Abstract
Epidemiological data demonstrates that improved regulation of blood glucose correlates with better cardiovascular (CV) outcomes. Conversely, some interventional studies have demonstrated that tight glycemic control has no benefit or can even result in worse CV outcomes. These conclusions parallel the paradox that glycemic control has proven beneficial for microvascular outcomes, while few studies have demonstrated significant macrovascular benefits. This imprecise understanding conveys the need to better comprehend the mechanisms of glycemic control and its impact on CV disease. Such variations in data also require a more comprehensive approach to diabetes and CV disease in which multiple biomarkers such as low density lipoprotein (LDL), low adiponectin, elevated C-reactive protein (CRP) and well established clinical parameters such as high blood pressure, weight, and functional status are incorporated into clinical decision making. Reliance on one parameter in isolation such as glycemic control and one biomarker such as HbA1C does not provide an accurate assessment of CV outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
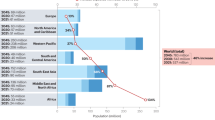
Type 2 diabetes (T2D) is one of the most commonly diagnosed illnesses worldwide. The prevalence of diabetes is growing at an alarming rate, it is estimated that 346 million people worldwide live with diabetes [1]. In the U.S alone 25.8 million Americans are affected by T2D, with 7 million of those cases still undiagnosed [2]. There is significant morbidity associated with diabetes, making it the 7th leading cause of death in the U.S [2].
Over the past two decades a variety of treatments have emerged to control blood glucose levels, and reduce or delay some of the detrimental impacts of this disease. While the American Diabetes Association (ADA) recommendations for HbA1C levels have remained around 7 %, dosage augmentation and combinational therapy have made it possible in some circumstances to significantly reduce blood glucose to near normal levels (~6.0 % HbA1C). This has provoked research studies to assess whether “intensive glycemic regulation” would reduce microvascular (neuropathy, retinopathy, nephropathy) and macrovascular (atherosclerosis, peripheral vascular disease, stroke) risks more than conventional treatment measures aimed at 7.0 % HbA1C. The United Kingdom Prospective Diabetes Study (UKPDS) was able to show a significant link between intensive glucose control and a decreased risk of microvascular outcomes (p = 0.0099), supported by later epidemiological studies [3, 4]. This result was validated by another randomized clinical trial (RCT), ADVANCE [5]. While these studies have reported risk reductions in microvascular outcomes with intensive regulation, the link between glycemic control and macrovascular outcomes has yet to be established. Single macrovascular endpoints have approached significance, such as myocardial infarction in UKPDS, but overall benefit remains non-significant across recent studies [3, 6]. Conflicting evidence, non-significant results, and protocol differences among the studies have prevented a solid conclusion from being made (Table 1). Part of this issue is the lack of consistency in defining what is meant by “tight” or intensive glycemic control and who constitutes the optimal patient population for such intervention. Thus, the current treatment recommendations of the ADA remain at an HbA1C of ≤7.0 % [12].
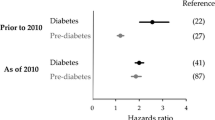
While diabetes raises the risk of many life-threatening illnesses, heart disease and stroke are the leading causes of death among diabetics, motivating the American Heart Association to label diabetes as one of the six major controllable risk factors for prevention of cardiovascular disease [13]. However, the impact of glycemic control is still not fully understood. Indirect benefit of glycemic control has been suggested through the reduction of microvascular outcomes associated with glycemic control, but recent interventional studies have yet to show overall cardiovascular macrovascular benefits of tight glycemic control [5, 7••, 14]. Furthermore, epidemiological studies have demonstrated that tight glycemic control could pose risks to cardiovascular health in high CV risk individuals possibly through pathological hypoglycemic events [7••, 8••, 9, 15]. This incomplete understanding ultimately necessitates further research into the effects of glycemia on microvascular and macrovascular disease onset (Fig. 1), as well as the precise mechanisms of hyperglycemia and hypoglycemia on cardiovascular outcomes. It is hypothesized that because microvascular disease occurs later in the course of disease and is a direct manifestation of glucose toxicity that tight control of blood sugars improves these outcomes [21]. In contrast, macrovascular diseases begin earlier in the course of diabetes, even before disease onset, and there are multiple mechanisms including inflammation, lipid oxidation, and platelet reactivity that contribute to its pathogenesis, and thus glycemic control alone may not fully impact outcomes [21]. To fully understand the impact of macrovascular disease, multiple biomarkers that reflect the complexity of macrovascular disease such as LDL, CRP and adiponectin need to be examined along with HbA1C.
