Opinion statement
Chronic myelomonocytic leukemia (CMML) is an aggressive myeloid neoplasm in which treatment strategies with the capacity to improve survival are currently lacking. Clinical features are heterogeneous and although the overall prognosis is poor, survival can vary significantly between individuals. This reflects the need for an individualized treatment approach which incorporates accurate risk stratification. Though numerous prognostic scores exist, newer CMML-specific models incorporating molecular data should be favored. While asymptomatic, low-risk patients should be observed until their disease progresses, the majority of patients will require treatment. Due to a deficiency in treatments with disease-modifying capacity, any patient who requires treatment should be considered for enrollment in clinical trials evaluating novel therapeutic approaches. Allogeneic stem cell transplant (allo-SCT) remains the only current therapy with the potential to cure the disease and should be considered in most patients with intermediate- to high-risk disease. However, substantial risks are involved and, in part, because of advanced age at diagnosis, a minority of patients are candidates. Hypomethylating agents (HMAs) have become a preferred treatment approach, and should be used in those with cytopenias. Patients presenting with proliferative features can be treated with hydroxyurea to manage their symptoms and control leukocytosis, though HMAs can be incorporated as well, particularly in patients with higher risk disease. HMAs should also be considered in patients with a high burden of disease prior to proceeding with allo-SCT. Induction chemotherapy should be reserved for younger, healthy patients who have transformed to acute myeloid leukemia to induce remission prior to transplant. Supportive care utilizing transfusion support, erythropoiesis-stimulating agents, and infection prevention measures should be incorporated into the care of all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic myelomonocytic leukemia (CMML) is a clonal myeloid neoplasm that is defined by the World Health Organization (WHO) by a persistent peripheral monocytosis (> 1 × 109 cells/L and > 10% of the total WBC count) and dysplastic changes in one or more lineages without defining features of a separate myeloproliferative neoplasm (MPN) [1•] (Fig. 1). It shares features of myelodysplastic syndromes (MDS) and MPNs which has led to an evolving classification since its initial description in 1937, but is currently classified as a distinct entity within the category of MDS/MPN syndromes by WHO [1•, 2]. It is further subclassified by WHO into three groups (CMML-0, CMML-1, and CMML-2) based on peripheral blood and bone marrow blast count and by the FAB system into myelodysplastic (MDS-CMML) and myeloproliferative (MPN-CMML) subtypes based on a white blood cell count of < 13 × 109/L or > 13 × 109/L, respectively [1•, 3].
Although the exact incidence is unknown, epidemiologic data suggests that the annual incidence rate in the USA is approximately 0.3 new cases per 100,000 patients, though this is likely underrepresentative of the true rate [4]. It is a disease of older adults with a median age at diagnosis of approximately 70 years old and a modest male predominance. The clinical features are heterogeneous, with MDS-CMML typically manifesting with cytopenias and MPN-CMML presenting with leukocytosis, splenomegaly, and constitutional symptoms. Cytogenetic changes can be identified in ~ 30% of patients while somatic mutations can be identified in > 90% of patients, with TET2 (~ 60%), SRSF2 (~ 50%), ASXL1 (~ 40%), and RAS (~ 30%) the most frequently mutated genes [5,6,7,8].
The overall prognosis is poor with an estimated median survival of 34 months and a risk of transformation to acute myeloid leukemia (AML) of approximately 20% [9•]. There have been at least 10 risk stratification systems used to prognosticate in CMML, some of which were developed in populations of predominantly MDS patients, while others are specific to CMML [7, 8, 10,11,12,13,14,15,16, 17•]. Each incorporates a unique set of overlapping clinical and, in some cases, genetic features. As the understanding of genetic changes in CMML has progressed, newer models have incorporated cytogenetic and molecular data with nonsense and frameshift mutations in the ASXL1 gene most consistently demonstrating a negative impact on overall survival [7, 8, 17•].
Historically, treatment has been extrapolated from studies of MDS, largely due to a lack of CMML-specific clinical trials. Allogeneic stem cell transplant (allo-SCT) remains the only potentially curative therapy; however, many patients are not candidates. While other treatments can be offered, none have clearly demonstrated true disease-modifying activity and thus clinical trials utilizing novel agents should be favored. Choice of therapy is otherwise based on patient-specific factors, risk stratification, and symptoms. Observation is a viable option in a subset of patients, while supportive care with transfusion support and erythropoiesis-stimulating agents (ESAs), cytoreductive therapies, and hypomethylating agents (HMAs) can be considered in others (Table 1). This review will further examine currently available treatment options as well as highlight recent and ongoing advances in the therapy of CMML.
Current pharmacologic treatment
Risk-adapted therapy
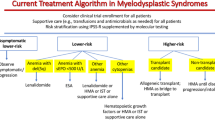
Accurate risk stratification can be challenging in CMML, but is an important aspect in appropriate treatment selection (Fig. 2). A number of models have been used over the past several decades to risk stratify CMML, with early models developed in populations of predominantly MDS patients, some of which excluded patients with proliferative CMML [10]. However, CMML-specific models have since been developed which incorporate a number of clinical variables such as age, WHO classification, FAB classification, bone marrow blast percent, laboratory data, and transfusion dependence [7, 8, 14,15,16, 17•]. Seven prognostic models were compared in a study that included over 1800 patients from 8 institutions [9•]. While each model evaluated was found to be valid, all were susceptible to upstaging and none of the models in this study incorporated molecular abnormalities. As our understanding of the molecular basis of CMML has progressed, newer models have begun to include somatic mutation data. Mutation of the ASXL1 gene has been shown in several studies to have a negative impact on overall survival and is included in the GFM and Molecular Mayo models while the CPPS-Mol model uses a genetic score that includes ASXL1 as well as NRAS, RUNX1, and SETBP1 and cytogenetic risk [7, 8, 17•]. The previously mentioned study of 1800 patients validated the adverse prognostic impact of ASXL1 and also identified CBL mutation as an independent negative predictor of survival. While no model has been shown to be superior, CMML-specific models should be favored and the evaluation and incorporation of molecular abnormalities should be considered in all patients as this data has been shown to independently impact survival.
