Abstract
Sclerosing mesenteritis is an uncommon and poorly understood inflammatory condition of the bowel mesentery which can often be confused with neoplasia, Crohn’s disease and other inflammatory conditions. We describe a case of complete small bowel obstruction and right sided hydronephrosis due to sclerosing mesenteritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case study
A 53-year-old female, presented with a 3-day history of abdominal pain, vomiting, abdominal distension and spiking pyrexia, with raised inflammatory markers. In the past she had similar but less severe attacks of abdominal pain for which she was investigated with gastroscopy, colonoscopy and ultrasound but no cause was found.
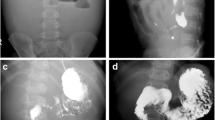
Abdominal examination revealed a large mass and tenderness in right iliac fossa. Computerized tomography (CT) of abdomen confirmed the presence of a large nonspecific inflammatory mass in the right iliac fossa, along with right sided hydronephrosis and ascitic fluid in the abdomen (Fig. 1). Despite conservative management the patient failed to improve and right hemi-colectomy with distal small bowel resection was performed.
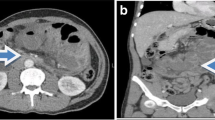
Surgical specimen showed replacement of fat in the mesentery of small intestine by fibrous tissue. In addition, fibrous tissue also replaced fat around blood vessels and nerves (Fig. 2). Furthermore, histopathology confirmed a SM (Fig. 3).
She had a good postoperative recovery for a short period. However, after 4–6 weeks her symptoms of abdominal pain and diarrhoea returned along with markedly elevated inflammatory markers. Therefore, she was commenced on 60 mg prednisolone and azathioprine 50 mg daily. Currently her symptoms are controlled with 125 mg of azathioprine and 5 mg of prednisolone.
The patient underwent cystoscopy and right retrograde pyelogram. Her hydronephrosis was due to extrinsic pressure on the ureter by inflamed mesentery that improved with steroids and azathioprine.
This case highlights the diagnostic and therapeutic challenges in managing patients with this disease, especially as its signs and symptoms can mimic a number of other benign and malignant conditions.
Discussion
Sclerosing mesenteritis is an uncommon and poorly understood inflammatory condition of the bowel mesentery which can often be confused with neoplasia, Crohn’s disease and other inflammatory conditions [1]. It encompasses a spectrum of diseases depending on histology. At one end of the spectrum inflammatory cells predominate in the mesentery when it is called mesenteric panniculitis while at the other hand the replacement of the mesenteric fat by fibrous tissue is the predominant feature, when it is called retractile mesenteritis [2].
It is nearly twice as common in males compared to females (1:1.9) and can occur in any age but is usually seen in the sixth decade of life [3]. The aetiology is poorly understood, however, various mechanisms such as trauma (including surgery), allergic, infections and autoimmune have been postulated as potential cause of SM [4]. In a review by Mayo clinic of 92 patients with SM about 40% cases had history of intra-abdominal surgery; most of them had either cholecystectomy or appendectomy [5].
Abdominal pain is the most common symptom of SM that is either due to inflammation in the mesentery or ischemia secondary to compression of the mesenteric blood vessels. In some cases mesenteric mass can compress the bowel, blood vessels and lymphatics resulting in intestinal obstruction, abdominal pain and chylous ascites. In addition to these symptoms, SM has been reported to be associated with protein losing enteropathy [6], autoimmune haemolytic anaemia [7], pyrexia of unknown origin [7] and retroperitoneal fibrosis [1].
Although histology is considered to be the gold standard in the diagnosis, CT imaging can reveal several nonspecific signs which may suggest SM. These include the so-called misty mesentery or hyperattenuated appearance of mesenteric fat on CT as well as the fat ring sign, describing preserved fat around mesenteric vessels [8].
Histologically SM encompasses spectrum of diseases which include fat necrosis in the early stages and replacement of fat by fibrosis on the other [2]. Clinically SM can progress in three different ways including partial or complete resolution, non-progressive or an aggressive course [2]. The clinical course and best option of treatment in SM was reviewed by a retrospective analysis, in which 92 cases of SM were retrospectively analysed for 23 years. Disease was self limiting in more than half of the patients (52%), only 13% patients were treated with surgery alone, with response rate of about 10%. Surgery followed by medical treatment was employed in 9% cases, with response rate of 20%. While the response rate was 41% in remaining 26% cases that were treated with medical therapy only [5].
A variety of immuno-suppressive agents such as prednisolone and azathioprine [9] have been successfully used in the treatment of SM. In addition, tamoxifen [5] along with prednisolone have also been used with success in the treatment of SM. In our case, azathioprine and steroid are used with success. She has responded well to azathioprine and plan is to wean her off steroid in long term and treat with azathioprine only.
This case report highlights the difficulties in diagnosing and managing this uncommon condition, it also suggests a trial of azathioprine may be of benefit for patients with poorly controlled disease, especially as a steroid sparing agent.
References
Lim CS, Singh RG, Tibrewal S et al (2006) SM presenting with small bowel obstruction and subsequent retroperitoneal fibrosis. Eur J of Gastroenterol Hepatol 18(12):1285–1287
Emory TS, Monihan JM, Carr NJ et al (1997) SM, mesenteric panniculitis and mesenteric lipodystrophy: a single entity? Am J Surg Path 21(4):392–398
Lyche SC (1996) Miscellaneous diseases of the peritoneum and mesentery. In: Freidman SL (ed) Current diagnosis and treatment in gastroenterology. Appleton and Lange, Norwalk, pp 141–150
Schaffler A, Scholmerich J, Buchler C (2005) Mechanisms of disease: adipocytokines and visceral adipose tissue—emerging role in intestinal and mesenteric diseases. Nat Clin Pract Gastroenterol Hepatol 2:103–111
Akram S, Pardi DS, Schaffner JA et al (2007) SM clinical feature, treatment and outcome in ninety-two patients. Clin Gastronterol Hepatol 5:589–596
Rajendran B, Duerksen DR (2006) Retractile mesenteritis presenting as protein-losing gastroenteropathy. Can J Gastroenterol 20:787–789
Papadaki HA, Kouroumalis EA, Stefanaki K et al (2000) Retractile mesenteritis presenting as fever of unknown origin and autoimmune haemolytic anaemia. Digestion 61:145–148
Winterbottom A, Choudhary AK, Freeman AH et al (2006) The CT appearance of SM and associated diseases. Clin Radiol 61:652–658
Bala A, Coderre SP, Johnson DR et al (2001) Treatment of SM with corticosteroids and azathioprine. Can J Gastroenterol 15:533–535
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hassan, T., Balsitis, M., Rawlings, D. et al. Sclerosing mesenteritis presenting with complete small bowel obstruction, abdominal mass and hydronephrosis. Ir J Med Sci 181, 393–395 (2012). https://doi.org/10.1007/s11845-010-0495-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-010-0495-1