Abstract
There has been a dramatic shift in the manner in which blood pressure (BP) is measured to provide far more comprehensive clinical information than that provided by a single set of office BP readings. Extensive clinical and epidemiological research shows an important role of ambulatory BP monitoring (ABPM) in the management of hypertensive patients. A 24-h BP profile helps to determine the absence of nocturnal dipping status and evaluate BP control in patients on antihypertensive therapy. The ability to detect white-coat or masked hypertension is enhanced by ambulatory BP monitoring. In 2001, the Center for Medicare and Medicaid Services approved ABPM for reimbursement for the identification of patients with white-coat hypertension. In 2011, the National Institute for Health and Clinical Excellence (NICE) in the UK published guidelines that recommended the routine use of ABPM in all patients suspected of having hypertension. The European Society of Hypertension (ESH) 2013 guidelines also support greater use of ABPM in clinical practice. While the advantages of ABPM are apparent from a clinical perspective, its use should be considered in relation to its cost, the complexity of data evaluation, as well as patient inconvenience. In this review, we evaluate the clinical importance of ABPM, highlighting its role in the current management of hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blood pressure (BP) has been traditionally measured in the physician’s office for medical decision-making. With the advent of technology, options for BP monitoring have extended to home BP monitoring (HBPM) and ambulatory BP monitoring (ABPM). BP measured out of the office enhances the ability to detect white-coat and masked hypertension. It also enables evaluation of BP control in subjects on complex antihypertensive drug regimens and the presence or absence of nocturnal hypertension [1•]. Several national and international guidelines have recommended the use of HBPM as an adjunct to office BP monitoring for the management of hypertension, including the European Society of Hypertension [2••], the American Society of Hypertension (ASH) [3], the American Heart Association (AHA) [4], the British Hypertension Society [5], the World Health Organization-International Society of Hypertension [6], and the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) [7].
Prospective cohort studies have shown that 24-h BP measured by ABPM is a more robust predictor of cardiovascular risk due to hypertension than BP measured in doctor’s office [8, 9]. In 2001, the Center for Medicare and Medicaid Services approved ABPM for reimbursement only for the identification of patients with white-coat hypertension [10]. Routine use of ABPM for the initial diagnosis of hypertension has been recommended by the UK National Clinical Guideline Centre (NCGC) in their recent guidelines published in May 2011 [11]. The European Society of Hypertension (ESH) 2013 guidelines recommend that all individuals with grade (stage) I hypertension in the office at low or moderate total cardiovascular risk should be evaluated with out-of-office BP monitoring (ambulatory or home) to exclude white-coat hypertension and those who have high–normal office BP or normal BP with asymptomatic organ damage or who are at high total cardiovascular risk be evaluated similarly to exclude masked hypertension [12••, 13••]. In most parts of the USA and Europe, ABPM is generally offered only in centers that specialize in hypertension or cardiovascular medicine [14]. Due to the lack of availability of ABPM in primary care practice, self- or home BP monitoring is often recommended [15••]. Implementation of ABPM entails equipment, staffing, and training costs. Hence, the question of the need for ABPM for the diagnosis and management of patients on antihypertensive therapy often arises.
Limitations of BP Measurement in the Doctor’s Office
Diagnosis and monitoring of BP has traditionally been done by measurement of BP in the physician’s office. It is a valuable clinical examination tool if measured properly. However, in today’s busy practice of medicine, it may be impractical to carry out repeated measurements over a period of several minutes with ideal environmental conditions. Additionally, there is increasing evidence that the traditional office BP measurement may yield inadequate or misleading estimates of a patient’s true BP status. BP values may be affected by factors like incorrect BP-measuring techniques such as rapid cuff deflation and improper cuff or bladder size, improper training of medical staff, and observer bias such as terminal digit preference (Table 1). Office BP measurements typically provide a limited number of readings. Large variations in BP may be seen within a single visit and among different clinic visits [1•, 16]. Twenty to thirty-five percent of patients diagnosed with hypertension may demonstrate a “white-coat effect” or “isolated office hypertension,” an increase in BP only in the medical care setting [16]. Masked hypertension, defined as the presence of elevated BP values outside of the medical care environment with normal in-clinic BP levels, has also been demonstrated. Thus, office BP measurements may not be representative of the true pressure values in some individuals. It is also important to reassess the BP responsiveness when patients initiate or change antihypertensive therapy. Though it is generally done in the doctor’s office, out-of-office BP monitoring gives additional information on the trough and peak responses of antihypertensive medications and encourages self-management by patients who are able to do so.
