Abstract
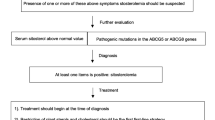
Sitosterolemia is a rare autosomal recessively inherited disease caused by mutations affecting ABCG5 or ABCG8, which are located on human chromosome band 2p21. Around 100 cases have been reported in the literature. Sitosterolemic patients typically exhibit a 30-fold to 100-fold increase in plasma concentrations of plant sterols. The clinical manifestations include xanthomas, premature atherosclerosis, hemolytic anemia, and macrothrombocytopenia. It is noteworthy that abnormal hematological parameters may be the only clinical feature of sitosterolemic patients, suggesting that sitosterolemia may be more frequent than previously thought. Severe accumulation of plant sterols in mouse models of sitosterolemia induced complex cardiac lesions, anemia, and macrothrombocytopenia, disrupted adrenal and liver cholesterol homeostasis, and caused infertility and hypertriglyceridemia. It remains unclear whether all disease traits are present in sitosterolemic patients. The drug ezetimibe appears to be effective in reducing plasma plant sterol levels, promotes xanthoma regression, and improves the cardiovascular and hematological signs in sitosterolemic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sitosterolemia (Online Mendelian Inheritance in Man 210250), also termed phytosterolemia, is a rare autosomal recessively inherited disease caused by homozygous or compound heterozygous mutations affecting one of two adjacent, half-sized sterol adenosine triphosphate binding cassette transporters, ABCG5 (sterolin 1) and ABCG8 (sterolin 2) [1–3]. ABCG5 and ABCG8 form heterodimers, which act as efflux pumps to preferentially export free sterols from hepatocytes or enterocytes into the lumen [4]. Plant sterols are poorly absorbed in healthy subjects (less than 5 %), but sitosterolemic patients have greatly increased concentrations of plasma and tissue plant sterols, especially sitosterol, campesterol, and stigmasterol, which are the commonest plant sterols, owing to intestinal hyperabsorption and low bile excretion [5, 6]. Patients with sitosterolemia have plasma plant sterol levels ranging from 10 to 65 mg/dL. The usual clinical enzymatic colorimetric methods cannot discriminate between cholesterol and plant sterols because their reactivity depends on the C-5 double bond or the presence of the 3β hydroxyl group, both of which are present in the two types of sterols [4]. Thus, the diagnosis requires gas chromatography or high-performance liquid chromatography to detect plasma plant sterol levels [5, 6]. The main clinical features of sitosterolemia are tendon or tuberous xanthomas and accelerated atherosclerosis [4]. Hematological abnormalities are invariably present and are frequently characterized by the presence of abnormally shaped erythrocytes (stomatocytes) and thrombocytopenia, which is frequently associated with giant platelets (macrothrombocytopenia). Therefore, sitosterolemia shares clinical features with familial hypercholesterolemia and cerebrotendinous xanthomatosis, namely, the presence of tendon xanthomas and premature cardiovascular disease. However, sitosterolemia may be differentiated from these diseases because adult sitosterolemic patients typically present with normal or moderately elevated cholesterol levels, without cataracts or neurological symptoms [4]. The generation of mouse models of sitosterolemia, such as ABCG5-deficient, ABCG8-deficient, or double ABCG5- and ABCG8-deficient mice has produced data concordant with human findings [7••]. This review aims to update recent findings on the diagnosis, investigation, and management of sitosterolemia.
Molecular Genetic Analyses
ABCG5 and ABCG8 are located head-to-head on chromosome band 2p21, each comprising 13 exons. It is likely that they have evolved by duplication and inversion from a common ancestral gene. Despite the proximity of both genes, ABCG8 contains more polymorphisms than ABCG5 [8]. This is not the case in rodents, where the numbers of ABCG5 and ABCG8 polymorphisms are almost similar [9, 10]. A similar number of rare variants associated with sitosterolemia has been reported in humans: Twenty-three different mutations in ABCG5 were identified in Asian patients (Chinese, Japanese, and Indian), and 31 were identified in ABCG8 in Caucasians (mostly of northern European origin). The genetic diagnosis of sitosterolemia is performed by direct sequencing of exons and intron–exon boundaries of the ABCG5 and ABCG8 genes.
To date, fewer than 100 individuals with sitosterolemia have been reported worldwide [4, 5], with 36 % homozygous or compound heterozygous mutations found in the ABCG5 gene and 64 % homozygous or compound heterozygous mutations found in the ABCG8 gene. It is noteworthy that 27 of 55 individuals (49 %) with sitosterolemia and mutations in ABCG8 presented with the rare variant p.Trp361X in homozygosis (33 %) or heterozygosis (67 %). The presence of this variant in many of the reported cases is consistent with the existence of a founder effect, thereby suggesting that sitosterolemia is perhaps a more than 4,000-year-old disease [11].