Review of Studies Illustrating the Benefits of Tight Glycemic Control
Interventional
United Kingdom Prospective Diabetes Study (UKPDS)
The United Kingdom Prospective Diabetes Study was the first large-scale, longitudinal study to follow individuals diagnosed with T2D. The interventional period ranged from 1977–1991 and patients were followed post interventionally for a median of 10 years [4]. Participants had a median age of 53 years, were newly diagnosed with T2D, and exclusionary criteria included myocardial infarction in the previous year, current angina or heart failure, or more than one previous vascular event [3]. The 4209 participants were divided into four cohorts: two “intensive therapy” groups, which utilized sulfonylureas with possible combination insulin, or metformin alone to lower glycated hemoglobin levels. Each intensive therapy group was then compared against a standard, “conventional therapy” cohort which continued dietary therapy in the absence of drugs. For sulfonylurea vs. conventional therapy, the intensive control group started with an HbA1C of 7.05 %, while the dietary therapy cohort had a median baseline HbA1C of 7.09 % [3]. In the metformin vs conventional therapy study, the intensive therapy metformin study group started with a median HbA1C of 7.3 %; the dietary therapy group median baseline HbA1C was 7.1 % [22]. Over 10 years, tight glycemic control with sulfonylureas achieved a median HbA1C level of 7.0 %, while the conventional therapy group limited levels to a median of 7.9 % [22]. Similarly, metformin-regulated tight glycemic control achieved an HbA1C level of 7.4 % vs. 8.0 % in the dietary control group [23].
Significant results of the sulfonylurea-insulin group include a 25 % decrease in risk of microvascular endpoints in the intensive therapy group versus conventional therapy (HR 0.75, CI 0.60–0.93, p = 0.0099) [3]. With regard to single endpoints, only a decreased risk in retinal photocoagulation was observed (HR 0.71, CI = 0.53–0.98, p = 0.0031). For the metformin cohort, there were significant risk reductions for any diabetes-related endpoint, diabetes-related deaths, and all-cause mortality (p ≤ 0.017 for all outcomes) [22]. No conclusive evidence could be drawn about other outcomes, though decreased risk of myocardial infarction approached significance in the sulfonylurea group (p = 0.052) [3]. There was no evidence found for differences in other macrovascular endpoints [3]. Overall, the study suggests that glycemic regulation has beneficial effects in reducing diabetic endpoints and microvascular disease, but plays little role in risk reduction of macrovascular end-points.
Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE)
ADVANCE was an international study, conducted from 2003–2008, to assess blood pressure regulation and glycemic control on microvascular and macrovascular disease. Median age was 66 years and all participants were considered at-risk for vascular events, including myocardial infarction, stroke, or unstable angina [24]. Over 11,140 participants were divided into two intensive therapy groups: one receiving perindopril/indapamide combinational therapy for blood pressure lowering, the other received the sulfonylurea gliclazide to intensively-regulate glycemic levels [24]. Each intensive therapy group was compared against a standard therapy group utilizing conventional therapy. Intensive glycemic regulation aimed for HbA1C levels at or below 6.5 %, and permitted additional treatments if necessary, to reach the desired A1C level [5]. The standard and intensive glycemic regulation groups had a mean A1C of 7.5 % at the start of the trial and over a median of 5 years of treatment, levels had receded to 7.3 % in the standard group and 6.5 % in the intensive treatment group [9]. Significant results in the intensive treatment group included microvascular risk reduction of 14 % (HR 0.86, CI 0.77–0.97, p = 0.01) with increased hypoglycemic events (HR 1.86, CI 1.42–2.40, p < 0.001) [9]. Intensive glycemic control also resulted in decreased systolic blood pressure, but with increased weight gain with respect to the standard therapy group (p < 0.001 for both outcomes) [5]. There was no significant difference between overall mortality rates of the group, or macrovascular end-points, despite the maintained glycemic differences by the different therapies [9]. The intensive therapy cohort experienced a nonsignificant decrease in cardiovascular mortality (12 %), though it was suggested that microvascular benefits could contribute to overall better cardiovascular outcomes [5].
Epidemiological
Several longitudinal epidemiological studies have utilized UKPDS data to draw conclusions about the effects of glycemic control on long-term mortality and development of cardiovascular disease [10, 25, 26]. In the ten-year follow up UKPDS study both conventional and intensive study cohorts were monitored after participants were released from commitment to their pre-prescribed therapies [4]. Participants were asked to attend UKPDS clinics for 5 years, and were monitored by annual questionnaires if not able to attend the clinics. Notable was the long-term maintenance of microvascular risk reduction of the sulfonylurea intensive therapy group compared to the standard treatment group (p = 0.001, HR 0.76, CI 0.64–0.89), despite the disappearance of glycemic differences between the two groups [4]. Additionally, the intensive glycemic control group showed significant relative risk decreases in any diabetes-related outcomes (p = 0.04), myocardial infarction (p = 0.01) and death from any cause (p = 0.007) [4]. The maintenance of risk reduction despite eventual increases in HbA1C is notable, and the results suggest that there may be legacy benefits of prior glycemic control that become more apparent over longer periods of time [3, 4].