Circadian Variation of Blood Pressure
Blood pressure and heart rate both exhibit a circadian pattern that has been shown to correlate with cardiovascular events, including both myocardial infarction and stroke [17]. Blood pressure during sleep is characterized by a low time period. This is followed by a post-awakening rise, which coincides with the transition from sleep to wakefulness, and a higher sustained span thereafter. The 24-h variation in BP occurs not only as a consequence of day–night or rest–activity but also due to alterations in behavior (such as activities, diet, and mental stress); environmental phenomena (such as ambient temperature); and endogenous circadian rhythms in neural, endocrine, and hemodynamic variables [18]. Shift workers are a classical example of the circadian periodicity of BP being synchronized with the sleep–wake cycle. A complete reversal of the BP rhythm is known to occur on the first occasion of a session of night shifts compared to daytime work hours [19]. These night workers demonstrate peak systolic BP (SBP) at about 11 p.m. and diastolic BP (DBP) at about 10 p.m. [20].
Clinical Importance of Nocturnal Blood Pressure
Reduction of about 10–30 % of blood pressure is observed during sleep relative to the awake period in majority of normotensive and hypertensive people. However, about 25–35 % of hypertensive patients (and probably a smaller proportion of normotensive people) have a lesser decline in nocturnal BP [21]. Non-dipping pattern, a reduced or absent decline in sleep BP (defined as less than 10 % decline), is more commonly seen in elderly population [22], in post-menopausal women [23], and in African–Americans [24]. This pattern is associated with increased target organ damage including left ventricular hypertrophy, albuminuria, and microvascular disease of the brain [25–27]. Patients with a non-dipping pattern are thus more prone to congestive heart failure, myocardial infarction, stroke, and progression to end-stage renal failure. Studies have consistently shown associations of blunted declines in sleep BP with increased incidence of fatal and non-fatal CV events [9, 28–30]. The conventional clinic BP measurements and the threshold of SBP/DBP of ≥140/90 mmHg used to diagnose hypertension do not take into consideration the circadian pattern in BP and corresponding increases in CV risk associated with non-dipping. Current recommendations for ambulatory BP measurements provide separate reference thresholds for daytime (135/85 mmHg) and nighttime spans (120/70 mmHg) while proposing the threshold value of 130/80 mmHg for 24-h SBP/DBP means [12••, 13••, 14]. This allows for better control of BP with adjustment of dose and timing of anti-hypertensive medications accordingly [12••].
The degree of dipping of BP at night is influenced by sleep quality and depth. Since the reproducibility of the nocturnal decline in BP is observed to be poor in some studies, nocturnal hypertension may be more appropriately defined with an absolute BP value, rather than a proportional reduction in BP [31–33]. Isolated nocturnal hypertension may be present in 7 % of hypertensive subjects and can only be diagnosed with ambulatory BP monitoring [27]. There is evidence that nocturnal BP is superior to daytime BP in predicting outcome [9, 34]. Isolated nocturnal hypertension predicted cardiovascular outcomes in a recent study from the International Database on Ambulatory Monitoring and Cardiovascular Outcomes (IDACO) [27]. However, the possibility of confounding needs to be kept in mind since many subjects with reduced or absent nocturnal dipping frequently are older, diabetics, obese, or have overt cardiovascular or renal disease [35–39]. This suggests that an absolute nocturnal BP may be a better parameter to evaluate the efficacy of antihypertensive agents in comparison to the proportional change in BP during sleep.
Clinical Importance of Early Morning Hypertension
An inappropriate rise in BP and heart rate may be observed in the morning upon awakening. This early morning hypertension is typically due to a “surge” pattern characterized by an exaggerated rate of rise of BP upon awakening or the “non-dipper/riser” pattern due to the reversal of the normal nocturnal decline in BP. A small increase in the morning BP (<15 mmHg) may be physiological while larger increase is likely to be pathological. Higher rates of cardiovascular events such as myocardial infarction, stroke, and sudden death have been observed in association with early morning rise in BP in various epidemiologic studies [40–48]. Some of these events may be due to plaque vulnerability because of prothrombotic state, increased coagulability, and reduced fibrinolysis observed in early morning [40]. Acute myocardial infarction is more commonly seen between 6 a.m. and noon than at other times of the day or night [41]. In addition, the highest incidence rates of subarachnoid hemorrhage [42], ischemic stroke [43], hemorrhagic stroke [44], and transient ischemic attacks [45] are also observed in the first few hours post-awakening.
