Abstract
A stroke system of care comprises a comprehensive, diverse, longitudinal system that addresses all aspects of stroke care in a coordinated manner. It includes the spectrum of stroke care from primary prevention to activation of emergency medical services, acute care, secondary prevention, rehabilitation and return to the community. Acute care for stroke can be initiated in acute stroke ready hospitals with subsequent transfer to either primary or comprehensive stroke centers. The attributes of an effective stroke system of care include coordinated care, customized to the local environment, able to make the best use of the resources available and that respects and maintains traditions of excellence. Care processes for patients with stroke can be improved through participation in certification and recognition programs such as the American Heart Association’s Get With The Guidelines-Stroke program. The final aim of stroke systems should be to integrate prevention and treatment and promote patient access to the best evidence-based care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stroke is the second leading cause of death globally. Approximately 800,000 American adults have a first or recurrent stroke each year, and stroke prevalence is projected to increase by 25 % between 2010 and 2030 [1••]. Additionally, the costs associated with stroke are considerable, with the estimated cost of stroke to the USA for 2010 being $53.9 billion. Moreover, direct medical costs for stroke management are expected to increase from $28.3 billion in 2010 to $95.6 billion by 2030, corresponding to a 238 % increase [1••, 2].
Patients with stroke treated at primary stroke centers (PSCs) are more likely to be alive, independent, and living at home 1 year after the stroke than those treated in general care hospitals. In the last two decades, stroke management has improved significantly, but unfortunately most patients with stroke are still not treated in the recommended therapeutic time window [3, 4•, 5]. In an observational registry–linkage study of patients with ischemic stroke treated in Finland, the number needed to treat to prevent one death or institutional care at 1 year compared with general non-stroke-center hospitals was 29 for comprehensive stroke centers (CSCs) and 40 for PSCs. Moreover, patients treated in stroke centers had lower mortality during the entire follow-up of up to 9 years and their median survival was increased by 1 year [4•].
The impact of reducing stroke mortality cannot be overemphasized. For example, a 2–3 % reduction in stroke deaths in the USA would mean 16,000–24,000 fewer deaths annually. Globally, this translates to 320,000–480,000 fewer stroke deaths each year [1••].
Definition of Stroke Systems of Care
Stroke systems of care comprise a comprehensive, diverse, longitudinal system that addresses all aspects of stroke care in an organized and coordinated manner. It includes the spectrum of stroke care from primary prevention to activation of emergency medical services (EMS), acute care, secondary prevention, rehabilitation, and return to the community. As with any system, stroke systems of care are only as strong as their weakest link [6].
The attributes of an effective stroke system of care include coordinated care, customized to the local environment, able to make the best use of the resources available and that respects and maintains traditions of excellence. Ideally, stroke systems should ensure effective interaction and collaboration among agencies, services, and key stakeholders, promote the use of a standardized approach in each facility and component of the system, identify performance measures, and include a mechanism for evaluating effectiveness throughout the entire system and its individual components. Stroke systems should also aim at continuous improvement to provide patients and health care professionals with the tools necessary to promote effective stroke prevention, treatment, and rehabilitation and also to ensure that decisions about protocols and patient care are based on what is in the best interests of stroke patients, identifying and addressing potential obstacles to successful implementation of processes [6, 7].
Prehospital Identification and Prenotification
EMS professionals are typically the first medical professionals with direct patient contact [8, 9]. Their initial assessments, actions, treatments, and decisions will have significant consequences for the patient’s subsequent care and even outcome. Their role in patient triage, diversion, and routing cannot be underestimated [10•].
Current EMS best practice when transporting stroke patients includes rapid prehospital care, routing directly to the PSC, prearrival notification, activation of the stroke team, and advice to make available a head CT/MRI scanner. Emerging practices include selective direct transport of selected patients to the CSC and administration of neuroprotective therapies as part of clinical trials [9, 11, 12]. The most innovative concept to be tested in the prehospital stroke arena recently involves a CT-equipped ambulance that is dispatched to the scene for on –scene evaluation and, when appropriate, “ambu-lysis” [13].
EMS responses can be improved by enhanced 911 systems automatically displaying the caller’s address, which can be especially helpful for dysarthric and aphasic patients, and having structured algorithms for caller interaction [14, 15].