Algorithm for initial treatment of chronic myelomonocytic leukemia. CMML, chronic myelomonocytic leukemia; ESA, erythropoiesis-stimulating agent; HMA, hypomethylating agent; HLA, human leukocyte antigen; Allo-SCT, allogeneic stem cell transplant. The asterisk indicates that supportive care should be incorporated into the treatment of all patients. The plus sign indicates all patients who require treatment should be considered for enrollment in a clinical trial.
While the overall prognosis is poor, significant heterogeneity is observed between individual patients and reflects the need for accurate risk stratification. All prognostic models have been shown to effectively stratify patients into separate risk groups, with high-risk patients typically having a median OS in the range of less than 1 year and an increased rate of leukemic transformation. There is greater variability between studies in the predicted median OS among low-risk patients, ranging from as short as 2 years to as long as > 144 months, though models incorporating molecular data seem to identify patients at the high end of this range [17•].
The identification of truly low-risk patients is vital given the lack of disease-modifying therapies and potential risks associated with treatment in comparison to the potentially indolent course a subset of CMML patients may experience. In low-risk patients who are not proliferative or symptomatic from their disease, observation is preferred until symptoms arise or evidence of clinical disease progression emerges. This strategy may help prevent unnecessary treatment-related morbidity and mortality and can allow for treatment-free intervals of several years in some patients. On the contrary, the benefits of treatment are more likely to outweigh associated risks in higher risk patients, and those that are candidates should be considered for allo-SCT. Pharmacologic treatment in such patients should be directed at symptoms, with cytoreductive therapies preferred for those with proliferative features and HMAs appropriate for those with significant cytopenias.
Allogeneic stem cell transplant
At this time, allo-SCT remains the only therapy in CMML with the potential to cure the disease and should be a consideration in nearly all patients. However, with a median age at diagnosis of approximately 70 years and frequent comorbid conditions, many patients are not candidates. The decision to proceed must factor in donor availability, patient’s preferences, and a detailed risk-benefit assessment which can be aided by risk assessment tools such as the HCT-CI score and is best performed by an experienced transplant physician [18].
While a number of studies have retrospectively evaluated allo-SCT in CMML, no prospective studies have been performed. The largest study to date was done by the European Group for Blood and Marrow Transplantation and included 513 CMML patients [19••]. They reported a 4-year OS and relapse-free survival of 33% and 27%, respectively, and found that complete response (CR) at time of transplant was the only predictor of survival. In a long-term follow-up study of 85 patients treated at a single institution, the 10-year OS was 40% with a 10-year non-relapse mortality (NRM) of 34% [20]. At 10 years, 27% of patients had relapsed (24% in the first 2 years) which was predicted by increased MDAPS score, while increasing age, higher HCT-CI score, and high-risk cytogenetics were predictors of inferior survival. Although these studies demonstrate long-term survival in a subset of patients, the median ages at transplant were 53 years and 51 years, respectively, significantly younger than most patients with the disease. Reduced intensity conditioning regimens can increase access to allo-SCT in older patients, and, while studied largely in populations of MDS, decrease NRM without compromising OS [21,22,23,24].
There are substantial risks involved and, for this reason, low-risk patients who are asymptomatic may elect to delay transplant until their disease progresses. However, higher risk patients with CMML have a poor prognosis and allo-SCT should be the treatment of choice, particularly in younger patients without significant comorbidities. Bridging therapy prior to transplant should be considered given the potential for improved outcomes in patients in CR at time of transplant [19••]. Studies in MDS have also suggested that increased disease burden at time of transplant has a negative impact on outcomes, with some suggesting therapy prior to transplant in patients with > 10% bone marrow blasts, particularly when receiving non-myeloablative regimens [25]. Safety and efficacy of HMA use prior to transplant have been established in several trials in MDS [26,27,28]. Kongtim et al. evaluated outcomes in 83 patients with CMML (36 of whom had progressed to AML) treated with HMAs or induction chemotherapy and found that treatment with a HMA and achievement of < 5% blasts prior to transplant were associated with a lower rate of relapse and improved PFS, without an increased NRM [29•].
Hypomethylating agents
The hypomethylating agents azacitidine and decitabine have become widely used therapies in the treatment of CMML. Both are cytidine nucleoside analogues that have been shown to incorporate into DNA causing irreversible binding to DNA methyltransferases, global hypomethylation of DNA and induction of DNA damage, though with drug-specific effects on gene expression, protein expression, and cell cycle [30, 31]. Both were approved based on randomized controlled trials (RCTs) demonstrating their safety and efficacy in MDS patients, including the pivotal AZA-001 study which demonstrated an improved overall survival in patients treated with azacitidine [32,33,34]. However, a total of just 44 out of the 719 patients that were collectively enrolled in these studies had CMML.