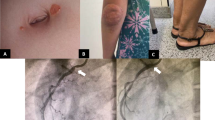
A novel mutation in compound heterozygosis was recently reported in a 15-month-old Korean girl who presented with severe hypercholesterolemia and intertriginous xanthomas [12]. The lesions were first noticed when the child was 3 months old when she was being breastfed. Direct sequencing of ABCG5 in the proband revealed a new compound heterozygous null mutation, c.904+1G>A (p.Met302Asnfs*82), and the previously described c.1336C>T (p.Arg446*) mutation. A genetic analysis of other family members revealed that the child’s 5-year-old sister had the same compound heterozygous mutations but was asymptomatic, thereby indicating that other factors influence disease onset. This report is in line with significant phenotypic heterogeneity previously described in sitosterolemic patients [13].
A recent report described 13 sitosterolemic patients with a large variety of clinical manifestations [14]. All the patients had thrombocytopenia and anemia, 11 had xanthomas, and two had coronary heart disease. In addition, three of eight families of Asian origin had rare variants in ABCG8 and five of 11 different mutations within this gene, thereby indicating that mutations in ABCG8 are not exclusive to Caucasians.
Plant Sterols and Cholesterol Metabolism
Plant sterols are plant-specific phytochemicals that are essential components of cell membranes. The term “plant sterols” includes phytosterols and their saturated forms, phytostanols. They are structurally related to cholesterol, although they differ in the complexity of their side chain, which is attached to the steroid ring [15]. Multiple evidence indicates that the Niemann–Pick C1 like 1 (NPC1L1) transporter has a significant role in the absorption of plant sterols [7••]. Mice lacking NPC1L1 have reduced intestinal absorption of both cholesterol and plant sterols [16, 17]. Ezetimibe, the first drug that specifically inhibits intestinal cholesterol absorption, targets NPC1L1 [18], and it is considered the most effective drug for treating sitosterolemia (see “Current Therapies for Sitosterolemia”).
NPC1L1 discriminates against plant sterols and allows predominantly cholesterol uptake into enterocytes [19]. Thus, NPC1L1 acts as a gatekeeper, which facilitates the uptake of cholesterol into enterocytes while limiting the uptake of plant sterols. A recent report demonstrated that the N-terminal domain of NPC1L1 has a cholesterol-binding pocket with broader sterol specificity; however, the addition of an ethyl group at C-24 in β-sitosterol results in an unfavorable steric clash, leading to less protein binding [20].
Plant sterols are poorly esterified by acyl coenzyme A:cholesterol acyltransferase 2 (ACAT2), thereby hindering incorporation of plant sterols into chylomicrons [21, 22]. Double ABCG5- and ABCG8-deficient mice showed only moderate amounts of β-sitosterol in the small intestine mucosa, and ACAT2 deficiency significantly attenuated this elevation [22]. Taken together, these findings support the concept that NPC1L1 and ACAT2 act together to limit dietary plant sterol absorption and that the ABCG5/ABCG8 function is critical for plant sterol excretion. Figure 1 shows a schematic diagram of cholesterol and plant sterol pathways in sitosterolemic patients. This combined system is very efficient because heterozygous sitosterolemic patients supplemented with plant sterols show only a slight increase in plasma levels of plant sterols [23].
Free cholesterol (C) and plant sterols (PS) are mainly absorbed from the intestinal epithelium via the Niemann–Pick C1 like 1 (NPC1L1) transporter. Cholesteryl esters (CE) are formed by acyl coenzyme A:cholesterol acyltransferase 2 (ACAT2) and are assembled with apolipoprotein B-48 to form chylomicrons, which are secreted into the lymph, where they enter the systemic circulation. PS are poorly esterified by ACAT2. Both PS and cholesterol are secreted into the intestinal lumen via the heterodimer ABCG5/ABCG8. Cholesterol may also be loaded by ABCA1 onto high-density lipoproteins (HDL) at the intestinal basolateral membrane and then enter the lymphatic system. The liver can take up chylomicrons and HDL-associated cholesterol via low-density lipoprotein receptor (LDLR), LDLR-related protein (LRP), and scavenger receptor class B member 1 (SR-BI). The liver can synthesize cholesterol de novo, excrete it into bile for biliary secretion via ABCG5/ABCG8, or return it to the circulation via very low density lipoprotein (VLDL) and HDL. Liver NPC1L1 can facilitate biliary cholesterol reuptake. Deficiency of ABCG5 or ABCG8 in sitosterolemic patients impairs excretion of PS into the intestinal lumen from enterocytes and the liver, thereby resulting in a severe accumulation of PS in plasma and tissues. Sitosterolemic patients have impaired liver cholesterol biosynthesis. Current sitosterolemia therapy is based on a diet low in PS and ezetimibe treatment. The use of cholestyramine may be recommended in ezetimibe-resistant patients
Plant sterols may also be loaded by ABCA1 onto high-density lipoproteins (HDLs) at the intestinal basolateral membrane [24•], esterified in HDLs by lecithin:cholesterol acyltransferase, and taken up by the liver [7••]. Plant sterols interfere with the synthesis of 27-hydroxycholesterol, which is a liver X receptor agonist, thus inhibiting cholesterol mobilization via ABCA1 in intestinal cells [24•].
