Abstract
Background
Planar bone scintigraphy (PBS) is a standard radiological technique to detect skeletal metastases from prostate cancer (PC), the addition of SPECT-CT to PBS improves its diagnostic accuracy. The aim of this study was to assess the additional value of targeted SPECT-CT with PBS in detecting skeletal metastasis form prostate cancer, considering resource implications in an Irish hospital setting.
Methods
54 PC patients with increased radiotracer uptake on PBS were retrospectively recruited from 2012 to 2013. All underwent targeted evaluation with SPECT-CT. PBS and SPECT-CT images were reviewed by two nuclear medicine radiologists and reported independently. The final diagnosis was made based on the CT finding corresponding to the area of radiotracer uptake.
Results
The mean age was 70.9 years (48–88 years) and median PSA at presentation was 13.9 ng/ml (4.2–215 ng/ml). 68.5 % (n = 37) men received treatment for PC while 31.5 % (n = 17) patients had not received treatment prior to PBS. 164 areas of increased radiotracer uptake were identified on PBS; 13 areas were characterised as metastatic on SPECT-CT; iliac bone (n = 3), ribs (n = 1), skull (n = 2), sacrum (n = 1), ischium (n = 1), femur (n = 3), thoracic spine (n = 1) and cervical spine (n = 1). 151 areas were characterised as benign on SPECT-CT. One area of increased radiotracer uptake in the ribs was subsequently described as indeterminate after evaluation with SPECT-CT.
Conclusion
SPECT-CT improves the diagnostic accuracy of PBS in detecting skeletal metastasis from PC and is superior to PBS alone in differentiating benign from malignant lesions. Notwithstanding resource implications of increased cost, specialist equipment and specialist manpower hours; we recommend the use of SPECT-CT in conjunction with PBS for targeted evaluation of suspicious bony lesions in this cohort of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer results in 563 deaths per year in the Republic of Ireland. Metastatic disease most frequently occurs in lymph nodes (74 %), bones (69 %), lungs (39 %), liver (40 %) and adrenal gland (11 %) [1]. Early detection and treatment of skeletal metastases is crucial to prevent serious complications of pathological fracture and spinal cord compression [2]. Planar bone scintigraphy (PBS) using technetium-99 m-labelled methylene diphosphonate (99mTc-MDP) is the standard radiological technique to detect skeletal metastasis from prostate cancer as it is widely available, relatively inexpensive and highly sensitive in detecting skeletal metastasis [3]. PBS does lack specificity, as many benign conditions, such as degenerative joint disease, infections, and benign bone tumours also exhibit increased uptake of radiotracer, and may result in false positive results [4–9]. The addition of SPECT-CT to PBS may improve accuracy in differentiating benign from malignant lesions by more precise anatomical localisation and attenuation correction of the radiotracer uptake on PBS, thus increasing the specificity [10–12].
The aim of this study was to evaluate our early experience in Ireland with the addition of SPECT-CT to PBS to detect skeletal metastasis from prostate cancer. In particular, we aim to evaluate the increased accuracy and potential clinical benefit of SPECT-CT versus increased demand on resources, including specialist equipment and specialist manpower hours.
Methods
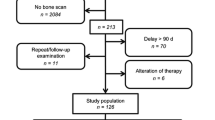
Fifty-four male prostate cancer patients were retrospectively recruited into this study from January 2012 to December 2013. All had increased radiotracer uptake on primary PBS and subsequently underwent immediate targeted evaluation with SPECT-CT. Institutional ethical board approval was granted for this study.
Standard PBS involved obtaining planar images of the entire skeleton 2–3 h after intravenous injection of 723.6 MBq 99mTc-MDP as specified by the Administration of Radioactive Substances Advisory Committee using a dual-head γ camera SPECT-CT system (Siemens Symbie True Point SPEC CT®). The PBS images were reviewed for increased radiotracer uptake by a nuclear medicine radiologist immediately after image acquisition. If increased areas of radiotracer uptake were detected, the patient then proceeded directly for targeted SPECT-CT for anatomic localisation and attenuation correction of all areas.
