Abstract
Purpose of Review
This review examines the recent literature on the use of low-dose aspirin (LDA) for primary and secondary prevention of cardiovascular disease in women, use of LDA for pre-eclampsia prevention in pregnancy, and the underutilization of aspirin therapy in women as compared to men.
Recent Findings
While men and women should not differ with respect to aspirin use for secondary prevention, its role in primary prevention remains unclear for both sexes, with particular uncertainty in women. Reflective of this are conflicting recommendations in current guidelines for primary prevention and thus investigations of primary prevention aspirin use are ongoing and will play an important role in elucidating its efficacy. While there is significant heterogeneity in studies to date of LDA for pre-eclampsia prevention, based on recent meta-analyses suggesting promising results, guidelines now recommend initiation in high risk women after the 12th week of gestation. Finally, studies consistently reveal that aspirin therapy is underutilized in women as compared to men, suggesting a need to better educate physicians and the general public about its use in women.
Summary
Further research is needed to better elucidate the role of aspirin in women for primary prevention of cardiovascular disease and for pre-eclampsia in high risk pregnant women. In addition, further investigation into the factors that lead to the current underutilization of aspirin in women are required in order to ensure that patients of both sexes are optimally treated, with the goal of improving cardiovascular outcomes in all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
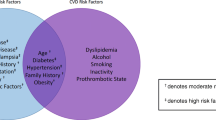
Cardiovascular disease is the leading cause of mortality in American men and women. Over decades, advances in cardiovascular medicine have lowered this incidence. However, it is well established that the reduction in women lags behind that of men. Ongoing research is needed to elucidate the reasons behind this discrepancy, which at least partly relates to differences in disease pathophysiology and under-representation of women in cardiovascular trials. Aspirin remains a cornerstone therapy of cardiovascular medicine and its efficacy and utilization in a variety of patient populations—including women—and disease states continues to evolve.
The goal of this review is to highlight the recent literature regarding the utilization and efficacy of aspirin in women for primary and secondary prevention of cardiovascular disease, as well as its role in pregnancy.
Sex Differences in the Response to Aspirin Therapy
Aspirin irreversibly inhibits cyclooxygenase 1 (COX-1), which ultimately reduces platelet aggregation. Several studies of platelet reactivity in men and women have found that women, even those without cardiovascular disease, exhibit greater baseline platelet reactivity as compared to men [1–4]. This finding has raised the question of whether men and women respond differently to aspirin therapy. In a study by Becker et al., aspirin at a dose of 81 mg resulted in near total suppression of platelet reactivity as assessed through COX-1 dependent mechanisms in healthy subjects of both sexes, despite higher baseline platelet reactivity measured in women [1]. However, slightly more women as compared to men exhibited greater residual platelet activity as assessed through pathways independent of COX-1. Similarly, Shen et al. report higher baseline platelet reactivity in women and greater residual platelet reactivity with aspirin 81 mg daily, primarily through pathways independent of COX-1 [2]. Using a definition of aspirin resistance as less than 70 % inhibition of collagen-induced platelet aggregation, these authors found significantly more women (30 %) as compared to men (16 %) who exhibited aspirin resistance (p = 0.0002) [1].
In order to investigate the effect of aspirin dosing, Qayyum et al. examined the degree of inhibition of platelet aggregation in response to daily aspirin 81 versus 325 mg in patients without cardiovascular disease [4]. This study again confirmed that women exhibited greater baseline platelet reactivity but both sexes experienced near total suppression of platelet aggregation through the direct COX-1 pathway at a dose of 81 mg, without an incremental benefit in either sex to 325 mg. However, women again exhibited greater residual platelet reactivity via indirect pathways such that with a dose of aspirin 325 mg, women demonstrated higher residual platelet aggregation through independent pathways as compared to men who had received a dose of 81 mg. Whether this contributes to a clinically meaningful difference in the benefit of aspirin between men and women, however, remains unknown. It does suggest that the efficacy of COX-1 inhibition of low-dose aspirin (LDA) does not differ between men and women and thus does not support, on a pharmacologic level, utilization of higher aspirin doses in women as compared to men.