Review of Studies that Suggest Detrimental or Insignificant Outcomes of Tight Glycemic Regulation
Interventional
Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study
The ACCORD study was a long-term, interventional study aimed at assessing cardiovascular impacts of tight glycemic control. Over 10,251 participants, with a median years of 62.2, and a median 9.0 years after initial diagnosis, were randomized and followed from 2003–2009 [27]. The study assigned participants to either a standard therapy group which targeted an HbA1C of 7.0 %–7.9 % or intensive therapy group aimed for normoglycemic levels of <6.0 % HbA1C [8••]. The groups were then randomized to receive either standard or intensive blood pressure regulation therapy, or lipid regulation therapy, with a statin plus either fenofibrate or placebo for intensive and standard therapy groups respectively. Intensive therapy treatment was terminated mid study due to increased mortality [28]. This is consistent with data from the point of intensive therapy termination, where death from any cause in the intensive-therapy group was 21 % higher (HR 1.46, CI 1.02–1.44, p = 0.036) [8••]. At the point of termination of intensive glycemic regulation nonfatal myocardial infarctions were lower in the intensive therapy group, a trend that maintained significance until the end of the study (p = 0.01 for both time points) [8••]. However, death from cardiovascular causes was higher in the intensive therapy group at the end of the study (p < 0.02) [14]. The increased mortality can be attributed to the study cohort’s baseline cardiovascular risk, as well as median duration of diabetes of 10 years, which has been implicated as a key factor in retrospective studies [29, 30].
Veterans Affairs Diabetes Trial (VADT)
The VADT was a five-year study aimed to assess cardiovascular effects of intensive glycemic regulation in T2Ds at high CV risk. Over 1791 participants were enrolled by 2003 and divided into intensive control and standard control cohorts [7••]. Participants were a mean 60 years of age, 97 % males, with a protocol-necessitated HbA1C > 7.5 % [7••]. Exclusion criteria included congestive heart failure, severe angina, or the occurrence of a cardiovascular event six months before study enrollment [31]. Both groups utilized the same pharmaceutical measures, but different dosage prescription aimed to generate an HbA1C difference of at least 1.5 % between the groups, and the intensive group attempted to achieve near normal levels of HbA1C [31]. The standard therapy and intensive therapy cohorts started with mean baseline HbA1C levels of 9.4 % and reduced these levels to 8.4 % in standard therapy and 6.9 % in intensive therapy over the five-year study period [7••]. There were no significant differences in microvascular events between the groups, nor significant differences in any of the primary and secondary outcomes, which included myocardial infarction, stroke, death from cardiovascular cause, congestive heart failure, and death from any cause. One retrospective study examined coronary artery calcification (CAC) and aortic artery calcification (ACC) specifically, and demonstrated no significant difference in progression of these pathologies between intensive therapy and standard therapy groups, though a similar retrospective analysis showed a significant reduction (p = 0.03) in cardiovascular events in the intensive therapy group among participants with lower baseline CAC [32, 33]. Significant results hinged upon differences in hypoglycemic events. Over eight separate measurements, the intensive therapy group scored significantly higher in the number of events (p < 0.001), including hypoglycemic events with symptoms, of which the standard therapy group experiences 383 events per 100 patient years, while the intensive therapy group experienced 1333 hypoglycemic events over the follow-up period (p < 0.001) [7••]. Ultimately, there was no relative decrease in cardiovascular outcomes for the intensive therapy group [7••].
Epidemiological
Retrospective epidemiological analyses have been conducted using the ADVANCE patient data as well. One study examined the correlations between hypoglycemic events and microvascular, macrovascular, and cardiovascular outcomes and found clear increases in severe hypoglycemic events (blood glucose <2.8 mmol/L) in the intensive therapy glycemic control group (HR 1.86 CI 1.40–2.40) [34]. Adjusting for co-variability (i.e., gender, disease duration, treatment, and risk factors), after one severe hypoglycemic event there was increased instances of macrovascular events (HR 3.45 CI 2.34–5.08 p < 0.001), microvascular events (HR 2.07, CI 1.32–3.26, p < 0.001), and death from cardiovascular cause (HR 3.78, CI 2.34–6.11, p < 0.001) [34]. The association between intensive glucose regulation and hypoglycemia from this study suggests intensive glycemic regulation is a predictor for increased vulnerability to microvascular, macrovascular, and adverse cardiovascular outcomes illustrated in other studies [27, 33].
Review of Antihyperglycemia Treatments on Cardiovascular Outcomes
With the advent of new drugs to treat T2D over the past decades, physicians now have greater ability to tailor individual treatment plans to better regulate hyperglycemia (Table 2). Consequently, this poses a dilemma for physicians who are now responsible for determining the best individualized treatment and motivates researchers to explore the effects of these drugs alone and in combination [75]. Of the 18.8 million individuals being treated for T2D, 58 % of individuals use oral medication(s) alone, while 14 % use a combination of insulin and oral medication, and 12 % are on insulin alone [2]. Similarly, VADT, ACCORD, ADVANCE, and UKPDS employed both monotherapy and a variety of available drugs based on HbA1C aims. Different drugs, alone or in combination, have retrospectively correlated with different microvascular and macrovascular outcomes (Table 2).
Biguanides
The most common biguanide currently prescribed is metformin. The metabolic effects of metformin which include increased insulin sensitivity and decreased hepatic glucose production are felt to be responsible for beneficial cardiovascular outcomes. In the UKPDS, metformin was shown to have greater relative risk reductions than the other drug treatments in any diabetes-related endpoint, all-cause mortality, and stroke (p ≤ 0.32 for all measures) [22]. Furthermore, in a recent meta-analysis of several RCTs metformin was linked to lower cardiovascular morbidity and mortality with respect to sulfonylurea-monotherapy [35].