Both cholesterol and plant sterols can also be excreted to bile via the ABCG5/ABCG8 heterodimer located in the canalicular membrane of hepatocytes, and liver NPC1L1 can facilitate biliary cholesterol reuptake [7••, 25]. Notably, liver transplantation in a sitosterolemic patient normalized plasma plant sterol levels, thereby indicating that restoring liver ABCG5/ABCG8 function is enough to reverse the accumulation of plasma plant sterols [26].
An important body of evidence has demonstrated that sitosterolemic patients have impaired liver cholesterol biosynthesis (reviewed in [15]). However, the effects of β-sitosterol on cholesterol synthesis in vitro and in experimental models have produced divergent results. Although β-sitosterol was not effective in reducing the activity of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase in human fibroblasts and intestinal cells and in livers of rats with high levels of circulating β-sitosterol [7••, 15], it inhibited HMG-CoA reductase in human liver and mouse macrophage cells [27, 28]. Furthermore, megakaryocytes of ABCG5-deficient mice had normal HMG-CoA reductase messenger RNA levels, despite having higher β-sitosterol and campesterol levels [29]. Nevertheless, other plant sterols, such as campesterol and stigmasterol, containing a double bond at C-22 in the side chain reduced HMG-CoA reductase activity in intestinal and adrenal cells [7••, 15]. High plant sterol levels disrupted adrenal cholesterol homeostasis in ABCG5-deficient, ABCG8-deficient, or double ABCG5- and ABCG8-deficient mice [30, 31••], but this did not impair adrenal function in double ABCG5- and ABCG8-deficient mice [30]. One report, however, found adrenal insufficiency and short stature in three sitosterolemic siblings, and the index case also had ovarian failure [32]. Further studies are required to establish which plant sterols contribute to reducing cholesterol biogenesis in patients with sitosterolemia and which tissues are mainly affected.
Xanthomas and Atherosclerosis
Cardiovascular risk is usually severe in sitosterolemia, with myocardial infarctions and multiple tuberous xanthomas reported in individuals as young as 4 years [33, 34]. As with cholesterol, plant sterols may penetrate the artery wall [35], induce foam cell formation [35, 36], and induce secretion of proinflammatory cytokines that attract additional monocytes and promote atherosclerosis progression. Similar mechanisms may be at work in xanthomas [37]. Lower plasma levels of plant sterols seem to induce the formation of xanthomas with respect to those needed in the case of plasma cholesterol [7••]. These findings are consistent with the higher cytotoxic activity of β-sitosterol in human endothelial cells as compared with cholesterol [38]. Furthermore, compared with cholesterol, plant sterols are highly susceptible to oxidative processes, and plant sterol oxidation products are proinflammatory and proatherogenic [39]. The potentially deleterious effects of individual plant sterols remain unclear. Indeed, the presence of stigmasterol in modified low-density lipoproteins promoted cholesterol efflux and suppressed inflammatory cytokine secretion, whereas the presence of sitosterol increased proinflammatory cytokine secretion [37]. In addition, β-sitosterol accumulation caused macrophage death, which may accelerate plaque necrosis [36].
A recent report demonstrated the deleterious effect of very high plant sterol levels in double ABCG5- and ABCG8-deficient mice given a high-plant-sterol-rich diet [40••]. This diet was extremely toxic, and the sitosterolemic mice showed highly complex cardiac lesions, liver damage, and hepatosplenomegaly, all of which were closely associated with the accumulation of plant sterols in these tissues and with premature death [40••].
Fat Morphology, Fertility, and Insulin Resistance
ABCG5- and ABCG8-deficient mice are infertile, despite having no structural defects in gonads [31••]. Sitosterolemic mice show a severe loss of abdominal and perigonadal fat [31••], a feature also found in double ABCG5- and ABCG8-deficient mice [41]. These changes are closely associated with significant alterations in lipolytic activities of adipose tissue [31••, 41]. Double ABCG5- and ABCG8-deficient mice exhibit hypertriglyceridemia by increasing liver and intestinal triglyceride secretion [41]. Liver triglyceride accumulation and insulin resistance were promoted in double ABCG5- and ABCG8-deficient mice given a high-fat diet, and these changes were independent of liver plant sterol accumulation [42]. However, the effect of ABCG5 or ABCG8 deficiency on fertility and triglyceride metabolism in humans remains unclear. There is evidence of fertility in some sitosterolemic women [43], and hypertriglyceridemia has been found in some [13, 32, 44] but not all [43, 45, 46] sitosterolemic patients.