Since their initial approval, the use of these agents in CMML-specific populations has been explored, though no large RCT has been completed. A number of phase 2 studies have validated their use in CMML, demonstrating a median OS of 12 to 37 months and overall response rates ranging from 26 to 69%, comparable to those observed in larger RCTs performed in MDS [35,36,37,38,39,40,41,42, 43••]. Cytogenetic responses were seen and although several studies demonstrated an improved OS in responders, randomized prospective studies are needed to confirm true disease-modifying activity of these agents [37, 38, 40, 41, 43••]. In multivariate analyses, Ades et al. demonstrated inferior survival in azacitidine-treated patients who had bone marrow blasts > 10% or palpable splenomegaly [41]. In a separate study, no genetic predictor of response could be identified when mutation status of ASXL1, RUNX1, JAK2, NRAS, KRAS, TET2, CBL, and FLT3 was evaluated [37]. However, a non-statistically significant trend toward improved response rate was seen in patients with mutations in TET2 (54% vs. 28%, p = 0.17), a predictor of response that has been demonstrated in patients with MDS and AML treated with HMAs [44,45,46]. Improved response rates have also been suggested in patients with MDS-CMML vs. MPN-CMML, though responses were seen in both groups [43••]. A single-center, retrospective study of 151 patients identified age < 70 years, lower CPSS cytogenetic risk, absence of peripheral blasts, and higher hemoglobin levels as predictors of improved OS with HMA therapy and also demonstrated a higher rate of CR in those treated with decitabine compared to azacitidine (58.3% vs. 20.6%, p < 0.001) [47•]. The same study demonstrated that similar to patients with MDS, prognosis after failure of HMA therapy in patients with CMML is dismal, with a median OS of 7 months from time of relapse.
Though they have not been definitively shown to alter the natural history of disease, activity of these agents in CMML has clearly been demonstrated and these agents should be considered a standard treatment option. Their use is preferred in intermediate- to high-risk patients with MDS-CMML and in those manifesting with significant cytopenias. However, they can also be used in patients with proliferative features, particularly high-risk patients and those who fail to respond to cytoreductive therapy alone. They are well tolerated by most patients, with myelosuppression the most frequently observed adverse effect, though constipation is also frequently reported. Though improved CR rates with decitabine were observed in a single study, these agents have not been compared head to head in prospective studies and neither is clearly superior, though the authors favor decitabine in patients with proliferative features [47•]. Patient comorbidities as well as preferences in the dosing schedule (7 day vs. 5 day) and route of administration (intravenous vs. subcutaneous) may be used in agent selection. Oral forms of decitabine (ASTX727) and azacitidine (CC-486) are currently under development for use in hematologic malignancies and may provide a more convenient option in the future [48, 49].
Cytoreductive therapy
Prior to the approval of azacitidine and decitabine, cytoreductive therapies were the cornerstone of treatment in CMML. Historically, a number of agents including topotecan, low-dose cytarabine, and etoposide have been used, with only modest activity [50]. However, a randomized trial comparing hydroxyurea (starting dose of 1 g/day) to etoposide in 105 CMML patients with proliferative features demonstrated increased response rates (60% vs. 36%) and improved survival (median OS of 20 vs. 9 months) with hydroxyurea treatment [51]. Along with its ease of use and tolerance, hydroxyurea is now considered standard therapy for those requiring cytoreduction.
MPN-CMML classification and a number of associated laboratory findings including WBC and absolute monocyte count have been predictive of inferior OS in most prognostic scores [7, 8, 13, 15, 16, 17•]. Additionally, clinical features such as constitutional symptoms (fever, weight loss, fatigue, night sweats) and splenomegaly are commonly observed and can have a profound impact on a patient’s quality of life. While cytoreductive therapies have not been clearly shown to impact the negative effect this phenotype has on prognosis, they can dramatically improve symptoms and normalize the WBC in those with significant leukocytosis. Hydroxyurea can be considered in patients in any risk group presenting with proliferative symptoms. However, in asymptomatic patients with leukocytosis, there is no consensus value at which to initiate therapy or target WBC value that should be achieved. Given the time to response seen with HMA therapy, hydroxyurea can also be considered in patients with proliferative features initiating such therapy until response is attained, as has been done in clinical trials of HMA therapy [37]. Intensive induction-type chemotherapy regimens have not been well studied in CMML and have shown only modest efficacy with the potential for treatment-related mortality in studies of MDS [52, 53]. Their use should generally be limited to patients with high blast counts or evolution to AML prior to proceeding with allo-SCT [54].
Supportive care
Expectant management is preferred in low-risk, asymptomatic patients, but may also be considered in elderly or frail patients in whom the potential for therapy-related complications is greatest. Regardless of age, performance status or additional therapies pursued, supportive measures are a vital component of treatment in all patients with CMML. There is minimal data to guide practice in CMML patients, and thus recommendations parallel guidelines developed in MDS. All patients should have blood counts monitored routinely to evaluate for complications or progression of disease. The risk of infection is increased, a feature that all patients should be counseled on and monitored closely for as this is a leading cause of death. Preventive measures including influenza and pneumococcal vaccination should be provided, while the use of myeloid growth factors and prophylactic antibiotics is generally not recommended.
In patients with anemia, erythropoiesis-stimulating agents (ESAs) should be considered. ESAs are capable of increasing hemoglobin levels and decreasing transfusion requirements, with response predicted by lower baseline erythropoietin (EPO) levels [55]. Transfusion support should be provided based on standard indications with treatment thresholds developed on an individualized basis. Patients with chronic transfusion dependence should be monitored for iron overload. Chelation therapy can be considered with a history > 20 transfusions and/or ferritin > 1000 mcg/L, though the benefit remains unclear and chelators are often poorly tolerated [56,57,58].
Emerging therapies under development
Despite responses seen to current therapies with potential improvements in symptoms and hematologic parameters, there is currently a lack of therapies with proven disease-modifying capacity in CMML. All patients should be considered for therapeutic clinical trials both to allow patients access to novel therapies and to further our understanding of the disease. Multiple strategies are currently being explored in the treatment of CMML, from unique combinations or modifications of existing therapies to novel therapies targeting the unique pathophysiology of CMML.