Thiazolidinediones (TZDs)
Thiazolidinediones (TZDs), pioglitazone and rosiglitazone, decrease blood glucose levels by increasing insulin sensitivity, and insulin-mediated glucose uptake into insulin-sensitive tissues (skeletal muscle, adipose tissue, etc.) [36]. In 2005, the RCT PROactive demonstrated the cardiovascular safety of Pioglitazone with decreased risk of stroke, all-cause mortality, and non-fatal myocardial infarction versus a placebo in 5238 individuals (HR 0.84 CI 0.72–0.98, p = 0.027) [37]. Aleglitazar, the newest TZD in development, has shown moderate decreases in markers of inflammation, blood pressure, LDL-C and triglycerides in a study of 332 patients [38]. Despite clinical trial data showing non-inferiority of Rosiglitazone, another TZD, meta-analyses have revealed the possibility of CV risk associated with this drug, causing it to be withdrawn from use in Europe and provoking the FDA to place strict limitations on its use [39–42].
Sulfonylureas
Sulfonylureas encompass the bulk of antihyperglycemic drugs currently available to treat T2D. Previously, there was fear that first-generation sulfonylureas could lead to increased cardiac mortality but this is not supported by recent data [3, 5, 43]. The UKPDS determined that there was no significant difference in risk of myocardial infarction, diabetes-related death, nor sudden death between the sulfonylurea and dietary treatment groups [3, 4]. ADVANCE also employed an intensive control therapy using the sulfonylurea gliclazide (Dimircon MR) [24]. All differences in cardiovascular, macrovascular, and mortality end-points were nonsignificant but generally favored the intensive therapy group, which had a 12 % nonsignificant reduction in cardiovascular outcomes [5]. Fear of the cardiovascular risks of these drugs seems to have diminished, but significant cardiovascular benefits have yet to be demonstrated.
Non-Sulfonylurea Secretagogues
Non-sulfonylurea secretagogues or meglitinides, include repaglinide and nateglinide. Meglitinides have increased affinity for pancreatic B-cell channels, suggesting minimal cardiovascular impact [44]. One interventional study assessing postprandial hyperglycemia in 175 patients showed significant carotid intima-media thickness decreases and greater reductions in C-reactive protein in patients taking repaglinide versus the sulfonylurea glyburide (p = 0.02) [45]. In an attempt to determine the broad cardiovascular impact of meglitinides the NAVIGATOR study assessed major cardiovascular outcomes of 9306 individuals taking nateglinide versus placebo treatment, but found no significant differences between the groups [46].
α-Glucosidase Inhibitors
α-Glucosidase inhibitors include miglitol, voglibose, and acarbose. Recently, a meta-analysis linked these drugs to lower levels of triglycerides, body weight, and systolic blood pressure [47]. A small, interventional study of 50 patients demonstrated that miglitol reduced inflammatory markers and improved endothelial dysfunction in patients with coronary artery disease with respect to voglibose [48]. A large multi-center trial enrolled 1429 patients and demonstrated a significant reduction in risk of myocardial infarction (HR 0.09 CI 0.01–0.72, p = 0.02) and new cases of hypertension (HR 0.66, CI 0.49–0.89, p = 0.006) among α-Glucosidase inhibitors versus a placebo, though, flaws in study design have called these results into question [49, 50]. These drugs are beneficial due to minimal weight gain and their ability to regress prediabetics back to normoglycemic levels [36]. To ascertain the effects of α-Glucosidase inhibitors on cardiovascular outcomes a multi-center trial, Acarbose Cardiovascular Evaluation (ACE), is currently underway with results expected in 2016 [51].
(GLP-1) Agonists
Glucagonlike peptide-1 (GLP-1) agonists, such as exenatide and liraglutide, stimulate glucose dependent insulin secretion [50]. Despite a lack of large clinical trial data, many smaller RCTs suggest that prolonging GLP-1 activity may have cardiovascular benefits. The precise mechanisms are unknown, but given that GLP-1 receptors are expressed throughout cardiac and endothelial tissue, it is possible that GLP-1 activation can have direct beneficial effects [52]. A small interventional study of 21 patients showed that short-term GLP-1 infusion in non-diabetic patients undergoing percutaneous coronary intervention improved left ventricular ejection fraction and wall motion score index [53]. This was demonstrated by a similar study of long-term GLP-1 treatment in 12 patients with chronic heart failure [54]. The impact of GLP-1 on endothelial function was illustrated by a small experimental study of ten patients with T2D and stable coronary artery disease that received acute administration of GLP-1, resulting in increased peripheral blood flow [55]. Additionally, a number of animal studies have demonstrated cardioprotective effects of GLP-1 through infarct size minimization and recovery enhancement [56–59]. Reduced hypoglycemia and cardiovascular benefits make these drugs promising for treatment of individuals with diabetes at increased risk of macrovascular disease.
Dipeptidyl Peptidase IV (DPP-4) Inhibitors (Gliptins)
Available DPP-4 inhibitors include saxagliptin, sitagliptin, linagliptin, and vildagliptin (approved outside of US). In a retrospective analysis of cardiovascular outcomes of saxagliptin versus a placebo treatment in 4607 patients in registration studies, patients taking saxagliptin has decreased risk of CV events (HR 0.44, CI 0.24–0.82) [60]. Meta-analyses of phase II/III trials suggest cardiovascular benefits, and clinical CV event trials are now underway to validate the risk reductions of DPP-4 inhibitors [61–65].