Long-term prospective studies have demonstrated the importance of early morning BP surge in predicting vascular events. Kario and coworkers conducted a prospective cohort study in 519 older Japanese patients with systolic hypertension with 41 months of follow-up and observed that for each 10 mmHg increase in baseline early morning SBP, the relative risk of stroke increased by 22 % [46]. Using ambulatory BP monitoring, the early morning BP surge was defined as the difference between the average SBP during the 2 h after awakening minus the average SBP during the 1 h that included the lowest sleeping SBP. Patients with a surge of ≥55 mmHg (top decile) showed a twofold higher risk of multiple lacunar infarctions after matching for age and the 24-h BP (57 vs. 33 %; P < 0.001) as compared to patients with no surge (average morning SBP increase of 9 mmHg). Another population-based study of 1430 people with a 10-year follow-up period showed that a large early morning BP surge was associated with the development of hemorrhagic stroke (P = 0.04) [47]. A meta-analysis by Li et al. reports that a greater than 90th percentile morning surge in BP is a significant and independent predictor of mortality and cardiovascular events [48].
Treatment that controls BP throughout the early morning hours is desirable, since it reduces the risk associated with the morning BP [49]. One of the approaches is to provide treatment that remains effective for all 24 h of the dosing period. Combining long-acting antihypertensive agents with short-acting agents given at bedtime may be another approach to provide optimal therapy for non-dipping patients with morning BP surge. In one prospective study, Hermida et al. demonstrated that using bedtime antihypertensive treatment improved 24-h BP control and reduced cardiovascular morbidity and mortality in patients with hypertension and type 2 diabetes [50]. It is often impractical and difficult to obtain multiple readings at different times of the day (and with relation to the dosing interval) in the outpatient medical care environment. Early morning BP, thus, can be more easily assessed and treated with the use of out-of-office monitoring.
Utility of Ambulatory BP Monitoring to Evaluate White-Coat Hypertension and White-Coat Effect
One of the major advantages of ambulatory BP monitoring is the ability to identify patients who have high BP readings in the medical care setting but normal readings during usual daily activities. The traditional definition of white-coat hypertension in untreated patients or a white-coat effect in treated patients is based on an elevated office BP ≥ 140 mmHg systolic and/or ≥90 mmHg diastolic with a mean awake ambulatory BP < 135/85 mmHg in untreated individuals. However, as mentioned in the previous section, since nocturnal BP is recognized to be superior to daytime BP in predicting cardiovascular risk, the latest guidelines and position papers propose including patients with office BP ≥ 140/90 mmHg and a mean 24-h BP < 130/80 mmHg [12••, 13••]. The white-coat effect is the rise in BP in a medical care environment regardless of the mean ambulatory BP value while being administered antihypertensive medications [13••]. Patients with office BPs ≥ 20 mmHg systolic or 10 mmHg diastolic higher than the awake ambulatory BP are labeled as having a clinically important white-coat effect [51]. The white-coat effect is an important cause of pseudo-resistant hypertension and highlights the importance of ambulatory BP monitoring in clinical settings where white-coat hypertension or effect are suspected.
White-coat hypertension, seen more common in the elderly, has a better prognosis than that for patients with sustained hypertension outside of the clinical environment [8, 9, 14]. In some clinical outcome studies, patients with white-coat hypertension (WCH) may have a slightly increased cardiovascular risk compared with normotensive individuals, though in most of the studies showing this effect, the ambulatory BP of the white-coat hypertension patients was higher than that in normotensive individuals [52–56]. The risk of developing sustained hypertension later in life may also be increased in patients with white-coat hypertension [54, 56]. In a meta-analysis performed by the IDACO group, patients with white-coat hypertension did not show an increase in cardiovascular events. However, there was a significant increase in risk in specific subgroups, including men and patients with diabetes [55]. The IDACO meta-analysis showed that any increased risk of future cardiovascular event in a patient with white-coat hypertension was very small and substantially lower than the risk seen with either persistent hypertension or masked hypertension.
Several hypertension guidelines recommend ambulatory BP measurement in situations where white-coat hypertension is suspected based on those patients with high office BP who report normal self-measured BP values [2••, 7]. In fact, this scenario is one of the primary indications for ambulatory BP monitoring recognized for approval by Centers for Medicare and Medicaid Services in the USA [10]. Hypertensive patients under evaluation for inadequate control of BP are observed to be better controlled when more carefully assessed by home or ambulatory BP recordings [57]. Hence, ambulatory BP monitoring may prevent excessive or unnecessary antihypertensive therapies in patients with white-coat effect. Patients with WCH may develop increased adverse effects of antihypertensive medications that are prescribed unnecessarily. Moreover, failure to identify WCH/WCE may have social consequences as patients may be penalized for employment and insurance policies. Ambulatory BP monitoring has been shown to be cost-effective as it reduces health care expenditures in terms of decreasing physician visits, drug costs, and management of adverse effects due to inappropriate treatment [58]. It is recommended that patients with WCH should have the diagnosis confirmed in about 6 months and be followed at yearly or biannual intervals with ambulatory BP or home BP monitoring [12••, 58].
