Abstract
Purpose of Review
Cardiovascular disease (CVD) is known to be an increasing cause of mortality among women, particularly postmenopausal women. Hormone replacement therapy (HRT) is a topic that has been investigated over the past decade for its known impact on the cardiovascular system. This review summarizes the evidence and current opinion on the associations between HRT and CVD, evidence both supporting and against HRT use as a prevention to the development of coronary heart disease (CHD).
Recent Findings
The majority of the new data available suggests the use of HRT has the potential to be more beneficial in the prevention of CVD if started in women at younger ages. Current studies also suggest that while starting HRT in older postmenopausal women may be associated with an initial slight increase in CVD, the overall lifetime occurrence rate is not increased. Several studies have also started to use the “timing hypothesis” to suggest that HRT initiated soon after menopause has the potential of being the greatest cardiovascular benefit to the patient. Overall, the data support the finding that HRT should be used only for symptomatic treatment, not in an attempt to slow progression of CVD.
Summary
Current evidence does not support the use of HRT for either primary or secondary prevention of CHD. HRT has different implications based on the temporal relationship in which it is initiated in relation to the onset of menopause. Overall, the use of HRT should be an individualized decision with each patient on the basis of the individual’s symptoms and overall risk profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) remains the leading cause of mortality for women both in the United States and throughout the world [1, 2]. There has been an increase in female-specific CVD research over the past 20 years in an effort to better understand the driving factors of coronary disease in women. Women are typically older than men at their first presentation for an acute coronary event, with an average age of 72 compared to 65 in men [1]. This difference suggests that women at younger ages have some protective factor that helps prevent CVD. It has been postulated that estrogens—through their effect on the vascular endothelium—serve as this protective factor [3]. Although the exact mechanism of action is largely unknown, estrogen does cause increased release of nitric oxide with resultant vasodilation; estrogen also affects prostaglandin synthesis and serves as an inhibitor of smooth muscle proliferation [4,5,6,7].
After menopause, women have a decline in circulating estrogen levels which is associated with an increase in atherosclerosis. The supplementation of estrogen after menopause remains a highly controversial and debated topic in the field of women’s health. There have been a multitude of studies done on the safety and efficacy of using hormone replacement therapy in postmenopausal women. In this article, the data surrounding the use of hormone replacement therapy in the prevention of cardiovascular disease in postmenopausal women will be examined and future challenges and prospects in this ever-evolving field will be highlighted.
Cardiovascular Effects of Estrogen
Many studies have investigated the effect of estrogens on the cardiovascular system and progression of heart disease [3,4,5,6,7]. Initial research demonstrated the majority of cardiovascular effects were associated with steroid receptors that, upon binding with estrogen, would function as transcription factors. One of these genes is the cardioactive nitric oxide synthase [5]. Through an increase of nitric oxide, estrogen works to regulate blood pressure and inhibit vascular smooth muscle proliferation.
Estrogens also act through the regulatory subunit of phosphatidylinositol-3-OH kinase, which leads to the activation of protein kinase B and endothelial nitric oxide synthase. These effects have been shown in animal models to lead to decreased leukocyte accumulation after an ischemic event and after reperfusion injuries. [8]
More recent research has investigated the effect of estrogen on the brain, as it relates to the cardiovascular system, specifically in regions that are known to regulate sympathetic activity and transducers of baro/chemoreceptors. Multiple studies have demonstrated a strong relationship between increased reactive oxygen species and increased vasomotor sympathetic tone [9,10,11].
Estrogen has also been shown to reduce cholesterol levels, particularly the low-density lipoprotein, through upregulation of the apolipoprotein B100 receptor [12]. Upregulation of this receptor also increases clearance of LDL from the circulation and theoretically decreases the likelihood that the LDL will become embedded in the subendothelial space. Estrogen has also been shown to increase hepatic synthesis of HDL [13].