Already a standard treatment option in CMML, hypomethylating agents continue to be explored. There is currently a phase 3 randomized trial comparing decitabine ± hydroxyurea in proliferative CMML underway in France, where decitabine is only approved in MDS-CMML (NCT02214407). ASTX727, oral decitabine combined with the cytidine deaminase inhibitor cedazuridine, showed equivalent pharmacokinetics, safety, and efficacy to that of IV decitabine in a phase 2 study, with a randomized phase 3 study comparing it directly to IV decitabine currently underway [48]. An oral form of azacitidine (CC-486) is also being developed in myeloid malignancies with promising activity in early trials including responses seen in patients with prior HMA failure, with phase 3 studies ongoing [49, 59, 60]. Guadecitabine (SG-110) is a novel dinucleotide of decitabine rendering it resistant to degradation by cytidine deaminase that is under development with promising phase 2 data in MDS and CMML [61, 62].
Our group has demonstrated that CMML is characterized by hematopoietic stem and progenitor cell hypersensitivity to GM-CSF, a pathway that was targetable with anti-GM-CSF antibodies and JAK2 inhibitors in preclinical study [63]. This has led to clinical study of the JAK2 inhibitor ruxolitinib, which is already approved in other MPNs including primary myelofibrosis. Safety and efficacy were demonstrated in phase 1 and preliminary phase 1/2 data, particularly in patients with proliferative symptoms and splenomegaly, with final data from the combined phase 1/2 study to be reported in the near future [64•, 65]. Pacritinib, a JAK2 inhibitor with a unique spectrum of anti-tyrosine kinase activity, including FLT3, has shown preclinical promise when combined with HMAs with initial clinical study underway [66]. Lenzilumab (KB003) is an anti-GM-CSF monoclonal antibody that has been studied in asthma and rheumatoid arthritis, which has demonstrated preclinical activity in CMML and recently completed enrollment in a phase 1 trial with results not yet reported [63].
Therapies targeting the unique molecular abnormalities in CMML also present a promising therapeutic strategy. Mutations in spliceosome encoding genes such as SRSF2, SF3B1, and U2AF1 are seen in over half of patients with CMML. The oral spliceosome modulator H3B-8800 has shown preclinical activity in cell and xenograft models of spliceosome-mutant malignancies with a phase 1 study in AML, MDS, and CMML patients currently open [67, 68]. RAS mutations are seen in 30% of CMML patients with additional activation of the MAPK pathway seen via separate mechanisms, making inhibition of this pathway a potential therapeutic target. Trametinib, an inhibitor of the downstream signaling mediator MEK, has shown single-agent efficacy in a phase 2 study of RAS mutant myeloid malignancies, including CMML, and likely holds potential in combination regimens [69]. Tipifarnib, a farnesyltransferase inhibitor that blocks an important post-translational modification of RAS, has shown promise in preliminary data from a phase 2 study in CMML as well as prior phase 2 data in MDS [70, 71]. Additionally, there have been recent approvals of drugs targeting both mutant IDH1 and IDH2 and, while IDH1/2 mutations are found in only ~ 5% of patients with CMML, this may represent a therapeutic strategy in this subset of patients.
SL-401 is a recombinant IL-3-diphteria toxin fusion protein selectively targeting the IL-3 receptor, CD123, which is expressed in both neoplastic myeloid cells as well as cells in the microenvironment. It is currently being studied in hematologic malignancies including CMML and blastic plasmacytoid dendritic cell neoplasm (BPDCN), with phase 2 studies ongoing and promising interim data presented at the European Hematology Association meeting in June, 2018 [72, 73]. Though the use of immunotherapy in myeloid neoplasms has not kept pace with advances in other malignancies, it continues to be investigated. The immune checkpoint proteins PD-1, CTLA4, PD-L1, and PD-L2 are expressed in malignant myeloid cells with upregulation demonstrated following treatment with HMAs [74]. A clinical trial exploring the combination of azacitidine with nivolumab or ipilimumab or both is currently being conducted (NCT02530463). Adoptive cell therapy with the use of chimeric antigen receptor (CAR) expressing T cells and NK cells is also being explored in myeloid malignancies [75].
Finally, therapies designed to specifically target cytopenias are under investigation. Luspatercept and sotatercept, both of which are fusion proteins involving the human activin receptor (type IIB and IIA, respectively) and Fc portion of IgG, have shown promise in treating anemia in lower risk MDS patients [76, 77]. Eltrombopag, a thrombopoietin receptor agonist, is also under evaluation in CMML patients with thrombocytopenia, though concerns have been raised regarding potential for increased blast counts and transformation to AML [78].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. https://doi.org/10.1182/blood-2016-03-643544. This is the most recent update to the WHO classification of myeloid malignancies, published in 2016, and contains the current criteria required to establish a diagnosis of CMML.
Smith GS. Chronic monocytic leukaemia. Br Med J. 1937;2(3991):1–26.2.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med. 1985;103(4):620–5.
Rollison DE, Howlader N, Smith MT, Strom SS, Merritt WD, Ries LA, et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001–2004, using data from the NAACCR and SEER programs. Blood. 2008;112(1):45–52. https://doi.org/10.1182/blood-2008-01-134858.
Wassie EA, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA, et al. Molecular and prognostic correlates of cytogenetic abnormalities in chronic myelomonocytic leukemia: a Mayo Clinic-French Consortium study. Am J Hematol. 2014;89(12):1111–5. https://doi.org/10.1002/ajh.23846.
Such E, Cervera J, Costa D, Sole F, Vallespi T, Luno E, et al. Cytogenetic risk stratification in chronic myelomonocytic leukemia. Haematologica. 2011;96(3):375–83. https://doi.org/10.3324/haematol.2010.030957.
Patnaik MM, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA, et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia. 2014;28(11):2206–12. https://doi.org/10.1038/leu.2014.125.
Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M, et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol. 2013;31(19):2428–36. https://doi.org/10.1200/JCO.2012.47.3314.
• Padron E, Garcia-Manero G, Patnaik MM, Itzykson R, Lasho T, Nazha A, et al. An international data set for CMML validates prognostic scoring systems and demonstrates a need for novel prognostication strategies. Blood Cancer J. 2015;5:e333. https://doi.org/10.1038/bcj.2015.53. Our group evaluated seven different prognostic scoring systems in a large cohort of 1800 patients and found that all systems were valid and comparable, though none of these included somatic mutations. This paper also validated the negative prognostic impact of ASXL1 mutation and, for the first time, identified an inferior OS associated with mutation in CBL.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6):2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. https://doi.org/10.1182/blood-2012-03-420489.
Germing U, Strupp C, Aivado M, Gattermann N. New prognostic parameters for chronic myelomonocytic leukemia. Blood. 2002;100(2):731–2; author reply 2–3.
Kantarjian H, O'Brien S, Ravandi F, Cortes J, Shan J, Bennett JM, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original International Prognostic Scoring System. Cancer. 2008;113(6):1351–61. https://doi.org/10.1002/cncr.23697.
Onida F, Kantarjian HM, Smith TL, Ball G, Keating MJ, Estey EH, et al. Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood. 2002;99(3):840–9.
Patnaik MM, Padron E, LaBorde RR, Lasho TL, Finke CM, Hanson CA, et al. Mayo prognostic model for WHO-defined chronic myelomonocytic leukemia: ASXL1 and spliceosome component mutations and outcomes. Leukemia. 2013;27(7):1504–10. https://doi.org/10.1038/leu.2013.88.
Such E, Germing U, Malcovati L, Cervera J, Kuendgen A, Della Porta MG, et al. Development and validation of a prognostic scoring system for patients with chronic myelomonocytic leukemia. Blood. 2013;121(15):3005–15. https://doi.org/10.1182/blood-2012-08-452938.
• Elena C, Galli A, Such E, Meggendorfer M, Germing U, Rizzo E, et al. Integrating clinical features and genetic lesions in the risk assessment of patients with chronic myelomonocytic leukemia. Blood. 2016;128(10):1408–17. https://doi.org/10.1182/blood-2016-05-714030. The CPSS-Mol model is the most recently created prognostic model and the most comprehensive with regard to incorporation of genetic information. It utilizes a genetic score that includes cytogenetics as well as the mutation status of ASXL1, RUNX1, NRAS, and SETBP1.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912–9. https://doi.org/10.1182/blood-2005-05-2004.
•• Symeonidis A, van Biezen A, de Wreede L, Piciocchi A, Finke J, Beelen D, et al. Achievement of complete remission predicts outcome of allogeneic haematopoietic stem cell transplantation in patients with chronic myelomonocytic leukaemia. A study of the Chronic Malignancies Working Party of the European Group for Blood and Marrow Transplantation. Br J Haematol. 2015;171(2):239–46. https://doi.org/10.1111/bjh.13576. Although there is no prospective data on allo-SCT in CMML, this is the largest retrospective series reported to date, with 513 patients included. Published by the European Group for Blood and Marrow Transplantation, 4-year OS and relapse-free survival of 33% and 27%, respectively, were observed.
Eissa H, Gooley TA, Sorror ML, Nguyen F, Scott BL, Doney K, et al. Allogeneic hematopoietic cell transplantation for chronic myelomonocytic leukemia: relapse-free survival is determined by karyotype and comorbidities. Biol Blood Marrow Transplant. 2011;17(6):908–15. https://doi.org/10.1016/j.bbmt.2010.09.018.
Koreth J, Pidala J, Perez WS, Deeg HJ, Garcia-Manero G, Malcovati L, et al. Role of reduced-intensity conditioning allogeneic hematopoietic stem-cell transplantation in older patients with de novo myelodysplastic syndromes: an international collaborative decision analysis. J Clin Oncol. 2013;31(21):2662–70. https://doi.org/10.1200/JCO.2012.46.8652.
Taussig DC, Davies AJ, Cavenagh JD, Oakervee H, Syndercombe-Court D, Kelsey S, et al. Durable remissions of myelodysplastic syndrome and acute myeloid leukemia after reduced-intensity allografting. J Clin Oncol. 2003;21(16):3060–5. https://doi.org/10.1200/JCO.2003.02.057.
Martino R, Iacobelli S, Brand R, Jansen T, van Biezen A, Finke J, et al. Retrospective comparison of reduced-intensity conditioning and conventional high-dose conditioning for allogeneic hematopoietic stem cell transplantation using HLA-identical sibling donors in myelodysplastic syndromes. Blood. 2006;108(3):836–46. https://doi.org/10.1182/blood-2005-11-4503.
Parker JE, Shafi T, Pagliuca A, Mijovic A, Devereux S, Potter M, et al. Allogeneic stem cell transplantation in the myelodysplastic syndromes: interim results of outcome following reduced-intensity conditioning compared with standard preparative regimens. Br J Haematol. 2002;119(1):144–54.
Brierley CK, Steensma DP. Allogeneic stem cell transplantation in myelodysplastic syndromes: does pretransplant clonal burden matter? Curr Opin Hematol. 2016;23(2):167–74. https://doi.org/10.1097/MOH.0000000000000217.
Damaj G, Duhamel A, Robin M, Beguin Y, Michallet M, Mohty M, et al. Impact of azacitidine before allogeneic stem-cell transplantation for myelodysplastic syndromes: a study by the Societe Francaise de Greffe de Moelle et de Therapie-Cellulaire and the Groupe-Francophone des Myelodysplasies. J Clin Oncol. 2012;30(36):4533–40. https://doi.org/10.1200/JCO.2012.44.3499.