In summary, women exhibit higher baseline platelet reactivity as compared to men. While both sexes experience near total suppression of platelet aggregation through COX-1 dependent mechanisms, women still exhibit higher platelet reactivity on aspirin therapy through mechanisms independent of COX-1. Whether this translates into a clinically meaningful difference in the efficacy of the drug between men and women is also unknown.
Aspirin for Primary Prevention
While the use of aspirin for secondary prevention is well established, its efficacy, especially in women, for primary prevention remains controversial. As with other cardiovascular trials, women remain under-represented in trials of primary prevention with aspirin. The Women’s Health Study (WHS) is the largest study to date to exclusively investigate primary prevention aspirin in women and randomized nearly 40,000 healthy women over the age of 45 to 100 mg of every other day aspirin versus placebo [5••]. While LDA reduced the incidence of stroke by 17 % in this population over the 10-year follow-up period, there was no reduction in the incidence of myocardial infarction (MI) or cardiovascular death. Based on subgroup analysis revealing that women aged 65 or older randomized to aspirin experienced a significant reduction in major cardiovascular events, ischemic stroke, and MI, recommendations emerged for LDA use only among older women. A subsequent analysis of the on-treatment population from the WHS found a similar reduction in total cardiovascular events as found in the intent-to-treat analysis, but a greater reduction in cardiovascular mortality of 24 %, though this did not reach significance [6]. More recently, in a risk model based on 15-year outcomes data from the WHS combining cardiovascular, oncologic, and major bleeding outcomes, the risk of bleeding outweighed the modest reduction in the risk of cardiovascular or oncologic disease in women younger than 65 years of age [7]. Cancer risk was included in this model in light of data suggesting a reduction in the risk of colorectal cancer and other gastrointestinal cancers with aspirin use [8]. While the risk of bleeding increased with age, the benefit gained from the reduction in cardiovascular events in women aged 65 and older out-weighted this risk, suggesting that selective treatment of older women may yield meaningful benefit: 29 women aged 65 and older would need to be treated to prevent one event [7].
Since the WHS, meta-analyses of primary prevention trials have been conducted in an attempt to further clarify the efficacy of primary prevention aspirin in women. In an analysis of six randomized controlled trials of primary prevention including nearly 100,000 patients, aspirin use resulted in a 12 % reduction in cardiovascular events (confidence interval [CI] 0.79–0.99, p = 0.03) and 17 % reduction in the incidence of stroke (CI 0.70–0.97, p = 0.02) without an effect on the incidence of myocardial infarction or either cardiovascular or all-cause mortality in women randomized to aspirin therapy as compared to those who were not [9]. Overall, however, the absolute risk reduction with aspirin was 0.30 % for women and 0.37 % for men, suggesting that the absolute benefit for both sexes is quite small [9]. Subsequently, the Antithrombotic Trialists’ Collaboration performed a patient-level meta-analysis across six trials, in which they found an overall 12 % proportional reduction in serious vascular events in patients randomized to aspirin therapy as compared to control (rate ratio 0.88, 95 % CI 0.82–0.94, p = 0.0001) [10]. In this analysis, however, no sex differences were appreciated with respect to prevention of vascular events. However, as compared to men, women experienced a greater proportional risk reduction with respect to ischemic stroke (p = 0.08 for heterogeneity of effect between men and women when considered in isolation) [10]. In a review performed for the US Preventive Service Task Force (USPSTF) of the current primary prevention literature, aspirin reduced the risk of nonfatal myocardial infarction by 22 %, primarily within the first 5 years of treatment, without an effect on nonfatal stroke or mortality (either all-cause or cardiovascular) [11]. While this analysis found that older individuals experienced a greater benefit with respect to MI, no sex-specific differences emerged.