Insulin
There are varied insulin treatment options for hyperglycemia. Short-acting regular insulin can be injected for rapid blood glucose decreases, although short-acting insulin analogs (Lispro, Aspart, Glulisine) are prescribed more readily, given their ability to dissociate more quickly into subunits, causing a faster increase in plasma insulin with respect to regular insulin [36]. Additionally, they result in less hypoglycemic episodes and modest reductions in HbA1C levels. Conversely, long-acting insulin analogs such as isophane/NPH, glargine, and detemir, result in slower degradation due to slower subunit dissociation [66]. This causes a less pronounced, but prolonged increase in blood insulin levels. Compared to other treatments for hyperglycemia, clinical trial data illustrates increased episodes of hypoglycemia and weight gain from insulin use, possibly indicating that insulin can increase microvascular and macrovascular risks in an indirect manner [3, 5]. Indeed epidemiological studies have shown significant increases in mortality among individuals using insulin compared to those utilizing other treatments [67–69]. Some large (n > 12,000 patients ) studies have also linked insulin use to significant increases in cardiovascular risk [69, 70]. While these studies suggest increased insulin use is related to adverse cardiovascular events, these correlations may neglect baseline characteristics of individuals more likely to utilize insulin as treatment, such as age or duration of diabetes, that could independently affect their risks of experiencing cardiovascular events [71]. Furthermore, a recent interventional study of 12,537 individuals compared insulin glargine treatment versus conventional treatment and determined no increase in cardiovascular risk with use of insulin [72]. The classes of insulin therapy have also been studied to determine if there are any differences in outcomes among the groups. An interventional trial utilizing biphasic insulin aspart, prandial insulin aspart, and basal insulin detemir to assess risks of hypoglycemia and other adverse effects in 708 participants found significantly increased hypoglycemic events in the basal insulin detemir cohort with respect to the other groups, but no differences in cardiovascular events [73, 74]. These studies as a whole suggest that insulin dosing should be closely regulated in diabetic treatment to minimize any potential negative cardiovascular outcomes.
HbA1C in not the Optimal Biomarker
Diabetes is a complex disease and at a molecular level thought to be due to impairments of insulin secretion and resistance, cellular bioenergetics and mitochondrial dysfunction [76]. Biomarkers combined with diagnostic tests such as assessment of endothelial dysfunction can provide insight into these fundamental derangements at the cellular level and may provide a better assessment of disease progression and patient outcomes. HbA1C is a biomarker that represents the “tip of the iceberg” and just one facet of the metabolic problem in diabetes but does not capture the complex problems with cellular bioenergetics. Using a multi modal approach with multiple biomarkers and diagnostic tests may provide a better understanding of the impact of diabetes. Numerous clinical trials have shown the danger of examining one biomarker such as HDL in isolation without looking at the entire lipid profile [77]. Novel biomarkers such as soluble receptor for advanced glycation end products (sRAGE), glycated albumin, urinary 8-hydroxydeoxyguanosine (8-OHdG) may eventually be more accurate in predicting macrovascular disease and onset of events [78, 79•, 80]. Ultimately there may need to be a new risk score for diabetes devised such as the Framingham risk score that incorporates multiple clinical parameters to accurately predict CV outcomes. While the UKPDS risk engine remains a recommended model from which to predict CV risk, particularly for lower-risk individuals, studies continue to illustrate both its suboptimal discrimination and calibration ultimately leading to an overestimation of CV risk [81–83].
Conclusion: Making Sense of the Paradox
Numerous studies have explored potential explanations for the observed differences in microvascular and macrovascular outcomes of glycemic regulation. Meta-analyses, which simultaneously analyze multiple cohorts of data, may reveal further insight, but often neglect heterogeneity between the studies. Demographic differences in patient populations, variable controls and randomization methods, and differing statistical analyses can often lead to nonsignificant results that may not accurately reflect the impact of glycemic regulation on cardiovascular outcomes. Even with many large, randomized clinical trials aimed at resolving this issue, there are still no significant results demonstrating macrovascular impacts of tight glycemic control. From these studies data trends and correlations have been drawn, but underlying mechanisms of hyperglycemia, hyperinsulinemia, and factors impacting CV disease progression are not well understood. In the future, utilization of more sophisticated biomarkers that examine fundamental pathophysiologic problems at the cellular level combined with diagnostic tests that assess multiple facets of the disease process will hopefully provide a better understanding of the true impact of glycemic control on cardiovascular outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Diabetes factsheet 312. In: World Health Organization. 2011. http://who.int/mediacentre/factsheets/fs312/en/index.html. Accessed 20 July 2012.
National Diabetes Factsheet. In: Center for Disease Control. 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf . Accessed 17 Jul 2012.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil AW. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Hellar SR. A summary of the ADVANCE trial. Diabetes Care. 2009;32:S357–61.
