Abstract
The clinical observation and treatment of young children with sitosterolemia has rarely been reported. We report clinical, biochemical, and molecular genetic observations and treatment outcomes for five Chinese children from four separate families presenting with sitosterolemia in whom we identified two new (Y329X, G269R) and three known (R446X, N437K, R389H) mutations in the ABCG5 gene. The R389H mutation was found in 50% of alleles. Three of these five patients received cholestyramine therapy with a very good response. However, all patients discontinued this therapy because of poor compliance. Finally, all patients were on ezetimibe therapy and had satisfactory total serum cholesterol levels, though their plant sterol levels were still higher than normal. Another noteworthy finding is that a female infant had a serum cholesterol level of 654 mg/dl at 7 months of age, despite being breast fed (with very tiny amounts of plant sterols) since birth and undergoing 4 months of ezetimibe administration. Although she failed to respond to ezetimibe during this period, she did show improvement when the therapy was started again at 2 years of age. It is possible that another 23-month-old female patient also responded more slowly to ezetimibe treatment than older patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sitosterolemia (MIM# 210250), also known as phytosterolemia, is a rare, inherited, autosomal recessive disorder of lipid metabolism characterized by increased absorption and decreased biliary excretion of plant sterols and cholesterol, resulting in prominently elevated plasma concentrations of plant sterols (such as sitosterol, sitostanol, campesterol and stigmasterol) (Bhattacharyya and Connor 1974; Salen et al. 1985) and low-density-lipoprotein (LDL) cholesterol in most pediatric patients (McArthur et al. 1986; Lee et al. 2001a, b). Patients suffering from sitosterolemia present primarily with tendinous and tuberous xanthomas, premature coronary and aortic atherosclerosis, arthralgia and arthritis, and, occasionally, abnormal liver function tests, hemolysis, or thrombocytopenia (Bjorkhem et al. 2001; Rees et al. 2005). The genetic defect in sitosterolemia was recently mapped to chromosome 2p21 (Patel et al. 1998a, b) and the disease attributed to mutations in one of two newly described, adjacent, half-size sterol adenosine triphosphate (ATP)-binding cassette transporters, ABCG5 (sterolin-1, MIM# 605459) and ABCG8 (sterolin-2, MIM# 605460) (Berge et al. 2000; Lee et al. 2001a, b). Thus far, 25 mutations of ABCG8 and 16 mutations of ABCG5 have been described (Berge et al. 2000; Lee et al. 2001a, b; Lu et al. 2001; Hubacek et al. 2001; Heimerl et al. 2002; Lam et al. 2002; Mymin et al. 2003; Wang et al. 2004; Su et al. 2006; Mannucci et al. 2007; Togo et al. 2008). It is noteworthy that most Asian probands presenting with sitosterolemia have mutations in ABCG5, whereas most probands of Caucasian origin have mutations in ABCG8 (Lu et al. 2001). We studied and report here the clinical, biochemical, and molecular genetic characteristics and treatment outcomes of five young Chinese children with sitosterolemia identified from four separate families.