Assessment of Masked Hypertension
Masked hypertension is present in patients with normal BP levels in the doctor’s office but elevated BP values outside of the medical care environment [59]. The prevalence of masked hypertension may be as high as 10–30 % among normotensive or prehypertensive patients [60, 61]. The cardiovascular risks associated with masked hypertension are similar to as seen in patients with sustained hypertension [52, 53, 61, 62]. A study by Stergiou et al. showed that ambulatory BP monitoring detects more patients with masked hypertension than home BP monitoring [60]. In another study by Viera and coworkers, masked hypertension was shown to have moderate reproducibility with ambulatory BP monitoring, favoring the hypothesis that office BP measurements may systematically fail to identify patients who should be treated as hypertensive [63•]. Home BP monitoring has not been found to be adequate for detecting this phenomenon. Despite this discrepancy, a recent meta-analysis concluded that the prognostic impact of masked hypertension is not affected by the different out-of-office BP methods used to detect its presence [64]. Hence, even though ambulatory BP monitoring is the gold standard for diagnosing masked hypertension, self- or home BP monitoring is a reasonable substitute when ambulatory BP monitoring is either not available or not feasible due to any reason [1•, 65].
Cardiovascular Risk Assessment
The utility of ambulatory BP monitoring has also been increasing in patients with primary hypertension [1•, 2••, 3]. Extensive data from multiple prospective clinical and population-based studies over the last four decades has consistently shown the predictive capability of ambulatory BP for cardiovascular events after adjustment for in-clinic BP values [66–68]. A seminal prospective cohort study by Perloff and Sokolow established that cardiovascular risk was greater in patients with higher daytime ambulatory BP than in those with lower daytime value, independent of the office BP values [66]. Ambulatory systolic BP in the elderly during the nighttime period was a better predictor of cardiovascular complications than clinic systolic BP in one of the placebo-controlled analyses from Syst-Eur trial [67, 68]. The Dublin Outcome Study that followed more than 5000 hypertensive patients for 5 years also showed that the nighttime BP was a superior predictor of cardiovascular mortality than the daytime BP [9]. While the 24-h mean BP is a better predictor of cardiovascular outcome than clinic BP, the use of the two methods together may increase the ability of BP to predict outcome [69].
Many clinical trials of ambulatory BP monitoring involved subjects who were untreated for hypertension. Hence, the effect of initiation or stopping of antihypertensive therapy to predict future cardiovascular events could not be determined in these cohorts. The Office versus Ambulatory Blood Pressure Study assessed the association between the ambulatory BP and future CV events in 1963 subjects on chronic antihypertensive therapy for a median duration of 5 years [8]. New CV events were documented in 157 patients. Elevated 24-h mean SBP and DBP were observed to be independent risk factors for CV events after adjusting for variables such as age, sex, smoking status, presence of diabetes mellitus, body mass index, use of lipid-lowering drugs, history of CV events, and clinic BP. After adjusting for office BP, the relative risk of CV events in patients with a mean 24-h systolic BP of 135 mmHg or higher was 1.74 when compared with patients with mean 24-h systolic BP <135 mmHg.
Ambulatory BP has also shown to be a better predictor of kidney outcomes when compared to clinic BP. Ambulatory BP and, in particular, nighttime BP were the strongest predictors of renal and cardiovascular risk in a study of 436 patients with non-dialysis chronic kidney disease. In contrast, office measurement of BP was less informative on prognosis, suggesting that ambulatory BP monitoring is of greater clinical utility in this high-risk population [70•].
Benefits of Using Ambulatory BP Monitoring in the General Evaluation and Treatment of Hypertension
Clinical evidence from more than 35 years of research demonstrates that ambulatory BP predicts cardiac, renal, and cerebrovascular events better than office BP in a variety of populations [16, 71]. Poor correlation between clinic BP measurements and 24-h mean ambulatory BP is often observed in patients, especially in men, both before and after initiation of antihypertensive treatment. The observation of higher CV event rate in patients with “normal” clinic systolic BP but a higher ambulatory systolic BP compared to patients with normal clinic and ambulatory BP values is a matter of concern [8]. Several such clinical studies suggest that ambulatory BP may be a better modality to manage hypertensive patients, especially those with high cardiovascular risk.