These inconsistent study results have ultimately led to heterogeneity in guideline recommendations (Table 1). The AHA guidelines for cardiovascular disease prevention in women cite aspirin use as a class II recommendation for women, particularly aged 65 or older, in whom the benefit of stroke or MI prevention may out-weight the risk of bleeding [12•]. In contrast, however, the European guidelines no longer support primary prevention aspirin for either sex based on a current lack of compelling evidence [13]. In addition the US Food and Drug Administration recently issued a statement recommending against the use of aspirin for primary prevention, regardless of sex [14]. Lastly, the USPSTF no longer includes sex-specific recommendations as it did in 2009, but rather stratifies its recommendation for primary prevention aspirin by age and 10-year cardiovascular disease risk [15]. Given the current uncertainty with respect to the efficacy of primary prevention aspirin, several large-scale randomized controlled trials of populations with varying cardiovascular disease risk are currently ongoing and hope to provide more definitive guidance to clinicians [16–19].
Until more definitive data emerges, recommendations regarding aspirin use for primary prevention should be individualized and the limitations of the current understanding of its efficacy should be discussed with patients. Those who are more likely to benefit based on our current knowledge are women aged 65 or older at low risk for bleeding, who may experience a modest reduction in cardiovascular events, primarily driven by a reduction in ischemic stroke. Whether men and women differ with respect to the efficacy of primary prevention of aspirin use, however, presently remains unclear.
Aspirin for Secondary Prevention
The efficacy of aspirin for secondary prevention is well established in both men and women, with similar efficacy between sexes [10, 20, 21]. In their specific guidelines for the prevention of cardiovascular disease in women, the American Heart Association (AHA) guidelines maintain a class I recommendation for secondary prevention for women, as is the case for men (Table 1) [12•]. A recent analysis of nearly 9000 post-menopausal women with stable cardiovascular disease enrolled in the Women Health Initiative Observational Study, 46 % were taking aspirin [22]. After multivariate adjustment, aspirin use resulted in a 14 % reduction in all-cause mortality (hazard ratio [HR] 0.86 [0.75–0.99]) and 25 % reduction in cardiovascular mortality (HR 0.75 [0.60–0.95]) as compared to non-use over the 6.5 year follow-up period [22]. Further, consistent with prior aspirin dosing data, with propensity matching, no differences in mortality or cardiovascular events emerged between patients taking 81 mg of aspirin as compared to 325 mg [22, 23].
Overall, aspirin remains the standard of care for secondary prevention, and men and women should not differ with respect to such treatment.
Prevalence of Aspirin Use Among Women
Data consistently reveal that significantly fewer women are taking daily aspirin for CVD prevention than warrant therapy, especially as compared to rates of use among men. Between 2004 and 2009, only 41 % of women surveyed who met AHA guideline criteria at that time for primary prevention and 48 % of women who met criteria for secondary prevention were taking daily aspirin [24]. Women of minority status and those not under physician-care were the least likely to be taking a daily aspirin despite meeting guideline criteria. These data were in agreement with observed rates of aspirin use in the Women’s Health Initiative Observational Study, which reported 46 % aspirin use among post-menopausal women with a history of stable cardiovascular disease [22]. Similarly, women who were black and had Medicaid insurance were less likely to be on aspirin therapy while those who were older and had a college education were more likely to be taking aspirin. In another database study of antiplatelet use among patients with cardiovascular, cerebrovascular, or peripheral vascular disease examining >25,000 patients between 2003 and 2004, women were significantly less likely to be on aspirin as compared to men, with 34 % of women and 24 % of men not taking aspirin [25]. A more recent survey from 2012 of >34,000 patients found that 76 % with a history of coronary disease or stroke had been advised by their physician to take low-dose aspirin and of these patients, 88 % were adhering to this advice [26]. As with prior analyses, women with a history of coronary disease were significantly less likely to be taking aspirin as compared to men (60.5 versus 73.1 %, p < 0.05). The same was true when including patients with a history of stroke (69.1 versus 55.3 %, p < 0.05). Recently, the Minnesota Heart survey revealed that utilization of aspirin for both primary and secondary prevention has increased steadily in both men and women between 1980 and 2009 [27]. However, consistent with prior studies, aspirin use in women was consistently lower than in men with 12 versus 21 % of women versus men receiving aspirin for primary prevention and 64 versus 74 % of women versus men receiving secondary prevention aspirin between 2007 and 2009.
