Abstract
Objection
We aimed to evaluate the role of bone scintigraphy (BS) which has long been the imaging modality of choice in prostate cancer (PCa) and performed a head-to-head comparison between BS, BS + SPECT/CT and 68 Ga-PSMA-PET/CT, for the detection of bone metastasis of PCa.
Methods
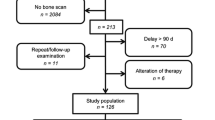
We evaluated 138 PCa patients who underwent BS and 68 Ga-PSMA PET/CT and SPECT/CT of 102 of 138 patients. Images were interpreted retrospectively and areas of abnormally increased tracer uptake related to PCa were documented as benign, metastatic or equivocal. Equivocal uptakes were finally diagnosed based on a consensus review of correlative imaging. Patient- and lesion-based analysis was performed. Patients with superscan images were excluded from lesion-based analysis.
Results
At least one metastatic or equivocal uptake in skeleton was defined in 76 of 138 (55%) BS, in 33 of 102 (32.3%) SPECT/CT, and in 49 of 138 (35.5%) 68 Ga-PSMA PET/CT. 23 (16.7%) patients had also superscan findings on BS and 68 Ga-PSMA PET/CT. For patient-based analysis, sensitivity, specificity, accuracy, PPV, and NPV were calculated as 91.1%, 64.5%, 73.1%, 55.4% and 93.7% for BS; 95.5%, 82.7%, 86.9%, 72.8% and 96.2% for BS + SPECT/CT; 97.7%, 95.7%, 95.6%, 91.6% and 98.8% for 68 Ga-PSMA PET/CT. For lesion-based analysis, sensitivity, specificity, accuracy, PPV, and NPV were 53%, 63.9%, 60.1%, 42.8% and 71.8% for BS; 59.2%, 87.6%, 77.7%, 62.6% and 80% for BS + SPECT/CT; 96.4%, 98.1%, 97.5%, 96.4% and 98.1% for 68 Ga-PSMA PET/CT.
Conclusion
This study has shown that 68 Ga-PSMA PET/CT overcomes the limitations of BS and proves superiority in detecting bone metastases, even in patients with SPECT/CT. Our findings present important implications that 68 Ga-PSMA PET/CT can replace BS in future practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) remains one of the most common cancers in men and incidence is increasing in recent years [1, 2]. Due to the early detection of disease, most patients have a localized disease at initial diagnosis; however, distant metastasis can occur in 35% of cases during follow-up [3]. Bone is the most common site of metastasis, detected in more than 80% of PCa patients with a high risk of morbidity [4]. Bone scintigraphy (BS) has been widely used for the detection of bone metastasis in PCa, for several decades. Although bone scintigraphy has advantages such as low cost and whole-body examination in single imaging, false-positive lesions are defined in almost 25% of patients and requires additional imaging for final diagnosis [5]. In addition to planar BS, SPECT/CT helps in evaluation of equivocal lesions and decreases false-positive rate [6]. Although, the diagnostic accuracy is improved with additional SPECT/CT, bone marrow metastasis, millimetric or lytic bone metastasis are usually missed with both modalities [7]. Besides that, flare phenomenon may cause false positivity on BS, due to osteoblastic response to healing bone metastases [8]. Recently, 68 Ga-PSMA PET/CT has been introduced, using prostate-specific membrane antigen (PSMA) as a target cell surface transmembrane protein, which significantly overexpressed in most of the PCa cases [9]. 68 Ga-PSMA PET/CT has remarkable detection rates for metastasis of PCa, even at low PSA levels [10, 11]. Despite lack of definite evidence, 68 Ga-PSMA PET/CT is rapidly being adopted into clinical practice. Haran et al. reported that, there was a 45.7% decline in the use of bone scintigraphy for PCa staging, after the commence of 68 Ga-PSMA PET/CT in their clinic [12]. However, recent EAU Guideline (2019) recommends 68 Ga-PSMA PET/CT for only biochemical recurrence (BCR) and still recommends BS for staging intermediate and high-risk PCa or restaging symptomatic patients, irrespective of serum PSA levels, based on the fact that limited published data are not clear [13]. Thus, we aimed to evaluate the role of BS which has long been the imaging modality of choice in PCa and performed a head-to-head comparison between BS, BS + SPECT/CT and 68 Ga-PSMA-PET/CT, for the detection of bone metastasis of PCa.
Materials and methods
Patients
One hundred and thirty-eight patients with PCa who underwent both BS and 68 Ga-PSMA PET/CT within 4 weeks of time span, between 2015 and 2019, were enrolled to this retrospective study. Mean age was 66 (range, 49–92 years), median PSA level of patients was 18.3 ng/ml (range: 0.3–853) and median Gleason score (GS) was 8 (range: 6–10). 68 Ga-PSMA PET/CT and BS were performed for staging in 77 patients and BCR in 61 patients. Additional SPECT/CT imaging was performed in 102 patients (73.9%). BS was performed before and after 68 Ga-PSMA PET/CT in 128 and 10 cases, respectively. Patient characteristics are given in Table 1. This retrospective study was approved by our institutional review board, and written informed consent was waived.