Usefulness of Ambulatory Monitoring of the Blood Pressure to Evaluate Therapy
Ambulatory BP monitoring plays an important role in the evaluation of drug efficacy. It may provide useful information on the pharmacokinetics and pharmacodynamics of antihypertensive agents that can aid in clinical management of the patients [71–73]. In a prospective study of >2000 patients, Hermida et al. studied the differential reduction of CV morbidity and mortality by a bedtime versus early morning hypertension treatment [74•]. Subjects ingesting medication at bedtime demonstrated lower nocturnal BP, reduced prevalence of non-dipping, and higher prevalence of ambulatory BP control. After a median follow-up of 5.6 years, significantly lower relative risk of CV events was observed in patients who were administered ≥1 antihypertensive medication at bedtime (odds ratio, 0.39 [95 % CI, 0.29–0.51]).
The importance of ambulatory BP monitoring in detecting pharmacological effects that would have been difficult to reproduce with conventional BP measurement has been shown in various studies using both the modalities [1•]. Marked attenuation in placebo effects of drugs on BP and white-coat reactions are observed with ABPM compared to clinical measurements. This reduces the magnitude of treatment-induced BP changes with ambulatory BP compared to office BP measurement. The pharmacodynamic effects of antihypertensive therapies and their effects on nighttime BP as well as BP variability are evaluated much more comprehensively with the use of ambulatory BP monitoring versus clinic BP measurements [73, 75].
Contrasting Home BP Monitoring to Clinic and Ambulatory BP Measurement
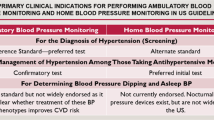
Both ambulatory and home BP play a complementary role in the management of hypertension. Ambulatory BP monitoring has the advantage of providing information on an individual’s BP status beyond what can be obtained using home BP such as nocturnal BP [1•]. However, it has its shortcomings too. It involves higher cost of the equipment. Training of the staff and data evaluation further adds to the cost of ABPM. Moreover, it is more inconvenient to the patient, hence cannot be done routinely. Pickering and White developed an algorithm on behalf of the American Society of Hypertension to guide toward the appropriate use of ambulatory BP monitoring in patients who would benefit from antihypertensive therapy (Fig. 1) [1•].
Algorithm for use of self (home) blood pressure monitoring and ambulatory blood pressure monitoring in the management of patients with hypertension. (Modified with permission from [1•]
Home BP measurements by the patient can provide targeted readings in their natural environment representative of their average daily pressure and detect white-coat or masked hypertension. Perhaps most importantly, using home BP monitoring encourages the patients to take active participation in their own care [76, 77].
A good correlation is observed between home BP readings and markers of hypertensive end-organ damage such as left ventricular hypertrophy, albuminuria, and carotid intimal–medial thickness [78–82]. Like ABPM, home BP has also shown to be a better predictor of future CV events than clinic BP [80, 81]. The PAMELA study showed incremental increase in cardiovascular mortality with a rise in ambulatory BP, followed by home and then office BP [81]. This reinforces the concept that 24-h ambulatory BP may be a better predictor of CV risk as it reflects various aspects of BP profile that may go undetected by other types of BP measurements such as circadian BP variability, the morning surge of BP, and the nocturnal dipping [26]. In the study by Viera et al., higher sensitivity and specificity of daytime ABPM–office pairing was observed compared to home BP monitoring, suggesting that ambulatory BP measurements are more suitable for detecting masked hypertension [63•].
When home BP monitoring is used for the diagnosis of hypertension, it is recommended that patients take two consecutive measurements at least 1 min apart in a seated position and record BP twice daily, ideally in the morning and evening prior to ingesting antihypertensive medication. BP should be recorded for at least 4 days, ideally for 7 days. The measurements taken on the first day should be discarded and the average value of all the remaining measurements should be used to confirm a diagnosis of hypertension or assess response to treatment. It should be noted that even at the end of this relatively demanding routine, patients still have no information related to the level of the nighttime BP, which is a sensitive predictor of CV outcome, particularly stroke [9]. Other important limitations of home BP measurement include inaccurate measurements and confounding due to reporting bias. Accurate BP values during physical activity or mental stress may not be reflected by home BP, as the readings are generally taken by the patients during periods of relative inactivity. Compared to home BP, ABPM has the advantage of obtaining a more comprehensive view of BP behavior during activities of usual daily life.
Ambulatory BP Monitoring in Clinical Practice
In the USA, ambulatory BP monitoring is relatively restricted to centers specializing in hypertension or cardiovascular medicine [15••]. ABPM is clinically indicated for the detection of masked and white-coat hypertension and assessment of response to antihypertensive therapy in patients on complicated antihypertensive regimens. Ambulatory BP monitoring is more accurate and cost-effective than office BP monitoring for confirming the diagnosis of hypertension. In the recently published guidelines for the clinical management of primary hypertension in adults, The National Clinical Guideline Centre (NCGC) in the UK recommends the routine use of ambulatory BP monitoring to confirm the initial diagnosis of hypertension and use home BP monitoring protocols when ABPM is not tolerated [14]. Since ABPM predicts future CV events better than clinic BP, drug treatment can be targeted to patients most likely to benefit [39, 68]. Also, inappropriate drug treatment in patients with white-coat effect is reduced with the use of ABPM [65].