The underutilization of aspirin for primary prevention may be due to uncertainty regarding its efficacy for this indication, especially in women. For example, in a cost analysis of primary prevention aspirin in men versus women weighing multiple competing factors including the balance of preventing of ischemic events against bleeding events, aspirin was only cost effective for women whose 10-year cardiovascular disease risk exceeded 15 %, while in men aspirin was cost effective when the 10-year cardiovascular disease risk exceeded 10 % [28]. Given that it remains unclear from the primary prevention literature who should receive aspirin therapy and whether men and women should be treated differently, the interpretation of the differential treatment of men and women for this indication also remains unclear. However, given that the strong recommendation for aspirin for secondary prevention is true for both sexes, the consistent underutilization of aspirin in women with established cardiovascular disease is concerning and increasing both physician recommendations for and patient adherence to aspirin therapy in both men and women with a history of cardiovascular disease may be critical for preventing recurrent cardiovascular events, especially in women.
Aspirin Use for Pre-eclampsia Prevention
Affecting approximately 3 to 7 % of pregnancies, pre-eclampsia is characterized by new-onset hypertension beyond the 20th week of gestation with proteinuria exceeding 300 mg over 24 h or development of thrombocytopenia, liver and renal impairment, pulmonary edema, and cerebral or visual disturbances [29, 30•, 31]. Given that pre-eclampsia and eclampsia account for 12 % of maternal mortality, 15 % of pre-term births, and over a third of obstetrical complications, there is significant interest in disease prevention [32–34]. While the pathophysiology of pre-eclampsia remains incompletely understood, as a placental disorder LDA may reduce the risk of pre-eclampsia through inhibition of thromboxane A2 synthesis (which may be increased in women with pre-eclampsia), enabling vasodilation and thus enhanced placental blood flow [35]. Early use of aspirin in pregnancy may be additionally beneficial in improving placentation, with inadequate trophoblastic invasion postulated as a pathophysiologic disease mechanism [35]. Prior studies have not suggested risk of congenital heart defects or other structural or developmental anomalies with aspirin therapy in the first trimester or an increased risk in antenatal ductus arteriosus closure in late pregnancy [36–39].
At present, the World Health Organization (WHO) and USPSTF recommend initiation of aspirin for women at high risk for developing pre-eclampsia (Table 1) [40, 41]. The USPSTF further recommends initiation after the 12th week of gestation in women at high risk for developing pre-eclampsia, including those with a history of pre-eclampsia, chronic hypertension, diabetes, renal disease, autoimmune diseases, and multiple gestations [42]. The American Congress of Obstetricians and Gynecologists (ACOG) similarly recommend initiating LDA in late first trimester in women, though initially in a more restricted population of women: those with a history of early-onset pre-eclampsia necessitating delivery prior to 34 weeks of gestation and those with pre-eclampsia complicating multiple prior pregnancies [43]. In one cost-effectiveness analysis, the more inclusive USPTF recommendations resulted in a greater degree of pre-eclampsia prevention as compared to the more stringent ACOG guidelines, though a strategy of universal LDA administration was not compelling given the low incidence of disease overall [44]. However, ACOG recently released updated recommendations through a practice advisory and now recommend initiation of LDA between the 12th and 28th weeks of gestation using the same high-risk criteria put forth by the USPSTF [45].