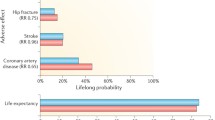
Women’s Health Initiative
The Women’s Health Initiative (WHI) was a randomized controlled trial (RCT) that enrolled women between the years of 1993 and 1998 in an attempt to assess the health consequences of hormone replacement therapy (HRT) [14]. The WHI included more than 25,000 women ages 50–79 on either estrogen alone or estrogen/progestin combination therapy. Women were followed for a total of 13 years. This study classified cardiovascular disease as an acute MI, silent MI, or CHD death. In the study arm of women with a uterus on the estrogen/progestin combination, CHD increased 80% in the first year but only 18% over the life of the treatment trial [14]. The WHI trial had an estrogen-therapy-only arm (ET) that included roughly 11,000 women aged 50 to 79 years who had a previous hysterectomy. Interestingly, estrogen monotherapy was not associated with an increase in coronary disease although there was an increased risk of stroke, and the initial WHI study reported no overall difference in CHD with the use of HRT. Post-trial subgroup analyses showed that women in their 50s fared better than older women with respect to cardiovascular outcomes. In the estrogen/progestin subgroup analysis, for every 10,000 women in their 50s who were treated over 1 year, there were five extra diagnoses of CHD versus 19 extra diagnoses for women in their 70s. These findings were not statistically significant as age affected absolute risk (older women expected to have more events). In the estrogen-only arm, for every 10,000 women in their 50s who were treated over 1 year, there were 11 fewer diagnoses of CHD compared to seven extra diagnoses in women in their 70s. The 40% reduction in heart attack became more significant when evaluated over the 13 years of follow-up. This reduction suggests that, for younger women without a uterus, estrogen alone may have a favorable and acceptable risk-versus-benefit profile. Both estrogen/progestin combination and estrogen only increased the risk of stroke and blood clots in the intervention phase but no appreciable diffrences noted in post-analysis [29].
The WHI Coronary Artery Calcium Study evaluated 1064 women aged 50–59 years who were previously enrolled in the ET arm of the WHI [15]. Because coronary atherosclerotic plaques have been associated with future CHD risk, the investigators used computed tomography heart imaging to determine the degree of coronary artery calcium burden. Coronary artery calcification scores were lower among those who received ET compared with those who received placebo (P = .03) and, if the medication regimen was adhered to for 5 or more years, ET use was associated with a significant reduction in the coronary artery calcification.
In a sub-study of the WHI, women in their 60s given conjugated equine estrogen immediately after bilateral oophorectomy were found to have a lower prevalence of coronary artery calcification (20) compared with women not given ET after oophorectomy [16]. Women who had prior use of ET before bilateral oophorectomy did not have higher prevalence of coronary artery calcium. The choice of the type of progestin may also affect the cardiovascular effects of HT. Synthetic medroxyprogesterone acetate is vasoconstrictive, while natural progesterone is known to have vasodilatory properties [17]. Natural progesterone has also been shown to have either a neutral or beneficial effect on blood pressure [18]. In contrast to most synthetic progestins, progesterone causes little or no reduction in high-density lipoprotein cholesterol levels [17] and has compared favorably in its effects on low-density lipoprotein cholesterol, low-density lipoprotein phospholipids, very low-density lipoprotein cholesterol, and very low-density lipoprotein triglycerides [19].
Additional Influential Randomized Control Trials
Between the years of 1990 and 1993, the Danish Osteoporosis Prevention Study looked at women who were treated with either estradiol or estradiol/norethisterone acetate for a total of 10 years, with 6 years of observational follow-up [20]. The study, among women receiving HRT early after progression into menopause, ultimately concluded that there was a significantly reduced risk of mortality, heart failure, and myocardial infarction.
A pilot study of the Women’s Health Initiative Exome Sequencing Project (WHISP) evaluated the effect of HRT among patients with known coronary heart disease. This trial enrolled women over the age of 55 at 2–28 days post-acute coronary syndrome. The patients were given either estradiol/norethisterone or placebo and followed for 12 months. The trial demonstrated a decrease in CHD events with no evidence of increased coagulation activation [21].
The Heart and Estrogen/Progestin Replacement Study (HERS) trial was a randomized, blinded, placebo–controlled trial followed by the randomized, unblinded follow-up trial (the HERS II trial) examining whether conjugated equine estrogen and medroxyprogesterone acetate altered CHD risk in patients with known CHD. After 4.1 years and subsequent 2.7 years of follow-up, respectively, these studies did not demonstrate a reduction in CHD risk. The women who received HRT had a 52% increased risk of CHD event in the first year. There was no difference in incidence of CHD events between the estrogen–progestin and placebo group in the HERS trial, despite a decrease in low-density lipoprotein (LDL) and an increase in high-density lipoprotein (HDL) in the experimental group [22, 23].
Meta-analyses/Cochrane Reviews
In 2009, a meta-analysis of observational and randomized control trials looking at the use of HRT was published and concluded that HRT decreased mortality of younger, postmenopausal women. This analysis demonstrated that HRT decreased the risk of coronary artery disease in younger (less than 10 years from menopause or < 60 years old) patients [23]. In agreement with this meta-analysis, a Cochrane review looked at all RCTs comparing HRT with placebo. The results were consistent in finding that the use of HRT in patients within 10 years of menopause onset was associated with a significantly decreased risk of CHD [24, 25•].