Despite the National Institute for Health and Clinical Excellence (NICE) recommendations noted above, in some instances, ambulatory BP monitoring would not be an appropriate initial option. This is true for a patient with severe hypertension and a clinic BP ≥ 180/110 mmHg with or without target organ injury. In such a case, antihypertensive drug treatment should be initiated immediately in patients with less severe hypertension but, with overt target-organ damage, cardiovascular disease, and renal disease, it would be reasonable to start antihypertensive drug therapy on their initial diagnosis of hypertension without proceeding to ABPM. In primary care settings where ABPM may not be available, self- or home BP monitoring could provide an alternative to ambulatory BP monitoring in such cases [65].
Conclusion
Ambulatory BP monitoring (ABPM), with its distinct advantages, has gradually become established in the diagnosis and management of patients with hypertension [83]. It provides an accurate reflection of the circadian variation of BP and assists substantially in the detection of masked and white-coat hypertension and assessment of response to antihypertensive therapy in patients on complicated antihypertensive regimens. Multiple studies have confirmed the prognostic value of ABPM as having the strongest predictor of cardiovascular events in patients with hypertension. During the past decade, several international guidelines have endorsed the use of ambulatory BP monitoring for initial diagnosis of hypertension. Home (or self) BP monitoring may be used as an alternative when ambulatory BP is unavailable or cannot be tolerated by the patient. Novel technological advancements in the ABPM technology and interpretative software could reduce its cost and may further lead to the acceptance of its use for the diagnosis and management of hypertension.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pickering TG, White WB. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2010;4:56–61. Consensus document on clinical and practical recommendations for using home and ambulatory blood pressure monitoring.
Mancia G, Fagard R, Narkiewicz K, Task Force Members, et al. 2013 ESH/ ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357. Consensus guidelines document of the ESH/ESC on management of hypertension.
Pickering T. Recommendations for the use of home (self) and ambulatory blood pressure monitoring. American Society of Hypertension Ad Hoc Panel. Am J Hypertens. 1996;9:1–11.
Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716.
Williams B, Poulter NR, Brown MJ, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens. 2004;18:139–85.
World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens 1999, 17:151–183.
Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–15.
Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61.
CMS.gov. Centers for Medicare & Medicaid Services. Medicare coverage policy decisions. ABPM monitoring (#CAG-00067N). 2001. http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=5&NcaName=Ambulatory+Blood+Pressure+Monitoring&ver=9&from=%252527lmrpstate%252527&contractor=22&name=CIGNA+Government+Services+(05535)+-+Carrier&letter_range=4&bc=gCAAAAAAIAAA. Assessed July 1 2014.
National Institute for Health and Clinical Excellence (NICE). Hypertension: the clinical management of primary hypertension in adults. Clinical Guideline 127. 2011. www.nice.org.uk/guidance/CG127. Assessed July 1 2014.
O’Brien E, Parati G, Stergiou G, The European Society of Hypertension Working Group on Blood Pressure Monitoring, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–67. Consensus document on fundamentals and recommendations for ABPM.
O’Brien E, Parati G, Stergiou G, et al. Ambulatory blood pressure measurement: what is the international consensus? Hypertension. 2013;62:988–94. Summary of the consensus document of ESH emphasizing clinically relevant issues in the use of ABPM.
Bloch MJ, Basile JN. New British guidelines mandate ambulatory blood pressure monitoring to diagnose hypertension in all patients: not ready for prime time in the United States. J Clin Hypertens (Greenwich). 2011;13:785–6.
Krause T, Lovibond K, Caulfield M, et al. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. An important summary of the updated NICE guidelines on the management of hypertension and one of the first evidence to support using ambulatory blood pressure monitoring in clinical practice.
White WB. Ambulatory blood-pressure monitoring in clinical practice. N Engl J Med. 2003;348:2377–8.
White WB. Circadian variation of blood pressure: clinical relevance and implications for cardiovascular chronotherapeutics. Blood Press Monit. 1997;2:47–51.
Hermida RC, Smolensky MH, Ayala DE, et al. 2013 Ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Chronobiol Int. 2013;30:3,355–410.
Sundberg S, Kohvakka A, Gordin A. Rapid reversal of circadian blood pressure rhythm in shift workers. J Hypertens. 1988;6:393–6.