Bone scintigraphy and SPECT/CT
BS was performed 3 h after the intravenous injection of 740 MBq (20 mCi) 99 m-Tc-MDP. Whole-body planar images were acquired at a table speed of 12 cm per minute using a 256 × 1024 matrix, by a dual head SPECT or a dedicated SPECT/CT gamma camera (Discovery NM 630, GE Healthcare, Chicago, USA or NM/CT 670; GE Healthcare, Waukesha, USA) installed with low-energy, high-resolution collimators. Additional regional planar images and SPECT/CT images were acquired, when there was suspicious findings on planar BS. SPECT images were acquired 60 frames, 20 s per frame over 360°, 128 × 128 matrix, with a body contoured scan. Images were reconstructed by iterative reconstruction and reconstructed images were corrected for scatter and attenuation. Low-dose CT images were obtained with the protocol of 70 mA, 120 kV, pitch 1.375, tube rotation time of 0.5 s and a slice thickness of 1.25 mm. All imaging data were reviewed and processed on a Xeleris workstation (GE Healthcare).
68 Ga-PSMA synthesis and PET/CT acquisition
We applied 68 Ga-PSMA labeling according to the protocol as described in the literature [14]. 68 Ga-PSMA PET-CT was performed at 45–60 min after the intravenous injection of approximately 185 MBq of 68 Ga-PSMA on a dedicated PET-CT scanner (Biograph TruePoint PET/CT; Siemens Healthcare. Erlangen, Germany). All patients were scanned from the top of the head through the upper thigh. Additionally, late pelvic images were acquired in all patients. CT acquisition was performed on a spiral CT scanner, with a slice thickness of 4 mm and a pitch of 1. After CT scan, 3D-PET images were acquired for 3 min per bed for limited whole-body imaging and late pelvic imaging. CT-based attenuation correction of the emission images was used. PET images were reconstructed by the iterative method using ordered-subset expectation maximization (OSEM; 2 iterations and 8 subsets).
Image analysis
All images were reviewed blindly by two experienced nuclear medicine physicians. Areas of abnormally increased tracer uptake related to PCa were documented as benign, metastatic or equivocal for BS, BS + SPECT/CT and 68 Ga-PSMA PET/CT, based on light of morphologic information on CT images. Lesion numbers and regions were defined for all imaging modalities. 1–3 bone metastases were defined as oligometastatic, 4–20 bone metastases were defined as multimetastatic bone involvement. Scans with numerous bone metastases on skeleton (> 20) were defined as superscan. All equivocal uptakes in bone/bone marrow were finally diagnosed based on a consensus review of at least one correlative imaging (BS, CT, MRI or 68 Ga-PSMA PET/CT) and clinical data at initial or follow-up visit, based on previously described flowchart reported by Werner et al. [15]. Histological verification was not performed for osseous metastasis. Patient-based analysis was performed based on the presence or lack of bone metastasis. Patients with metastatic superscan were not included in lesion-based analysis due to the numerous bone metastases. In remaining patients, lesions with increased and equivocal uptake counted as positive for lesion-based analysis on BS, BS + SPECT/CT and 68 Ga-PSMA PET/CT separately. Subgroup analysis were performed based on the clinic status of patients by dividing staging and BCR group.
Statistical analysis
Sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) were calculated for patient- and lesion-based analysis. Receiver-operating characteristics (ROC) analysis including calculation of the area under the curve (AUC) was performed with MedCalc Software (Version 19.2.1) for diagnostic accuracy of imaging modalities and comparison of ROC curves. p value lower than 0.05 was considered significant.
Results
According to imaging results, at least one metastatic or equivocal uptake was defined 76 of 138 (55%), 33 of 102 (32.3%), and 49 of 138 (35.5%) patients in BS, BS + SPECT/CT and 68 Ga-PSMA PET/CT scans, respectively. 23 (16.7%) patients who had widespread bone metastases were interpreted as superscan with BS and 68 Ga-PSMA PET/CT. Details of metastatic and equivocal uptakes of all imaging modalities including final results are given in Table 2.
BS vs. BS + SPECT/CT: false-positive/negative results
BS determined 97 equivocal uptakes in 30 of 76 patients. 50 (51.5%) equivocal uptakes were revealed as benign pathologies, and 14 (14.4%) equivocal uptakes interpreted as metastasis in SPECT/CT. 33 of 97 uptakes remained equivocal, and in 22 of them SPECT/CT was not conclusive; thus, further imaging was required. Finally, 30 of them were documented as benign and 3 of them as bone metastasis with correlative imaging. False-positive uptakes were mostly located in vertebral column (43.1%) and ribs (29.5%) (Fig. 1).