Common Themes
A common theme throughout the majority of previous research is the increased benefit of HRT when it is begun by women at a younger age. This has been called the “timing hypothesis.” This finding is potentially secondary to the lower risk of developing coronary plaque at a younger age and of allowing HRT to be more preventative secondary to mechanisms previously described. The aforementioned studies also demonstrate that the use of HRT in women who are further from onset of menopause might have an initial increase in CHD. However, this initial increase in CHD is not, in the long run, significantly associated with HRT.
Early vs Late Intervention Trial with Estradiol (ELITE), a single-center, randomized, double-blind, placebo-controlled trial demonstrated that women who received estradiol, rather than placebo, had lower rates of subclinical atherosclerosis progression, but only when therapy was started within 6 years after menopause [26•]. Healthy postmenopausal women without diabetes or clinical evidence of cardiovascular disease participated in the ELITE study. The women were randomly assigned to receive either oral 17 beta-estradiol or placebo. At the time of randomization, the women were stratified into two groups on the basis of their number of postmenopausal years. The early postmenopause group consisted of women who had reached menopause < 6 years before (median time since menopause: 3.5 years and median age: 55.4 years at enrollment). Women who were postmenopausal for ≥ 10 years were stratified to the late postmenopause group (median time since menopause: 14.3 years and median age: 63.6 years). Baseline carotid-artery intima-media thickness (CIMT) was measured in all women. The rate of change in CIMT was the trial’s primary outcome. The degree of coronary atherosclerosis measured by cardiac computer was a secondary end point. The results indicated that estradiol therapy, compared with placebo, was associated with less progression of CIMT in the early but not the late postmenopause group. Estradiol therapy had no significant effect on secondary outcomes—CT measures of coronary artery calcium, total stenosis, and total plaque—in either group [27].
The Kronos Early Estrogen Prevention Study (KEEPS) examined the effect of two estrogen plus progesterone regimens, compared to placebo, on atherosclerosis progression in 727 healthy women aged 42 to 58 years who were within 3 years of their final menstrual period at the trial’s enrollment. The intervention groups received either low-dose oral conjugated estrogens at 45 mg/d or transdermal 17-beta-estradiol (t-E2) at 50 mcg/d for 4 years, plus 200 mg of oral progesterone for 12 days [28]. Neither regimen had any significant positive or negative effect on CIMT progression.
Conculsions
Menopausal HT should not be used for the primary or secondary prevention of CHD at the present time. Recent analyses suggest that HT does not increase CHD risk for healthy women who have recently experienced menopause. This explanation, known as the “timing hypothesis,” asserts that initiation of hormone replacement therapy soon after menopause—when women’s hearts are younger and their coronary arteries are more receptive to the beneficial effects of estrogen—could decrease the risk of heart disease. However, the initiation of therapy later in menopause, when women tend to be older, may have no cardiovascular benefit and may even be harmful. While data accrue in support of the safe use of estrogen replacement therapy for younger, generally healthy women, many experts suggest that treatment decisions should be individualized—taking into account not only a woman’s age and time since menopause—but her symptoms, treatment preference, and overall risk profile. Heart-healthy lifestyles should be encouraged.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Mozaffarian D, Benjamin EJ, Arnett DK, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Gholizadeh L, Davidson P. More similarities than differences: an international comparison of CVD mortality and risk factors in women. Health Care Women Int. 2008;29:3–22.
Chakrabarti S, Morton JS, Davidge ST. Mechanisms of estrogen effects on the endothelium: an overview. Can J Cardiol. 2014;30(7):705–12.
Khalil RA. Sex hormones as potential modulators of vascular function in hypertension. Hypertension. 2005;46(2):249–54.
Mendelsohn ME, Karas RH. The Protective Effects of Estrogen on the Cardiovascular System. N Engl J Med. 1999;340(23):1801–11.
Hermeneglido C, Oviedo PJ, Cano A. Cyclooxygenases regulation by estradiol on the endothelium. Curr Pharm Des. 2006;12(2):205–15.
Gilligan DM, Badar DM, Panza JA, et al. Acute vascular effects of estrogen in postmenopausal women. Circulation. 1994;90:786–91.