Patients: characteristics and clinical observations
Patient 1, an 8-year-old girl, was brought to our genetics clinic by her mother who had recently noted the presence of multiple xanthomas over her heels and elbows. The serum lipid analysis, using Hitachi 7600 instrumentation (Hitachi High-Technologies, Tokyo, Japan), revealed the presence of 427 mg/dl total, 346 mg/dl LDL, and normal high-density-lipoprotein (HDL) cholesterol concentrations and normal total triglycerides (Table 1). Alanine transaminase (ALT) and aspartate aminotransferase (AST) were normal, and the peripheral blood count revealed a mild normochromic anemia and platelets within normal limits (Table 1). Since both parents had normal serum lipid profiles, sitosterolemia or autosomal recessive hypercholesterolemia was suspected. Large peaks of serum plant sterols were identified by nuclear magnetic resonance (NMR) spectroscopy, but the exact concentrations of these sterols were unable to be determined at a local lipid research laboratory. After 10 days of treatment with cholestyramine (1 g four times daily), coincidentally, the patient developed a right lower-lobe pneumonia and was admitted to our hospital. On the day of admission, total cholesterol had decreased to 116 mg/dl and hemoglobin to 7.8 g/dl. Further hematologic tests revealed the presence of slight erythrocyte anisocytosis and polychromasia, normal platelet morphology and count, normal direct and indirect Coomb’s test, a positive autohemolysis test, and an elevated haptoglobin concentration of 407 mg/dl (normal range 30–200). When discharged from the hospital 7 days later, hemoglobin had returned to 9.8 g/dl. However, treatment with cholestyramine was discontinued by the parents, who kept the patient on a sterol-restricted diet and did not return for follow-up appointments until 5 years later. At this time, a physical examination indicated that the multiple xanthomas had completely disappeared and the lipid profile had normalized (total: 191 mg/dl, LDL: 135 mg/dl). The peripheral blood count revealed hemoglobin of 10.2 g/dl and a platelet count of 494,000 cells/mm3. The morphologies of platelets and erythrocytes were normal in the peripheral blood smear. Liver function tests also were normal.
Patient 2, an 18-month-old girl, was seen in our clinic for evaluation of multiple xanthomas on her heels, knees, and elbows. Her mother first noted the presence of flat yellow streaks on both heels when she was 3 months of age. Laboratory analyses showed 705 mg/dl total, 565 mg/dl LDL, and normal HDL cholesterol concentrations, normal total triglycerides, and normal ALT, AST, and peripheral blood counts (Table 1). The morphologies of platelets and erythrocytes were normal in the peripheral blood smear. The lipid profiles of both parents were normal. Cholestyramine was administered at 1 g four times daily, and within 1 month, total cholesterol had decreased to 152 mg/dl and LDL cholesterol to 71 mg/dl. HDL cholesterol was 67 mg/dl. The xanthomas disappeared gradually over 8 months of treatment. However, because of poor compliance and an increase in total cholesterol to 360 mg/dl, cholestyramine was replaced 1 year later by ezetimibe, 10 mg daily, which was well-tolerated. After 1 month of ezetimibe treatment, total cholesterol decreased to 176 mg/dl and serum lipid profile remained within normal limits for >2 years. However, after 3 years of ezetimibe therapy, her plasma plant sterol concentrations remained high (Table 1), although serum total cholesterol level was normal (181 mg/dl).
Patient 3, a younger sister of patient 2, was born after her sister’s diagnosis of sitosterolemia was made. No prenatal investigations were undertaken, and she was first seen in our clinic at the age of 3 months. Although she was breast feeding, serum lipid analysis revealed the presence of 402 mg/dl total and 304 mg/dl LDL cholesterol concentrations. The peripheral blood count was normal except for a high platelet count. The morphologies of erythrocytes and platelets were normal, ALT was at the upper limit of normal, and AST was elevated (Table 1). Upon the parents’ request, ezetimibe treatment was begun at 5 mg daily with a gradual increase to 10 mg daily. However, despite 4 months of ezetimibe administration, serum cholesterol rose to 654 mg/dl, whereas ALT decreased to 31 U/l, AST to 67 U/l, and platelet count to 410,000/mm3. Treatment with ezetimibe was replaced by cholestyramine 0.5 gm four times daily, which, within 1 month, lowered the total serum cholesterol concentration to 220 mg/dl and LDL cholesterol concentration to 140 mg/dl, ALT to 17 and AST to 45 U/l, and the platelet count to 375,000/mm3. At 2 years of age, the patient began refusing treatment with cholestyramine, and total cholesterol gradually increased to 364 mg/dl. Because of the compliance and effectiveness observed in her sister, treatment with ezetimibe was resumed at a daily dose of 10 mg, and total cholesterol decreased to 269 mg/dl within 2 months and 206 mg/dl within 3 months. After 1 year of ezetimibe treatment, her total cholesterol level had dropped to 208 mg/dl, but plant sterol concentrations remained elevated (Table 1).