The PBS and SPECT-CT images were then independently reviewed by two nuclear medicine radiologists and reported separately. The final diagnosis was made based on the CT finding corresponding to the area of increased radiotracer uptake on PBS. Areas of radiotracer uptake on PBS were characterised as benign on SPECT-CT when degenerative changes, fractures, joint inflammation or infection were detected at the corresponding CT location. Metastatic lesions were diagnosed if they had the characteristic osteosclerotic morphology on SPECT-CT.
Results
The mean age was 70.9 years (48–88 years) and median PSA at presentation was 13.9 ng/ml (4.2–215 ng/ml). 70 % of patients (n = 38) had received treatment for prostate cancer prior to imaging while 30 % (n = 16) had not received any treatment prior to PBS.
The median PSA of patients with skeletal metastasis (n = 8) was 39.4 ng/ml (5.3–215 ng/ml) and the median PSA of those with benign lesions (n = 46) was 11.4 ng/ml (4.2–54.9 ng/ml). 75 % of patients with skeletal metastasis had received treatment prior to PBS; systemic treatment with androgen deprivation therapy in all cases (n = 6). 25 % had not received any treatment prior to PBS. Systemic treatment was administered to 17.4 % of patients with benign skeletal lesions (n = 8), 26.1 % received local treatment of surgery or radiotherapy (n = 12), 26.1 % received combined local and systemic treatment (n = 12) while 30.4 % had not received any treatment prior to PBS (n = 14). Patient demographics and treatment received prior to PBS are outlined in Table 1.
165 areas of increased radiotracer uptake were identified on PBS in 54 patients, all underwent targeted evaluated with SPECT-CT. Most areas were located in the spine, shoulder and knee joints (Table 2).
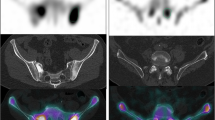
13 areas of increased uptake in 8 patients were characterised as metastatic lesions on SPECT-CT. Metastatic sites included; iliac bone (n = 3), ribs (n = 1), skull (n = 2), sacrum (n = 1), ischium (n = 1), femur (n = 3), thoracic spine (n = 1) and cervical spine (n = 1) (Fig. 1a,b; Table 2).
151 areas of increased uptake in 46 patients were characterised as benign lesions on subsequent SPECT-CT. Benign lesions included; degenerative change in the hand (n = 6), wrist (n = 7), shoulder (n = 13), sternum (n = 1), ribs (n = 2), cervical spine (n = 7), thoracic spine (n = 15), lumbar spine (n = 20), sacroiliac joint (n = 2), hip joint (n = 11), knee joint (n = 21), ankle (n = 2), tarsus (n = 4) and foot (n = 13); inflammation in the acromioclavicular joint (n = 1), mandible (n = 2), sacroiliac joint (n = 1) and ischial tuberosity (n = 1). Infection of the sterno-clavicular joint (n = 1); cervical spondylosis (n = 5); diffused idiopathic hyperostosis of the thoracic spine (n = 1); osteophytosis of the lumbar spine (n = 1); old fractures involving the sternum (n = 1), ribs (n = 5), femur (n = 1) and tibia (n = 1); previous sternotomy (n = 1); bursitis of the greater trochanter of the femur (n = 2); an old bone infarct of the iliac bone (n = 1); and osteoma of the skull (n = 1) (Table 2).
One area of increased radiotracer uptake in the ribs was subsequently described as indeterminate after evaluation with SPECT-CT.
Discussion
The primary goal of PBS in patients with prostate cancer is early detection of bony metastases that can lead to serious complications of pathological fracture and spinal cord compression. Differentiation between benign and malignant lesions can be difficult on PBS alone, as PBS primarily provides functional, rather than anatomical, information about a bony lesion [13]. The addition of SPECT-CT for targeted evaluation of equivocal lesions can differentiate between benign and malignant lesions [13]. The detection of fractures, degenerative changes or joint infection on CT, in corresponding location with increased 99mTc-labelled diphosphonate uptake on PBS determines the benign nature of these lesions. The specificity of PBS has been shown to improve from 69 to 92 % when combined with SPECT-CT on a patient-based analysis; on lesion-based analyses, the specificity improved from 39 to 71 % [11]. The increased specificity of SPECT-CT has also been previously reported for lower thoracic, lumbar, skull, rib-cage, long bone and pelvic lesions [11, 12, 14, 15].