Significant heterogeneity exists in the outcomes of studies examining the efficacy of LDA in reducing the risk of pre-eclampsia. Some of this heterogeneity may be due to differences in timing of aspirin initiation (with several studies suggesting that the benefit is strongest prior to 16 weeks of gestation), dosing differences (with some studies employing doses as low as 50–60 mg, which may not effectively inhibit placental thromboxane), and differences in the risk profiles of study participants [35]. However, meta-analyses examining pooled data have recently suggested that LDA is efficacious for reduction of pre-eclampsia, pre-term birth, and IUGR. In a recent meta-analysis of 29 randomized controlled trials, LDA reduced the risk of pre-eclampsia by 29 %, pre-term birth by 19 %, and IUGR by 20 %, with a greater benefit to initiation of therapy prior to 16 weeks of gestation as compared to after 16 weeks [46•]. While these authors found an increase in the risk of placental abruption, they did not find an increased risk of spontaneous abortion or either antepartum or postpartum hemorrhage. In agreement with these findings, a meta-analysis conducted for the USPSTF reported at least a 10 % reduction in pre-eclampsia, 20 % reduction in IUGR, and 14 % reduction in pre-term birth without an effect on fetal intracranial bleeding or postpartum hemorrhage [32]. Similarly, another meta-analysis inclusive of 27 randomized controlled trials found that randomization to LDA at 16 weeks or earlier yielded a significant reduction in the incidence of pre-eclampsia (relative risk [RR] 0.47, 95 % CI 0.34–0.65) and IUGR (RR 0.44; 95 % CI 0.30–0.65), though treatment after 16 weeks did not [47•]. This analysis did not find an increase in the risk of placental abruption. Given the heterogeneity of randomized trial results despite promising results from recent meta-analyses, the Aspirin for evidence-based PREeclampsia prevention (ASPRE) study is currently being conducted and will be the largest multicenter, double-blinded randomized placebo-controlled trial to study the effect of LDA on pre-eclampsia prevention using an enhanced screening approach initiated in the first trimester [48]. To help determine whether LDA may have a role in low-risk women, an open-label randomized controlled trial examining both low- and high-risk women is also underway and may widen the application for aspirin therapy in pregnancy for the prevention of pre-eclampsia [49].
As in the general population, aspirin resistance may be prevalent in the pregnant population, with 28.7 % of women exhibiting non-responsiveness in one study [50]. As determined by platelet function testing on whole blood using the Platelet Function Analyzer (PFA-100®), a significant number of non-responders to a dose of aspirin 81 mg responded to a dose of 162 mg, suggesting that dose adjustment may have a role in aspirin resistance during pregnancy. While prospective studies are needed to define its role in clinical practice, a retrospective analysis found a significant reduction in the incidence of pre-eclampsia among women treated with aspirin who were followed with PFA-100® testing versus those who were treated with aspirin but not followed with testing (15.3 versus 30.8 %; adjusted odds ratio 0.35, 95 % CI 0.19–0.67), as well as a reduction in the incidence of severe pre-eclampsia (3.6 versus 15.1 %; adjusted odds ratio 0.22, 95 % CI 0.07–0.66) [51]. While this study is hypothesis generating, whether routine platelet function testing and dose adjustment in high risk women has a role in general practice remains to be seen.
Given the heterogeneity of the results of studies of LDA for pre-eclampsia prevention thus far, developing an optimal strategy for its utilization requires further investigation. Overall, studies suggest that LDA is safe in pregnancy both from the standpoint of significant maternal and neonatal bleeding events as well as fetal development. In addition, data consistently suggest that the benefit of LDA may be greatest when initiated early. Guideline recommendations now consistently recommend LDA initiation as early as possible (ideally after the 12th week of gestation) in women with a high-risk profile for the development of pre-eclampsia. However, the optimal target population, optimum point at which to initiate therapy, and whether platelet function testing and consequent dose escalation may improve pre-eclampsia prevention in pregnant women is not yet known.
Conclusions
While the role of secondary prevention aspirin use is clear, its indication for primary prevention in women requires further investigation. Ongoing trials of aspirin for primary prevention should aim to enroll enough women to elucidate its efficacy in both sexes. Similarly, ongoing studies of LDA for pre-eclampsia will hopefully shed light on better characterization methods for defining high-risk patients, optimal timing of therapy initiation (with evidence that earlier may be better), and whether lower-risk patients may also benefit from therapy. Given that women with pre-eclampsia are at higher risk for cardiovascular disease in later life, it is possible that a reduction in the incidence of pre-eclampsia will in turn translate into the lowering of the incidence of cardiovascular disease in women, a question that also warrants further investigation [52–56]. In light of the high prevalence of aspirin resistance both among women in general as well as in pregnancy, further study is also required to determine whether routine platelet testing should be conducted to identify aspirin-resistant patients and whether dose escalation on the basis of such testing improves clinically meaningful results. Finally, the role of aspirin outside of cardiovascular disease continues to grow, with emerging evidence suggesting a role for LDA for cancer prevention—including prevention of breast and cervical cancers—which requires further investigation [57–59].