Patient 4, a 23-month-old girl, was referred to our clinic for evaluation of multiple xanthomas on her heels, knees, and elbows. Her parents first noted the presence of flat, yellow streaks on both heels when she was approximately 10 months of age. Serum lipid analysis revealed 640 mg/dl total, 519 mg/dl LDL, and normal HDL cholesterol concentrations and normal total triglycerides (Table 1). ALT and AST were within the normal range (Table 1), as were the peripheral blood counts, except for a prominent thrombocytosis (Table 1). The morphologies of erythrocytes and platelets were normal. Parental serum lipid profiles were normal. Ezetimibe was prescribed at 10 mg/day, and serum cholesterol gradually decreased to 569 mg/dl within 1 month, 357 mg/dl within 3 months, and 245 mg/dl within 4 months of treatment. After 1 year of ezetimibe therapy, her total cholesterol level was 223 mg/dl, but plant sterol concentrations remained elevated.
Patient 5, a 12 year-old girl, was referred to our clinic for evaluation of persistent hypercholesterolemia. Her mother first noted the presence of multiple xanthomas on both knees when she was approximately 4 years of age. Hypercholesterolemia (372 mg/dl) was noted at 10 years of age. Because both parents had mild elevations of serum cholesterol (around 240 mg/dl), a mild form of homozygous familial hypercholesterolemia was suspected. A statin drug (atorvastatin, 10 mg/day) was prescribed but without significant response, and analysis of the LDL receptor gene was negative for both the patient and her parents. Initial data for lipid profile, peripheral blood count, and liver function are shown in Table 1. When the statin was discontinued and ezetimibe therapy initiated at 10 mg/daily, total cholesterol decreased to 213 mg/dl within 2 months. After about 6 months of ezetimibe treatment, her total cholesterol level was 193 mg/dl, but her plant sterol concentrations remained elevated (Table 1).
Method of the ABCG5/G8 gene analysis
Genomic DNA was extracted from peripheral leucocytes using a standard procedure. The patients or their parents were informed of the mutation analysis and granted their written consent to participate. Primers used for genomic amplification and sequencing of ABCG5 and ABCG8 were according to a previous report (Hubacek et al. 2001). Polymerase chain reaction (PCR) conditions for each primer were optimized in our laboratory. Cycle sequencing was performed using the original primers and a commercial kit (PerkinElmer) to amplify the PCR products. The sequence was analyzed using an ABI PRISM® 3730 automatic DNA sequencer (PerkinElmer). All procedures followed the instructions supplied by the manufacturer.
Results of mutation analyses
Patient 1 had compound heterozygous mutations, p.Y329X and p.N437K. The new mutation, p.Y329X (c.987C>A), located in exon 8, substituted an amino acid codon (tyrosine) to a stop codon at codon 329. The other mutation, N437K (c.1311C>G), located in exon 9, substituted an asparagine to a lysine at codon 437. This mutation has been previously described in a Chinese patient (Hubacek et al. 2001). Patients 2 and 3 also had compound heterozygous mutations (R389H and R446X). R389H (c.1166G>A), located in exon 9, caused an arginine to be replaced by a histidine at codon 389. This mutation is common in Japanese patients suffering from sitosterolemia (Lee et al. 2001a, b). R446X (c.1336C>T), located at exon 10, substituted an arginine codon for a stop codon at codon 446. This mutation was recently observed in a family of Iranian origin (Mannucci et al. 2007). Patient 4 had a homozygous mutation, R389H. Patient 5 had compound heterozygous mutations, p.R389H and p.G269R. The p.G269R (c.850G>A) mutation, located in exon 7, substituted a glycine for an arginine at codon 269. This codon is highly conserved among human ABCG transporters (ABCG1–5) (Graf et al. 2003). This new mutation, p.G269R, was not detected in 50 healthy controls.