Red Cell Alterations, Bleeding Abnormalities, and Macrothrombocytopenia
Hemolytic anemia and abnormal bleeding are features of sitosterolemia [29, 40••, 46–48, 49••]. Given that the proteins ABCG5 and ABCG8 are not present on blood cells or platelets [50], acquired accumulation of circulating plant sterols and their insertion into the membranes of blood cells is the most likely explanation for their abnormal morphology and function in sitosterolemic patients. Excess levels of plant sterols are thought to promote membrane stiffness, and therefore plant-sterol-enriched red cells are more prone to rupture [46]. They are thought to exert similar effects on platelets. Therefore, plant sterol enrichment in platelet membranes might affect their size, number, and function, and this could be related to bleeding episodes. ABCG5-deficient mice have been reported to exhibit anemia, macrothrombocytopenia, and prolonged bleeding times [48]. More recently, there have been significant advances in the understanding of the mechanisms related to changes in the platelet phenotype and bleeding outcomes [49••]. In ABCG5- and ABCG8-deficient mice fed a high-plant-sterol diet, the accumulation of free sterols within membranes of platelets was reported to elicit hyperactivatable platelets [49••]. Sterol-induced platelet hyper-reactivity led to impaired platelet function due to dysregulation of multiple platelet activation pathways (i.e., internalization of the αIIbβ3 complex and filamin A degradation) in these mice, and the alterations were found to be consistent with macrothrombocytopenia and impairment of hemostatic functions [49••].
As mentioned already (see “Molecular Genetic Analyses”), hematological problems have been occasionally reported as the only clinical symptom observed in asymptomatic sitosterolemic patients [14, 51•, 52]. This is a critical point because these patients may be at high risk of being misdiagnosed and inappropriately treated [14, 51•, 52]. It also suggests that sitosterolemia may be more frequent than previously thought.
Although the management of hematological abnormalities in patients with sitosterolemia is not yet completely established, some of the abnormalities can be controlled with current therapies, as outlined next.
Current Therapies for Sitosterolemia
The available therapies for sitosterolemia include dietary therapy using a low-plant-sterol diet and restriction of shellfish intake, which contains high amounts of the algae-derived plant sterol brassicasterol, as well as pharmacological therapy with bile acid binding resins, statins, sitostanol, and ezetimibe, and surgical methods, such as ileal bypass surgery [7••] (as summarized in Table 1).
Low-plant-sterol diets reduce plasma plant sterol levels in sitosterolemic patients, but this treatment is only partially effective because plant sterols are found in all plant-based foods [7••]. This therapeutic option has produced divergent effects on the progression of xanthomas [7••, 53•].
Bile acid sequestrants disrupt the enterohepatic circulation of bile acids, thereby preventing reabsorption in the ileum [6]. Several studies showed that the bile acid sequestrant cholestyramine reduced plasma levels of plant sterols by 50 % in most sitosterolemic patients, although it was ineffective in some cases [6, 7••, 45]. The administration of a low-fat/low-cholesterol diet and cholestyramine to a 15-month-old Korean girl with severe hypercholesterolemia and intertriginous xanthomas (described in “Molecular Genetic Analyses”) dramatically reduced her plasma cholesterol levels and normalized them in 2 months [12]. Furthermore, the xanthomas regressed and disappeared at the age of 3 years [12]. In the same patient, cholestyramine treatment was discontinued, and plasma β-sitosterol levels remained very high [12]. These results indicate that sitosterolemia should be considered when bile acid binding resins normalize cholesterol levels rapidly or when there is xanthoma regression. However, as shown in another study, the bile salt binding resin colesevelam hydrochloride seems to be ineffective in preventing xanthomas and red blood cell abnormalities [53•], although this study reported only one case.
Statins have not been shown to be effective for lowering plasma plant sterol concentrations in sitosterolemia because the synthesis of liver cholesterol is very low, and further inhibition of HMG-CoA reductase does not upregulate low-density lipoprotein receptor expression [6, 54].
Sitostanol has also been used as a therapeutic strategy to reduce plasma of sitosterol and campesterol levels in sitosterolemic patients [54]. However, the use of sitostanol has raised some concerns because it increased plasma sitostanol and campestanol levels in some sitosterolemic patients [55].
As occurred with bile acid sequestrants, ileal bypass surgery affects bile acid reabsorption. Plasma plant sterol levels were reduced in sitosterolemic subjects who underwent partial or complete ileal bypass surgery [5, 6].