Our initial Irish experience with SPECT-CT in conjunction with PBS supports the current literature. All patients studied had a suspected or confirmed diagnosis of prostate cancer prior to PBS. Those with benign skeletal lesions were younger, and had a lower PSA at presentation. Systemic treatment with androgen deprivation therapy had been administered to a greater proportion of patients with malignant skeletal lesions than those with benign lesions; indicating that systemic treatment did not alter the presence or progression to metastatic disease in these patients. A greater proportion of patients with benign skeletal lesions had initially received local treatment; while a similar proportion of patients with benign and malignant lesions had not received any treatment prior to PBS.
Targeted SPECT-CT was performed on all patients in this study with areas of increased radiotracer uptake on PBS, correctly distinguishing 13 metastatic lesions from 151 benign lesions in a total of 164 areas of increased radiotracer uptake. Metastatic lesions were found in the skull, spine, pelvis and femur. Benign lesions were also diagnosed on SPECT-CT in these areas; as benign lesions were found throughout the skeleton (Table 2). This indicates that SPECT-CT can differentiate between benign and metastatic lesions at the same anatomic location. If PBS alone is used, the area of increased radiotracer uptake on this imaging modality appears the same in benign and malignant lesions. Benign lesions, as diagnosed by SPECT-CT, were largely secondary to degenerative change; indicating that SPECT-CT was particularly helpful in identifying osteoarthritis in areas of radiotracer uptake on PBS. Old rib fractures frequently pose a specificity challenge on PBS as they have similar characteristics to metastatic deposits. SPECT-CT increases specificity sufficiently to correctly diagnose these lesions as benign. The use of SPECT-CT in our institution has certainly proved to be a useful diagnostic tool for the early detection of skeletal metastases in prostate cancer patients.
The addition of SPECT-CT to PBS increases the overall cost of image acquisition as two imaging modalities are used. SPECT-CT costs 1.5 times that of PBS [16]. Additional time is needed for acquisition of the SPECT-CT image and additional manpower hours are required to review and compare both images. However, it is likely that the increased costs are offset by a more accurate diagnosis, reducing time to treatment and patient anxiety from an unknown diagnosis. Radiation dose is increased with the addition of SPECT-CT, from 3 to 5 mSv [16]. SPECT-CT alone may not be sufficient in some cases for precise localisation of bony lesions; further correlation with MRI may also be required [17]. Despite imaging with PBS and SPECT-CT in our study, one rib lesion was still described as indeterminate. Conversely, separate imaging modalities are not required for all patients, necessitating correct identification of those patients in whom both imaging modalities are needed to influence patient care and outcome [10].
By confirming or excluding the presence of skeletal metastasis in prostate cancer patients, SPECT-CT also has implications on treatment plan, quality of life and overall patient survival. Earlier detection of metastatic disease will result in earlier initiation of hormonal treatment, or palliative radiotherapy for painful bone metastases. An earlier and more definitive diagnosis of skeletal metastases can also alleviate patient anxiety that may result from an inconclusive PBS.
This is a single-centre, retrospective analysis of 54 patients over a 2-year period, and so is liable to selection and recall bias. However, each PBS and SPECT-CT image was reviewed by two independent radiologists; supporting the validity of our results. Histopathological evaluation of bony lesions was not performed, as is standard practice; skeletal metastasis was identified by radiologic studies alone and subsequent clinical course. Our study was limited to prostate cancer patients, excluding those with metastatic disease from other primary cancers.
Conclusion
This initial report of the Irish experience of the use of PBS in conjunction with SPECT-CT has found that SPECT-CT improves the diagnostic accuracy of PBS in detecting skeletal metastasis from prostate cancer, and is superior to PBS alone in differentiating benign from malignant lesions. Notwithstanding the associated increased radiation dose and resource implications; including available facilities, specialist manpower hours, and costs; we now recommend the judicious use of SPECT-CT in conjunction with PBS for targeted evaluation of suspicious areas of radiotracer uptake in this cohort of patients.