Discussion
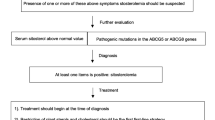
Xanthomatosis is rarely observed in pediatric patients. When present, homozygous familial hypercholesterolemia due to an LDL receptor defect is most often suspected (Sethuraman et al. 2007). However, sitosterolemia (Yoshida et al. 2000), cerebrotendinous xanthomatosis (Moghadasian 2004), and autosomal recessive hypercholesterolemia (Thomas et al. 2004) should also be considered. Other familial hypercholesterolemia, such as familial defective apoB 100 or gain of function mutations in PCSK9 gene might also cause hypercholesterolemia in children. However, they rarely cause xanthomatosis in this age group (Naoumova et al. 2005, Schaefer et al. 1997). An accurate diagnosis is critical, as each disease mandates different treatments and has a different prognosis. Patients with homozygous familial hypercholesterolemia can be clinically distinguished from other children with xanthomatosis by the presence of hypercholesterolemia in both parents, whereas patients with cerebrotendinous xanthomatosis can be identified by an elevation of serum cholestanol (but a normal cholesterol concentration), the presence of an early childhood onset protracted diarrhea and failure to thrive, late-childhood-onset cataracts, and adult-onset neurological involvements (Berginer et al. 2009). Measuring serum plant sterol levels is the most reliable diagnostic test for sitosterolemia. Unfortunately, routine clinical analytical colorimetric and enzymatic methods cannot distinguish plant sterols from cholesterol and require more sophisticated methods, such as high-performance liquid or capillary gas chromatography. However, these methods may not be available in most clinical laboratories, particularly outside the Western world. Therefore, our patients were confirmed to have sitosterolemia by mutational analysis of ABCG5 and ABCG8 genes.
Most of the pediatric patients with sitosterolemia not only have elevated serum plant sterols, but also have significantly elevated serum cholesterol levels (Lee et al. 2001a, b, Low et al. 1991, Yoshida et al. 2000). Sometimes, the cholesterol levels could be as high as 1,000 mg/dl, though these levels do not seem to be present in adult cases (Lee et al. 2001a, b). Some of these children were initially diagnosed with pseudohomozygous hypercholesterolemia based on the high cholesterol levels, but no defects in the LDL-receptor activities were identified (Morganroth et al. 1974, Masana et al. 1990). With time, these seemed to fall, though Patel and coworkers rediagnosed some of these individuals as suffering from sitosterolemia (Lee et al. 2001a, Lee et al. 2001b, Lu et al. 2001). Why are the cholesterol levels so elevated in children? One possibility is that the LDL-receptor activity in the liver could be initially potentially suppressed by the accumulation of plant sterols, resulting in suppression of synthesis and LDL-R activity mediated by sterol regulatory element binding protein (SREBP) pathway (Brown and Goldstein 1997). Interestingly, in adult sitosterolemia, there is dissociation between regulation of LDL receptor expression and 3-hydroxy-3-methylglutaryl-coenzyme A (HMG CoA) reductase, where the liver shows increased LDL-R expression in the face of suppressed HMG CoA reductase, as well as other cholesterol synthesis enzymes (Nguyen et al. 1990, Patel et al. 1998b). This may highlight a difference between liver sterol regulation between adults and children.