Ezetimibe has emerged as a successful agent for sitosterolemia treatment because it induces a marked improvement in plasma plant sterol levels [7••, 54]. Furthermore, in sitosterolemic patients treated with ezetimibe, xanthomas regressed [56, 57], carotid bruits disappeared, and cardiac murmurs improved [57]. In line with these findings, a recent report showed that after 10 months of treatment in a 13-year-old sitosterolemic patient, ezetimibe was effective in lowering plasma plant sterol levels and reversing stomatocytic anemia and thrombocytopenia while also inducing a decrease in liver and spleen size [58]. In addition, ezetimibe normalized most hematological abnormalities, including hemoglobin levels, red cell morphology, reticulocyte counts, and bilirubin levels after 2 years of treatment in a 23-year-old sitosterolemic patient [53•]. However, ezetimibe did not affect platelet counts, which remained low, and plasma plant sterol levels remained high, with only a mild reduction in campestanol concentration, thereby suggesting that this drug may not improve all features of sitosterolemia [53•]. In contrast, the addition of ezetimibe to a cholestyramine regimen further reduced plasma plant sterol levels and normalized platelet counts [57].
Several studies indicated that the immature intestine is able to absorb higher amounts of cholesterol compared with that of adults (reviewed in [59]). This could be related to the abnormal very high cholesterol levels in pediatric sitosterolemic patients [5]. One study found that two sitosterolemic patients younger than 2 years old did not respond to treatment with ezetimibe [60]. The study authors hypothesized that the immature glucuronidation system of infants may affect the generation of ezetimibe-related glucuronide metabolites, which have a higher affinity for binding to NPC1L1 [61], thereby limiting the effectiveness of ezetimibe in these infants. In this context, cholesterol levels started to improve in these sitosterolemic children when the therapy was restarted at 2 years of age [60].
Conclusions
Recent reports have shown that the characteristic hematological abnormalities of sitosterolemia may often be misdiagnosed, with the disease being confused with other types of chronic thrombocytopenias, thus supporting the concept that this disease may not be as rare as previously thought. A diagnosis based on the plasma concentration of plant sterols and/or ABCG5 and ABCG8 gene sequencing may be appropriate in certain clinical circumstances when hematological abnormalities remain unexplained. Investigations in mouse models of sitosterolemia have shown that accumulation of plant sterols disrupts cholesterol metabolism in the liver and adrenal glands and causes severe cardiac lesions. Accumulation of plant sterols also had negative effects on adipose tissue function, fertility, and triglyceride metabolism in these mouse models, but these features were not found consistently in sitosterolemic patients. Long-term follow-up treatment with ezetimibe appears to be a promising therapy, with patients showing a good response with regard to plant sterol levels. However, further studies are needed to prove its effectiveness in reducing the severity of other features of sitosterolemia.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Patel SB, Salen G, Hidaka H, Kwiterovich PO, Stalenhoef AF, Miettinen TA, et al. Mapping a gene involved in regulating dietary cholesterol absorption. The sitosterolemia locus is found at chromosome 2p21. J Clin Invest. 1998;102(5):1041–4.
Berge KE, Tian H, Graf GA, Yu L, Grishin NV, Schultz J, et al. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science. 2000;290(5497):1771–5.
Lee MH, Lu K, Hazard S, Yu H, Shulenin S, Hidaka H, et al. Identification of a gene, ABCG5, important in the regulation of dietary cholesterol absorption. Nat Genet. 2001;27(1):79–83.
Kidambi S, Patel SB. Sitosterolaemia: pathophysiology, clinical presentation and laboratory diagnosis. J Clin Pathol. 2008;61(5):588–94.
Merkens LS, Myrie SB, Steiner RD, Mymin D. Sitosterolemia. In: Pagon RA, Adam MP, Ardinger HH, Bird TD, Dolan CR, Fong C-T, Smith RJH, Stephens K, editors. GeneReviews. Seattle: University of Washington; 1993–2014. http://www.ncbi.nlm.nih.gov/books/NBK131810/.
Salen G, Shefer S, Nguyen L, Ness GC, Tint GS, Shore V. Sitosterolemia. J Lipid Res. 1992;33(7):945–55.
Othman RA, Myrie SB, Jones PJ. Non-cholesterol sterols and cholesterol metabolism in sitosterolemia. Atherosclerosis. 2013;231(2):291–9. This timely review discusses recent findings on sterol metabolism alterations in sitosterolemic patients.
Hazard SE, Patel SB. Sterolins ABCG5 and ABCG8: regulators of whole body dietary sterols. Pflugers Arch. 2007;453(5):745–52.
Lu K, Lee MH, Yu H, Zhou Y, Sandell SA, Salen G, et al. Molecular cloning, genomic organization, genetic variations, and characterization of murine sterolin genes Abcg5 and Abcg8. J Lipid Res. 2002;43(4):565–78.
Yu H, Pandit B, Klett E, Lee MH, Lu K, Helou K, et al. The rat STSL locus: characterization, chromosomal assignment, and genetic variations in sitosterolemic hypertensive rats. BMC Cardiovasc Disord. 2003;3:4.