Stroke screening instruments can also improve EMS prehospital stroke recognition. The most commonly used scales include the Los Angeles Prehospital Stroke Screen (LAPSS), the Cincinnati Prehospital Stroke Scale (CPSS), the Face Arm Speech Test, the Paramedic Quick Screen (San Diego), the Miami Evaluation of Neurologic Deficit (MEND), the UAB Stroke Observational Scale (SOS), the Maryland Tele-BAT, and the Expanded LAPSS (Melbourne Acute Stroke Screen) [15]. LAPSS and CPSS emphasize motor deficits taking into account that 83–90 % of all strokes have motor symptoms and that hemiparesis is a major determinant of long-term disability [16, 17]. Furthermore, motor testing can be performed reliably and briefly by health personnel not specifically trained in neurology [15].
Concept of Acute Stroke Ready Hospitals
Acute stroke ready hospitals are typically small facilities, located remotely away from a PSC or CSC serving small cities or rural populations. The stroke population evaluated in acute stroke ready hospitals is small (one patient a week on average), and such hospitals have limited staffing and bed availability [15]. EMS should take patients to the nearest acute stroke ready hospital for initial diagnosis, immediate stabilization, and immediate treatments, and then ideally transfer them to the nearest PSC or CSC if their medical needs require a higher level of care (Fig. 1). The key elements of acute stroke ready hospitals include acute stroke teams (at least two members; staffed 24/7; at the bedside within 15 min), EMS and emergency department care protocols (annual training and education), the ability to perform rapid brain imaging and laboratory testing (45-min turnaround time), protocols for intravenous administration of recombinant tissue plasminogen activator (rt-PA) with a goal of 60-min door-to-needle times, written transfer protocols (to a CSC or PSC), and if telestroke support is used, then availability of a telemedicine consult within 20 min [15].
Evaluation of stroke severity, time to first brain imaging, door-to-needle time for intravenous administration of rt-PA, time to initiation of anticoagulation reversal therapy in patients with hemorrhagic stroke and impaired coagulation, time to initiation of telemedicine link, time to transfer of the patient to the PSC or CSC, and protocol violations are all possible performance metrics that would be applicable in acute stroke ready hospitals [15].
Primary Stroke Centers
In 2000, the Brain Attack Coalition (BAC) published the initial recommendations for the establishment of PSCs. According to the BAC, PSCs should have designated acute stroke teams, stroke units, written care protocols, and an integrated emergency response system along with quick access to ancillary investigations including laboratory studies and CT. The BAC supported formal certification programs such as the Joint Commission Disease-Specific Certification process [18, 19]. Since the first publication of BAC recommendations to establish PSCs, approximately 1,000 acute care hospitals in the USA have achieved PSC designation [7].
After the initial publication of the PSC recommendations in 2000, there have been substantive modifications and changes in how patients with stroke are diagnosed and treated. Revised and updated recommendations for the establishment of PSCs now also include the need for on-site early rehabilitation services, institutional commitment and support, the need for a PSC director, reimbursement for stroke call coverage, maintenance of a stroke registry with outcomes and quality improvement components, and provision of public and professional educational programs [7].
In 2011, preferential EMS routing of suspected acute stroke patients to a PSC was present in 20 states (covering 54 % of the US population), but 46 % of the US population still lived in jurisdictions with nonselective routing to the geographically nearest hospital regardless of its stroke capabilities [15, 20]. Measures of the impact of PSC designation have been limited by a lack of precertification baseline hospital data. Several observational studies have demonstrated that PSC certification improves stroke management in different ways. For example, certification is associated with decreasing door to physician evaluation time, door-to-neuroimaging time, and door to intravenous administration of rt-PA time, as well as by increasing rates of intravenous thrombolysis [3, 5, 19, 21]. Hospitals with organized stroke care have sustained improvements in several quality indicators of stroke care, such as increased rates of thrombolysis, increased lipid profile testing, and improved deep vein thrombosis prophylaxis [3, 21]. However, other data suggest that many centers were achieving these milestones before achieving certification, so the effects of certification may be tempered by selection bias of high-performing sites choosing to become certified [22].