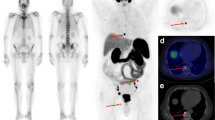
An 87-year-old male who had radical prostatectomy 3 years ago was referred to our clinic due to biochemical recurrence (GS: 4 + 4, PSA:5.17 ng/ml). Intense osteoblastic uptake in sacral fracture was detected in BS (a, b) and SPECT/CT (d, f). Beyond that equivocal uptakes in cervical and thoracic vertebrae (b) in BS was interpreted as benign arthritic changes by SPECT/CT. The sacral uptake was interpreted as suspicious for pathologic fracture, due to the lack of any other bone metastasis which was explaining elevated PSA levels. In 68 Ga-PSMA PET/CT (c), no PSMA uptake was detected in sacrum (e), interpreted as benign sacral fracture. However, intense PSMA uptake was detected in a pheriferally sclerotic lesion located in left iliac bone (g, yellow arrow), which was negative on BS + SPECT/CT (a, b, f). 68 Ga-PSMA PET/CT defined benign and malign lesions accurately. Patient received salvage radiotherapy
In 16 of 138 patients (11.5%), 53 bone metastases were missed in BS. False-negative lesions were mostly located in vertebral column (39.5%) and pelvis (35.4%) (Fig. 2). SPECT/CT has revealed 7 metastatic lesions which were missed in BS, and the number of false-negative lesions was reduced to 46 in 10 patients (7.2%) with SPECT/CT.
A 77-year-old male with newly diagnosed prostate cancer was referred to our clinic for initial staging (GS: 4 + 5, PSA:155 ng/ml). Despite the patient had high PSA level, only 3 equivocal uptakes in left 1st rib (d, yellow arrow), 8th thoracic vertebra (f, yellow arrow) and left iliac bone (j, yellow arrow) were detected in BS (a, b) and SPECT/CT (d, f, j) images. In 68 Ga-PSMA PET/CT (c), intense PSMA uptake in left 1st rib (e, yellow arrow), 8th thoracic vertebra (g, yellow arrow) and left iliac bone (k, yellow arrow) determined as bone metastases and additionally unknown PSMA avid metastatic lesions were detected in right glenoid (c, red arrow), ribs (c, blue arrows), 5th lumbar vertebra (i, red arrow), right iliac bone (i, yellow arrow) and multiple metastatic lymph nodes (a). Metastatic status of patient was upgraded from oligometastatic disease to limited multimetastatic disease and patient received systemic therapy
68 Ga-PSMA PET/CT: false-positive/negative results
Four (2.8%) equivocal PSMA bone uptake required further investigations in 138 68 Ga-PSMA PET/CT scans. False-positive PSMA uptake due to healing trauma in the ribs (n = 2), arthritic changes in the sacrum (n = 1) and medullary infarction (n = 1) in the femur were determined as false positive based on correlative imaging.
68 Ga-PSMA PET/CT missed 4 metastatic lesions in only 2 of 138 patients (1.4%). Missed lesions showed low or no PSMA uptake, but increased osteoblastic uptake which was determined in SPECT/CT (Fig. 3).
A 70-year-old male who had radical prostatectomy 6 years ago was referred to our clinic due to biochemical recurrence (GS: 4 + 3, PSA:12,3 ng/ml). In 68 Ga-PSMA PET/CT (c, e, g, i), sclerotic lesions located in right iliac bone (k, yellow arrow), right femur (o, yellow arrow) and right ischium (o, red arrow) had only mild PSMA uptake and a PSMA-negative sclerotic lesion in left ischium (m, yellow arrow) was also detected. Beyond that, BS (a, b) determined unknown metastatic lesions in 4th thoracic vertebra corpus (d, yellow arrow) and left transvers procesus (f, yellow arrow), right iliac crest (h, yellow arrow) and left ischium (l) in addition to right iliac bone (j, yellow arrow), right femur (n, yellow arrow) and right ischium (n, red arrow), which were correlated with SPECT/CT images. Metastatic status of patient was upgraded from oligometastatic disease to limited multimetastatic disease. Patient received systemic therapy; however, PSA increased under the therapy. In follow-up BS imaging, multiple new lesions were detected
Patient-based analysis
Patient-based analysis revealed a sensitivity, specificity, accuracy, PPV, and NPV of 91.1%, 64.5%, 73.1%, 55.4% and 93.7% for BS; 95.5%, 82.7%, 86.9%, 72.8% and 96.2% for BS + SPECT/CT; 97.7%, 95.7%, 95.6%, 91.6% and 98.8% for 68 Ga-PSMA PET/CT, respectively. Accuracy of the diagnostic test as measured by ROC was significantly higher for 68 Ga-PSMA PET/CT than for BS (AUC:0.967 vs AUC:0.778, p ≤ 0.0001) and BS + SPECT/CT (AUC:0.967 vs AUC:0.892, p = 0.0238); while, it was higher for BS + SPECT/CT than BS alone (AUC:0.892 vs AUC:0.778, p = 0.0006). Details are given in Table 3.