In this study, patient 3 was noted to have very high plasma cholesterol levels, even though she had only been breast fed. This finding suggests that hyperabsorption of cholesterol can occur without concurrent intake of plant sterols. It also reminds us that besides plant sterols, the hyperabsorption of cholesterol in young patients is also an important pathogenic factor. Premature atherosclerosis and early onset myocardial infarction, as early as 5 years of age, has been reported in a patient with sitosterolemia (Wang et al. 2004). Therefore, early therapeutic intervention is warranted. However, treatment of young children with sitosterolemia has rarely been described. Although patient 1 responded favorably to a low-sterol diet, a sterol-restricted diet is very difficult for most patients to adhere to and sometimes causes a paradoxical increase in plasma plant sterol concentrations (Nguyen et al. 1991). Bile acid sequestrants (cholestyramine) have been reported to be able to reduce about 50% of serum total sterols in patients with sitosterolemia (Wang et al. 2004, Parsons et al. 1995, Belamarich et al. 1990). However, some Japanese families were reported to show poor response to cholestyramine (Hidaka et al. 1990). In our study, the youngest group ever reported, all patients who received cholestyramine had a rapid therapeutic response.
However, compliance with cholestyramine is problematic, owing to its inconvenient administration (the unpleasant texture of cholestyramine) and gastrointestinal adverse effects, including abdominal bloating and loss of appetite in our patients. Ezetimibe, a new cholesterol-lowering agent that blocks Niemann-Pick C1-like 1 (NPC1L1), a putative cholesterol receptor, limits the entry of cholesterol and noncholesterol sterols across the intestinal wall but does not interfere with the absorption of triglycerides, bile or fatty acids, and fat-soluble vitamins. Recently, several studies showed that ezetimibe lowered plasma plant sterol concentrations significantly in patients with sitosterolemia (Salen et al. 2004; Lütjohann et al. 2008, Musliner et al. 2008). In these studies, all participants were older than 10 years of age. In our study, patient 2, who received ezetimibe at the age of 3 years, responded readily to therapy, whereas the response of patient 4, who received ezetimibe at 2 years of age, was slower. In contrast with adult sitosterolemia patients who typically reached full treatment response within 2–8 weeks of treatment (Salen et al. 2004), 4 months of treatment was required to significantly lower the cholesterol level in patient 4. It is noteworthy that patient 3, a younger sister of patient 2, did not respond to ezetimibe at all at 3 months of age. (The parents assured us that they gave ezetimibe properly to the child, but whether this was the case was not confirmed by scientific methods, such as measuring serum level of ezetimibe, etc.). However, she responded fully after 3 months of treatment when the drug was administered 2 years later. The precise mechanism behind the poor response in infants is unknown, but several hypotheses include: (1) poor ezetimibe absorption, (2) failure of ezetimibe to undergo glucuronidation in the intestine, (3) failure of glucuronidated ezetimibe secretion into bile, or (4) failure of ezetimibe to interact with NPC1L1 in the gut. Since a glucuronide of ezetimibe is more effective than the parent compound in inhibiting the absorption of cholesterol (Van Heek et al. 2000), and since hepatic glucuronidation is considerably weaker in human infants than in adults (Strassburg et al. 2002), we strongly suspect that the immature glucuronidation system of infants limits the effectiveness of ezetimibe. The use of ezetimibe has not previously been described in infants, and more studies are needed to further characterize the therapeutic properties of this drug in this age group.
Sitosterolemia can be associated with hemolysis and macrothrombocytopenia (Bjorkhem et al. 2001; Rees et al. 2005; Su et al. 2006). These findings are also seen in Abcg5 mice, and the development of abnormal platelets is reversible with ezetimibe treatment (Kruit et al. 2008). In this study, another noteworthy observation is the high prevalence of thrombocytosis observed among our patients, in contrast with other studies of sitosterolemia, in which a high prevalence of thrombocytopenia was observed (Bjorkhem et al. 2001; Rees et al. 2005). The different platelet profile observed in our patients versus those in other reports is unclear and might be an early manifestation of platelet dysfunction in young children with sitosterolemia, an observation that warrants further investigations.