Zoungas S, Galan BE, Ninomiya T, et al. Combined effects of routine blood pressure lowering and intensive glucose control on macrovascular and microvascular outcomes in patients with type 2 diabetes. Diabetes Care. 2009;32:2068–74.
•• Duckworth W, Abraira C, Mortiz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39. A comprehensive summary of VADT aims, methods, and results.
•• Gerstein HC, Miller ME, Genuth S, et al. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 2011;364:818–28. A comprehensive summary of ACCORD trial aims, methods, and results.
Patel A, MacMahon S, Chalmers J. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Adler AI, Levy JC, Matthews DR, et al. Insulin sensitivity at diagnosis of Type 2 diabetes is not associated with subsequent cardiovascular disease (UKPDS 67). Diabet Med. 2005;22:206–11.
Ismail-Beigi F, Craven T, Baneni MA. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomized trial. Lancet. 2010;276:419–30.
Checking your blood glucose. In: American Diabetes Association. http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/checking-your-blood-glucose.html. Accessed 17 July 2012.
Cardiovascular Disease and Diabetes. In: American Heart Association. http://www.heart.org/HEARTORG/Conditions/Diabetes/WhyDiabetesMatters/Cardiovascular-Disease-Diabetes_UCM_313865_Article.jsp. Accessed 27 Jul 2012.
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemic and risks of vascular events and death. N Engl J Med. 2010;363:1410–8.
Kendall DM, Cuddihy RM, Bergenstal RM. Clinical application of incretin-based therapy: therapeutic potential, patient selection and clinical use. Am J Med. 2009;122(6 Suppl):S37–50.
Kendall DM, Bergenstal RM. Comprehensive management of patients with type 2 diabetes: establishing priorities of care. Am J Manag Care. 2001;7(10 Suppl):S327–43.
Skyler JS. Diabetic complications. The importance of glucose control. Endocrinol Metab Clin North Am. 1996;25:243–54.
DCCT study group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329:977–86.
Stratton IM, Adler AI, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–12.
Grundy SM. Pre-diabetes, metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2012;59:635–43.
UK Prospective Diabetes Study Group. Effects of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:845–65.
American Diabetes Association. Implications of the United Kingdom prospective diabetes study. Diabetes Care. 2002;25(S1):S28–32.
ADVANCE Collaborative Group. ADVANCE—Action in Diabetes and Vascular disease: patient recruitment and characteristics of the study population at baseline. Diabet Med. 2005;22:882–8.
Adler AI, Neil HA, Manley SE, et al. Hyperglycemia and hyperinsulinemia at diagnosis of diabetes and their association with subsequent cardiovascular disease in the United Kingdon prospective diabetes study (UKPDS 47). Am Heart J. 1999;138:S353–9.
Colaqiuri S, Cull CA, Holman RR, UKPDS group. Are lower fasting plasma glucose levels at diagnosis of type 2 diabetes associated with improved outcomes?: U.K. prospective diabetes study 61. Diabetes Care. 2002;25:1410–7.
The ACCORD study group. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol. 2007;99:21i–33i.
Riddle MC, Ambrousius WT, Brillon DJ, et al. Epidemiological relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care. 2010;33:983–90.
Genuth S, Ismail-Beigi F. Clinical implications of the ACCORD trial. J Clin Endocrinol Metab. 2012;97:41–8.
Terry T, Raravikar K. Does aggressive glycemic control benefit macrovascular and microvascular disease in type 2 diabetes?: insights from ACCORD, ADVANCE, and VADT. Curr Cardiol Rep. 2012;14:79–88.
Abraira C, Duckworth W, McCarren M, et al. Design of the cooperative study on glycemic control and complications in diabetes mellitus type 2 veterans affairs diabetes trial. J Diabetes Complications. 2003;17:314–22.
Saremi A, Moritz TE, Anderson RJ. Rates and determinants of coronary and abdominal aortic artery calcium progression in the veterans affairs diabetes trial (VADT). Diabetes Care. 2012;33:1642–7.
Reaven PD, Moritz TE, Schwenke DC. Intensive glucose-lowering therapy reduces cardiovascular disease events in veterans affairs diabetes trial participants with lower calcified coronary atherosclerosis. Diabetes. 2009;58:2642–8.
Zoungas S, Patel A, Chalmers J, et al. Sever hypoglycemia and risks of vascular events and death. N Engl J Med. 2010;163:1410–8.
Qaseem A, Humphrey LL, Sweet DE, et al. Oral pharmacologic treatment of type 2 diabetes mellitus: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2012;156:218–31.
Powers AC, D’Alessio D. Endocrine pancreas and pharmacotherapy of diabetes mellitus and hypoglycemia. In: Brunton L, Chabner B, Knollman B, editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 12th ed. USA: McGraw-Hill Companies; 2012. p. 1237–74.
Dormandy JA, Charbonnel B, Eckland DJ, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomized clinical trial. Lancet. 2005;366:1279–89.
Henry RR, Lincoff AM, Mudaliar S, et al. Effect of the duel peroxisome profilerator-activated receptor-alpha/gamma agonist aleglitazar on risk of cardiovascular disease in patients with type 2 diabetes (SYNCHRONY): a phase II randomized, dose-ranging study. Lancet. 2009;374:126–35.