Lesion-based analysis
Superscan images were excluded in lesion-based analysis. Sensitivity, specificity, accuracy, PPV, and NPV were 53%, 63.9%, 60.1%, 42.8% and 71.8% for BS; 59.2%, 87.6%, 77.7%, 62.6% and 80% for BS + SPECT/CT; 96.4%, 98.1%, 97.5%, 96.4% and 98.1% for 68 Ga-PSMA PET/CT for each lesion, respectively. Accuracy of the diagnostic test as measured by ROC was significantly higher for 68 Ga-PSMA PET/CT than for BS (AUC:0.973 vs AUC:0.585, p ≤ 0.0001) and BS + SPECT/CT (AUC:0.973 vs AUC:0.725, p ≤ 0.0001), while higher for BS + SPECT/CT than BS alone (AUC:0.725 vs AUC:0.585, p ≤ 0.0001). Details are given in Table 3.
Subgroup analysis
Staging group
In 77 patients, 17 patients had bone metastasis with 61.53 ng/ml median PSA value. In 7 of 17 patients (41%), superscan findings were detected on all imaging modalities. The remaining 60 patients had no bone metastasis and median PSA level of the patients was 17.6 ng/ml. For patient-based analysis; sensitivity, specificity, accuracy, PPV, and NPV were 88.2%, 63.3%, 68.8%, 40.5% and 95% for BS; 88.2%, 81.6%, 83.1%, 57.6% and 96.1 for BS + SPECT/CT; 100%, 96.6%, 97.4%, 89.4% and 100% for 68 Ga-PSMA PET/CT. Accuracy of the diagnostic test as measured by ROC was significantly higher for 68 Ga-PSMA PET/CT than for BS (AUC:0.983 vs AUC:0.758, p = 0.0003) and BS + SPECT/CT (AUC:0.983 vs AUC:0.850, p = 0.0160), and higher for BS + SPECT/CT than BS alone (AUC:0.8501 vs AUC:0.758, p = 0.0209). For lesion-based analysis; sensitivity, specificity, accuracy, PPV, and NPV were 38.8%, 51.1%, 46.7%, 30.6% and 60% for BS; 42.8%, 81.8%, 67.8%, 56.7% and 72% for BS + SPECT/CT; 100%, 97.7%, 98.5%, 96.1% and 100% for 68 Ga-PSMA PET/CT. Accuracy of the diagnostic test as measured by ROC was significantly higher for 68 Ga-PSMA PET/CT than for BS (AUC:0.989 vs AUC:0.550, p ≤ 0.0001) and BS + SPECT/CT (AUC:0.989 vs AUC:0.623, p ≤ 0.0001); while, no statistical differences were found between BS and BS + SPECT/CT (AUC:0.550 vs AUC:0.623, p = 0.0761). Details are given in Table 4.
BCR group
In 61 patients, 28 patients had bone metastasis with 47.5 ng/ml median PSA value. In 16 of 28 patients (57%), superscan findings were detected on all imaging modalities. The remaining 33 patients had no bone metastasis and median PSA level of the patients was 4.59 ng/ml. For patient-based analysis; sensitivity, specificity, accuracy, PPV, and NPV were 92.8%, 66.6%, 78.6%, 70.2% and 91.6% for BS, 100%, 84.8%, 91.8%, 84.8% and 100 for BS + SPECT/CT; 94.4%, 93.9%, 95%, 93.1% and 96.8% for 68 Ga-PSMA PET/CT. Accuracy of the diagnostic test as measured by ROC was significantly higher for 68 Ga-PSMA PET/CT than for BS (AUC:0.952 vs AUC:0.798, p = 0.036) and higher for BS + SPECT/CT than BS alone (AUC:0.924 vs AUC:0.798, p = 0.0406); while, no statistical differences were found between BS + SPECT/CT and 68 Ga-PSMA PET/CT (AUC:0.924 vs AUC:0.952, p = 0.534). For lesion-based analysis; sensitivity, specificity, accuracy, PPV, and NPV were 64%, 64.2%, 64.1%, 52.5% and 77.5% for BS; 71.8%, 90.2%, 83.9%, 76.6% and 86% for BS + SPECT/CT; 93.7%, 98.3%, 96.7%, 96.7% and 96.8% for 68 Ga-PSMA PET/CT. Accuracy of the diagnostic test as measured by ROC was significantly higher for 68 Ga-PSMA PET/CT than for BS (AUC:0.961 vs AUC:0.670, p ≤ 0.0001) and BS + SPECT/CT (AUC:0.961 vs AUC:0.802, p ≤ 0.0001), and higher for BS + SPECT/CT than BS alone (AUC:0.670 vs AUC:0.802, p = 0.0001). Details are given in Table 4.
