic and prognostic value of myocardial scintigraphy with thallium-201 and gallium-67 in cardiac sarcoidosis. Chest. 1995;107:330–4.
Kiuchi S, Teraoka K, Koizumi K, Takazawa K, Yamashina A. Usefulness of late gadolinium enhancement combined with MRI and 67-Ga scintigraphy in the diagnosis of cardiac sarcoidosis and disease activity evaluation. Int J Cardiovasc Imaging. 2007;23:237–41.
Tadamura E, Yamamuro M, Kubo S, et al. Effectiveness of delayed enhanced MRI for identification of cardiac sarcoidosis: comparison with radionuclide imaging. AJR Am J Roentgenol. 2005;185:110–5.
Yamagishi H, Shirai N, Takagi M, et al. Identification of cardiac sarcoidosis with (13)N-NH(3)/(18)F-FDG PET. J Nucl Med Off Publ Soc Nucl Med. 2003;44:1030–6.
Langah R, Spicer K, Gebregziabher M, Gordon L. Effectiveness of prolonged fasting 18f-FDG PET-CT in the detection of cardiac sarcoidosis. J Nucl Cardiol Off Publ Am Soc Nucl Cardiol. 2009;16:801–10.
Ishimaru S, Tsujino I, Sakaue S, et al. Combination of 18F-fluoro-2-deoxyglucose positron emission tomography and magnetic resonance imaging in assessing cardiac sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis Off J WASOG World Assoc Sarcoidosis Other Granulomatous Disord. 2005;22:234–5.
Smedema JP, Truter R, de Klerk PA, Zaaiman L, White L, Doubell AF. Cardiac sarcoidosis evaluated with gadolinium-enhanced magnetic resonance and contrast-enhanced 64-slice computed tomography. Int J Cardiol. 2006;112:261–3.
Kanao S, Tadamura E, Yamamuro M, et al. Demonstration of cardiac involvement of sarcoidosis by contrast-enhanced multislice computed tomography and delayed-enhanced magnetic resonance imaging. J Comput Assist Tomogr. 2005;29:745–8.
Freeman AM, Curran-Everett D, Weinberger HD, et al. Predictors of cardiac sarcoidosis using commonly available cardiac studies. Am J Cardiol. 2013;112:280–5.
Schatka I, Bengel FM. Advanced imaging of cardiac sarcoidosis. J Nucl Med Off Publ Soc Nucl Med. 2014;55:99–106.
Yang Y, Safka K, Graham JJ, et al. Correlation of late gadolinium enhancement MRI and quantitative T2 measurement in cardiac sarcoidosis. J Magn Reson Imaging JMRI. 2014;39:609–16. Study assessing myocardial tissue characterization in systemic sarcoidosis finding CMR-LGE sensitive at detecting subtle myocardial lesions, and decreased T2 may reflect inactive phase of CS, providing a potential new method for monitoring disease activity or therapy.
Vignaux O. Cardiac sarcoidosis: spectrum of MRI features. AJR Am J Roentgenol. 2005;184:249–54.
Crouser ED, Ono C, Tran T, He X, Raman SV. Improved detection of cardiac sarcoidosis using magnetic resonance with myocardial T2 mapping. Am J Respir Crit Care Med. 2014;189:109–12.
Eitel I, Friedrich MG. T2-weighted cardiovascular magnetic resonance in acute cardiac disease. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2011;13:13.
Hamzeh NY, Wamboldt FS, Weinberger HD. Management of cardiac sarcoidosis in the United States: a Delphi study. Chest. 2012;141:154–62.
Smedema JP, Snoep G, van Kroonenburgh MP, et al. Cardiac involvement in patients with pulmonary sarcoidosis assessed at two university medical centers in the Netherlands. Chest. 2005;128:30–5.
Sharma S. Cardiac imaging in myocardial sarcoidosis and other cardiomyopathies. Curr Opin Pulm Med. 2009;15:507–12.