Comprehensive Stroke Centers
CSCs provide complete care to patients with the severest and most complex strokes. These include large ischemic strokes that might need intracranial pressure monitoring, intraparenchymal and subarachnoid hemorrhage, and those with cardiorespiratory compromise; in summary, patients with complex medical needs and who might require surgical or endovascular interventions and neurointensive care. This might also include providing expertise to other non-CSC hospitals in the region for managing particular cases, offering guidance for triage of patients, making available laboratory and neuroimaging examinations and specific treatments for patients treated initially at a PSC or acute stroke ready hospital, and being a source of educational programs for health care professionals in a region [23, 24].
The challenges to becoming a CSC range from having dedicated personnel for endovascular procedures available 24/7 to multidisciplinary teams for care and interventions and the need for expertise in neurological critical care. A team with expertise in neurointerventional and vascular neurosurgical procedures is a necessary constituent of a CSC, as are minimum volume requirements for competency in these complex procedures. The variety of procedures that might be performed at a CSC is quite diverse, and having skills in one procedure does not necessarily mean having equivalent skills in others. Therefore, hospitals are moving toward procedure-specific credentialing based on procedural volume to ensure the adequacy of training programs and as a prerequisite for acquiring hospital procedural privileges [23, 24]. In a study evaluating the volumes of neurointerventional procedures performed in various hospitals across the USA with subsequent comparisons with rates of minimum procedural volumes recommended by professional bodies or used in clinical trials to ensure adequate operator experience, very few hospitals met all the neurointerventional procedural volume criteria for all endovascular procedures recommended to ensure adequate operator experience. This suggests that the creation of specialized regional centers for ensuring adequate procedural volume within treating hospitals might be necessary, with directed triage of these patients to advanced centers [25]. Strategies that limit the number of centers in a given geographic region that can perform certain complex procedures based on the expected frequency of demand are infrequently applied in the US health care market.
Cost-Effectiveness of Stroke Centers for Acute Stroke Care
In a cost analysis review of telestroke and rt-PA use for ischemic stroke, the data available for rt-PA use showed higher hospitalization costs but long-term cost savings owing to decreased rehabilitation and nursing home costs. No cost-effectiveness studies for telemedicine programs were identified, although telemedicine programs have demonstrated increased rates of rt-PA administration within 3 h of the onset of stroke symptoms [26, 27].
Although some studies provide critical data on the comparative clinical effectiveness of PSCs, actual cost data from cost-effectiveness analyses of PSCs are scarce. In a decision-analytic model to project the lifetime outcomes, quality of life, and economic outcomes and costs of two hypothetical cohorts of patients with acute ischemic stroke, admission to a PAC resulted in a gain of 0.22 years of life and 0.15 quality-adjusted life years per patient, at a cost of $3600 per patient, compared with admission to a nonprimary stroke center hospital. The incremental cost/quality-adjusted life year gained was $24000 [28].
Accreditation, Recognition, and Certification for Stroke Centers
The quality of care provided to patients with stroke still differs substantially among hospitals in a single country and dramatically across different countries. Broad variations in adherence to guideline-based measures may result from differences in training, guideline awareness, active participation of the hospital administration in quality improvement initiatives, and implementation of methods to confirm that evidence-based care is delivered. The development of strategies to improve the overall quality of stroke care is crucial. Although there has been substantial improvement in care of stroke patients recently, with certain quality indicators achieving high conformity rates, there are still several care processes that need to be improved [29, 30].
Accreditation is the process by which an outside body deems that an institution is capable of providing care by certain criteria. Accreditation programs usually involve evaluation of structural elements for care and the level of performance in relation to established standards and implementation of ways to continuously improve care. Most accreditation programs do not require specific levels of performance in quality-indicators or outcomes for a center to become or remain accredited [29, 31]. Conversely, hospital recognition programs focus on the achievement of specific performance levels on selected quality measures [32, 33]. Finally, hospital certification joins elements that exist in both accreditation and recognition, including evaluation of clinical pathways and structural elements for care and achievement of performance targets for quality indicators [22, 29].
In the USA, there are several accreditation, recognition, and certification programs for hospitals. Examples of accreditation programs include accreditation by the Joint Commission or the Centers for Medicare and Medicaid Services (CMS). Accreditation by the Joint Commission depends on the hospital’s compliance with a set of standards. The Get With The Guidelines (GWTG) programs are examples of performance improvement programs developed by the American Heart Association/American Stroke Association for acute myocardial infarction, heart failure, and stroke that incorporate recognition awards for the achievement of certain benchmarked levels of adherence. Data suggest that achieving these benchmarks may be associated with improvements in short-term and longer-term outcomes [29, 32].