Home PD, Pocock SJ, Beck-Nielsen H, et al. Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicenter, randomized, open-label trial. Lancet. 2009;373:2125–35.
Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356:2457–71.
European Medicines Agency recommends suspension of Avandia, Avandamet and Avaglim. In: European Medicines Agency. http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2010/09/WC500096996.pdf. Accessed 1 August 2012.
FDA Drug safety website. http://www.fda.gov/Drugs/DrugSafety/ucm255005.htm#Safety_Announcement. Accessed 18 Jul 2012.
Leibel B. An analysis of the University Group Diabetes Study Program: data results and conclusions. Can Med Assoc J. 1971;105(105):292–4.
Stephan D, Winkler M, Kuhner P, et al. Selectivity of repaglinide and glibenclamide for the pancreatic over the cardiovascular K(ATP) channels. Diabetologia. 2006;49:2039–48.
Esposito K, Giugliano D, Nappo F, et al. Regression of carotid atherosclerosis by control of postprandial hyperglycemia in type 2 diabetes mellitus. Circulation. 2004;110:214–9.
Holman RR, Haffner SM, McMurray JJ. Effect of nateglinide on the incidence of diabetes and cardiovascular events. N Engl J Med. 2010;362:1463–76.
Hanefeld M, Cagatau M, Petrowitsch, et al. Acarbose reduces the risk for myocardial infarction in type 2 diabetic patients: meta-analysis. Eur Heart J. 2004;25:10–6.
Emoto T, Sawada T, Hashimoto M, et al. Effect of 3-month repeated administration of Miglitol on vascular endothelial function in patients with diabetes mellitus and coronary artery disease. Am J Cardiol. 2012;109:42–6.
Chiasson JL, Josse RG, Gomis R, et al. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;23:486–94.
Kaiser T, Sawicki PT. Acarbose for prevention of diabetes, hypertension and cardiovascular events. A critical analysis of the STOP-NIDDM data. Diabetologia. 2004;47:575–80.
Acarbose Cardiovascular evaluation. In NIH Clinical Trials. 2012. NLM identifier: NCT00829660. http://clinicaltrials.gov/ct2/show/NCT00829660. Accessed 19 Jul 2012.
Grieve DJ, Cassidy RS, Green BD. Emerging cardiovascular actions of the incretin hormone glucagon-like peptide-1: potential therapeutic benefits beyond glycaemic control? Br J Pharmacol. 2009;157:1340–51.
Nikolaidis LA, Mankad S, Sokos GG, et al. Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation. 2004;109:962–5.
Sokos GG, Nikolaidis LA, Mankad S, et al. Glucagon-like peptide-1 infusion improves left ventricular ejection fraction and functional status in patients with chronic heart failure. J Card Fail. 2006;12:694–9.
Nystrom T, et al. Effect of glucagon-like peptide-1 on endothelial function in type 2 diabetes patients with stable coronary artery disease. Physiol Endocrinol Metab. 2004;287:E1209–15.
Noyan-Ashraf MH, Momen M, Ban K, et al. GLP-1R agonist liraglutide activates cytoprotective pathways and improves outcomes after experimental myocardial infarction in mice. Diabetes. 2009;58:975–83.
Nikolaidis LA, Elahi D, Hentosz T, et al. Recombinant glucagon-like peptide-1 increases myocardial glucose uptake and improves left ventricular performance in conscious dogs with pacing-induced dilated cardiomyopathy. Circulation. 2004;110:955–61.
Bose AK, Mocanu MM, Carr RD, et al. Glucagon-like peptide 1 can directly protect the heart against ischemia/reperfusion injury. Diabetes. 2005;54:146–51.
Hattori Y, Jojima T, Tomizawa A, et al. A glucagon-like peptide-1 (GLP-1) analogue, liraglutide, upregulates nitric oxide production and exerts anti-inflammatory action in endothelial cells. Diabetologia. 2010;53:2256–63.
Frederich R, Alexander JH, Fiedorek FT, et al. A systematic assessment of cardiovascular outcomes in the saxagliptin drug development program for type 2 diabetes. Postgrad Med. 2010;122:16–7.
Sitagliptin cardiovascular outcome study (TECOS). In: NIH Clinical Trials. NLM Identifier: NCT00790205. http://clinicaltrials.gov/ct2/show/NCT00790205?term=TECOS&rank=1. Accessed 20 July 2012.
CAROLINA: Cardiovascular Outcome Study of Linagliptin Versus Climepiride in Patients With Type 2 Diabetes. InL NIH Clinical Trials. NLM Identifier: NCT01243424. http://clinicaltrials.gov/ct2/show/NCT01243424?term=carolina+linagliptin&rank=1. Accessed 20 July 2012.
Cardiovascular Outcomes Study of Alogliptin in Subjects With Type 2 Diabetes and Acute Coronary Syndrome, (EXAMINE). In: NIH Clinical Trials. NLM Identifier: NCT00968708. http://clinicaltrials.gov/ct2/show/NCT00968708?term=Examine&rank=1. Accessed 20 July 2012.