Sternberg H, Rosenthal T, Shamiss A, Green M. Altered circadian rhythm of blood pressure in shift workers. J Hum Hypertens. 1995;9:349–53.
White WB, Mansoor GA, Tendler BE, Anwar YA. Nocturnal blood pressure epidemiology, determinants, and effects of antihypertensive therapy. Blood Press Monit. 1998;3:43–51.
Di Iorio A, Marini E, Lupinetti M, Zito M, Abate G. Blood pressure rhythm and prevalence of vascular events in hypertensive subjects. Age Ageing. 1999;28:23–8.
Sherwood A, Thurston R, Steffen P, et al. Blunted nighttime blood pressure dipping in postmenopausal women. Am J Hypertens. 2001;14:749–54.
Harshfield GA, Hwang C, Grim CE. Circadian variation of blood pressure in blacks: influence of age, gender and activity. J Hum Hypertens. 1990;4:43–7.
Cuspidi C, Giudici V, Negri F, Sala C. Nocturnal nondipping and left ventricular hypertrophy in hypertension: an updated review. Expert Rev Cardiovasc Ther. 2010;8:781–92.
Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–74.
Fan HQ, Li Y, Thijs L, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010;28:2036–45.
Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Brotman DJ, Davidson MB, Boumitri M, et al. Impaired diurnal blood pressure variation and all-cause mortality. Am J Hypertens. 2008;21:92–7.
Hermida RC, Ayala DE, Fernandez JR, et al. Sleep-time blood pressure: prognostic value and relevance as a therapeutic target for cardiovascular risk reduction. Chronobiol Int. 2013;30:68–86.
White WB, Larocca GM. Improving the utility of the nocturnal hypertension definition by using absolute sleep blood pressure rather than the “dipping” proportion. Am J Cardiol. 2003;92:1439–41.
Mochizuki Y, Okutani M, Donfeng Y, et al. Limited reproducibility of circadian variation in blood pressure dippers and nondippers. Am J Hypertens. 1998;11:403–9.
Omboni S, Parati G, Palatini P, et al. Reproducibility and clinical value of nocturnal hypotension: prospective evidence from the SAMPLE study. Study on Ambulatory Monitoring of Pressure and Lisinopril Evaluation. J Hypertens. 1998;16:733–8.
Ohkubo T, Hozawa A, Yamaguchi J, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. Hypertension. 2002;20:2183–9.
Gorostidi M, Sobrino J, Segura J, et al. Ambulatory blood pressure monitoring in hypertensive patients with high cardiovascular risk: a cross-sectional analysis of a 20,000-patient database in Spain. J Hypertens. 2007;25:977–84.
de la Sierra A, Segura J, Gorostidi M, et al. Diurnal blood pressure variation, risk categories and antihypertensive treatment. Hypertens Res. 2010;33:767–71.
de la Sierra A, Redon J, Banegas JR, et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466–72.
Cuspidi C, Macca G, Sampieri L, et al. Target organ damage and non-dipping pattern defined by two sessions of ambulatory blood pressure monitoring in recently diagnosed essential hypertensive patients. J Hypertens. 2001;19:1539–45.
Verdecchia P. Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension. 2000;35:844–51.
Kario K, White WB. Early morning hypertension: what does it contribute to overall cardiovascular risk assessment? J Am Soc Hypertens. 2008;2:397–402.
White WB. Cardiovascular risk and therapeutic intervention for the early morning surge in blood pressure and heart rate. Blood Press Monit. 2001;6:63–72.
Wroe SJ, Sandercock P, Bamford J, et al. Diurnal variation in incidence of stroke: Oxfordshire community stroke project. BMJ. 1992;304:155–7.
Elliott WJ. Circadian variation in the timing of stroke onset: a meta-analysis. Stroke. 1998;29:992–6.
Casetta I, Granieri E, Portaluppi F, Manfredini R. Circadian variability in hemorrhagic stroke. JAMA. 2002;287:1266–7.
Gallerani M, Manfredini R, Ricci L, et al. Chronobiological aspects of acute cerebrovascular diseases. Acta Neurol Scand. 1993;87:482–7.
Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6.
Metoki H, Ohkubo T, Kikuya M, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149–54.
Li Y, Thijs L, Hansen TW, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8.
White WB. Importance of blood pressure control over a 24-hour period. J Manag Care Pharm. 2007;13(Suppl B):34–9.
Hermida RC, Ayala DE, Mojon A, et al. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care. 2011;34:1270–6.
Myers MG, Reeves RA. White coat phenomenon in patients receiving antihypertensive therapy. Am J Hypertens. 1991;4:844–9.
Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25:2193–8.
Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24:52–8.
Mancia G, Bombelli M, Facchetti R, et al. Long term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009;54:226–32.
Franklin SS, Thijs L, Hansen TW, International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators, et al. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension. 2012;59:564–71.
Bjorklund K, Lind L, Vessby B, et al. Different metabolic predictors of white-coat and sustained hypertension over a 20-year follow-up period: a population-based study of elderly men. Circulation. 2002;106:63–8.
Sander GE, Giles TD. Resistant hypertension: concepts and approach to management. Curr Hypertens Rep. 2011;13:347–55.
O’Brien E, Coats A, Owens P, et al. Use and interpretation of ambulatory blood pressure monitoring; recommendations of the British Hypertension Society. BMJ. 2000;320:1128–34.
Yano Y, Bakris GL. Recognition and management of masked hypertension: a review and novel approach. J Am Soc Hypertens. 2013;7:244–52.
Stergiou GS, Salgami EV, Tzamouranis DG, Roussias LG. Masked hypertension assessed by ambulatory blood pressure versus home blood pressure monitoring: is it the same phenomenon? Am J Hypertens. 2005;18:772–8.
Pickering T, Davidson K, Gerin W, et al. Masked hypertension. Hypertension. 2002;40:795–6.
Liu JE, Roman MJ, Pini R, et al. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med. 1999;131:564–72.
Viera AJ, Hinderliter AL, Kshirsagar AV, Fine J, Dominik R. Reproducibility of masked hypertension in adults with untreated borderline office blood pressure: comparison of ambulatory and home monitoring. Am J Hypertens. 2010;23:1190–7. Illustrates that home blood pressure monitoring may not be adequate to detect masked hypertension.
Verberk WJ, Kessels AG, de Leeuw PW. Prevalence, causes, and consequences of masked hypertension: a meta-analysis. Am J Hypertens. 2008;21:969–75.
Hodgkinson J, Mant J, Martin U, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011;342:d3621.
Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressures. JAMA. 1983;249:2792–8.
Fagard RH, Staessen JA, Thijs L, et al. Response to antihypertensive therapy in older patients with sustained and nonsustained systolic hypertension. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Circulation. 2000;102:1139–44.
Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA. 1999;282:539–46.
Mancia G, Facchetti R, Bombelli M, et al. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension. 2006;47:846–53.
Minutolo R, Agarwal R, Borrelli S, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–8. Demonstrates the importance and utility of using ambulatory blood pressure monitoring in patients with chronic kidney disease as it relates to cardiovascular and renal outcomes.
Neutel JM. The importance of 24-h blood pressure control. Blood Press Monit. 2001;6:9–16.
White WB, Lacourciere Y, Davidai G. Effects of the angiotensin II receptor blockers telmisartan versus valsartan on the circadian variation of blood pressure: impact on the early morning period. Am J Hypertens. 2004;17:347–53.
O’Brien E. The value of 24-h blood pressure monitoring to assess the efficacy of antihypertensive drug treatment. Hot Topics Hypertens. 2011;4:7–23.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629–51. This article provides information on the effect of timing of hypertension treatment using ambulatory blood pressure monitoring and actigraphy.
Mancia G, Parati G. Office compared with ambulatory blood pressure in assessing response to antihypertensive treatment: a meta-analysis. J Hypertens. 2004;22:435–45.
Graves JW, Nash C, Burger K, Bailey K, Sheps SG. Clinical decision-making in hypertension using an automated (BpTRU) measurement device. J Hum Hypertens. 2003;17:823–7.
Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Am Soc Hypertens. 2008;2:192–202.
Mule G, Caimi G, Cottone S, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk. 2002;9:123–9.
Tachibana R, Tabara Y, Kondo I, Miki T, Kohara K. Home blood pressure is a better predictor of carotid atherosclerosis than office blood pressure in community-dwelling subjects. Hypertens Res. 2004;27:633–9.
Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5.
Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Agarwal R, Andersen MJ. Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int. 2006;69:406–11.
White WB, Maraka S. Is it possible to manage hypertension and evaluate therapy without ambulatory blood pressure monitoring? Curr Hypertens Rep. 2012;14:366–73.
Compliance with Ethics Guidelines
Conflict of Interest
William B. White and Vinay Gulati declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Hypertension
Rights and permissions
About this article
Cite this article
White, W.B., Gulati, V. Managing Hypertension with Ambulatory Blood Pressure Monitoring. Curr Cardiol Rep 17, 2 (2015). https://doi.org/10.1007/s11886-014-0556-6
Published:
DOI: https://doi.org/10.1007/s11886-014-0556-6