The delivery of evidence-based care for patients with stroke can be improved through participation in recognition programs such as the GWTG. There is good evidence that participation in data registries improves adherence to performance measures. The program aims to address the adherence gap to stroke guidelines by focusing on the redesign of hospital systems of care [32, 34]. Public reporting has, in some reports, been associated with improved health outcomes. For instance, in a large study using propensity score matching, public reporting of hospital outcomes was associated with reductions in mortality for sepsis, acute myocardial infarction, congestive heart failure, and stroke [35, 36]. This is especially true when public reporting relies on source data that is a trusted and reliable measure of hospital performance rather than results calculated from claims data that were not intended for this purpose. Clinical registries hold great promise for improving health outcomes owing to the transparency of data measurement and the participatory nature of the programs in which the data are collected.
In hospitals participating in the GWTG-Stroke program, demographic and clinical data are entered for every patient admitted with acute stroke. Hospitals can track the performance on a variety of indicators, including predetermined stroke performance measures. These measures focus on early identification and treatment with tissue plasminogen activator (t-PA), prevention of in-hospital complications, and secondary stroke prevention. The performance measures evaluated are deep vein thrombosis prophylaxis, discharge while receiving antithrombotics, anticoagulation therapy for atrial fibrillation, consideration for t-PA for eligible patients, antithrombotic medication within 48 h of hospitalization, evaluation of lipid profile, screen for dysphagia, stroke education for the patient and families, smoking cessation counseling, and consideration for rehabilitation [37]. Finally, hospital certification programs evaluate structural elements, standards of care, and achievement of performance for treating specific diseases. The Joint Commission in conjunction with the American Heart Association/American Stroke Association established the Primary Stroke Center Certification program. Certification is based on on-site inspection and is warranted if a hospital is compliant with the published PSC recommendations, clinical practice guidelines, and performance measurement and improvement activities [29]. Because there is no required national standard by which to evaluate hospitals for the quality of their stroke management, there is no homogeneous or recognizable method to determine which health care system provides quality standards for stroke care. Therefore, national hospital certification programs that combine adherence to infrastructure and protocol standards while achieving benchmarked goals of patient-level care delivery could contribute substantially to identifying high-performing hospitals providing high-quality care to patients with stroke [21, 29]. The recent inclusion of stroke measures into the CMS core measure set will provide national US data on hospital performance for the first time across the vast majority of US hospitals.
Participation in Data Registries and Adherence to Performance Measures: Data from the GWTG-Stroke Program
Published data from the GWTG-Stroke program help to continuously understand the gaps in stroke care from the prehospital phase through inpatient care to discharge. On the basis of these data, focused analyses to understand the quality of stroke systems of care have been undertaken, and in some cases, interventions such as the American Heart Association’s Target: Stroke campaign have been implemented [38].
One of the earliest reports of improvement in the GWTG-Stroke program was published in 2008. Improvements in adherence to 11 of 13 quality indicators in stroke treatment were present after 1 year in hospitals participating in the national implementation of the GWTG-Stroke program [34]. Sustained changes were also observed in the care of stroke patients after a 5-year comparison in 790 US hospitals participating in the GWTG-Stroke program [37]. These early reports laid the groundwork for a robust set of investigations over the next decade, which are summarized in a recent publication on the impact and evolution of the GWTG–Stroke program [39].
Several reports using contemporary nationwide GWTG-Stroke data on EMS use by stroke patients have been published [40, 41]. Although EMS hospital prenotification is recommended by the guideline, in one third of patients transported to GWTG-Stroke hospitals, prenotification was not performed [41]. The activation of EMS has the potential to improve acute stroke care by reducing the times for evaluation and treatment. Therefore, these GWTG-Stroke data suggest that campaigns should be implemented focusing on eradicating barriers to increasing EMS use, targeting populations at high risk, those with economic disincentives to use EMS, and those with inadequate access to information.