Field T, Perkins J, Huang Y, Kharfan-Dabaja MA, Alsina M, Ayala E, et al. 5-Azacitidine for myelodysplasia before allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2010;45(2):255–60. https://doi.org/10.1038/bmt.2009.134.
Cogle CR, Imanirad I, Wiggins LE, Hsu J, Brown R, Scornik JC, et al. Hypomethylating agent induction therapy followed by hematopoietic cell transplantation is feasible in patients with myelodysplastic syndromes. Clin Adv Hematol Oncol. 2010;8(1):40–6.
• Kongtim P, Popat U, Jimenez A, Gaballa S, El Fakih R, Rondon G, et al. Treatment with hypomethylating agents before allogeneic stem cell transplant improves progression-free survival for patients with chronic myelomonocytic leukemia. Biol Blood Marrow Transplant. 2016;22(1):47–53. https://doi.org/10.1016/j.bbmt.2015.08.031. Although most evidence in this area is extrapolated from MDS patients, this study evaluated therapies preceding allo-SCT in 83 patients with CMML. Treatment with a HMA and achievement of bone marrow blasts < 5% prior to transplant were associated with improved PFS.
Hollenbach PW, Nguyen AN, Brady H, Williams M, Ning Y, Richard N, et al. A comparison of azacitidine and decitabine activities in acute myeloid leukemia cell lines. PLoS One. 2010;5(2):e9001. https://doi.org/10.1371/journal.pone.0009001.
Christman JK. 5-Azacytidine and 5-aza-2′-deoxycytidine as inhibitors of DNA methylation: mechanistic studies and their implications for cancer therapy. Oncogene. 2002;21(35):5483–95. https://doi.org/10.1038/sj.onc.1205699.
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the Cancer and Leukemia Group B. J Clin Oncol. 2002;20(10):2429–40. https://doi.org/10.1200/JCO.2002.04.117.
Kantarjian H, Issa JP, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106(8):1794–803. https://doi.org/10.1002/cncr.21792.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32. https://doi.org/10.1016/S1470-2045(09)70003-8.
Aribi A, Borthakur G, Ravandi F, Shan J, Davisson J, Cortes J, et al. Activity of decitabine, a hypomethylating agent, in chronic myelomonocytic leukemia. Cancer. 2007;109(4):713–7. https://doi.org/10.1002/cncr.22457.
Wijermans PW, Ruter B, Baer MR, Slack JL, Saba HI, Lubbert M. Efficacy of decitabine in the treatment of patients with chronic myelomonocytic leukemia (CMML). Leuk Res. 2008;32(4):587–91. https://doi.org/10.1016/j.leukres.2007.08.004.
Braun T, Itzykson R, Renneville A, de Renzis B, Dreyfus F, Laribi K, et al. Molecular predictors of response to decitabine in advanced chronic myelomonocytic leukemia: a phase 2 trial. Blood. 2011;118(14):3824–31. https://doi.org/10.1182/blood-2011-05-352039.
Costa R, Abdulhaq H, Haq B, Shadduck RK, Latsko J, Zenati M, et al. Activity of azacitidine in chronic myelomonocytic leukemia. Cancer. 2011;117(12):2690–6. https://doi.org/10.1002/cncr.25759.
Thorpe M, Montalvao A, Pierdomenico F, Moita F, Almeida A. Treatment of chronic myelomonocytic leukemia with 5-azacitidine: a case series and literature review. Leuk Res. 2012;36(8):1071–3. https://doi.org/10.1016/j.leukres.2012.04.024.
Fianchi L, Criscuolo M, Breccia M, Maurillo L, Salvi F, Musto P, et al. High rate of remissions in chronic myelomonocytic leukemia treated with 5-azacytidine: results of an Italian retrospective study. Leuk Lymphoma. 2013;54(3):658–61. https://doi.org/10.3109/10428194.2012.719617.
Ades L, Sekeres MA, Wolfromm A, Teichman ML, Tiu RV, Itzykson R, et al. Predictive factors of response and survival among chronic myelomonocytic leukemia patients treated with azacitidine. Leuk Res. 2013;37(6):609–13. https://doi.org/10.1016/j.leukres.2013.01.004.
Wong E, Seymour JF, Kenealy M, Westerman D, Herbert K, Dickinson M. Treatment of chronic myelomonocytic leukemia with azacitidine. Leuk Lymphoma. 2013;54(4):878–80. https://doi.org/10.3109/10428194.2012.730615.
•• Santini V, Allione B, Zini G, Gioia D, Lunghi M, Poloni A, et al. A phase II, multicentre trial of decitabine in higher-risk chronic myelomonocytic leukemia. Leukemia. 2018;32(2):413–8. https://doi.org/10.1038/leu.2017.186. This is the most recently published phase 2 study evaluating HMA use in a CMML-specific population. Forty-three predominantly high-risk patients were treated with decitabine with an overall response rate of 47% and median OS of 17 months, with a significant improvement in OS observed in responders (31 months in those with CR). No somatic mutation was predictive of response.
Itzykson R, Kosmider O, Cluzeau T, Mansat-De Mas V, Dreyfus F, Beyne-Rauzy O, et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia. 2011;25(7):1147–52. https://doi.org/10.1038/leu.2011.71.
Traina F, Visconte V, Elson P, Tabarroki A, Jankowska AM, Hasrouni E, et al. Impact of molecular mutations on treatment response to DNMT inhibitors in myelodysplasia and related neoplasms. Leukemia. 2014;28(1):78–87. https://doi.org/10.1038/leu.2013.269.