Lee MH, Gordon D, Ott J, Lu K, Ose L, Miettinen T, et al. Fine mapping of a gene responsible for regulating dietary cholesterol absorption; founder effects underlie cases of phytosterolaemia in multiple communities. Eur J Hum Genet. 2001;9(5):375–84.
Heum Park J, Chung IH, Hyun Kim D, Ho Choi M, Garg A, Yoo EG. Sitosterolemia presenting with severe hypercholesterolemia and intertriginous xanthomas in a breastfed infant: case report and brief review. J Clin Endocrinol Metab. 2014. doi:10.1210/jc.2013-3274.
Wang J, Joy T, Mymin D, Frohlich J, Hegele RA. Phenotypic heterogeneity of sitosterolemia. J Lipid Res. 2004;45(12):2361–7.
Wang Z, Cao L, Su Y, Wang G, Wang R, Yu Z, et al. Specific macrothrombocytopenia/hemolytic anemia associated with sitosterolemia. Am J Hematol. 2014;89(3):320–4.
Calpe-Berdiel L, Escola-Gil JC, Blanco-Vaca F. New insights into the molecular actions of plant sterols and stanols in cholesterol metabolism. Atherosclerosis. 2009;203(1):18–31.
Davis Jr HR, Zhu LJ, Hoos LM, Tetzloff G, Maguire M, Liu J, et al. Niemann-Pick C1 like 1 (NPC1L1) is the intestinal phytosterol and cholesterol transporter and a key modulator of whole-body cholesterol homeostasis. J Biol Chem. 2004;279(32):33586–92.
Tang W, Ma Y, Jia L, Ioannou YA, Davies JP, Yu L. Genetic inactivation of NPC1L1 protects against sitosterolemia in mice lacking ABCG5/ABCG8. J Lipid Res. 2009;50(2):293–300.
Garcia-Calvo M, Lisnock J, Bull HG, Hawes BE, Burnett DA, Braun MP, et al. The target of ezetimibe is Niemann-Pick C1-like 1 (NPC1L1). Proc Natl Acad Sci U S A. 2005;102(23):8132–7.
Yamanashi Y, Takada T, Suzuki H. Niemann-Pick C1-like 1 overexpression facilitates ezetimibe-sensitive cholesterol and β-sitosterol uptake in CaCo-2 cells. J Pharmacol Exp Ther. 2007;320(2):559–64.
Kwon HJ, Palnitkar M, Deisenhofer J. The structure of the NPC1L1 N-terminal domain in a closed conformation. PLoS One. 2011;6(4):e18722.
Temel RE, Gebre AK, Parks JS, Rudel LL. Compared with acyl-CoA:cholesterol O-acyltransferase (ACAT) 1 and lecithin:cholesterol acyltransferase, ACAT2 displays the greatest capacity to differentiate cholesterol from sitosterol. J Biol Chem. 2003;278(48):47594–601.
Nguyen TM, Sawyer JK, Kelley KL, Davis MA, Kent CR, Rudel LL. ACAT2 and ABCG5/G8 are both required for efficient cholesterol absorption in mice: evidence from thoracic lymph duct cannulation. J Lipid Res. 2012;53(8):1598–609.
Myrie SB, Mymin D, Triggs-Raine B, Jones PJ. Serum lipids, plant sterols, and cholesterol kinetic responses to plant sterol supplementation in phytosterolemia heterozygotes and control individuals. Am J Clin Nutr. 2012;95(4):837–44.
Brauner R, Johannes C, Ploessl F, Bracher F, Lorenz RL. Phytosterols reduce cholesterol absorption by inhibition of 27-hydroxycholesterol generation, liver X receptor α activation, and expression of the basolateral sterol exporter ATP-binding cassette A1 in Caco-2 enterocytes. J Nutr. 2013;142(6):981–9. This article shows that plant sterols interfere with the formation of 27-hydroxycholesterol in intestinal cells and repress ABCA1-mediated incorporation of cholesterol into HDL.
Abumrad NA, Davidson NO. Role of the gut in lipid homeostasis. Physiol Rev. 2012;92(3):1061–85.
Miettinen TA, Klett EL, Gylling H, Isoniemi H, Patel SB. Liver transplantation in a patient with sitosterolemia and cirrhosis. Gastroenterology. 2006;130(2):542–7.
Park Y, Carr TP. Unsaturated fatty acids and phytosterols regulate cholesterol transporter genes in Caco-2 and HepG2 cell lines. Nutr Res. 2013;33(2):154–61.
Rosenblat M, Volkova N, Aviram M. Pomegranate phytosterol (β-sitosterol) and polyphenolic antioxidant (punicalagin) addition to statin, significantly protected against macrophage foam cells formation. Atherosclerosis. 2013;226(1):110–7.