A recent GWTG-Stroke report showed that prenotification by EMS was associated with more timely evaluation and treatment of acute ischemic stroke. From 2003 to 2011, there were 1,585 participating GWTG-Stroke hospitals at which 372,000 EMS-transported confirmed ischemic stroke patients were evaluated. Hospital prenotification was performed in 67 % of the cases. Door-to-imaging times, door-to-needle times and onset-to-needle times were significantly shorter when prenotification was performed. The practice of prenotification varied considerably according to hospital type, state, and geographic region. These results suggest the need to improve prenotification systems [40].
A review of more than 400,000 patients admitted with stroke between 2003 and 2009 to more than 1,200 GWTG-Stroke participating hospitals showed that more than one quarter of the patients were admitted within the therapeutic window for treatment with intravenously administered rt-PA; however, this percentage remained stable over the years [42]. It is somewhat discouraging that after all the efforts made to educate the public in the USA, these percentages have remained unchanged. These results reinforce the need to develop newer and more effective methods to promote public awareness campaigns educating the population about the signs and symptoms of stroke, as well as on the importance of activating EMS when acute stroke symptoms are suspected. Data from GWTG-Stroke clearly show an association between shorter door-to-needle times and reduced in-hospital mortality. A study including 25,504 acute ischemic stroke patients treated with rt-PA within 3 h of symptom onset at 1,082 hospital sites using GWTG-Stroke data revealed that after adjustment, every 15-min reduction in door-to-needle time was associated with 5 % lower odds of in-hospital mortality [43]. This effect was corroborated in a recent GWTG-Stroke publication which confirmed that this effect was driven by shorter onset-to-needle times, and that improvements in onset-to-needle times were associated with lower mortality, lower rates of symptomatic hemorrhage, improved ambulation, and improved likelihood of returning to home on hospital discharge [44].
The patterns of stroke treatment during the emergency and inpatient phases of hospital admission can be continuously monitored using GWTG-Stroke data. Delays in brain imaging are still a problem even in the self-selected hospitals participating in GWTG-Stroke. In a study of more than 600,000 patients, less than 50 % of the patients had brain imaging within the first 25 min, as recommended by professional society guidelines [45]. Female patients, the elderly, nonwhites, and diabetics had higher risk of delays in brain imaging. This study pointed out the need for improvement in the structure of stroke services so that patients can undergo more rapid diagnosis and neuroimaging [45]. A shorter door-to-imaging time has the potential to increase the accurate diagnosis of stroke, and translate into higher rates of treatment with reperfusion therapies with improvement in patient outcomes. Another report from GWTG-Stroke showed that less than one third of patients treated with intravenously administered rt-PA had door-to-needle times of 60 min or less, with only modest improvement from 2003 to 2009 [43]. These findings supported the creation of a targeted initiative to improve the timeliness of reperfusion in acute ischemic stroke called Target: Stroke. The aim of Target: Stroke was to increase the proportion of patients receiving intravenously administration of t-PA within 60 min of arrival in the emergency department from 29 % to 50 % [38]. Given the findings from prior GWTG-Stroke reports, this shift in times could be expected to produce a substantial improvement in mortality, hemorrhage rates. and patient outcomes.
The analysis of practices such as dysphagia screening and stroke education, as well as the use of secondary prophylaxis measures, can be monitored through the quality indicators collected by GWTG-Stroke. For example, although national guidelines recommend dysphagia screening before oral intake in stroke patients to reduce hospital-acquired pneumonia, GWTG-Stroke data showed that dysphagia screening did not occur in one third of eligible patients [46]. An important measure of secondary prophylaxis in patients with ischemic stroke is the use of oral anticoagulation for patients with atrial fibrillation. Data from more than 1.000 hospitals participating in the GWTG-Stroke program showed that the practice of oral anticoagulation for eligible patients rose from 88.4 % to 95.2 % from 2003 to 2010 [47]. The duration of participation in GWTG-Stroke was associated with better initiation of anticoagulation of eligible patients, with the greatest impact in patients whose atrial fibrillation was observed and confirmed by ECG or telemetry during the admission, as compared with those with a history of paroxysmal fibrillation which was not captured during the admission [48].