Bejar R, Lord A, Stevenson K, Bar-Natan M, Perez-Ladaga A, Zaneveld J, et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood. 2014;124(17):2705–12. https://doi.org/10.1182/blood-2014-06-582809.
• Alfonso A, Montalban-Bravo G, Takahashi K, Jabbour EJ, Kadia T, Ravandi F, et al. Natural history of chronic myelomonocytic leukemia treated with hypomethylating agents. Am J Hematol. 2017;92(7):599–606. https://doi.org/10.1002/ajh.24735. This is a large retrospective analysis of 151 CMML patients treated with HMA at a single institution. Several predictors of improved OS were observed, as was a higher rate of CR in those treated with decitabine compared to azacitidine (58.3% vs. 20.6%, p < 0.001). A dismal prognosis after HMA failure was identified, with median OS of 7 months after relapse.
Garcia-Manero G, Griffiths EA, Roboz GJ, Busque L, Wells RA, Odenike O, et al. A phase 2 dose-confirmation study of oral ASTX727, a combination of oral decitabine with a cytidine deaminase inhibitor (CDAi) cedazuridine (E7727), in subjects with myelodysplastic syndromes (MDS). Blood. 2017;130(Suppl 1):4274.
Savona MR, Kolibaba K, Conkling P, Kingsley EC, Becerra C, Morris JC, et al. Extended dosing with CC-486 (oral azacitidine) in patients with myeloid malignancies. Am J Hematol. 2018. https://doi.org/10.1002/ajh.25216.
Beran M, Estey E, O'Brien S, Cortes J, Koller CA, Giles FJ, et al. Topotecan and cytarabine is an active combination regimen in myelodysplastic syndromes and chronic myelomonocytic leukemia. J Clin Oncol. 1999;17(9):2819–30. https://doi.org/10.1200/JCO.1999.17.9.2819.
Wattel E, Guerci A, Hecquet B, Economopoulos T, Copplestone A, Mahe B, et al. A randomized trial of hydroxyurea versus VP16 in adult chronic myelomonocytic leukemia. Groupe Francais des Myelodysplasies and European CMML group. Blood. 1996;88(7):2480–7.
Tricot G, Boogaerts MA. The role of aggressive chemotherapy in the treatment of the myelodysplastic syndromes. Br J Haematol. 1986;63(3):477–83.
Kantarjian HM, O'Brien S, Huang X, Garcia-Manero G, Ravandi F, Cortes J, et al. Survival advantage with decitabine versus intensive chemotherapy in patients with higher risk myelodysplastic syndrome: comparison with historical experience. Cancer. 2007;109(6):1133–7. https://doi.org/10.1002/cncr.22508.
de Witte T, Suciu S, Verhoef G, Labar B, Archimbaud E, Aul C, et al. Intensive chemotherapy followed by allogeneic or autologous stem cell transplantation for patients with myelodysplastic syndromes (MDSs) and acute myeloid leukemia following MDS. Blood. 2001;98(8):2326–31.
Ross SD, Allen IE, Probst CA, Sercus B, Crean SM, Ranganathan G. Efficacy and safety of erythropoiesis-stimulating proteins in myelodysplastic syndrome: a systematic review and meta-analysis. Oncologist. 2007;12(10):1264–73. https://doi.org/10.1634/theoncologist.12-10-1264.
List AF, Baer MR, Steensma DP, Raza A, Esposito J, Martinez-Lopez N, et al. Deferasirox reduces serum ferritin and labile plasma iron in RBC transfusion-dependent patients with myelodysplastic syndrome. J Clin Oncol. 2012;30(17):2134–9. https://doi.org/10.1200/JCO.2010.34.1222.
Stone RM. How I treat patients with myelodysplastic syndromes. Blood. 2009;113(25):6296–303. https://doi.org/10.1182/blood-2008-09-038935.
Gattermann N. Overview of guidelines on iron chelation therapy in patients with myelodysplastic syndromes and transfusional iron overload. Int J Hematol. 2008;88(1):24–9. https://doi.org/10.1007/s12185-008-0118-z.
Garcia-Manero G, Gore SD, Kambhampati S, Scott B, Tefferi A, Cogle CR, et al. Efficacy and safety of extended dosing schedules of CC-486 (oral azacitidine) in patients with lower-risk myelodysplastic syndromes. Leukemia. 2016;30(4):889–96. https://doi.org/10.1038/leu.2015.265.
Garcia-Manero G, Savona MR, Gore SD, Scott BL, Cogle CR, Boyd T, et al. CC-486 (oral azacitidine) in patients with hematological malignancies who had received prior treatment with injectable hypomethylating agents (HMAs): results from phase 1/2 CC-486 studies. Blood. 2016;128(22):905.
Issa JJ, Roboz G, Rizzieri D, Jabbour E, Stock W, O'Connell C, et al. Safety and tolerability of guadecitabine (SGI-110) in patients with myelodysplastic syndrome and acute myeloid leukaemia: a multicentre, randomised, dose-escalation phase 1 study. Lancet Oncol. 2015;16(9):1099–110. https://doi.org/10.1016/S1470-2045(15)00038-8.
Montalban-Bravo G, Bose P, Alvarado Y, Daver NG, Ravandi F, Borthakur G, et al. Updated results from phase II study of guadecitabine for patients with higher risk myelodysplastic syndromes or chronic myelomonocytic leukemia. J Clin Oncol. 2017;35(15_suppl):7020. https://doi.org/10.1200/JCO.2017.35.15_suppl.7020.
Padron E, Painter JS, Kunigal S, Mailloux AW, McGraw K, McDaniel JM, et al. GM-CSF-dependent pSTAT5 sensitivity is a feature with therapeutic potential in chronic myelomonocytic leukemia. Blood. 2013;121(25):5068–77. https://doi.org/10.1182/blood-2012-10-460170.