Additional findings of 68 Ga-PSMA PET/CT
68 Ga-PSMA PET/CT defined at least one non-osseous metastasis in 43 patients (31.1%) who had no bone metastasis. Overall, increased PSMA uptake was determined in prostate/prostatic bed in 107 patients (77.5%). Gross invasion to the seminal vesicle, bladder or rectum was reported in 23 patients (16.6%). At least one PSMA-positive lymph node was defined in 61 patients (44.2%). Pelvic lymph nodes were defined in 58 patients (42%), abdominal lymph nodes were defined in 28 patients (20.2%) and supradiaphragmatic lymph nodes were defined in 17 patients (12.3%). Visceral metastases were detected in 8 patients (4.7%), located in lung (n: 7) and liver (n: 3). In addition, a suspicious brain uptake was determined as meningioma by MRI findings, and an incidental suspicious PSMA avid mass in kidney was revealed as renal cell carcinoma, histopathologically.
According to final diagnosis, 93 (67.4%) patients had no bone metastasis, 12 (8.7%) patients had oligometastasis, 10 (7.2%) patients had multimetastasis and 23 (16.7%) patients showed metastatic superscan findings. 68 Ga-PSMA PET/CT altered the status of bone involvement in 5 patients (3.6%) by defining unknown bone metastasis (n: 3), and by upgrading to oligo/multimetastatic disease (n: 2), adjunct to BS + SPECT/CT findings. Additionally, 68 Ga-PSMA PET/CT reduced false-positive results in 27 patients (19.5%) and detected non-osseous metastases in 43 patients (31.1%) who had no bone metastasis.
Discussion
Recent EAU Guideline (2019) recommends 68 Ga-PSMA PET/CT for only BCR and still recommends BS for staging intermediate- and high-risk PCa or restaging symptomatic patients, irrespective of serum PSA levels [13]. BS may be replaced by more sensitive tests in PCa staging; however, definite evidence is not present yet, according to EAU. Zacho et al. published a systematic review of the literature and concluded that previous studies have limited clinical evidence for the use of 68 Ga-PSMA PET/CT in the evaluation of bone in PCa [16]. Thus, we performed a head-to-head comparison between BS, BS + SPECT/CT and 68 Ga-PSMA-PET/CT, regarding the determination of bone metastasis of PCa. Based on our results, 68 Ga-PSMA PET/CT was superior to BS for patient-based analysis, with especially high specificity, accuracy and PPV, even in the cases with additional SPECT/CT. The sensitivity was 91.1–95.5%, favorable for BS and BS + SPECT/CT for patient-based analyses; however, it decreased to 53–59.2% for lesion-based analyses, while it was 96.4% for 68 Ga-PSMA PET/CT. Since the number of bone metastases may change the therapy management, correct identification of all bone lesions is crucial. According to lesion-based analysis, 68 Ga-PSMA PET/CT had excellent results for correct identification of lesions, compared to BS and BS + SPECT/CT, including all diagnostic parameters.
Pyka et al. reported a study with 126 patients and reported that 68 Ga-PSMA PET/CT outperforms BS for detection of overall bone involvement in PCa, with 100% sensitivity and 87.1% specificity; while, BS has 84.6% and 45.2%; BS + SPECT has 88.5% and 51.6% sensitivity and specificity, respectively, when all equivocal uptakes are accepted as positive in patient-based analysis [17]. A possible explanation for the higher specificity in our study maybe the higher proportion of SPECT/CT images (73.9%) compared to the study by Pyka et al. (45.2%) and all SPECT images in our study were performed on a dedicated SPECT/CT with integrated CT images, unlike the study by Pyka et al. The diagnostic accuracy of 68 Ga-PSMA PET/CT was statistically higher than BS and BS + SPECT in that study, similar to our results. However, they found no statistical differences in diagnostic accuracy of BS and BS + SPECT, unlike our study.