The degree to which guideline-recommended stroke treatments differ by region for patients treated at hospitals participating in GWTG-Stroke has also been evaluated. In general, the compliance with guideline-recommended therapies was high; however, significant regional differences were observed in the adherence to specific measures. Treatments with substantial variation included the use in eligible patients of intravenously administered rt-PA and lipid-lowering and antihypertensive medications, as well as the provision of “defect free care,” a measure which evaluates the proportion of subjects who receive all seven evidence-based interventions for which they were eligible [49]. These regional differences were noted despite participation in a program that aims to standardize care on the basis of published guidelines, and points to the need to better understand the local factors which influence the translation of evidence into practice.
In response to increasing interest in hospital ranking based on stroke mortality, and concerns about inadequate risk adjustment by systems using only administrative data that lack stroke severity indices, investigators developed a stroke mortality risk tool to predict in-hospital mortality in GWTG-Stroke [50, 51]. Predicting the risk of death during admission for stroke can be useful to help determine prognosis, counsel patients and families, apply increased resources to those patients at highest risk, and help clinicians and hospitals understand whether stroke case fatality rates are similar. Two risk tools have been developed and reported: one for ischemic stroke alone and one that can be used across all stroke types [50, 51]. The single prediction tool for all stroke types was developed to predict the risk of in-hospital death following admission for stroke of all subtypes based on GWTG-Stroke data variables of the patient’s age, National Institutes of Health Stroke Scale score at admission, mode of arrival, stroke subtype and the presence of stroke risk factors and comorbidities (male gender, atrial fibrillation, dyslipidemia, coronary heart disease, peripheral artery disease), and time of hospital arrival. This was the first validated clinical risk score for discrimination of death in all three major stroke types and had good calibration and discrimination [50]. It has also been shown that when the National Institutes of Health Stroke Scale score from GWTG-Stroke was added to a model of risk-standardized mortality developed by CMS, there was substantial improvement in classification of performance and dramatic shifts in the model output related to hospitals being above average, average, or below average in their mortality rates compared with what was expected [51].
Stroke Units in Low-Income and Middle-Income Countries
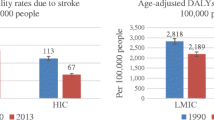
In high-income countries, results from randomized trials and systematic reviews have shown that care in a stroke unit can improve the outcome of patients with stroke [52, 53]. The question of whether stroke unit care is important and feasible in low-income and middle-income countries is an important one. Studies using different methodological approaches comparing care in a dedicated stroke unit with care in a general ward in countries classified as low-income or middle-income countries according to the World Bank definitions showed lower death rates in the stroke unit group than in the control group [54].
Applying the experience of stroke unit trials from high-income countries to low- or middle-resourced settings can be challenging. Although most patients with stroke do not need expensive, highly resourced facilities, a hospital area with dedicated resources for stroke care and trained professionals (physicians, nurses, allied health professionals) is a minimum requirement for stroke unit care [54]. In general wards, simple measures of care to prevent complications of stroke (e.g., deep vein thrombosis, aspiration pneumonia, urinary tract infection) and increase the odds of good functional outcomes (e.g., early mobilization, rehabilitation therapies) after a stroke are not routinely provided, especially when resources are scarce. Additionally, a physical stroke unit can support ongoing stroke education for hospital staff [52, 54].
Conclusions
In conclusion, although CSCs will likely benefit the most severely affected patients, not all patients will need care at a CSC. PSCs have been shown to improve a variety of outcomes, so they must remain the major facility component of stroke systems of care. Future challenges of stroke systems of care include improving EMS triage and increasing rural access to quick diagnosis, treatment, and stabilization pending transfer to a PSC or CSC. Fragmentation of health care delivery produces suboptimal treatment, safety concerns, and inefficient use of resources and therefore should be avoided. The final aim of stroke systems should be to integrate prevention and treatment and promote patient access to the best evidence-based care.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44. This article provides evidence of the substantial increase in the prevalence and costs of cerebrovascular diseases and suggests that effective prevention strategies are needed in order to limit the growing burden of cerebrovascular diseases.
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–245.
Douglas VC, Tong DC, Gillum LA, et al. Do the brain attack coalition’s criteria for stroke centers improve care for ischemic stroke? Neurology. 2005;64:422–7.
• Meretoja A, Roine RO, Kaste M, et al. Effectiveness of primary and comprehensive stroke centers: perfect stroke: a nationwide observational study from Finland. Stroke. 2010;41:1102–7. In this observational register–linkage study of all patients with ischemic stroke treated in Finland between 1999 and 2006, a clear association between the level of acute stroke care and patient outcome was demonstrated, supporting the use of published criteria for PSCs and CSCs.