In our patients, we found that total cholesterol levels were kept in or near the normal range and that xanthomas disappeared gradually after ezetimibe treatment. However, the levels of plant sterols remained elevated. Several studies indicate that mild elevations of plant sterols may increase the risk for cardiovascular disease (Rajaratnam et al. 2000; Sudhop et al. 2002). Do these patients still have high risk for cardiovascular disease later in life? What are the appropriate therapeutic goals for reducing serum plant sterol levels in these patients? Recently, Salen et al. (2006) reported using combination treatments of ezetimibe (10 mg) and cholestyramine (2 mg, a relatively low dosage) on an 11-year-old girl with sitosterolemia for 1 year and found that plant plasma sterol concentrations decreased by about 50%. Because of the unsatisfactory levels of plant sterols in our patients after ezetimibe therapy, we think it is reasonable to initiate a study using combination treatments of ezetimibe and cholestyramine. However, further investigations are still warranted.
In our findings, cholestyramine has the potential to control serum total cholesterol levels of sitosterolemia patients, even for very young children. However, children presenting with sitosterolemia who are <2 year of age might not respond well to treatment with ezetimibe. Further controlled clinical studies and more clinical data are necessary to verify these findings.
References
Belamarich PF, Deckelbaum RJ, Starc TJ, Dobrin BE, Tint GS, Salen G (1990) Response to diet and cholestyramine in a patient with sitosterolemia. Pediatrics 86:977–981
Berge KE, Tian H, Graf GA, Yu L, Grishin NV, Schultz J, Kwiterovich P, Shan B, Barnes R, Hobbs HH (2000) Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science 290:1771–1775
Berginer VM, Gross B, Morad K, Kfir N, Morkos S, Aaref S, Falik-Zaccai TC (2009) Chronic diarrhea and juvenile cataracts: think cerebrotendinous xanthomatosis and treat. Pediatrics 123:143–147
Bhattacharyya AK, Connor WE (1974) β-Sitosterolemia and xanthomatosis-a newly described lipid storage disease in two sisters. J Clin Invest 53:1033–1043
Bjorkhem I, Boberg KM, Leitersdorf E (2001) Inborn errors in bile acid biosynthesis and storage of sterols other than cholesterol. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic and molecular bases of inherited disease, 8th edn. McGraw-Hill, New York, pp 2961–2988
Brown MS, Goldstein JL (1997) The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell 89:331–340
Graf GA, Yu L, Li WP, Gerard R (2003) ABCG5 and ABCG8 are obligate heterodimers for protein trafficking and biliary cholesterol excretion. J Biol Chem 278:48275–48282
Heimerl S, Langmann T, Moehle C (2002) Mutations in the human ATP-binding cassette transporters ABCG5 and ABCG8 in sitosterolemia. Hum Mutat 20:151
Hidaka H, Nakamura T, Aoki T, Kojima H, Nakajima Y, Kosugi K, Hatanaka I, Harada M, Kobayashi M, Tamura A (1990) Increased plasma plant sterol levels in heterozygotes with sitosterolemia and xanthomatosis. J Lipid Res 31:881–888
Hubacek JA, Berge KE, Cohen JC, Hobbs HH (2001) Mutations in ATP-cassette binding proteins G5 (ABCG5) and G8 (ABCG8) causing sitosterolemia. Hum Mutat 18:359–360
Kruit JK, Drayer AL, Bloks VW (2008) Plant sterols cause macrothrombocytopenia in a mouse model of sitosterolemia. J Biol Chem 283:6281–6287