False-positive osteoblastic uptake due to benign bone pathologies is the most common pitfall of BS that requires further imaging and decreases diagnostic accuracy [5]. Additionally, flare phenomenon may cause false positivity in BS, due to the consisting osteoblastic healing processes after therapy [8]. In the present study, specificity, accuracy and PPV markedly increases with additional SPECT/CT, due to the contribution of anatomic and morphologic information of CT. However, 68 Ga-PSMA PET/CT was still superior to BS + SPECT/CT, with limited number of false-positive patients, similar to a previous study by Janssen et al. [18]. False-positive lesions defined by BS were mostly localized to vertebral column and ribs, where the benign osteoblastic uptakes are mostly seen due to the trauma or benign degenerative changes. In present study, limited number of patients had false-positive lesions with mild PSMA uptake on 68 Ga-PSMA PET/CT, diagnosed as benign bone pathologies. In the literature, non-metastatic PSMA uptake in bone is reported in several case reports [19,20,21,22]. Increased vascularity can cause the PSMA uptake, and it should be aware of these pitfalls when interpreting 68 Ga-PSMA PET/CT. Beyond that, several studies reported the impact of androgen deprivation therapies, which can alter the PSMA expression of metastases based on the short or long term of usage [23,24,25]. However, the outcomes of reported studies are controversial. In fact, 68 Ga-PSMA PET/CT can accurately evaluate therapy response without being affected by flare phenomenon of therapies, unlike BS imaging, according to the reported studies [26, 27].
Until now, all large retrospective series of BS results were mostly correlated with other imaging before using 68 Ga-PSMA PET/CT scan. According to an epidemiologic study in North America, sensitivity, specificity, accuracy, PPV, and NPV were reported as 90.8%, 76.3%, 76.5%, 5.7% and 99.8% for BS, respectively [5]. Although the reported sensitivity of BS was high, bone marrow metastasis, millimetric or lytic bone metastasis is easily missed with BS [7]. Yuminaga et al. recently reported a study, which investigated PSA failure in 384 post-prostatectomy patients with 68 Ga-PSMA PET/CT, CT and BS, and revealed that 68 Ga-PSMA PET/CT detected bone metastasis in 6.7% of patients with negative BS [28]. In our cohort, BS totally missed 53 lesions in 11.5% of patients. SPECT/CT reduced the number of missing lesions to 46 in 7.2% of patients; while, 68 Ga-PSMA PET/CT defined all missing lesions correctly. On the other hand, 68 Ga-PSMA PET/CT missed only 4 metastatic lesions in 2 patients who were described as metastatic by SPECT/CT with increased osteoblastic activity. It is known that up to 10% of prostate cancers appear not to express PSMA glycoprotein [29], and should be remembered that false negativity of 68 Ga-PSMA PET/CT can occur rarely.
In our subgroup analysis, the sensitivity and specificity of BS and BS + SPECT/CT were higher in BCR group compared with staging group, especially in lesion-based analysis. In staging group, the sensitivity and specificity were reduced to 38.8% and 51.1% for BS; 42.8% and 81.8% for BS + SPECT/CT in lesion-based analysis; while, 68 Ga-PSMA PET/CT has 100% sensitivity and 97.7% specificity. 68 Ga-PSMA PET/CT had significantly higher diagnostic power than BS and BS + SPECT/CT for both staging and BCR group, according to lesion-based analysis. In the patient-based analysis, 68 Ga-PSMA PET/CT was only superior to BS, when the SPECT/CT was not performed. Our patient profile was heterogenous including different PSA levels and stages. The proportion of superscan images was mostly detected in BCR group. Therefore, the diagnostic impact of 68 Ga-PSMA PET/CT on detection of bone involvement was limited in BCR group when SPECT/CT was used. Soydal et al. also performed subgroup analysis in PCa patients, and reported poor sensitivity and specificity for BS, 50% and 19.2% in staging group; and 33.3% and 40% in BCR group, when all equivocal uptakes are accepted as positive in patient-based analysis [30]. In that study, SPECT/CT was not performed conversely to our study, and diagnostic performance of BS was found limited. According to our results, 68 Ga-PSMA PET/CT seems to be more useful for both staging and BCR of PCa patients, by defining lesions accurately comparing with BS including SPECT/CT.
Overall, 68 Ga-PSMA PET/CT altered the therapy management by defining unknown bone metastasis or upgrading bone involvement to oligo/multimetastasis in 3.6% of the patients, by decreasing false-positive rate in 19.5% of the patients, and by detection of non-osseous metastases in 31.1% of the patients with no bone metastasis. 68 Ga-PSMA PET/CT correctly determined non-osseous metastasis of PCa, as a prominent advantage compared to BS, owing to excellent diagnostic power in detecting bone involvement of PCa. Large series of 68 Ga-PSMA PET/CT findings reported high numbers of non-osseous metastasis of PCa and pointed out that non-osseous metastases were mostly underdiagnosed by routine imaging modalities [10, 11, 31]. In the present study, 68 Ga-PSMA PET/CT defined at least one non-osseous metastasis, in 43 patients without bone metastasis. Overall, lymph node metastasis was defined in 44.2% of the patients whereas visceral metastases were defined in 4.7% of total patients. Incidentally, PSMA avid meningioma and renal cell carcinoma were detected by 68 Ga-PSMA PET/CT. Even well-designed cost-effective studies are not published yet, 68 Ga-PSMA PET/CT seems to be useful and cost effective in appropriate patient, by avoiding incorrect therapies and reducing the waste of money and resources, according to a recently published review [32]. Based on our results, 68 Ga-PSMA PET/CT seems more beneficial in detecting metastasis for patients with none or oligo bone metastases, instead of widespread metastatic disease (superscan) and BS had no contribution to 68 Ga-PSMA PET/CT, unless tumors had no PSMA expression which is very rare.