Xian Y, Holloway RG, Chan PS, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305:373–80.
Schwamm LH, Pancioli A, Acker 3rd JE, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association’s task force on the development of stroke systems. Circulation. 2005;111:1078–91.
Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42:2651–65.
Wein TH, Staub L, Felberg R, et al. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke. 2000;31:1925–8.
Potvin JH. Emergency medical services in stroke care: a Rhode Island perspective. Med Health R I. 2011;94:353–6.
• McKinney JS, Mylavarapu K, Lane J, et al. Hospital prenotification of stroke patients by emergency medical services improves stroke time targets. J Stroke Cerebrovasc Dis. 2013;22:113–8. This article demonstrates that prehospital notification of suspected stroke patients reduced the time to stroke team arrival, neuroimaging completion, and neuroimaging interpretation. Furthermore, intravenous thrombolysis occurred twice as often in the prenotification group.
Kuster GW, Bueno Alves M, Cendoroglo Neto M, et al. Determinants of emergency medical services use in a Brazilian population with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2013;22:244–9.
Abdullah AR, Smith EE, Biddinger PD, et al. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehosp Emerg Care. 2008;12:426–31.
Weber JE, Ebinger M, Rozanski M, et al. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology. 2013;80:163–8.
Patel MD, Rose KM, O’Brien EC, et al. Prehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina Stroke Care Collaborative. Stroke. 2011;42:2263–8.
Jauch EC, Saver JL, Adams Jr HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947.
Kidwell CS, Starkman S, Eckstein M, et al. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000;31:71–6.
Kothari RU, Pancioli A, Liu T, et al. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med. 1999;33:373–8.
Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;283:3102–9.
Chaudhry FS, Schneck MJ, Warady J, et al. Primary stroke center concept: strengths and limitations. Front Neurol. 2012;3:108.
Pedigo AS, Odoi A. Investigation of disparities in geographic accessibility to emergency stroke and myocardial infarction care in east Tennessee using geographic information systems and network analysis. Ann Epidemiol. 2010;20:924–30.
Stradling D, Yu W, Langdorf ML, et al. Stroke care delivery before vs after JCAHO stroke center certification. Neurology. 2007;68:469–70.
Lichtman JH, Allen NB, Wang Y, et al. Stroke patient outcomes in US hospitals before the start of the Joint Commission Primary Stroke Center certification program. Stroke. 2009;40:3574–9.
Alberts MJ, Latchaw RE, Selman WR, et al. Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke. 2005;36:1597–616.
Leifer D, Bravata DM, Connors 3rd JJ, et al. Metrics for measuring quality of care in comprehensive stroke centers: detailed follow-up to Brain Attack Coalition comprehensive stroke center recommendations: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:849–77.
Grigoryan M, Chaudhry SA, Hassan AE, et al. Neurointerventional procedural volume per hospital in United States: implications for comprehensive stroke center designation. Stroke. 2012;43:1309–14.
Demaerschalk BM, Hwang HM, Leung G. Cost analysis review of stroke centers, telestroke, and rt-PA. Am J Manag Care. 2010;16:537–44.
Silva GS, Schwamm LH. Use of telemedicine and other strategies to increase the number of patients that may be treated with intravenous thrombolysis. Curr Neurol Neurosci Rep. 2012;12:10–6.
Guzauskas GF, Boudreau DM, Villa KF, et al. The cost-effectiveness of primary stroke centers for acute stroke care. Stroke. 2012;43:1617–23.
Fonarow GC, Gregory T, Driskill M, et al. Hospital certification for optimizing cardiovascular disease and stroke quality of care and outcomes. Circulation. 2010;122:2459–69.
Jones DW, Peterson ED, Bonow RO, et al. Translating research into practice for healthcare providers: the American Heart Association’s strategy for building healthier lives, free of cardiovascular diseases and stroke. Circulation. 2008;118:687–96.
Roberts JS, Coale JG, Redman RR. A history of the Joint Commission on Accreditation of Hospitals. JAMA. 1987;258:936–40.