Steckman DA, Schneider PM, Schuller JL, et al. Utility of cardiac magnetic resonance imaging to differentiate cardiac sarcoidosis from arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. 2012;110:575–9. Clinically useful paper that compares and contrasts the charactersistic findings of ARVC and CS on CMR.
Vignaux O, Dhote R, Duboc D, et al. Clinical significance of myocardial magnetic resonance abnormalities in patients with sarcoidosis: a 1-year follow-up study. Chest. 2002;122:1895–901.
Shimada T, Shimada K, Sakane T, et al. Diagnosis of cardiac sarcoidosis and evaluation of the effects of steroid therapy by gadolinium-DTPA-enhanced magnetic resonance imaging. Am J Med. 2001;110:520–7.
Dhote R, Vignaux O, Blanche P, et al. Value of MRI for the diagnosis of cardiac involvement in sarcoidosis. Revue Med Interne / fondee par la Societe Nationale Francaise de Med Interne. 2003;24:151–7.
Youssef G, Leung E, Mylonas I, et al. The use of 18F-FDG PET in the diagnosis of cardiac sarcoidosis: a systematic review and metaanalysis including the Ontario experience. J Nucl Med Off Publ Soc Nucl Med. 2012;53:241–8. High diagnostic accuracy for (18)F-FDG PET seen in metaanalysis of 7 studies with total of 164 patients, suggesting potential value for diagnosis of CS, with pooled estimates for (18)F-FDG PET of 89 % sensitivity and 78 % specificity.
Okumura W, Iwasaki T, Toyama T, et al. Usefulness of fasting 18F-FDG PET in identification of cardiac sarcoidosis. J Nucl Med Off Publ Soc Nucl Med. 2004;45:1989–98.
Mc Ardle BA, Birnie DH, Klein R, et al. Is there an association between clinical presentation and the location and extent of myocardial involvement of cardiac sarcoidosis as assessed by (1)(8)F-fluorodoexyglucose positron emission tomography? Circ Cardiovasc Imaging. 2013;6:617–26. Study of 27 consecutive patients demonstrated that CS patients with VT displayed significantly higher FDG uptake when compared with those with AVB and asymptomatic controls.
Tahara N, Tahara A, Nitta Y, et al. Heterogeneous myocardial FDG uptake and the disease activity in cardiac sarcoidosis. J Am Coll Cardiol Img. 2010;3:1219–28.
Blankstein R, Osborne M, Naya M, et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol. 2014;63:329–36. Study of 118 patients demonstrating the prognostic value of FDG-PET in CS; the presence of focal PD and FDG uptake on cardiac PET identified patients at higher risk of death or VT.
Ishida Y, Yoshinaga K, Miyagawa M, et al. Recommendations for (18)F-fluorodeoxyglucose positron emission tomography imaging for cardiac sarcoidosis: Japanese Society of Nuclear Cardiology recommendations. Ann Nucl Med. 2014;28:393–403. Excellent review paper with current recmmendations on technical aspects of FDG-PET scanning and interpretation.
Kaneta T, Hakamatsuka T, Takanami K, et al. Evaluation of the relationship between physiological FDG uptake in the heart and age, blood glucose level, fasting period, and hospitalization. Ann Nucl Med. 2006;20:203–8.
Fukuchi K, Ohta H, Matsumura K, Ishida Y. Benign variations and incidental abnormalities of myocardial FDG uptake in the fasting state as encountered during routine oncology positron emission tomography studies. Br J Radiol. 2007;80:3–11.
Morooka M, Moroi M, Uno K, et al. Long fasting is effective in inhibiting physiological myocardial 18F-FDG uptake and for evaluating active lesions of cardiac sarcoidosis. EJNMMI Res. 2014;4:1.
Asmal AC, Leary WP, Thandroyen F, Botha J, Wattrus S. A dose–response study of the anticoagulant and lipolytic activities of heparin in normal subjects. Br J Clin Pharmacol. 1979;7:531–3.