The main limitation of the present study was the lack of histopathological verification for metastatic lesions which was not possible due to the practical and ethical reasons. The other limitation was the retrospective design of analysis and heterogeneous patient profile with different PSA level and GS.
Conclusion
The purpose of this study was to evaluate the potential of 68 Ga-PSMA PET/CT to overcome the limitations of BS which has long been the imaging of choice in PCa despite its poor specificity. This study has shown that 68 Ga-PSMA PET/CT not only overcomes these limitations and proves superiority in detecting bone metastases, but also shows non-osseous metastases which can alter patient management. In this regard, our findings present important implications that 68 Ga-PSMA PET/CT can replace BS in future practice.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA. 2017;67(1):7–30.
Arnold M, Karim-Kos HE, Coebergh JW, Byrnes G, Antilla A, Ferlay J, et al. Recent trends in incidence of five common cancers in 26 European countries since 1988: analysis of the European Cancer Observatory. Eur J Cancer. 2015;51(9):1164–87.
Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol. 2000;31(5):578–83.
Sturge J, Caley MP, Waxman J. Bone metastasis in prostate cancer: emerging therapeutic strategies. Nat Rev Clin Oncol. 2011;8(6):357.
Preisser F, Mazzone E, Nazzani S, Marchioni M, Bandini M, Tian Z, et al. North American population-based validation of the National Comprehensive Cancer Network Practice Guideline Recommendations for locoregional lymph node and bone imaging in prostate cancer patients. Bone. 2018;194(98):4.
Palmedo H, Marx C, Ebert A, Kreft B, Ko Y, Türler A, et al. Whole-body SPECT/CT for bone scintigraphy: diagnostic value and effect on patient management in oncological patients. Eur J Nucl Med Mol Imaging. 2014;41(1):59–67.
Lengana T, Lawal IO, Boshomane TG, Popoola GO, Mokoala KM, Moshokoa E, et al. 68Ga-PSMA PET/CT replacing bone scan in the initial staging of skeletal metastasis in prostate cancer: a fait accompli? Clin Genitourin cancer. 2018;16(5):392–401.
Pollen JJ, Witztum K, Ashburn WL. The flare phenomenon on radionuclide bone scan in metastatic prostate cancer. Am J Roentgenol. 1984;142(4):773–6.
Sweat SD, Pacelli A, Murphy GP, Bostwick DG. Prostate-specific membrane antigen expression is greatest in prostate adenocarcinoma and lymph node metastases. Urology. 1998;52(4):637–40.
Afshar-Oromieh A, Holland-Letz T, Giesel FL, Kratochwil C, Mier W, Haufe S, et al. Diagnostic performance of 68 Ga-PSMA-11 (HBED-CC) PET/CT in patients with recurrent prostate cancer: evaluation in 1007 patients. Eur J Nucl Med Mol Imaging. 2017;44(8):1258–68.
Yaxley JW, Raveenthiran S, Nouhaud F-X, Samaratunga H, Yaxley WJ, Coughlin G, et al. Risk of metastatic disease on 68gallium-prostate-specific membrane antigen positron emission tomography/computed tomography scan for primary staging of 1253 men at the diagnosis of prostate cancer. Bju Int. 2019;124(3):401–7.
Haran C, McBean R, Parsons R, Wong D. Five-year trends of bone scan and prostate-specific membrane antigen positron emission tomography utilization in prostate cancer: a retrospective review in a private centre. J Med Imaging Radiat Oncol. 2019;63:495–9.
Mottet N, van den Bergh R, Briers E, Cornford P, De Santis M, Fanti S, et al. EAU-EANM-ESTRO-ESUR-SIOG. Eur Urol. 2019;76:790–813.
Sanli Y, Kuyumcu S, Sanli O, Buyukkaya F, İribaş A, Alcin G, et al. Relationships between serum PSA levels, Gleason scores and results of 68Ga-PSMAPET/CT in patients with recurrent prostate cancer. Ann Nucl Med. 2017;31(9):709–17.
Werner RA, Bundschuh RA, Bundschuh L, Javadi MS, Higuchi T, Weich A, et al. Molecular imaging reporting and data systems (MI-RADS): a generalizable framework for targeted radiotracers with theranostic implications. Ann Nucl Med. 2018;32(8):512–22.
Zacho HD, Nielsen JB, Haberkorn U, Stenholt L, Petersen LJ. 68Ga-PSMA PET/CT for the detection of bone metastases in prostate cancer: a systematic review of the published literature. Clin Physiol Funct Imaging. 2018;38(6):911–22.