Given that cardiovascular outcomes are not improving in women at the same rate as they are in men, improving the diagnosis and treatment of cardiovascular disease in women is critical. Paramount to this effort is further investigation into the factors that result in the consistent underutilization of cardiovascular treatments in women as compared to men, including aspirin therapy. While some of the underutilization for primary prevention may stem from uncertainty regarding its efficacy for this indication, given equal efficacy in both sexes for secondary prevention, both research and advocacy efforts should focus on ensuring that women with a history of cardiovascular disease are prescribed and counseled to take aspirin for secondary prevention, barring any contraindication to this therapy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Becker DM, Segal J, Vaidya D, Yanek LR, Herrera-Galeano JE, Bray PF, et al. Sex differences in platelet reactivity and response to low-dose aspirin therapy. JAMA. 2006;295:1420–7.
Shen H, Herzog W, Drolet M, Pakyz R, Newcomer S, Sack P, et al. Aspirin resistance in healthy drug-naive men versus women (from the Heredity and Phenotype Intervention Heart Study). Am J Cardiol. 2009;104:606–12.
Gum PA, Kottke-Marchant K, Poggio ED, Gurm H, Welsh PA, Brooks L, et al. Profile and prevalence of aspirin resistance in patients with cardiovascular disease. Am J Cardiol. 2001;88:230–5.
Qayyum R, Becker DM, Yanek LR, Moy TF, Becker LC, Faraday N, et al. Platelet inhibition by aspirin 81 and 325 mg/day in men versus women without clinically apparent cardiovascular disease. Am J Cardiol. 2008;101:1359–63.
•• Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–304. The Women’s Health Study remains the largest randomized trial of primary prevention aspirin in women to date.
Cook NR, Cole SR, Buring JE. Aspirin in the primary prevention of cardiovascular disease in the Women’s Health Study: effect of noncompliance. Eur J Epidemiol. 2012;27:431–8.
van Kruijsdijk RC, Visseren FL, Ridker PM, Dorresteijn JA, Buring JE, van der Graaf Y, et al. Individualised prediction of alternate-day aspirin treatment effects on the combined risk of cancer, cardiovascular disease and gastrointestinal bleeding in healthy women. Heart. 2015;101:369–76.
Algra AM, Rothwell PM. Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol. 2012;13:518–27.
Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306–13.
Antithrombotic Trialists’ (ATT) Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–60.
Guirguis-Blake JM, Evans CV, Senger CA, O’Connor EA, Whitlock EP. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. preventive services task force. Ann Intern Med. 2016;164:804–13.
• Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American heart association. Circulation. 2011;123:1243–62. Updated National Guidelines on Prevention of Cardiovascular Disease in Women.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren WM, et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012): the fifth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Int J Behav Med. 2012;19:403–88.
United States Food and Drug Administration. Use of Aspirin for Primary Prevention of Heart Attack and Stroke. 2014. http://www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm390574.htm.
Bibbins-Domingo K, U.S. Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. 2016;164:836–45.
ASPREE Investigator Group. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials. 2013;36:555–64.
De Berardis G, Sacco M, Evangelista V, Filippi A, Giorda CB, Tognoni G, et al. Aspirin and Simvastatin Combination for Cardiovascular Events Prevention Trial in Diabetes (ACCEPT-D): design of a randomized study of the efficacy of low-dose aspirin in the prevention of cardiovascular events in subjects with diabetes mellitus treated with statins. Trials. 2007;8:21.
Aung T, Haynes R, Barton J, Cox J, Murawska A, Murphy K et al. Cost-effect recruitment methods for a large randomised trial in people with diabetes: A Study of Cardiovascular Events iN Diabetes (ASCEND). Trials. 2016;17(1). doi:10.1186/s13063-016-1354-9.