Ahmadian A, Brogan A, Berman J, et al. Quantitative interpretation of FDG PET/CT with myocardial perfusion imaging increases diagnostic information in the evaluation of cardiac sarcoidosis. J Nucl Cardiol. 2014;21(5):925–39. Prospective study that assessed methods to quantify FDG uptake in CS; these were found to correlate with impaired LV systolic function, clinical events, and immunosuppression treatment.
Manabe O, Yoshinaga K, Ohira H, et al. Right ventricular (18)F-FDG uptake is an important indicator for cardiac involvement in patients with suspected cardiac sarcoidosis. Ann Nucl Med. 2014;28(7):656–63. Study of 59 patients showing that although FDG-PET RV uptake was less frequent in patients with CS, RV uptake was associated with greater number of LV-involved segments and met the JMHW diagnostic criteria more frequently, suggesting it may be useful in diagnosing cardiac involvement in sarcoidosis.
Osborne MT, Hulten EA, Singh A, et al. Reduction in (1)(8)F-fluorodeoxyglucose uptake on serial cardiac positron emission tomography is associated with improved left ventricular ejection fraction in patients with cardiac sarcoidosis. J Nucl Cardiol Off Publ Am Soc Nucl Cardiol. 2014;21:166–74. Longitudinal study of 23 patients with serial FDG-PET that suggests this may help guide titration of immunosuppressive therapy to improve or prevent heart failure in CS.
White JA, Rajchl M, Butler J, Thompson RT, Prato FS, Wisenberg G. Active cardiac sarcoidosis: first clinical experience of simultaneous positron emission tomography–magnetic resonance imaging for the diagnosis of cardiac disease. Circulation. 2013;127:e639–41.
Schneider S, Batrice A, Rischpler C, Eiber M, Ibrahim T, Nekolla SG. Utility of multimodal cardiac imaging with PET/MRI in cardiac sarcoidosis: implications for diagnosis, monitoring and treatment. Eur Heart J. 2014;35:312.
Wicks E, Menezes L, Pantazis A, et al. 135 Novel hybrid positron emission tomography—magnetic resonance (PET-MR) multi-modality inflammatory imaging has improved diagnostic accuracy for detecting cardiac sarcoidosis. Heart. 2014;100 Suppl 3:A80.
Acknowledgments
Rob S.B. Beanlands is a Career Investigator supported by the Heart and Stroke Foundation of Ontario (HFSO), the University of Ottawa Heart Institute (UOHI) Vered Chair in Cardiology and a Tier 1 University of Ottawa Chair in Cardiovascular Research. David Birnie is a Mid-career Investigator supported by the HSFO. Hiroshi Ohira was supported by the Molecular Function and Imaging HSFO Program Grant (#PRG6242); the University of Ottawa, Department of Medicine, the Hokkaido Heart Association Grant for Research and The University of Ottawa Heart Institute’s Whit & Heather Tucker Endowed Research Fellowship. The work has been supported in part by a research trial grant from the Ministry of Health and Long Term Care Research (Grant # 06374) for The Cardiac Sarcoidosis Cohort Study (CHASMCS). The project is in collaboration with the Canadian Cardiovascular Network of Ontario Working Group for Cardiac PET in collaboration with the PET Steering Committee of Ontario. This work has also been partially supported by IMAGE-HF (Imaging Modalities to Assist with Guiding Therapy and the Evaluation of Patients with Heart Failure; Canadian Institute of Health Research team grant no. CIF 99470).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Chadi Ayoub, Hiroshi Ohira, Alexander Dick, Eugene Leung, Pablo B. Nery, and David Birnie declare that they have no conflict of interest. Elena Pena has received lecture fees from GE Healthcare Canada. Rob S.B. Beanlands is a consultant and has received grant funding from Lantheus Medical Imaging, Jubilant DRAXImage (JDI) and GE Healthcare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiac PET, CT, and MRI
Rights and permissions
About this article
Cite this article
Ayoub, C., Pena, E., Ohira, H. et al. Advanced Imaging of Cardiac Sarcoidosis. Curr Cardiol Rep 17, 17 (2015). https://doi.org/10.1007/s11886-015-0572-1
Published:
DOI: https://doi.org/10.1007/s11886-015-0572-1