Kruit JK, Drayer AL, Bloks VW, Blom N, Olthof SG, Sauer PJ, et al. Plant sterols cause macrothrombocytopenia in a mouse model of sitosterolemia. J Biol Chem. 2008;283(10):6281–7.
Yang C, Yu L, Li W, Xu F, Cohen JC, Hobbs HH. Disruption of cholesterol homeostasis by plant sterols. J Clin Invest. 2004;114(6):813–22.
Solca C, Tint GS, Patel SB. Dietary xenosterols lead to infertility and loss of abdominal adipose tissue in sterolin-deficient mice. J Lipid Res. 2013;54(2):397–409. This study explores the mechanisms by which two mouse models of sitosterolemia show infertility and loss of abdominal fat.
Mushtaq T, Wales JK, Wright NP. Adrenal insufficiency in phytosterolaemia. Eur J Endocrinol. 2007;157 Suppl 1:S61–5.
Mymin D, Wang J, Frohlich J, Hegele RA. Image in cardiovascular medicine. Aortic xanthomatosis with coronary ostial occlusion in a child homozygous for a nonsense mutation in ABCG8. Circulation. 2003;107(5):791.
Cheng WF, Yuen YP, Chow CB, Au KM, Chan YW, Tam SC. Sitosterolaemia and xanthomatosis in a child. Hong Kong Med J. 2003;9(3):206–9.
Salen G, Horak I, Rothkopf M, Cohen JL, Speck J, Tint GS, et al. Lethal atherosclerosis associated with abnormal plasma and tissue sterol composition in sitosterolemia with xanthomatosis. J Lipid Res. 1985;26(9):1126–33.
Bao L, Li Y, Deng SX, Landry D, Tabas I. Sitosterol-containing lipoproteins trigger free sterol-induced caspase-independent death in ACAT-competent macrophages. J Biol Chem. 2006;281(44):33635–49.
Sabeva NS, McPhaul CM, Li X, Cory TJ, Feola DJ, Graf GA. Phytosterols differentially influence ABC transporter expression, cholesterol efflux and inflammatory cytokine secretion in macrophage foam cells. J Nutr Biochem. 2011;22(8):777–83.
Rubis B, Paszel A, Kaczmarek M, Rudzinska M, Jelen H, Rybczynska M. Beneficial or harmful influence of phytosterols on human cells? Br J Nutr. 2008;100(6):1183–91.
O'Callaghan Y, McCarthy FO, O'Brien NM. Recent advances in phytosterol oxidation products. Biochem Biophys Res Commun. 2014. doi:10.1016/j.bbrc.2014.01.148.
McDaniel AL, Alger HM, Sawyer JK, Kelley KL, Kock ND, Brown JM, et al. Phytosterol feeding causes toxicity in ABCG5/G8 knockout mice. Am J Pathol. 2013;182(4):1131–8. This study shows that a high-plant-sterol diet is extremely toxic to sitosterolemic mice and induces liver abnormalities and severe cardiac lesions.
Mendez-Gonzalez J, Julve J, Rotllan N, Llaverias G, Blanco-Vaca F, Escola-Gil JC. ATP-binding cassette G5/G8 deficiency causes hypertriglyceridemia by affecting multiple metabolic pathways. Biochim Biophys Acta. 2011;1811(12):1186–93.
Su K, Sabeva NS, Liu J, Wang Y, Bhatnagar S, van der Westhuyzen DR, et al. The ABCG5 ABCG8 sterol transporter opposes the development of fatty liver disease and loss of glycemic control independently of phytosterol accumulation. J Biol Chem. 2011;287(34):28564–75.
Mannucci L, Guardamagna O, Bertucci P, Pisciotta L, Liberatoscioli L, Bertolini S, et al. Beta-sitosterolaemia: a new nonsense mutation in the ABCG5 gene. Eur J Clin Invest. 2007;37(12):997–1000.
Salen G, von Bergmann K, Lutjohann D, Kwiterovich P, Kane J, Patel SB, et al. Ezetimibe effectively reduces plasma plant sterols in patients with sitosterolemia. Circulation. 2004;109(8):966–71.
Hidaka H, Nakamura T, Aoki T, Kojima H, Nakajima Y, Kosugi K, et al. Increased plasma plant sterol levels in heterozygotes with sitosterolemia and xanthomatosis. J Lipid Res. 1990;31(5):881–8.
Su Y, Wang Z, Yang H, Cao L, Liu F, Bai X, et al. Clinical and molecular genetic analysis of a family with sitosterolemia and co-existing erythrocyte and platelet abnormalities. Haematologica. 2006;91(10):1392–5.
Rees DC, Iolascon A, Carella M, O'Marcaigh AS, Kendra JR, Jowitt SN, et al. Stomatocytic haemolysis and macrothrombocytopenia (Mediterranean stomatocytosis/macrothrombocytopenia) is the haematological presentation of phytosterolaemia. Br J Haematol. 2005;130(2):297–309.