Heidenreich PA, Lewis WR, LaBresh KA, et al. Hospital performance recognition with the Get With The Guidelines program and mortality for acute myocardial infarction and heart failure. Am Heart J. 2009;158:546–53.
Smith EE, Liang L, Hernandez A, et al. Influence of stroke subtype on quality of care in the Get With The Guidelines-Stroke program. Neurology. 2009;73:709–16.
LaBresh KA, Reeves MJ, Frankel MR, et al. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med. 2008;168:411–7.
Hollenbeak CS, Gorton CP, Tabak YP, et al. Reductions in mortality associated with intensive public reporting of hospital outcomes. Am J Med Qual. 2008;23:279–86.
Saposnik G, Estol CJ. Translational research: from observational studies to health policy: how a cohort study can help improve outcomes after stroke. Stroke. 2011;42:3336–7.
Schwamm LH, Fonarow GC, Reeves MJ, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–15.
Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association’s Target: stroke initiative. Stroke. 2011;42:2983–9.
Schwamm L, Fayad P, Acker 3rd JE, et al. Translating evidence into practice: a decade of efforts by the American Heart Association/American Stroke Association to reduce death and disability due to stroke: a presidential advisory from the American Heart Association/American Stroke Association. Stroke. 2010;41:1051–65.
Lin CB, Peterson ED, Smith EE, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. J Am Heart Assoc. 2012;1:e002345.
Ekundayo OJ, Saver JL, Fonarow GC, et al. Patterns of emergency medical services use and its association with timely stroke treatment. Circ Cardiovasc Qual Outcomes. 2013;6:212–69.
Tong D, Reeves MJ, Hernandez AF, et al. Times from symptom onset to hospital arrival in the Get With The Guidelines–Stroke program 2002 to 2009: temporal trends and implications. Stroke. 2012;43:1912–7.
Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–8.
Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309:2480–8.
Kelly AG, Hellkamp AS, Olson D, et al. Analysis of the Get With The Guidelines-Stroke program. Stroke. 2012;43:1279–84.
Masrur S, Smith EE, Saver JL, et al. Dysphagia screening and hospital-acquired pneumonia in patients with acute ischemic stroke: findings from Get with the Guidelines-Stroke. J Stroke Cerebrovasc Dis. 2013. doi:10.1016/j.jstrokecerebrovasdis.2012.11.013.
Lewis WR, Fonarow GC, Grau-Sepulveda MV, et al. Improvement in use of anticoagulation therapy in patients with ischemic stroke: results from Get With The Guidelines-Stroke. Am Heart J. 2011;162:692–9e.2.
Lewis WR, Fonarow GC, LaBresh KA, et al. Differential use of warfarin for secondary stroke prevention in patients with various types of atrial fibrillation. Am J Cardiol. 2009;103:227–31.
Allen NB, Kaltenbach L, Goldstein LB, et al. Regional variation in recommended treatments for ischemic stroke and TIA: Get With The Guidelines–Stroke 2003–2010. Stroke. 2012;43:1858–64.
Smith EE, Shobha N, Dai D, et al. A risk score for in-hospital death in patients admitted with ischemic or hemorrhagic stroke. J Am Heart Assoc. 2013;2:e005207.
Fonarow GC, Pan W, Saver JL, et al. Comparison of 30-day mortality models for profiling hospital performance in acute ischemic stroke with vs without adjustment for stroke severity. JAMA. 2012;308:257–64.
Langhorne P, Dennis MS. Stroke units: the next 10 years. Lancet. 2004;363:834–5.
53 Organised inpatient (stroke unit) care for stroke. Stroke Unit Trialists’ Collaboration. Cochrane Database Syst Rev 2000:CD000197.
Langhorne P, de Villiers L, Pandian JD. Applicability of stroke-unit care to low-income and middle-income countries. Lancet Neurol. 2012;11:341–8.
Conflict of Interest
Gisele Sampaio Silva declares no conflict of interest.
Lee H. Schwamm declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiovascular Disease and Stroke
Rights and permissions
About this article
Cite this article
Silva, G.S., Schwamm, L.H. Review of Stroke Center Effectiveness and Other Get with the Guidelines Data. Curr Atheroscler Rep 15, 350 (2013). https://doi.org/10.1007/s11883-013-0350-8
Published:
DOI: https://doi.org/10.1007/s11883-013-0350-8