Kwiterovich PO Jr, Chen SC, Virgil DG, Schweitzer A, Arnold DR, Kratz LE (2003) Response of obligate heterozygotes for phytosterolemia to a low-fat diet and to a plant sterol ester dietary challenge. J Lipid Res 44:1143–1155
Lam CW, Cheng AW, Tong SF (2002) Novel donor splice site mutation of ABCG5 gene in sitosterolemia. Mol Genet Metab 75:178–180
Lee MH, Lu K, Hazard S, Yu H (2001a) Identification of a gene, ABCG5, important in the regulation of dietary cholesterol absorption. Nat Genet 27:79–83
Lee MH, Lu K, Patel SB (2001b) Genetic basis of sitosterolemia. Curr Opin Lipidol 12:141–149
Low LC, Lin HJ, Lau KS, Kung AW, Yeung CY (1991) Phytosterolemia and pseudohomozygous type II hypercholesterolemia in two Chinese patients. J Pediatr 118:746–749
Lu K, Lee MH, Hazard S, Brooks-Wilson A (2001) Two genes that map to the STSL locus cause sitosterolemia: genomic structure and spectrum of mutations involving sterolin-1 and sterolin-2, encoded by ABCG5 and ABCG8, respectively. Am J Hum Genet 69:278–290
Lütjohann D, von Bergmann K, Sirah W, Macdonell G, Johnson-Levonas AO, Shah A, Lin J, Sapre A, Musliner T (2008) Long-term efficacy and safety of ezetimibe 10 mg in patients with homozygous sitosterolemia: a 2-year, open-label extension study. Int J Clin Pract 62:1499–1510
Mannucci L, Guardamagna O, Bertucci P (2007) Beta-sitosterolaemia: a new nonsense mutation in the ABCG5 gene. Eur J Clin Invest 37:997–1000
Masana L, Joven J, Rubiés-Prat J, Lewis B (1990) Low density lipoprotein metabolism and receptor studies in a patient with pseudohomozygous familial hypercholesterolaemia. Acta Paediatr Scand 79(4):475–476
McArthur RG, Roncari DA, Little JA (1986) Phytosterolemia and hypercholesterolemia in childhood. J Pediatr 108:254–256
Moghadasian MH (2004) Cerebrotendinous xanthomatosis: clinical course, genotypes and metabolic backgrounds. Clin Invest Med 27:42–50
Morganroth J, Levy RI, McMahon AE, Gotto AM Jr (1974) Pseudohomozygous type II hyperlipoproteinemia. J Pediatr 85:639–643
Musliner T, Cselovszky D, Sirah W, McCrary Sisk C, Sapre A, Salen G, Lütjohann D, von Bergmann K (2008) Efficacy and safety of ezetimibe 40 mg vs. ezetimibe 10 mg in the treatment of patients with homozygous sitosterolaemia. Int J Clin Pract 62:995–1000
Mymin D, Wang J, Frohlich J (2003) Image in cardiovascular medicine. Aortic xanthomatosis with coronary ostial occlusion in a child homozygous for a nonsense mutation in ABCG8. Circulation 107:791
Naoumova RP, Tosi I, Patel D, Neuwirth C, Horswell SD, Marais AD, van Heyningen C, Soutar AK (2005) Severe hypercholesterolemia in four British families with the D374Y mutation in the PCSK9 gene: long-term follow-up and treatment response. Arterioscler Thromb Vasc Biol 25:2654–2660
Nguyen LB, Shefer S, Salen G, Ness GC, Tint GS, Zaki FG, Rani I (1990) A molecular defect in hepatic cholesterol biosynthesis in sitosterolemia with xanthomatosis. J Clin Invest 86:923–931
Nguyen LB, Cobb M, Shefer S (1991) Regulation of cholesterol biosynthesis in sitosterolemia: effects of lovastatin, cholestyramine, and dietary sterol restriction. J Lipid Res 32:1941–1948l
Patel SB, Salen G, Hidaka H (1998a) Mapping a gene involved in regulating dietary cholesterol absorption. The sitosterolemia locus is found at chromosome 2p21. J Clin Invest 102:1041–1044
Patel SB, Honda A, Salen G (1998b) Sitosterolemia: exclusion of genes involved in reduced cholesterol biosynthesis. J Lipid Res 39:1055–1061
Parsons HG, Jamal R, Baylis B (1995) A marked and sustained reduction in LDL sterols by diet and cholestyramine in sitosterolemia. Clin Invest Med 18:389–400