• Padron E, Dezern A, Andrade-Campos M, Vaddi K, Scherle P, Zhang Q, et al. A multi-institution phase I trial of ruxolitinib in patients with chronic myelomonocytic leukemia (CMML). Clin Cancer Res. 2016;22(15):3746–54. https://doi.org/10.1158/1078-0432.CCR-15-2781. The results of a phase 1 study of ruxolitinib in CMML, which demonstrated safety and efficacy. Ruxolitinib was particularly successful at controlling splenomegaly and constitutional symptoms, suggesting an additional therapeutic option in patients presenting with such symptoms. Final combined phase 1/2 data will be reported soon.
Padron E, DeZern AE, Niyongere S, Ball MC, Balasis M, Ramadan H, et al. Promising results of a phase 1/2 clinical trial of ruxolitinib in patients with chronic myelomonocytic leukemia. Blood. 2017;130(Suppl 1):162.
Ma Y, Rix LR, Zhang Q, Balasis ME, Komrokji RS, Rix U, et al. Pacritinib (PAC) synergistically potentiates azacitidine (5AZA) cytotoxicity in chronic myelomonocytic leukemia (CMML). Blood. 2015;126(23):1658.
Buonamici S, Yoshimi A, Thomas M, Seiler M, Chan B, Caleb B, et al. H3B-8800, an orally bioavailable modulator of the SF3b complex, shows efficacy in spliceosome-mutant myeloid malignancies. Blood. 2016;128(22):966.
Seiler M, Yoshimi A, Darman R, Chan B, Keaney G, Thomas M, et al. H3B-8800, an orally available small-molecule splicing modulator, induces lethality in spliceosome-mutant cancers. Nat Med. 2018;24:497–504. https://doi.org/10.1038/nm.4493 https://www.nature.com/articles/nm.4493#supplementary-information,.
Borthakur G, Popplewell L, Boyiadzis M, Foran J, Platzbecker U, Vey N, et al. Activity of the oral mitogen-activated protein kinase kinase inhibitor trametinib in RAS-mutant relapsed or refractory myeloid malignancies. Cancer. 2016;122(12):1871–9. https://doi.org/10.1002/cncr.29986.
Patnaik MM, Sallman DA, Sekeres MA, Luger S, Bejar R, Hobbs GS, et al. Preliminary results from an open-label, phase 2 study of tipifarnib in chronic myelomonocytic leukemia (CMML). Blood. 2017;130(Suppl 1):2963.
Fenaux P, Raza A, Mufti GJ, Aul C, Germing U, Kantarjian H, et al. A multicenter phase 2 study of the farnesyltransferase inhibitor tipifarnib in intermediate- to high-risk myelodysplastic syndrome. Blood. 2007;109(10):4158–63. https://doi.org/10.1182/blood-2006-07-035725.
Patnaik MM, Gupta V, Gotlib JR, Carraway HE, Wadleigh M, Schiller GJ, et al. Results from ongoing phase 2 trial of SL-401 in patients with advanced, high-risk myeloproliferative neoplasms including chronic myelomonocytic leukemia. Blood. 2016;128(22):4245.
23rd Congress of the European Hematology Association Stockholm, Sweden, June 14–17, 2018. HemaSphere 2018;2(S1):1–1113. https://doi.org/10.1097/hs9.0000000000000060.
Yang H, Bueso-Ramos C, DiNardo C, Estecio MR, Davanlou M, Geng QR, et al. Expression of PD-L1, PD-L2, PD-1 and CTLA4 in myelodysplastic syndromes is enhanced by treatment with hypomethylating agents. Leukemia. 2014;28(6):1280–8. https://doi.org/10.1038/leu.2013.355.
Tang X, Yang L, Li Z, Nalin AP, Dai H, Xu T, et al. First-in-man clinical trial of CAR NK-92 cells: safety test of CD33-CAR NK-92 cells in patients with relapsed and refractory acute myeloid leukemia. Am J Cancer Res. 2018;8(6):1083–9.
Giagounidis A, Platzbecker U, Germing U, Götze K, Kiewe P, Mayer KT, et al. Luspatercept treatment leads to long term increases in hemoglobin and reductions in transfusion burden in patients with low or intermediate-1 risk myelodysplastic syndromes (MDS): preliminary results from the phase 2 PACE-MDS extension study. Blood. 2015;126(23):92.
Komrokji R, Garcia-Manero G, Ades L, Prebet T, Steensma DP, Jurcic JG, et al. Sotatercept with long-term extension for the treatment of anaemia in patients with lower-risk myelodysplastic syndromes: a phase 2, dose-ranging trial. Lancet Haematol. 2018;5(2):e63–72. https://doi.org/10.1016/S2352-3026(18)30002-4.
Ramadan H, Duong VH, Al Ali N, Padron E, Zhang L, Lancet JE, et al. Eltrombopag use in patients with chronic myelomonocytic leukemia (CMML): a cautionary tale. Clin Lymphoma Myeloma Leuk. 2016;16(16 Suppl):S64–6. https://doi.org/10.1016/j.clml.2016.02.009.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Anthony M. Hunter declares that he has no conflict of interest.
Ling Zhang declares that she has no conflict of interest.
Eric Padron has received research funding from Kura Oncology, Incyte Corporation, and KaloBios Pharmaceuticals.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Leukemia
Rights and permissions
About this article
Cite this article
Hunter, A.M., Zhang, L. & Padron, E. Current Management and Recent Advances in the Treatment of Chronic Myelomonocytic Leukemia. Curr. Treat. Options in Oncol. 19, 67 (2018). https://doi.org/10.1007/s11864-018-0581-6
Published:
DOI: https://doi.org/10.1007/s11864-018-0581-6