A study to assess the efficacy and safety of enteric-coated acetylsalicylic acid in patients at moderate risk of cardiovascular disease (ARRIVE). ClinicalTrials.gov Identifier NCT00501059. 2016. https://clinicaltrials.gov/ct2/show/NCT00501059.
Mora S. Aspirin therapy in women: back to the ABCs. Circ Cardiovasc Qual Outcomes. 2009;2:63–4.
ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1998;2:349–60.
Berger JS, Brown DL, Burke GL, Oberman A, Kostis JB, Langer RD, et al. Aspirin use, dose, and clinical outcomes in postmenopausal women with stable cardiovascular disease: the Women’s Health Initiative Observational Study. Circ Cardiovasc Qual Outcomes. 2009;2:78–87.
Mehta SR, Bassand JP, Chrolavicious S, Diaz R, Eikelboom JW et al. Dose comparisons of clopidogrel and aspirin in acute coronary syndromes. N Engl J Med. 2010;363:930–42.
Rivera CM, Song J, Copeland L, Buirge C, Ory M, McNeal CJ. Underuse of aspirin for primary and secondary prevention of cardiovascular disease events in women. J Women’s Health. 2012;21:379–87.
Cannon CP, Rhee KE, Califf RM, Boden WE, Hirsch AT, Alberts MJ, et al. Current use of aspirin and antithrombotic agents in the United States among outpatients with atherothrombotic disease (from the REduction of Atherothrombosis for Continued Health [REACH] Registry). Am J Cardiol. 2010;105:445–52.
Fang J, George MG, Gindi RM, Hong Y, Yang Q, Ayala C, et al. Use of low-dose aspirin as secondary prevention of atherosclerotic cardiovascular disease in US adults (from the National Health Interview Survey, 2012). Am J Cardiol. 2015;115:895–900.
Luepker RV, Steffen LM, Duval S, Zantek ND, Zhou X, Hirsch AT. Population trends in aspirin use for cardiovascular disease prevention 1980–2009: The Minnesota Heart Survey. J Am Heart Assoc. 2015;4.
Greving JP, Buskens E, Koffijberg H, Algra A. Cost-effectiveness of aspirin treatment in the primary prevention of cardiovascular disease events in subgroups based on age, gender, and varying cardiovascular risk. Circulation. 2008;117:2875–83.
Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ. 2013;347:f6564.
• LeFevre ML, U.S. Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:819–26. National recommendations on aspirin use for women at risk for preeclampsia.
Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS. Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol. 2014;124:771–81.
Henderson JT, O’Connor E, Whitlock EP. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia. Ann Intern Med. 2014;161:613–4.
Schaap TP, Knight M, Zwart JJ, Kurinczuk JJ, Brocklehurst P, van Roosmalen J, et al. Eclampsia, a comparison within the International Network of Obstetric Survey Systems. BJOG. 2014;121:1521–8.
Gold RA, Gold KR, Schilling MF, Modilevsky T. Effect of age, parity, and race on the incidence of pregnancy associated hypertension and eclampsia in the United States. Pregnancy Hypertens. 2014;4:46–53.
Katsi V, Kanellopoulou T, Makris T, Nihoyannopoulos P, Nomikou E, Tousoulis D. Aspirin vs heparin for the prevention of preeclampsia. Curr Hypertens Rep. 2016;18:57.
Slone D, Siskind V, Heinonen OP, Monson RR, Kaufman DW, Shapiro S. Aspirin and congenital malformations. Lancet. 1976;1:1373–5.
Werler MM, Mitchell AA, Shapiro S. The relation of aspirin use during the first trimester of pregnancy to congenital cardiac defects. N Engl J Med. 1989;321:1639–42.
Di Sessa TG, Moretti ML, Khoury A, Pulliam DA, Arheart KL, Sibai BM. Cardiac function in fetuses and newborns exposed to low-dose aspirin during pregnancy. Am J Obstet Gynecol. 1994;171:892–900.
Wyatt-Ashmead J. Antenatal closure of the ductus arteriosus and hydrops fetalis. Pediatr Dev Pathol: Off J Soc Pediatr Pathol Paediatr Pathol Soc. 2011;14:469–74.