Rajaratnam RA, Gylling H, Miettinen TA (2000) Independent association of serum squalene and noncholesterol sterols with coronary artery disease in postmenopausal women. J Am Coll Cardiol 35:1185–1191
Rees DC, Iolascon A, Carella M (2005) Stomatocytic haemolysis and macrothrombocytopenia (Mediterranean stomatocytosis/ macrothrombocytopenia) is the haematological presentation of phytosterolaemia. Br J Haematol 130:297–309
Salen G, Kwiterovich PO Jr, Shefer S (1985) Increased plasma cholestanol and 5 alpha-saturated plant sterol derivatives in subjects with sitosterolemia and xanthomatosis. J Lipid Res 26:203–209
Salen G, Shefer S, Nguyen L (1992) Sitosterolemia. J Lipid Res 33:945–955
Salen G, von Bergmann K, Lütjohann D (2004) Multicenter sitosterolemia study group. Ezetimibe effectively reduces plasma plant sterols in patients with sitosterolemia. Circulation 109:966–971
Salen G, Starc T, Sisk CM (2006) Intestinal cholesterol absorption inhibitor ezetimibe added to cholestyramine for sitosterolemia and xanthomatosis. Gastroenterology 130:1853–1857
Sethuraman G, Sugandhan S, Sharma G et al (2007) Familial homozygous hypercholesterolemia: report of two patients and review of the literature. Pediatr Dermatol 24:230–234
Schaefer JR, Scharnagl H, Baumstark MW, Schweer H, Zech LA, Seyberth H, Winkler K, Steinmetz A, März W (1997) Homozygous familial defective apolipoprotein B 100. Enhaced removal of apolipoprotein E containing VLDLs and decreased production of LDLs. Arterioscler Thromb Vasc Biol 17:348–353
Su Y, Wang Z, Yang H et al (2006) Clinical and molecular genetic analysis of a family with sitosterolemia and co-existing erythrocyte and platelet abnormalities. Haematologica 91:1392–1395
Sudhop T, Gottwald BM, von Bergmann K (2002) Serum plant sterols as a potential risk factor for coronary heart disease. Metabolism 51:1519–1521
Strassburg CP, Strassburg A, Kneip S et al (2002) Developmental aspects of human hepatic drug glucuronidation in young children and adults. Gut 50:259–265
Thomas HP, Vogt A, Wilund KR et al (2004) Autosomal recessive hypercholesterolemia in three sisters with phenotypic homozygous familial hypercholesterolemia: diagnostic and therapeutic procedures. Ther Apher Dial 8:275–280
Togo M, Hashimoto Y, Iso-O N, Kurano M, Hara M, Kadowaki T, Koike K, Tsukamoto K (2008) Identification of a novel mutation for phytosterolemia. Genetic analyses of 2 cases. Clin Chim Acta 401:165–169
Van Heek M, Farley C, Compton DS et al (2000) Comparison of the activity and disposition of the novel cholesterol absorption inhibitor, SCH58235, and its glucuronide, SCH60663. Br J Pharmacol 129:1748–1754
Wang J, Joy T, Mymin D, Frohlich J et al (2004) Phenotypic heterogeneity of sitosterolemia. J Lipid Res 45:2361–2367
Yoshida A, Naito M, Miyazaki K (2000) Japanese sisters associated with pseudohomozygous familial hypercholesterolemia and sitosterolemia. J Atheroscler Thromb 7:33–38
Author information
Authors and Affiliations
Corresponding authors
Additional information
Communicated by: Robert Steiner
Competing interest: None declared.
Rights and permissions
About this article
Cite this article
Niu, DM., Chong, KW., Hsu, JH. et al. Clinical observations, molecular genetic analysis, and treatment of sitosterolemia in infants and children. J Inherit Metab Dis 33, 437–443 (2010). https://doi.org/10.1007/s10545-010-9126-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-010-9126-2