Pyka T, Okamoto S, Dahlbender M, Tauber R, Retz M, Heck M, et al. Comparison of bone scintigraphy and 68Ga-PSMA PET for skeletal staging in prostate cancer. Eur J Nucl Med Mol Imaging. 2016;43(12):2114–211.
Janssen J-C, Meißner S, Woythal N, Prasad V, Brenner W, Diederichs G, et al. Comparison of hybrid 68 Ga-PSMA-PET/CT and 99m Tc-DPD-SPECT/CT for the detection of bone metastases in prostate cancer patients: additional value of morphologic information from low dose CT. Eur Radiol. 2018;28(2):610–9.
Artigas C, Alexiou J, Garcia C, Wimana Z, Otte F, Gil T, et al. Paget bone disease demonstrated on (68) Ga-PSMA ligand PET/CT. Eur J Nucl Med Mol Imaging. 2016;43(1):195–6.
De Coster L, Sciot R, Everaerts W, Gheysens O, Verscuren R, Deroose CM, et al. Fibrous dysplasia mimicking bone metastasis on 68 GA-PSMA PET/MRI. Eur J Nucl Med Mol Imaging. 2017;44(9):1607–8.
Jochumsen MR, Madsen MA, Gammelgaard L, Bouchelouche K. Lumbar Osteophyte Avid on 68Ga-Prostate-Specific Membrane Antigen PET/CT. Clin Nucl Med. 2018;43(6):456–7.
Jochumsen MR, Dias AH, Bouchelouche K. Benign traumatic rib fracture: a potential pitfall on 68Ga-prostate-specific membrane Antigen PET/CT for prostate cancer. Clin Nucl Med. 2018;43(1):38–40.
Wright GL, Grob BM, Haley C, Grossman K, Newhall K, Petrylak D, et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology. 1996;48(2):326–34.
Afshar-Oromieh A, Debus N, Uhrig M, Hope TA, Evans MJ, Holland-Letz T, et al. Impact of long-term androgen deprivation therapy on PSMA ligand PET/CT in patients with castration-sensitive prostate cancer. Eur J Nucl Med Mol Imaging. 2018;45(12):2045–54.
Liu T, Wu LY, Fulton MD, Johnson JM, Berkman CE. Prolonged androgen deprivation leads to downregulation of androgen receptor and prostate-specific membrane antigen in prostate cancer cells. Int J Oncol. 2012;41(6):2087–92.
Schmidkonz C, Cordes M, Goetz TI, Prante O, Kuwert T, Ritt P, et al. 68Ga-PSMA-11 PET/CT derived quantitative volumetric tumor parameters for classification and evaluation of therapeutic response of bone metastases in prostate cancer patients. Ann Nucl Med. 2019;33(10):766–75.
Schmuck S, von Klot CA, Henkenberens C, Sohns JM, Christiansen H, Wester H-J, et al. Initial experience with volumetric 68Ga-PSMA I&T PET/CT for assessment of whole-body tumor burden as a quantitative imaging biomarker in patients with prostate cancer. J Nucl Med. 2017;58(12):1962–8.
Yuminaga Y, Rothe C, Kam J, Beattie K, Arianayagam M, Bui C, et al. 68Ga-PSMA PET/CT versus CT and bone scan for investigation of PSA failure post radical prostatectomy. Asian J Urol. 2020. https://doi.org/10.1016/j.ajur.2020.02.001.
Wright GL Jr, Haley C, Beckett ML, Schellhammer PF, editors. Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urologic oncology: Seminars and Original Investigations. Amsterdam: Elsevier; 1995.
Soydal C, Nak D, Araz M, Akkus P, Urun Y, Ozkan E, et al. Comparison of bone scintigraphy and Ga-68 prostate-specific membrane antigen positron emission tomography/computed tomography in the detection of bone metastases of prostate carcinoma. Nucl Med Commun. 2019;40(12):1243–9.
Simsek DH, Sanli Y, Kuyumcu S, Engin MN, Buyukkaya F, Demirci E. Clinical impact of lower limb imaging in 68Ga-PSMA PET-CT for patients with prostate cancer. J Nucl Med Technol. 2019. https://doi.org/10.2967/jnmt.118.224303.
Morigi JJ, Anderson J, Fanti S. Promise of PET imaging in prostate cancer: improvement or waste of money? Curr Opin Urol. 2020;30(1):9–16.
Funding
The authors have no financial or personal relationships with other people or organizations that could inappropriately influence this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simsek, D.H., Sanli, Y., Civan, C. et al. Does bone scintigraphy still have a role in the era of 68 Ga-PSMA PET/CT in prostate cancer?. Ann Nucl Med 34, 476–485 (2020). https://doi.org/10.1007/s12149-020-01474-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-020-01474-7