Chase TH, Lyons BL, Bronson RT, Foreman O, Donahue LR, Burzenski LM, et al. The mouse mutation “thrombocytopenia and cardiomyopathy” (trac) disrupts Abcg5: a spontaneous single gene model for human hereditary phytosterolemia/sitosterolemia. Blood. 2010;115(6):1267–76.
Kanaji T, Kanaji S, Montgomery RR, Patel SB, Newman PJ. Platelet hyperreactivity explains the bleeding abnormality and macrothrombocytopenia in a murine model of sitosterolemia. Blood. 2013;122(15):2732–42. This study describes the mechanistic impact of plant sterols on the platelet phenotype and functionality in a mouse model of sitosterolemia.
Matsuo M. ATP-binding cassette proteins involved in glucose and lipid homeostasis. Biosci Biotechnol Biochem. 2010;74(5):899–907.
Wang G, Cao L, Wang Z, Jiang M, Sun X, Bai X, et al. Macrothrombocytopenia/stomatocytosis specially associated with phytosterolemia. Clin Appl Thromb Hemost. 2012;18(6):582–7. This study highlights a clinically relevant concern for physicians in recognizing blood cell dysmorphologies associated with sitosterolemia, with most sitosterolemic patients studied initially misdiagnosed with other chronic thrombocytopenias and, consequently, treated incorrectly.
Neff AT. Sitosterolemia's stomatocytosis and macrothrombocytopenia. Blood. 2012;120(22):4283.
Quintás-Cardama A, McCarthy JJ. Long-term follow-up of a patient with sitosterolemia and hemolytic anemia with excellent response to ezetimibe. J Genet Disord Genet Rep. 2013;2:1. This short report describes the long-term follow-up of a patient with sitosterolemia associated with hemolytic anemia, successfully managed with ezetimibe.
Tsubakio-Yamamoto K, Nishida M, Nakagawa-Toyama Y, Masuda D, Ohama T, Yamashita S. Current therapy for patients with sitosterolemia – effect of ezetimibe on plant sterol metabolism. J Atheroscler Thromb. 2010;17(9):891–900.
Connor WE, Lin DS, Pappu AS, Frohlich J, Gerhard G. Dietary sitostanol and campestanol: accumulation in the blood of humans with sitosterolemia and xanthomatosis and in rat tissues. Lipids. 2005;40(9):919–23.
Solca C, Stanga Z, Pandit B, Diem P, Greeve J, Patel SB. Sitosterolaemia in Switzerland: molecular genetics links the US Amish-Mennonites to their European roots. Clin Genet. 2005;68(2):174–8.
Salen G, Starc T, Sisk CM, Patel SB. Intestinal cholesterol absorption inhibitor ezetimibe added to cholestyramine for sitosterolemia and xanthomatosis. Gastroenterology. 2006;130(6):1853–7.
Hung C-N, Lee C-Y. A case of sitosterolaemia with stomatocyticanaemia and thrombocytopenia treated with ezetimibe with good response. Int J Pediatr Endocrinol. 2013;2013 Suppl 1:174.
Drozdowski LA, Clandinin T, Thomson AB. Ontogeny, growth and development of the small intestine: understanding pediatric gastroenterology. World J Gastroenterol. 2010;16(7):787–99.
Niu DM, Chong KW, Hsu JH, Wu TJ, Yu HC, Huang CH, et al. Clinical observations, molecular genetic analysis, and treatment of sitosterolemia in infants and children. J Inherit Metab Dis. 2010;33(4):437–43.
Davis HR, Veltri EP. Zetia: inhibition of Niemann-Pick C1 like 1 (NPC1L1) to reduce intestinal cholesterol absorption and treat hyperlipidemia. J Atheroscler Thromb. 2007;14(3):99–108.
Acknowledgments
This work was partly funded by the Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III, CP13-00070 (to Josep Julve), CD12-00533 (to Helena Quesada), FIS 11-0176 (to Francisco Blanco-Vaca), and FIS 12-00291 (to Joan Carles Escolà-Gil).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Joan Carles Escolà-Gil, Helena Quesada, Josep Julve, Jesús M. Martín-Campos, Lídia Cedó, and Francisco Blanco-Vaca declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Joan Carles Escolà-Gil and Helena Quesada contributed equally to this work.
This article is part of the Topical Collection on Rare Diseases and Lipid Metabolism
Rights and permissions
About this article
Cite this article
Escolà-Gil, J.C., Quesada, H., Julve, J. et al. Sitosterolemia: Diagnosis, Investigation, and Management. Curr Atheroscler Rep 16, 424 (2014). https://doi.org/10.1007/s11883-014-0424-2
Published:
DOI: https://doi.org/10.1007/s11883-014-0424-2