References
Hassan FU, Mohan HK, Gnanasegaran G, Vijayanathan S, Fogelman I (2011) Beware of the focal uptake at the ischium on the bone scan in prostate cancer. Nucl Med Commun 32(4):320–323 Epub 2011/01/13
Saitoh H, Hida M, Shimbo T, Nakamura K, Yamagata J, Satoh T (1984) Metastatic patterns of prostatic cancer. Correlation between sites and number of organs involved. Cancer 54(12):3078–3084 (Epub 1984/12/15)
Strobel K, Burger C, Seifert B, Husarik DB, Soyka JD, Hany TF (2007) Characterization of focal bone lesions in the axial skeleton: performance of planar bone scintigraphy compared with SPECT and SPECT fused with CT. Am J Roentgenol 188(5):W467–W474
Jacobson AF, Fogelman I (1998) Bone scanning in clinical oncology: does it have a future? Eur J Nucl Med 25(9):1219–1223 (Epub 1998/09/02)
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ (2003) Radionuclide bone imaging: an illustrative review. Radiographics 23(2):341–358 (Epub 2003/03/18)
Palmedo H, Marx C, Ebert A, Kreft B, Ko Y, Turler A et al (2014) Whole-body SPECT/CT for bone scintigraphy: diagnostic value and effect on patient management in oncological patients. Eur J Nucl Med Mol Imaging 41(1):59–67 (Epub 2013/08/27)
Schirrmeister H, Guhlmann A, Elsner K, Kotzerke J, Glatting G, Rentschler M et al (1999) Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med Off Publ Soc Nucl Med 40(10):1623–1629 (Epub 1999/10/16)
Schirrmeister H, Glatting G, Hetzel J, Nussle K, Arslandemir C, Buck AK et al (2001) Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med Off Publ Soc Nucl Med 42(12):1800–1804 (Epub 2001/12/26)
Minoves M (2003) Bone and joint sports injuries: the role of bone scintigraphy. Nucl Med Commun 24(1):3–10 (Epub 2002/12/26)
Cook GJ, Ott RJ (2001) Dual-modality imaging. Eur Radiol 11(10):1857–1858 (Epub 2001/11/10)
Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I (2006) The detection of bone metastases in patients with high-risk prostate cancer: Tc-99 m-MDP planar bone scintigraphy, single- and multi-field-of-view SPECT, F-18-fluoride PET, and F-18-fluoride PET/CT. J Nucl Med 47(2):287–297
Savelli G, Maffioli L, Maccauro M, De Deckere E, Bombardieri E (2001) Bone scintigraphy and the added value of SPECT (single photon emission tomography) in detecting skeletal lesions. Q J Nucl Med 45(1):27–37
Utsunomiya D, Shiraishi S, Imuta M, Tomiguchi S, Kawanaka K, Morishita S et al (2006) Added value of SPECT/CT fusion in assessing suspected bone metastasis: comparison with scintigraphy alone and nonfused scintigraphy and CT. Radiology 238(1):264–271 (Epub 2005/11/24)
Even-Sapir E, Martin RH, Barnes DC, Pringle CR, Iles SE, Mitchell MJ (1993) Role of SPECT in differentiating malignant from benign lesions in the lower thoracic and lumbar vertebrae. Radiology 187(1):193–198 (Epub 1993/04/01)
Savelli G, Maffioli L, Maccauro M, De Deckere E, Bombardieri E (2001) Bone scintigraphy and the added value of SPECT (single photon emission tomography) in detecting skeletal lesions. Q J Nucl Med 45(1):27–37 (Epub 2001/07/18)
Helyar V, Mohan HK, Barwick T, Livieratos L, Gnanasegaran G, Clarke SE et al (2010) The added value of multislice SPECT/CT in patients with equivocal bony metastasis from carcinoma of the prostate. Eur J Nucl Med Mol Imaging 37(4):706–713 (Epub 2009/12/18)
Rybak LD, Rosenthal DI (2001) Radiological imaging for the diagnosis of bone metastases. Q J Nucl Med 45(1):53–64 (Epub 2001/07/18)
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McLoughlin, L.C., O’Kelly, F., O’Brien, C. et al. The improved accuracy of planar bone scintigraphy by adding single photon emission computed tomography (SPECT-CT) to detect skeletal metastases from prostate cancer. Ir J Med Sci 185, 101–105 (2016). https://doi.org/10.1007/s11845-014-1228-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-014-1228-7