Henderson JT, Whitlock EP, O’Conner E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for the prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the US preventive services task force. Rockville (MD)2014.
World Health Organization. WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. 2011. http://apps.who.int/iris/bitstream/10665/44703/1/9789241548335_eng.pdf.
Henderson JT, Whitlock EP, O’Connor E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160:695–703.
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–31.
Werner EF, Hauspurg AK, Rouse DJ. A cost-benefit analysis of low-dose aspirin prophylaxis for the prevention of preeclampsia in the United States. Obstet Gynecol. 2015;126:1242–50.
American Congress of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. 2016. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations.
• Xu TT, Zhou F, Deng CY, Huang GQ, Li JK, Wang XD. Low-dose aspirin for preventing preeclampsia and its complications: a meta-analysis. J Clin Hypertens. 2015;17:567–73. A recent meta-analysis examining 29 randomized controlled trials of low dose aspirin for pre-eclampsia prevention, which revealed a reduction in the incidence of pre-eclampsia, with greatest efficacy prior to 16 weeks of gestation.
• Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116:402–14. A meta-analysis of 34 randomized controlled trials of low dose aspirin, which revealed that initiation of low dose aspirin at 16 weeks of gestation or earlier yielded a significant reduction in the incidence of pre-eclampsia, whereas initiation after 16 weeks of gestation did not.
O’Gorman N, Wright D, Rolnik DL, Nicolaides KH, Poon LC. Study protocol for the randomised controlled trial: combined multimarker screening and randomised patient treatment with ASpirin for evidence-based PREeclampsia prevention (ASPRE). BMJ Open. 2016;6, e011801.
Mone F, Mulcahy C, McParland P, Stanton A, Culliton M, Downey P, et al. An open-label randomized-controlled trial of low dose aspirin with an early screening test for pre-eclampsia and growth restriction (TEST): Trial protocol. Contemp Clin Trials. 2016.
Caron N, Rivard GE, Michon N, Morin F, Pilon D, Moutquin JM, et al. Low-dose ASA response using the PFA-100 in women with high-risk pregnancy. JOGC. 2009;31:1022–7.
Rey E, Rivard GE. Is testing for aspirin response worthwhile in high-risk pregnancy? Eur J Obstet Gynecol Reprod Biol. 2011;157:38–42.
Mannisto T, Mendola P, Vaarasmaki M, Jarvelin MR, Hartikainen AL, Pouta A, et al. Elevated blood pressure in pregnancy and subsequent chronic disease risk. Circulation. 2013;127:681–90.
Black MH, Zhou H, Sacks DA, Dublin S, Lawrence JM, Harrison TN, et al. Hypertensive disorders first identified in pregnancy increase risk for incident prehypertension and hypertension in the year after delivery. J Hypertens. 2016;34:728–35.
Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974.
Wikstrom AK, Haglund B, Olovsson M, Lindeberg SN. The risk of maternal ischaemic heart disease after gestational hypertensive disease. BJOG. 2005;112:1486–91.
Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, Paidas MJ. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944–51.
Cao Y, Nishihara R, Wu K, Wang M, Ogino S, Willett WC, et al. Population-wide impact of long-term use of aspirin and the risk for cancer. JAMA Oncol. 2016;2:762–9.
Bardia A, Keenan TE, Ebbert JO, Lazovich D, Wang AH, Vierkant RA, et al. Personalizing aspirin use for targeted breast cancer chemoprevention in postmenopausal women. Mayo Clin Proc. 2016;91:71–80.
Friel G, Liu CS, Kolomeyevskaya NV, Hampras SS, Kruszka B, Schmitt K, et al. Aspirin and acetaminophen use and the risk of cervical cancer. J Low Genit Tract Dis. 2015;19:189–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Amy Sarma and Nandita S. Scott declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Women and Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Sarma, A., Scott, N.S. Aspirin Use in Women: Current Perspectives and Future Directions. Curr Atheroscler Rep 18, 74 (2016). https://doi.org/10.1007/s11883-016-0630-1
Published:
DOI: https://doi.org/10.1007/s11883-016-0630-1