Double blind placebo study of vildagliptin in prehypertensives type II diabetics (Prediab). In NIH Clinical Trials. NLM Identifier: NCT01001962. http://clinicaltrials.gov/ct2/show/NCT01001962?term=PREDIAB&rank=1. Accessed 20 July 2012.
Effects of vildagliptin on left ventricular function in patients with type 1 diabetes and congestive heart failure. In: NIH Clinical Trials. NLM identifier: NCT00894868. http://clinicaltrials.gov/ct2/show/NCT00894868?term=effect+of+vildagliptin+on+left+ventricular+function&rank=1. Accessed 20 July 2012.
Woodworth JR, Howey DC, Bowsher RR. Establishment of time-action profiles for regular and NPH insulin using pharmacodynamic modeling. Diabetes Care. 1994;17:64–9.
Anselmino M, Ohrvik J, Malmberg K, et al. Glucose lowering treatment in patients with coronary arter disease is prognostically important not only in established but also in newly detected diabetes mellitus: a report from the Euro Heart Survey on Diabetes and the Heart. Eur Heart J. 2008;29:177–84.
Smooke S, Horwich TB, Fonarow GC, et al. Insulin-treated diabetes is associated with a marked increase in mortality in patients with advanced heart failure. Am Heart J. 2005;149:168–74.
Currie CJ, Peters JR, Tynan A, et al. Survival as a function of Hba(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375:481–9.
Gamble JM, Simpson SH, Eurich DT, et al. Insulin use and increased risk of mortality in type 2 diabetes: a cohort study. Diabetes Obes Metab. 1987;12:47–53.
Rensing KL, Reuwer AQ, Arsenault BJ, et al. Reducing cardiovascular disease risk in patients with type 2 diabtes and concomitant macrovascular disease: can insulin be too much of a good thing? Diabetes Obes Metab. 2011;13:1073–87.
Gerstein HC, Bosch J, Dagenais GR. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012. doi:10.1056/NEJMoa1203858.
Holman RR, Thorne KI, Farmer AJ, et al. Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med. 2007;357:1716–30.
Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736–47.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemic in type 2 diabtes: A patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2012;55:1577–96.
Kim J, Wei Y, Sowers JR. Role of mitochondrial dysfunction in insulin resistance. Circ Res. 2008;102:401–14.
Boden WE, Probstfield JL, Anderson T, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255–67.
Lindsey JB, de Lemos JA, Cipollone F. Association between circulating soluble receptor for advanced glycation end products and atherosclerosis observations from the Dallas Heart Study. Diabetes Care. 2009;32:1218–20.
• Juraschek SP, Steffes MW, Miller 3rd ER, Selvin E. Alternative markers of hyperglucemia and risk of diabetes. Diabetes Care. 2012. doi:10.2337/dc12-0787. Illustrates the potential use of new biomarkers for diagnosing and treating diabetes.
Nishikawa T, Sasahara T, Kiritoshi S, et al. Evaulation of urinary 8-hydroxydeoxyguanosine as a novel biomarker of macrovascular complications in type 2 diabetes. Diabetes Care. 2003;26:1507–12.
NICE clinical guideline 87 – Type 2 diabetes. In: Type 2 diabetes. The management type 2 diabetes. National Institute for Health and Clinical Excellence. http://www.nice.org.uk/nicemedia/pdf/CG87NICEGuideline.pdf. Accessed 13 Sep 2012.
Simmons RK, Coleman RL, Price HC, et al. Performance of the UK Prospective Diabetes Study Risk Engine and the Framingham Risk Equations in estimating cardiovascular disease in the EPIC-Norfolk cohort. Diabetes Care. 2009;32:708–13.
van Dieren S, Peelen ML, Nothlings U, et al. External validation of the UK Prospective Diabetes Study (UKPDS) risk engine in patients with type 2 diabetes. Diabetologia. 2011;54:264–70.
Disclosure
Conflicts of interest P.R. Taub: none; E. Higginbotham: none; R.R. Henry: has board membership with Amylin Pharmaceuticals, Boehringer Ingelheim, Lilly Pharmaceuticals, Merck Pharmaceuticals, Novo Nordisk, Gilead Pharmaceuticals, Intarcia Pharmaceuticals; has been a consultant for Amgen Pharmaceuticals, Boehringer Ingelheim, Sanofi Aventis, Merck Pharmaceuticals, Gilead Pharmaceuticals, Isis Pharmaceuticals; has received grant support from Amylin Pharmaceuticals, Amgen Pharmaceuticals, Bristol Myers Squibb/AstraZeneca, Johnson & Johnson/Jenssen, Eli Lilly Pharmaceuticals, Sanofi Aventis; and has received payment for development of educational presentations including service on speakers’ bureaus from Boehringer Ingelheim/Lilly Pharmaceuticals
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Diabetes and Cardiovascular Disease
Rights and permissions
About this article
Cite this article
Taub, P.R., Higginbotham, E. & Henry, R.R. Beneficial and Detrimental Effects of Glycemic Control on Cardiovascular Disease in Type 2 Diabetes. Curr Cardiol Rep 15, 332 (2013). https://doi.org/10.1007/s11886-012-0332-4
Published:
DOI: https://doi.org/10.1007/s11886-012-0332-4