Simoncini T, Hafezi-Moghadam A, Brazil DP, Ley K, Chin WW, Liao JK. Interaction of oestrogen receptor with the regulatory subunit of phoshatidyllinisitol 3 kinase. Nature. 2000;407(6803):538–41.
Chan SH, Chan JY. Brain stem NOS and ROS in neural mechanisms of hypertension. Antioxid Redox Signal. 2015;20(1):146–83.
Kaludercic N, Deshwal S, Di Lisa F. Reactive oxygen species and redox compartmentalization. Front Physiol. 2014;5:285.
Rubattu S, Bianchi F, Busceti CL, et al. Differential modulation of AMPK/PPARalpha/UCP2 axis in relation to hypertension and aging in the brain, kidneys and heart of two closely related spontaneously hypertensive rat strains. Oncotarget. 2015;6(22):18800–18.
Whitcroft SI, Crook D, Marsh MS, et al. Long-term effects of oral and transdermal hormone replacement therapies on serum lipid and lipoprotein concentrations. Obstet Gynecol. 1994;84(2):222–6.
Feingold KM, Brinton EA., Grunfeld C. The effect of endocrine disorders on lipids and lipoproteins. In: De Groot LJ, Chrousos G., et al., Endotext (internet). South Dartmouth (MA): MD text.com, Inc., 2000. 2017 Feb 24.
Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA. 2002;288:321–33.
Manson JE, Allison MA, Rossouw JE, Carr JJ, Langer RD, Hia J, et al. Estrogen therapy and coronary-artery calcification. WHI and WHI-CACS investigators. N Engl J Med. 2007;356:2591–602.
Allison MA, Manson JE, Langer RD, Carr JJ, Rossouw JE, Pettinger MB, et al. Oophorectomy, hormone therapy, and subclinical coronary artery disease in women with hysterectomy: the women’s health initiative coronary artery calcium study. women’s health initiative and women’s health initiative coronary artery calcium study investigators. Menopause. 2008;15:639–47.
Bernstein P, Pohost G. Progesterone, progestins, and the heart. Rev Cardiovasc Med. 2010;11:228–36.
Lee DY, Kim JY, Kim JH, Choi DS, Kim DK, Koh KK, et al. Effects of hormone therapy on ambulatory blood pressure in postmenopausal Korean women. Climacteric. 2011;14:92–9.
Fahraeus L, Larsson-Cohn U, Wallentin L. L-norgestrel and progesterone have different influences on plasma lipoproteins. Eur J Clin Investig. 1983;13:447–53.
Schierbeck LL, Rejnmark L, Tofteng CL, et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomized trial. Br Med J. 2012;e6409:345.
Collins P, Flather M, Lees B, et al. Randomized trial effects of continuous combined HRT on markers of lipids and coagulation in women with acute coronary syndromes: WHISP pilot study. Eur Heart J. 2006;27:2046–53.
Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women, Heart and Estrogen/progestin Replacement Study (HERS Research Group). JAMA. 1998;280:605–13.
Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement Study follow-up (HERS II). HERS Research Group [published erratum appears in JAMA] 2002; 288:1064. JAMA. 2002;288:49–57.
Salpeter SR, Walsh JME, Greyber E, Salpeter EE. Coronary heart disease events associated with hormone therapy in younger and older women. J Gen Intern Med. 2006;21:363–6.
• Boardman HM, Hartley L, Eisinga A et al. Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database Syst Rev. 2015:10(3). A large updated Cochrane review that reviewed the effects of hormone therapy for prevention of cardiovascular disease.
• Hodis HN, Mack WJ, Henderson VW. Vascular effects of early versus late postmenopausal treatment with estradiol. N Engl J Med. 2016;374:1221–31 A good study evaluating the atherosclerotic progression based on timing of hormorne replacement therapy.
Hodis NH, Mack WJ, Lobo RA, et al. Estrogen in the prevention of atherosclerosis: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2001;135:939–53.
Barker C, Manson JE. The Kronos Early Estrogen Prevention Study. Women Health. 2013;9(1):9–11.
Manson JE, Chlebowski RT, Stefanick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the women’s health initiative randomized trials. JAMA. 2013;310(13):1353–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carson Keck and Marian Taylor declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of theTopical Collection on Women and Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Keck, C., Taylor, M. Emerging Research on the Implications of Hormone Replacement Therapy on Coronary Heart Disease. Curr Atheroscler Rep 20, 57 (2018). https://doi.org/10.1007/s11883-018-0758-2
Published:
DOI: https://doi.org/10.1007/s11883-018-0758-2